Abstract
Objective
To compare the acceptance rates of written versus verbal pharmacotherapy recommendations made by pharmacy students on an ambulatory care advanced pharmacy practice experience (APPE).
Methods
Fourth-year pharmacy students made written and verbal pharmacotherapy recommendations to resident physicians in an internal medicine clinic at an urban, teaching hospital over a 10-month period. The types of recommendations and outcomes of the interventions were recorded using a data collection form to determine differences in acceptance rates for written versus verbal recommendations. The recommendation types and corresponding acceptance rates were also compared.
Results
Of 542 pharmacotherapy recommendations made by 14 APPE students during the 10-month study period, 65.1% were written and 34.9% were verbal. Of the 189 verbal recommendations, 97.9% were accepted, compared with 83.6% of written recommendations (p < 0.0001). The most frequent types of recommendations and overall rates of acceptance were dosage change (87.0%), laboratory monitoring (85.8%), and medication initiation based on evidence-based medicine guidelines (79.3%).
Conclusion
Verbal pharmacotherapy recommendations made by pharmacy students were accepted by resident physicians at a significantly higher rate than written recommendations in an outpatient internal medicine clinic.
Keywords: clinical interventions, ambulatory care, interprofessional relationships, pharmacotherapy, advanced pharmacy practice experience (APPE), outcomes
BACKGROUND
Advanced pharmacy practice experiences (APPEs) must include direct interaction with diverse patient populations in a variety of practice settings and involve collaboration with other healthcare professionals to prepare pharmacy students for their future role as clinical healthcare providers. In addition, ACPE requires that student performance, nature, and extent of healthcare professional interactions must be documented and assessed.1 As healthcare providers, pharmacists must communicate with physicians and other healthcare professionals regarding pharmacotherapy concerns. Typically, APPE students’ pharmacotherapy recommendations are made under the supervision of the clinical pharmacy preceptor, either through verbal communication with physicians or via an intervention form placed in the patient's medical record. Documenting the number and type of pharmacotherapy recommendations a student makes during an APPE is an effective method to determine the quality and quantity of interactions with physicians and other healthcare professionals.
Student-initiated pharmacotherapy recommendations play an important role in improving patient care and reducing costs in inpatient and outpatient settings.2-7 Interventions in an outpatient ambulatory care clinic made by a clinical pharmacist not only improved patient care, but also yielded a cost savings 4 times the pharmacist salary when compared to a similar clinic without a pharmacist.8,9 To date, there have been no studies that compared pharmacy students’ written versus verbal recommendations in an ambulatory clinic setting. The purpose of this study was to compare the acceptance rates of written versus verbal pharmacotherapy recommendations made by pharmacy students completing an ambulatory care APPE in an outpatient internal medicine clinic.
METHODS
Between March 2007 and February 2008 (excluding July and December 2007), fourth-year pharmacy students completing a 5-week ambulatory care APPE made written and verbal pharmacotherapy recommendations to resident physicians in an internal medicine clinic at an urban, teaching hospital. The timeframe is consistent with the months that students were completing the APPE at the internal medicine clinic. Students reviewed patient medical records the day prior to patients’ appointments, focusing on disease states and corresponding pharmacotherapy. Each medication in the patient profile was reviewed for appropriate indications and dosing regimen. Laboratory data were reviewed for all patients, and appropriate monitoring parameters were recommended for each prescribed medication. Patients’ treatment regimens were compared to clinical practice guidelines for chronic disease states (eg, diabetes, hypertension, heart failure, dyslipidemia), and medication initiation or titration recommendations were made based on evidence-based medicine. Upon clinic discharge, each patient's prescription was reviewed for accuracy and completeness.
If a written recommendation was deemed necessary, a pharmacotherapy note was completed, cosigned by the preceptor, and placed in the front of the patient's medical record (not a permanent part of the medical record) for the resident physician to review. The pharmacotherapy notes were written on a standardized form and contained objective patient information (eg, current medication list, laboratory results, most recent vital signs) and recommendations. To increase resident physician awareness of the written recommendations, the pharmacotherapy notes were on blue paper, a unique color in the medical record, and placed in a prominent location within the medical record.
Students’ verbal recommendations were made to the resident physician at the point of care, while the physician was examining the patient. If a verbal recommendation was deemed necessary, it was discussed with the clinical pharmacy preceptor prior to the student independently discussing the recommendation with the resident physician.
The types of recommendations and outcomes of the interventions were documented daily using a data collection form. Verbal and written recommendation types on the data collection form included: dose change, frequency change, laboratory monitoring, initiate medication, discontinue medication, clarification, and cost-savings opportunity. Clarifications requested were for illegible prescriptions, drug allergies, and inconsistencies in medication name, dose, or frequency between the medical record and prescriptions written. Outcomes documentation on the data collection form noted whether each recommendation was accepted or declined. If the resident physician took no action, the recommendation was considered declined.
The primary endpoint was to determine differences in acceptance rates for written versus verbal recommendations made by pharmacy students to resident physicians. Secondary endpoints included comparing specific recommendation types and their corresponding acceptance rates. The primary endpoint was analyzed using chi-square statistics; secondary endpoints were summarized with descriptive statistics. A p value less than or equal to 0.05 was considered significant.
RESULTS
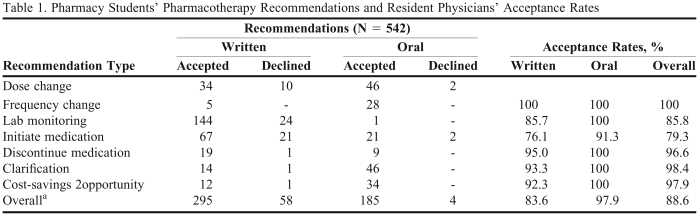
Five hundred forty-two pharmacotherapy recommendations were made by 14 students during the 10-month study period. The average number of recommendations per student was 38.7 (range 27 - 52) and 65% (353) were written. The physician acceptance rate for all pharmacotherapy recommendations was 88.6% (Table 1), with 97.9% of verbal recommendations accepted compared to 83.6% of written recommendations (p < 0.0001).
Table 1.
Pharmacy Students’ Pharmacotherapy Recommendations and Resident Physicians’ Acceptance Rates
ap < 0.0001
The most frequent types of pharmacotherapy recommendations included: laboratory monitoring (n = 169, 31.2%); medication initiation based on evidence-based medicine guidelines (n = 111, 20.5%); and dosage change (n = 92, 17%). The acceptance rate for frequency change was the same for both written and verbal recommendations. For all other types, verbal recommendations had a higher acceptance rate than written recommendations.
DISCUSSION
Pharmacy students’ pharmacotherapy recommendations, both verbal and written, were well received by physicians, with verbal recommendations accepted at a significantly higher rate than written recommendations (97.9% vs 83.6%, respectively). Previously documented acceptance rates for pharmacy students’ verbal and written recommendations range from 64% and 95%.2-7,10 Verbal recommendations may have a higher rate of acceptance due to student's face-to-face time with the resident physician and the opportunity to engage in discussions regarding patient-specific recommendations. Although the resident physicians in this study were trained to look for the pharmacotherapy notes in the medical record, the possibility exists that the students’ written recommendations were overlooked.
No other study had examined the difference in physician acceptance of verbal versus written recommendations by pharmacy students completing an APPE in an outpatient setting. In a 5-month study of pharmacy students’ written and verbal recommendations in an internal medicine inpatient setting, 82.8% of verbal recommendations were accepted compared to 54.2% of written recommendations.10 Although the types of recommendations made differed from those in our study, verbal recommendations were accepted at a higher rate than written recommendations for all top 5 recommendation types (indication for use, inappropriate dose, inappropriate drug, inappropriate route, and duplicate therapy), leading the investigators to conclude that pharmacy students should participate in inpatient teaching rounds as a part of their experiential education to maximize the potential for verbal recommendations and impact favorably patient care.10
Several limitations have been identified in this study. While pharmacy students’ written recommendations were easily verified and reviewed via the students’ pharmacotherapy notes in the medical record; verbal recommendations were subject to student recall and documentation skills. Although verbal recommendations were discussed with the preceptor before the student shared them with the resident physician, the possibility exists that the student might not have documented some verbal recommendations on intervention forms. Therefore, there may have been more verbal recommendations than documented.
An additional limitation was the students’ dependence on the medical record information for the written recommendations. Patient status may have changed significantly since the patient's last visit to the internal medicine clinic, medications could have been adjusted, or pertinent laboratory monitoring could have been completed by a healthcare provider outside the health system.
No correlation was attempted regarding the time during the 5-week APPE that recommendations were made to determine if professional familiarity between the resident physician and specific students affected the acceptance rates of recommendations. Also, it was not determined whether the resident physician felt external pressure to accept the pharmacotherapy recommendations. Even though the student discussed the recommendation with the resident physician one-on-one, it is possible that the attending physician overheard the conversation and that influenced whether the recommendations were accepted or declined. Also, because the pharmacotherapy notes were color-coded and located in a prominent place in the medical record, they could be viewed by other healthcare providers. This may also have influenced the resident physician's acceptance of the recommendations.
No specific evaluation of students’ communication abilities was completed. Even though all verbal recommendations were discussed with the clinical pharmacy preceptor prior to the student independently making the recommendation to the resident physician, no assessment of the students’ oral communication techniques were documented. All written recommendations; however, were reviewed and cosigned by the preceptor prior to being placed in the medical record to assure that written recommendations were communicated appropriately.
This study revealed that pharmacy students’ verbal communication with resident physicians was more effective than written communication, based on the rates of pharmacotherapy recommendation acceptance. To maximize students’ pharmacotherapy recommendations in the future, resident physicians may require additional training on the purpose of written pharmacotherapy recommendation notes. Students should communicate verbally with resident physicians regarding written pharmacotherapy recommendations that are not addressed (neither accepted nor declined).
CONCLUSION
Pharmacy students’ pharmacotherapy recommendations, both written and verbal were well received by resident physicians in an outpatient internal medicine clinic. Pharmacy students’ face-to-face interactions with physicians regarding pharmacotherapy recommendations resulted in a significantly higher rate of acceptance than recommendations made via written communication.
REFERENCES
- 1. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Accreditation Council for Pharmacy Education. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed September 8, 2009.
- 2.Briceland LL, Kane MP, Hamilton RA. Evaluation of patient-care interventions by PharmD clerkship students. Am J Health-Syst Pharm. 1992;49(5):1130–1132. [PubMed] [Google Scholar]
- 3.Dennehy CE, Kroon LA, Byrne M, Koda-Kimble MA. Increase in number and diversity of clinical interventions by PharmD students over a clerkship rotation. Am J Pharm Educ. 1998;62(4):373–379. [Google Scholar]
- 4.Brockmiller H, Abel CP, Koh-Knox CP, Birk CW. Cost impact of PharmD candidates’ drug therapy recommendations. Am J Health-Syst Pharm. 1999;56(9):882–884. doi: 10.1093/ajhp/56.9.882. [DOI] [PubMed] [Google Scholar]
- 5.Taylor CT, Church CO, Byrd DC. Documentation of clinical interventions by pharmacy faculty, residents, and students. Ann Pharmacother. 2000;34(7):843–847. doi: 10.1345/aph.19310. [DOI] [PubMed] [Google Scholar]
- 6.Pham DQ. Evaluating the impact of clinical interventions by PharmD students on internal medicine clerkships: the results of a 3-year study. Ann Pharmacother. 2006;40(9):1541–1545. doi: 10.1345/aph.1H142. [DOI] [PubMed] [Google Scholar]
- 7.Slaughter RL, Erickson SR, Thomson PA. Clinical Interventions provided by doctor of pharmacy students. Ann Pharmacother. 1994;28(5):665–670. doi: 10.1177/106002809402800519. [DOI] [PubMed] [Google Scholar]
- 8.Mason JD, Colley CA. Effectiveness of an ambulatory care clinical pharmacist: a controlled trial. Ann Pharmacother. 1993;27(5):555–559. doi: 10.1177/106002809302700503. [DOI] [PubMed] [Google Scholar]
- 9.Singhal PK, Raisch DW, Gupchup GV. The impact of pharmaceutical services in community and ambulatory care settings: evidence and recommendations for future research. Ann Pharmacother. 1999;33(12):1336–1355. doi: 10.1345/aph.18440. [DOI] [PubMed] [Google Scholar]
- 10.Pound MW, Miller SM. Written versus oral recommendations made by pharmacy students during internal medicine rotations. Ann Pharmacother. 2007;41(5):772–776. doi: 10.1345/aph.1H668. [DOI] [PubMed] [Google Scholar]