Abstract
Objective
The purpose of this paper is to present a preliminary model to identify the effects of expectancy of treatment success and the patient-provider encounter (PPE) on outcomes in an open-label randomized trial.
Methods
80 participants with chronic cervicogenic headache (CGH) were randomized to 4 groups: 2 levels of treatment dose (8 or 16) and 2 levels of therapy from a chiropractor (spinal manipulation or light massage). Providers were instructed to have equal enthusiasm for all care. Structural equation modeling with standardized path coefficients (β) was used in a path analysis to identify the effects of patient expectancy and the PPE on CGH pain. The model included monthly pain from baseline to 12 weeks. Expectancy and PPE were evaluated on Likert scales. The PPE was measured as patient perception of chiropractor enthusiasm, confidence, and comfort with care.
Results
Baseline patient expectancy was balanced across groups. PPE measures were balanced across groups and consistent over the 8-week treatment period. Treatment and baseline pain had the strongest effects on pain outcomes (|β| =.46 to .59). Expectations had little effect on pain (|β| < .15). The PPE had a weak effect on pain (|β| = .03 to .27) and on subsequent confidence in treatment success (|β| = .09 and .12).
Conclusions
Encouraging equipoise in the provider-patient encounter and balancing expectancy across treatment groups may protect against some confounding related to the absence of blinding in a randomized controlled trial of pain. In this trial, their effects were found to be small relative to the effects of treatment and baseline values.
INTRODUCTION
The therapeutic effects of care are complex and include far more than the consequences of a specific intervention.1 Hence, nonspecific effects of care clearly need to be addressed in the design of randomized trials. Patient response expectancy can be a major contributor to an observed treatment effect,2,3 and provider enthusiasm during the patient-provider encounter (PPE) can also have a positive effect on treatment outcomes.4 Three trials on chronic and one on acute low back pain have reported the effects of baseline expectation of treatment success on functional disability with mixed results.5–8 For acute pain, general expectancy of success, but not expectation of specific treatments’ success, was observed to be a determinant in a choice trial on acute low back pain that included chiropractic as an option.5 For chronic pain, expectation of success in the treatment that the participant received was an important determinant of outcomes in a comparison of acupuncture and massage.6 Expectancy also affected outcomes in a trial comparing physical therapy, cognitive-behavioral therapy and combination of the two.7 However, expectation of success did not affect outcomes in a more recent trial comparing acupuncture, sham acupuncture, and medical care.8 None of these trials looked at the influence of evolving expectations over time or the PPE on outcomes.
It is well known that blinding of participant and provider is important in establishing the internal validity for randomized trials of treatment efficacy.9 Blinding of participant and provider are universally included as important components of quality scoring instruments used for systematic reviews of randomized trials.10,11 Blinding serves to control the effects of expectancy of treatment success and the nonspecific effects of PPE across groups in studies of efficacy, where the goal is to isolate the specific effects of an intervention above and beyond its social contexts. Unfortunately, it is often not possible to blind patients and providers in studies evaluating the efficacy or relative efficacy of manual therapies. However, steps can be taken that can help minimize the effects expectation and the PPE.
We conducted a randomized trial, described below, evaluating the efficacy of spinal manipulative therapy and comparing two doses of intervention provided by a chiropractor for the care of cervicogenic headache (CGH).12 We found that SMT had a clinically important advantage over light massage and there was little effect of dose on headache pain and number. The purpose of this report is to describe the methods we used for addressing initial expectancy and the PPE, and to present a preliminary path analysis modeling the effects of ongoing expectation of success and PPE on CGH number and pain outcomes.
METHODS
Design and Protocol
The methods are presented in detail in the principal report of trial outcomes.12 Briefly, a prospective randomized controlled trial was conducted using a 2×2 balanced factorial design. A total of 80 participants (n = 20 per group) were randomized. Patients were allocated to two levels of dose (8 or 16 treatment sessions). They were also randomized to 2 levels of intervention: spinal manipulation (SMT) or a minimal light massage (LM) control to isolate the effect of SMT above the effect of touching the patient therapeutically. Randomization was conducted using computer-generated, design adaptive allocation13,14 to balance 7 potential confounding baseline variables. Most relevant to this report was the difference in patient confidence in the success of SMT and LM. The other variables were age, gender, migraine, CGH pain intensity, number of CGH, and difference in expected optimal number of sessions for treatment with SMT and LM. Some of these variables were collected at the time of randomization so that allocation to treatment group was concealed from all study personnel. Participants and treating chiropractors were not blinded to intervention after randomization.
All participants were scheduled to receive 16 office visits of 10 minutes duration to a study chiropractor, 2 per week for 8 weeks. Patients were treated (SMT or LM) once or twice per week. Participants allocated to 8 treatment sessions were also assigned to 8 visits for a manual examination once per week. These attention-control visits were used to control time and interaction with the chiropractor, as well as the effects of touching the patients.
Prior to randomization, participants were informed that we were investigation the effects of a manipulation and massage protocol. They were told dispassionately that there was potential benefit from either treatment, with no emphasis placed on either regimen. Descriptions were scripted for the phone interview and the consent form signed by the patients. Participants were told they would be randomized to receive either spinal manipulation or light massage. The screening chiropractor described study manipulation and massage in detail.
The treating chiropractors interacted with the patients at each visit. They took brief histories and chatted with the patients as in usual practice. The chiropractors were asked to interact with the participants with equal enthusiasm for care across the different interventions and doses of care. Equipoise in enthusiasm and other variables were monitored through patient questionnaire described below. Study investigators (chiropractors) were also asked to give feedback to the treating chiropractors if they noted any patterns of unintentional breach of equipoise across groups during study-visit observations.
Follow-up of study outcomes used in this report was conducted by mailed questionnaire at 12 weeks and through phone interview by a blinded research assistant at 4 and 8 weeks. The primary outcome, identified in advance, was self-reported CGH pain intensity. Analysis was conducted using the intention-to-treat principle.
The trial was approved by the Western States Chiropractic College Institutional Review Board (FWA 851). It was registered on ClinicalTrials.gov (NLM identifier NCT00246350).
Participants
Volunteers were eligible if they had a history of at least 5 CGH per month for 3 months, with CGH as defined by the International Headache Society (IHS) in 1998 (excluding the radiographic criterion).15 The IHS criteria were: 1) pain localized in the neck and occipital region that may project to forehead, orbital region, temples, vertex, or ears; 2) pain precipitated or aggravated by particular neck movements or posture; and 3) either resistance/limitation of passive neck motion, palpatory changes in neck musculature or altered response to stretching/contraction, or abnormal neck muscle tenderness. Participants had a minimum score of 25 on the 100-point pain intensity scale to prevent floor effects.
Potential participants were excluded if they were taking prophylactic medication for headache, or had manipulation/professional massage care for the neck or for headache in the prior 3 months. Participants were ineligible for contraindications to spinal manipulation16 or complicating conditions that may be related to clinical outcomes: malignancy, spinal infection, vertebral tumors or fracture, cervical instability, blood dyscrasia or anti-coagulant therapy, thrombophlebitis, long-term corticosteroid use, stroke risk, severe head/neck trauma, neck/intracranial surgery within the previous 5 years, radiating pain/neurological deficits to the upper extremities or cervical disc condition, arthritis of the cervical spine, severe osteoporosis, referred neck pain of organic origin, or pregnancy. Persons were also ineligible for other types of headache with etiologies that may confound the effects of manipulation on the cervicogenic component: cluster, metabolic/toxic, sinus, and HA associated with temporomandibular disease, tumors, and glaucoma.
Assessment and Intervention
A chiropractor/faculty member with 15 years experience screened volunteers for study eligibility through case history, standard orthopedic/neurological exam, heat sensitivity test, and 3-view cervical x-ray using the protocols of Vernon17 and Souza18 for CGH and those of Gatterman and Panzer16 for the cervical region. Four chiropractors with over 20 years of experience served as the study treatment providers.
The 2 SMT groups received high velocity, low amplitude spinal manipulation of the cervical and upper thoracic (transitional region) spine at each visit as described by Peterson and Bergmann.19 Modifications in manipulation recommended for older patients were permitted as required.20,21 To relax the neck and upper back in preparation for spinal manipulation,22 the chiropractor administered a moist heat pack for 5 minutes and conducted a light massage for 2 minutes (described below) as in previous headache trials.23,24
The 2 LM control groups received 5 minutes of moist heat (as above) followed by 5 minutes of light massage. Light massage consisted of gentle effleurage (gliding) and gentle pétrissage (kneading) of the neck and shoulder muscles.19,25 This allowed us to control contact with the patient with an intervention that was expected to have relatively small specific effects. This was because SMT had been shown superior to deep massage26 and the LM application was much lighter and of much shorter duration than found in massage trials and common practice.27,28
Participants receiving only 8 treatment sessions attended the attention-control examination visits. These included a standardized manual examination: motion and static palpation of the cervical and upper thoracic regions, inclinometric evaluation of active cervical range of motion and associated pain, and algometric pain threshold evaluated over articular pillars/transverse processes.19
Study Variables for this Report
CGH pain intensity, the primary study outcome, was evaluated using the Modified Von Korff pain scale of Underwood et al.29 It is the average of three 11-point numerical rating scales: CGH pain today, worst CGH pain in last 4 weeks, and average CGH pain in the last 4 weeks. The scale is scored from 0 to 100 with a lower score more favorable. A 10-point difference between groups was designated in advance as clinically important.11 The scale has been shown to be reliable, valid, and responsive for measuring pain (including headache) and was chosen for its brevity, simplicity, acceptability to participants, and validity as a phone questionnaire.29 CGH pain improvement (CGH Δ Pain) was defined as follow-up pain minus baseline pain.
Patient expectation was evaluated as confidence in the success of assigned study intervention using Interstudy’s Low Back Pain TyPE Specification instrument30 (e.g., “How confident are you that spinal manipulation therapy will be able to successfully treat your headache problem?”). The 6-point Likert scales were anchored by “extremely uncertain” and “extremely certain.” Measures of the PPE included measures of patient perception of chiropractor enthusiasm for care, comfort treating CGH, confidence in care success, and adequate time spent with the patient. For example, “My doctor seemed enthusiastic about my treatment program.” The 4 variables were measured on 5-point Likert scales anchored by “strongly disagree” to strongly agree.”31,32 The initial evaluation of these 4 variables at 2 weeks (i.e., least likely to be confounded with treatment effects) were used as the measures of equipoise.
Statistical Analysis
Structural Equation Modeling33 was used to conduct a path analysis to identify the direct and indirect effects of patient expectancy (expressed as confidence in treatment success) and the patient-provider encounter on CGH pain improvement. All measured variables in the analyses were standardized (mean = 0, SD = 1), while latent variables were standardized so that their residual variances were 1.0. Path coefficients (β) are generally on a −1 to 1 scale and are analogous to standardized partial regression coefficients. The absolute magnitudes |β| indicate the strength of the relationship between variables. Statistical significance was not included because of the preliminary nature of the model.
A latent variable was created to represent the generalized treatment effect on outcomes. This latent treatment variable was defined to be influenced by 3 treatment indicators: intervention (manipulation vs. light massage), dose (16 vs. 8 visits), and intervention × dose interaction. Latent variables were also created to represent the PPE at 3 time points. They were defined by their influences on the measures of patient perception of the chiropractor (enthusiasm for treatment, comfort with treatment, confidence in treatment, and adequacy of time spent).
In the structural equation model, CGH pain improvement was predicted by the latent treatment variable, baseline CGH pain, expectation of treatment success, and by the PPE. The PPE also was presumed to influence subsequent expectations. In addition, pain improvement was presumed to influence concurrent expectations and PPE.
A second path analysis was conducted. In this model, the outcome was improvement in the number of CGH in the prior 4 weeks compared the number of CGH in the prior 4 weeks at baseline.
RESULTS
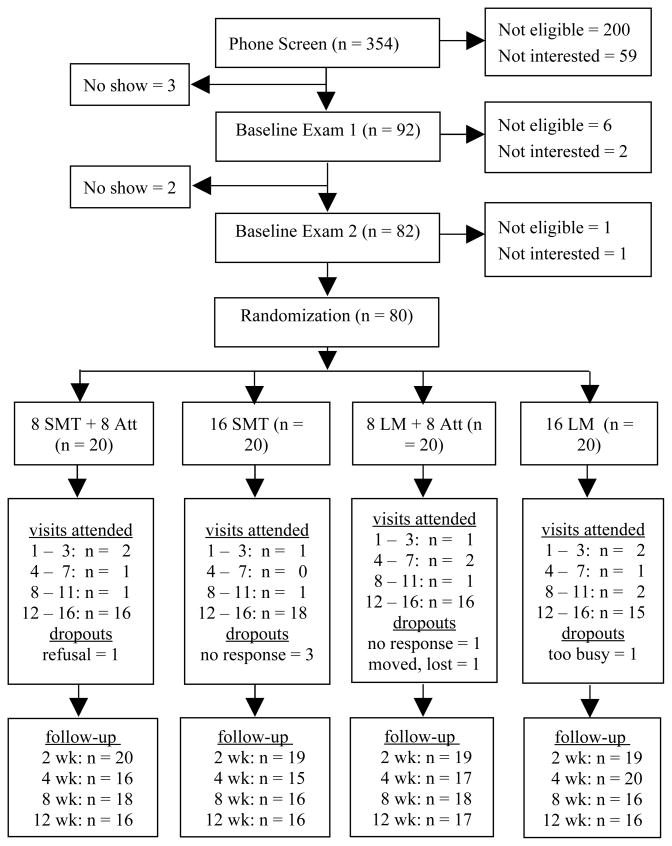
The study flow chart and details of adherence to treatment and compliance with follow-up are presented in Figure 1 with further details published elsewhere.12 On average, patients complied with 86% of study visits. Overall, 83% to 100% of patient data for each variable were available for this analysis.
Figure 1.
Study flow chart.
Baseline characteristics are presented in Table 1. Participants were generally young and predominantly women. They averaged about 4 CGH per week and had a mean pain intensity of 54.3 (SD = 16.9). About a quarter were also migraine sufferers. Table 2 shows improvement in pain and number of headaches in all groups. Differences between SMT and LM in pain intensity and headache number have been previously reported as statistically significant and clinically important; dose effects were small.12
Table 1.
Baseline participant characteristics*
| SMT 8 visits | SMT 16 visits | LM 8 visits | LM 16 visits | All | |
|---|---|---|---|---|---|
| (n = 20) | (n = 20) | (n = 20) | (n = 20) | (n = 80) | |
| Sociodemographic information | |||||
| Age (years) | 38 ± 10 | 35 ± 12 | 37 ± 13 | 34 ± 10 | 36 ± 11 |
| Gender (female) | 80% | 80% | 75% | 85% | 80% |
| Cervicogenic headaches | |||||
| Pain intensity (100-point scale) | 51.2 ± 17.7 | 50.7 ± 16.8 | 56.8 ± 15.8 | 58.7 ± 17.1 | 54.3 ± 16.9 |
| Number of headaches in the past 4 weeks | 14.8 ± 8.4 | 16.0 ± 7.7 | 15.8 ± 8.7 | 16.2 ± 7.0 | 15.7 ± 7.9 |
| Health status | |||||
| Migraine sufferer (self report) | 6 (30%) | 6 (30%) | 5 (25%) | 5 (25%) | 22 (28%) |
| Optimal number of treatments (4 – 20) | |||||
| SMT | 12.4 ± 4.8 | 13.4 ± 5.1 | 11.6 ± 5.3 | 13.4 ± 4.7 | 12.7 ± 5.0 |
| LM | 14.4 ± 5.1 | 14.2 ± 4.6 | 13.2 ± 5.5 | 15.2 ± 5.1 | 14.3 ± 5.0 |
| Expectations † | |||||
| Confidence in success of my treatment | 4.4 ± 1.3 | 4.0 ± 1.1 | 4.0 ± 1.1 | 4.2 ± 1.3 | 4.1 ± 1.2 |
| Confidence in success of SMT | 4.4 ± 1.3 | 4.0 ± 1.1 | 4.0 ± 1.5 | 4.2 ± 1.3 | 4.1 ± 1.3 |
| Confidence in success of LM | 4.1 ± 1.1 | 4.0 ± 1.3 | 4.0 ± 1.1 | 4.2 ± 1.3 | 4.1 ± 1.2 |
| Initial patient-provider encounter ‡ | |||||
| DC comfortable treating headache pain | 4.8 ± 0.6 | 4.8 ± 0.4 | 4.5 ± 0.6 | 4.8 ± 0.4 | 4.7 ± 0.5 |
| DC enthusiastic about treatment | 4.6 ± 0.7 | 4.7 ± 0.5 | 4.3 ± 0.9 | 4.3 ± 1.1 | 4.5 ± 0.8 |
| DC spent adequate time listening | 4.5 ± 0.8 | 4.3 ± 1.0 | 4.7 ± 0.6 | 4.3 ± 1.1 | 4.4 ± 0.9 |
| DC confident in treatment success | 4.3 ± 0.9 | 4.4 ± 0.8 | 3.3 ± 0.5 | 3.3 ± 1.3 | 3.8 ± 1.0 |
SMT, spinal manipulative therapy; LM, light massage.
Values are means ± SD or number (%).
6-point Likert scale anchored by 1 extremely uncertain and 6 extremely certain.
5-point Likert scale with 1 indicating strongly disagree and 5 indicating strongly agree. These were reported 2 weeks after enrollment.
Table 2.
Path analysis variables*
| SMT 8 visits | SMT 16 visits | LM 8 visits | LM 16 visits | All Participants | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| week | n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | n | Mean ± SD | n | Mean ± SD |
| Cervicogenic headaches | ||||||||||
| Pain intensity (100-point scale) | ||||||||||
| 0 | 20 | 51.2 ± 17.7 | 20 | 50.7 ± 16.8 | 20 | 56.8 ± 15.8 | 20 | 58.7 ± 17.1 | 80 | 54.3 ± 16.9 |
| 4 | 17 | 36.5 ± 17.7 | 16 | 31.7 ± 13.7 | 17 | 49.8 ± 12.9 | 20 | 46.5 ± 17.7 | 70 | 41.5 ± 17.1 |
| 8 | 17 | 37.1 ± 16.8 | 16 | 30.2 ± 17.0 | 19 | 42.1 ± 16.0 | 16 | 44.8 ± 17.3 | 68 | 38.7 ± 17.2 |
| 12 | 16 | 30.8 ± 20.0 | 17 | 29.6 ± 23.7 | 17 | 42.0 ± 20.6 | 16 | 49.4 ± 19.0 | 66 | 37.9 ± 22.0 |
| Number of cervicogenic headaches in the past 4 weeks | ||||||||||
| 0 | 20 | 14.8 ± 8.4 | 20 | 16.0 ± 7.7 | 20 | 15.8 ± 8.7 | 20 | 16.2 ± 7.0 | 80 | 15.7 ± 7.9 |
| 4 | 17 | 9.4 ± 5.2 | 16 | 10.0 ± 8.3 | 17 | 14.2 ± 8.6 | 20 | 12.7 ± 8.7 | 70 | 11.7 ± 7.9 |
| 8 | 17 | 8.8 ± 5.6 | 16 | 7.1 ± 7.2 | 19 | 12.7 ± 9.4 | 16 | 11.1 ± 6.4 | 68 | 10.0 ± 7.5 |
| 12 | 16 | 5.8 ± 4.8 | 17 | 6.4 ± 6.8 | 17 | 9.8 ± 6.7 | 16 | 12.9 ± 8.8 | 66 | 8.7 ± 7.3 |
| Expectations: Confidence in success of my treatment † | ||||||||||
| 0 | 20 | 4.4 ± 1.3 | 20 | 4.0 ± 1.1 | 20 | 4.0 ± 1.1 | 20 | 4.2 ± 1.3 | 80 | 4.1 ± 1.2 |
| 4 | 17 | 4.7 ± 1.2 | 16 | 4.8 ± 1.0 | 17 | 4.0 ± 1.3 | 20 | 3.5 ± 1.4 | 70 | 4.2 ± 1.4 |
| 8 | 17 | 4.9 ± 0.7 | 16 | 5.0 ± 1.1 | 19 | 4.2 ± 1.4 | 16 | 4.3 ± 1.2 | 68 | 4.6 ± 1.2 |
| Patient-provider encounter ‡ | ||||||||||
| DC comfortable treating headache pain | ||||||||||
| 2 | 20 | 4.8 ± 0.6 | 19 | 4.8 ± 0.4 | 19 | 4.5 ± 0.6 | 19 | 4.8 ± 0.4 | 77 | 4.7 ± 0.5 |
| 4 | 17 | 4.8 ± 0.8 | 16 | 4.9 ± 0.3 | 17 | 4.8 ± 0.4 | 20 | 4.7 ± 0.8 | 70 | 4.8 ± 0.6 |
| 8 | 16 | 4.8 ± 0.6 | 16 | 4.8 ± 0.4 | 19 | 4.8 ± 0.4 | 16 | 4.8 ± 0.6 | 67 | 4.8 ± 0.5 |
| DC enthusiastic about treatment | ||||||||||
| 2 | 20 | 4.6 ± 0.7 | 19 | 4.7 ± 0.5 | 19 | 4.3 ± 0.9 | 19 | 4.3 ± 1.1 | 77 | 4.5 ± 0.8 |
| 4 | 17 | 4.5 ± 0.8 | 16 | 4.8 ± 0.6 | 17 | 4.4 ± 0.9 | 19 | 4.6 ± 1.0 | 69 | 4.6 ± 0.8 |
| 8 | 16 | 4.6 ± 0.7 | 16 | 4.8 ± 0.6 | 19 | 4.5 ± 0.6 | 16 | 4.6 ± 1.0 | 67 | 4.6 ± 0.7 |
| DC spent adequate time listening | ||||||||||
| 2 | 20 | 4.5 ± 0.8 | 19 | 4.3 ± 1.0 | 19 | 4.7 ± 0.6 | 19 | 4.3 ± 1.1 | 77 | 4.4 ± 0.9 |
| 4 | 17 | 4.7 ± 0.6 | 16 | 4.6 ± 0.9 | 17 | 4.5 ± 0.6 | 20 | 4.7 ± 0.7 | 70 | 4.6 ± 0.7 |
| 8 | 16 | 4.6 ± 0.8 | 16 | 4.4 ± 1.0 | 19 | 4.7 ± 0.5 | 16 | 4.8 ± 0.4 | 67 | 4.6 ± 0.7 |
| DC confident in treatment success | ||||||||||
| 2 | 20 | 4.3 ± 0.9 | 19 | 4.4 ± 0.8 | 19 | 3.3 ± 0.5 | 19 | 3.3 ± 1.3 | 77 | 3.8 ± 1.0 |
| 4 | 15 | 4.6 ± 0.6 | 16 | 4.4 ± 0.9 | 17 | 3.6 ± 0.9 | 19 | 4.0 ± 1.0 | 67 | 4.1 ± 0.9 |
| 8 | 16 | 4.3 ± 0.9 | 16 | 4.5 ± 0.8 | 19 | 4.1 ± 0.8 | 15 | 3.9 ± 1.3 | 66 | 4.3 ± 0.9 |
SMT, spinal manipulative therapy; LM, light massage.
These variables are included in the structural equation models.
6-point Likert scale anchored by 1 extremely uncertain and 6 extremely certain.
5-point Likert scale with 1 indicating strongly disagree and 5 indicating strongly agree.
Expectations and PPE
Patient confidence in and anticipated dose required for treatment success for the two interventions were balanced across groups at baseline (Table 1). Patient confidence in the success of the study treatment received was also balanced across groups at baseline. Confidence grew over time in the groups receiving SMT, perhaps due to better outcomes (Table 2). Consistent with a goal of this study, the PPE measures were generally balanced across groups at each time point. Furthermore, inspection of Table 2 shows that the PPE variables were stable over the 8-week treatment period. One exception to balance across groups was perception of provider confidence. However, we must caution that some participants brought to our attention that the question was not applicable for them and they were forced to guess. We do not know the extent, distribution, or effect of this problem.
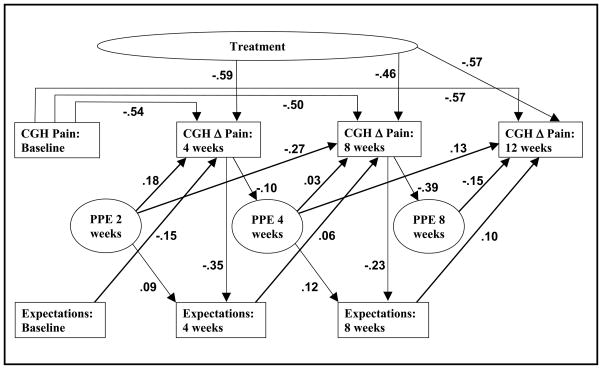
Structural Equation Model
The structural equation model is presented in Figure 2. Squares show measured variables and circles represent theoretical constructs (latent variables). The arrows represent the direction of presumed influence. The path coefficients for the 4 perception variables and 3 treatment indicators that define the latent variables are omitted from Figure 2 and presented below.
Figure 2.
Structural equation model.
The principal findings of the study were that expectations at one time point had little effect on pain improvement at the next time point (|β| = 0.06 to 0.15) and the PPE was weakly related to subsequent pain improvement (|β| = 0.03 to 0.27). These findings were in contrast with the effects of baseline pain (|β| = 0.50 to 0.57) and treatment (|β| = 0.46 to 0.59) on pain outcomes. As such, expectation and PPE had a relatively small effect on outcomes relative to the care and baseline pain parameters in this study.
Also of interest, the PPE had a weak effect on subsequent patient expectations of treatment success (|β| = 0.09 and 0.12). Hence, at 4 and 8 weeks, pain improvement had at most a modest effect on concurrent expectations (|β| = 0.35 and 0.23) and an inconsistent effect on concurrent PPE (|β| = 0.10 and 0.39).
For simplicity of presentation, the path coefficients for the measured treatment and PPE variables were omitted from Figure 2. The latent treatment variable was influenced by intervention, dose, and intervention × dose interaction as follows: |β| = 0.53, 0.31, and 0.11, respectively. The PPE latent variables at 2, 4, and 8 weeks also had a meaningful effect on patient perception of chiropractor enthusiasm, confidence, comfort with care, and sufficiency of time spent with the patient (|β| > 0.60 for 10 of the 12 perception measures).
The signs of the path coefficients can be interpreted as follows. The negative sign showed that greater decrease in pain was associated with greater baseline pain. Greater decrease in pain was also associated with SMT intervention and the higher dose of care. Greater decrease in pain was associated to a modest extent with higher concurrent expectation of treatment success, despite expectation not influencing subsequent outcomes. Greater decrease in pain at 8 weeks was also modestly associated with a more positive PPE at that time point. The path coefficient connecting PPE to later outcomes was expected to be negative (i.e., a more positive encounter would lead to more improvement). Figure 2 shows that the signs for these small path coefficients were mixed.
There were no noteworthy distinctions between the structural equation models for improvement in CGH pain and for improvement in the number of CGH. The latter model is thus not shown.
DISCUSSION
Patient-Provider Encounter
Overall, the treating chiropractors were able to interact with their patients with equipoise regarding 2 manual therapies and 2 doses of intervention in an open-label randomized controlled trial. Balance was maintained longitudinally between and within groups. We were specifically interested in balancing chiropractor enthusiasm, a characteristic that we felt the chiropractors could be mindful of and deliberately control. This was particularly important because the same chiropractors provided both manual therapies in the study. Our study suggests that studies can be designed where treating chiropractors do not interact with the participants differentially across treatment groups, and systematic bias favoring SMT from provider-created expectancy can be controlled to the extent that it would not be an important contributor to observed treatment effects.
Although we sought balance in the PPE across groups, we did not try to control the level of individual provider enthusiasm and other patient-interaction parameters. We assumed variability between providers because of differing chiropractor personalities and variability within providers because of differing patient-provider dynamics. The small standard deviations of the variables measured indicate that actual provider variability did not greatly influence the patient perception of the PPE. Furthermore, the path coefficients showed that the PPE was at most weakly associated with outcomes. Either there was in fact little variation between doctors, or personality differences simply did not affect patient perception of the PPE.
It must be pointed out that this study was not designed to assess the magnitude of the contribution of provider enthusiasm to outcomes (i.e., we did not randomize level of chiropractor enthusiasm). Future research would be required to evaluate the possibility that the PPE contributes a uniform ceiling effect that limits patient improvement from study interventions, despite PPE balance across groups and low association with outcomes.
Expectations
The second major finding of our analysis was that expectation did not appreciably influence subsequent pain improvement outcomes. There are several possible explanations. Expectation may truly have no causal effect on subsequent pain improvement in the population under study conditions of a randomized trial. Finally, different relationships across groups between expectation and outcomes (interaction effect) may have obscured the influence of expectation on pain improvement. In any event, expectation has been shown to be a determinant of disability outcomes in both acute5 and chronic6 low back pain in other studies.
In our study, balance in expectation for success of the assigned treatment across study groups (Table 2) occurred because participants rated confidence in success equally for both treatments (SMT and LM). This was unanticipated. One would guess that SMT would be more appealing than the light massage described in the consent form. The fact that expectation for success of the assigned treatment was balanced across groups and unrelated to outcomes was fortuitous. However, it does show that prior expectation does not necessarily affect outcomes in unblinded trials of manual therapies.
Randomization can be used to balance expectation for each of the interventions across treatment groups in a trial. There is no guarantee, however, that randomization will balance baseline expectation for the actual assigned treatment. This is because if there is a systematic difference in prior expectation between treatments, then randomization that balances expectation of both treatments across groups will preserve the systematic difference in expectation of “my own” treatment success. This can have several consequences. First, despite randomization, an expectation that influences outcomes in participants aware of their treatment will introduce bias in an unblinded randomized trial, unless mean expectations for both study interventions are fortuitously the same. Second, assigned treatment expectation or assigned minus comparison treatment expectation can be determinants of outcomes, whereas expectations of the individual treatments or difference between treatments might not.
It is advantageous to evaluate expectations in randomized trials of manual therapy and investigators should consider balancing them across study groups. One methodological question that remains to be answered is which form of expectation variables should be used as baseline covariates in the analysis of efficacy studies seeking to isolate the effect of a single component of care, such as SMT. Potential baseline covariates fall into 2 categories: those that cannot be used in treatment allocation and those that can (e.g., in stratification or design-adaptive allocation). Possibilities for those that cannot be allocated include expectation of the assigned treatment or the difference between assigned treatment and a comparison intervention. Alternatively, variables that can be used in treatment allocation are difference between 2 treatment expectations or expectations for both treatments. Another important question is whether covariates should be included in the primary or a sensitivity analysis. Finally, a more interesting methodological question is whether the PPE can mitigate the effect of expectation on outcomes after baseline.
Limitations
There are important limitations to our structural equation models. Although sample size in this study is small for a structural equation analysis, the exercise was worthwhile nonetheless, for indicating potentially large or potentially nonexistent effects. Standardization of variables is justified because the indicative results were to serve as general guides, rather than definitive results.
Our model must be considered preliminary because precise and stable estimates of the path coefficients for a model of this complexity requires at least several hundreds of patients.33 Second, path analysis is only as good as the variables in the model and the presumed pathways included. Other important determinants, confounders, and paths between variables could change the relationship of outcomes with expectancy or the PPE. For example, different measures of expectancy and the PPE might yield different results. In addition, expectations might influence subsequent PPE; these paths were not included. Also, there could be feedback loops between concurrent outcomes, expectations, and the PPE; that is, there can be mutual causal relationships between these variables. A larger sample is required to construct a more sophisticated model to take all these possibilities into account.
In general, Latent variables must be used with caution. Our constructs for treatment and the PPE appear reasonable, however, because of the strength of the path coefficients connecting treatment to intervention and dose, and connecting the PPE to patient perception of the interaction with the chiropractor. In addition, we wanted to make an assessment of whether expectancy or PPE could provide alternative explanations for treatment effects. This would have been the indication if treatment effects had vanished when these factors were included in the model, and the only way to test this was to include treatment effects.
It must also be emphasized that our findings are only applicable to studies of efficacy where the PPE and associated expectations are considered confounders to be controlled. In other study designs, nonspecific effects are considered beneficial to the patient and considered a component of the therapy under investigation. These include, for example, studies of efficacy of whole systems and effectiveness of real world practice. The design of these studies may avoid suppression of the influence of the PPE or even seek to enhance it. The path coefficients connected the PPE to outcomes would be expected to be significantly larger for these study designs.
CONCLUSION
Several expected relationships were found supporting confidence that the analysis contains no serious bias in estimating the effects of baseline or treatment on outcomes. There was evidence for a coherent PPE variable, as judged by the patient. There was indication that successful treatment leads to increased expectation of further benefit. There was no evidence for strong consistent effects of either patient expectation or patient assessment of patient-practitioner encounter on the reported CGH pain improvement and number of headaches. Based on an elaborate structural equation model, in a relatively small sample, we did not find that either expectation or patient-practitioner encounter effects on outcomes provide better explanations than are provided by the effects of balanced treatment assignments.
Clearly, blinding is often not possible in efficacy and relative efficacy studies seeking to evaluate the independent effects of a single component of care (such as SMT). It is therefore important to control the effects of the patient-provider interaction on study outcomes to help optimize study internal validity. It appears that equipoise by the same providers across intervention types can be accomplished. It also appears that it is possible to reduce the confounding effect of the patient-provider encounter to a relatively small proportion of the treatment effect found for the interventions under study. A challenging methodological issue that remains is determining to what extent equipoise in the patient-provider encounter across treatment arms can serve as a surrogate for double-blinding in randomized controlled trials.
PRACTICAL APPLICATIONS
Chiropractors can provide care with equipoise in an open-label randomized controlled trial evaluating the effects of manual therapy and dose of care.
The patient-provider encounter can have minimal effect on pain outcomes in an unblinded randomized controlled trial evaluating spinal manipulation.
Patient expectation can have minimal impact on pain outcomes in an unblinded randomized controlled trial evaluating spinal manipulation.
Acknowledgments
FUNDING SOURCES AND CONFLICTS OF INTEREST
No conflicts of interest were reported for this study. This study was supported by the National Center for Complementary and Alternative Medicine, Department of Health and Human Services (grant no. R21 AT002324).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Moerman DE. Explanatory mechanisms for placebo effects: cultural influences and the meaning response. In: Guess HA, Kleinman A, Kusek JW, Engel LW, editors. The science of the placebo: toward an intedisciplinary research agenda. London: BMJ Books; 2002. pp. 77–107. [Google Scholar]
- 2.Kirsch I, Lynn SJ. Automaticity in clinical psychology. Am Psychol. 1999;54:504–15. doi: 10.1037//0003-066x.54.7.504. [DOI] [PubMed] [Google Scholar]
- 3.Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you’ll do? A systematic review of the evidence for a relation between patients’ recovery expectations and health outcomes. CMAJ. 2001;165:174–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Crow R, Gage H, Hampson S, Hart J, Kimber A, Thomas H. The role of expectancies in the placebo effect and their use in the delivery of health care: a systematic review. Health Technol Assess. 1999;3(3) [PubMed] [Google Scholar]
- 5.Myers SS, Phillips RS, Davis RB, et al. Patient expectations as predictors of outcome in patients with acute low back pain. J Gen Intern Med. 2008;23:148–53. doi: 10.1007/s11606-007-0460-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo RA. Lessons from a trial of acupuncture and massage for low back pain: patient expectations and treatment effects. Spine. 2001;26:1418–24. doi: 10.1097/00007632-200107010-00005. [DOI] [PubMed] [Google Scholar]
- 7.Smeets RJ, Beelen S, Goossens ME, Schouten EG, Knottnerus JA, Vlaeyen JW. Treatment expectancy and credibility are associated with the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. Clin J Pain. 2008;24:305–15. doi: 10.1097/AJP.0b013e318164aa75. [DOI] [PubMed] [Google Scholar]
- 8.Cherkin DC, Sherman KJ, Avins AL, et al. A randomized trial comparing acupuncture, simulated acupuncture, and usual care for chronic low back pain. Arch Intern Med. 2009;169:858–66. doi: 10.1001/archinternmed.2009.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 10.Moher D, Jadad AR, Nichol G, Penman M, Tugwell P, Walsh S. Assessing the quality of randomized controlled trials: an annotated bibliography of scales and checklists. Control Clin Trials. 1995;16:62–73. doi: 10.1016/0197-2456(94)00031-w. [DOI] [PubMed] [Google Scholar]
- 11.Bronfort G, Nilsson N, Haas M, Evans R, Assendelft WJJ, Bouter LM. Noninvasive physical treatments for chronic headache. Cochrane Database Syst Rev. 2004;(3):CD001878. doi: 10.1002/14651858.CD001878.pub2. [DOI] [PubMed] [Google Scholar]
- 12.Haas M, Spegman A, Peterson DH, Aickin M, Vavrek D. Dose-response and efficacy of spinal manipulation for chronic cervicogenic headache. Spine J. 2010 doi: 10.1016/j.spinee.2009.09.002. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aickin M. Randomization, balance, and the validity and efficiency of design-adaptive allocation methods. J Statist Plann Inference. 2001;94:97–119. [Google Scholar]
- 14.Aickin M. A simulation study of the validity and efficiency of design-adaptive allocation to two groups in the regression situation. Int J Biostat. 2009;5:19. doi: 10.2202/1557-4679.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.International Headache Society. Classification and diagnostic criteria for headache disorders, cranial neuralgias, and facial pain. Cephalalgia. 1988;8(suppl 7):1–96. [PubMed] [Google Scholar]
- 16.Gatterman MI, Panzer DM. Disorders of the cervical spine. In: Gatterman MI, editor. Chiropractic management of spine related disorders. Baltimore: Williams & Wilkins; 1990. pp. 205–55. [Google Scholar]
- 17.Vernon H. Spinal manipulation and headaches: an update. Top Clin Chiropr. 1995;2:34–47. [Google Scholar]
- 18.Souza TA. Differential diagnosis for the chiropractor: protocols and algorithms. Gaithersburg, MD: Aspen Publishers, Inc; 1998. pp. 383–402. [Google Scholar]
- 19.Peterson DH, Bergmann TF. Chiropractic technique: principles and practice. 2. St. Louis: Mosby; 2002. [Google Scholar]
- 20.Cooperstein R, Killinger L. Chiropractic techniques in the care of the geriatric patient. In: Gleberzon BJ, editor. Chiropractic care of the older patient. Boston: Butterworth-Heinemann; 2001. pp. 359–83. [Google Scholar]
- 21.Bergmann TF, Larson L. Manipulative care and older persons. Top Clin Chiropr. 1996;3:56–65. [Google Scholar]
- 22.McDowell BL. Adjunctive procedures: physiological therapeutics. In: Gatterman MI, editor. Chiropractic management of spine related disorders. Baltimore: Williams & Wilkins; 1990. pp. 330–78. [Google Scholar]
- 23.Nelson CF, Bronfort G, Evans R, Boline P, Goldsmith CH, Anderson AV. The efficacy of spinal manipulation, amitriptyline and the combination of both therapies for the prophylaxis of migraine headache. J Manipulative Physiol Ther. 1998;21:511–9. [PubMed] [Google Scholar]
- 24.Boline PD, Kassak K, Bronfort G, Nelson C, Anderson AV. Spinal manipulation vs Amitriptyline for the treatment of chronic tension-type headaches: a randomized clinical trial. J Manipulative Physiol Ther. 1995;18:148–54. [PubMed] [Google Scholar]
- 25.Nicholson GG, Clendaniel RA. Manual Techniques. In: Scully RM, Barnes MR, editors. Physical Therapy. Philadelphia: J.B. Lippincott Company; 1989. pp. 926–85. [Google Scholar]
- 26.Nilsson N, Christensen HW, Hartvigsen J. The effect of spinal manipulation in the treatment of cervicogenic headache. J Manipulative Physiol Ther. 1997;20:326–30. [PubMed] [Google Scholar]
- 27.Furlan AD, Brosseau L, Imamura M, Irvin E. Massage for low back pain: a systematic review within the framework of the Cochrane collaboration back review group. Spine. 2002;27:1896–910. doi: 10.1097/00007632-200209010-00017. [DOI] [PubMed] [Google Scholar]
- 28.Cherkin DC, Deyo RA, Sherman KJ, et al. Characteristics of licensed acupuncturists, chiropractors, massage thrapists and naturapthic physicians. J Am Board Fam Pract. 2002;15:463–72. [PubMed] [Google Scholar]
- 29.Underwood MR, Barnett AG, Vickers MR. Evaluation of two time-specific back pain outcome measures. Spine. 1999;24:1104–12. doi: 10.1097/00007632-199906010-00010. [DOI] [PubMed] [Google Scholar]
- 30.Quality Quest. 1989. Users manual: low back pain TyPEsm specification. Version 1. [Google Scholar]
- 31.Cherkin D, Deyo RA, Berg AO. Evaluation of a physician education intervention to improve primary care for low-back pain: II. Impact on patients Spine. 1991;16:1173–8. doi: 10.1097/00007632-199110000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Cherkin DC, MacCornack FA. Patient evaluations of low back pain care from family physicians and chiropractors. West J Med. 1989;150:351–5. [PMC free article] [PubMed] [Google Scholar]
- 33.Neale MC, Boker SM, Xie G, Maes HH. Mx: statistical modeling. 6. VCU Box 900126, Richmond, VA 23298: Department of Psychiatry; 2003. [Google Scholar]