Abstract
Objective
To estimate the strength of association between first-trimester bleeding and miscarriage, setting aside the bleeding at time of loss.
Methods
Women enrolled in a community-based pregnancy cohort study before or during early pregnancy. Detailed, first-trimester bleeding data were collected by telephone interview. Bleeding episodes proximal to miscarriage (within 4 days) were excluded. We used discrete-time hazard models to evaluate the association between bleeding and miscarriage. Models were adjusted for maternal age, prior miscarriage, and smoking. Exploratory regression tree analysis was used to evaluate the relative importance of other bleeding characteristics (duration, associated pain, color, timing).
Results
Of the 4510 participants, 1204 (27%) reported some first-trimester vaginal bleeding or spotting, and 517 miscarriages were observed. Eight percent of those with bleeding reported heavy bleeding episodes. When we evaluated any bleeding, including episodes of only spotting, the unadjusted relative odds (OR) of miscarriage for women with bleeding (n=1204) was 1.1 (95% confidence interval [CI] 0.9–1.3). However, women who reported heavy bleeding (n=97)had nearly three times the risk of miscarriage compared to women without bleeding during the first trimester (OR 3.0, 95% CI 1.9–4.6). Adjustment for covariates had little effect on estimates. Further analyses suggested that women with heavy bleeding accompanied by pain were the group accounting for most of the elevated risk.
Conclusion
Heavy bleeding in the first trimester, particularly when accompanied by pain, is associated with higher risk of miscarriage. Spotting and light episodes are not, especially if only lasting 1–2 days..
INTRODUCTION
Vaginal bleeding is a common first trimester complication, often considered to be a sign of a problem in pregnancy. Bleeding has been related to preterm birth, low birthweight, and small-for-gestational age infants (1–4). Inconsistent results have been reported in relation to bleeding and congenital malformations (5–7). These studies are limited by focusing on bleeding episodes that come to clinical attention or bleeding episodes that are reported late in pregnancy or after delivery. Such methodologic differences result in widely varying baseline bleeding prevalences in these studies (7 to 24%), making it difficult to compare results.
Studies that have looked specifically at the relationship between bleeding and miscarriage are usually conducted in populations recruited from hospitals or emergency departments (8–12). Many of the bleeding episodes which require immediate medical attention mark the actual miscarriage event; thus, these studies do not provide useful information about the risk of miscarriage for women who experience bleeding that does not immediately precede miscarriage. Only two studies have evaluated bleeding that is temporally separated from miscarriage. Both studies evaluated first-trimester bleeding in relation to second-trimester miscarriage, and both reported increased risk of late loss, especially for heavy bleeding (odds ratios for heavy bleeding were 3.6 and 4.9) (13, 14).
However, most miscarriage occurs during the first trimester, and study of this outcome requires enrollment early in pregnancy so that early miscarriages can be identified. We collected detailed data about the timing and characteristics of first trimester bleeding from a large, community-based study that enrolled early in pregnancy or prior to pregnancy in order to examine the association between bleeding and miscarriage, including first-trimester miscarriage.
METHODS
Right From the Start (RFTS) is an ongoing community-based pregnancy cohort that began enrollment of pregnant women in 2000. Over time, the study has included three phases (RFTS 1, 2, and 3) and has been active in Galveston, TX, Memphis and Nashville, TN, and the Triangle region of NC (including Raleigh, Durham, and Chapel Hill, NC). Participants were at least 18 years old, spoke English or Spanish, had not used assisted reproductive technologies to conceive, and intended to carry the pregnancy to term. Women who were not yet pregnant but trying to conceive could pre-enroll prior to pregnancy and were followed until formal enrollment at the time of a positive pregnancy test. Pre-enrolled women must have been attempting pregnancy for fewer than six months (RFTS 1 and 2) or fewer than three months (RFTS 3). Women entered the study prior to twelve completed weeks of gestation (RFTS 1), prior to nine completed weeks of gestation (RFTS 2), or only pre-enrolled (RFTS 3). Formal enrollment occurred, on average, at 53 days of gestation for women who enrolled while pregnant (n=3581), and at 38 days of gestation for women who pre-enrolled in the study (n=958). Institutional Review Boards of all institutions involved approved this project (University of Tennessee at Memphis, University of Texas at Galveston, University of North Carolina at Chapel Hill, Vanderbilt University Medical Center, National Institute of Environmental Health Sciences). Informed, signed consent was obtained from each study participant in compliance with all Institutional Review Board procedures.
Participants had an early pregnancy ultrasound to assess fetal viability and document the gestational age of the fetus. Gestational age was calculated based on self-reported last menstrual period (LMP). If self-reported LMP was unavailable, ultrasound-based LMP was used (n=15). Seventy-five percent of ultrasounds were completed by the end of the ninth week of gestation, and the average difference between LMP- and ultrasound-based gestational age for ongoing pregnancies was less than one day in a RFTS 1 validation substudy (15).
Participants completed an intake telephone interview. Additional telephone interviews were conducted to collect more detailed information about each participant, including demographic data such as race/ethnicity and education, reproductive history, behaviors, such as smoking, and symptoms, including bleeding. All women, regardless of outcome, provided this detailed information. In the first phase of the study, two telephone interviews were conducted after intake: one occurred shortly after enrollment during the first trimester, followed by a second interview around 20 weeks of pregnancy. Data from both interviews were compiled to obtain an assessment of events and conditions occurring during the entire first trimester. Later phases of RFTS included only one telephone interview after intake, conducted at the end of the first trimester, no later than the sixteenth week of pregnancy. Average time of completion of this interview was during the fourteenth week of pregnancy. Participants who experienced pregnancy loss before the scheduled interview were interviewed as soon as possible after miscarriage. We refer to the interviews that provide our data as the `first trimester interview'.
Women who had their last menstrual period before July 14, 2008 were included in this analysis. Exclusions from the analysis sample include: women who did not complete the first trimester interview (n=170), participants missing both LMP and ultrasound (n=2), women with inconsistent enrollment or pregnancy end dates (n=6), and women with ectopic pregnancies (n=5). Women could enroll during more than one pregnancy, but only the first enrolled pregnancy was included (n=238 subsequent pregnancies excluded). An additional 26 women were excluded from this analysis because they had immediate losses or were lost to follow-up in the same week in which they enrolled. A total of 4510 pregnancies contributed to this analysis.
Bleeding was self-reported by each participant in the first trimester interview. Participants reported the total number of episodes experienced during the first trimester, and detailed information was collected about the timing, heaviness, color, duration, and pain associated with the first three reported episodes. If bleeding stopped for at least two days and then started again, we considered these as two separate episodes of bleeding. Participants provided the exact date on which an episode began; if this was unavailable, the week and month in which the episode occurred was recorded. The duration of the episode was reported in days. The heaviness of each episode was defined according to the heaviest flow in an episode. A `spotting' episode was one that was only noticed when wiping, a `light bleeding' episode was defined as being lighter than the heavy flow of a usual menstrual period, and a `heavy bleeding' episode had at least one day when flow was as heavy or heavier than the heavy flow of a usual menstrual period. Participants could describe the color of each episode as `red,' `brown,' or `pink.' Participants were also asked if bleeding was associated with pain, and if so, to characterize the pain as mild, moderate, or severe.
This analysis focused on bleeding episodes that occurred during the first trimester. To exclude bleeding that occurs at the time of miscarriage, we did not include any episodes that ended less than 4 days before a miscarriage, and conducted a sensitivity analysis in which this cutpoint was extended to 7 days prior to miscarriage. These cutpoints were chosen based on the distribution of episodes in the data.
Pregnancy was verified by ultrasound or pregnancy test. Miscarriage was defined as loss of a recognized pregnancy prior to twenty completed weeks of gestation. Women with fetal non-viability on ultrasound followed by dilatation and curettage were classified as having a miscarriage. Outcomes were self-reported, and prenatal records were obtained to verify the outcome. The date of a miscarriage was self reported as the date of dilatation and evacuation or as the date of most severe bleeding. Women with induced abortions (n=14) were censored at the time of the induced abortion.
All analyses were conducted in Stata, version 9.2 (College Station, TX) and DTREG (Brentwood, TN). We used discrete-time hazard models, a survival analysis model, to evaluate the relationship between first trimester bleeding episodes and miscarriage. This model is more appropriate when the time of outcome (miscarriage) is measured on a discrete time scale (such as weeks of pregnancy). This model is implemented as a logistic model that is conditioned on time as a unit of analysis. We calculated week-specific odds ratios for the probability of having a miscarriage in a given gestational week, conditional on a woman still being pregnant at the beginning of that week. Due to the rarity of week-specific miscarriage in our sample, the conditional odds ratios obtained from this model closely approximate the risk ratio. Thus, we refer to our results using `risk' terminology. Women who were missing information about bleeding episodes were not included in the survival analysis (n=21). Our preliminary calculations indicated that we had over 90% power to detect an OR of 1.4.
Weeks of pregnancy were calculated beginning with the date of the last menstrual period, and women entered analysis at the gestational week following their enrollment (e.g. a woman who enrolled on day 2 of gestational week 5 would enter analysis at gestational week 6). Participants contributed to analysis risk sets until an outcome occurred or loss to follow-up. All participants were censored at week 20 if an outcome or loss to follow-up had not yet occurred.
Because bleeding episodes are considered a marker of a pregnancy at risk, the effect of a bleeding episode was considered to extend indefinitely during the pregnancy (e.g., if bleeding occurred at week 5, a woman was entered as having bleeding in all subsequent weeks).
We conducted both unadjusted and adjusted analyses. In adjusted analyses, we controlled for maternal age, prior miscarriage, and maternal smoking status. Women who reported smoking during pregnancy were identified as smokers. Estimates for any bleeding and heaviness of bleeding (none, spotting, light, heavy) were calculated. In the hazard model, the heaviest episode prior to each analysis week was used to define heaviness (e.g., if a woman had light bleeding in week 6, heavy bleeding in week 8, and light bleeding in week 10, she would be initially coded none, then light, then heavy, which would then remain despite the subsequent light bleed).
We evaluated other characteristics of bleeding episodes, such as duration, color, and associated pain, using a two-phase approach that involved preliminary descriptive assessment of characteristics associated with miscarriage using classification and regression tree (CART) analysis, followed by an analysis of interactions with bleeding characteristics in the main model (16). CART is a data-driven analysis tool that splits the data into sub-groups that differentially predict an outcome (in this case, miscarriage). Our CART analysis evaluated the relationship between miscarriage and the following characteristics of bleeding: heaviness, duration, color, timing, and associated pain.
After using CART to identify bleeding episode characteristics that were important predictors of miscarriage, we extended our main analysis of the relationship between these combined characteristics and miscarriage. Several specifications of each variable were considered, informed by patterns observed in the CART analysis. Heaviness was specified as either a binary variable (heavy or not heavy) or as a three-level variable (spotting, light, or heavy bleeding). Pain was coded as a binary variable (present, absent) or as a four-level variable including pain severity (none, mild, moderate, severe pain). Duration was coded as a binary (<3 days, 3+ days) and as a three-level variable (1 day, 2 days, 3+ days). The contribution of the combination of bleeding characteristics to the main models was evaluated using Akaike's information criterion and likelihood ratio tests for nested models (p=0.10).
Because previous studies have evaluated the relationship between bleeding and second trimester miscarriage, we used logistic regression models to replicate these analyses, obtaining estimates for any bleeding and heaviness of bleeding.
We conducted sensitivity analyses to assess the consistency of our results under various scenarios. (1) We re-analyzed our data using a 7-day rather than 4-day cutpoint to reduce the number of bleeding episodes that were close in time to the miscarriage. (2) We restricted the study population to participants for whom gestational age by ultrasound and by last menstrual period differed by no more than 3 or 7 days. This step reduced the number of women whose reporting of early pregnancy events and symptoms may be inaccurate (potentially confusing an episode of early bleeding with the last menstrual period) and also reducing the proportion of fetuses that display early signs of abnormal development and growth. (3) We stratified our analysis by whether participants completed their interview before or after the time of miscarriage. (4) We restricted our analyses to women in their first pregnancy to eliminate the potential for prior pregnancy outcomes having an influence on the quality of reporting. (5) We also restricted our analysis to exclude those women with no documented fetal cardiac motion at ultrasound.
RESULTS
The 4510 women in this study ranged in age from 18 to 45. Most were white, but substantial numbers of blacks and Hispanics also participated. Eighty percent had more than a high school education (Table 1). About one-third were pregnant for the first time. Twenty-seven percent reported at least one episode of bleeding during the first trimester. Of those reporting bleeding, 70.9% reported only one episode (n=854); 20.0% reported two episodes (n=241); and 9.1%, three or more (n=109). About eight percent of women with bleeding reported heavy episodes.
Table 1.
Participants of Right From the Start, 2000–2008 (n=4510).
| Frequency | % | |
|---|---|---|
| Age | ||
| 18–28 years | 1783 | 39.5 |
| 28–34 years | 2068 | 45.9 |
| 34–45 years | 659 | 14.6 |
| Missing | 0 | |
| Race/ethnicity | ||
| White, non-Hispanic | 3002 | 66.7 |
| Black, non-Hispanic | 960 | 21.3 |
| Hispanic ethnicity | 340 | 7.6 |
| Other | 201 | 4.5 |
| Missing | 7 | |
| Education | ||
| High school or less | 895 | 19.9 |
| Some college | 819 | 18.2 |
| College or more | 2795 | 62.0 |
| Missing | 1 | |
| Smoking | ||
| No | 3921 | 87.2 |
| Yes | 574 | 12.8 |
| Missing | 15 | |
| Gravidity | ||
| Primigravida | 1515 | 33.6 |
| One or more prior pregnancy | 2983 | 66.1 |
| Missing | 12 | |
| Bleeding | ||
| None | 3285 | 73.2 |
| Any bleeding | 1204 | 26.8 |
| Missing | 21 | |
| Heaviness of bleeding | ||
| No bleeding | 3285 | 73.2 |
| Spotting | 866 | 19.3 |
| Light | 240 | 5.4 |
| Heavy | 97 | 2.2 |
| Missing | 22 | |
| Outcome | ||
| Miscarriage | 517 | 11.5 |
| Live birth | 3690 | 81.8 |
| Other | 40 | 0.9 |
| Missing* | 263 | 5.8 |
Missing includes 69 women who are known to be beyond 20 weeks of pregnancy but had not reported deliveries at the time of this analysis. The remaining missing observations were censored at the last time of contact with the study, at median 15 gestational weeks and interquartile range 13 to 20.
The association between bleeding and miscarriage is shown in Table 2. Overall, twelve percent of participants experienced a miscarriage, and bleeding in pregnancy was not associated with a significantly increased risk of miscarriage (OR 1.10, 95% CI: 0.90, 1.34). However, 24% of women with heavy bleeding experienced miscarriage (n=23) and this represented a significantly elevated risk (OR 2.97, 95% CI: 1.93, 4.56). Adjustment of our results for age, prior miscarriage history, or smoking status had little effect on the estimates.
Table 2.
Association between bleeding and miscarriage, Right From the Start, 2000–2008 (n=4510).
| Total n (%) | Miscarriage (% of total) | Unadjusted OR | 95% CI | Adjusted OR* | 95% CI | |
|---|---|---|---|---|---|---|
| Presence of any bleeding | ||||||
| None | 3285 (73.2) | 381 (11.6) | 1.00 | 1.00 | ||
| Any | 1204 (26.8) | 131 (10.9) | 1.10 | 0.90, 1.34 | 1.10 | 0.90, 1.35 |
| Heaviness of bleeding | ||||||
| None | 3285 (73.2) | 381 (11.6) | 1.00 | 1.00 | ||
| Spotting | 866 (19.3) | 80 (9.2) | 0.91 | 0.72, 1.17 | 0.93 | 0.73, 1.19 |
| Light | 240 (5.3) | 28 (11.7) | 1.18 | 0.80, 1.74 | 1.16 | 0.78, 1.71 |
| Heavy | 97 (2.2) | 23 (23.7) | 2.97 | 1.93, 4.56 | 2.84 | 1.82, 4.43 |
Adjusted for maternal age, smoking, prior miscarriage
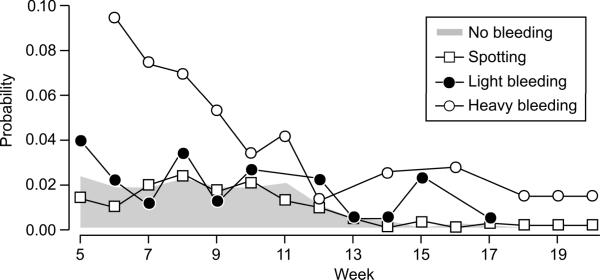
Figure 1 shows the probability of miscarriage, conditional on survival to that week of pregnancy, for women who had experienced different levels of bleeding heaviness. Given the small number of losses in any given week by heaviness of bleeding, confidence intervals are broad (not shown). Data were not sufficient to estimate miscarriage risk for some weeks in which outcomes occurred only among those with bleeding (light bleeding: weeks 11, 16, 18–20; heavy bleeding: weeks 5, 13, 15, 17). However, women who experienced heavy bleeding were at increased risk of both first and second trimester miscarriage, while the risk for women with less severe bleeding (spotting, light bleeding) was similar to those for women who did not bleed.
Figure 1.
Week-specific probability of miscarriage by bleeding status, Right From the Start, 2000–2008 (n=4510).
Because previous studies of bleeding and miscarriage looked only at second trimester miscarriage, we also formally examined that outcome. The risk of second-trimester miscarriage (n=64) for women reporting first-trimester bleeding was 2.2% and the risk for those who reported none was 1.2%. Among women reporting heavy bleeding, the absolute risk was 8.2%. The relative risks comparing any bleeding and heavy bleeding to no bleeding were 1.8 (95% CI 1.1, 3.0) and 7.2 (95% CI 3.1, 16.7), respectively.
To assure that bleeding episodes for women who miscarried were not all clustered near the time of loss, we examined the time from bleeding episodes to time of miscarriage for both heavy and spotting/light episodes. For heavy episodes, the median time from the end of the index episode to the time of miscarriage was 13 days (interquartile range (IQR) 6, 46), and for spotting and light episodes, the median time from the end of the index episode to time of miscarriage was 20 days (IQR 10, 33).
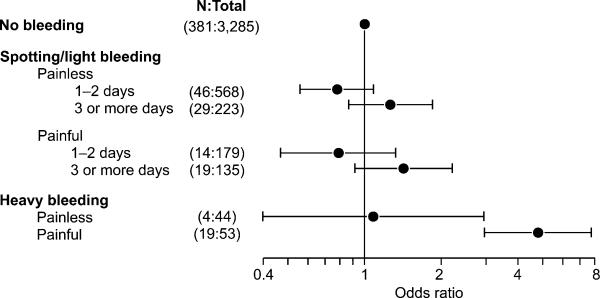
Of the characteristics of bleeding evaluated in the exploratory CART analysis, heaviness and pain associated with bleeding appeared to be the two most important characteristics predicting miscarriage, followed by duration (data not shown). The total number of episodes and color of bleeding appeared to have little importance. Based on these results, we evaluated the risk of miscarriage associated with combinations of heaviness, pain, and duration by including subgroups of these characteristics in the overall unadjusted hazard model. Figure 2 shows the relationship between specific types of bleeding episodes and miscarriage. Women with heavy bleeding and pain had the highest risk of miscarriage (OR 4.79, 95% CI: 2.97, 7.73).
Figure 2.
Relationship between bleeding episodes, characterized by levels of heaviness, pain, and duration, and miscarriage, Right From the Start, 2000–2008 (Total n=4510). Heavy bleeding categories could not be subdivided by duration because of small numbers. N refers to the number of miscarriages in each category.
The finding that miscarriage was associated with heavy bleeding but not less severe bleeding was robust to sensitivity tests (Table 3). These included changes in our definition of bleeding episodes, consideration of the time of interview in relation to the loss, and limiting analysis to women with fetal cardiac motion at time of study ultrasound. In all cases the risk of miscarriage was low for spotting and light bleeding (unadjusted odds ratios all below 1.5) but moderate to high for heavy bleeding (unadjusted odds ratios varied from 2.1 to 4.5).
Table 3.
Further analyses and restrictions to evaluate the association between bleeding and miscarriage, Right From the Start study (2000–2008)
| No bleeding | Any bleeding | Spotting/Light | Heavy | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | n SAB* | OR | n | n SAB* | OR** (95% CI) | n | n SAB* | OR** (95% CI) | n | n SAB* | OR** (95% CI) | |
| Changing episode definition | ||||||||||||
| 4 days (overall analysis results) | 3285 | 381 | 1.0 | 1204 | 131 | 1.1 (0.9, 1.3) | 1106 | 108 | 1.0 (0.8, 1.2) | 97 | 23 | 3.0 (1.9, 4.6) |
| 7 days | 3306 | 402 | 1.0 | 1183 | 110 | 0.9 (0.7, 1.1) | 1091 | 93 | 0.8 (0.6, 1.0) | 91 | 17 | 2.1 (1.3, 3.5) |
| Gestational age*** | ||||||||||||
| 3 days | 1408 | 53 | 1.0 | 532 | 21 | 1.2 (0.7, 2.0) | 495 | 18 | 1.1 (0.6, 1.8) | 37 | 3 | 2.5 (0.8, 8.2) |
| 7 days | 2124 | 82 | 1.0 | 797 | 33 | 1.2 (0.8, 1.8) | 743 | 29 | 1.1 (0.7, 1.7) | 54 | 4 | 2.4 (0.9, 6.5) |
| Loss and interview timing | ||||||||||||
| Loss before interview | 2904 | 244 | 1.0 | 1073 | 61 | 0.9 (0.6, 1.1) | 998 | 52 | 0.8 (0.6, 1.0) | 74 | 9 | 2.1 (1.1, 4.1) |
| Interview before loss | 2904 | 135 | 1.0 | 1073 | 67 | 1.5 (1.1, 2.0) | 998 | 54 | 1.3 (0.9, 1.8) | 74 | 13 | 4.5 (2.5, 8.0) |
| Restriction | ||||||||||||
| Women in first pregnancy | 1087 | 98 | 1.0 | 419 | 46 | 1.4 (1.0, 2.0) | 391 | 41 | 1.4 (0.9, 2.0) | 27 | 5 | 2.7 (1.1, 6.8) |
| Women with fetal cardiac motion | 3203 | 321 | 1.0 | 1180 | 117 | 1.2 (1.0, 1.5) | 1084 | 95 | 1.0 (0.8, 1.3) | 95 | 22 | 3.4 (2.2, 5.3) |
SAB: spontaneous abortion, or miscarriage
unadjusted odds ratio
only including pregnancies whose gestational age calculated by last menstrual period and by ultrasound agree within the specified amount (3 days or 7 days).
DISCUSSION
Vaginal bleeding is a common, and potentially alarming, symptom in early pregnancy. Our aim was to investigate whether such bleeding was a risk factor for subsequent miscarriage. After setting aside the miscarriage bleeding, we found that heavy bleeding (similar or greater than that seen during a woman's normal menses) was strongly predictive of subsequent miscarriage, with three times the risk of women without bleeding. Further analyses suggested that women who had heavy bleeding that was accompanied by pain were at the greatest risk. Women with spotting or light bleeding that was associated with pain and continued for several days may also be at increased risk, though confidence intervals were wide.
Adjustment for maternal age, prior miscarriage, and smoking status did not affect our results, suggesting that bleeding is not merely a mediator of adverse effects on pregnancy reflected in these factors. We emphasize the unadjusted results because they are applicable to clinical care. If a pregnant woman informs her obstetrician of a prior episode of bleeding or spotting during a prenatal visit and inquires about the potential impact of such an episode on the health of her pregnancy, our results provide risk estimates.
Our main results showed no substantial differences when subjected to several sensitivity analyses. Results were similar when analysis was restricted to women in their first pregnancy, to women whose gestational dating by LMP was consistent with ultrasound, to women whose time of interview occurred either before or after the loss, and to women whose fetuses exhibited fetal cardiac motion at time of ultrasound. Little changed when we excluded bleeding episodes within 7 days of a loss instead of within 4 days as in the main analysis.
Several previous studies estimated the risk of miscarriage for women presenting to emergency or hospital care (9–11). Many women in such a sample would be presenting with a current miscarriage, and these studies exclude many pregnant women who experience bleeding but do not seek emergency care. Two previous population-based studies examined the relationship between first-trimester bleeding and second-trimester miscarriage (13, 14). We replicated these analyses, and obtained similar results.
In the Right From the Start sample, bleeding prevalence is highest around gestational week 5–8 (manuscript in preparation). The subset of heavy bleeding episodes has a similar distribution to the distribution of all bleeding episodes. The timing of this peak coincides with the timing of important phases of placental development. A hormonally functional placenta is required for the luteal to placental shift in progesterone production that occurs around gestational week 7 (17). Additionally, around the 10th week of pregnancy, the trophoblast blockage of the spiral arteries breaks down, remodeling of the arteries occurs, and the resulting blood flow to the developing placenta dramatically increases the oxygen tension (18). Premature onset of maternal-fetal circulation may expose the placenta and fetus to harmful levels of oxidative stress. Heavy bleeding during this time in pregnancy may be indicative of an underlying defect in placental development. Early placental insufficiency has been implicated in several adverse pregnancy outcomes, including miscarriage (19). Additionally, our observation that the most substantial increase in risk occurs for heavy, painful bleeding episodes suggests the presence of uterine contractions, which may occur due to low progesterone levels. Presence of contractions may facilitate the transfer of pathogens from the vagina to the uterus, (20) further jeopardizing pregnancy. A pregnancy study that prospectively monitors hormone levels and placental blood flow could provide valuable insights on potential mechanisms.
Importantly, our study provides evidence that spotting or light bleeding episodes, especially those without pain and lasting only a day or two, do not increase the risk of miscarriage above baseline risk, i.e. the risk for women with no bleeding. However, pregnant women reporting these symptoms can be reassured that their relative risk of miscarriage is not increased compared to the general population. Most previous studies have been unable to assess the effect of light bleeding or spotting because most were conducted in hospital or clinic-based populations, or based entirely on medical records, and such episodes come to clinical attention less frequently (8–11, 21). Furthermore, rigorous evaluation of the relationship between early pregnancy bleeding and first-trimester miscarriage requires enrollment early in pregnancy, which other population-based bleeding studies have not done (13, 14)..
Our study is also strengthened by other factors. The incorporation of early pregnancy ultrasound allows assessment of fetal viability and verification of gestational dating early during pregnancy. Right From the Start participants are a highly motivated group of women who have demonstrated their ability to provide accurate data on the presence and timing of early pregnancy events, such as timing of last menses (15).
Limitations of this analysis include our inability to know the exact time of fetal demise. Although we have removed those bleeding episodes that immediately precede miscarriage, we may be including some loss-specific episodes in our bleeding definition if miscarriage does not result within 4 days of the end of the episode. We do not have access to detailed ultrasound reports conducted at the time of a bleeding episode; such ultrasounds would be conducted as part of each participant's prenatal care and not as part of the study protocol. Additionally, despite our relatively large study population, few women reported heavy bleeding episodes, yielding imprecise estimates. Our study is also limited by the timing of bleeding ascertainment. Bleeding data were collected after the time of loss for 60% of the losses, raising the potential for recall bias. Finally, our analysis relied on subjective reports of bleeding episode heaviness.
To conclude, we found that painful bleeding episodes with heaviness similar to or greater than usual menses were associated with risk of miscarriage. Although only about 2% of pregnant women in our study sample reported heavy bleeding, reports of such episodes warrant greater concern for the health of the pregnancy. Among intrauterine pregnancies, light bleeding or spotting of short duration does not increase the risk of miscarriage.
Acknowledgments
Support The field research was supported in part by grants from the National Institute of Child and Human Development (5R01HD043883 and 5R01HD049675) and the American Water Works Association Research Foundation (2579). Additional funds were provided by the National Institute of Environmental Health Sciences (Intramural Research Program and P30ES10126).
Footnotes
Financial Disclosure: The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Williams MA, Mittendorf R, Lieberman E, Monson RR. Adverse infant outcomes associated with first-trimester vaginal bleeding. Obstet Gynecol. 1991;78:14–8. [PubMed] [Google Scholar]
- 2.Ananth CV, Savitz DA. Vaginal bleeding and adverse reproductive outcomes: a meta-analysis. Paediatr Perinat Epidemiol. 1994;8:62–78. doi: 10.1111/j.1365-3016.1994.tb00436.x. [DOI] [PubMed] [Google Scholar]
- 3.Yang J, Hartmann KE, Savitz DA, et al. Vaginal bleeding during pregnancy and preterm birth. Am J Epidemiol. 2004;160:118–25. doi: 10.1093/aje/kwh180. [DOI] [PubMed] [Google Scholar]
- 4.Berkowitz GS, Harlap S, Beck GJ, Freeman DH, Baras M. Early gestational bleeding and pregnancy outcome: a multivariable analysis. Int J Epidemiol. 1983;12:165–73. doi: 10.1093/ije/12.2.165. [DOI] [PubMed] [Google Scholar]
- 5.Sipila P, Hartikainen-Sorri AL, Oja H, Von Wendt L. Perinatal outcome of pregnancies complicated by vaginal bleeding. Br J Obstet Gynaecol. 1992;99:959–63. doi: 10.1111/j.1471-0528.1992.tb13697.x. [DOI] [PubMed] [Google Scholar]
- 6.South J, Naldrett J. The effect of vaginal bleeding in early pregnancy on the infant born after the 28th week of pregnancy. J Obstet Gynaecol Br Commonw. 1973;80:236–41. doi: 10.1111/j.1471-0528.1973.tb02191.x. [DOI] [PubMed] [Google Scholar]
- 7.Hertz JB, Heisterberg L. The outcome of pregnancy after threatened abortion. Acta Obstet Gynecol Scand. 1985;64:151–6. doi: 10.3109/00016348509154709. [DOI] [PubMed] [Google Scholar]
- 8.Bennett GL, Bromley B, Lieberman E, Benacerraf BR. Subchorionic hemorrhage in first-trimester pregnancies: prediction of pregnancy outcome with sonography. Radiology. 1996;200:803–6. doi: 10.1148/radiology.200.3.8756935. [DOI] [PubMed] [Google Scholar]
- 9.Gracia CR, Sammel MD, Chittams J, Hummel AC, Shaunik A, Barnhart KT. Risk factors for spontaneous abortion in early symptomatic first-trimester pregnancies. Obstet Gynecol. 2005;106:993–9. doi: 10.1097/01.AOG.0000183604.09922.e0. [DOI] [PubMed] [Google Scholar]
- 10.Tongsong T, Srisomboon J, Wanapirak C, Sirichotiyakul S, Pongsatha S, Polsrisuthikul T. Pregnancy outcome of threatened abortion with demonstrable fetal cardiac activity: a cohort study. J Obstet Gynaecol. 1995;21:331–5. doi: 10.1111/j.1447-0756.1995.tb01019.x. [DOI] [PubMed] [Google Scholar]
- 11.Chung TK, Sahota DS, Lau TK, Mongelli JM, Spencer JA, Haines CJ. Threatened abortion: prediction of viability based on signs and symptoms. Aust N Z J Obstet Gynaecol. 1999;39:443–7. doi: 10.1111/j.1479-828x.1999.tb03129.x. [DOI] [PubMed] [Google Scholar]
- 12.Basama FM, Crosfill F. The outcome of pregnancies in 182 women with threatened miscarriage. Arch Gynecol Obstet. 2004;270:86–90. doi: 10.1007/s00404-003-0475-z. [DOI] [PubMed] [Google Scholar]
- 13.Weiss JL, Malone FD, Vidaver J, et al. Threatened abortion: A risk factor for poor pregnancy outcome, a population-based screening study. Am J Obstet Gynecol. 2004;190:745–50. doi: 10.1016/j.ajog.2003.09.023. [DOI] [PubMed] [Google Scholar]
- 14.Strobino BA, Pantel-Silverman J. First-trimester vaginal bleeding and the loss of chromosomally normal and abnormal conceptions. Am J Obstet Gynecol. 1987;157:1150–4. doi: 10.1016/s0002-9378(87)80280-6. [DOI] [PubMed] [Google Scholar]
- 15.Hoffman CS, Messer LC, Mendola P, Savitz DA, Herring AH, Hartmann KE. Comparison of gestational age at birth based on last menstrual period and ultrasound during the first trimester. Paediatr Perinat Epidemiol. 2008;22:587–96. doi: 10.1111/j.1365-3016.2008.00965.x. [DOI] [PubMed] [Google Scholar]
- 16.Pawloski LR, Kitsantas P. Classification tree analysis of stunting in Malian adolescent girls. Am J Hum Biol. 2008;20:285–91. doi: 10.1002/ajhb.20716. [DOI] [PubMed] [Google Scholar]
- 17.Csapo AI, Pulkkinen M. Indispensability of the human corpus luteum in the maintenance of early pregnancy. Luteectomy evidence. Obstet Gynecol Surv. 1978;33:69–81. doi: 10.1097/00006254-197802000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Jauniaux E, Johns J, Burton GJ. The role of ultrasound imaging in diagnosing and investigating early pregnancy failure. Ultrasound Obstet Gynecol. 2005;25:613–24. doi: 10.1002/uog.1892. [DOI] [PubMed] [Google Scholar]
- 19.Jauniaux E, Poston L, Burton GJ. Placental-related diseases of pregnancy: Involvement of oxidative stress and implications in human evolution. Hum Reprod Update. 2006;12:747–55. doi: 10.1093/humupd/dml016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seong HS, Lee SE, Kang JH, Romero R, Yoon BH. The frequency of microbial invasion of the amniotic cavity and histologic chorioamnionitis in women at term with intact membranes in the presence or absence of labor. Am J Obstet Gynecol. 2008;199:375, e1–5. doi: 10.1016/j.ajog.2008.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Everett C. Incidence and outcome of bleeding before the 20th week of pregnancy: prospective study from general practice. Bmj. 1997;315:32–4. doi: 10.1136/bmj.315.7099.32. [DOI] [PMC free article] [PubMed] [Google Scholar]