Abstract
Objective
Compare results of cochlear implantation in younger and older adults in the domains of disability and handicap, as well as in tests of word recognition and localization, across unilateral implant (CI), bilateral (CI+CI) and CI with an acoustic hearing aid in the non-implanted ear (CI+HA).
Design
Three parts: retrospective (post-implant only) analysis; prospective (pre-versus post-implant); correlation between age and benefit from CI versus CI+CI. Two age groups, above and below 60 years, for the first two analyses; age is a continuous variable for the third analysis.
Setting
Tertiary referral hospital clinic
Patients
Postlingually severely-to-profoundly hearing impaired adults: Totals of 68 CI, 36 CI+CI, and 38 CI+HA in the retrospective part of the study; totals of 30 CI, 18 CI+CI and 16 CI+HA in the prospective parts. Numbers vary from these totals on individual measures.
Interventions
Patients receive either one or two cochlear implants; some with one CI opt to retain a hearing aid in the non-implanted ear.
Outcome measures
Principal measures: Hearing Handicap Inventory for the Elderly, Hearing Handicap Questionnaire, Speech, Spatial and Qualities of Hearing scale, word recognition test, and soundfield localization test. The study is exploratory, but proceeding from a null hypothesis of no expected contrast as a function of patient age.
Results
All patient groups show significant benefit following implantation. No significant age-related differences are observed in patients with unilateral implant, nor in CI+HA group. In the CI+CI group, the younger cohort showed very substantial increases in both performance and self-rated abilities; the older cohort provides more mixed outcomes.
Conclusion
Results for the CI group confirm and extend earlier research. The result for the younger group of CI+CI patients demonstrates the consistent incremental benefit obtained from a bilateral procedure. The mixed outcome observed in the older CI+CI group might be due to individual differences in interaction between effects of aging and the ability to integrate binaural cues.
Introduction
There has been growing interest by clinical researchers in the outcomes for people with cochlear implants in terms of effects on their everyday lives. This represents a broadening of attention from outcomes based on performance test results to consequences for the person in terms of real-world functioning and quality of life (1–6). Investigation at this level reflects a concern to understand where benefits of implantation arise for patients in everyday terms, and equally where residual disabilities and handicaps remain.
The terms disability and handicap are as defined by the World Health Organisation (7). Disability refers to everyday problems due directly to hearing impairment, such as difficulty following a conversation, or telling the location of events; handicap refers to non-auditory consequences which flow from disabilities, such as heightened stress level, or restricted social engagement.
Several research groups have investigated the relative benefit of implantation as a function of adult age. This is motivated by concern about the value of the procedure among people late in life, particularly in view of the high cost, the possibility of reduced effectiveness in “aging auditory systems”, and the general health effects of any surgical procedure, even one like cochlear implantation that is considered low risk. One particular issue for implantation is the value added by a second implant. Ours appears to be the first report to examine the issue of bilateral implantation in relation to patient age.
Most investigations looking at adult age and implantation have focused on performance tests, typically using speech materials. Two papers from early in the current decade (8,9) provide partial reviews of studies on the issue of adult age and (unilateral) implantation that were reported in the previous decade, as well as reporting their own findings. Typically, an age between 55 and 65 years is taken as distinguishing younger from older adult subgroups. Performance measures have consistently shown that older recipients benefit from the implant procedure, and there is no indication that this benefit is less significant than in younger adults.
Attention was given in one or two of the above studies to patients’ reported use and benefit of their implant. Djalilian and colleagues (8) used a modified version of an inventory compiled by Horn et al. (10) to inquire about the length of time each day the implant was used, the benefit (or otherwise) it conferred in different conversational contexts, and effects on “quality of life” and social confidence. No differences were observed in the rates of positive responding to these questions between those younger and older than 60 years.
There has been a continuing flow of studies, based on standard performance measures of speech perception, comparing younger and older adult implant recipients (11–16). The conclusion from earlier investigations is not altered by this subsequent work, to the effect that no significant differences are found on these measures between older and younger adult patients. If “older adult” is defined as greater than 70 years, there is an indication that post-implantation speech performance is lower than for those below that age (12,16).
Maillet, Tyler and Jordan (2) correlated chronological age with measures of quality of life (17) in a sample of implant patients ranging from 30 to 80 years. A small but statistically significant negative relation was observed between age and the degree of pre-post-implant difference in self-rated quality of life, indicating that older respondents experienced less change than those younger. A somewhat stronger negative correlation was observed between reported duration of deafness and change in self-rated quality of life.
Vermeire et al. (4) studied quality-of-life benefit as a function of adult implant age, along with a performance test of speech perception (monosyllable recognition). The quality-of-life measures included the Hearing Handicap Inventory for Adults (18) and the Glasgow Benefit Inventory (19). Vermeire et al. divided their sample into three age categories. They reported on outcomes for a group aged less than 55 years, a group aged 56 to 69, and one aged 70 and older. With that split, it was found that the oldest subgroup showed statistically significantly lower speech performance than the other groups, both pre- and post-operatively, but no differences across age groups in the extent of pre- to post-implant improvement on the speech test. On the HHIA and GBI there were no differences among age groups.
In concluding their report, Vermeire et al. suggested that a more detailed appraisal of the disabling effects of hearing impairment could provide richer information about consequences of implantation as a function of age. They identified the Speech, Spatial and Qualities of Hearing scale (SSQ) (20) as such a measure for this purpose. Our project (6) has included the SSQ; there is opportunity, therefore, to examine self-rated disabilities in addition to performance and handicap ratings in our patient groups as a function of chronological age. A novel feature of our data is that they have been provided by patients comprising three different implant configurations, namely, unilateral (CI), bilateral (CI+CI) and an implant plus acoustic hearing aid voluntarily retained in the non-implanted ear (CI+HA).
Method
Participants and materials
The design of the study is both prospective and retrospective. In the latter case, results of patients with more than 100 months of implant experience are not included, as earlier analysis (5) showed that such long-term cases tended to have slightly lower disability and handicap scores. Also, these longer-term cases are almost exclusively unilateral CI, so comparative results across implant profiles would be slightly biased by their inclusion. The age distribution of patients makes a split at 60 years practical. A subset of patients undertook self-rating and performance testing pre- as well as post-implantation, and these data offer a prospective view of outcomes across the range of implant profiles, as a function of adult age. Not all patients completed every aspect of the assessment protocol, and variations in numbers are reported at appropriate points in the results section of the paper.
Details of materials and procedures are given in our previous reports (5,6). Briefly, pre-implant performance and self-report measures were obtained several weeks, and never more than one or two months, prior to implantation. Post-implant measures were obtained at least 12 months post-implantation. The self-report components of the assessment protocol comprise the Hearing Handicap Inventory for the Elderly (21), the Hearing Handicap Questionnaire (20), and the SSQ (20). These were completed by patients as part of a package of survey instruments; The two performance measures — recorded CNC words (22) and an everyday sounds horizontal plane localization test (23)— were completed during visits to the University of Iowa Otolaryngology clinic. All participants in this project were recruited as part of the ongoing cochlear implant research program, as approved by the Institutional Review Board, with participants giving written consent.
Results
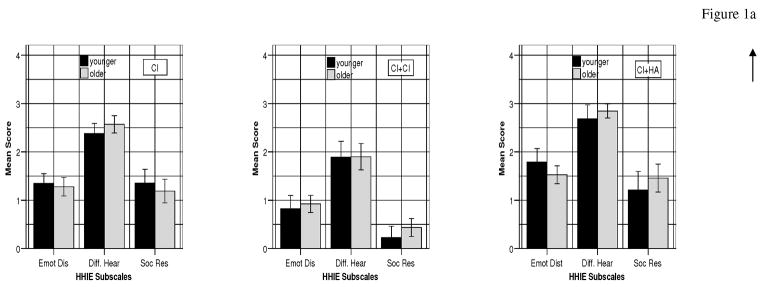
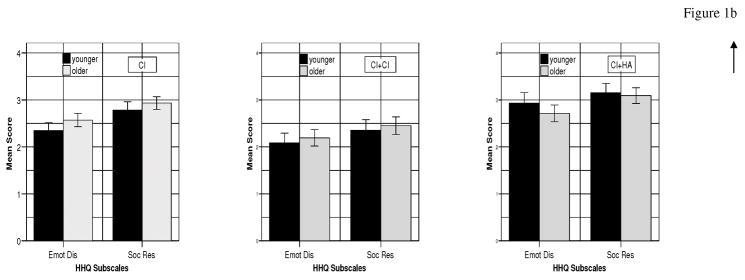
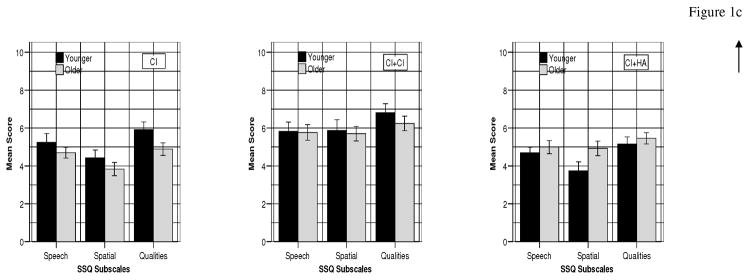
The self-report data are presented in subscales derived from items in the measures used. In the case of the HHIE and HHQ these subscales are the result of factor analyses whose details are described in Noble et al. (5). From the factor analysis of the HHIE one subscale was interpreted as measuring in the disability rather than handicap domain, and was labelled “difficulty in hearing”; this interpretation is supported by the consistently higher average scores on that subscale (Figures 1a and 2a) compared with the other two. In the case of the SSQ, results are reported for the three major subsections (Speech, Spatial, and Qualities of hearing). The speech test data are percent correct scores; localization performance is expressed as RMS error between actual and perceived locations.
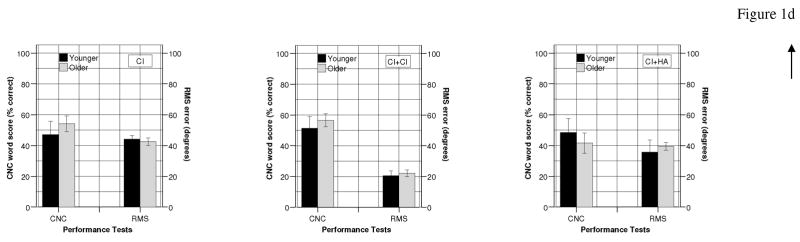
Figure 1.
Figure 1a: HHIE subscale scores for CI (Younger n=31; Older n=37), CI+CI (n=13; 23), and CI+HA (n=14; 24) groups.
Figure 1b: HHQ subscale scores for CI (Younger n=31; Older =36), CI+CI (n=13; 23), and CI+HA (n=13; 24) groups
Figure 1c: SSQ subscale scores for CI, CI+CI, and CI+HA groups (sample sizes as for Figure 1a).
Figure 1d: Mean % correct on the speech performance measure (CNC) for CI (Younger n=7; Older n=17), CI+CI (n=9; 18), and CI+HA (n=4; 7) groups: mean error on localization task (RMS) for CI (n=3; 7), CI+CI (n=13; 22) and CI+HA (n=2; 2) groups.
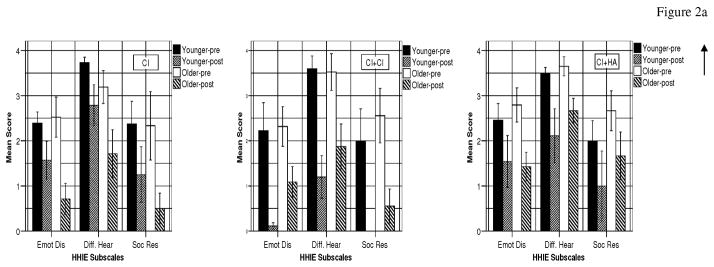
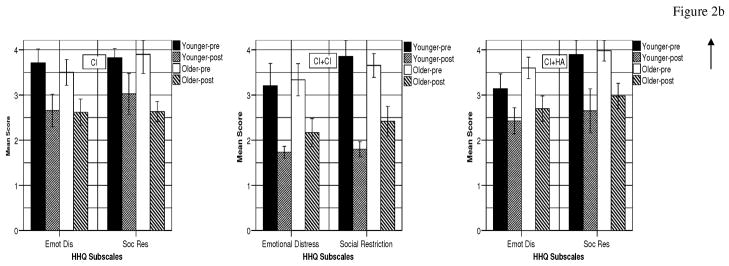
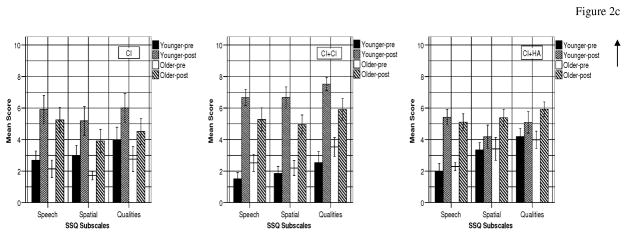
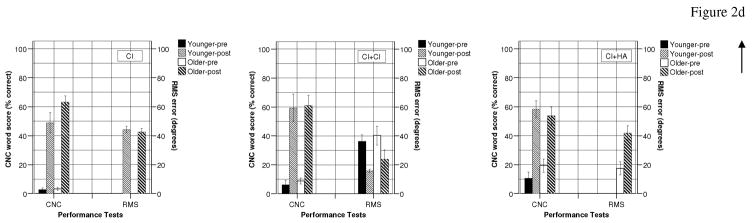
Figure 2.
Figure 2a: Pre-post HHIE subscale scores for CI (Younger n=8; Older n=6), CI+CI (n=5; 9), and CI+HA (n=5; 9) groups.
Figure 2b: Pre-post HHQ subscale scores for CI (Younger n=8; Older n=6), CI+CI (n=7; 11), and CI+HA (n=4; 10) groups.
Figure 2c: Pre-post SSQ subscale scores for CI (n=8; 6), CI+CI (n=8; 10), and CI+HA (n=5; 11) groups.
Figure 2d: Pre-post mean % correct on speech performance measure (CNC) for CI (Younger n=12; Older n=18), CI+CI (n=6; 8), and CI+HA (n=4; 12) groups: pre-post mean error on localization task (RMS) for CIi (n=3; 7), CI+CI (n=7; 5), and CI+HAii (n=0; 2) groups.
iThere are no pre localization scores in the CI group.
iiThere are no younger patients providing pre-post localization scores in the CI+HA group.
Results are in three sections: 1. Post-implant outcomes as a function of age and implant profile (these are the most numerous data); 2. Pre-post implant contrasts as a function of age and implant profile (smaller data sets); 3. Unilateral and bilateral benefit and chronological age (comparison of pre-post implant contrasts as a function of age for CI and CI+CI patients).
1. Post-implant outcomes as a function of age and implant configuration
The left-hand part of Table 1 shows numbers and demographic features of patients who completed the HHIE and SSQ post-implant. There was one less (older) patient in the CI group and one less (younger) in the CI+HA group who completed the HHQ; such differences minimally affect the demographic pattern shown in the left-hand part of Table 1. The right-hand part of Table 1 gives numbers and demographics of patients who completed the speech test post-implant. There are greater differences between these numbers and those in the left-hand part of the Table, consequently the demographics vary to a rather greater extent. There were different numbers again completing the localization test (as shown by the numbers in square brackets), and the demographics vary slightly from those of the speech test groups. With the exception of gender proportions, none of the differences between groups, and variations in those differences, is statistically significant.
Table 1.
Number of patients, gender distribution, average age, and time since implantation (SDs in brackets) in one CI, two CI (CI+CI), and CI and hearing aid (CI+HA) groups completing HHIE/SSQ, speech test (CNC) and localization test [Loc] post-implantation.
| HHIE/SSQ | CNC/[Loc] | |||||
|---|---|---|---|---|---|---|
| Younger | Older | Younger | Older | |||
| Number | CI | 31 | 37 | CI | 7 [3] | 17 [7] |
| CI+CI | 13i | 23ii | CI+CI | 9 [13] | 18 [22] | |
| CI+HA | 14 | 24 | CI+HA | 4 [2] | 7 [2] | |
| %Female | CI | 45.2% | 51.4% | CI | 0% [33.3%] | 58.8% [57.1%] |
| CI+CI | 53.8% | 56.5% | CI+CI | 66.7% [53.8%] | 50% [54.5%] | |
| CI+HA | 85.7% | 66.7% | CI+HA | 100% [100%] | 71.4% [50%] | |
| Age (in years) | CI | 46.9(8.2) | 72.2(8.3) | CI | 47.7(5.9) | 74.9(7.3) |
| CI+CI | 47.5(11.0) | 74.5(6.3) | CI+CI | 50.9(6.8) | 74.7(6.7) | |
| CI+HA | 44.1(11.9) | 71.5(5.9) | CI+HA | 47.6(14.0) | 70.1(6.7) | |
| Post-implantation time (in months) | CI | 39.0(24.7) | 44.6(28.8) | CI | 65.3(20.8) | 58.5(31.6) |
| CI+CI | 34.7(23.9) | 34.4(25.4) | CI+CI | 42.8(24.6) | 38.7(25.0) | |
| CI+HA | 31.7(15.3) | 23.7(13.0) | CI+HA | 42.0(6.9) | 28.1(9.0) | |
12 of the younger CI+CI cases received bilateral implants simultaneously (1 successively)
19 of the older CI+CI cases received bilateral implants simultaneously (4 successively)
Figures 1a to 1d show, respectively, average post-implantation ratings on the three self-report measures (HHIE, HHQ, and SSQ) and on the two performance tests (speech recognition and sound source localization). Outcomes for the three implant configurations (CI, CI+CI, CI+HA) are graphed separately for the two age cohorts: 20–59 years and 60–91 years. For the HHIE and HHQ the higher the histogram the greater is rated handicap as defined earlier (and disability, in the case of the HHIE “difficulty in hearing” subscale). For the SSQ the higher the histogram the greater is rated ability.
There are no significant differences (t-tests) between younger and older cohorts in the CI, CI+CI or CI+HA groups on the HHIE and HHQ subscales. On the SSQ there is a trend among the CI and CI+CI groups toward higher ability ratings in the younger than the older cohorts, bordering on significance (p=0.051) among the CI patients in the case of the Qualities subscale. The opposite trend can be seen in the CI+HA group. These trends are paralleled by results on the HHQ (where a higher histogram means greater rated handicap). There are no differences in speech or localization test performance between younger and older groups in any of the three implant profiles. (As may be seen, irrespective of age group, there are some notably different outcomes among implant configurations: this feature of the data is the focus of our previous reports [5,6], hence is not commented on further in this paper.)
2. Pre-post implant contrasts as a function of age and implant configuration
The left-hand part of Table 2 shows the numbers and demographic features of patients who completed pre- as well as post-implant SSQ self-ratings. In braces are shown the numbers who completed the HHIE, pre- as well as post-implantation. There were further variations, but only by one case, in the numbers completing the HHQ. As can be seen there are moderate differences in the numbers of people providing pre- as well as post-implant data on the self-assessment scales. These differences were associated with minor variations in the demographics of the samples, none of which reached statistical significance. Hence the values for gender proportions, age, and time since implantation for the groups completing the SSQ are representative of the groups overall, as regards the self-report measures.
Table 2.
Number of patients, gender distribution, average age, and time since implantation (SDs in brackets) in one CI, two CI (CI+CI), and CI and hearing aid (CI+HA) groups, pre- and post-implantation, completing SSQ/HHIE, speech test (CNC) and localization [Loc] test. Braces in the 3rd and 4th columns show numbers in CI+CI and CI+HA groups completing HHIE. Square brackets in the last two columns show numbers and proportions of females completing Loc test.
| SSQ/HHIE | CNC/[Loc] | |||||
|---|---|---|---|---|---|---|
| Younger | Older | Younger | Older | |||
| Number | CI | 8 | 6 | CI | 12 [3] | 18 [7] |
| CI+CI | 8{5} | 10{9} | CI+CI | 6 [7] | 8 [5] | |
| CI+HA | 5 | 11{9} | CI+HA | 4 [nil] | 12 [2] | |
| %Female | CI | 62.5% | 50.0% | CI | 33.3 % [33.3%] | 50% [57.1%] |
| CI+CI | 60.0% | 33.3% | CI+CI | 83.3% [85.7%] | 50% [20%] | |
| CI+HA | 60.0% | 77.8% | CI+HA | 75% [nil] | 58.3% [50%] | |
| Age (in years) | CI | 43.4(12.4) | 67.7(6.7) | CI | 48.0(5.4) | 73.8(7.2) |
| CI+CI | 39.4(13.7) | 74.4(5.5) | CI+CI | 47.2(8.4) | 77.4(5.7) | |
| CI+HA | 48.6(8.3) | 71.1(5.2) | CI+HA | 49.3(10.3) | 71.6(6.4) | |
| Post-implantation time (in months) | CI | 18.0(9.1) | 16.0(6.2) | CI | 67.8(25.9) | 75.3(34.1) |
| CI+CI | 21.6(15.7) | 25.6(14.9) | CI+CI | 43.3(26.0) | 51.8(29.6) | |
| CI+HA | 16.8(6.6) | 17.3(6.3) | CI+HA | 42.0(23.0) | 38.2(19.8) | |
The right-hand part of Table 2 shows demographic data for patients who completed the speech test pre- as well as post-implantation. While the gender proportions and ages of these groups are not substantially different from the values shown in the left-hand part of the Table, the lengths of time since implantation are significantly greater. The differences in the latter data, both as between self-report and speech test groups and as between speech and localization test groups, reflect the point that pre- as well as post-implantation speech testing has been part of clinical appraisal for many years in the Iowa program, whereas localization testing and self-ratings pre-implantation are a more recent addition to the protocol. In square brackets are the numbers of patients completing the localization performance test pre- as well as post-implantation, and the proportions of females in each such group. There are no substantial differences in time since implantation across the younger versus older groups in any one implant profile within any one measure, hence the comparisons of interest are not likely to be biased by that factor. Because sample sizes in this part of the report are limited, results of this prospective analyses should be regarded as indicative only, requiring further investigation.
Figures 2a to 2d show pre- and post-implant self-ratings and performance scores for younger and older groups as a function of implant configuration. As before, for the HHIE and HHQ the higher the histogram the greater is rated handicap; for the SSQ the higher the histogram the greater is rated ability. Thus it will be expected, and as can be seen, pre-implant ratings on the HHIE and HHQ are higher than post-implant; the opposite is expected, and observed, for the SSQ.
It is evident that all groups show reductions in handicap and increases in both self-rated and measured ability, regardless of age group. There is a trend in the CI group’s data toward stronger pre-post contrast in handicap ratings (HHIE and HHQ) among older compared with younger patients. The contrary trend is seen in the CI+CI groups, with no trend across age groups in the CI+HA group. On the disability measure (SSQ) there is no evident difference in pre-post contrast across age groups among the CI patients, while there is a clear age-group difference for the CI+CI patients. The younger CI+CI patients show strongly improved post-implant ratings across the three subscales, and coming from a lower pre-implant baseline, compared with the older patients. By comparison, the younger CI+HA patients record modest post-implant improvements, especially in self-rated Spatial and Qualities domains.
Pre- versus post-implant speech performance data show no age contrast in any of the implant groups, although older CI+HA patients have smaller post-implant performance improvement than do younger. Pre-post localization data are limited. The post-implant-only localization data for the CI group show no age difference; the pre-post contrasts in the CI+CI group suggest a greater proportionate improvement in younger versus older patients, mirroring the pre-post contrast in Spatial subscale ratings for the SSQ across the two age cohorts.
To examine these outcomes more closely, “change” scores (post- minus pre-implantation ratings and performance levels) were computed and compared between age groups in the three implant groups. No significant age-related differences in these change scores were observed across the range of measures for the CI and CI+HA groups. The same is true in the CI+CI group for the scores on the HHIE and HHQ, and on the two performance tests; but there are significantly greater change scores in the younger versus older group on two SSQ subscales: Speech [t(16)=2.71, p=.02] and Qualities[t(16)=2.20, p=.04]. Inspection of individual data revealed two cases in the older CI+CI age group whose SSQ post-implantation scores were basically unchanged compared with pre-implant ratings. Given the limited sample size, these two cases influence the overall result.
3. Unilateral and bilateral benefit as a function of age (correlation)
In this section the correlation is examined between chronological age and the effect of being fit with one versus two cochlear implants, using the pre-to-post-implant change scores in self-ratings and performance referred to in the previous section (for this analysis the data from the CI+HA groups are not considered). The analysis allows observation of the influence of age on the extent of benefit from implantation, and the influence of age on relative benefit of one versus two cochlear implants. The null hypothesis is that there is no correlation between age and implant benefit.
Table 3 lists correlation coefficients between chronological age and the degree of difference between pre- and post-implant self-ratings/performance for the CI and CI+CI groups. (Partial correlation analyses were also undertaken, controlling for time since implantation: this factor showed minimal impact on the correlation values in Table 3.) In brackets, for the CI+CI group, are correlations between the variables of interest but excluding the two cases mentioned in the previous section.
Table 3.
Correlations of difference scores for HHIE, HHQ, SSQ subscales, Speech test (CNC), and Localization test (Loc) with chronological age. Values in brackets under CI+CI group are after removal of two cases (see text).
| HHIE subscales difference score (Post-Pre) | CI n = 14 | CI+CI n=14 (n=12) |
|---|---|---|
| Emotional Distress | −.29 | .06 (−.07) |
| Difficulty in Hearing | −.15 | .12 (−.05) |
| Social Restriction | .02 | −.13 (−.34) |
| HHQ subscales difference score (Post-Pre) | CI (n = 14) | CI+CI n=18 (n=16) |
| Emotional Distress | .03 | −.08 (−.17) |
| Social Restriction | −.24 | .19 (−.07) |
| SSQ subscales difference score (Post-Pre) | CI (n = 14) | CI+CI n=18(n=16) |
| Speech | −.03 | −.55* (−.51*) |
| Spatial | .03 | −.48* (−.41) |
| Qualities | −.18 | −.45 (−.36) |
| Speech test difference score (Post-Pre) | CI (n = 30) | CI+CI n=14(n=13) |
| CNC | .22 | −.31 (−.26) |
| Localization test difference score (Post-Pre) | CI | CI+CI n=12(n=11) |
| Loc | no pre-test data | .15 (.17) |
p < .05
For the CI group there are no significant correlations between chronological age and self-rated changes in disability or handicap, indicating that age does not bear on the outcome of implantation on the scales reported on here. This is consistent with results reported in the previous section. For the CI+CI group, there are no significant correlations between age and pre-post changes in handicap rating, but there are significant negative correlations between age and the extent of reduction in self-rated disability, as reflected in Speech and Spatial subscales of the SSQ. When the two CI+CI cases who showed essentially no change in pre-post SSQ ratings are excluded from the analysis, the correlations with age become non-significant for the Spatial subscale while a significant negative correlation remains for the Speech subscale. There are no significant correlations between age and change in speech recognition or localization performance.
Changes in self-rated disability can be better appreciated by noting, first, that the self-rating scale used in the SSQ runs from 0 to 10, with 0 representing complete inability with regard to the item in question, 10 representing perfect ability. Noble and Gatehouse (24) compared SSQ ratings of clinic clients not yet acoustically aided with those of clients fit with one versus two hearing aids. They found that average differences in SSQ ratings, between unaided and aided samples, of one-to-two scale points, were statistically significant, and, as a proportional change in score, can be considered a moderate effect. By extension, a change of two-to-four scale points represents a large effect, and a change of more than four scale points a substantial effect.
Table 4 shows the numbers of younger (to age 59 years) and older CI and CI+CI patients falling into categories of benefit as defined by the foregoing criteria. In the case of unilateral implantation, the data in Table 4 support a conclusion that chronological age has no obvious bearing on how much benefit can be expected. It is also fair to observe that younger adults consistently show signs of major benefit from bilateral implantation; and significant benefit is also observed, if less consistently, in older CI+CI patients.
Table 4.
Numbers of younger and older CI and CI+CI patients in different categories of change in SSQ score from pre- to post-implantation. Category 1 = increase in score by ≥4 points; category 2 = increase by >2<4 points; category 3 = increase by 1–2 points; no change = increase/decrease by <1 point; negative = decrease by >1 point.
| CI | CI+CI | |||
|---|---|---|---|---|
| category | younger | older | younger | older |
| 1 | 3 | 1 | 5 | 2 |
| 2 | 1 | 2 | 3 | 5 |
| 3 | 2 | 2 | - | 1 |
| no change | 1 | 1 | - | 2 |
| negative | 1 | - | - | - |
| total | 8 | 6 | 8 | 10 |
Discussion and Conclusions
An extensive literature accumulating over the last two decades, reviewed in the Introduction, and largely based on speech test performance, leads to a conclusion that adult chronological age does not seem to have a bearing on the effectiveness of cochlear implantation. A threshold age used in different studies is around 60 years, and the consistent finding is of no performance difference between those below or above it. People older than 70 years may show reduced performance on standard speech tests (13, 17), but one study (4) that also used standard self-report measures of benefit and handicap found no age-related differences in these measures even though the 70-and-over group had lower speech performance than younger participants, both pre- and post-operatively. (Results of an independent study [25] could explain this: those investigators showed that the major driver of improved self-assessment, was the degree of contrast between pre- and post-operative auditory threshold, rather than post-operative threshold as such.) These observations are with respect to unilateral implantation, and the present report is consistent with them.
To our knowledge, the present study is the first that examines chronological age in relation to bilateral as well as unilateral implantation; it also includes an extensive measure of self-rated disabilities. This measure indicated the possibility of a contrast between unilateral and bilateral implantation in relation to increasing age.
From the literature reviewed in the Introduction, the null hypothesis was strongly suggested, namely, that chronological age has no bearing on observed benefit. But some recent findings in relation to binaural function and ageing could be of relevance to the outcome with bilateral implantation observed here. Recent studies (26, 27) report that in elderly listeners with clinically normal peripheral hearing function, there are signs of reduced binaural ability resulting in poorer speech recognition in noise compared with younger listeners. One of these (27) also found reduced activation in the bilateral superior temporal gyrus in members of their older sample. A similar study (28) reported that decline in medial olivocochlear function might explain the poorer speech perception in noise observed in elderly listeners. The present outcomes, together with these recent reports, suggest a need for deliberate research strategies and designs to investigate further the impact of bilateral implantation as a function of chronological age.
As regards the patients with a single CI who opt to retain an acoustic aid in the non-implanted ear (CI+HA), previous analyses (5,6) have shown that this group of patients generally fares less well than might be expected. We have suggested (6, p.513) that this could be because patients who opt to retain a hearing aid in the non-implanted ear do so because of less benefit from their CI, compared to other single CI users who are getting adequate benefit and who therefore choose not to retain their hearing aid in the unimplanted ear. There are no strong indications in the present data that chronological age is driving a preference for retention of the HA, with some opposing trends in the self-report versus speech performance data in this group. Notwithstanding the finding that a small number of older CI+CI patients may not be getting benefit from that profile, as reflected in their own assessments of abilities, it remains evident that bilateral implantation offers substantial benefits across the age spectrum. It may emerge from systematic investigation of this issue that more refined pre-assessments are called for in determining optimum candidacy for a bilateral procedure. For example, some older patients might require tailored binaural fitting and training.
Acknowledgments
This research was supported in part by research grant P50 DC000242-21 from the National Institute on Deafness and Other Communication Disorders, National Institutes of Health; grant RR00059 from the General Clinical Research Centers Program, Division of Research Resources, National Institutes of Health; the Lions Clubs International Foundation; and the Iowa Lions Foundation. Our thanks to Haihong (Helena) Ji and Shelley Witt for the time they have given to data management and retrieval.
References
- 1.Hawthorne G, Hogan A, Giles E, et al. Evaluating the health-related quality of life effects of cochlear implants: a prospective study of an adult cochlear implant program. International Journal of Audiology. 2004;43:183–92. doi: 10.1080/14992020400050026. [DOI] [PubMed] [Google Scholar]
- 2.Maillet CJ, Tyler RS, Jordan HN. Change in the quality of life of adult cochlear implant patients. Annals of Otology, Rhinology & Laryngology. 1995;104:31–48. [PubMed] [Google Scholar]
- 3.Summerfield AQ, Barton GR, Toner J, et al. Self-reported benefits from successive bilateral cochlear implantation in postlingually deafened adults: randomised controlled trial. International Journal of Audiology. 2006;45 (Suppl 1):S99–S107. doi: 10.1080/14992020600783079. [DOI] [PubMed] [Google Scholar]
- 4.Vermeire K, Brokx JP, Wuyts FL, et al. Quality-of-life benefit from cochlear implantation in the elderly. Otology & Neurotology. 2005;26:188–95. doi: 10.1097/00129492-200503000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Noble W, Tyler RS, Dunn C, et al. Hearing handicap ratings among different profiles of adult cochlear implant users. Ear & Hearing. 2008a;29:112–20. doi: 10.1097/AUD.0b013e31815d6da8. [DOI] [PubMed] [Google Scholar]
- 6.Noble W, Tyler RS, Dunn C, et al. Unilateral and bilateral cochlear implants and the implant-plus-hearing aid profile: Comparing self-assessed and measured abilities. International Journal of Audiology. 2008b;47:505–14. doi: 10.1080/14992020802070770. [DOI] [PubMed] [Google Scholar]
- 7.WHO. International classification of impairments, disabilities, and handicaps. Geneva: World Health Organization; 1980. [Google Scholar]
- 8.Djalilian HR, King TA, Smith SL, et al. Cochlear implantation in the elderly: Results and quality-of-life assessment. Annals of Otology Rhinology and Otolaryngology. 2002;111:890–5. doi: 10.1177/000348940211101005. [DOI] [PubMed] [Google Scholar]
- 9.Shin YJ, Fraysse B, Deguine O, et al. Benefits of cochlear implantation in elderly patients. Otolaryngology — Head and Neck Surgery. 2000;122:602–6. doi: 10.1067/mhn.2000.98317. [DOI] [PubMed] [Google Scholar]
- 10.Horn KL, McMahon NB, McMahon DC, et al. Functional use of the nucleus 22-channel cochlear implant in the elderly. The Laryngoscope. 1991;101:284–8. doi: 10.1288/00005537-199103000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Chan V, Tong M, Yue V, et al. Performance of older adult cochlear implant users in Hong Kong. Ear & Hearing. 2007;28 (Suppl 2):52S–5S. doi: 10.1097/AUD.0b013e318031509d. [DOI] [PubMed] [Google Scholar]
- 12.Chatelin V, Kim EJ, Driscoll C, et al. Cochlear implant outcomes in the elderly. Otology & Neurotology. 2004:25. doi: 10.1097/00129492-200405000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Hay-McCutcheon MJ, Pisoni DB, Kirk KI. Audiovisual speech perception in elderly cochlear implant recipients. Laryngoscope. 2005;115:1887–94. doi: 10.1097/01.mlg.0000173197.94769.ba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Labadie RF, Carrasco VN, Gilmer CH, et al. Cochlear implant performance in senior citizens. Otolaryngology — Head and Neck Surgery. 2000;123:419–24. doi: 10.1067/mhn.2000.109759. [DOI] [PubMed] [Google Scholar]
- 15.Leung J, Wang NY, Yeagle JD, et al. Predictive models for cochlear implantation in elderly candidates. Archives of Otolaryngology — Head and Neck Surgery. 2005;131:1049–54. doi: 10.1001/archotol.131.12.1049. [DOI] [PubMed] [Google Scholar]
- 16.Sterkers O, Mosnier I, Ambert-Dahan E, et al. Cochlear implants in elderly people: Preliminary results. Acta Oto-Laryngologica. 2004;124 (Supplement 552):64–7. doi: 10.1080/03655230410017184. [DOI] [PubMed] [Google Scholar]
- 17.Wexler M, Miller LW, Berliner KI, et al. Psychological effects of cochlear implant: Patient and “index relative” comparisons. Annals of Otology, Rhinology and Laryngology. 1982;91 (2):59–61. [PubMed] [Google Scholar]
- 18.Newman CW, Weinstein BE, Jacobson GP, et al. The Hearing Handicap Inventory for Adults: Psychometric adequacy and audiometric correlates. Ear and Hearing. 1990;11:430–3. doi: 10.1097/00003446-199012000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Robinson K, Gatehouse S, Browning GG. Measuring patient benefit from otorhinolaryngological surgery and therapy. Annals of Otology, Rhinology & Laryngology. 1996;106:415–22. doi: 10.1177/000348949610500601. [DOI] [PubMed] [Google Scholar]
- 20.Gatehouse S, Noble W. The Speech, Spatial and Qualities of Hearing Scale (SSQ) International Journal of Audiology. 2004;43:85–99. doi: 10.1080/14992020400050014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ventry IM, Weinstein BE. The Hearing Handicap Inventory for the Elderly: A new tool. Ear and Hearing. 1982;3:128–34. doi: 10.1097/00003446-198205000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Tillman TW, Carhart R. Northwestern University Auditory Test No. 6: Technical Report No. SAM-TR-66-55. USAF School of Aerospace Medicine, Brooks Air Force Base; Texas: 1966. An expanded test for speech discrimination utilizing CNC monosyllabic words. [DOI] [PubMed] [Google Scholar]
- 23.Dunn CC, Tyler RS, Witt SA. Benefit of wearing a hearing aid on the unimplanted ear in adult users of a cochlear implant. Journal of Speech, Language, and Hearing Research. 2005;48:668–80. doi: 10.1044/1092-4388(2005/046). [DOI] [PubMed] [Google Scholar]
- 24.Noble W, Gatehouse S. Effects of bilateral versus unilateral hearing aid fitting on abilities measured by the speech, spatial, and qualities of hearing scale (SSQ) International Journal of Audiology. 2006;45:172–81. doi: 10.1080/14992020500376933. [DOI] [PubMed] [Google Scholar]
- 25.Korsten-Meijer AGW, Wit HP, Albers FWJ. Evaluation of the relation between audiometric and psychometric measures of hearing after tympanoplasty. European Archives of Oto-Rhino-Laryngology. 2006;263:256–62. doi: 10.1007/s00405-005-0983-5. [DOI] [PubMed] [Google Scholar]
- 26.Hwang JH, Li CW, Wu CW, et al. Aging effects on the activation of the auditory cortex during binaural speech listening in white noise: an fMRI study. Audiology and Neuro-Otology. 2007;12:285–94. doi: 10.1159/000103209. [DOI] [PubMed] [Google Scholar]
- 27.Kim SH, Frisina RD, Mapes FM, et al. Effect of age on binaural speech intelligibility in normal hearing adults. Speech Communicatiion. 2006;48:591–7. [Google Scholar]
- 28.Mukari SZMS, Mamat WHW. Medial olivocochlear functioning and speech perception in noise in older adults. Audiology and Neuro-Otology. 2008;13:328–34. doi: 10.1159/000128978. [DOI] [PubMed] [Google Scholar]