Abstract
AIM: To compare the efficacy and safety of radical and conservative surgical interventions for liver hydatid disease.
METHODS: The study comprised 59 patients in two groups who had undergone radical and conservative surgical procedures for liver hydatid disease in our department between 2004 and 2009. Preoperative diagnostic tools, medical treatments, demographic and clinical characteristics, postoperative follow-up, and recurrence were compared in both groups.
RESULTS: This non-randomized retrospective study included 59 patients who had undergone liver hydatid disease surgery. The radical technique was used in 18 patients (mean age: 42.1 ± 13.5 years, seven male, 11 female), and the conservative technique was used in 41 patients (mean age: 43.5 ± 13.9 years, 17 male, 24 female). The follow-up period ranged from 3 to 58 mo. Although operative time was significantly shorter in the conservative group (P < 0.001), recurrence was significantly reduced in the radical group (P = 0.045). No statistically significant differences were found in terms of hospitalization duration, cyst count and size, location, postoperative complications, scolicidal solution usage, or follow-up duration between the two groups.
CONCLUSION: The more effective method for preventing postoperative recurrence is radical surgery. Endoscopic retrograde cholangiopancreatography for bile leakage in the early postoperative period may decrease the requirement for repeat surgery.
Keywords: Echinococcosis, Endoscopic retrograde cholangiopancreatography, Digestive system surgery
INTRODUCTION
Hydatid cysts are common in societies where agriculture and raising animals are common, and hydatid disease continues to be a serious public health problem in many countries, including Turkey[1-3]. Hydatid cysts can develop in any organ of the body, but are most frequently seen in the liver (60%-70%) and lungs (20%-30%)[4-6]. Infection rates are lowest in urban environments; in endemic rural areas, prevalence rates of 2%-6% or higher have been recorded[7]. In Turkey, hydatid disease is more common in Eastern and Middle Anatolia and in the Marmara and Trakya regions[3]. The first step in the prevention of hydatid disease is basic hygiene and the second step involves the approach to treatment. No consensus exists regarding the optimal treatment, although medical treatment is effective against larval Echinococcus granulosus (E. granulosus). Surgical treatment varies from complete resection to minimally invasive procedures (e.g. percutaneous aspiration)[8-12].
In this study, we present the surgical approach to hydatid disease patients at our clinic in Diyarbakir, eastern Eastern Anatolia, and a comparison of the efficacy and safety of radical surgery and conservative surgery for liver hydatid disease.
MATERIALS AND METHODS
A total of 59 patients who had undergone surgery for liver hydatid cysts between January 2004 and July 2009 were investigated retrospectively. All the patients in the study were operated on by two surgeons. Patients were divided into two groups according to the type of surgery. The radical surgery group (n = 18) consisted of patients whose treatment involved pericystectomy or left lobe segmentectomy. The conservative surgery group (n = 41) included patients who underwent conservative surgery, including partial cystectomy plus external drainage plus omentopexy, or cystectomy plus external drainage. The data analyzed included patient age, sex, occupation, residence, symptoms, diagnostic tools used, type of cyst, type of surgical procedure, and maximum diameter of the cyst, postoperative complications, preoperative and postoperative anti-helminthic treatment, recurrence, and length of follow-up.
Clinical presentation
For 43 (72.8%) patients, abdominal pain was the initial symptom of hydatid disease. Seven of 43 patients experienced recurrence of the disease between 5 and 22 years after one or more operations elsewhere. In 14 patients, the diagnosis was made incidentally during a medical checkup. Two patients were diagnosed with a hydatid cyst preoperatively during diagnostic laparoscopy for gynecological disease.
Preoperative diagnosis
The preoperative evaluation of the patients included liver function tests, a complete blood count, indirect hemagglutination antibody (IHA), abdominal ultrasonography (USG), and abdominal computed tomography (CT). The cysts were classified according to the five categories described by Gharbi et al[13]. The distribution of the patients according the Gharbi classification is shown in Table 1. CT was performed in 19 patients who had more than one cyst, to obtain detailed information on the location of the cysts (Figure 1, Figure 2A and B). Magnetic resonance cholangiopancreatography was used to confirm the diagnosis in two patients who had suspicious dilatation of the common bile duct (CBD) and three patients with elevated liver function tests. Dilatation of the CBD was observed in only one patient on magnetic resonance imaging. This patient underwent a sphincterotomy via endoscopic retrograde cholangiopancreatography (ERCP) preoperatively.
Table 1.
Comparison of both groups according to Gharbi classification
| Type of cyst | Gharbi classification | Radical surgery | Conservative surgery | Total |
| Type I | Pure fluid collection | Excluded | 0 | |
| Type II | Fluid collection with a split wall | 2 | 7 | 9 |
| Type III | Fluid collection with septal | 5 | 14 | 19 |
| Type IV | Heterogenous acho pattern | 4 | 8 | 12 |
| Type V | Reflecting thick walls | Excluded | 0 | |
| Type III-IV | 4 | 7 | 11 | |
| Type III-IV-V | 3 | 5 | 8 | |
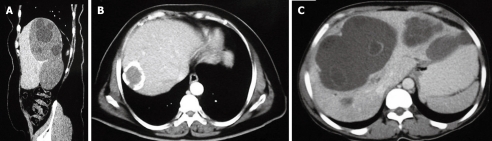
Figure 1.
Multi-detector computed tomography (CT) images in different planes following contrast injection. A: Sagittal plane multi-detector CT images showed cystic lesions in segments 6 and 7 of the right liver lobe; B: A cystic lesion with a calcified wall located in the subcapsular region in the right lobe posterior segment was seen in contrast-enhanced axial plane CT sections; C: Contrast-enhanced axial plane CT images showed widespread cysts with separate membranes in an enlarged liver.
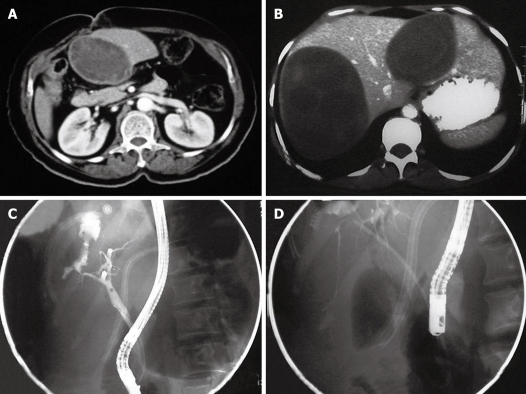
Figure 2.
Contrast-enhanced axial CT and endoscopic retrograde cholangiopancreatography (ERCP) images of three different patients. A: A cystic lesion located in segment 3 of the left lobe was seen in contrast-enhanced axial plane CT images; B: A cystic lesion in the right lobe posterior superior and left lobe medial segment was seen in oral and intravenous contrast-enhanced axial plane CT images; C: Leakage of contrast material into the cyst cavity was observed after placing a cannula and injecting radiopaque material into the biliary tract; D: The same patient after performing a sphincterotomy and inserting a 7 Fr biliary stent.
Cyst characteristics
The size of the cysts was measured by USG and CT; the number of the cysts was counted radiologically and confirmation was made by sight during surgery.
The mean ± SD size of the cysts was 16.28 ± 6.97 cm (range: 8-32 cm) in the RS group vs 12.98 ± 4.90 cm (range: 6-26 cm) in the CS group. There was no significant difference in cyst count (P > 0.694), cyst size (P > 0.088) and in location (P > 0.650) between the two groups. The other cyst characteristics are summarized in Table 2.
Table 2.
Comparison of surgical characteristics, follow-up time and postoperative complications among the both groups n (%)
| Surgical features | Radical surgery | Conservative surgery | Total | P |
| Number of patients | 18 (30.5) | 41 (69.5) | 59 (100) | |
| Operation time (min) | 83.25 ± 12.09 | 51.97 ± 15.07 | 60.91 ± 19.92 | < 0.001 |
| Hospitalization time (d) | 7.62 ± 1.49 (5-10) | 7.24 ± 1.86 (4-21) | 7.42 ± 1.69 | NS |
| Cyst count | 1.72 ± 1.0 (1-4) | 1.99 ± 1.33 (1-6) | 1.86 ± 1.24 | NS |
| Cyst size (cm) | 16.27 ± 7.1 (8-32) | 12.98 ± 4.9 (6-26) | 13.98 ± 5.83 | NS |
| Location | NS | |||
| Right | 9 (50.0) | 23 (56.1) | 32 (54.2) | |
| Left | 5 (27.8) | 7 (17.1) | 12 (20.4) | |
| Bilateral | 4 (22.2) | 11 (26.8) | 15 (25.4) | |
| Postoperative complication | NS | |||
| Biliary leakage | 2 (11.1) | 3 (7.3) | 5 (8.5) | |
| Atelectasis | 1 (5.5) | 1 (2.4) | 2 (3.3) | |
| Bilioma | 0 | 1 (2.4) | 1 (1.6) | |
| Pneumonia | 0 | 2 (4.8) | 2 (3.3) | |
| Wound infection | 0 | 3 (7.3) | 3 (5.0) | |
| Surgical procedures | NS | |||
| Pericystectomy | 14 (77.7) | 0 | 14 (23.7) | |
| Segmentectomy | 4 (22.3) | 0 | 4 (6.8) | |
| PC + D + Om | 0 | 36 (87.8) | 36 (61) | |
| PC + D | 0 | 5 (12.2) | 5 (8.5) | |
| Scolocidal solution | NS | |||
| Saline | 12 (66.7) | 29 (70.7) | 41 (69.5) | |
| Betadine | 6 (33.3) | 12 (29.3) | 18 (30.5) | |
| Follow-up time (mo) | 30.72 ± 17.92 | 30.29 ± 15.08 | 30.42 ± 15.71 | NS |
| Recurrence disease | 0 | 7 (17) | 7 (11.8) | 0.045 |
NS: Not significant.
Our approaches to liver hydatid cysts
As liver hydatid disease is endemic in the area where we work, a general consensus has been established for patients to be operated upon. Accordingly, the patients presenting at our clinic were categorized according to the following criteria GharbiI: all the patients in this group were referred to other hospitals as there was the possibility of percutaneous drainage. We have recently started laparoscopy drainage techniques. This group of patients was not included in this study; (2) Gharbi II, III and IV group cases with cysts sized > 10 cm were recommended for surgery; (3) Type II-IV cystic lesions in which there was compression underwent surgery regardless of size (e.g. in our cases where location was in the left lobe lateral segment and posterior to the gallbladder); (4) In the Gharbi V group, if the patient was symptomatic or if there was compression of the stomach, gallbladder or intestines, surgery was recommended (there were no such patients in this study). Otherwise type V cysts were kept under observation; and (5) Asymptomatic cysts < 5 cm were followed-up. If the size was seen to have increased, firstly albendazole treatment was administered. If the size continued to increase despite this, then surgery was planned.
Albendazole treatment
All patients with hydatid disease at our clinic were administered 10 mg/kg albendazole for 14-21 d preoperatively. During this period, liver function tests were closely observed. For all patients undergoing surgery, the same treatment protocol was recommenced on postoperative day 1 and continued for 14-21 d. If patients experienced recurrence during follow-up, again 14-21 d treatment was administered preoperatively, and the postoperative treatment period was 2 mo.
Surgical procedure
In all patients, the pericystic area and operating field were covered with sponges soaked with 20% hypertonic saline or 10% povidone-iodine (Betadine®) solution. Before injecting this solution into the cyst cavity, the cyst was punctured and as much fluid as possible was aspirated to prevent dilution of the agent. Then, 10% Betadine® or 20% hypertonic serum was instilled into the cyst cavity in a volume equal to the amount aspirated. After 15 min, the cyst fluid was aspirated again.
The surgical method was decided by collating the factors of patient age, general condition, systemic disease, American Society of Anesthesiologists (ASA) values, viral hepatitis markers, radiological images, liver function tests, blood group and the surgeon’s experience.
Radical surgery: In the pericystectomy technique, the cyst was totally removed together with 1 cm of the liver parenchyma, without opening the cavity. In a left lobe lateral segmentectomy, to secure the vasculature of the left lobe lateral segment, the segmentectomy was performed after taking the mesentery. In both situations, one or two drains were placed in the operated area.
Conservative surgery: The anterior wall of the cystic lesion was removed as widely as possible. All the components of the cyst were removed from the interior. After washing the operated area with saline or Betadine solution, one or two drains were placed. Omentopexy was not performed when cysts were located proximally but was performed when cysts were located inferior to the liver.
Postoperative follow-up
Postoperative follow-up was carried out by physical examination, IHA, USG and CT. In order for there not to be any confusion as to whether there had been any recurrence of the disease in the future, all patients underwent IHA and abdominal CT examination at the end of the first postoperative month. Thus, we obtained baseline results for future comparison. The follow-up period was completed with IHA + USG at 6 mo, IHA + CT at 1 year, IHA + USG at 18 mo, IHA + CT at 2 years, IHA + CT at 3 years, and only USG at 4 years. During this period, any cases suspected of recurrence were examined more frequently.
Statistical analysis
All data were collected and analyzed using SPSS version 11.5 (SPSS, Chicago, IL, USA). Comparison between two groups was done by independent sample Student’s t test for continuous variables and χ2 test for categoric variables. P < 0.05 was considered statistically significant.
RESULTS
All demographic and clinical characteristics, operative factors, postoperative outcomes, and surgical complications of the patients in the two groups are presented in Tables 2 and 3. Group-CS comprised 41 patients, 17 male and 24 female, with a mean age of 43.5 ± 13.9 years (range: 17-67 years). Group-RS comprised 18 patients, seven male and 11 female, with a mean age of 42.1 ± 13.5 years (range: 19-62 years). There was no significant difference in age (P > 0.703), sex (P > 0.831), residence (P > 0.416) and occupation (P > 0.853) between the two groups.
Table 3.
Comparison of both groups in terms of clinical and demographic characteristics n (%)
| Demographic features | Radical surgery | Conservative surgery | Total | P |
| Number of patient | 18 (30.5) | 41 (69.5) | 59 (100) | NS |
| Male | 7 (38.9) | 17 (41.5) | 24 (40.6) | |
| Female | 11 (61.1) | 24 (58.5) | 35 (59.4) | |
| Age (yr) | 42.1 ± 13.87 | 43.5 ± 13.9 | 43.0 ± 13.77 | NS |
| Distribution according to age | NS | |||
| < 40 | 6 (33.3) | 17 (41.46) | 23 (39.0) | |
| 40-60 | 9 (50.0) | 19 (46.34) | 28 (47.5) | |
| > 60 | 3 (16.7) | 5 (12.20) | 8 (13.5) | |
| Residence | NS | |||
| Village | 9 (50.0) | 26 (63.4) | 35 (59.3) | |
| Suburban | 7 (38.9) | 9 (22.0) | 16 (27.1) | |
| Urban | 2 (11.1) | 6 (14.6) | 8 (13.6) | |
| Occupation | NS | |||
| Housewife | 7 (38.9) | 21 (51.2) | 28 (47.5) | |
| Shepherd | 4 (22.2) | 7 (17.1) | 11 (18.6) | |
| Farmer | 4 (22.2) | 8 (19.5) | 12 (20.3) | |
| Student | 1 (5.6) | 3 (7.3) | 4 (6.8) | |
| Officer | 2 (11.1) | 2 (4.9) | 4 (6.8) | |
Surgical characteristics
In the radical surgery group, 1-4 cysts occurred in 10, five, one and two patients, respectively. The cysts were located in the right lobe in nine patients, left lobe in five, and in both lobes in four. Fourteen patients with an exophytic cyst underwent complete pericystectomy, whereas four patients with two cysts in the left lateral segment underwent left lobe lateral segmentectomy.
In the conservative surgery group, 1-6 cysts occurred in 23, eight, four, three, two and one patients, respectively. The cysts were located in the right lobe in 23 patients, left lobe in seven, and in both lobes in 11. Partial cystectomy plus external drainage plus omentopexy was performed in 36 patients, whereas five patients had partial cystectomy plus external drainage.
In four patients, intraoperative observation revealed that the cyst cavity was connected to the biliary system. In one of these four patients, the diameter of the CBD was enlarged and exploration of the CBD and T-tube drainage were performed. In three of these four patients, the open biliary duct in the cyst was closed primarily. None of these four patients had postoperative bile leakage. Mean operation time of the radical and conservative surgery group, was 83.25 ± 12.0 min and 51.97 ± 15.0 min, respectively. The mean operation time was significantly longer in the radical than conservative surgery group (P < 0.001). There was no significant difference in duration of hospitalization (P > 0.361), and in scolicidal usage (P > 0.756) between the two groups.
Early postoperative complications
The postoperative complications and the approach to these complications are summarized in Table 4. There was no significant difference in postoperative complications (P > 0.338) between the two groups. On postoperative days 2-4, five patients had drainage of 250-400 mL of bile. Since the drainage did not decrease after being monitored for 3 d, ERCP was performed and four patients underwent sphincterotomy. In the case shown in Figure 2C and D, because the open biliary duct in the cystic cavity was dilated, a sphincterotomy was performed in this patient and an internal biliary stent that reached the leaking biliary duct was placed. Seven days after drainage stopped, which was 3 mo after placement, the stent was removed. One patient had 300-350 mL of bile leakage and elevated liver function tests. In addition, the CBD was dilated on CT. This patient had a previous gastrojejunostomy, therefore, ERCP was unsuccessful and repeat surgery was performed. Exploration of the CBD and T-tube drainage were performed. The drainage stopped on postoperative day 18 and the tube was removed.
Table 4.
Postoperative complications and management
| Complications | Radical surgery | Conservative surgery | Management |
| Bilioma | 0 | 1 | Percutaneous drainage (other center) |
| Wound infection | 0 | 3 | Secondary healing therapy |
| Atelectasis | 1 | 1 | PEEP |
| Pneumonia | 0 | 2 | PEEP + antibiotherapy |
| Biliary leakage | 2 | 3 | 3 cases: ERCP + sphincterotomy |
| 1 case: ERCP + sphincterotomy + internal biliary stent | |||
| 1 case: choledoc exploration + T-tube drainage |
PEEP: Positive end-expiratory pressure.
One patient developed a postoperative biloma that was confirmed by CT. This patient underwent percutaneous drainage elsewhere. Local infection developed in three patients, who were treated appropriately. Four elderly patients developed atelectasis and pneumonia on the fourth postoperative day. These patients were treated with respiratory physiotherapy and antibiotic therapy.
Follow-up and recurrence
The follow-up duration ranged from 3 to 58 mo. Seven patients developed recurrences at 8-17 mo (mean: 13.1 mo) postoperatively. Although the recurrence rate was reduced significantly in the radical surgery group (P < 0.045), no statistically significant difference was found in terms of follow-up duration between the two groups (P > 0.429).
The preoperative IHA values were similar in all patients who had recurrences. Cystic lesions in all seven patients were confirmed using CT. Saline solution was used as the scolocidal agent in all patients who had recurrence. No recurrence was observed in patients who underwent radical surgery. Two of the seven patients refused repeat surgery, since they were asymptomatic. In the remaining five patients, the recurrent cystic lesions were treated with a partial cystectomy and drainage.
DISCUSSION
Hydatid liver disease is still endemic in certain regions of the world. The incidence of hydatid disease in Turkey ranges from 2/1 000 000 to 1/2000 in different studies[14-17]. The symptoms of hydatid liver disease generally differ according to the location, size, and grade of the cyst[18,19]. Overall, 75% of the patients are identified incidentally and are asymptomatic[4,19]. In our study, 23.7% of the patients were identified incidentally at routine examinations and 72.8% of the patients were identified after complaining of abdominal pain. All symptomatic and asymptomatic patients with cysts > 5 cm in diameter should be considered as candidates for surgery[19]. In our study, 72.8% of the patients were symptomatic, while 27.2% were asymptomatic. In all of the patients, the cysts found were ≥ 6 cm.
Which treatment modality should be used for liver hydatid cysts is still a subject of controversy. Agents which are effective on E. granulosus larvae, such as albendazole and mebendazole are used as medical therapy. It has been reported that this treatment is administered 7-21 d preoperatively and continues for 2-3 mo postoperatively[6,18,20,21].
As this treatment is given both pre- and postoperatively, the risk of postoperative secondary disease developing has been seen to be low. When we look at choice of surgical treatment used, conservative surgery is the most common, then radical surgery, and more recently, laparoscopy. Conservative surgery is recommended for the elderly, those with high ASA levels, deeply located cysts ≥ 10 cm, more than one cyst at the same time, cysts located in both lobes and in the liver posterior segment. Radical surgery can be carried out by experienced hepatobiliary surgeons on younger patients, where the cysts are located in the anterior superior liver and in the left lobe lateral segment, those with exophytic location, alveolar hydatid cyst and cysts ≥ 5 cm in diameter.
Although the rate of recurrence is lower with radical surgery, application is limited as the associated morbidity and mortality rates are high[6,18,22]. In the radical surgery cases in our study, four were in the left lobe lateral segment with straightforward localization and the other 14 were exophytic locations, therefore, there was no mortality or morbidity related to surgery. The laparoscopic approach is a treatment method developed in recent years using an umbrella trocar to perform partial or total cystectomy[23].
Topcu et al [2] have reported cysts with biliary system involvement that were > 10 cm in diameter in 22.2% of patients. In our study, the biliary system was connected to the cyst cavity in nine patients (15.2%); this was discovered intraoperatively in four patients and postoperatively in five. Six of these cysts were in the right lobe and > 15 cm in size.
Most studies assert that rupture of the cyst into the biliary system is the most important complication[2]. In our study, while exploring the CBD in a patient with a dilated CBD, a daughter vesicle was found and T-tube drainage was performed. The cysts in our study were larger than those reported in the literature, although no rupture into the biliary system was observed with these large cysts.
Ezer et al[18] found biliary leakage in 18.3% of their patients and five of the leaks closed spontaneously within 7 d. Kayaalp et al[24] found biliary leakage in 26% of their patients and seven of the leaks closed within 1 wk, while biliary fistulas occurred in five patients. In our study, biliary leakage occurred in only 8.5% of the patients and a biloma developed in one (1.6%) patient.
Recurrence is one of the major problems in the management of hepatic liver disease. Recurrent disease is defined as the appearance of new active cysts after therapy for intra- or extrahepatic disease. The failure to achieve permanent control of the primary treated cyst is considered to be the cause of local recurrence. Local recurrence occurs after surgical or radiological intervention and manifests as the reappearance of live cysts at the site of a previously treated cyst, or the appearance of new extrahepatic disease resulting from procedure-related spillage. The incidence of recurrence after liver cyst hydatid surgery is reported to range from 0% to 25% in various studies[4,18,20,25-28]. Although this rate ranges from 0% to 4.65% in patients who have had radical surgery[4,26,28], it ranges from 4.65% to 25% in those who have had conservative surgery[4,18,20,21,27,28]. In our study, recurrence occurred in none of the patients treated with radical surgery and 11.8% of those treated with conservative surgery. Recurrence may occur many years later, however, and longer follow-up is recommended when possible.
Postoperative recurrence has been reported to have developed at different periods from 4 mo to 35 years[4,18,20,26-28]. In our study, this period was found to be a mean 13.1 mo Our experience indicates that it is beneficial to have a longer follow-up period for cases of conservative surgery.
There are several studies which state that it is preferable to use a conservative approach when possible on patients who develop recurrence, because there are more problems associated with a second operation, such as mortality, damage to the gallbladder, and a lengthy postoperative stay. In our own study, five cases in which recurrence developed were treated with conservative surgery.
Several studies have been published on the use of different concentrations of scolicidal agents over different periods of time for the development of complications such as recurrence and postoperative cholangitis. The leading scolicidal agents that have been the subject of research are hypertonic saline (3%-30% and 5-30 min), povidone-iodine (10%), formalin, cetrimide (0.1%-0.4%), chlorhexidine (0.04%-4%), hydrogen peroxide (3%) and ethyl alcohol (95%).
Hypertonic saline solution and Betadine are the most frequently used scolicidal agents in Turkey[2,29,30]. Besim et al[29] have compared the effects of different scolicidal agents at different concentrations and found that the use of Betadine, 20% saline, 3% hydrogen peroxide, 95% ethyl alcohol, and 10% Savlon solutions for 15 min inactivated the protoscoleces. The infectivity was higher using concentrations of < 20% and for < 5 min. Sclerosing cholangitis has been reported with the use of 20% and 30% hypertonic saline solutions[30-32]. In our study, we used either 20% saline or 10% Betadine solution in the cystic cavity for 15 min. None of our cases developed any metabolic problem or sclerosing cholangitis.
In conclusion, the most effective method for preventing postoperative recurrences is radical surgery. This is indicated for patients meeting the indications in terms of age, medical history, location and size of the cyst, and relation of the cyst to the vasculature and biliary tree. When ≥ 250 mL of biliary leakage occurs in the early postoperative period, performing sphincterotomy with ERCP or a stent within 3-5 d allows early discharge from hospital, decreases the need for repeat surgery, and reduces the costs and psychosocial problems that may occur with prolonged follow-up.
COMMENTS
Background
The development of hydatid disease associated with Echinococcus granulosus is still an important health problem. Treatment choices are medical, conservative surgery, radical surgery, laparoscopic surgery and PAIR technique. The advantages and disadvantages of these techniques have not as yet been fully clarified.
Research frontiers
In this study, although the patients who had undergone radical surgery did not experience any recurrence of the disease during postoperative follow-up, the operating time was significantly shorter for conservative surgery.
Peer review
The overall impression of the article is positive and it might be relevant for publication in World Journal of Gastroenterology as it deals with an important and relatively rare disease, which has no clear and unequivocal management guidelines.
Footnotes
Peer reviewers: Hussein M Atta, MD, PhD, Department of Surgery, Faculty of Medicine, Minia University, Mir-Aswan Road, El-Minia 61519, Egypt; Giedrius Barauskas, Professor, Department of Surgery, Kaunas University of Medicine, Eiveniu str. 2, Kaunas, LT-50009, Lithuania; Dr. Cuneyt Kayaalp, MD, Professor, Department of General Surgery, Staff Surgeon of Gastrointestinal Surgery, Turgut Ozal Medical Center, Inonu University, Malatya 44315, Turkey
S- Editor Tian L L- Editor Kerr C E- Editor Zheng XM
References
- 1.Jenkins DJ, Romig T, Thompson RC. Emergence/re-emergence of Echinococcus spp.--a global update. Int J Parasitol. 2005;35:1205–1219. doi: 10.1016/j.ijpara.2005.07.014. [DOI] [PubMed] [Google Scholar]
- 2.Topcu O, Sumer Z, Tuncer E, Aydin C, Koyuncu A. Efficacy of chlorhexidine gluconate during surgery for hydatid cyst. World J Surg. 2009;33:1274–1280. doi: 10.1007/s00268-009-9971-z. [DOI] [PubMed] [Google Scholar]
- 3.Hakverdi S, Sayar H, Yaldiz M, Erdoğan S, Akansu B, Canda MS. [Unusual localization of echinococcosis in cukurova (134 case)] Turkiye Parazitol Derg. 2009;33:77–81. [PubMed] [Google Scholar]
- 4.Xiao N, Qiu J, Nakao M, Li T, Yang W, Chen X, Schantz PM, Craig PS, Ito A. Echinococcus shiquicus, a new species from the Qinghai-Tibet plateau region of China: discovery and epidemiological implications. Parasitol Int. 2006;55 Suppl:S233–S236. doi: 10.1016/j.parint.2005.11.035. [DOI] [PubMed] [Google Scholar]
- 5.Harris KM, Morris DL, Tudor R, Toghill P, Hardcastle JD. Clinical and radiographic features of simple and hydatid cysts of the liver. Br J Surg. 1986;73:835–838. doi: 10.1002/bjs.1800731025. [DOI] [PubMed] [Google Scholar]
- 6.Aydin U, Yazici P, Onen Z, Ozsoy M, Zeytunlu M, Kiliç M, Coker A. The optimal treatment of hydatid cyst of the liver: radical surgery with a significant reduced risk of recurrence. Turk J Gastroenterol. 2008;19:33–39. [PubMed] [Google Scholar]
- 7.Moro P, Schantz PM. Echinococcosis: a review. Int J Infect Dis. 2009;13:125–133. doi: 10.1016/j.ijid.2008.03.037. [DOI] [PubMed] [Google Scholar]
- 8.Aeberhard P, Fuhrimann R, Strahm P, Thommen A. Surgical treatment of hydatid disease of the liver: an experience from outside the endemic area. Hepatogastroenterology. 1996;43:627–636. [PubMed] [Google Scholar]
- 9.Alfieri S, Doglietto GB, Pacelli F, Costamagna G, Carriero C, Mutignani M, Liberatori M, Crucitti F. Radical surgery for liver hydatid disease: a study of 89 consecutive patients. Hepatogastroenterology. 1997;44:496–500. [PubMed] [Google Scholar]
- 10.Uravic M, Stimac D, Lenac T, Ivanis N, Petrosic N, Rubinic M, Skarpa A. Diagnosis and treatment of liver hydatid disease. Hepatogastroenterology. 1998;45:2265–2269. [PubMed] [Google Scholar]
- 11.Men S, Hekimoğlu B, Yücesoy C, Arda IS, Baran I. Percutaneous treatment of hepatic hydatid cysts: an alternative to surgery. AJR Am J Roentgenol. 1999;172:83–89. doi: 10.2214/ajr.172.1.9888745. [DOI] [PubMed] [Google Scholar]
- 12.Ustünsöz B, Akhan O, Kamiloğlu MA, Somuncu I, Uğurel MS, Cetiner S. Percutaneous treatment of hydatid cysts of the liver: long-term results. AJR Am J Roentgenol. 1999;172:91–96. doi: 10.2214/ajr.172.1.9888746. [DOI] [PubMed] [Google Scholar]
- 13.Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic liver. Radiology. 1981;139:459–463. doi: 10.1148/radiology.139.2.7220891. [DOI] [PubMed] [Google Scholar]
- 14.De Werra C, Condurro S, Tramontano S, Perone M, Donzelli I, Di Lauro S, Di Giuseppe M, Di Micco R, Pascariello A, Pastore A, et al. Hydatid disease of the liver: thirty years of surgical experience. Chir Ital. 2007;59:611–625. [PubMed] [Google Scholar]
- 15.Cobanoğlu U. [Postoperative hypernatremia in liver hydatid disease: a case report] Turkiye Parazitol Derg. 2008;32:167–170. [PubMed] [Google Scholar]
- 16.Altintas N. Past to present: echinococcosis in Turkey. Acta Trop. 2003;85:105–112. doi: 10.1016/s0001-706x(02)00213-9. [DOI] [PubMed] [Google Scholar]
- 17.Yazar S. [Cystic echinococcosis in Kayseri during the last six years.] Turkiye Parazitol Derg. 2005;29:241–243. [PubMed] [Google Scholar]
- 18.Ezer A, Nursal TZ, Moray G, Yildirim S, Karakayali F, Noyan T, Haberal M. Surgical treatment of liver hydatid cysts. HPB (Oxford) 2006;8:38–42. doi: 10.1080/13651820500468000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tolga Muftuoglu MA, Koksal N, Topaloglu U. The role of omentoplasty in the surgical management of remnant cavity in hepatic hydatid cyst. HPB (Oxford) 2005;7:231–234. doi: 10.1080/13651820410022889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prousalidis J, Kosmidis C, Anthimidis G, Fachantidis E, Harlaftis N, Aletras H. Forty-four years' experience (1963-2006) in the management of primarily infected hydatid cyst of the liver. HPB (Oxford) 2008;10:18–24. doi: 10.1080/13651820701854669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prousalidis J, Kosmidis Ch, Fahantidis E, Harlaftis N, Aletras O. Surgical treatment of multiple cystic echinococcosis. HPB (Oxford) 2004;6:110–114. doi: 10.1080/16515320410026068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Secchi MA, Pettinari R, Mercapide C, Bracco R, Castilla C, Cassone E, Sisco P, Andriani O, Rossi L, Grondona J, et al. Surgical management of liver hydatidosis: a multicentre series of 1412 patients. Liver Int. 2010;30:85–93. doi: 10.1111/j.1478-3231.2009.02116.x. [DOI] [PubMed] [Google Scholar]
- 23.Seven R, Berber E, Mercan S, Eminoglu L, Budak D. Laparoscopic treatment of hepatic hydatid cysts. Surgery. 2000;128:36–40. doi: 10.1067/msy.2000.107062. [DOI] [PubMed] [Google Scholar]
- 24.Kayaalp C, Bzeizi K, Demirbag AE, Akoglu M. Biliary complications after hydatid liver surgery: incidence and risk factors. J Gastrointest Surg. 2002;6:706–712. doi: 10.1016/s1091-255x(02)00046-x. [DOI] [PubMed] [Google Scholar]
- 25.Dawson JL, Stamatakis JD, Stringer MD, Williams R. Surgical treatment of hepatic hydatid disease. Br J Surg. 1988;75:946–950. doi: 10.1002/bjs.1800751004. [DOI] [PubMed] [Google Scholar]
- 26.Chautems R, Buhler L, Gold B, Chilcott M, Morel P, Mentha G. Long term results after complete or incomplete surgical resection of liver hydatid disease. Swiss Med Wkly. 2003;133:258–262. doi: 10.4414/smw.2003.10168. [DOI] [PubMed] [Google Scholar]
- 27.Stoot JH, Jongsma CK, Limantoro I, Terpstra OT, Breslau PJ. More than 25 years of surgical treatment of hydatid cysts in a nonendemic area using the "frozen seal" method. World J Surg. 2010;34:106–113. doi: 10.1007/s00268-009-0267-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kapan M, Kapan S, Goksoy E, Perek S, Kol E. Postoperative recurrence in hepatic hydatid disease. J Gastrointest Surg. 2006;10:734–739. doi: 10.1016/j.gassur.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 29.Besim H, Karayalçin K, Hamamci O, Güngör C, Korkmaz A. Scolicidal agents in hydatid cyst surgery. HPB Surg. 1998;10:347–351. doi: 10.1155/1998/78170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kayaalp C, Balkan M, Aydin C, Ozgurtas T, Tanyuksel M, Kirimlioglu V, Akoglu M, Oner K, Pekcan M. Hypertonic saline in hydatid disease. World J Surg. 2001;25:975–979. doi: 10.1007/s00268-001-0065-9. [DOI] [PubMed] [Google Scholar]
- 31.Castellano G, Moreno-Sanchez D, Gutierrez J, Moreno-Gonzalez E, Colina F, Solis-Herruzo JA. Caustic sclerosing cholangitis. Report of four cases and a cumulative review of the literature. Hepatogastroenterology. 1994;41:458–470. [PubMed] [Google Scholar]
- 32.Stoianov G, Genchev G, Dimitrov A. [Secondary sclerosing cholangitis after echinococcectomy] Khirurgiia (Sofiia) 1998;51:40–41. [PubMed] [Google Scholar]