Abstract
OBJECTIVE
Relatives of type 1 diabetic patients are at enhanced risk of developing diabetes. We investigated the mode of onset of hyperglycemia and how insulin sensitivity and β-cell function contribute to the progression to the disease.
RESEARCH DESIGN AND METHODS
In 328 islet cell autoantibody–positive, nondiabetic relatives from the observational arms of the Diabetes Prevention Trial-1 Study (median age 11 years [interquartile range 8], sequential OGTTs (2,143 in total) were performed at baseline, every 6 months, and 2.7 years [2.7] later, when 115 subjects became diabetic. β-Cell glucose sensitivity (slope of the insulin-secretion/plasma glucose dose-response function) and insulin sensitivity were obtained by mathematical modeling of the OGTT glucose/C-peptide responses.
RESULTS
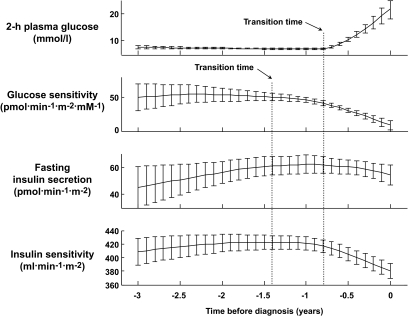
In progressors, baseline insulin sensitivity, fasting insulin secretion, and total postglucose insulin output were similar to those of nonprogressors, whereas β-cell glucose sensitivity was impaired (median 48 pmol/min per m2 per mmol/l [interquartile range 36] vs. 87 pmol/min per m2 per mmol/l [67]; P < 0.0001) and predicted incident diabetes (P < 0.0001) independently of sex, age, BMI, and clinical risk. In progressors, 2-h glucose levels changed little until 0.78 years before diagnosis, when they started to rise rapidly (∼13 mmol · l−1 · year−1); glucose sensitivity began to decline significantly (P < 0.0001) earlier (1.45 years before diagnosis) than the plasma glucose surge. During this anticipation phase, both insulin secretion and insulin sensitivity were essentially stable.
CONCLUSIONS
In high-risk relatives, β-cell glucose sensitivity is impaired and is a strong predictor of diabetes progression. The time trajectories of plasma glucose are frequently biphasic, with a slow linear increase followed by a rapid surge, and are anticipated by a further deterioration of β-cell glucose sensitivity.
The onset of type 1 diabetes typically is acute. The immune-mediated destruction of pancreatic β-cells, however, is known to occur over years (1,2). During this prodromic phase, several classes of autoantibodies can be detected in the serum of many, though not all, subjects progressing to diabetes (3–5). Number and titer of such autoantibodies mark the risk of disease, particularly in genetically predisposed individuals (6), but do not tell when hyperglycemia will emerge (7). What precipitates β-cell failure remains unknown. A reduced acute insulin response to an intravenous glucose challenge is thought to reflect reduction of β-cells below a critical mass or function and is used as a metabolic marker of future diabetes (8,9), but the natural history of β-cell incompetence has not clearly been defined. Furthermore, the contribution of insulin resistance to metabolic decompensation is controversial. Thus, in the Seattle Family Study, insulin sensitivity (as the SI from an intravenous glucose challenge) did not distinguish between progressors and nonprogressors (10); likewise, insulin resistance (as the homeostasis model assessment of insulin resistance index) did not affect progression when insulin secretion was relatively well preserved in the ENDIT study (11). In contrast, in the Melbourne Pre-diabetes Family study, Fourlanos et al. (12) found that insulin resistance (as the homeostasis model assessment of insulin resistance factored by acute insulin response) was a significant predictor of incident type 1 diabetes over a 4-year follow up. In any event, the interactions between insulin release, β-cell dysfunction, and insulin resistance have not been dissected out.
The Diabetes Prevention Trial–Type 1 (DPT-1) recruited a large number of autoantibody-positive relatives of probands with type 1 diabetes who were at risk of disease because of multiple autoantibody positivity or reduced acute insulin response to intravenous glucose (13). Oral glucose tolerance was tested at frequent intervals over the course of several years until appearance of diabetes or study end (14). Measurement of the C-peptide response to oral glucose makes it possible to quantify β-cell function and estimate insulin sensitivity (15). The DPT-1 cohort was therefore uniquely suited to investigate mechanisms and mode of onset of type 1 diabetes.
RESEARCH DESIGN AND METHODS
The DPT-1 screened 103,391 relatives of individuals with type 1 diabetes who had been diagnosed before age 45 years. To have been eligible for screening, an individual must have been a first-degree relative of a patient with type 1 diabetes aged between 3 and 45 years or a second-degree relative aged between 3 and 20 years. The 3,483 relatives who were found to be islet cell –antibody (ICA) positive were staged to quantify the projected 5-year risk of diabetes (13). Staging consisted of ICA confirmation, HLA-DQ typing, determination of insulin autoantibodies, and oral (OGTT) and intravenous glucose tolerance testing. Relatives with HLA-DQA 1*0102/DQB1*0602 were excluded (16). Those considered to be at a >50% 5-year risk were eligible for entry into the parenteral insulin trial if either the first-phase insulin response to intravenous glucose was below the 1st–10th percentile (depending on age and relation to the proband) on two occasions or there were abnormalities (other than diabetes) on the OGTT (17). If none of these metabolic abnormalities were present, first-phase insulin response was above threshold (≥10th percentile for siblings, offspring, and second-degree relatives and ≥1st percentile for parents), insulin autoantibodies were positive, and the 5-year risk was 25–50%, participants were entered for the oral insulin trial (18). Subjects were randomly assigned to receive insulin intervention or matched placebo/observation, respectively. Neither intervention showed a statistically significant difference between the treatment arms in terms of progression to diabetes (17,18). We report here on the 180 participants in the oral insulin trial (moderate-risk group) and the 148 subjects in the parenteral trial (high-risk group) who were randomized to the placebo/observation arms of the study.
Study protocol.
At baseline and follow up, the OGTT was performed using a dose of glucose of 1.75 g/kg body wt (maximum 75 g). After an overnight fast, blood samples were obtained through indwelling catheters for plasma glucose and serum C-peptide measurements in the fasting state and 30, 60, 90, and 120 min later.
Follow-up.
After the baseline study, subjects received an OGTT every 6 months until development of diabetes (median 2.2 years) or study end (median 3.2 years). A total of 2,143 OGTTs were available for analysis.
Diagnosis of diabetes.
Diabetes was diagnosed if the fasting glucose was ≥7.0 mmol/l or the 2-h glucose was ≥11.1 mmol/l, with confirmation by either an elevated fasting or 2-h glucose level at a special follow-up visit or a random plasma glucose ≥11.1 mmol/l accompanied by symptoms of polyuria, polydipsia, or weight loss. Impaired glucose tolerance (IGT) was defined as a fasting glucose <7.0 mmol/l and a 2-h glucose between 7.8 and 11.1 mmol/l (19).
Analytical measurements.
Plasma glucose was measured by the glucose oxidase method. Serum C-peptide was determined by radioimmunoassay as previously described (20), with an interassay coefficient of variation of 6.9% in a reference pool with relatively high values and 7.8% in a reference pool with relatively low values.
Data analysis.
Modeling methods are described in detail in an online appendix, available at http://diabetes.diabetesjournals.org/cgi/content/full/db09-1378/DC1. In brief, β-cell function parameters were obtained from the OGTT using a model (21) that describes the relationship between insulin secretion and glucose concentration. Characteristic β-cell function parameters reported here are fasting insulin secretion rate (in picomoles per min per square meter of body surface area); insulin output, i.e., the integral of insulin secretion during the 2-h OGTT; and β-cell glucose sensitivity, i.e., the mean slope of the dose response relating insulin secretion to glucose concentration within the observed glucose range. As defined and used here, in vivo β-cell glucose sensitivity quantifies an overall relationship and does reflect specifically the cellular processes governing glucose sensing (glucose transport through GLUT2, phosphorylation by glucokinase, etc.). Insulin sensitivity was calculated using the oral glucose–derived insulin sensitivity index (OGIS) (22), which provides a validated estimate of the glucose clearance (in milliliters per min per square meter of body surface area) during the insulin-stimulated conditions of the euglycemic-hyperglycemic clamp. The time trajectories of glucose concentration and the model-derived parameters were analyzed using a function of time capable of representing a biphasic pattern, with an initial phase in which the variable changes slowly with time and a late phase in which the change is accelerated.
Statistical analysis.
All data are presented as median [interquartile range]. Group comparisons were performed using the Mann-Whitney U or Wilcoxon signed-rank test (for unpaired and paired observations, respectively) and the χ2 test for categorical variables. Kaplan-Meier plots were used to compare diabetes-free survival curves by means of the log-rank χ2 statistic. Cox proportional hazards models were used to estimate hazard ratios (HRs) (95% CI). The proportional hazards assumption was confirmed by examining the log cumulative survival plots. P values are two sided, and P < 0.05 was accepted as statistically significant. All analyses were performed using JMP, version 3.1 (SAS Institute, Cary, NC).
RESULTS
Baseline.
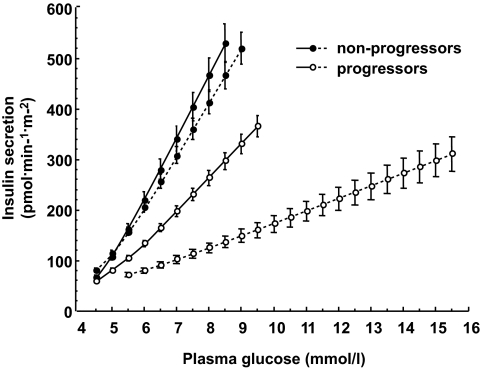
Subjects who progressed to diabetes (progressors) were younger and leaner than those who remained diabetes free over the follow-up period and were more often IGT than nonprogressors, as manifested by their higher 2-h plasma glucose levels (Table 1). The insulin secretion/plasma glucose dose-response curve was considerably flatter in progressors than in nonprogressors. Its descriptive parameter, the slope or β-cell glucose sensitivity, was 45% lower in progressors, whereas fasting insulin secretion rate, total insulin output, and insulin sensitivity were similar in the two groups. After excluding subjects with IGT (30 progressors and 18 nonprogressors), glucose sensitivity was still significantly impaired in subjects converting to diabetes (median 54 pmol/min per m2 per mmol/l [interquartile range 38] vs. 90 pmol/min per m2 per mmol/l [73] of nonprogressors; P < 0.0001) (Fig. 1).
TABLE 1.
Anthropometric and metabolic parameters at baseline
| Nonprogressors | Progressors | P* | |
|---|---|---|---|
| n | 213 | 115 | |
| Sex (male/female) | 118/95 | 57/58 | ns |
| Age (years) | 11.7 (8.8) | 9.7 (5.4) | 0.0006 |
| Height (m) | 1.49 (0.41) | 1.41 (0.32) | 0.015 |
| Weight (kg) | 41 (38) | 35 (26) | 0.02 |
| BMI (kg/m2) | 18.7 (6.6) | 18.0 (5.7) | ns |
| Fasting glucose (mmol/l) | 4.77 (0.55) | 4.83 (0.74) | ns |
| 2-h glucose (mmol/l) | 5.94 (1.78) | 6.83 (1.88) | <0.0001 |
| NGT/IGT (%) | 92/8 | 74/26 | <0.0001 |
| Fasting insulin secretion (pmol/min per m2) | 52 (36) | 48 (36) | ns |
| Insulin output (nmol/m2) | 28 (15) | 26 (13) | ns |
| Glucose sensitivity (pmol/min per m2 per mmol/l) | 87 (67) | 48 (36) | <0.0001 |
| Insulin sensitivity (ml/min per m2) | 434 (76) | 432 (76) | ns |
Data are median (interquartile range) or n unless otherwise indicated.
*Progressors vs. nonprogressors. ns, not significant.
FIG. 1.
Dose-response curve of insulin secretion rates vs. plasma glucose levels during the OGTT in 280 subjects with normal glucose tolerance according to whether (progressors) or not (nonprogressors) they developed diabetes. Data are means ± SEM. The mean slope of the dose response is β-cell glucose sensitivity. Full lines, baseline data; dotted lines, data at follow-up.
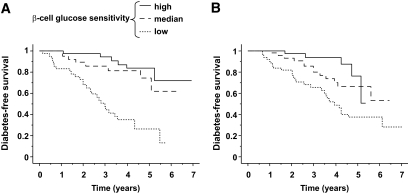
In female subjects, younger age and higher BMI were positive predictors of incident diabetes, whereas a good β-cell glucose sensitivity was a strong protective factor. In male subjects, only a younger age was a risk factor, while both β-cell glucose sensitivity and insulin sensitivity were protective (Table 2). Of note is that a high a priori risk (assessed at staging as a composite of relation to proband and reduced acute insulin response to intravenous glucose) was a significant predictor of conversion to diabetes only in female subjects and did not replace either glucose sensitivity or insulin sensitivity. With regard to plasma glucose levels themselves, in univariate analysis 2-h glucose levels predicted incident diabetes, with HRs (1.81 [95% CI 1.37–2.40], χ2 = 16 in male subjects and 2.35 [1.72–3.21], χ2 = 29 in female subjects) that were lower than the univariate HRs carried by β-cell glucose sensitivity (0.32 [0.17–0.56], χ2 = 20 in male subjects and 0.24 [0.14–0.38], χ2 = 46 in female subjects). Thus, in the multivariate models of Table 2, neither fasting nor 2-h glucose was a significant independent predictor in male subjects and only 2-h glucose was an additional predictor in female subjects (P = 0.03). Even in subjects with normal glucose tolerance (n = 280), diabetes-free survival was strongly dependent on baseline β-cell glucose sensitivity in both sexes (Fig. 2).
TABLE 2.
Predictors of incident type 1 diabetes
| Risk ratio (95% CI) | P | |
|---|---|---|
| Female subjects (n = 153) | ||
| Risk at staging (high vs. moderate) | 1.75 (1.25–2.48) | 0.001 |
| Age | 0.30 (0.17–0.50) | <0.0001 |
| BMI | 2.25 (1.31–3.79) | 0.003 |
| β-Cell glucose sensitivity | 0.29 (0.17–0.47) | <0.0001 |
| Insulin sensitivity | 0.76 (0.53–1.09) | 0.133 |
| Male subjects (n = 175) | ||
| Risk at staging (high vs. moderate) | 1.12 (0.83–1.52) | 0.465 |
| Age | 0.55 (0.35–0.81) | 0.002 |
| BMI | 1.27 (0.72–2.13) | 0.403 |
| β-Cell glucose sensitivity | 0.29 (0.15–0.53) | <0.0001 |
| Insulin sensitivity | 0.46 (0.29–0.73) | 0.001 |
Multivariate analysis; risk ratios for age, BMI, β-cell glucose sensitivity, and insulin sensitivity were calculated for the sex-specific interquartile range of their respective values.
FIG. 2.
Kaplan-Meier plots of diabetes-free survival in 280 subjects with normal glucose tolerance at baseline according to tertile of baseline β-cell glucose sensitivity (log-rank χ2 = 25.5, P < 0.0001, and 13.2, P = 0.0003, in female [A] and male [B] subjects, respectively). The risk ratio of subjects in the bottom tertile of β-cell glucose sensitivity (dotted line) is 2.40 (95% CI 1.76–3.30), P < 0.0001 vs. the top tertile, adjusted for sex, age, and BMI.
Follow-up.
Fasting and 2-h plasma glucose concentrations had risen slightly in nonprogressors, who now counted as 41 subjects in the IGT category. Both fasting insulin secretion rate and insulin output were higher than at baseline, whereas insulin sensitivity and β-cell glucose sensitivity were slightly but significantly worse. In progressors, the marked rise in fasting and 2-h plasma glucose levels was accompanied by a fall in insulin output and insulin sensitivity and a further, drastic decline in glucose sensitivity (Table 3).
TABLE 3.
Anthropometric and metabolic parameters at follow-up
| Nonprogressors (n = 213) | Progressors (n = 115) | P§ | |
|---|---|---|---|
| Follow-up (years) | 3.2 (2.8) | 2.2 (3.3) | <0.0001 |
| Age (years) | 14.7 (9.6)* | 12.0 (5.7)* | <0.0001 |
| Height (m) | 1.63 (0.25)* | 1.52 (0.30)* | 0.0007 |
| Weight (kg) | 57 (33)* | 47 (31)* | 0.0035 |
| BMI (kg/m2) | 21.1 (6.0)* | 19.6 (6.1)* | <0.05 |
| Fasting glucose (mmol/l) | 4.89 (0.65)* | 5.75 (1.22)* | <0.0001 |
| 2-h glucose (mmol/l) | 6.27 (2.25)* | 13.05 (6.52)* | <0.0001 |
| Glucose tolerance (NGT/IGT) (%) | 81/19* | — | <0.0001 |
| Fasting insulin secretion (pmol/min per m2) | 65 (33)* | 65 (44)* | ns |
| Insulin output (nmol/m2) | 31 (14)* | 21 (15)* | <0.0001 |
| Glucose sensitivity (pmol/min per m2 per mmol/l) | 72 (57)* | 17 (19)* | <0.0001 |
| Insulin sensitivity (ml/min per m2) | 411 (76)* | 380 (77)* | <0.0001 |
Data are median (interquartile range) or n unless otherwise indicated.
§Progressors vs. nonprogressors.
*P < 0.01 vs. baseline. ns, not significant.
Time trajectories.
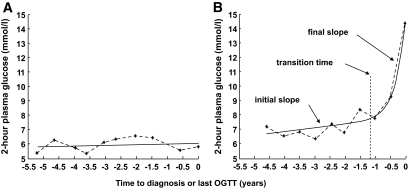
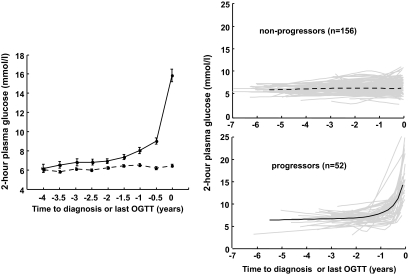
In the subjects with four or more sequential OGTTs (n = 208), the individual time series could generally be described as approximately linear with time (i.e., a monophasic time course) or as biphasic (i.e., displaying a definite change in slope at an identifiable transition time) (Fig. 3). For the 2-h plasma glucose concentrations, both the raw values and their fitting functions revealed a predominantly biphasic pattern in progressors (n = 52) and a mostly monophasic one among nonprogressors (n = 156) (Fig. 4). The statistical analysis of all the OGTT-derived parameters is given in supplemental Table A1. For 2-h glucose concentrations, glucose sensitivity, and insulin sensitivity, the average time course was significantly better described by a biphasic than a monophasic fit in progressors compared with nonprogressors. Accordingly, the initial and final slopes of the respective time series were not different from one another in nonprogressors, whereas the final slopes were much steeper than the initial slopes in the progressors. This difference in time course was not found for fasting insulin secretion rate.
FIG. 3.
Example of a monophasic (A) (subject YW3599) and a biphasic (B) (subject HR2920) time course of 2-h plasma glucose concentrations; note the change in slope at transition time in the biphasic time pattern.
FIG. 4.
Half-yearly averages of 2-h plasma glucose concentrations (left panel) and individual fits of their time series (right panel) in nonprogressors and progressors. The thick lines are the mean of the individual fitting functions.
Among progressors, 36 subjects (or 70%) had a biphasic time course for 2-h glucose levels (on a median of 6 [interquartile range 2] tests), while for glucose sensitivity a similar pattern was present in 30 subjects. In these individuals, the transition time for 2-h glucose was positively correlated with the transition time for glucose sensitivity (ρ = 0.43; P = 0.020). In addition, the transition to an increased rate of decrease in glucose sensitivity occurred earlier than the corresponding 2-h glucose transition (−1.3 [1.2] vs. −0.77 [1.0] years; P = 0.035) (Fig. 5). When 2-h glucose levels were synchronized on the individual transition times, it became clear that plasma glucose levels changed little until 0.78 years before diagnosis, when they started to rise at a rate of ∼13 mmol/l per year. When the time series of the metabolic parameters were synchronized with the glucose time series, it was found that glucose sensitivity had begun to decline (at a rate of 29 pmol/min per m2 per mmol/l) 1.45 years before diagnosis, i.e., significantly (P < 0.0001) earlier than the plasma glucose surge. During this anticipation phase–lasting a median 4.3 months–both insulin secretion and insulin sensitivity were essentially stable. In progressors (n = 30) with an unequivocally biphasic time course of 2-h glucose concentrations, the transition times of β-cell glucose sensitivity were positively associated with the transition times of 2-h plasma glucose concentration (supplemental Fig. A1).
FIG. 5.
Time course of 2-h plasma glucose concentrations, glucose sensitivity, fasting insulin secretion, and insulin sensitivity in the progressor group. Time series are synchronized on the transition time of 2-h plasma glucose levels.
DISCUSSION
By selection, our subjects were at enhanced risk of progressing to diabetes by genetic makeup (kinship and lack of protective genotype) as well as clinical phenotype (presence of ICA and insulin autoantibodies or reduced acute insulin response to intravenous glucose). Accordingly, 35% developed diabetes over the follow-up period, a crude rate of ∼13% per year (in the range of that of similar cohorts [23,24]). The most striking findings relate to β-cell function. At baseline, insulin secretion rates and insulin sensitivity were no different between progressors and nonprogressors while β-cell glucose sensitivity was markedly impaired (by ∼45%). This was true also when comparing only NGT subjects (Fig. 1), and was only reflected in a 0.78 mmol/l difference in 2-h glucose concentrations while fasting glucose was virtually identical (median 4.83 mmol/l [interquartile range 0.72] vs. 4.80 mmol/l [0.63]). Over time, some deterioration of all metabolic parameters was seen in the whole cohort; emergence of overt diabetes, however, was marked by a further, drastic (70%) decline in β-cell glucose sensitivity (Table 2). Consistent with these time-related changes are the predictive models of incident diabetes: younger age and worse β-cell glucose sensitivity were the strongest independent predictors of progression in both sexes, with BMI (in female subjects) and insulin resistance (in male subjects) as additional risk factors (Table 2).
These findings have pathophysiological implications. First, absolute rates of insulin secretion (or plasma insulin concentrations) do not track a failing β-cell function. In fact, fasting insulin secretion increased over time in progressors and nonprogressors alike, while even in progressors insulin output was diminished by only 20% at the time of diagnosis (Table 2). The time course of insulin secretion rates in progressors (Fig. 5) is reminiscent of the inverted-U shape of plasma insulin concentrations in individuals progressing to type 2 diabetes (25), which is also termed the Starling curve of the pancreas (26). On the other hand, β-cell glucose sensitivity was specifically associated with glucose tolerance across groups and over time, was the strongest predictor of the diabetes outcome, and declined as a monotonical function of time in progressors (Fig. 5). Thus, absolute insulin secretion rates can be viewed as reflecting the secretory tone of the β-cell, which adapts to chronically raised glucose levels by upregulating release of the hormone. Glucose sensitivity, in contrast, expresses the ability of the β-cell to quickly respond to acute changes in plasma glucose levels in vivo, thereby directly controlling glucose tolerance. It is this latter function that we found to be compromised long (years) before the onset of type 1 diabetes. At this time, there was little in the clinical and metabolic phenotype—other than a younger age (−2 years) and a 15% increase in 2-h glucose concentrations— that differentiated subjects who were to become diabetic from those who remained nondiabetic over the observation period. Thus, in vivo β-cell glucose insensitivity is an early defect in type 1 diabetes.
The question stands whether the whole DPT-1 cohort—and not just the subjects who progressed within ∼3 years—was one characterized by a defect in β-cell glucose sensitivity. The present study did not include a control group matched to the DPT-1 participants. However, from data collected in the RISC study (27) we selected 90 young (median age 32 years [interquartile range 3]), lean (BMI 22.6 kg/m2 [4.2]) volunteers with a negative family history of diabetes in whom β-cell function and insulin sensitivity were assessed with the same methodology as used in the present study. In these historical controls, median β-cell glucose sensitivity was 138 pmol/min per m2 per mmol/l (interquartile range 72) and insulin sensitivity was 460 ml/min per m2 (69). Thus, this comparison suggests that both β-cell glucose sensitivity and insulin sensitivity may have been less than normal even in the nonprogressors of DPT-1 at the time of staging. Whether the DPT-1 population had entirely normal metabolic functions prior to the autoimmune attack on the β-cell is not known.
Secondly, the tight association between β-cell glucose insensitivity and glucose tolerance does not per se establish a cause-effect link: a primary β-cell defect can clearly cause loss of glucose tolerance but might also result from toxic effects of mild but persistent hyperglycemia on β-cells. It should be stressed that the primary β-cell defect could consist in a reduction in number of normally functioning β-cells, a dysfunction of a normal number of β-cells, or a combination of the two. In vivo assessment of β-cell glucose sensitivity does not allow for distinction between these underlying defects. Glucose toxicity, on the other hand, can acutely depress both the insulin secretory response to glucose (28) and insulin sensitivity (29).
The time series analysis of our data shows that in two-thirds of the progressors, the trajectory of plasma glucose concentrations was distinctly biphasic, with a slow rise turning into a brisk surge ∼0.7 years before diagnosis (research design and methods). In these individuals, a transition of β-cell glucose sensitivity from a flat time course to a clear decline occurred ∼1.4 years prior to diagnosis and consistently anticipated the transition of glucose levels (Fig. 5). In other words, the trajectories of plasma glucose and β-cell function were shifted with respect to one another by 6–8 months, during which time neither absolute insulin secretion nor insulin sensitivity was changing appreciably. These findings provide strong support for the conclusion that a loss of β-cell glucose sensitivity effectively is a potent drive for the acceleration of hyperglycemia in high-risk subjects rapidly progressing to diabetes. Of note is that recent work carried out in nondiabetic patients undergoing pancreatectomy (30) has revealed a curvilinear reciprocal association between 2-h plasma glucose concentration and β-cell relative volume, suggesting that β-cell function/mass may decrease initially without much impact on glucose levels but then—beyond a certain critical level—cause an exponential rise in glycemia.
Finally, the characteristic biphasic time pattern of conversion in DPT-1 screenees is consistent with a previous preliminary finding from DPT-1 (15) and is reminiscent of what happens in type 2 diabetes. In three prospective analyses of incident type 2 diabetes (31–33), an acceleration of plasma glucose increments preceded the emergence of clinical diabetes by 3–6 years. The similarity is striking: a few years (type 2 diabetes [31–33]) or months (type 1 diabetes [present study]) before diagnosis, glucose tolerance characteristically begins to deteriorate at a much faster rate than during the preceding years. The fact that the pathogenesis and natural history of the two forms of diabetes are distinct suggests that a more general factor may be at play. Glucose homeostasis relies on multiple controls: to name only the main ones, insulin sensitivity of liver, fat, and skeletal muscle tissues as well as β-cell and α-cell function. In the individual who is destined to become diabetic—whether type 2 or type 1 diabetes—several of the factors that govern glucose tolerance are more or less altered, generating a critical state of instability. In such a condition, phase transition can be triggered by small further changes in the controlling variables and occurs relatively rapidly. For type 1 diabetes (34), this instability paradigm—borrowed from physics (35)—has been formulated mathematically by rate equations describing the changes in numbers of β-cells, macrophages, and Th-lymphocytes eventually leading to self-sustained β-cell elimination. The conclusion of this theoretical study was that onset of type 1 diabetes is due to a collective, dynamical instability rather than being caused by a single etiological factor (34). Our results support this paradigm. In progressors, transition to the phase of rapid plasma glucose increases was characterized by a precipitous fall in insulin sensitivity plus an acceleration of glucose insensitivity; in the meantime, insulin secretion was failing to keep up with the rising glucose (Fig. 5). Thus, a state of critical instability transitioned to a phase of impending global failure. Different time patterns, linear or erratic, could be equally explained by different combinations of rates of failure of the determinants of glucose tolerance. In summary, a defect in β-cell glucose sensitivity is detectable in at-risk subjects years before diagnosis, anticipates plasma glucose increments, and in combination with progressive insulin resistance and secretory insufficiency produces the acute hyperglycemia of type 1 diabetes.
Supplementary Material
ACKNOWLEDGMENTS
DPT-1 was supported through cooperative agreements by the Division of Diabetes, Endocrinology, and Metabolic Diseases, National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health; the National Institute of Allergy and Infectious Diseases; the National Institute of Child Health and Human Development; the National Center for Research Resources; the American Diabetes Association; the Juvenile Diabetes Research Foundation; and various corporate sponsors.
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Gorsuch AN, Spencer KM, Lister J, McNally JM, Dean BM, Bottazzo GF, Cudworth AG: Evidence for a long prediabetic period in type I (insulin-dependent) diabetes mellitus. Lancet 1981; 2: 1363– 1365 [DOI] [PubMed] [Google Scholar]
- 2.Eisenbarth GS: Prediction of type 1 diabetes: the natural history of the prediabetic period. Adv Exp Med Biol 2004; 552: 268– 290 [PubMed] [Google Scholar]
- 3.Bonifacio E, Bingley PJ, Shattock M, Dean BM, Dunger D, Gale EA, Bottazzo GF: Quantification of islet-cell antibodies and prediction of insulin-dependent diabetes. Lancet 1990; 335: 147– 149 [DOI] [PubMed] [Google Scholar]
- 4.Riley WJ, Maclaren NK, Krischer J, Spillar RP, Silverstein JH, Schatz DA, Schwartz S, Malone J, Shah S, Vadheim C, et al. : A prospective study of the development of diabetes in relatives of patients with insulin-dependent diabetes. N Engl J Med 1990; 323: 1167– 1172 [DOI] [PubMed] [Google Scholar]
- 5.Wasserfall CH, Atkinson MA: Autoantibody markers for the diagnosis and prediction of type 1 diabetes. Autoimmun Rev 2006; 5: 424– 428 [DOI] [PubMed] [Google Scholar]
- 6.Verge CF, Gianani R, Kawasaki E, Yu L, Pietropaolo M, Jackson RA, Chase HP, Eisenbarth GS: Prediction of type I diabetes in first-degree relatives using a combination of insulin, GAD, and ICA512bdc/IA-2 autoantibodies. Diabetes 1996; 45: 926– 933 [DOI] [PubMed] [Google Scholar]
- 7.Bingley PJ, Bonifacio E, Gale EA: Can we really predict IDDM? Diabetes 1993; 42: 213– 220 [DOI] [PubMed] [Google Scholar]
- 8.Vardi P, Crisa L, Jackson RA: Predictive value of intravenous glucose tolerance test insulin secretion less than or greater than the first percentile in islet cell antibody positive relatives of type 1 (insulin-dependent) diabetic patients. Diabetologia 1991; 34: 93– 102 [DOI] [PubMed] [Google Scholar]
- 9.Chase HP, Cuthbertson DD, Dolan LM, Kaufman F, Krischer JP, Schatz DA, White NH, Wilson DM, Wolfsdorf J: First-phase insulin release during the intravenous glucose tolerance test as a risk factor for type 1 diabetes. J Pediatr 2001; 138: 244– 249 [DOI] [PubMed] [Google Scholar]
- 10.Greenbaum CJ, Sears KL, Kahn SE, Palmer JP: Relationship of β-cell function and autoantibodies to progression and nonprogression of subclinical type 1 diabetes: follow-up of the Seattle Family Study. Diabetes 1999; 48: 170– 175 [DOI] [PubMed] [Google Scholar]
- 11.Bingley PJ, Mahon JL, Gale EA: Insulin resistance and progression to type 1 diabetes in the European Nicotinamide Diabetes Intervention Trial (ENDIT). Diabetes Care 2008; 31: 146– 150 [DOI] [PubMed] [Google Scholar]
- 12.Fourlanos S, Narendran P, Byrnes GB, Colman PG, Harrison LC: Insulin resistance is a risk factor for progression to type 1 diabetes. Diabetologia 2004; 47: 1661– 1667 [DOI] [PubMed] [Google Scholar]
- 13.Krischer JP, Cuthbertson DD, Yu L, Orban T, Maclaren N, Jackson R, Winter WE, Schatz DA, Palmer JP, Eisenbarth GS: Screening strategies for the identification of multiple antibody-positive relatives of individuals with type 1 diabetes. J Clin Endocrinol Metab 2003; 88: 103– 108 [DOI] [PubMed] [Google Scholar]
- 14.Sosenko JM, Palmer JP, Greenbaum CJ, Mahon J, Cowie C, Krischer JP, Chase HP, White NH, Buckingham B, Herold KC, Cuthbertson D, Skyler JS: Increasing the accuracy of oral glucose tolerance testing and extending its application to individuals with normal glucose tolerance for the prediction of type 1 diabetes: the Diabetes Prevention Trial-Type 1. Diabetes Care 2007; 30: 38– 42 [DOI] [PubMed] [Google Scholar]
- 15.Sosenko JM, Palmer JP, Greenbaum CJ, Mahon J, Cowie C, Krischer JP, Chase HP, White NH, Buckingham B, Herold KC, Cuthbertson D, Skyler JS: Patterns of metabolic progression to type 1 diabetes in the Diabetes Prevention Trial-Type 1. Diabetes Care 2006; 29: 643– 649 [DOI] [PubMed] [Google Scholar]
- 16.Greenbaum CJ, Schatz DA, Cuthbertson D, Zeidler A, Eisenbarth GS, Krischer JP: Islet cell antibody-positive relatives with human leukocyte antigen DQA1*0102, DQB1*0602: identification by the Diabetes Prevention Trial-type 1. J Clin Endocrinol Metab 2000; 85: 1255– 1260 [DOI] [PubMed] [Google Scholar]
- 17.Effects of insulin in relatives of patients with type 1 diabetes mellitus. N Engl J Med 2002; 346: 1685– 1691 [DOI] [PubMed] [Google Scholar]
- 18.Skyler JS, Krischer JP, Wolfsdorf J, Cowie C, Palmer JP, Greenbaum C, Cuthbertson D, Rafkin-Mervis LE, Chase HP, Leschek E: Effects of oral insulin in relatives of patients with type 1 diabetes: the Diabetes Prevention Trial–Type 1. Diabetes Care 2005; 28: 1068– 1076 [DOI] [PubMed] [Google Scholar]
- 19.Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997; 20: 1183– 1197 [DOI] [PubMed] [Google Scholar]
- 20.Sosenko JM, Palmer JP, Rafkin-Mervis L, Krischer JP, Cuthbertson D, Matheson D, Skyler JS: Glucose and C-peptide changes in the perionset period of type 1 diabetes in the Diabetes Prevention Trial–Type 1. Diabetes Care 2008; 31: 2188– 2192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mari A, Tura A, Gastaldelli A, Ferrannini E: Assessing insulin secretion by modeling in multiple-meal tests: role of potentiation. Diabetes 2002; 51( Suppl. 1): S221– S226 [DOI] [PubMed] [Google Scholar]
- 22.Mari A, Pacini G, Murphy E, Ludvik B, Nolan JJ: A model-based method for assessing insulin sensitivity from the oral glucose tolerance test. Diabetes Care 2001; 24: 539– 548 [DOI] [PubMed] [Google Scholar]
- 23.Bingley PJ, Gale EA: Progression to type 1 diabetes in islet cell antibody-positive relatives in the European Nicotinamide Diabetes Intervention Trial: the role of additional immune, genetic and metabolic markers of risk. Diabetologia 2006; 49: 881– 890 [DOI] [PubMed] [Google Scholar]
- 24.Karvonen M, Viik-Kajander M, Moltchanova E, Libman I, LaPorte R, Tuomilehto J: the Diabetes Mondiale (DiaMond) Project Group. Incidence of childhood type 1 diabetes worldwide. Diabetes Care 2000; 23: 1516– 1526 [DOI] [PubMed] [Google Scholar]
- 25.Saad MF, Knowler WC, Pettitt DJ, Nelson RG, Mott DM, Bennett PH: Sequential changes in serum insulin concentration during development of non-insulin-dependent diabetes. Lancet 1989; 1: 1356– 1359 [DOI] [PubMed] [Google Scholar]
- 26.DeFronzo RA: Pathogenesis of type 2 diabetes mellitus. Med Clin North Am 2004; 88: 787– 835 [DOI] [PubMed] [Google Scholar]
- 27.Ferrannini E, Balkau B, Coppack SW, Dekker JM, Mari A, Nolan J, Walker M, Natali A, Beck-Nielsen H: Insulin resistance, insulin response, and obesity as indicators of metabolic risk. J Clin Endocrinol Metab 2007; 92: 2885– 2892 [DOI] [PubMed] [Google Scholar]
- 28.Toschi E, Camastra S, Sironi AM, Masoni A, Gastaldelli A, Mari A, Ferrannini E, Natali A: Effect of acute hyperglycemia on insulin secretion in humans. Diabetes 2002; 51( Suppl. 1): S130– S133 [DOI] [PubMed] [Google Scholar]
- 29.Vuorinen-Markkola H, Koivisto VA, Yki-Jarvinen H: Mechanisms of hyperglycemia-induced insulin resistance in whole body and skeletal muscle of type I diabetic patients. Diabetes 1992; 41: 571– 580 [DOI] [PubMed] [Google Scholar]
- 30.Meier JJ, Menge BA, Breuer TG, Muller CA, Tannapfel A, Uhl W, Schmidt WE, Schrader H: Functional assessment of pancreatic β-cell area in humans. Diabetes 2009; 58: 1595– 1603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ferrannini E, Nannipieri M, Williams K, Gonzales C, Haffner SM, Stern MP: Mode of onset of type 2 diabetes from normal or impaired glucose tolerance. Diabetes 2004; 53: 160– 165 [DOI] [PubMed] [Google Scholar]
- 32.Mason CC, Hanson RL, Knowler WC: Progression to type 2 diabetes characterized by moderate then rapid glucose increases. Diabetes 2007; 56: 2054– 2061 [DOI] [PubMed] [Google Scholar]
- 33.Tabak AG, Jokela M, Akbaraly TN, Brunner EJ, Kivimaki M, Witte DR: Trajectories of glycaemia, insulin sensitivity, and insulin secretion before diagnosis of type 2 diabetes: an analysis from the Whitehall II study. Lancet 2009; 373: 2215– 2221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Freiesleben De Blasio B, Bak P, Pociot F, Karlsen AE, Nerup J: Onset of type 1 diabetes: a dynamical instability. Diabetes 1999; 48: 1677– 1685 [DOI] [PubMed] [Google Scholar]
- 35.Nowak MA, Bangham CR: Population dynamics of immune responses to persistent viruses. Science 1996; 272: 74– 79 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.