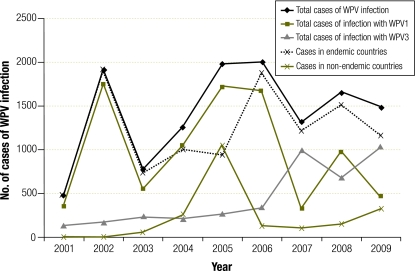
In its history of more than two decades, the Global Polio Eradication Initiative (GPEI), led by national governments and the World Health Organization, has made remarkable headway, punctuated by a few public health riddles. Globally, the number of cases of poliomyelitis (polio) confirmed annually dropped from an estimated 350 000 in 1988 to 1651 in 2008.1 By 2 December 2009, the number of cases of wild poliovirus (WPV) infection reported by endemic countries had declined somewhat, but the number reported by non-endemic countries had nearly tripled (Fig. 1). Indigenous WPV type 1 (WPV1) and WPV type 3 (WPV3) have been eliminated from all countries except Afghanistan, India, Nigeria and Pakistan, yet in 2008 outbreaks resulting from imported cases were reported by 12 countries, in five of which transmission has lasted for more than 12 months. Furthermore, cases of infection with the vaccine-derived poliovirus still occur, and this virus will continue to circulate and cause outbreaks for as long as oral polio vaccine is used. The time has not yet come when routine vaccination is no longer required, a hallmark that eradication has been achieved. In the midst of these virological considerations, the key lesson that emanates from the Indian experience is that the social determinants of programme implementation are as important as the technical ones – and this lesson has a significant bearing on other disease elimination programmes as well.
Fig. 1.
Global trends in cases of wild poliovirus infection, 2001–2009a
WPV, wild poliovirus; WPV1, wild poliovirus type 1; WPV3, wild poliovirus type 3.
a Cases for 2009 reported until 8 December.
Based on data from the World Health Organization.
Polio elimination in India
Efforts to eliminate polio in India may provide insights as to the factors that can influence the success or failure of polio elimination strategies and ultimate disease eradication. In India, 659 cases of WPV infection (predominantly with WPV3) and 15 cases of vaccine-derived poliovirus infection had been reported by 4 December 2009, about 80% of them in the state of Uttar Pradesh and 17% in the state of Bihar. Children aged less than 2 years were the most affected group. On the surveillance front, stool collection within 14 days of the onset of paralysis, as mandated by India’s National Polio Surveillance Project, has hovered between 84% and 85% of all reported cases of acute flaccid paralysis in 2008 and 2009 – figures that maintain the prescribed target of 80% or above. This is a critical component of the polio eradication strategy, since ascertaining that the poliovirus is the cause of a child’s paralysis is only possible by examining a stool specimen. However, in the last decade the incidence of non-polio acute flaccid paralysis in India has increased 10-fold (from the WHO benchmark of at least 1 per 100 000), and in 2009 Bihar reported 29 cases per 100 000 population (based on stool tests conducted in 86% of cases of acute flaccid paralysis). Questions have thus been raised about the robustness of polio surveillance, and there is concern that cases of poliomyelitic acute flaccid paralysis that are reported late may be lurking among “suspected” cases.
Under the GPEI Strategic Plan 2009–2013, the goal is to achieve polio eradication by 2013. With only 66 cases of WPV infection in 2005, India was seemingly at the threshold of eradicating polio; however, the 10-fold rise in cases of infection by WPV observed over the four ensuing years has put the goal beyond reach. There is a need to critically re-examine realities on the ground in India in an effort to understand what has gone wrong.
Supplementary immunization activities
The current polio elimination strategy has focused primarily on interrupting WPV1 transmission based on the epidemiological argument that WPV1 causes higher rates of paralysis than other wild poliovirus types and is likely to spread to polio-free areas. In 2005, monovalent oral polio vaccine against WPV1 (mOPV1) replaced the trivalent oral polio vaccine (tOPV) in some supplementary immunization rounds. After the WPV1 outbreak in 2006, the mOPV1 was administered to children through several supplementary immunization activities (SIAs). Consensus support for the use of the monovalent oral vaccine gradually emerged despite the lack of a sound body of evidence for its efficacy. Major differences in the efficacy of tOPV estimated for the adjoining states of Uttar Pradesh and Bihar, which are comparable in demographic characteristics, diarrhoea incidence, sanitation and overcrowding, remain an enigma.2 This is important, for these were the factors used to explain the low efficacy of tOPV and introduce mOPV1 in SIAs. However, WPV1 transmission was interrupted for more than one year in the endemic western districts of Uttar Pradesh for the first time during 2007–2008.
Epidemiological arguments apart, the deployment of mOPV1 raised an ethical issue as well. At the level of the individual child, the paralysis caused by WPV3 is no less severe than that caused by other WPV types. According to the Indian Academy of Paediatrics, the surge in polio cases caused by WPV3 in 2008 and 2009 was the iatrogenic result of having replaced tOPV with mOPV1 in many SIAs. It was also of the opinion that local expert advice was ignored while making such critical decisions.3 Gains in containing the incidence and transmission of WPV1 infection have proved fragile. Importation of WPV1 from Bihar in mid-2008 resulted in its re-establishment in western Uttar Pradesh, a situation aggravated by a routine immunization coverage of around 30%. Having adhered to frequent rounds of mOPV1, communities faced an unprecedented outbreak of WPV3 infection. In such circumstances, pockets of social resistance to immunization programmes are likely to emerge.
Several unambiguous lessons are apparent. The oral vaccine has proved effective even in the most difficult areas, but gains with monovalent vaccines are likely to be short-lived unless both WPV1 and WPV3 are addressed and high routine immunization coverage is sustained. Bivalent oral polio vaccine (bOPV) containing WPV1 and WPV3, to be introduced in SIAs shortly, seems promising. Routine immunization coverage in high-risk districts must be sufficiently high to sustain the gains of SIAs, lest we are kept engaged with counting cases of WPV infection. Sustained high routine immunization coverage in the states of Himachal Pradesh and Tamil Nadu has prevented the re-establishment of local transmission chains following occasional importation of cases of infection with WPV. Despite intensive tracking of births for administration of a zero-day dose (at considerable cost), the vaccine was not received by 18% of neonates in a rural block and by 37% of neonates in the urban fringes of Moradabad district in western Uttar Pradesh. As many as 42% of all children aged < 2 years in the district received no dose of OPV through routine immunization.4
The experience gained globally with the injected form of the polio vaccine (specifically, the enhanced inactivated polio vaccine, or e-IPV) makes a strong case for its inclusion in the post-eradication phase, but its suitability as a pre-eradication tool has also been intensely debated. It is thought that naso-oral and pharyngeal transmission may account for the low median age of incident cases (12–18 months) and for the high transmission rates in endemic districts. Accordingly, the use of the IPV in the pre-eradication phase in India was considered.5 However, as indicated by the results of a recent study from Uttar Pradesh, the injected vaccine may not be logistically suitable for SIAs for a variety of reasons, among them a shortage of trained vaccinators, parents’ concerns about injection safety, and an increase in social resistance.6 Those who must decide on whether or not to introduce the injected polio vaccine will have to take all these issues into account.
Social determinants of programme implementation
While programme managers and academics concentrate on vaccine innovations and molecular epidemiology, the critical path to success may lie in overcoming social resistance to available interventions.7 Overall vaccination coverage at the district level offers a false sense of security as long as less visible clusters of perpetually unimmunized children persist. Such clusters, however minuscule, may sustain low levels of WPV circulation, particularly among densely populated settlements with undernourished children suffering from intestinal infections, poor environmental hygiene, and low routine immunization coverage. Despite 97% vaccination coverage in the Netherlands, several outbreaks of polio have occurred in the last three decades among clustered, unvaccinated persons.8 In areas of poor development and inadequate health care, marginalised communities, regardless of religion or social group, are mistrustful of SIAs. Some circulating rumours pointed to elements of religious and cultural resistance as well.7 Allaying the fears and suspicions of these marginalised segments of the population will require improved primary health care and the visible involvement of volunteers from local communities in the microplanning of SIAs.
The way towards polio elimination
For India to eliminate polio, WPV circulation must cease simultaneously in all endemic areas in the country, and all new cases of infection with WPV and vaccine-derived poliovirus must be identified and aggressively managed. Rounds of supplementary immunization can lead to sustained achievements only if background routine immunization coverage is sufficiently high. In the current scenario, this is feasible provided success indicators for supplementary immunization are co-factored with those of routine immunization. The GPEI must see to it that these two equally critical activities are integrated. The rigour with which surveillance for acute flaccid paralysis is conducted must be re-examined and improved, and social resistance to SIAs needs to be addressed with urgency and sensitivity to local cultural norms.
Overassertive and demonstrative political and administrative action can make communities somewhat apprehensive. People have started asking “why only polio?” Questions such as these require emic solutions, i.e. a serious reexamination of the programme from the vantage point of a reluctant client or a fatigued health worker. While international expertise brings in global knowledge, involving newer grassroots partners can rejuvenate vaccine delivery systems. Local wisdom and leadership must be recognized, nurtured and given a front-line role on issues of micro-level communication, programme delivery and community mobilization.
In its last lap, polio eradication is much more than a technical mission. What has been learned so far about the social determinants of programme implementation is widely applicable, both geopolitically and in terms of the technical and operational aspects of future efforts to eliminate other diseases. The “vertical” nature of all such efforts and people’s perceptions about them demand a thorough deconstruction. The voices of the most peripheral health workers and marginalised clients, ignored under the glamour of international advocacy, need to be seriously heeded, for they will give us many answers. ■
Footnotes
Competing interests: The authors are affiliated with institutions that support the Global Polio Eradication Initiative.
References
- 1.Centers for Disease Control and Prevention Progress toward interruption of wild poliovirus transmission--worldwide, 2008. MMWR Morb Mortal Wkly Rep. 2009;58:308–12. [PubMed] [Google Scholar]
- 2.Grassly NC, Fraser C, Wenger J, Deshpande JM, Sutter RW, Heymann DL, et al. New strategies for the elimination of polio from India. Science. 2006;314:1150–3. doi: 10.1126/science.1130388. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal RK. Polio eradication in india: a tale of science, ethics, dogmas and strategy! Indian Pediatr. 2008;45:349–51. [PubMed] [Google Scholar]
- 4.Rainey JJ, Bhatnagar P, Estivariz CF, Durrani S, Galway M, Sandhu H, et al. Providing monovalent oral polio vaccine type 1 to newborns: findings from a pilot birth-dose project in Moradabad district, India. Bull World Health Organ. 2009;87:955–9. doi: 10.2471/BLT.08.061556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.John TJ. Antibody response to pulse polio immunisation in Aligarh. Indian Pediatr. 2005;42:91–2. [PubMed] [Google Scholar]
- 6.Dasgupta R, Chaturvedi S, Adhish V, Ganguly KK, Rai S, Sushant L, et al. Towards polio ‘endgame’: need to focus on social determinants. Indian Pediatr. 2008;45:357–65. [PubMed] [Google Scholar]
- 7.Chaturvedi S, Dasgupta R, Adhish V, Ganguly KK, Rai S, Sushant L. Srabasti, Arora NK. Deconstructing social resistance to pulse polio campaign in two North Indian Districts. Indian Pediatr. 2009;46:963–74. [PubMed] [Google Scholar]
- 8.Conyn-Van Spaendonck MA, de Melker HE, Abbink F, Elzinga-Gholizadea N, Kimman TG, van Loon T. Immunity to poliomyelitis in the Netherlands. Am J Epidemiol. 2001;153:207–14. doi: 10.1093/aje/153.3.207. [DOI] [PubMed] [Google Scholar]