Summary
Microbial pathogens use adhesive surface proteins to bind to and interact with host tissues, events that are universal for the pathogenesis of infectious diseases. A surface adhesin of Bacillus anthracis, the causative agent of anthrax, required to mediate these steps has not been discovered. Previous work identified BslA, an S-layer protein, to be necessary and sufficient for adhesion of the anthrax vaccine strain, Bacillus anthracis Sterne, to host cells. Here we asked whether encapsulated bacilli require BslA for anthrax pathogenesis in guinea pigs. Compared with the highly virulent parent strain B. anthracis Ames, bslA mutants displayed a dramatic increase in the lethal dose and in mean time-to-death. Whereas all tissues of animals infected with B. anthracis Ames contained high numbers of bacilli, only few vegetative forms could be recovered from internal organs of animals infected with the bslA mutant. Surface display of BslA occurred at the poles of encapsulated bacilli and enabled the binding of vegetative forms to host cells. Together these results suggest that BslA functions as the surface adhesin of the anthrax pathogen B. anthracis strain Ames.
Introduction
Bacillus anthracis causes lethal infections in mammals when introduced to the host via cutaneous inoculation, inhalation or ingestion (Mock & Fouet, 2001). Towards the end of the nineteenth century, Robert Koch and Louis Pasteur established B. anthracis as the first model for bacterial pathogenesis (Koch, 1876) and protective immunity (Pasteur, 1881), respectively. These efforts as well as work by Max Sterne in the 1930s (Sterne, 1937) were responsible for producing attenuated strains of B. anthracis that lacked one of two large virulence plasmids, pXO1 and pXO2 (Okinaka et al., 1999a), for vaccine protection of livestock from anthrax disease (Grabenstein, 2008). Continued study of B. anthracis biology established the paradigm that anthrax pathogenesis is primarily mediated via the two virulence plasmids (Mock & Fouet, 2001). Anthrax toxins, i.e. edema toxin and lethal toxin, are encoded by pagA, lef, and cya on pXO1 (Smith et al., 1955, Vodkin & Leppla, 1983, Leppla, 1982, Robertson & Leppla, 1986). The secreted toxins enable bacilli to evade immune defenses and kill their host (Collier & Young, 2003). The poly-γ-D-glutamic acid (PDGA) capsule is synthesized by products of the capBCADE operon, which is located on pXO2 (Candela & Fouet, 2006). PDGA capsule endows the vegetative forms of B. anthracis with resistance to phagocytic killing (Drysdale et al., 2005).
Anthrax disease is remarkable for causing lethality from very low inocula of spores (LD50 < 30). Loss of pXO2 as well as mutations in capBCADE that abrogate PDGA capsule formation both cause a large reduction in the virulence of B. anthracis (Drysdale et al., 2005, Richter et al., 2009). Loss of pXO1 also leads to a dramatic decrease in virulence of B. anthracis strain Ames and abolishes the vaccine protection of variants derived from B. anthracis strain Sterne (Sterne, 1937, Little & Knudson, 1986, Singh et al., 1998). Although mutations in pagA, lef or cya abolish the function of lethal and/or edema toxin, these mutants remain fully virulent in mouse models of systemic and respiratory anthrax (Pezard et al., 1991, Heninger et al., 2006, Chand et al., 2009). pXO1-encoded genes that are universally required for anthrax pathogenesis have not been identified.
A striking feature of anthrax is the extraordinary abundance of bacilli, 108-1010 colony forming units (CFU) per gram of tissue, that accumulate in all organ systems of infected animals (Koch, 1876). Initial steps in the infectious process involve interactions between spores of the anthrax pathogen and host phagocytes (Dixon et al., 2000). Once taken up, spores germinate in the phagosome and the resulting vegetative forms replicate until an infected cell has been lysed (Guidi-Rontani et al., 1999, Guidi-Rontani et al., 2001, Ruthel et al., 2004). Once extracellular, vegetative forms produce a PDGA capsule to avoid phagocytic killing (Drysdale et al., 2005). B. anthracis is non-motile (Read et al., 2003). How, then, does the anthrax pathogen achieve the ubiquitous dissemination of bacilli throughout host tissues? Dissemination presumably depends on the circulation of body fluids and cells as well as on the ability of bacilli to adhere to cells and tissues of their infected hosts. If so, surface proteins of bacilli may have evolved to function as adhesins. In addition to the toxin and capsule biosynthesis genes, pXO1 and pXO2 encode for over 200 genes whose roles in the lifecycle of B. anthracis have yet to be described (Okinaka et al., 1999b, Okinaka et al., 1999a). These genes may include the presumed adhesins of the anthrax pathogen.
We recently demonstrated that vegetative forms of B. anthracis Sterne, the anthrax vaccine strain, employ the SLH protein BslA for adhesion to host cells (Kern & Schneewind, 2008). Its structural gene, bslA, is located within the pXO1 pathogenicity island that also codes for toxin genes (pagA, lef, and cya)(Kern & Schneewind, 2008). The predicted primary translation product of bslA includes an N-terminal signal peptide, which initiates the protein into the (Sec) secretion pathway as well as three tandem S-layer Homology domains (SLH) (Kern & Schneewind, 2008), features that predict targeting of proteins to the B. anthracis surface-layer (S-layer) (Mesnage et al., 2000, Mesnage et al., 1999). The S-layer of B. anthracis and other microbes can be thought of as a surface organelle of vegetative forms, assembled from proteins that generate a para-crystalline sheath (Sleytr, 1997, Bahl et al., 1997). Given that many bacterial pathogens require adherence to host tissues to mediate infection and that bslA is linked to genes known to be required for virulence, we hypothesized that the highly virulent pathogen, B. anthracis strain Ames, may require bslA to cause anthrax disease.
Results
B. anthracis Ames lacking bslA is toxigenic and encapsulated
Previous experiments on bslA were carried out in B. anthracis Sterne (Kern & Schneewind, 2008), which does not cause anthrax disease in immune-competent hosts (Welkos et al., 1986, Welkos et al., 1989). Therefore, to test if bslA is required for anthrax pathogenesis in the fully virulent clinical isolate B. anthracis strain Ames (Read et al., 2002), we replaced the bslA open reading frame with a spectinomycin resistance cassette via allelic replacement (Marraffini & Schneewind, 2006), generating the B. anthracis Ames bslA mutant. To ensure that these strains are both toxigenic and encapsulated, total protein extracts from the bslA mutant and its isogenic parent B. anthracis Ames strain were subjected to SDS-PAGE and probed with specific antisera raised against purified recombinant protective antigen (PagA) and against BslA (Fig. 1A). As expected, both strains produced equivalent quantities of PagA, but only the wild-type strain produced BslA (Fig. 1A). Thus, although wild-type and bslA mutant harbor pXO1 plasmid and are both able to secret toxin, only the wild-type strain Ames secretes the S-layer protein BslA (Fig. 1A). Next, to ensure that these bacteria are encapsulated, we propagated wild-type and bslA mutant colonies on media that induce capsule formation (Richter et al., 2009). Both strains formed colonies that appeared smooth and mucoid, a trait associated with encapsulated strains (data not shown)(Preisz, 1909). Several colonies from each strain were formalin fixed and scored for their ability to produce capsule by immunofluorescence microscopy with PDGA specific rabbit antiserum (Fig. 1B). Both wild-type and bslA mutant bacilli elaborated similar amounts of capsule material, as their vegetative forms generated PDGA-specific immunofluorescent signals with equal intensity (Fig. 1B). As a control, bacilli from the same cultures incubated with naïve rabbit sera (NRS) did not produce immunofluorescence staining when analyzed under similar conditions (Fig. 1B).
Figure 1. Mutations in bslA do not affect toxin secretion and capsule production of B. anthracis Ames.
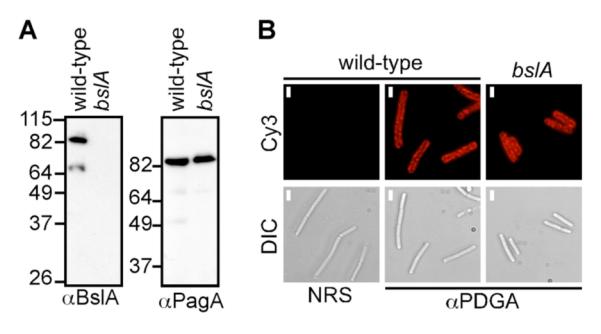
A. Immunoblots of B. anthracis wild-type and bslA deficient strains demonstrate that both strains produce the toxin component protective antigen (PagA). Total protein extracts were subjected to SDS-PAGE and blotted with antisera specific for BslA and PagA.
B. Fluorescence micrographs show poly-γ-D-glutamic acid (PDGA) capsule staining for both wild-type and bslA mutants. Bacteria were grown in capsule-inducing culture conditions, fixed and stained with either naïve rabbit sera (NRS) or with PDGA-specific antisera and a Cy3-conjugated secondary. Scale bars – 1 μm
BslA mediates adherence between B. anthracis Ames vegetative forms and host cells
In B. anthracis Sterne, we have shown that BslA mediates adherence between vegetative bacilli and host cells (Kern & Schneewind, 2008). The most striking difference between the envelope and surface attributes of B. anthracis Ames and B. anthracis Sterne strains is the presence of a thick layer of PDGA capsule in the former. Previous studies had shown that antibodies against other S-layer proteins only labeled small portions of the bacteria, presumably because the thick capsule occludes antibody-antigen binding (Mesnage et al., 1998). We wondered, therefore, if BslA was capable of mediating adherence between encapsulated vegetative bacilli and host cells. First, we propagated B. anthracis Ames and the isogenic bslA mutant on heart infusion agar supplemented sodium bicarbonate in the presence of 5% CO2, culture conditions that are known to induce the expression of both BslA and capsule (Kern & Schneewind, 2008, Richter et al., 2009). Vegetative bacilli were suspended and labeled with AlexaFluor 488 dye. Equal numbers of labeled bacilli were then added to monolayers of HeLa tissue culture cells. After incubation, the cells were washed rigorously and fixed, stained with Hoechst and rhodamine-phalloidin, and imaged. Fluorescent micrographs of HeLa cell monolayers infected with wild-type, but not with bslA mutant, cultures revealed adherent bacilli, indicating that encapsulated B. anthracis Ames is able to bind tissue culture cells and that the bslA gene is indeed required to mediate adherence between host cells and vegetative forms in encapsulated strains (Fig. 2A).
Figure 2. BslA is displayed on the surface of encapsulated bacteria and mediates B. anthracis Ames adherence to tissue culture cells.
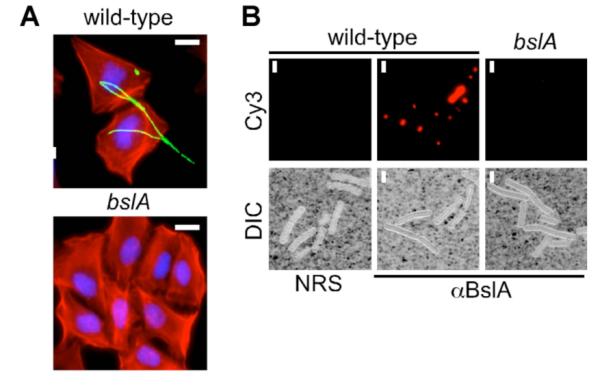
A. Fluorescent micrographs of wild-type, but not bslA mutant, bacilli adhering to HeLa cell monolayers. Bacilli were induced for BslA and capsule expression, labeled with AlexaFluor488 (green), added to HeLa monolayers, washed and then fixed. Actin filaments were labeled with rhodamine-phalloidin (red) and nuclei were labeled with Hoescht (blue). Scale bar = 10 μm.
B. Immunofluorescence micrographs of BslA expression during infection. Spleen tissues were fixed and homogenized from animals that died of anthrax infections. Homogenates were labeled with antisera specific for BslA or with NRS and then stained with Cy3-conjugated secondary. India ink exclusion in the DIC images is a measure of encapsulation. Scale bar = 1 μm.
We reasoned, therefore, that in order to mediate this adherence, portions of the vegetative bacterial surface must display S-layer proteins and, consequently, BslA. To test if this hypothesis held true in vivo, we isolated bacilli from the spleens of guinea pigs that had succumbed to anthrax disease (red circles, Fig. 3A) and labeled them using naïve rabbit sera or antisera specific for BslA followed by a fluorescent-conjugated secondary antibody. Fluorescent micrographs of these bacilli revealed a striking staining pattern – BslA-specific staining could be observed at or near the cell poles, but not on or around the lateral cell walls (Fig. 2B). A distinct halo of India-ink exclusion can be seen in DIC micrographs, confirming that these bacilli are encapsulated (Fig. 2B). These data demonstrate that B. anthracis Ames expresses and displays BslA on the surface during infection, thereby enabling the adhesin to interact with host tissues. The observed polar staining pattern of BslA may be due to differences in the density of capsule material at different locations on the cell surface. We assume the capsule is less abundant at the poles of vegetative forms, permitting antibody binding to BslA that is deposited in the S-layer. Presumably, the BslA molecules at the poles of vegetative forms can engage their ligands on the surface of host cells.
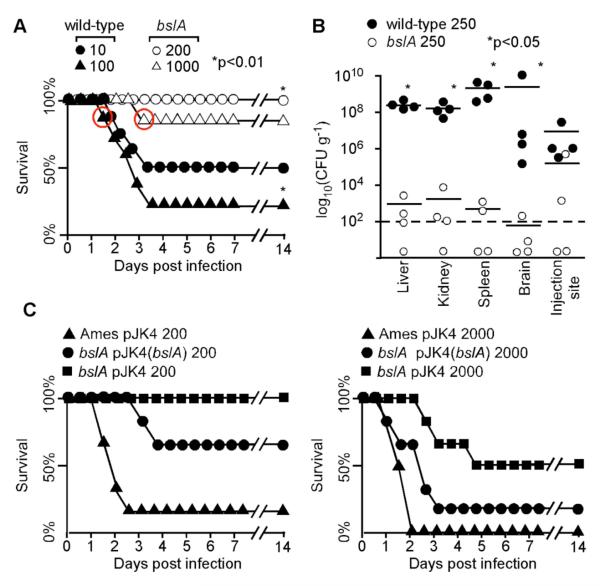
Figure 3. bslA is required for the pathogenesis of anthrax disease caused by B. anthracis strain Ames.
A. Kaplan-Meier curves comparing survival rates between wild-type and bslA mutant infected guinea pigs. Cohorts of eight guinea pigs were inoculated sub-cutaneously with 10 or 100 wild-type spores or with 200 or 1000 bslA mutant spores. Animal health was monitored in 8-hour intervals for 14 days.
B. CFU counts from tissue homogenates of animals infected with 250 spores from either wild-type or bslA mutant B. anthracis strains. The arithmetic mean value for each cohort is represented by a horizontal line.
C. Kaplan-Meier curves comparing survival rates between wild-type + pJK4, bslA + pJK4 and bslA + pJK4(bslA). Cohorts of six guinea pigs were inoculated sub-cutaneously with 200 (left panel) or 2000 (right panel) spores. Animal health was measured in 8-hour intervals for 14 days.
B. anthracis bslA is required for anthrax disease
Many bacteria synthesize adhesive structures to mediate essential steps in the process of infection and dissemination (Isberg, 1991, Navarre & Schneewind, 1999). B. anthracis spores are believed to interact with local phagocytes in the initial stages of infection, ultimately traveling with these cells to the nearest lymph node, and multiplying within their cytoplasm (Dixon et al., 2000, Guidi-Rontani et al., 2001). Eventually, vegetative bacilli lyse the phagocytic cell that harbors them and then replicate extracellularly throughout the host (Mock & Fouet, 2001). To date, no adhesive molecule has been assigned an essential role in these early steps of infection or in the later steps of dissemination and immune evasion. Given that the same pathogenicity island that encodes genes for the anthrax toxins contains bslA, we hypothesized that B. anthracis may require bslA during infection to cause anthrax disease (Okinaka et al., 1999b).
We compared the ability of bslA deficient and wild-type B. anthracis Ames spores to cause disease in a guinea pig model of anthrax. Cohorts of eight guinea pigs were inoculated with 10 or 100 spores of the wild-type strain or with 200 or 1000 spores of the bslA mutant and monitored for 14 days. A dose of ten wild-type spores was sufficient to cause lethal anthrax disease in four of eight animals with a mean-time-to-death (MTD) of 64.5 hours and a dose of 100 wild-type spores killed six of eight animals with an MTD of 61 hours (Fig. 3A). In contrast, only one of eight animals challenged with 1,000 spores of the bslA mutant died at 84 hours, indicating that a deletion in bslA results in a greater than 100-fold increase in the LD50 of its isogenic parent strain Ames and that animals infected with bslA spores survive longer (Fig. 3A). To the best of our knowledge, this is the first time that a B. anthracis SLH protein has been confirmed as a virulence factor.
Given the elevated LD50 in the bslA mutant, we wondered if mutants lacking the bslA gene were capable of disseminating and replicating throughout host tissues, a hallmark of anthrax disease (Koch, 1876). Groups of four guinea pigs were challenged with a dose of 250 wild-type or bslA mutant spores. All four animals infected with wild-type spores became moribund within 48 hours, whereas none of the four guinea pigs infected with bslA mutant spores displayed any signs of disease. As the wild-type animals succumbed to infection, each was killed along with a corresponding animal infected with spores lacking bslA. The liver, kidney, spleen, and brain were harvested along with the lymphatic tissue at the injection site. Each of these tissues was homogenized, serially diluted and plated on agar medium for colony formation to enumerate bacterial load. An average of 5 − 107 CFU per gram of tissue was isolated from the injection sites of animals infected with wild-type B. anthracis, which was associated with disseminated infection and 108 or more bacilli in liver, spleen and brain tissue (Fig. 3B). In contrast, animals infected with the bslA mutant contained far fewer CFU at the site of injection on average and between 102 and 103 bacteria in various organ systems (Fig. 3B).
We next sought to restore the virulence defect observed in bslA mutants by providing complementation in trans. Plasmid complementation of virulence defects in bacterial pathogens during animal experiments is complicated by differences in gene dosage between plasmids or chromosomes, plasmid stability in the absence of antibiotic selection and differences in gene regulation between wild-type and complementing alleles (Lee & Schneewind, 1999). To test best of our knowledge, this has not yet been accomplished for B. anthracis virulence genes (toxins or capsule) (Drysdale et al., 2005). Wild-type Ames was transformed with the empty vector pJK4 and the bslA mutant strain was transformed with pJK4 or with pJK4(bslA), a plasmid containing the bslA open reading frame under IPTG-inducible control of the Spac promoter on pJK4. Proteins precipitated from whole cultures were immunoblotted with sera specific for PagA and BslA, confirming that pJK4(bslA) restores the expression of this adhesin in bslA mutants (Fig. S1). Spores were purified from cultures harboring these plasmids and subsequently cultured and confirmed to retain the plasmid and produce both toxin and BslA.
We tested the ability of bslA spores complemented with pJK4(bslA) to cause anthrax disease. Cohorts of six guinea pigs were challenged by subcutaneous injection with 200 or 2000 spores from each strain and monitored for 14 days. As expected, we observed an increase in the LD50 of bslA (pJK4) (approximately 2000 CFU) as compared to wild-type (pJK4) spores (less than 200 CFU) and a commensurate increase in the MTD from 30 hours [wild-type (pJK4)] to 66 hours [bslA ( pJK4)] (Fig. 3C). In contrast, guinea pigs challenged with either 200 or 2000 spores of bslA transformed with the complementing plasmid, pJK4(bslA), demonstrated a decreased rate of survival as well as a decreased MTD (78 and 48.4 hours, respectively) when compared to those infected with bslA spores containing only the vector control (Fig. 3C). Of note, pJK4(bslA) restored the ability of bslA mutants to cause lethal infections and their associated MTD almost to wild-type levels. Limits in cohort size (six animals per challenge strain) failed to generate statistical significant differences between groups. Nevertheless, we interpret the observed increase in LD50 and the associate decrease in MTD for bslA [pJK4(bslA)] spores as evidence that the virulence defect of bslA mutants can at least in part be complemented in trans by plasmid encoded bslA. We assume, therefore, that the reduced virulence of bslA mutants is caused by their defect in the expression of BslA adhesin during infection.
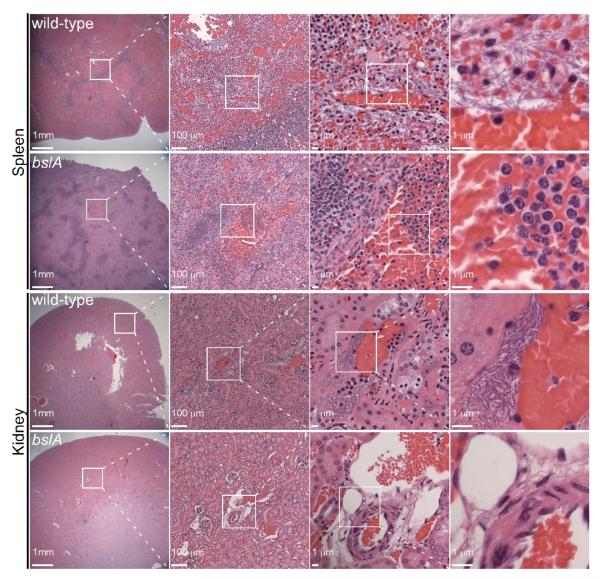
In order to visualize anthrax bacilli in situ, small portions of organs harvested from animals that succumbed to infection were fixed in fomalin, sectioned and stained with hematoxylin and eosin. Micrographs of the kidney and spleen samples contain abundant numbers of darkly stained rods in all wild-type tissues, which were absent from tissues harvested from guinea pigs infected with the bslA mutant (Fig. 4). Rod-shaped bacteria were also easily located within the brain and liver of animals infected with wild-type spores but not with bslA deficient spores (data not shown). These data indicate that the fully virulent strain B. anthracis Ames requires its adhesin, bslA, in order to cause anthrax disease, measured either by LD50 or by bacterial load.
Figure 4. Histopathology of guinea pig tissue infected with wild-type or bslA mutant B. anthracis strain Ames.
Micrographs of H&E stained sections from organs harvested from animals infected in Figure 3B. Abundant rod-shaped bacilli are seen in tissues from animals infected with wild-type but not those infected with bslA mutant spores.
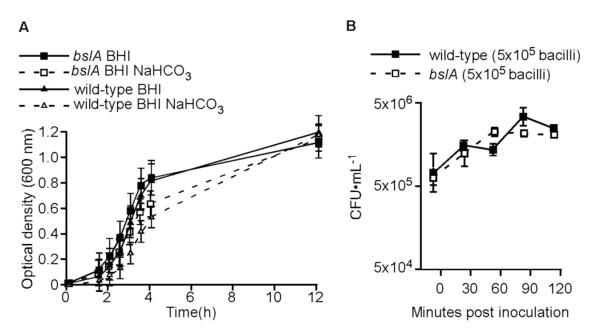
bslA is dispensable for growth in laboratory broth or whole blood
We reasoned that the difference in the LD50 dose and in the load of B. anthracis vegetative forms observed between wild-type and bslA strains could result from the mutant’s inability to engage its host ligand(s). If so, this could lead to defects in immune evasion and/or in dissemination, or a reduced capacity to replicate inside host tissues. B. anthracis Ames wild-type and bslA mutant strains display no difference in their ability to grow in laboratory broth and have identical doubling times regardless of whether or not they are induced for capsule, toxin and BslA production (Fig. 5A). As a model tissue for in vivo growth, we used the blood of naïve guinea pigs to measure the growth rates of both strains. Equal numbers of bacilli, grown in laboratory broth supplemented with sodium bicarbonate to induce toxin, capsule and BslA expression, were inoculated into guinea pig blood. The bacterial load was measured as CFU•mL−1 every 30 minutes for two hours from three independent infections. Blood cells in sample aliquots of each infection were lysed with saponin, serially diluted and plated on agar media. The means of CFU in blood cultures inoculated with B. anthracis Ames wild-type or bslA were not statistically different at any time point (Fig. 5B). Thus, both wild-type and bslA mutant bacilli not only survive in blood but their vegetative forms even expand over the time period tested (Fig. 5). The data suggest further that bacilli lacking bslA are able to resist phagocytic killing, but that bslA is required at discrete stages of anthrax infection that enable the dissemination of vegetative forms.
Figure 5. Wild-type and bslA mutant bacteria grow equally well in laboratory broth or whole blood.
A. Growth curves from cultures of B. anthracis wild-type or bslA mutants cultured in BHI or BHI + 0.8% NaHCO3. OD600 values between wild-type and bslA cultures were not statistically different at any time point. Data are represented as mean values, error bars denote the standard deviation from the mean.
B. Equal numbers (5 × 105) of wild-type and bslA mutant bacilli were inoculated into naïve, whole guinea pig blood (T=0) and enumerated every 30 minutes for two hours. The numbers of wild-type and bslA mutant CFU are not statistically different for the duration of the experiment. Data are represented as mean values, error bars denote the standard deviation from the mean.
Discussion
Many phylogenetically distinct groups of bacteria synthesize an S-layer from one or more protein precursors, to mediate processes as disparate as proteolysis, metabolism, peptidoglycan catabolism, adhesion, and immune evasion (Bahl et al., 1997, Sleytr, 1997). Previous work on the S-layer of B. anthracis focused on the two most abundant S-layer components, Sap and EA1 (Mesnage et al., 1997, Mesnage et al., 1999). These studies reported that Sap and EA1 were not required for anthrax pathogenesis but left unresolved what roles, if any, the 22 less-abundant SLH-domain containing proteins have in the infectious lifecycle (Mesnage et al., 2000). Here we report that the S-layer adhesin, BslA, is required for anthrax pathogenesis and suggest that other SLH proteins may contribute to the B. anthracis lifecycle. Spores of the bslA mutant are unable to cause lethality at the same dose as spores from the wild-type parent strain, likely because bacilli lacking bslA are defective in the dissemination and replication of bacilli within multiple different host organ systems. Future work must discover the host molecule(s) that interacts with BslA and the precise stages of infection when these interactions are important. Although the N-terminal SLH domains readily identify BslA as an S-layer protein, a functional assignment cannot be derived from the remainder of the BslA sequence. Homology searches suggest that the C-terminal region of BslA resembles the N-terminal domain of SMC (structural maintenance of chromosomes) proteins (Hirano, 2006). In both prokaryotes and eukaryotes, SMC proteins provide ATP-dependent cohesive forces necessary to physically maintain chromosomes during cell division. Although BslA lacks the Walker A box known to be vital to SMC protein function, perhaps BslA mediates adherence by co-opting protein-protein interactions that initially evolved in SMC proteins.
The pXO1 plasmid is absolutely required for pathogenesis; over a century of research, dating back to Louis Pasteur’s development of the first vaccine strains (Pasteur, 1881), demonstrated that the plasmid encodes genes with important contributions to anthrax disease (Vodkin & Leppla, 1983, Leppla, 1982, Bragg & Robertson, 1989, Okinaka et al., 1999b). This report adds bslA to the list of pXO1-encoded genes that promote anthrax disease in mammalian hosts. The plasmid contains nearly 200 open reading frames many of which have no predicted function (Okinaka et al., 1999b). Moreover, encapsulated strains of Bacillus cereus containing pXO1 (and bslA) have been recovered from animals that died of anthrax infection, underscoring the intimate relationship between this plasmid and the pathogenic potential of Bacillus species (Hoffmaster et al., 2004). The abundance, genetic requirement for disease pathogenesis, and surface localization of BslA suggest that this protein may be an attractive target for vaccine development. Discovering the molecular role BslA plays during anthrax pathogenesis and identifying its host cell receptor should be important goals for biodefense research.
Experimental Procedures
Bacterial strains and plasmids
Bacillus anthracis strain Ames or its variants were grown in brain heart infusion broth (BHI) or Luria broth (LB) at 37°C or at 30°C when transformed with pLM4-derived plasmids (Marraffini & Schneewind, 2006). Adherence was induced by culturing bacteria in BHI supplemented with 0.8% NaHCO3. Spores were purified from B. anthracis cultures grown for five days in 2× SG medium at 30°C. Bacterial sediments were washed extensively with water and heat shocked at 65°C for 30 min prior to dilution and enumeration on agar medium. Media were supplemented with kanamycin (20 μg ml−1) to maintain plasmid selection in B. anthracis where appropriate. Plasmid pJK66 was purified from E. coli strain K1077 (dam−, dcm−) grown in LB broth at 37°C supplemented with kanamycin (50 μg ml−1). The B. anthracis strain Ames bslA::ΩSpR mutant (bslA mutant) was constructed by allelic replacement with pJK66. Transformants were grown at 30°C overnight and single recombinants selected by plating at 43°C overnight on LB agar containing kanamycin. Single colonies were then passed at 30°C four times serially to induce a second recombination event and loss of pJK66. Mutations were confirmed by PCR and immunoblotting with BslA-specific antibodies. Complementation studies were preformed using pJK4, a thermo-stable variant of the pE194ts-based pLM5. Three nucleotide substitutions, designed to revert the pE194ts origin of pLM5 to that of the thermo-stable pE194, were made by pfu mutagenesis. pLM5 plasmid DNA template, purified from E. coli DH5α was amplified using pfu Turbo (Stratagene) using the primers P371 5′- AGGGATACTGATACAGAAGGTAGGATGAAAAAAGAGC-3′ and P372 5′- GCTCTTTTTTCATCCTACCTTCTGTATCAGTATCCCT-3′. These reactions were restricted with DpnI and transformed into E. coli DH5α. Plasmid DNA with the expected nucleotide sequence was then used as the template for successive substitutions following the same protocol, using primer pairs P373 5′- ATGACTAAATTTTGTTAAGTGTATTAGCACCGTTATT-3′/P374 5′- AATAACGGTGCTAATACACTTAACAAAATTTAGTCAT-3′ and P375 5′- GTTGGGAGGTACAGTGATGGTTGTAGATAGAAAAGAA-3′/P376 5′- TTCTTTTCTATCTACAACCATCACTGTACCTCCCAAC-3′. Both pJK4 plasmid DNA and PCR-amplified DNA coding for bslA (amplified from Ames chromosomal DNA template with P186 5′- TTTTCTAGAATGAAAAAAAGAAAGATAAAAGCTATTACG – 3′ and P187 5′ - TTTGGTACCTTAACTGTTTGGTATTCTAAGTTTAGGAAATT – 3′) were restricted with XbaI and KpnI and ligated together. Ligation products were transformed into E. coli DH5α. The ability of the pJK4 and pJK4(bslA) plasmid to replicate in B. anthracis Ames at 37°C was confirmed by measuring the plasmid content of cultures by PCR.
Adherence assays
B. anthracis overnight cultures were sedimented by centrifugation and washed with PBS. Equal numbers of B. anthracis Ames or bslA mutants were then incubated with Alexafluor 488 and 0.1M NaHCO3 according to the manufacturer’s recommendations. Labeled bacteria were then incubated with monolayers of HeLa cells for three hours. Infected tissue culture cells were washed extensively with PBS and fixed with gluteraldehyde. Fixed cells were incubated with 0.1% Triton-X100 in PBS for 30 minutes and then stained with rhodamine-phalloidin and Hoechst in PBS containing 5% dried non-fat milk. Fluorescence micrographs were collected digitally on a TE-2000 inverted microscope (Nikon) at 200× magnification.
Immunofluorescence
The spleens of moribund, anthrax infected guinea pigs were fixed for six weeks in 10% formalin and then homogenized in PBS. Tissue homogenates were stained with naïve rabbit sera or with antisera specific for BslA or PDGA followed by Cy3-conjugated anti-rabbit IgG (ZyMed). Stained homogenates were wet-mounted with or without India Ink (BD) for microscopy analysis. DIC images and fluorescent micrographs were collected on an Olympus Provis axial microscope (1,000× magnification) equipped with a CCD camera.
Immunoblotting
B. anthracis cultures, grown overnight in BHI supplemented with 0.8% NaHCO3 were either filter-sterilized and proteins precipitated by addition of trichloroacetic acid to a final concentration of 7.5% or bacterial sediments boiled in sample buffer. Protein pellets from culture filtrates were then solubilized by boiling in sample buffer. These samples were subjected to SDS-PAGE, electrotransferred to PVDF membranes and protein species detected by incubation with specific sera raised in rabbits.
Guinea pig model of anthrax infection and whole blood growth assay
Six-week old female Hartley guinea pigs were injected subcutaneously with a suspension of spores diluted in 100 μL of PBS. Animal health was subsequently monitored in 8-hour intervals. Moribund animals were killed by asphyxiation and cervical dislocation. Organs were harvested at the time-of-death, homogenized in PBS, serially diluted and plated in duplicate on agar media to determine bacterial load. Organ samples were fixed in 100 mL 10% formalin for 14 days, transferred to 100 mL fresh 10% formalin and incubated for an additional 14 days. Slide preparation and H&E staining was carried out by the University of Chicago immunohistochemistry core laboratory. The whole blood growth assay was carried out by adding equal numbers (5 × 105) of B. anthracis bacilli grown in laboratory broth to 200 μL of Refluden-treated (50 μg/mL) whole, naïve guinea pig blood. Aliquotes were removed every 30 minutes, incubated with a final concentration of 0.2% saponin in PBS, serially diluted and plated. All animal experiments and select agent experiments were performed in accordance with institutional guidelines following experimental protocol review and approval by the Institutional Biosafety Committee and the Institutional Animal Care and Use Committee at the University of Chicago. Logrank tests were used to compare the statistical significance of mortality between wild-type and bslA mutant strains. The ranksum test was used for pairwise analyses of bacterial load in infected animal tissues.
Supplementary Material
Acknowledgements
We thank members of our laboratory for critical comments and discussion. This work was supported by a grant from the National Institute of Allergy and Infectious Diseases (NIAID), Infectious Diseases Branch (AI69227) to O.S. J.W.K. acknowledges support from the Molecular Cell Biology Training Grant (GM007183) at the University of Chicago. The authors acknowledge membership within and support from the Region V “Great Lakes” Regional Center of Excellence in Biodefense and Emerging Infectious Diseases Consortium (GLRCE, National Institute of Allergy and Infectious Diseases Award 1-U54-AI-057153).
References
- Bahl H, Scholz H, Bayan N, Chami M, Leblon G, Gulik-Krzywicki T, Shechter E, Fouet A, Mesnage S, Tosi-Couture E, Gounon P, Mock M, de Macario E. Conway, Macario AJ, Fernández-Herrero LA, Olabarría G, Berenguer J, Blaser MJ, Kuen B, Lubitz W, Sára M, Pouwels PH, Kolen CP, Boot HJ, Resch S. Molecular biology of S-layers. FEMS Microbiol. Rev. 1997;20:47–98. doi: 10.1111/j.1574-6976.1997.tb00304.x. [DOI] [PubMed] [Google Scholar]
- Bragg TS, Robertson DL. Nucleotide sequence and analysis of the lethal factor gene (lef) from Bacillus anthracis. Gene. 1989;81:45–54. doi: 10.1016/0378-1119(89)90335-1. [DOI] [PubMed] [Google Scholar]
- Candela T, Fouet A. Poly-gamma-glutamate in bacteria. Mol. Microbiol. 2006;60:1091–1098. doi: 10.1111/j.1365-2958.2006.05179.x. [DOI] [PubMed] [Google Scholar]
- Chand HS, Drysdale M, Lovchik J, Koehler TM, Lipscomb MF, Lyons CR. Discriminating virulence mechanisms among Bacillus anthracis strains by using a murine subcutaneous infection model. Infect. Immun. 2009;77:429–435. doi: 10.1128/IAI.00647-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier RJ, Young JA. Anthrax toxin. Annu. Rev. Cell Dev. Biol. 2003;19:45–70. doi: 10.1146/annurev.cellbio.19.111301.140655. [DOI] [PubMed] [Google Scholar]
- Dixon TC, Fadl AA, Koehler TM, Swanson JA, Hanna PC. Early Bacillus anthracis-macrophage interactions: intracellular survival survival and escape. Cell. Microbiol. 2000;2:453–463. doi: 10.1046/j.1462-5822.2000.00067.x. [DOI] [PubMed] [Google Scholar]
- Drysdale M, Heninger S, Hutt J, Chen Y, Lyons CR, Koehler TM. Capsule synthesis by Bacillus anthracis is required for dissemination in murine inhalation anthrax. EMBO J. 2005;24:221–227. doi: 10.1038/sj.emboj.7600495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabenstein JD. Vaccines: countering anthrax: vaccines and immunoglobulins. Clin. Infect. Dis. 2008;46:129–136. doi: 10.1086/523578. [DOI] [PubMed] [Google Scholar]
- Guidi-Rontani C, Levy M, Ohayon H, Mock M. Fate of germinated Bacillus anthracis spores in primary murine macrophages. Mol. Microbiol. 2001;42:931–938. doi: 10.1046/j.1365-2958.2001.02695.x. [DOI] [PubMed] [Google Scholar]
- Guidi-Rontani C, Weber-Levy M, Labruyere E, Mock M. Germination of Bacillus anthracis spores within alveolar macrophages. Mol. Microbiol. 1999;31:9–17. doi: 10.1046/j.1365-2958.1999.01137.x. [DOI] [PubMed] [Google Scholar]
- Heninger S, Drysdale M, Lovchik J, Hutt J, Lipscomb MF, Koehler TM, Lyons CR. Toxin-deficient mutants of Bacillus anthracis are lethal in a murine model for pulmonary anthrax. Infect. Immun. 2006;74:6067–6074. doi: 10.1128/IAI.00719-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirano T. At the heart of the chromosome: SMC proteins in action. Nat. Rev. Mol. Cell. Biol. 2006;7:311–322. doi: 10.1038/nrm1909. [DOI] [PubMed] [Google Scholar]
- Hoffmaster AR, Ravel J, Rasko DA, Chapman GD, Chute MD, Marston CK, De BK, Sacchi CT, Fitzgerald C, Mayer LW, Maiden MC, Priest FG, Barker M, Jiang L, Cer RZ, Rilstone J, Peterson SN, Weyant RS, Galloway DR, Read TD, Popovic T, Fraser CM. Identification of anthrax toxin genes in a Bacillus cereus associated with an illness resembling inhalation anthrax. Proc. Natl. Acad. Sci. USA. 2004;101:8449–8454. doi: 10.1073/pnas.0402414101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isberg RR. Discrimination between intracellular uptake and surface adhesion of bacterial pathogens. Science. 1991;252:934–938. doi: 10.1126/science.1674624. [DOI] [PubMed] [Google Scholar]
- Kern JW, Schneewind O. BslA, a pXO1-encoded adhesin of Bacillus anthracis. Mol. Microbiol. 2008;68:504–515. doi: 10.1111/j.1365-2958.2008.06169.x. [DOI] [PubMed] [Google Scholar]
- Koch R. Die Ätiologie der Milzbrand-Krankheit, begründet auf die Entwicklungsgeschichte des Bacillus anthracis. Beiträge zur Biologie der Pflanzen. 1876;2:277–310. [Google Scholar]
- Lee VT, Schneewind O. Type III machines of pathogenic yersiniae secrete virulence factors into the extracellular milieu. Mol. Microbiol. 1999;31:1619–1629. doi: 10.1046/j.1365-2958.1999.01270.x. [DOI] [PubMed] [Google Scholar]
- Leppla SH. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclin AMP concentrations in eukaryotic cells. Proc. Natl. Acad. Sci. USA. 1982;79:3162–3166. doi: 10.1073/pnas.79.10.3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little SF, Knudson GB. Comparative efficacy of Bacillus anthracis live spore vaccine and protective antigen vaccine against anthrax in the guinea pig. Infect. Immun. 1986;52:509–512. doi: 10.1128/iai.52.2.509-512.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraffini LA, Schneewind O. Targeting proteins to the cell wall of sporulating Bacillus anthracis. Mol. Microbiol. 2006;62:1402–1417. doi: 10.1111/j.1365-2958.2006.05469.x. [DOI] [PubMed] [Google Scholar]
- Mesnage S, Fontaine T, Mignot T, Delepierre M, Mock M, Fouet A. Bacterial SLH domain proteins are non-covalently anchored to the cell surface via a conserved mechanism involving wall polysaccharide pyruvylation. EMBO J. 2000;19:4473–4484. doi: 10.1093/emboj/19.17.4473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesnage S, Tosi-Couture E, Fouet A. Production and cell surface anchoring of functional fusions between the SLH motifs of the Bacillus anthracis S-layer proteins and the Bacillus subtilis levansucrase. Mol. Microbiol. 1999;31:927–936. doi: 10.1046/j.1365-2958.1999.01232.x. [DOI] [PubMed] [Google Scholar]
- Mesnage S, Tosi-Couture E, Gounon P, Mock M, Fouet A. The capsule and S-layer: two independent and yet compatible macromolecular structures in Bacillus anthracis. J. Bacteriol. 1998;180:52–58. doi: 10.1128/jb.180.1.52-58.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesnage S, Tosi-Couture E, Mock M, Gounon P, Fouet A. Molecular characterization of the Bacillus anthracis main S-layer component: evidence that it is the major cell-assoiated antigen. Mol. Microbiol. 1997;23:1147–1155. doi: 10.1046/j.1365-2958.1997.2941659.x. [DOI] [PubMed] [Google Scholar]
- Mock M, Fouet A. Anthrax. Annu. Rev. Microbiol. 2001;55:647–671. doi: 10.1146/annurev.micro.55.1.647. [DOI] [PubMed] [Google Scholar]
- Navarre WW, Schneewind O. Surface proteins of Gram-positive bacteria and the mechanisms of their targeting to the cell wall envelope. Microbiol. Mol. Biol. Rev. 1999;63:174–229. doi: 10.1128/mmbr.63.1.174-229.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okinaka R, Cloud K, Hampton O, Hoffmaster A, Hill K, Keim P, Koehler T, Lamke G, Kumano S, Manter D, Martinez Y, Ricke D, Svensson R, Jackson P. Sequence, assembly and analysis of pX01 and pX02. J. Appl. Microbiol. 1999a;87:261–262. doi: 10.1046/j.1365-2672.1999.00883.x. [DOI] [PubMed] [Google Scholar]
- Okinaka RT, Cloud K, Hampton O, Hoffmaster AR, Hill KK, Keim P, Koehler TM, Lamke G, Kumano S, Mahillon J, Manter D, Martinez Y, Ricke D, Svensson R, Jackson PJ. Sequence and organization of pXO1, the large Bacillus anthracis plasmid harboring the anthrax toxin genes. J. Bacteriol. 1999b;181:6509–6515. doi: 10.1128/jb.181.20.6509-6515.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasteur L. Le vaccin du charbon. Comptes Rendus Hebdomadaires des Scéances de l’Académie des Sciences. 1881;92:666–668. [Google Scholar]
- Pezard C, Berche P, Mock M. Contribution of individual toxin components to virulence of Bacillus anthracis. Infect. Immun. 1991;59:3472–3477. doi: 10.1128/iai.59.10.3472-3477.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preisz H. Experimentelle Studien über Virulenz, Empfänglichkeit und Immunität beim Milzbrand. Zeitschrift für Immunitäts-Forschung. 1909;5:341–452. [Google Scholar]
- Read TD, Peterson SN, Tourasse N, Baille LW, Paulsen IT, Nelson KE, Tettelin H, Fouts DE, Eisen JA, Gill SR, Holtzapple EK, Okstad OA, Helgason E, Rilstone J, Wu M, Kolonay JF, Beanan MJ, Dodson RJ, Brinkac LM, Gwinn M, DeBoy RT, Madpu R, Daugherty SC, Durkin AS, Haft DH, Nelson WC, Peterson JD, Pop M, Khouri HM, Radune D, Benton JL, Mahamoud Y, Jiang L, Hance IR, Weidman JF, Berry KJ, Plaut RD, Wolf AM, Watkins KL, Nierman WC, Hazen A, Cline RT, Redmond C, Thwaite JE, WHite O, Salzberg SL, Thomason B, Friedlander AM, Koehler TM, Hanna PC, Kolsto AB, Fraser CM. The genome sequence of Bacillus anthracis Ames and comparison to closely related bacteria. Nature. 2003;423:81–86. doi: 10.1038/nature01586. [DOI] [PubMed] [Google Scholar]
- Read TD, Salzberg SL, Pop M, Shumway M, Umayam L, Jiang L, Holtzapple E, Busch JD, Smith KL, Schupp JM, Solomon D, Keim P, Fraser CM. Comparative genome sequencing for discovery of novel polymorphisms in Bacillus anthracis. Science. 2002;296:2028–2033. doi: 10.1126/science.1071837. [DOI] [PubMed] [Google Scholar]
- Richter GS, Anderson VJ, Garufi G, Lu L, Joachimiak A, He C, Schneewind O, Missiakas D. Capsule anchoring in Bacillus anthracis occurs by a transpeptidation mechanism that is inhibited by capsidin. Mol. Microbiol. 2009;71:404–420. doi: 10.1111/j.1365-2958.2008.06533.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson DL, Leppla SH. Molecular cloning and expression in Escherichia coli of the lethal factor gene of Bacillus anthracis. Gene. 1986;44:71–78. doi: 10.1016/0378-1119(86)90044-2. [DOI] [PubMed] [Google Scholar]
- Ruthel G, Ribot WJ, Bavari S, Hoover T. Time-lapse confocal imaging of development of Bacillus anthracis in macrophages. J. Infect. Dis. 2004;189:1313–1316. doi: 10.1086/382656. [DOI] [PubMed] [Google Scholar]
- Singh Y, Ivins BE, Leppla SH. Study of immunization against anthrax with the purified recombinant protective antigen of Bacillus anthracis. Infect. Immun. 1998;66:347–348. doi: 10.1128/iai.66.7.3447-3448.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleytr UB. Basc and applied S-layer research: an overview. FEMS Microbiol. Rev. 1997;20:5–12. [Google Scholar]
- Smith H, Keppie J, Stanley JL. The chemical basis of the virulence of Bacillus anthracis. V. The specific toxin produced by Bacillus anthracis in vivo. Br. J. Exp. Pathol. 1955;36:460–472. [PMC free article] [PubMed] [Google Scholar]
- Sterne M. Avirulent anthrax vaccine. Onderstepoort J. Vet. Sci. Animal Ind. 1937;21:41–43. [PubMed] [Google Scholar]
- Vodkin MH, Leppla SH. Cloning of the protective antigen gene of Bacillus anthracis. Cell. 1983;34:693–697. doi: 10.1016/0092-8674(83)90402-6. [DOI] [PubMed] [Google Scholar]
- Welkos SL, Keener TJ, Gibbs PH. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect. Immun. 1986;51:795–800. doi: 10.1128/iai.51.3.795-800.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welkos SL, Trotter RW, Becker DM, Nelson GO. Resistance to the Sterne strain of B. anthracis: phagocytic cell responses of resistant and susceptible mice. Microb. Pathogen. 1989;7:15–35. doi: 10.1016/0882-4010(89)90108-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.