Abstract
Background
The relationship between the degree of glycaemic control and mortality remains an important topic of discussion.
Aim
This study aimed to investigate this relationship.
Design of study
Prospective cohort study.
Setting
Primary care.
Method
A total of 1145 patients with type 2 diabetes were enrolled in the Zwolle Outpatient Diabetes project Integrating Available Care (ZODIAC) in 1998. Their survival status was recorded in September 2004. Mortality ratios were calculated using standardised mortality ratios (SMRs). Associations between haemoglobin A1c (HbA1c) levels and mortality were studied with a Cox proportional hazard model. HbA1c levels were studied as continuous and as categorical variables.
Results
A total of 335 patients died after a median follow-up period of 5.8 years. The SMR (95% confidence interval [CI]) for total mortality was 1.86 (95% CI = 1.66 to 2.06) and 2.24 (95% CI = 1.91 to 2.61) for cardiovascular mortality. For each 1% increase in HbA1c there was a 21% increase in the hazard ratio for total mortality. When compared with the target HbA1c group (HbA1c 6.5–7%), the group with very poor glycaemic control (HbA1c >9%) had a hazard ratio of 2.21 (95% CI = 1.42 to 3.42) for total mortality. The group with normal glycaemic control (HbA1c <6.5%) had a hazard ratio of 1.00 (95% CI = 0.46 to 2.19) for total mortality.
Conclusion
HbA1c level was associated with mortality and this effect seemed largely attributable to patients who were in really poor glycaemic control. The absence of differences in mortality in the groups with lower HbA1c levels supports the position that there is no basis for continually decreasing the therapeutic target HbA1c level in patients with type 2 diabetes mellitus.
Keywords: blood glucose, mortality, type 2 diabetes mellitus
INTRODUCTION
Patients with type 2 diabetes mellitus have a two- to fivefold increase in risk for developing cardiovascular disease compared to people without diabetes.1,2 Between 50% and 75% of all deaths seen in patients with type 2 diabetes are related to cardiovascular complications.3 Since this excess risk is only partially explained by traditional risk factors, such as obesity, dyslipidaemia, and hypertension, type 2 diabetes is often considered an independent risk factor for cardiovascular morbidity and mortality.
A strong body of evidence links chronic hyperglycaemia to microvascular complications. A meta-analysis of observational studies suggests that hyperglycaemia is also associated with an increased risk for cardiovascular mortality in patients with type 2 diabetes.4 In the UK Prospective Diabetes Study (UKPDS), a continuous relationship was found between glycosylated haemoglobin (HbA1c) levels and rates of macrovascular complications. For every 1% decrease in HbA1c level, investigators estimated a 14% decrease in myocardial infarction, a 12% decrease in stroke, and a 14% reduction in all-cause mortality.5 Results from a meta-analysis of all the randomised trials in which glycaemic control and its relationship to macrovascular risk were studied in patients with both type 1 and type 2 diabetes, showed that glucose lowering itself reduces cardiovascular risk.6
Three recently performed studies have investigated the role of intensive glycaemic control.7–9 The Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial showed a significantly higher mortality rate in the intensive treatment group compared to the standard glucose-lowering therapy group.7 The two other trials, the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) trial and the Veterans Affairs Diabetes Trial (VADT), found no effect of intensive glycaemic control on the occurrence of major macrovascular events or all-cause mortality compared to the control group.8,9 The post-trial study from the UKPDS suggested that the effects on mortality of a more intensive strategy to control blood glucose levels in patients with newly diagnosed type 2 diabetes were sustained for up to 10 years after the cessation of randomised interventions.10 The major difference between the three recently performed studies and the post-trial study from the UKPDS is that in the UKPDS only patients with newly diagnosed type 2 diabetes were included.
In light of these results, the goal of this study was to investigate the relationship between glycaemic control (as indicated by HbA1c level) and mortality in patients with type 2 diabetes, in a prospective observational setting.
METHOD
In 1998, in the Zwolle region (the Netherlands), a large shared-care diabetes project was initiated, the Zwolle Outpatient Diabetes project Integrating Available Care (ZODIAC). In this project, GPs were assisted in their care of patients with type 2 diabetes by hospital-based nurses specialising in diabetes. As part of this project, the patients with type 2 diabetes in 32 primary care practices consulted (and still consult) these diabetes specialist nurses annually. Patients with a very short life expectancy (including patients with active cancer) or insufficient cognitive abilities were excluded. During the first year of the project, 1664 subjects with type 2 diabetes were identified in these practices. Patients being treated by specialists in internal medicine (n = 338) were excluded. Fifty-seven patients were excluded by their GPs due to an estimated very short life-expectancy or insufficient cognitive abilities. Of the 1269 patients who were invited to participate, 1149 (91%) agreed. Four patients were excluded due to insufficient baseline data. Details of the ZODIAC study have been published previously.11
How this fits in
Three recent randomised studies (the ACCORD, ADVANCE, and VADT trials) showed that a low haemoglobin A1c (HbA1c) target level does not result in decreased mortality. In this study, HbA1c was a significant predictor for mortality. This effect seems largely attributable to poor glycaemic control. The study data suggest that for patients with moderate glycaemic control, it may be better to focus on other risk factors than to keep on lowering the target values for HbA1c.
Baseline data were collected in 1998 and 1999 and involved a full medical history, including the presence or absence of macrovascular complications, medication use, and tobacco consumption. Laboratory and physical assessment data were collected on a yearly basis and included lipid profile, creatinine, (micro)albuminuria, blood pressure, weight, and height. HbA1c was measured first at baseline and annually thereafter. An updated mean of annually measured HbA1c was calculated for each individual from baseline to the end of the follow-up period. This is in accordance with the technique used in the UKPDS 35.5 For example, at 2 years the updated mean is calculated using the average of the baseline, 1-year, and 2-year values, and at 4 years, the updated mean is the average of the baseline, 1-year, 2-year, 3-year, and 4-year values.
Records maintained by the hospital and the GPs were used to obtain cause of death information for the patients who died during the study. The causes of death were coded according to The International Classification of Diseases, 9th Revision (ICD-9). To study the incidence of cardiovascular-related mortality, standardised mortality ratios (SMRs) were calculated using general mortality reference rates from the eastern part of the Netherlands.12 A Cox proportional hazard model was then used to assess the association between updated mean HbA1c levels and mortality (all-cause and cardiovascular). The updated mean value was included as a time-dependent covariate to evaluate glycaemic control during follow-up. Using updated mean HbA1c levels as a continuous variable, models were developed and applied to determine the all-cause mortality risk associated with a 1% reduction in the HbA1c level. Separate analyses were done for HbA1c as a grouped variable (<6.5%, 6.5–7%, 7–8%, 8–9%, and ≥9%), and the therapeutic target range for HbA1c (between 6.5% and 7%) was used as a reference. The following variables were included in the models as possible confounders: age, sex, smoking (never, previous, and current), duration of diabetes, creatinine, body mass index, systolic blood pressure, total cholesterol-HDL (high-density lipoprotein) ratio, macrovascular complications (yes/no), use of statins (yes/no), insulin use (yes/no), and albuminuria (yes/no).
RESULTS
The baseline characteristics of the study population are shown in Table 1. A total of 335 (31%) patients died during a median follow-up of 5.8 years. Date and cause of death could not be traced in 6 and 20 patients, respectively. Out of the 315 known causes of death, 51% (n = 161) were attributable to cardiovascular disease, 21% (n = 70) to malignancies, and 10% (n = 34) to respiratory diseases.
Table 1.
Baseline characteristics.
| Characteristics | Total (n = 1145) | Deceased patients (n = 335) | Patients that survived (n = 810) |
|---|---|---|---|
| Age, years | 68.7 (±11.5) | 76.5 (±8.7) | 65.5 (±11.0)a |
| Female, % | 54.3 | 58.8 | 57.5 |
| Diabetes duration, years | 7.7 (±7.5) | 9.2 (±8.5) | 7.1 (±7.0)a |
| Smoking, % | |||
| Never | 50.4 | 51.9 | 49.8 |
| Former smoker | 30.6 | 31.6 | 30.1 |
| Current smoker | 18.1 | 14.9 | 19.4 |
| BMI, kg/m2 | 28.9 (±4.8) | 28.3 (±5.0) | 29.2 (±4.7)b |
| Systolic blood pressure, mmHg | 155.1 (±25) | 154.0 (±27) | 154.3 (±24) |
| HbA1c, % | 7.5 (±1.3) | 7.6 (±1.3) | 7.5 (±1.2)c |
| Creatinine clearance, ml/min | 63.2 (±20.0) | 51.5 (±16.7) | 68.1 (±19.2)a |
| Total cholesterol/HDL ratio | 5.3 (±1.60) | 5.2 (±1.7) | 5.2 (±1.5) |
| LDL cholesterol, mmol/l | 3.4 (±1.0) | 3.3 (±1.0) | 3.4 (±1.0) |
| Statin use, % | 11.2 | 10.2 | 12.1 |
| Insulin use, % | 15.4 | 21.2 | 12.3a |
| Microalbuminuria, % | 41.8 | 55.3 | 36.6a |
| Macroalbuminuria, % | 5.5 | 7.9 | 4.5c |
| Macrovascular complications, % | 61.4 | 77.9 | 54.5a |
HDL = high-density lipoprotein. LDL = low-density lipoprotein. Data are means (± standard deviation) or %.
P<0.001.
P<0.01.
P<0.05.
The SMR (95% confidence interval [CI]) for total mortality was 1.86 (95% CI = 1.66 to 2.06) and 2.21 (95% CI = 1.42 to 3.42) for cardiovascular mortality.
The hazard ratio (HR) for the updated HbA1c mean (continuous variable) was 1.21 (95% CI = 1.07 to 1.36) for all-cause mortality.
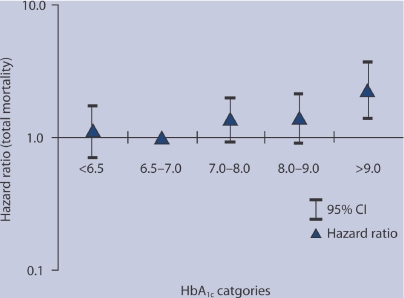
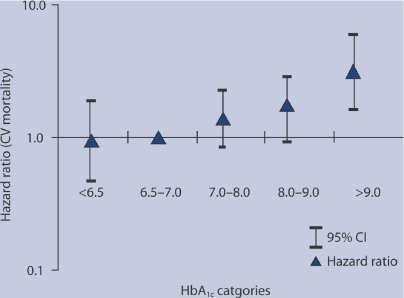
HRs for the updated HbA1c mean in the categories <6.5% (n = 228), 7–8% (n = 318), 8–9% (n = 208), and ≥9% (n = 144) were 1.11 (95% CI = 0.71 to 1.74), 1.40 (95% CI = 0.99 to 1.97), 1.43 (95% CI = 0.97 to 2.10), and 2.26 (95% CI = 1.39 to 3.67) respectively compared to HbA1c 6.5–7% (n = 245) for all-cause mortality (Figure 1). HRs for the updated HbA1c mean in the categories <6.5% (n = 228), 7–8% (n = 318), 8–9% (n = 208), and ≥9% (n = 144) were 0.94 (95% CI = 0.47 to 1.91), 1.40 (95% CI = 0.84 to 2.31), 1.71 (95% CI = 0.99 to 2.96), and 3.13 (95% CI = 1.62 to 6.05) respectively, compared to HbA1c 6.5–7% (n = 245) for cardiovascular mortality (Figure 2).
Figure 1.
Hazard ratio's for total mortality for five HbA1c categories, reference category is 6.5–7.0.
Figure 2.
Hazard ratio's for cardiovascular mortality for five HbA1c categories, reference category is 6.5–7.0.
DISCUSSION
Summary of main findings
HbA1c seems to be a predictor for mortality in type 2 diabetes mellitus, but whether this predictive value translates to causality is unknown. In the present study cohort, the increased mortality risk, corrected for risk factors including diabetes duration, seems largely attributable to those patients with poor glycaemic control.
Patients with an average HbA1c ≥9% have a 2.26 higher total mortality risk and a 3.13 higher cardiovascular mortality risk compared to the group with an HbA1c at the current therapeutic target level (6.5–7%). Patients with an average HbA1c <9% did not have significantly different risks for total and cardiovascular mortality. A HbA1c level <6.5% does not seem to change cardiovascular and all-cause mortality risks when compared with the normal target range of 6.5–7%.
There are several plausible physiological explanations for the effect of chronically elevated glucose levels on cardiovascular disease risk. Glucose can react with various proteins to form advanced glycation end-products, which may contribute to long-term complications of diabetes, plaque formation, and atherosclerosis. These effects are gradual and likely to be cumulative.13
Strengths and limitations of the study
Because of the observational nature of the study, the associations found do not imply causality. The study population itself presents other limitations. A patient population of 1145 is rather small. Second, it is comprised of patients treated in primary health care, and therefore might represent a population with less overall risk, since many subjects with more complicated disease will be treated in secondary care in the Netherlands. However, approximately 80% of the patients with type 2 diabetes are treated at the primary healthcare level, allowing the study conclusions to be applicable to a majority of patients with type 2 diabetes.
Comparison with existing literature
The results of this study agree with those reported in the ACCORD,7 ADVANCE,8 and VADT9 studies, that a low HbA1c therapeutic target level does not result in decreased mortality. In fact, in the ACCORD trial, increased mortality was seen in the intensive treatment group.7 It is possible that the use of multiple types of medications in an attempt to achieve normal blood glucose levels in patients with longstanding type 2 diabetes results in increased side-effects, and perhaps also increased mortality.
Implications for clinical practice
The results of this observational study show that there is not much difference in mortality risk, as long as HbA1c levels are below 9%. Postponing death is not the only treatment goal in patients with type 2 diabetes, and the prevention of microvascular complications with strict metabolic control should also be a priority. The study data suggest that, in order to increase the life expectancy in these patients, glycaemic control is important in patients with poor control (HbA1c >9%). For patients with moderate glycaemic control and longstanding diabetes, it may be better to focus on other risk factors, such as smoking, high blood pressure, and lipid profile disturbances, than to aim for increasingly lower therapeutic target values for HbA1c.
Ethics committee
The ZODIAC Study was approved by the medical ethics committee, (reference number 03.0316) and all patients provided informed consent.
Competing interests
The authors have stated that there are none.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Haffner SM, Lehto S, Ronnemaa T, et al. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339(4):229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 2.Saydah SH, Miret M, Sung J, et al. Postchallenge hyperglycemia and mortality in a national sample of US adults. Diabetes Care. 2001;24(8):1397–1402. doi: 10.2337/diacare.24.8.1397. [DOI] [PubMed] [Google Scholar]
- 3.Moss SE, Klein R, Klein BE. Cause-specific mortality in a population-based study of diabetes. Am J Public Health. 1991;81(9):1158–1162. doi: 10.2105/ajph.81.9.1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Selvin E, Marinopoulos S, Berkenblit G, et al. Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med. 2004;141(6):421–431. doi: 10.7326/0003-4819-141-6-200409210-00007. [DOI] [PubMed] [Google Scholar]
- 5.Stratton IM, Adler AI, Neil AW, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stettler C, Allemann S, Jüni P, et al. Glycemic control and macrovascular disease in types 1 and 2 diabetes mellitus: Meta-analysis of randomized trials. Am Heart J. 2006;152(1):27–38. doi: 10.1016/j.ahj.2005.09.015. [DOI] [PubMed] [Google Scholar]
- 7.Gerstein HC, Miller ME, Byington RP, et al. The Action to Control Cardiovascular Risk in Diabetes Study Group Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(22):2545–2559. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel A, MacMahon S, Chalmers J, et al. The ADVANCE Collaborative Group Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–2572. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 9.Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Eng J Med. 2009;360(2):129–139. doi: 10.1056/NEJMoa0808431. [DOI] [PubMed] [Google Scholar]
- 10.Holman RR, Paul SK, Bethel MA, et al. 10-Year follow-up of intensive glucose control in type 2 diabetes. N Eng J Med. 2008;359(15):1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 11.Ubink-Veltmaat LJ, Bilo HJG, Groenier KH, et al. Shared care with task delegation to nurses for type 2 diabetes, a prospective observational study. Neth J Med. 2005;63(3):103–110. [PubMed] [Google Scholar]
- 12. Data published by Statistics Netherlands. Humans and society. http://statline.cbs.nl/StatWeb/ (accessed 25 Sept 2009)
- 13.Sheetz MJ, King GL. Molecular understanding of hyperglycemia's adverse effects for diabetic complications. JAMA. 2002;288(20):2579–2588. doi: 10.1001/jama.288.20.2579. [DOI] [PubMed] [Google Scholar]