Abstract
Background
Immunisation coverage in New Zealand is lower than what is necessary to prevent large epidemics of pertussis. Primary care is where most immunisation delivery occurs. General practices vary in their structure and organisation, both in a general sense and specifically with respect to immunisation delivery.
Aim
To identify the structural and organisational characteristics of general practices associated with higher immunisation coverage and more timely immunisation delivery.
Design of study
A random sample of practices during 2005 and 2006.
Setting
General practices in the Auckland and Midland regions, with over-sampling of indigenous Maori governance practices.
Method
Practice immunisation coverage and timeliness were measured. Primary care practice characteristics relevant to immunisation delivery by the practice were described. Associations of these practice characteristics with higher practice immunisation coverage and more timely immunisation delivery were determined.
Results
A total of 124 (61%) of 205 eligible practices were recruited. A median (25th to 75th centile) of 71% (57–77%) of registered children at each practice were fully immunised, and 56% (40–64%) had no immunisation delay. In multivariate analyses, both practice immunisation coverage (P<0.001) and timeliness (P<0.001) decreased with increased social deprivation. After adjustment for socioeconomic deprivation, region, and governance, immunisation coverage and timeliness were better at practices that enrolled children at a younger age (coverage: P = 0.002; timeliness P = 0.007), used one of the four available practice management systems (coverage: P<0.001; timeliness: P = 0.006), and had no staff shortages (coverage: P = 0.027; timeliness: P = 0.021).
Conclusion
Practice immunisation coverage and timeliness vary widely in New Zealand. General organisational and structural aspects of general practices are key determinants of general practice immunisation delivery.
Keywords: delivery of health care, family practice, immunisation, primary health care
INTRODUCTION
Immunisation is the most cost-effective intervention modern medicine has to offer.1 To achieve the full benefits of immunisation, both high coverage and timely delivery of scheduled immunisations are necessary.
Immunisation coverage in New Zealand (NZ) is mediocre. In the 2005 national survey, only 77% of children at 2 years of age had received all scheduled childhood immunisations. Coverage for indigenous (Maori) and Pacific children is lower, despite the NZ Ministry of Health's goal of 95% for all.2 As a consequence, NZ continues to experience large epidemics of pertussis. The infant pertussis hospitalisation rate is three to six times higher than contemporary rates for Australia, England, and the US.3–6
Timeliness of delivery is as important as coverage. Delay in receipt of the first vaccine dose in the primary series is one of the strongest predictors of subsequent incomplete immunisation.7 Delay in receipt of any of the three infant doses of pertussis vaccine increases the risk of hospital admission with pertussis.8
Socioeconomic factors, healthcare system factors, and parental attitudes contribute to incomplete immunisation.9 Research to date in NZ on immunisation coverage has focused on the characteristics of the child, family, or household. Internationally, it is well recognised that health systems and their providers make significant contributions to gaining and maintaining high coverage.10,11 The identification of health system barriers has been an essential component of immunisation coverage improvements in Australia and the US.12,13
Most immunisation delivery occurs in primary care. While the attitude of healthcare providers is crucial to achieving maximal immunisation uptake, healthcare structural and organisation factors also determine immunisation delivery.14 Aspects that have been identified as important include record keeping and documentation, recall/reminder, and tracking systems and practice settings.15–17
The aim of this study was to determine the structural and organisation characteristics of general practices that are associated with higher immunisation coverage and more timely immunisation delivery.
METHOD
Study design and setting
Approval was obtained from the Ministry of Health Ethics Committee. General practices in two NZ regions (Auckland and Midland) were enrolled during 2005 and 2006. Approximately 50% of all NZ children aged 0 to 4 years reside in the study region.
A random sample of practices was recruited, with stratification by region and oversampling of Maori governance practices (these are independent Maori health providers that target services primarily towards Maori and have a Maori management and governance structure).18 There were 11 such Maori governance practices in Auckland and 50 in Midland.
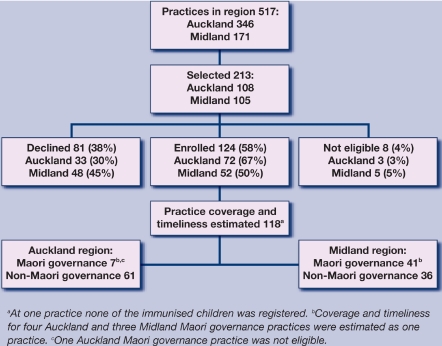
A total of 213 of the 517 practices in the study region were selected. In Auckland this included all Maori governance practices plus a random 29% of the non-Maori governance practices. In Midland it included a random sample of 62% of the Maori governance practices and 61% of non-Maori governance practices. From this sample it was possible to recruit 124 practices: 72 from Auckland and 52 from Midland.
Sample size estimates
A total of 124 practices was sufficient to yield 80% power to show statistical significance at the 5% level for a practice characteristic associated with higher coverage or more timely immunisation delivery. These calculations assumed the characteristic being examined had a frequency between 10% and 70% and was present in 20–25% more of the practices with higher coverage or better timeliness.
How this fits in
General practices are where most immunisation delivery occurs. Preventive health service delivery by practices requires appropriate structure and organisation. General organisational characteristics of practices (age when children registered, type of practice management system used, and stability of staffing) are key practice determinants of immunisation delivery. These areas, rather than more immunisation-specific factors, should be addressed first when seeking to improve general practice immunisation delivery.
Data collection and measurements
Practice immunisation coverage and timeliness were measured by electronic audit of the immunisation records for all children aged 6 weeks to 23 months. During this study the NZ immunisation schedule included a ‘6 week, 3 month, 5 month’ primary series of diphtheria, tetanus, pertussis (DTaP); polio; Haemophilus influenzae type b (Hib); and hepatitis B vaccines and; at age 15 months, measles, mumps, rubella vaccine plus a booster dose of DTaP and Hib vaccines.2
‘Practice structure and organisation’ was defined as those aspects of the practice that were independent of the characteristics of a specific GP or practice nurse, but were liable to influence the care they delivered when working within that practice. These characteristics were divided into those relevant to all aspects of primary healthcare delivery by the practice and those that were specific to immunisation delivery. For example, characteristics relevant to all aspects of primary care delivery include the age at which children being seen at the practice were registered with the practice and whether or not the practice had staff shortages (that is, unfilled positions for doctors, nurses, or other practice staff). In NZ, when this study was conducted, patients could be seen as casual patients at any practice. Registration with the practice indicated that the practice was the provider of this child's preventive health care and that the practice would maintain a record of the health care received by the child. Examples of characteristics specific to immunisation delivery include whether the practice had specific immunisation clinics and whether GPs at the practice sometimes gave immunisations.
The practice structure and organisation was described from a face-to-face interview with the practice manager, lead GP, or senior practice nurse. Practice population demographics (ethnicity and socioeconomic deprivation) were obtained from the Ministry of Health. Socioeconomic deprivation was measured using the NZDep2001 Index of Deprivation, a small area-based measure that combines nine variables from the 2001 Census that reflect aspects of household material and social deprivation, and is used to group NZ households into socioeconomic quintiles or deciles.19
Immunisation coverage was measured based on the child's age in relation to the immunisation schedule. For example, a child aged 10 weeks was fully immunised if they had received all of the immunisations scheduled to be given at age 6 weeks, and a child aged 6 months was fully immunised if they had received all of the immunisations scheduled to be given at age 6 weeks, 3 months, and 5 months.
Immunisation coverage was defined using the third dose assumption. If the third in a series of vaccine doses was recorded as given, then it was assumed that the previous doses had also been given.20 This assumption results in a small overestimate of coverage that is less than the underestimate that occurs if only recorded doses are counted.20
The Ministry of Health's National Immunisation Register definition of timeliness was used.21 An immunisation was defined as delayed if not received within 4 weeks of the first due date for the 6 week immunisations, and within 6 weeks for 3 month, 5 month, and 15 month immunisations.21
Data analysis
Immunisation coverage and timeliness were described for the children aged 6 weeks to 23 months registered at each practice. The proportion of children fully immunised and the proportion with no delayed immunisation were transformed to facilitate analysis using the arcsin of the square root of the variable. This transformation made the variance constant across the distribution of coverage and number of children at each practice. Examination was carried out for interaction with either region or practice governance for any of the variables associated with coverage. Variables for which such interaction was present were not included in the statistical models.
A general linear model was created with arcsin of the square root of the proportion immunised as the outcome variable. For the regression analyses a base model was created that included region, practice governance, socioeconomic deprivation, and the age, and age at registration, of the children as explanatory variables.
Additional explanatory variables that described practice structure and organisation were then added to this model. Practice structure and organisational variables were retained in the final models of coverage and timeliness if they increased the model's explanatory power or remained significantly associated with practice coverage or timeliness. Analyses were performed using SAS (version 9.1; SAS Institute, Cary, NC, US).
RESULTS
Practice recruitment
There were 517 practices in the study region. A total of 213 practices (41%) were randomly selected: 108 (31%) in Auckland and 105 (61%) in Midland. A small number of practices were ineligible, mainly because they did not provide Well-Child care. Thirty-nine per cent of selected practices declined to participate. The percentage of practices that declined was higher in Midland than Auckland (45% versus 30%, P = 0.015). Practices that declined to participate were smaller (mean number of registered patients 3644 versus 4339) and had a larger proportion of registered patients living in the most deprived quintile of households (26% versus 24%, P<0.001; see Figure 1).
Figure 1.
Summary of practice recruitment and enrolment.
Practice immunisation coverage and timeliness
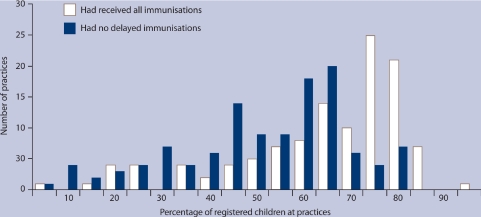
The median (25th to 75th centile) number of children aged 6 weeks to 23 months registered at each practice was 116 (62–193); with these registered children being 75% (64–88) of all children in this age group seen at each practice. A median (25th to 75th) percentage of 71% (57–77%) of the children registered at each practice were fully immunised and 56% (42–64%) were not delayed for any immunisations. The percentage of children registered at each practice that had received all immunisations and were not delayed varied widely (Figure 2). Practice immunisation coverage and timeliness were highly correlated (Spearman's rank correlation coefficient r = 0.77, P<0.001).
Figure 2.
Immunisation coverage and timeliness by practice.
Regional, governance, socioeconomic, and age-related factors
Practice immunisation coverage (P<0.001) and timeliness (P = 0.002) both decreased as the socioeconomic deprivation of the registered practice population increased (Table 1). Practice coverage was higher in Midland than Auckland (73% versus 68%, P = 0.004). Immunisation timeliness was lower at Maori governance practices versus non-Maori governance practices (P = 0.03). Younger age at registration was associated with higher immunisation coverage (P = 0.02) and more timely immunisation delivery (P = 0.02). Coverage decreased with increasing age of the child (P<0.001).
Table 1.
Associations of region, practice governance, socioeconomic deprivation, child's age, and child's registration age with practice immunisation coverage and timeliness.
| Immunisation coverage | Immunisation timeliness | |||||
|---|---|---|---|---|---|---|
| Practice characteristic (number of practices) | Median % (25th to 75th centile) | Univariate P-value | Multivariate P-valuea | Median % (25th to 75th centile) | Univariate P-value | Multivariate P-valuea |
| Region | ||||||
| Auckland (68) | 68 (53–75) | 0.020 | 0.004 | 55 (41–66) | 0.250 | 0.350 |
| Midland (50) | 73 (58–79) | |||||
| Practice governance | ||||||
| Maori (21) | 56 (44–62) | 0.006 | 0.110 | 40 (25–47) | 0.002 | 0.030 |
| Non-Maori (97) | 73 (63–79) | 59 (47–66) | ||||
| P-value adjusted for region and governance | P-value adjusted for region and governance | |||||
| % of registered patients in most deprived quintileb | ||||||
| <30% (86) | 74 (63–79) | <0.001 | <0.001 | 60 (47–66) | <0.001 | 0.002 |
| ≥30% (32) | 58 (35–65) | 42 (25–58) | ||||
| Median age of registered children at each practice | ||||||
| <13 months (48) | 73 (65–78) | 0.001 | <0.001 | 61 (54–66) | 0.001 | 0.560 |
| ≥13 months (70) | 64 (49–77) | 48 (34–63) | ||||
| Median age of children at registration | ||||||
| <3 months (72) | 74 (63–79) | 0.040 | 0.020 | 60 (46–66) | 0.140 | 0.020 |
| ≥3 months (46) | 63 (46–73) | 47 (35–62) | ||||
Adjusted for other variables in table with socioeconomic deprivation, age, and age at enrolment all entered into model as continuous variables.
Percentage in most socioeconomically deprived quintile included in model as a continuous variable. Socioeconomic deprivation measured using the NZDep2001 Index of Deprivation, a small area-based measure that combines nine variables from the 2001 Census that reflect aspects of material and social deprivation.19
Generic practice organisational features
Four different electronic practice management systems were used, with one system (Medtech32, 2008, Medtech Global Ltd, Auckland, NZ) being predominant (n = 89; 76%). After adjustment for region, governance, social deprivation, and age, immunisation coverage (P = 0.001) and timeliness (P = 0.01) were higher at practices that used Medtech32 (Table 2).
Table 2.
Associations of practice structure and organisation with practice immunisation coverage and timeliness.
| Coverage | Timeliness | |||||
|---|---|---|---|---|---|---|
| Practice characteristic (number of practices) | Median % received all immunisations (25–75th centile) | P-value adjusted for region and governance | P-value adjusted for region, governance, social deprivationa, age and age at registration | Median % with no delayed immunisations (25–75th centile) | P-value adjusted for region and governance | P-value adjusted for region, governance, social deprivationa, age, and age at registration |
| Generic practice factors | ||||||
| Practice management system used | ||||||
| Medtech32 (89) | 72 (62–78) | <0.001 | 0.001 | 59 (46–64) | <0.001 | 0.010 |
| Other (28) | 63 (44–76) | 42 (25–60) | ||||
| Staff shortages | ||||||
| Yes (76) | 67 (53–75) | 0.010 | 0.100 | 50 (37–63) | 0.007 | 0.040 |
| No (41) | 76 (65–79) | 61 (44–66) | ||||
| Practice charges for visits by registered patients | ||||||
| Yes (31) | 75 (70–82) | <0.001 | 0.200 | 49 (35–64) | 0.002 | 0.240 |
| No (86) | 65 (52–75) | 61 (57–64) | ||||
| Percentage of patients owing money to practice | ||||||
| >15% (43) | 62 (47–73) | <0.001 | 0.270 | 47 (32–62) | <0.001 | 0.180 |
| ≤15% (73) | 75 (65–80) | 60 (47–66) | ||||
| Immunisation-specific practice factors | ||||||
| Specified appointments or clinics for immunisation | ||||||
| Yes (40) | 69 (59–77) | 0.030 | 0.270 | 57 (43–64) | 0.050 | 0.430 |
| No (77) | 71 (57–77) | 55 (38–64) | ||||
| GPs sometimes give the immunisations | ||||||
| Yes (44) | 70 (64–79) | 0.110 | 0.580 | 60 (46–66) | 0.020 | 0.200 |
| No (73) | 70 (54–75) | 55 (32–62) | ||||
| Frequency of immunisation audit | ||||||
| At least monthly (32) | 72 (62–77) | 0.005 | 0.250 | 58 (47–62) | 0.070 | 0.900 |
| Less often (85) | 70 (56–77) | 51 (37–65) | ||||
Percentage in most socioeconomically deprived quintile included in model as a continuous variable. Socioeconomic deprivation measured using the NZDep2001 Index of Deprivation, a small area-based measure that combines nine variables from the 2001 Census that reflect aspects of material and social deprivation.19
Approximately two-thirds of practices (n = 76, 65%) experienced staff shortages, with such staffing issues being associated with less timely immunisation delivery (P = 0.04).
While all childhood immunisation visits were free, practice charges for other visits ranged from $0 to $30 for children <6-years old, and from $0 to >$60 for adults. The majority of practices were owed money by their registered patients. At 41 practices (35%) less than 5% of patients owed money, at 32 (28%) 5–15% owed money, and at 43 (37%) more than 15% of patients owed the practice money.
In univariate analyses both coverage and timeliness were higher at practices that charged for visits and at practices where 15% or less of patients owed money. These associations were no longer evident after adjustment for socioeconomic deprivation.
Immunisation-specific practice organisational features
Practices varied with respect to their immunisation-specific characteristics. One-third of practices (n = 40, 34%) had specific clinics or allocated appointments for immunisation. At 44 practices (38%), GPs sometimes gave immunisations. Immunisation audits were completed at least monthly at 32 (27%) practices. After adjustment for region, governance, socioeconomic deprivation, child's age, and age at registration, none of these immunisation-specific practice features were associated with coverage or timeliness. (Table 2).
Multivariate analysis of generic and immunisation-specific practice characteristics
Multivariate models describing the specific practice characteristics and their associations with practice immunisation coverage and timeliness were created by the addition of these variables to the base model described (region, practice governance, social deprivation, child's age, and age at registration). In this multivariate analysis, immunisation coverage varied by region (P = 0.002) and was lower in practices whose registered population was more socioeconomically deprived (P<0.001). Coverage was higher at practices where children were registered at a younger age (P = 0.002), used Medtech32 as their practice management system (P<0.001), or did not experience staff shortages (P = 0.027). Timeliness was lower at Maori governance practices (P = 0.020) and at practices whose registered population was more socioeconomically deprived (P<0.001). Timeliness was higher for practices with populations with younger children (P = 0.046), at practices where children were registered at a younger age (P = 0.007), at practices that used Medtech32 as their practice management system (P = 0.006), and at practices that did not experience staff shortages (P = 0.021; Table 3).
Table 3.
Multivariate analysis of practice structure and organisation factors and their associations with practice immunisation coverage and timeliness.
| Practice immunisation coveragea | Practice immunisation timelinessb | |||
|---|---|---|---|---|
| Coefficient (95% CIs) | P-value | Coefficient (95% CIs) | P-value | |
| Region | ||||
| Auckland | −0.091 (−0.147 to −0.036) | 0.002 | −0.029 (−0.083 to 0.026) | 0.31 |
| Midland | – | – | ||
| Practice governance | ||||
| Maori | −0.073 (−0.155 to 0.001) | 0.09 | −0.096 (−0.177 to −0.015) | 0.02 |
| Non-Maori | – | – | ||
| % of registered patients in most socioeconomically deprived quintilec | −0.003 (−0.004 to −0.001) | <0.001 | −0.003 (−0.003 to −0.003) | <0.001 |
| Median age of children at practice | −0.001 (−0.001 to 0.000) | 0.13 | 0.001 (0.000 to 0.001) | 0.046 |
| Median age of children at time of registration with practice | −0.001 (−0.002 to −0.001) | 0.002 | −0.001 (−0.001 to −0.001) | 0.007 |
| Practice management system used | ||||
| Medtech32 | 0.215 (0.105 to 0.324) | <0.001 | 0.154 (0.047 to 0.26) | 0.006 |
| Other | – | – | ||
| Practice experiences staff shortages | ||||
| Yes | −0.074 (−0.138 to −0.010) | 0.027 | −0.076 (−0.139 to −0.013) | 0.02 |
| No | – | – | ||
Data from 95 practices in multivariate model, r2 for model = 0.60.
Data from 95 practices in multivariate model, r2 for model = 0.45.
Socioeconomic deprivation measured using the NZDep2001 Index of Deprivation, a small area-based measure that combines nine variables from the 2001 Census that reflect aspects of material and social deprivation.19
DISCUSSION
Summary of main findings
Both immunisation coverage and timeliness varied widely in this sample of NZ general practices. Median percentages of children registered at each practice that were fully immunised (71%) and not delayed for any immunisations (56%) were both too low to realise the full health benefit from a national immunisation schedule.
In multivariate analyses, the practice structure and organisational factors associated with immunisation coverage and timeliness were similar. Socioeconomic deprivation of the enrolled practice population was a dominant factor in both multivariate models. For both coverage and timeliness, three practice characteristics were significant: younger age at registration, use of one of four available practice management systems, and not having staff shortages. None of the immunisation-specific practice factors explained any additional variance between practices in immunisation coverage or timeliness.
Strengths and limitations of the study
The immunisation audit was completed at each practice using computer programmes developed specifically for this purpose. Thus, an independent measure of practice immunisation delivery was obtained. For each practice this was a single point estimate and, therefore, less precise than one based on repeated measures, especially for smaller practices.22 Because of this, the regression analysis used a transformed dependent variable, with this transformation making the variance constant across the range of practices sizes.
The response rate among eligible practices was 61% and the final multivariate models of immunisation coverage and timeliness included only 95 (45%) of 213 invited practices. This project coincided with a national meningococcal immunisation strategy and a large practice accreditation process in Midland; both affected practices' ability to engage with this project. Practices struggling to cope with these competing issues may have been less likely to participate in this study. Such non-participation could in part explain the higher practice coverage in the Midland region.
Although oversampling of Maori governance practices added complexity to the data analysis, it did ensure the study included practices serving populations for whom immunisation coverage is lower.2 If Maori governance practices had not been actively recruited, the enrolment bias towards practices that served a less socioeconomically deprived population would have been greater. Thus the authors believe the study sampling strategy helped to include a broad spectrum of practices and hence increased the generalisability of the study findings to the study region.
Comparison with existing literature
Practice registration at a younger age increases the likelihood that the first doses of the primary immunisation series are delivered on time. Timely delivery of this first immunisation is one of the strongest predictors of subsequent completion of the immunisation series.7 National immunisation registers can aid the early enrolment of a child with the practice.23 NZ introduced a national immunisation register in 2005. The present study indicates that one priority for this register must be to facilitate early enrolment of newborn infants with their primary care provider. Early enrolment is likely to lead to a stronger relationship between the practice and family. This is of particular importance in NZ where perinatal primary care is fragmented. Primary health care during pregnancy and post-partum is delivered predominantly by midwives, and the timing of transition of infant care responsibility from midwife to GP varies.
To improve immunisation delivery practice, management systems need to have a functionality that extends beyond enabling the practice to claim reimbursement for immunisations given. The quality of data in the national immunisation register is dependent on the quality of data transferred from the practice management system. Practice management systems that are used to report immunisation data are not designed specifically for this purpose. Considerable variability was observed between the different practice management systems, in terms of staff competence and confidence with the system and the ease of access that practice staff had when technical support was required.24
As was found in this project, and as has been shown in other primary care practices in NZ, the quality of immunisation data that such systems report is variable.24,25 Practice management systems used in NZ have design features that can minimise data entry errors. However, currently, the systems enable users to alter these features, thus introducing practice-level variability in recording of immunisation data.
Preventive health service delivery is particularly vulnerable to staff shortages and high staff turnover. Understaffed practices do not have the time or the consistency of personnel to reflect upon their work and adopt a proactive rather than a reactive approach to service delivery issues. General practices in NZ do have a preventive service orientation, but there is variability in how well individual practices use their practice management systems to support immunisation delivery. Important aspects include office coordination of preventive services, a system to ensure all visits become preventive care opportunities, and regular performance monitoring.26
Staffing shortages may also reflect broader issues of organisational culture and practice leadership. They reflect how people work together, communicate, and resolve conflict within a general practice.26 Staff shortages are financially costly for a practice, with the resources spent on recruitment and training not available for service delivery.27
The socioeconomic deprivation of the practice population was a consistently strong determinant of practice immunisation delivery in both the coverage and timeliness models. Poverty and factors related to poverty are recognised as being among the more persistent barriers to immunisation.13,28 The significance of this for children living in poorer households is increased by such households also being places where exposure to vaccine-preventable disease is increased.29
The relationship between socioeconomic deprivation and practice immunisation delivery appears to be specific rather than a more general feature across all indicators of quality of primary care.30 This is probably a reflection of immunisation-specific issues. Examples of such issues include the necessity for multiple appointments to receive the complete immunisation series, and the contribution of missed immunisation opportunities that occur at acute illness visits.31,32 Children living in more socially deprived households have more frequent episodes of acute illness. Healthcare visits for such illnesses account for the majority of missed immunisation opportunities.32
Implications for clinical practice
Wide variability between primary care practices in preventive service delivery to children is acknowledged as a current weakness of primary care in the US.33 This study indicates that such variability is also a current weakness of primary care in NZ. Important practice characteristics include staffing levels and stability, practice orientation to preventive services, and adaptation to the population context in which preventive service delivery occurs.26 This study implies that these basic issues of primary care structure and organisation need to be addressed to obtain full return on immunisation-specific initiatives.
Funding body
This project was funded predominantly by the Health Research Council and the Ministry of Health Immunisation Research Strategy through the Health Research Council of New Zealand Partnership Programme. The project was also supported by two smaller grants (each for less than 10% of the project budget) received from GlaxoSmithKline and the Royal New Zealand College of General Practitioners. The Immunisation Research Strategy funded the employment of staff necessary to recruit participants, collect, manage, analyse, and report the data. The GlaxoSmithKline grant was used to pay staff involved in data collection. The Royal New Zealand College of General Practitioners grant was used to recompense enrolled practices for their time.
Ethical approval
Approval was obtained from the Ministry of Health Northern X Ethics Committee. AKX/04/09/265 ‘General practice and health professional determinants of immunisation coverage’.
Competing interests
Cameron C Grant completed a consultancy on rotavirus gastroenteritis for GlaxoSmithKline during 2005 and 2006. Nikki M Turner, Deon G York, Felicity Goodyear-Smith, and Helen A Petousis-Harris have no competing interests to declare. None of the authors has any financial interest in any of the practice management systems used by the practices enrolled in this study.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Plotkin SA, Orenstein WA. Vaccines. 4th edn. Philadelphia: Elsevier Inc; 2004. [Google Scholar]
- 2.Ministry of Health. Immunisation handbook 2006. Wellington: Ministry of Health; 2006. [Google Scholar]
- 3.Somerville RL, Grant CC, Grimwood K, et al. Infants hospitalised with pertussis: estimating the true disease burden. J Paediatr Child Health. 2007;43(9):617–622. doi: 10.1111/j.1440-1754.2007.01154.x. [DOI] [PubMed] [Google Scholar]
- 4.Elliott E, McIntyre P, Ridley G, et al. National study of infants hospitalised with pertussis in the acellular vaccine era. Pediatr Infect Dis J. 2004;23(3):246–252. doi: 10.1097/01.inf.0000116023.56344.46. [DOI] [PubMed] [Google Scholar]
- 5.Van Buynder PG, Owen D, Vurdien JE, et al. Bordetella pertussis surveillance in England and Wales: 1995–7. Epidemiol Infect. 1999;123(3):403–411. doi: 10.1017/s0950268899003052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tanaka M, Vitek CR, Pascual FB, et al. Trends in pertussis among infants in the United States, 1980–1999. JAMA. 2003;290(22):2968–2975. doi: 10.1001/jama.290.22.2968. [DOI] [PubMed] [Google Scholar]
- 7.Guyer B, Hughart N, Holt E, et al. Immunization coverage and its relationship to preventive health care visits among inner-city children in Baltimore. Pediatrics. 1994;94(1):53–58. [PubMed] [Google Scholar]
- 8.Grant CC, Roberts M, Scragg R, et al. Delayed immunisation and risk of pertussis in infants: unmatched case-control study. BMJ. 2003;326(7394):852–853. doi: 10.1136/bmj.326.7394.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bobo JK, Gale JL, Thapa PB, Wassilak SG. Risk factors for delayed immunization in a random sample of 1163 children from Oregon and Washington. Pediatrics. 1993;91(2):308–314. [PubMed] [Google Scholar]
- 10.Anonymous. Immunisation policy: recipes for success. Lancet. 1987;2(8550):78–80. [PubMed] [Google Scholar]
- 11.Nicoll A, Elliman D, Begg NT. Immunisation: causes of failure and strategies and tactics for success. BMJ. 1989;299(6703):808–812. doi: 10.1136/bmj.299.6703.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lister S, McIntyre PB, Burgess MA, O'Brien ED. Immunisation coverage in Australian children: a systematic review 1990–1998. Commun Dis Intell. 1999;23(6):145–170. [PubMed] [Google Scholar]
- 13.Anonymous. Strategies to sustain success in childhood immunizations. The National Vaccine Advisory Committee. JAMA. 1999;282(4):363–370. doi: 10.1001/jama.282.4.363. [DOI] [PubMed] [Google Scholar]
- 14.Gindler JS, Cutts FT, Barnett Antinori ME, et al. Successes and failures in vaccine delivery: evaluation of the immunization delivery system in Puerto Rico. Pediatrics. 1993;91(2):315–320. [PubMed] [Google Scholar]
- 15.Williams IT, Milton JD, Farrell JB, Graham NM. Interaction of socioeconomic status and provider practices as predictors of immunization coverage in Virginia children. Pediatrics. 1995;96(3 Pt 1):439–446. [PubMed] [Google Scholar]
- 16.Kimmel SR, Burns IT, Zimmerman RK. Addressing immunization barriers, benefits, and risks. J Fam Pract. 2003;52(1 Suppl):S47–55. [PubMed] [Google Scholar]
- 17.Sabnis SS, Pomeranz AJ, Lye PS, Amateau MM. Do missed opportunities stay missed? A 6-month follow-up of missed vaccine opportunities in inner city Milwaukee children. Pediatrics. 1998;101(5):E5. doi: 10.1542/peds.101.5.e5. [DOI] [PubMed] [Google Scholar]
- 18.Ministry of Health. Maori providers: primary health care delivered by doctors and nurses: The National Primary Medical Care Survey (NatMedCa): 2001/02 Report 3. Wellington: Ministry of Health; 2004. [Google Scholar]
- 19.Crampton P, Salmond C, Kirkpatrick R. Degrees of deprivation in New Zealand: an atlas of socioeconomic difference (2001 edition) Auckland: David Bateman Ltd; 2004. [Google Scholar]
- 20.Hull BP, Lawrence GL, MacIntyre CR, McIntyre PB. Estimating immunisation coverage: is the ‘third dose assumption’ still valid? Commun Dis Intell. 2003;27(3):357–361. [PubMed] [Google Scholar]
- 21.Ministry of Health. National immunisation register. http://www.moh.govt.nz/nir (accessed 27 Aug 2009)
- 22.Barker LE, Smith PJ, Gerzoff RB, et al. Ranking states' immunization coverage: an example from the National Immunization Survey. Stat Med. 2005;24(4):605–613. doi: 10.1002/sim.2039. [DOI] [PubMed] [Google Scholar]
- 23.Freeman VA, DeFriese GH. The challenge and potential of childhood immunization registries. Annu Rev Public Health. 2003;24:227–246. doi: 10.1146/annurev.publhealth.24.100901.140831. [DOI] [PubMed] [Google Scholar]
- 24.Goodyear-Smith F, Grant C, York D, et al. Determining immunisation coverage rates in primary health care practices: a simple goal but a complex task. Int J Med Inform. 2008;77(7):477–485. doi: 10.1016/j.ijmedinf.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 25.Poskitt N, Taft S. National Immunisation Register inaccuracies and duplications. NZ Med J. 2009;122(1288):113. [PubMed] [Google Scholar]
- 26.Randolph G, Fried B, Loeding L, et al. Organizational characteristics and preventive service delivery in private practices: a peek inside the ‘black box’ of private practices caring for children. Pediatrics. 2005;115(60):1704–1711. doi: 10.1542/peds.2004-1131. [DOI] [PubMed] [Google Scholar]
- 27.Waldman JD, Kelly F, Arora S, Smith HL. The shocking cost of turnover in health care. Health Care Manage Rev. 2004;29(1):2–7. doi: 10.1097/00004010-200401000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Lynch M. Effect of practice and patient population characteristics on the uptake of childhood immunizations. Br J Gen Pract. 1995;45(393):205–208. [PMC free article] [PubMed] [Google Scholar]
- 29.Singleton R, Holve S, Groom A, et al. Impact of immunizations on the disease burden of American Indian and Alaska native children. Arch Pediatr Adolesc Med. 2009;163(5):446–453. doi: 10.1001/archpediatrics.2009.44. [DOI] [PubMed] [Google Scholar]
- 30.Ashworth M, Seed P, Armstrong D, et al. The relationship between social deprivation and the quality of primary care: a national survey using indicators from the UK Quality and Outcomes Framework. Br J Gen Pract. 2007;57(539):441–448. [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen NJ, Lauderdale DS, Shete PB, et al. Physician knowledge of catch-up regimens and contraindications for childhood immunizations. Pediatrics. 2003;111(5 Pt 1):925–932. doi: 10.1542/peds.111.5.925. [DOI] [PubMed] [Google Scholar]
- 32.Turner N, Grant C, Goodyear-Smith F, Petousis-Harris H. Seize the moments: missed opportunities to immunize at the family practice level. Fam Pract. 2009;26(4):275–278. doi: 10.1093/fampra/cmp028. [DOI] [PubMed] [Google Scholar]
- 33.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington, DC: Institute of Medicine; 2001. [PubMed] [Google Scholar]