Abstract
Background
Smoking represents the most important cause of avoidable morbidity and mortality in the economically developed world. The UK has recently introduced a range of initiatives aiming to reduce smoking prevalence and smoking-related health inequalities.
Aim
To investigate the epidemiology of smoking in UK general practice.
Design of study
Cross-sectional study.
Setting
A total of 525 general practices contributing to the QRESEARCH database.
Method
A dataset was extracted on 2.7 million patients around each financial year for the period 2001–2007, including, age, sex, deprivation, and smoking status. For patients newly recorded as smoking, data were extracted on receipt of smoking cessation advice and referral to stop-smoking services.
Results
Over the study period, the proportion of people with smoking status recorded increased by 32.9% (2001/2002: 46.6% to 2006/2007: 79.5%). A large overall increase in the provision of smoking cessation advice (2001/2002: 43.6% to 2006/2007: 84.0%) and referral to stop-smoking services (2001/2002: 1.0% to 2006/2007: 6.6%) was also observed. The proportion of people who smoked (with a recorded smoking status) reduced by 6.0% (2001/2002: 28.4% to 2006/2007: 22.4%). This decrease was greatest among patients in the most deprived areas (7.2%) and the youngest patients (16–25 years: 7.1%). In 2006/2007, more than twice as many patients in deprived areas smoked as those in affluent areas (most deprived: 33.8%; most affluent: 14.1%).
Conclusion
A significant and important reduction in the number of UK smokers occurred between April 2001 and April 2007. However, although this is an improvement, comparatively high rates of smoking remain among younger adults and those who are the most socioeconomically deprived.
Keywords: epidemiology, general practice, QRESEARCH, smoking, socioeconomic status
INTRODUCTION
In 1972, almost half of the UK adult population was found to smoke. Over the next two decades, this reduced dramatically to less than one-third. However, in the 1990s the decline in the rate of smoking slowed.1 The White Paper on tobacco, Smoking Kills,2 and the command paper, The NHS Plan: a plan for investment, a plan for reform,3 published in 1998 and 2000 respectively, highlighted that smoking was the principal avoidable cause of premature death in the UK, and drew attention to the fact that the most vulnerable in society were most likely to suffer from the adverse effects of smoking.
The government's multifaceted plans (introduced in 1999) to reduce smoking included a £50 million (€60 million) publicity campaign to shift attitudes and change behaviour; a substantial increase in tax to reduce the affordability of smoking; a £35 million (€42 million) investment in customs to reduce tobacco smuggling; and a £60 million (€72 million) smoking cessation service provided by the NHS. This latter initiative included the introduction of prescribing of nicotine replacement therapy and other smoking cessation treatments, and an increase in specialist cessation services for the most heavily dependent smokers. A European-wide banning of smoking advertising was endorsed, and the Tobacco Advertising and Promotion Act 2002 passed to create a timetable for the ban on tobacco advertising and sponsorship, such that by 31 July 2005 most tobacco advertising and sponsorship would cease.
In April 2004, a quality-based General Medical Services (GMS) contract was introduced into UK primary care.4 This new contract reduced the proportion of income GPs derived from per capita payments and increased the proportion derived from the recording of patient information (usually onto electronic patient records) and implementation of good quality of care. An average practice could be paid £1371 (€1577) if smoking status was recorded in at least 75% of registered patients aged 15–75 years. Further income (a mean of £8724; €10 033 per practice) could be generated if smoking status was recorded in patients with chronic diseases (such as diabetes or coronary heart disease), and smoking cessation support was provided to patients who smoked (assuming a payment of £124.60; €143.30 per quality outcome framework point). The introduction of these figures meant that by 2006, the UK was considered to be the second most effective country in the European Union (behind the Republic of Ireland) for implementing tobacco control policies.5
The current government has repeatedly acknowledged the wide gap between health needs and service delivery, and highlighted that the reduction in the socioeconomic gradient in smoking is probably the single most effective thing government can do to reduce inequalities in health. This has led to the targeting of resources towards the reduction of these socioeconomic health inequalities.6 Thus, commissioners and providers of health care are, for example, now assessed in relation to the extent to which they are successful in reducing smoking inequalities.7
Large electronic national healthcare datasets, with their key strengths of large numbers and representative data, can offer an important method for monitoring trends in smoking and also provide important insights into the impact of the new GMS contract. With individual patient-level data available, inequalities between different groups of patients can also be determined. Building on previous work with the Information Centre for Health and Social Care,8–12 this study sought to confirm the recent acceleration in smoking reduction found using survey data,1 and also describe the recording of smoking status, provision of smoking advice, and referral to specialist stop-smoking services in patients registered in primary care in the UK. It also aimed to investigate whether these trends differed between sex, age, and deprivation groups.
How this fits in
The UK has recently introduced initiatives aiming to reduce smoking prevalence and smoking-related health inequalities. A significant and important increase in the recording of smoking status and issuing of smoking cessation advice by general practice in the UK occurred between April 2001 and April 2007. There was also a reduction in the proportion of people found to smoke. However, comparatively high rates of smoking remain among younger adults and those who are the most socioeconomically deprived. There is a continued need to focus greater resources and efforts on targeting the prevention of smoking uptake in children and adolescents and providing more resources for smoking cessation services aimed at younger and socioeconomically-deprived adults.
METHOD
Version 10 of the QRESEARCH database was used for this analysis. This database contains representative anonymised aggregated health data derived from 525 general practices. Although these practices are self-selected, they are broadly representative of primary care practices in the UK.13 Data were extracted for the period 1 April 2001 (2 708 917 patients) to 1 April 2007 (2 708 867 patients). The same practices were used throughout the study period. These data were used in the published report: A Summary of Public Health Indicators using Electronic Data from Primary Care,9 and are freely available in aggregate form from the QRESEARCH website.14 The methods used to collect primary care data for the QRESEARCH database have been previously described.8
In the UK the majority of individuals resident (including children) are registered with primary care, which is free at the point of contact. Patients were included if they were registered on 1 April each year and were registered for the preceding 12 months and aged 16 years or over. For simplicity, the financial year April 2001 to April 2002 is represented as 2001/2002 and April 2006 to April 2007 as 2006/2007. Those with incomplete data (temporary residents, newly registered patients, and those who joined, left, or died during the study year) were excluded.
Smokers were defined as the proportion of patients with smoking status code (Read Code: 137 and below) in the last 5 years recorded as a current smoker (in the year of study). To estimate the actual number of people who smoked in the UK, the data were scaled up, using the UK 2001 Census and mid-year population estimates.15 For patients who had been recorded as smokers in the previous 12 months researchers determined the in-house smoking cessation advice provided (Read Codes: 6791, 67A3, 8B2B, 8CAL, 8HTK, 13p., 9OO., 9N4M, 9N2k, 8H7i, 67H1, 8B3Y, 8B3f) and referral to a stop-smoking specialist (Read Codes: 8H7i and 8HTK). Socioeconomic deprivation was defined on the basis of the Townsend score associated with the output area of the patient's postcode. The Townsend score is a composite score based on unemployment, overcrowding, lack of car ownership, and non-owner occupancy. Higher scores indicate greater levels of socioeconomic deprivation. The cut-offs for the quintiles are based on the national distribution of Townsend scores derived from the UK 2001 Census.
Statistical methods
The χ2 test was used to compare categorical variables in different groups of patients. The Mantel-Haenszel χ2 test was used to investigate trends over time, this analysis being undertaken using Epi Info2000 (Centers for Disease Control and Prevention, Atlanta, US). Where appropriate, 95% confidence intervals (95% CIs) are reported.
RESULTS
Smoking status recording
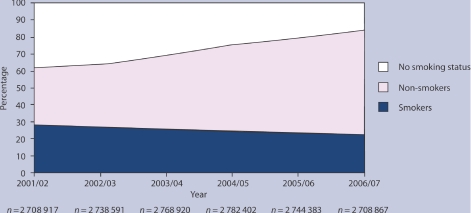
In 2001/2002, women and people living in more deprived socioeconomic areas were most likely to have smoking status recorded (P<0.001; online Table 1). In 2006/2007, sex differences persisted, but no socioeconomic differences were apparent (Table 1). From 2001/2002 to 2006/2007, there was a highly significant increase in the recording of smoking status in all patients (P<0.001; Figure 1), but most particularly in the oldest group of patients (Table 1), such that by 2006/2007, the oldest age group had the highest proportion of patients with a smoking status recorded (Table 1).
Table 1.
Patients aged >15 years with smoking status recorded.
| 2001/2002 | 2006/2007 | ||||
|---|---|---|---|---|---|
| n (total n) | % (95% CI) | n (total n) | % (95% CI) | % change 2001–2007 | |
| All patients | 1 263 496 (2 708 917) | 46.64 (46.58 to 46.70) | 2 154 658 (2 708 867) | 79.54 (79.49 to 79.59) | 32.90 |
| Sex | |||||
| Female | 726 917 (1 374 252) | 52.90 (52.81 to 52.98) | 1 176 377 (1 367 817) | 86.00 (85.95 to 86.06) | 33.10 |
| Male | 536 579 (1 334 665) | 40.20 (40.12 to 40.29) | 978 281 (1 341 050) | 72.95 (72.87 to 73.02) | 32.75 |
| Age-band, years | |||||
| 16–24 | 129 809 (331 782) | 39.12 (38.96 to 39.29) | 243 516 (349 400) | 69.70 (69.54 to 69.85) | 30.58 |
| 25–34 | 241 662 (450 280) | 53.67 (53.52 to 53.81) | 322 694 (412 811) | 78.17 (78.04 to 78.30) | 24.50 |
| 35–44 | 241 387 (529 104) | 45.62 (45.49 to 45.76) | 390 805 (523 909) | 74.59 (74.48 to 74.71) | 28.97 |
| 45–54 | 195 069 (441 617) | 44.17 (44.03 to 44.32) | 347 819 (450 530) | 77.20 (77.08 to 77.32) | 33.03 |
| 55–64 | 186 339 (389 128) | 47.89 (47.73 to 48.04) | 340 240 (408 567) | 83.28 (83.16 to 83.39) | 35.39 |
| 65–74 | 144 796 (288 339) | 50.22 (50.03 to 50.40) | 255 073 (283 923) | 89.84 (89.73 to 89.95) | 39.62 |
| ≥75 | 124 434 (278 667) | 44.65 (44.47 to 44.84) | 254 511 (279 727) | 90.99 (90.88 to 91.09) | 46.34 |
| Socioeconomic statusa | |||||
| Quintile 1 | 276 107 (607 528) | 45.45 (45.32 to 45.57) | 489 931 (612 866) | 79.94 (79.84 to 80.04) | 34.49 |
| Quintile 2 | 247 693 (539 442) | 45.92 (45.78 to 46.05) | 435 846 (544 339) | 80.07 (79.96 to 80.17) | 34.15 |
| Quintile 3 | 236 964 (506 448) | 46.79 (46.65 to 46.93) | 412 719 (513 362) | 80.40 (80.29 to 80.50) | 33.61 |
| Quintile 4 | 224 884 (463 323) | 48.54 (48.39 to 48.68) | 375 533 (467 692) | 80.29 (80.18 to 80.41) | 31.75 |
| Quintile 5 | 236 925 (476 786) | 49.69 (49.55 to 49.83) | 395 645 (496 427) | 79.70 (79.59 to 79.81) | 30.01 |
Higher quintiles indicate areas of greater socioeconomic deprivation.
Figure 1.
Proportion of smokers, non-smokers, and patients with no smoking status recorded (2001–2007).
Smoking rates
In both 2001/2002 and 2006/2007, the higher rates of smoking were found among males, younger patients, and those in the most deprived areas who had more than twice the rate of smoking than the most affluent patients (P<0.001; Table 2). In 2006/2007, the highest prevalence of smoking was found among men aged 35–44 years who were in the most deprived group (44.6%; 95% CI = 44.1 to 45.1; n = 16 720 of 37 495). There was a decrease over the study period in the proportion of people recorded as smokers (P<0.001; Figure 1). This was most apparent in the youngest patients and those who lived in the most deprived areas (Table 2).
Table 2.
Patients aged >15 years with smoking status recorded as smokers.
| 2001/2002 | 2006/2007 | ||||
|---|---|---|---|---|---|
| n (total n) | % (95% CI) | n (total n) | % (95% CI) | % change 2001–2007 | |
| All patients | 358 956 (1 263 496) | 28.41 (28.33 to 28.49) | 483 239 (2 154 658) | 22.43 (22.37 to 22.48) | −5.98 |
| Sex | |||||
| Female | 190 219 (726 917) | 26.17 (26.07 to 26.27) | 235 614 (1 176 377) | 20.03 (19.96 to 20.10) | −6.14 |
| Male | 168 737 (536 579) | 31.45 (31.32 to 31.57) | 247 625 (978 281) | 25.31 (25.23 to 25.40) | −6.14 |
| Age-band, years | |||||
| 16–24 | 43 089 (129 809) | 33.19 (32.94 to 33.45) | 63 565 (243 516) | 26.10 (25.93 to 26.28) | −7.09 |
| 25–34 | 86 209 (241 662) | 35.67 (35.48 to 35.86) | 99 748 (322 694) | 30.91 (30.75 to 31.07) | −4.76 |
| 35–44 | 76 722 (241 387) | 31.78 (31.60 to 31.97) | 107 714 (390 805) | 27.56 (27.42 to 27.70) | −4.22 |
| 45–54 | 60 954 (195 069) | 31.25 (31.04 to 31.45) | 87 310 (347 819) | 25.10 (24.96 to 25.25) | −6.15 |
| 55–64 | 49 122 (186 339) | 26.36 (26.16 to 26.56) | 69 307 (340 240) | 20.37 (20.23 to 20.51) | −5.99 |
| 65–74 | 27 551 (144 796) | 19.03 (18.83 to 19.23) | 35 608 (255 073) | 13.96 (13.83 to 14.09) | −5.07 |
| ≥75 | 15 309 (124 434) | 12.30 (12.12 to 12.49) | 19 987 (254 511) | 7.85 (7.75 to 7.96) | −4.45 |
| Socioeconomic statusa | |||||
| Quintile 1 | 51 861 (276 107) | 18.78 (18.64 to 18.93) | 69 242 (489 931) | 14.13 (14.04 to 14.23) | −4.65 |
| Quintile 2 | 55 252 (247 693) | 22.31 (22.14 to 22.47) | 75 370 (435 846) | 17.29 (17.18 to 17.41) | −5.02 |
| Quintile 3 | 65 491 (236 964) | 27.64 (27.46 to 27.82) | 90 364 (412 719) | 21.89 (21.77 to 22.02) | −5.70 |
| Quintile 4 | 76 279 (224 884) | 33.92 (33.72 to 34.11) | 104 718 (375 533) | 27.89 (27.74 to 28.03) | −6.03 |
| Quintile 5 | 97 221 (236 925) | 41.03 (40.84 to 41.23) | 133 806 (395 645) | 33.82 (33.67 to 33.97) | −7.21 |
Higher quintiles indicate areas of greater socioeconomic deprivation.
Based on the rates of smoking among patients registered to QRESEARCH practices, the estimated number of adult smokers in the UK in 2006/2007 was 13 676 782 (95% CI = 13 640 197 to 13 707 270).
Smoking cessation advice and referral to stop-smoking specialists
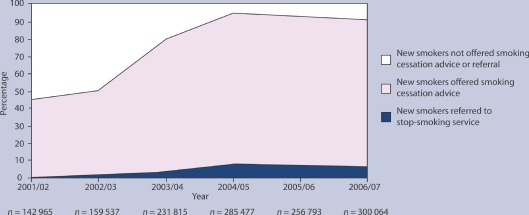
In 2001/2002, male, older, and patients in deprived areas (who had been recorded as smokers in the last 12 months) received the most smoking cessation advice (P<0.001; Table 3). However, although age differences persisted in 2006/2007, more women than men, and similar proportions from the most affluent and most deprived groups, were provided with smoking cessation advice (Table 3). In 2001/2002, patients in deprived areas were more likely to be referred to a specialist stop-smoking service (P<0.001; Table 4). In 2006/2007, those older patients and those living in the most deprived areas were most likely to be referred (Table 4). Between 2001/2002 and 2006/2007 there was a substantial increase in the proportion of newly recorded smokers offered smoking cessation advice (P<0.001; Figure 2), particularly among the oldest patients (Table 3). Large increases in the number of patients referred to a specialist stop-smoking service were also found (P<0.001; Figure 2), most particularly among older patients and those in the most deprived areas (Table 4).
Table 3.
Patients aged >15 years recorded as smokers in the last 12 months who were provided with smoking cessation advice from primary care.
| 2001/2002 | 2006/2007 | ||||
|---|---|---|---|---|---|
| n (total n) | % (95% CI) | n (total n) | % (95% CI) | % change 2001–2007 | |
| All patients | 62 393 (142 695) | 43.64 (43.39 to 43.90) | 252 042 (300 064) | 84.00 (83.87 to 84.13) | 40.36 |
| Sex | |||||
| Female | 37 441 (87 176) | 42.95 (42.62 to 43.28) | 138 328 (162 614) | 85.07 (84.89 to 85.24) | 42.12 |
| Male | 24 952 (55 789) | 44.73 (44.31 to 45.14) | 113 714 (137 450) | 82.73 (82.53 to 82.93) | 38.00 |
| Age-band, years | |||||
| 16–24 | 7 644 (19 307) | 39.59 (38.90 to 40.28) | 31 554 (38 358) | 82.26 (81.88 to 82.64) | 42.67 |
| 25–34 | 11 833 (28 154) | 42.03 (41.45 to 42.61) | 41 401 (51 078) | 81.05 (80.71 to 81.39) | 39.02 |
| 35–44 | 11 428 (25 859) | 44.19 (43.59 to 44.80) | 48 613 (59 697) | 81.43 (81.12 to 81.74) | 37.24 |
| 45–54 | 11 039 (24 452) | 45.15 (44.52 to 45.77) | 45 020 (53 541) | 84.09 (83.78 to 84.39) | 38.94 |
| 55–64 | 10 772 (22 973) | 46.89 (46.24 to 47.54) | 43 054 (49 556) | 86.88 (86.58 to 87.18) | 39.99 |
| 65–74 | 6852 (14 551) | 47.09 (46.28 to 47.90) | 26 886 (30 197) | 89.03 (88.68 to 89.39) | 41.94 |
| ≥75 | 2825 (7 669) | 36.84 (35.76 to 37.92) | 15 514 (17 637) | 87.96 (87.48 to 88.44) | 51.12 |
| Socioeconomic statusa | |||||
| Quintile 1 | 8943 (20 885) | 42.82 (42.15 to 43.49) | 36 219 (43 492) | 83.27 (82.93 to 83.63) | 40.45 |
| Quintile 2 | 9726 (22 646) | 42.95 (42.30 to 43.59) | 39 586 (47 273) | 83.74 (83.41 to 84.07) | 40.79 |
| Quintile 3 | 11 430 (26 699) | 42.81 (42.21 to 43.40) | 47 559 (56 809) | 83.71 (83.41 to 84.02) | 40.90 |
| Quintile 4 | 13 449 (30 386) | 44.26 (43.70 to 44.82) | 54 600 (64 663) | 84.44 (84.16 to 84.72) | 40.18 |
| Quintile 5 | 16 819 (37 278) | 45.12 (44.61 to 45.62) | 68 516 (81 598) | 83.97 (83.72 to 84.22) | 38.85 |
Higher quintiles indicate areas of greater socioeconomic deprivation.
Table 4.
Patients aged >15 years recorded as smokers in the last 12 months who were referred to a stop-smoking service in the last 12 months.
| 2001/2002 | 2006/2007 | ||||
|---|---|---|---|---|---|
| n (total n) | % (95% CI) | n (total n) | % (95% CI) | % change 2001–2007 | |
| All patients | 1360 (142 965) | 0.95 (0.91 to 1.00) | 19 699 (300 064) | 6.56 (6.48 to 6.65) | 5.61 |
| Sex | |||||
| Female | 858 (87 176) | 0.98 (0.92 to 1.05) | 10 624 (162 614) | 6.53 (6.41 to 6.65) | 5.55 |
| Male | 502 (55 789) | 0.90 (0.82 to 0.98) | 9075 (137 450) | 6.60 (6.47 to 6.73) | 5.70 |
| Age-band, years | |||||
| 16–24 | 109 (19 307) | 0.56 (0.46 to 0.67) | 1875 (38 358) | 4.89 (4.67 to 5.10) | 4.33 |
| 25–34 | 250 (28 154) | 0.89 (0.78 to 1.00) | 3042 (51 078) | 5.96 (5.75 to 6.16) | 5.07 |
| 35–44 | 302 (25 859) | 1.17 (1.04 to 1.30) | 3932 (59 697) | 6.59 (6.39 to 6.79) | 5.42 |
| 45–54 | 299 (24 452) | 1.22 (1.09 to 1.36) | 3880 (53 541) | 7.25 (7.03 to 7.47) | 6.03 |
| 55–64 | 236 (22 973) | 1.03 (0.90 to 1.16) | 3694 (49 556) | 7.45 (7.22 to 7.69) | 6.42 |
| 65–74 | 130 (14 551) | 0.89 (0.74 to 1.04) | 2332 (30 197) | 7.72 (7.42 to 8.02) | 6.83 |
| ≥75 | 34 (7 669) | 0.44 (0.29 to 0.59) | 944 (17 637) | 5.35 (5.02 to 5.68) | 4.91 |
| Socioeconomic statusa | |||||
| Quintile 1 | 108 (20 885) | 0.52 (0.43 to 0.61) | 2282 (43 492) | 5.25 (5.04 to 5.46) | 4.73 |
| Quintile 2 | 119 (22 646) | 0.53 (0.43 to 0.62) | 2559 (47 273) | 5.41 (5.21 to 5.62) | 4.88 |
| Quintile 3 | 160 (26 699) | 0.60 (0.51 to 0.69) | 3380 (56 809) | 5.95 (5.76 to 6.14) | 5.35 |
| Quintile 4 | 248 (30 386) | 0.82 (0.72 to 0.92) | 4255 (64 663) | 6.58 (6.39 to 6.78) | 5.76 |
| Quintile 5 | 723 (37 278) | 1.94 (1.80 to 2.08) | 6984 (81 598) | 8.56 (8.37 to 8.75) | 6.62 |
Higher quintiles indicate areas of greater socioeconomic deprivation.
Figure 2.
Proportion of new smokers (recorded in the previous 12 months) given smoking cessation advice or referred to stop-smoking service (2001–2007).
DISCUSSION
Summary of main findings
This study, using routinely collected electronic data from one of the world's largest national datasets, found a significant decline in the rate of smoking from 2001 to 2007. Over the study period, increases occurred in the provision of smoking cessation advice to smokers and referral to specialist services. However, high rates of smoking continued among younger adults and those in the most socioeconomically deprived areas in the UK. Overall, the numbers of smokers in the UK in 2007 was estimated at 13.7 million.
Strengths and limitations of the study
The main strengths of this study include the interrogation of an extremely large nationally representative dataset and the use of data from primary care practices, where the majority of services are free at the point of care and the majority of people in the UK are registered. Also, all contributing practices are accustomed to electronically recording routine data and use the same computing system.
There are a number of limitations related to the use of routinely collected data from primary care, including improvements in recording over the study time period and a lack of any direct validation of smoking status in the QRESEARCH database. It is possible that decreases in the proportion of people found to smoke could be overestimated, due to a larger number of non-smokers being recorded over time. Similarly, it is possible that increases in the provision of smoking cessation advice and referral could be underestimated, if in the past only new smokers who were referred or given advice were recorded by general practice as opposed to any newly recorded smokers. It is also possible that the number of non-smokers has been underestimated. This may be as a result of the increasing numbers of smokers being referred to smoking cessation programmes, with some of these patients giving up in the short term, being recorded as non-smokers and then reverting back to smoking without being recorded as such. It is likely though that smoking status (where recorded) is accurate,16 and routine visits to practices by quality assurance and appraisal teams help to ensure the accuracy of practice-held electronic data that are relevant to the Quality and Outcomes Framework.17
Univariate analyses were carried out, and therefore it is possible that although trends over time are likely to be real, differences between groups of patients could be explained by demographic or comorbidity variations across the study period. The observational nature of this study also means that it is not possible to attribute directly the changes observed here to the introduction of government anti-smoking initiatives.
Comparison with existing literature
Large increases in the collection of clinical indicator data (such as smoking status) by GPs after the introduction of the new GMS contract have also been found in populations with cardiovascular disease.18–20 Although the proportion of adult smokers in the QRESEARCH dataset in 2001/2002 (28%) and 2006/2007 (22%) was slightly higher than that found in the General Household Survey (2002: 27%; 2007: 21%),1 and slightly higher than the Health Survey for England in 2002 (26%), by 2007 the proportion of adult smokers in the QRESEARCH population was the same as in the Health Survey for England (22%).21 It is also reassuring to note that the reported decrease in the rate of smoking (6%) was similar to that reported in the General Household Survey.1 The mean rate of smoking in 2002 was also considerably lower than the mean rate of smoking reported in Europe (33%),22 but more than found in a national survey in the US (21%; 2005).23 The rate of smoking among the most affluent patients (14%) in 2007 was lower than that found in non-manual groups in the English General Household Survey (16%), and was considerably higher for the most deprived groups (34%) when compared with manual workers (28%).1
Implications for future research and clinical practice
The decline in the rate of smoking suggests that the UK has now achieved the overall threshold of 24% set out for smoking in the 2004 Public Service Agreement,24 and is near to achieving the 2010 Public Service Agreement target of 21%.25 With the introduction of new laws in the UK to prohibit smoking in enclosed public places and workplaces,26 the rise in the minimum age of smoking to 18 years, and the introduction of pictorial images on cigarette packaging, it is hoped that rates of smoking will continue to fall. However, substantial socioeconomic and age group differences in smoking rates have continued, suggesting a need to reinvigorate and introduce new measures aimed at reducing smoking rates among patients in more socioeconomically deprived areas and younger people in the UK population.27 Such measures include the need for further targeting of resources to help increase the proportion of deprived and younger patients receiving smoking cessation advice, the continued limiting of cigarette advertisement and sponsorship, and the banning of point of sale displays and cigarette vending machines (which is known to have the highest influence on young smokers).28 The substantial improvements in the recording of smoking status in the UK population by general practice have coincided with the introduction of financial incentives as part of the new GMS contract in 2004.4 The continued collection of such data will help ensure that progress of any trends can be monitored and also provide a detailed picture of lifestyle risks in the UK.
A significant and important reduction in the numbers of UK smokers occurred between April 2001 and April 2007. However, although this is an improvement, comparatively high rates of smoking remain among younger adults and those who are the most socioeconomically deprived. Furthermore, there is the need to focus greater resources and efforts on targeting the prevention of smoking uptake in children and adolescents, and providing more resources for smoking cessation services among younger adults and in deprived areas.
Acknowledgments
We would like to record our thanks to the contributing EMIS practices and patients, and to EMIS for providing technical expertise in creating and maintaining QRESEARCH. We thank QRESEARCH staff for their contribution to data extraction, analysis, and presentation. These findings have been reported in A Summary of Public Health Indicators Using Electronic Data from Primary Care,9 which is published by the NHS Health and Social Care Information Centre.
Funding body
Colin R Simpson is supported by a health services and health of the public postdoctoral fellowship from the Chief Scientist Office of the Scottish Government (PDF/08/02)
Ethics committee
All data analyses were conducted using de-identified data and were subject to the QRESEARCH research governance processes
Competing interests
Julia Hippisley-Cox is Director of QRESEARCH (a not-for-profit organisation owned by the University of Nottingham and EMIS, commercial supplier of computer systems for 60% of GP practices in the UK). Colin R Simpson and Aziz Sheikh have no competing interests
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Office for National Statistics. General household survey, 2006. Colchester, Essex: UK Data Archive, Office for National Statistics, Social Survey Division; 2009. [Google Scholar]
- 2.Department of Health. Smoking kills. A White Paper on tobacco. London: The Stationery Office; 1998. [Google Scholar]
- 3.Department of Health. The NHS plan: a plan for investment, a plan for reform. London: HMSO; 2000. [Google Scholar]
- 4.The NHS Confederation. Investing in general practice: the new general medical services contract. http://www.bma.org.uk/employmentandcontracts/independent_contractors/general_medical_services_contract/investinggp.jsp (accessed 7 Sep 2009)
- 5.Joossens L, Raw M. The Tobacco Control Scale: a new scale to measure country activity. Tob Control. 2006;15(3):247–253. doi: 10.1136/tc.2005.015347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Health. Health inequalities: progress and next steps. London: HMSO; 2008. [Google Scholar]
- 7.North East Public Health Observatory. Occasional paper number 20. Are NHS stop smoking services reducing health inequalities in the north east of England? http://www.nepho.org.uk/index.php?c=1095 (accessed 1 Sep 2009)
- 8.Sheikh A, Hippisley-Cox J, Newton J, Fenty J. Trends in national incidence, lifetime prevalence and adrenaline prescribing for anaphylaxis in England. J R Soc Med. 2008;101(3):139–435. doi: 10.1258/jrsm.2008.070306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.QRESEARCH and the Information Centre for Health and Social Care. A summary of public health indicators using electronic data from primary care. Nottingham: QRESEARCH; 2008. [Google Scholar]
- 10.Ghouri N, Hippisley-Cox J, Newton J, Sheikh A. Trends in the epidemiology and prescribing of medication for allergic rhinitis in England. J R Soc Med. 2008;101(9):466–472. doi: 10.1258/jrsm.2008.080096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Simpson CR, Newton J, Hippisley-Cox J, Sheikh A. Incidence and prevalence of multiple allergic disorders recorded in a national primary care database. J R Soc Med. 2008;101(11):558–563. doi: 10.1258/jrsm.2008.080196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simpson CR, Newton J, Hippisley-Cox J, Sheikh A. Trends in the epidemiology and prescribing of medication for eczema in England. J R Soc Med. 2009;102(3):108–117. doi: 10.1258/jrsm.2009.080211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hippisley-Cox J, Vinogradova Y, Coupland C, Pringle M. Comparison of key practice characteristics between general practices in England and Wales and general practices in the QRESEARCH database. Report to the Health and Social Care Information Centre. University of Nottingham: QRESEARCH; 2005. [Google Scholar]
- 14.QRESEARCH. The QRESEARCH database. Available from: http://www.qresearch.org (accessed 1 Sep 2009)
- 15.Department of Health. Population estimates for UK, England and Wales, Scotland and Northern Ireland. http://www.statistics.gov.uk/statbase/Product.asp?vlnk=601&More=N (accessed 1 Sep 2009)
- 16.Mant J, Murphy M, Rose P, Vessey M. The accuracy of general practitioner records of smoking and alcohol use: comparison with patient questionnaires. J Public Health Med. 2000;22(2):198–201. doi: 10.1093/pubmed/22.2.198. [DOI] [PubMed] [Google Scholar]
- 17.Department of Health. The Quality and Outcomes Framework guidance. London: The Department of Health; 2004. [Google Scholar]
- 18.Simpson CR, Hannaford PC, Lefevre K, Williams D. The effect of the UK incentive–based contract on the management of patients with stroke in primary care. Stroke. 2006;37(9):2354–2360. doi: 10.1161/01.STR.0000236067.37267.88. [DOI] [PubMed] [Google Scholar]
- 19.McGovern MP, Boroujerdi MA, Taylor MW, et al. The effect of the UK incentive-based contract on the management of patients with coronary heart disease in primary care. Fam Pract. 2008;25(1):33–39. doi: 10.1093/fampra/cmm073. [DOI] [PubMed] [Google Scholar]
- 20.McGovern MP, Williams DJ, Hannaford PC, et al. Introduction of a new incentive target based contract for family physicians in the United Kingdom: good for older patients with diabetes but less good for women? Diabet Med. 2008;25(9):1083–1089. doi: 10.1111/j.1464-5491.2008.02544.x. [DOI] [PubMed] [Google Scholar]
- 21.The Information Centre for Health and Social Care. Health Survey for England 2007: latest trends. http://www.ic.nhs.uk/statistics-and-data-collections/health-and-lifestyles-related-surveys/health-survey-for-england/health-survey-for-england-2007-latest-trends-%5Bns%5D (accessed 1 Sept 2009)
- 22.Strong K, Guthold R, Lang J, et al. Tobacco use in the European region. Eur J Cancer Prev. 2008;17(2):162–168. doi: 10.1097/CEJ.0b013e3282b6fcc9. [DOI] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. National Health Interview Survey (NHIS) 2005. Atlanta: Centers for Disease Control and Prevention US Department of Health and Human Services; 2005. [Google Scholar]
- 24.Her Majesty's Treasury. 2004 spending review. Public Service Agreements 2005–8. London: Her Majesty's Treasury; 2004. [Google Scholar]
- 25.The Department of Health. Spending Review 2004 Public Service Agreement. London: HMSO; 2004. [Google Scholar]
- 26.Chapman S. The future of smoke-free legislation. BMJ. 2007;335(7619):521–522. doi: 10.1136/bmj.39315.616169.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wanless D. Securing good health for the whole population. London: HMSO; 2004. [Google Scholar]
- 28.Ling PM, Neilands TB, Glantz SA. Young adult smoking behaviour: a national survey. Am J Prev Med. 2009;36(5):389–394. doi: 10.1016/j.amepre.2009.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]