Abstract
One way of developing culturally relevant health communication in the African American church setting is to develop spiritually based interventions, in which the health message is framed by relevant spiritual themes and scripture. In this article we describe the development of a community health advisor (CHA)-led intervention aimed at increasing informed decision making (IDM) for prostate cancer screening among church-attending African American men. Full-color print educational booklets were developed and pilot tested with extensive community participation of church-attending African American men age-eligible for screening. The intervention development phase consisted of ideas solicited from an advisory panel of African American men (N = 10), who identified core content and developed the spiritual themes. In the intervention pilot testing phase, prototypes of the intervention materials were pilot tested for graphic appeal in two focus groups (N = 16), and content was tested for acceptability and comprehension using individual cognitive response interviews (N = 10). Recommendations were made for project branding and logo and for use of graphics of real people in the educational materials. Significant feedback was obtained from the focus groups, on the graphics, colors, fonts, continuity, titles, and booklet size/shape. The importance of working closely with the community when developing interventions is discussed, as well as the importance of pilot testing of educational materials.
African American Men and Prostate Cancer
Prostate cancer is the leading cancer in terms of incidence in U.S. men, and the second in cancer mortality only to lung cancer (American Cancer Society, 2004). Significant racial disparities exist such that African American men are 60% more likely to develop prostate cancer and twice as likely to die from the disease than are White men (Stanford et al., 1999). The National Institute on Aging (NIA) strategic plan on health disparities (NIA, 2000) emphasizes the role of ethnicity in prostate cancer, and that African American men are suffering from prostate cancer disparities to a greater extent than are other groups. The plan also emphasizes the need for culturally appropriate health promotion interventions and strategies. The development of a culturally appropriate intervention to increase IDM for prostate cancer screening is consistent with these goals.
Informed Decision Making (IDM) Regarding Prostate Cancer Screening
As illustrated by Bowen and colleagues (2006), IDM is
defined as the process that patients go through to make a decision about engaging in a medical or health-related procedure or activity, considering the benefits, harms, risks, health improvements, the match between these properties and personal values and preferences, and understanding the uncertainty and limitations of the procedures. (p. 202)
Informed decision making (IDM) involves knowledge as well as preferences and values, and both the patient and the provider play a role in the decision-making process. Informed decision making (IDM) interventions should be based on theoretical models; however, many are not (Bowen et al., 2006).
Although there is no empirical evidence as of yet that prostate cancer screening reduces mortality, screening may be beneficial for men at increased risk for prostate cancer, such as African American men (Harris, Parrott, & Dorgan, 2004). For African American men, IDM may involve consideration of the elevated incidence and mortality rates of prostate cancer within their race, along with other factors that any man may consider such as age, lifestyle, family history, and the strengths and limitations of screening. African American men have had significant decreases in prostate cancer-related distress after receiving a negative screening result (Taylor, Shelby, Kerner, Redd, & Lynch, 2002).
One aspect of the controversy surrounding prostate cancer screening involves the potential for unnecessary surgeries and treatments for cancers that were never life threatening (Catalona, 2003). Even though awareness of potential benefits of screening has been found to be high, awareness of the limitations of screening was low in the aforementioned sample, with men reporting significantly fewer limitations (p < .01) following screening than before screening (Taylor et al., 2002). In light of the limited knowledge even among those African American men regarding the advantages and particularly the limitations regarding screening, and considering the disproportionate prostate cancer incidence and mortality in this group, IDM interventions are appropriate for these men.
Interventions to Increase IDM for Prostate Cancer Screening
Cancer communication interventions provide one effective approach to increasing IDM for prostate cancer screening. These interventions, sometimes termed decision aids, are proposed to be more effective when they address cultural beliefs (Chan et al., 2003; Chavez, McMullin, Mishra, & Hubbell, 2001) and are developed using community-based research (Breckon, Harvey, & Lancaster, 1994; Woods, Montgomery, & Herring, 2004). This entails significant involvement of the priority population in all stages of the intervention development. Decision aids, or interventions to increase IDM, were modestly effective for increasing prostate cancer knowledge among 63 African American men (List, Sinner, & Chodak, 1999). Although knowledge scores increased significantly from 20% to 57% (p < .001), these scores showed room for improvement. Given that African American men suffer higher prostate cancer incidence and mortality than other men (Stanford et al., 1999), these types of interventions are particularly important for this group, among whom informed decision making regarding screening plays a significant role, along with factors such as access to adequate medical care and preventive behaviors in their lifestyle.
Church-Based Interventions for Prostate Cancer Screening IDM
The church continues to be a viable access point for reaching African Americans. Members have looked to the church for leadership in areas beyond spirituality and religion. There have been several church-based interventions aimed at increasing prostate cancer knowledge or screening for prostate cancer among African American men. It has been suggested that recruitment of African American men into prostate cancer educational programs must focus on a community orientation rather than on a provider or health site orientation (Weinrich, Boyd, Bradford, Mossa, & Weinrich, 1998). In one program, knowledge and self-efficacy for prostate cancer screening was targeted, using Social Cognitive Theory (Boehm et al., 1995). This intervention used lay health educators, African American men who had been diagnosed and treated for prostate cancer, as role models and to deliver the intervention. Knowledge and self-efficacy scores improved significantly (p < .001) after the intervention among the sample of 102 participants.
In another study, churches were among several community venues used to deliver a prostate cancer screening intervention in a sample of 1,522 men age 40–70 that was 72% African American (Tingen, Weinrich, Heydt, Boyd, & Weinrich, 1998). Screening was predicted significantly by perceived benefits of screening, and African Americans, those not married, and those with less than a high school education were significantly less likely to be screened than Whites, married men, and those with more than a high school education. Receiving an intervention with a peer educator was also a significant predictor of participation in screening. In a previous church-based educational program aimed at increasing knowledge and self-efficacy for prostate cancer screening, lay educators also were used, who were men previously diagnosed with the disease and could serve as role models (Boehm et al., 1995). This program resulted in significant increases in knowledge and self-efficacy scores.
In another multiple-venue project including churches, 900 African American men were provided with a 1-hour educational seminar, developed with involvement of the lay and medical community and delivered through an African American health educator (Wilkinson, List, Sinner, Dai, & Chodak, 2003). Awareness scores increased significantly (p < .001) from 26% before the session to 73% after the session. In another community-based program including churches and targeting African American men age 23–88 (N = 75), knowledge significantly increased from 23% to 64% in a short-term follow-up (Collins, 1997). In a church-based prostate cancer educational program for men age 40–70 (N = 393 African American; N = 104 White), having a member of the congregation previously diagnosed with prostate cancer was a significant predictor of program attendance (p < .05; Weinrich, Holdford, et al., 1998). When free prostate cancer screenings were offered to 1,369 African American men, the highest participation in the screenings was found in churches, fairgrounds, and work sites, relative to barber shops, housing projects, and National Association for the Advancement of Colored Persons sites (Weinrich, Boyds, Bradferd, Mossa, & Weinrich, 1998).
These church-based prostate cancer screening IDM programs resulted in modest short-term gains in knowledge; however, knowledge among African American men was still low, as was screening. Although churches have served as a venue for prostate cancer education and screening programs, none of these church-based interventions used a spiritually based approach. Rather, they have used the church solely as a venue. This approach may underutilize the potential of churches for effective health education.
Religion and Health in the African American Community
For many African Americans, religion (e.g., “religious involvement”) plays an important role in daily life and is a central element of the cultural fabric (Taylor & Chatters, 1986). African Americans, especially those who are older, often have high religious involvement (Ferraro & Koch, 1994). Church provides African Americans with social support (Taylor, 1993). African American men reported relying on their faith to stay healthy (Holt, Lewellyn, & Rathweg, 2005; Lambert, Fearing, Bell, & Newton, 2002). Individuals in the African American community traditionally have sought out the church for health information and guidance. Research suggests that African Americans find their religion useful in addressing health concerns and other stressful issues (Ellison & Taylor, 1996; Rogers-Dulan, 1998), including cancer (Potts, 1996). Positive associations have been demonstrated between religious involvement and cancer control behaviors such as mammography (Holt, Lukwago, & Kreuter, 2003), use of pap tests (Naguib, Geiser, & Comstock, 1968), and fruit and vegetable consumption among African Americans (Holt, Haire-Joshu, Lukwago, Lewellyn, & Kreuter, 2005). Religious involvement was associated with mental health and lower rates of alcohol and tobacco use among 537 African American men (Brown & Gary, 1994).
In a sample of African American men age 40 and older (N = 199), religious involvement was significantly predictive of having had a digital rectal examination to test for prostate cancer (Holt, Wynn, & Darrington, 2008). Screening among African American men, however, is still underutilized relative to White men (Tingen et al., 1998). In a sample of men with prostate cancer (14 African American, 24 White), the men perceived their faith to benefit their coping, church provided both social and spiritual support, and their faith in God had endured (Bowie, Sydnor, Granot, & Pargament, 2004). In the same sample, high levels of church attendance and affiliation were reported, and many had spoken to their doctors about spiritual and religious beliefs (Bowie, Sydnor, & Granot, 2003).
Spiritually Based Cancer Communication Interventions for African Americans
Cancer communication interventions that integrate spiritually based content, in which relevant spiritual themes and scriptures are identified by community members and are used to frame the health message, may have increased cultural appropriateness (Harris, Thoresen, McCullough, & Larson, 1999; Holt, Kyles, Wiehagen, & Casey, 2003; Winett et al., 1999). This approach may be particularly appropriate for use in church-based settings. In this context we use the term spiritually based rather than religiously based (except when summarizing the work of others where their terminology is retained). While we recognize that these terms are distinct yet overlapping (Musick, Traphagan, Koenig, & Larson, 2000), and the present approach involves religious concepts, it also may involve broader concepts (e.g., healthy body, mind, and spirit) reflective of “spirituality.”
Church-based interventions can be characterized by a typology in accord with level of religious orientation (Winett et al., 1999). Level 1 interventions use the church as a venue for recruitment, but intervention content is secular in nature. In Level 2, secular interventions are implemented in church settings by health care professionals. In Level 3, lay individuals from the church implement secular interventions. Finally, Level 4 interventions integrate religious or spiritual themes into the intervention content. This may involve the use of scripture or spiritual themes such as taking care of the body, which is a gift from God, or supporting one another's health through the fellowship of the church. Relevant spiritual themes frame the cancer educational message, thus putting health in a spiritual context. These themes are identified through working closely with the priority population and conducting pilot testing of messages for acceptability (Holt, Kyles, et al., 2003). Winett and colleagues (1999) view this level as a necessary but not sufficient approach for continued behavior change. The aim of these interventions is not to increase religiosity or spirituality, but to work within an existing cultural framework to increase the cultural relevance, and therefore effectiveness, of a health communication intervention. Spiritually based approaches may be more effective than their nonspiritual counterparts based on the notion that they are more personally relevant to the receiver (Holt, Lee, & Wright, 2008).
The Present Study
The aims of the present study were to develop and pilot test for acceptability a spiritually based prostate cancer screening IDM intervention for African American men who attend church. Spiritually based cancer communication interventions can be developed by using relevant spiritual themes to frame the cancer educational message thus increasing personal relevance by putting health in a spiritual context. Although the spiritually based approach has been applied to other groups and health issues, it has not yet been tested for IDM for prostate cancer screening among African American men. Matthews and colleagues found in focus groups for their church-based REACH 2010 project encouraging breast and cervical cancer early detection, that their participants perceived an importance of using scripture to frame a health message, and a strong sense of the relationship among religion, spirituality, and health (Matthews, Berrios, Darnell, & Calhoun, 2006).
This article chronicles the development and pilot testing of the print materials used as the basis for the intervention. The intervention consists of an educational session to be led by a trained Community Health Advisor (CHA) from each church. Each session will be conducted in “Sunday School” fashion, led by the CHA, guided by the print materials. The intervention materials and framework were developed by working closely with the community, were pilot tested using focus groups and cognitive response testing with the priority population (see Figure 1), and were finalized based on feedback from these activities.
Figure 1.
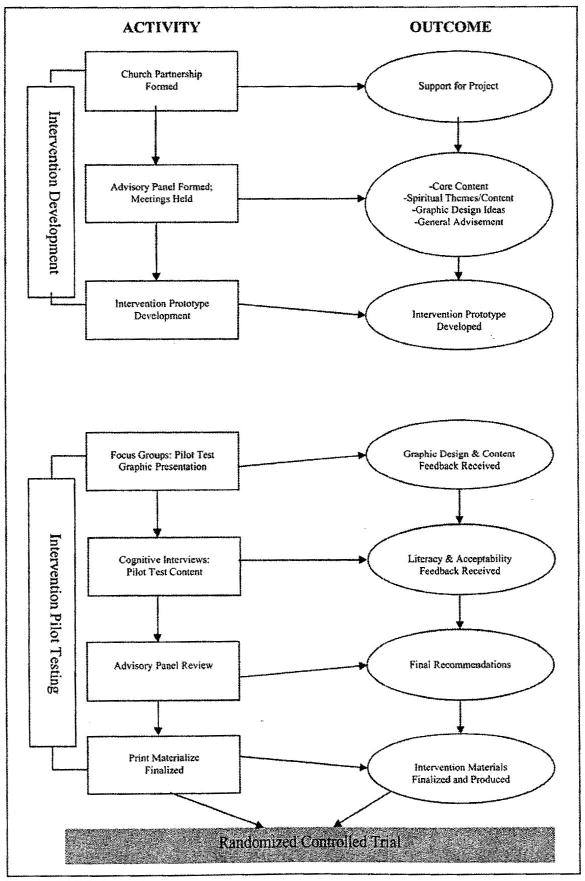
Intervention development and pilot testing activities.
Method
Overview
Intervention development involved working with an advisory panel, who provided input on all aspects of the intervention, two focus groups used to pilot test the educational session graphical presentation, and cognitive response interviews to ensure that all content was understandable and appropriate. The final intervention product also is described.
Intervention Development
Advisory Panel
The intervention development occurred through a community-based methodology whereby 10 African American men from a church in the greater Birmingham area served on the advisory panel (see Table 1). The men were identified through a gatekeeper who was a member of the church. The primary role of the advisory panel was to identify spiritual themes and other elements to be included in the intervention materials. The group included prostate cancer survivors as well as a minister. The advisory panel had significant input into all aspects of the intervention, including how long the educational sessions should last, how to maximize men's participation in such a session, and the design of the print materials. These objectives were achieved across eight monthly meetings. Early meetings were moderated by the program manager and principal investigator, and later meetings were moderated by the advisory panel chairman. Meetings followed an agenda, which reflected the project stage and activities, and were built upon the progress of the previous meeting. Early meetings generated ideas for the intervention and content and moved to development of the spiritually based messages and themes, and finally to integration of the feedback from the other pilot testing activities and finalizing the intervention materials and procedures. Each member of the panel received a payment of $100 value.
Table 1.
Demographic characteristics of formative research participants
| Advisory panel | Focus groups | Cognitive response interviews | |
|---|---|---|---|
| N | 10 | 16 | 10 |
| Mean age (SD) | 49 (13.14) | 55 (6.10) | 55 (8.63) |
| PC survivor | 2 | 0 | 0 |
| Relationship status | |||
| Never married | 1 | 1 | – |
| Married or living with partner | 8 | 14 | 8 |
| Separated/divorced | – | 1 | 1 |
| Widowed | – | – | 1 |
| No answer | 1 | – | – |
| Education | # | ||
| High school or GED | – | – | – |
| Some college | – | – | – |
| Bachelor's | 4 | 17.27 (1.87)* | 16.50 (2.72)* |
| Master's or higher | 1 | – | – |
| No answer | 1 | – | – |
| Employment | # | ||
| Full time | 7 | 12 | 6 |
| Part time | – | 2 | 1 |
| Retired | 2 | 1 | 1 |
| Not employed | – | 1 | 1 |
| No answer | 1 | – | – |
Education in these activities was assessed as number of years as opposed to categories.
Missing some data in this category.
Advisory Panel Recommendations for Intervention
The advisory panel recommended particular scriptures they felt reflected a theme of health and wellness, as well as spiritual themes including a balance of body, mind, and soul, and a generational theme where men talk to others in their family about prostate cancer. They made recommendations for core content such as the role of family history, race, diet, insurance coverage of screening, and prostate cancer statistics pertinent to African American men, and they felt that a clear call to action was needed. The panel recommended that the project make use of “branding” and have its own identity through a name, logo, and identifiable materials. The daughter of the advisory panel chairman volunteered her time to develop a project logo, which consisted of the letters “P” and “C” (for prostate cancer) in the formation of a cross. The panel provided recommendations regarding the print materials to be used in the educational sessions, for example, avoiding use of Eurocentric icons of Jesus Christ in favor of a more neutral cross iconography. They also felt that pictures of “real people” were appealing, and consented to having their own photographs taken and used for the print materials. They provided recommendations on the color scheme of the materials, in favor of a softer color scheme of green and blue with brown, over an Afro-Centric scheme of black, red, yellow, and green. A recommendation was made that the print materials be slim enough so that they could fit into a man's suit coat inside pocket. Based on the advisory panel recommendations, two prototype educational booklets were developed for pilot testing.
Pilot Testing the Intervention for Acceptability
Focus Groups
Two focus groups of additional African American men congregation members aged 45 and older were used to pilot test the educational session graphical presentation (see Table 1). These men were convenience samples recruited from local African American churches not associated with the advisory panel nor with the randomized controlled trial to be conducted in the latter phase of the project. Eligibility criteria included being an African American male, aged 45 and older, with no history of prostate cancer, and who could read material written at the fifth-grade reading level. The groups were presented with prototypes of the print materials and provided feedback on the acceptability of the graphical presentation. Trained focus group moderators asked the participants questions based on a semistructured topic guide, on factors such as the booklet size and shape, color scheme, graphics, and fonts. Each member of the focus group received a $25 gift card. The group was audiotaped and transcribed. The verbatim transcripts were reviewed independently by the investigative team, and, by consensus, recommendations were made for modifications to the prototypes. A second set of prototypes was generated between the first and second groups, resulting in an iterative pilot testing and feedback process. Agreement between reviewers approached 100% on recommendations for modifications based on the focus group data.
Focus Group Recommendations for Intervention
Participants in the first focus group provided extensive feedback on the print materials prototypes. The first version included a photograph of half of a man's face on the cover, which the men disliked because they felt that by showing half of the face, it meant that either the man was not fully informed or that he had something to hide. Participants recommended use of a larger font size for easier reading. They preferred the title “A Brother-to-Brother Guide to Prostate Cancer & Screening” over another candidate that they felt was too “youngish.” They preferred graphics showing older men but not too old; a mix of men of different ages was preferred. Participants did not want to see men that were too happy or too smiling, however, in that prostate cancer is a serious topic. They recommended use of pictures of real people if possible, and preferred brighter, bolder, yet masculine colors. A prototype with a green, brown, and light blue color scheme was not well received in that the colors were not bold enough. Participants indicated the need for a stronger linkage between the booklet title, cover graphics, and inside content, that it needed to be more spiritually based but yet not “preachy.” They recommended that the spiritually based nature of the content be presented clearly and early in the booklet. They also called for use of more bullet points for easier reading, rather than long paragraphs of text.
After the above changes were made, a second set of prototypes was provided to the second focus group for consideration. They recommended that the word “cancer” (as opposed to “prostate health”) remain in the title, in order to maintain the serious tone of the booklet. There was a series of three graphics of people on the cover that they felt were disconnected and should be reordered to show progression from young man to older couple, reflecting the life course. The group liked the main graphic of an older gentleman on the cover. They called for a thinning of the word count so that the booklet is not so “busy.” They liked the revised color scheme of green and blue with brown.
Cognitive Response Interviews
Ten additional African American men congregation members aged 45 and older tested the content of the print-based materials, particularly focusing on the spiritually based messages (see Table 1). These men were a convenience sample recruited from a pool of church-attending men from churches not selected for the intervention trial. They were recruited and screened for eligibility as in the focus groups. They made 1-hour appointments with research staff to read passages from the intervention and answer open-ended questions about what they read (cognitive response technique). Cognitive response procedures involve intensive one-on-one interviews in which participants were asked to think aloud about the passages, paraphrase the content, and respond to other inquiries and probes (Forsyth & Lessler, 1991; Sudman, Bradburn, & Schwartz, 1996). The interviews were audiorecorded, transcribed, and reviewed by the investigative team. This testing occurred in the project offices, with one occurring in the participant's home. Each cognitive response interview participant received a $25 gift card. Verbatim transcripts and field notes were reviewed by the investigative team. By consensus, recommendations then were made for the revision of difficult material.
Recommendations From Cognitive Response Interviews
Only minor modifications were suggested based on the cognitive response interviews. Most of the material was easily understood by the participants and was well accepted. Particular words in the text were emphasized through a bold font or underlining, to make certain passages more clear (e.g., prostate cancer is the second leading cause of cancer death for African American men). The passage explaining the controversy on not all experts agreeing that all men should obtain prostate cancer screening was clarified. This is a challenging concept to explain in limited space, but it appears as though this objective was achieved. The spiritual themes and scripture were all well received by the participants.
Final Intervention
The intervention builds upon a previous study and pilot work with African American women in which a spiritually based approach was used to encourage mammography screening for breast cancer (Holt & Klem, 2005; Holt, Kyles, et al., 2003). Many of the processes of intervention development and pilot testing that were successful in the previous study were applied to the present study. Consistent with previous research (Boehm et al., 1995), the final approved intervention covers content areas including anatomy and physiology, incidence, development, and treatment of prostate cancer, assessment of one's personal risk factors for prostate cancer (e.g., age, race, family history), screening options and their risks and benefits, and the importance of initial and repeat screening. The intervention encourages men to talk to their family and their pastor, and to involve family in their decision making. It also covers symptoms of prostate cancer. The intervention incorporates Social Cognitive Theory (Bandura, 1986) through the use of peer role models (the CHAs) and aims to increase self-efficacy for screening. The Health Belief Model (Rosenstock, 1960) is incorporated by attempting to reduce barriers to IDM and screening, and to increase knowledge of and perceived benefits of screening. Because the focus of the intervention is IDM, the potential risks of screening also are addressed, and each man is encouraged to weigh his own risk profile and make a decision regarding screening that he is comfortable with, given his risk profile. For example, a man with a strong family history of prostate cancer might give more serious consideration to screening than a man with a normal risk profile, who may decide that, for himself, the risks of screening (e.g., false positive, unnecessary biopsy) are not worth the potential benefit.
The educational sessions are guided by print materials encouraging IDM for prostate cancer screening. The CHA uses the print materials to lead his educational session, and to teach from the materials as is done in “Sunday School.” Each man who attends receives his own copy to follow along and keep. The materials consist of a professionally designed and produced 16-page full-color booklet on the aforementioned topics. The materials contain spiritual content (e.g., spiritual testimonials from cancer survivors, relevant scripture, notion that God will take care of us but we have to do our part and take personal responsibility, passing knowledge on from generation to generation), along with wellness and prostate information. Example spiritually based messages include the following: “God gives us the free will and the medical technology to fight this disease—it's our responsibility to use it” and “God promises to take care of his children, but we have to take that first step and do our part.” The print materials were tested for readability using the Simplified Measure of Gobbledygook (SMOG) formula and revised to the sixth-grade level.
Discussion
The aims of the present study were to develop and pilot test for acceptability a spiritually based prostate cancer screening IDM intervention for African American men who attend church. This was made possible by working closely with the community on a number of levels. Convening an advisory panel of men representing the community, who are committed and passionate about the project, has made for a more relevant approach in a number of ways. This panel provided not only the spiritual foundation (they were recruited from a church) for the intervention, they also provided advice and feedback on issues such as structure and content of the CHA trainings, as well as structure and content of the educational session itself. Their participation in the monthly meetings dovetailed with other intervention development and pilot testing activities such as focus groups and cognitive response interviews, such that they were able to provide their critical input at every step of the way.
From the focus groups we learned that the first series of educational booklet prototypes were inadequate in several ways. Color schemes were stereotypical Afro-centric or too pale and perceived as weak. Graphics of people smiling were not taken seriously in that prostate cancer is a life-threatening disease. There was a lack of flow in the spiritual theme, which was apparent in a disconnect among the booklet title, graphics, and opening content. The Eurocentric Jesus who appeared in some of the pages was offensive. Much helpful information was learned from this pilot testing, which made for a better product in the end. Several iterations of graphic and content versions were developed in order to “tweak” the material to its best presentation. The cognitive response interviews indicated that the material was largely understandable, with several exceptions. This was also material however, that had gone through several iterations of not only project team but advisory panel and focus group feedback and editing. The importance of working closely with the community and engaging in pilot testing activities cannot be overstated.
Several qualitative examinations have reported on African American men's knowledge, beliefs about prostate cancer, and barriers to screening, many for use in the development of cancer communication interventions for this population. In one study, in which focus groups were used to develop a culturally relevant intervention, it was reported that religious involvement, including beliefs and church support, were important for screening, as well as faith and church leadership and the belief about God's will for health outcomes (Blocker et al., 2006). Barriers to screening included mistrust of the medical community and negative attitudes toward particular screening modalities. These findings are similar to the present study, particularly those involving religious influences and beliefs.
Other focus groups for the development of a prostate cancer screening educational intervention for African American and Hispanic men revealed that for African Americans, work, family, and faith were themes of major importance (Meade, Calvo, Rivera, & Baer, 2003). These were similar for the Hispanic men as well. The men recommended use of cancer survivors as educators and interactive group discussions, and information that is easy to understand. These findings are similar to those in the present study in that the men indicated the importance of family and faith, survivors were involved in the intervention development and delivery of the all-male group discussions, and the print materials were brief and easy to digest.
Strengths and Limitations
Several strengths of the present study are notable. First, there was community involvement at all levels from the advisory panel in which the spiritual content was developed and recommendations for the intervention approach were obtained, to the pilot testing in which feedback was obtained on the details of the print materials. The careful systematic process of intervention development and pilot testing itself is also a strength and led from prototypes to polished final materials that are well received by the priority population. Finally, the use of testimonials from men in the community who have gone through prostate cancer and treatment provides a powerful communication strategy for this group.
There are also several limitations to the approach taken in the development of the present intervention. It is possible that the members composing the advisory panel, because they were all from the same church, may hold views that are not representative of the local African American community. This was not evident in the pilot testing, in which men were recruited from other congregations. It is unknown, however, whether the materials will be well received in the congregations that host the randomized controlled trial. It is also unknown whether the materials would be generalizable for church-attending African American men in other parts of the country. They may not be relevant for those who do not consider themselves Christian, in that some of the spiritual themes were based on scripture from the Bible. If such an intervention were to be used with diverse religious groups, it would have to be modified and re-pilot tested. This is both the advantage but also the limitation of such targeted materials, whether the targeting be by sex, race, age, or geographic region.
Future Research
In the next phase of the project, the spiritually based intervention will be compared with a nonspiritual intervention of the same core (prostate cancer IDM) content to determine whether it has any differential effectiveness on IDM for prostate cancer screening. The impact of the intervention will be evaluated through use of baseline and follow-up self-administered questionnaires assessing the study outcome of IDM for prostate cancer screening. If the spiritually based intervention is found to be effective for increasing IDM, a next logical step would be to build onto the intervention or to follow the cohort of men for a longer period of time to determine the effects on actual screening behavior. The spiritually based approach also could be used in the church setting for other health issues such as hypertension or diabetes. The approach should be explored also with other religious groups.
Acknowledgments
This study was supported by a grant from the University of Alabama at Birmingham Comprehensive Cancer Center through the American Cancer Society Institutional Research Grant Program (#ACS IRG-60-001-47, NCI-CA-13148-31) and was approved by the University of Alabama at Birmingham Institutional Review Board.
Contributor Information
Cheryl L. Holt, Department of Public and Community Health in the School of Public Health, College Park, Maryland, USA
Theresa A. Wynn, University of Alabama at Birmingham School of Medicine-Division of Preventive Medicine, Birmingham, Alabama, USA
Penny Southward, Media for Health, Birmingham, Alabama, USA.
Mark s. Litaker, Department of Diagnostic Sciences at the University of Alabama at Birmingham, Birmingham, Alabama, USA
Sanford Jeames, UMass Donahue Institute, Hadley, Massachusetts, USA.
Emily Schulz, University of Alabama at Birmingham School of Medicine-Division of Preventive Medicine, Birmingham, Alabama, USA.
References
- American Cancer Society. Cancer facts and figures 2004. Atlanta, Georgia: American Cancer Society Inc; 2004. [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Blocker DE, Romocki LS, Thomas KB, Jones BL, Jackson EJ, Reid L, Campbell MK. Knowledge, beliefs and barriers associated with prostate cancer prevention and screening behaviors among African-American men. Journal of the National Medical Association. 2006;98:1286–1295. [PMC free article] [PubMed] [Google Scholar]
- Boehm S, Coleman-Burns P, Schlenk EA, Funnell MM, Parzuchowski J, Powell IJ. Prostate cancer in African American men: Increasing knowledge and self-efficacy. Journal of Community Health Nursing. 1995;12:161–169. doi: 10.1207/s15327655jchn1203_4. [DOI] [PubMed] [Google Scholar]
- Bowen DJ, Allen JD, Vu T, Johnson RE, Fryer-Edwards K, Hart A., Jr Theoretical foundations for interventions designed to promote informed decision making for cancer screening. Annals of Behavioral Medicine. 2006;32:202–210. doi: 10.1207/s15324796abm3203_5. [DOI] [PubMed] [Google Scholar]
- Bowie JV, Sydnor KD, Granot M. Spirituality and care of prostate cancer patients: A pilot study. Journal of the National Medical Association. 2003;95:951–954. [PMC free article] [PubMed] [Google Scholar]
- Bowie JV, Sydnor KD, Granot M, Pargament KI. Spirituality and coping among survivors of prostate cancer. Journal of Psychosocial Oncology. 2004;22:41–56. [Google Scholar]
- Breckon DJ, Harvey JR, Lancaster RB, editors. Community health education: Settings, roles, and skills for the 21st century. Gaithersburg, MD: Aspen Publishing; 1994. [Google Scholar]
- Brown DR, Gary LE. Religious involvement and health status among African-American males. Journal of the National Medical Association. 1994;86:825–831. [PMC free article] [PubMed] [Google Scholar]
- Catalona WJ. Informed consent for prostate-specific antigen screening. Urology. 2003;61:17–19. doi: 10.1016/s0090-4295(02)02007-1. [DOI] [PubMed] [Google Scholar]
- Chan EC, Vernon SW, O'Donnell FT, Ahn C, Greisinger A, Aga DW. Informed consent for cancer screening with prostate-specific antigen: How well are men getting the message? American Journal of Public Health. 2003;93:779–785. doi: 10.2105/ajph.93.5.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez LR, McMullin JM, Mishra SI, Hubbell FA. Beliefs matter: Cultural beliefs and the use of cervical cancer-screening tests. American Anthropologist. 2001;103:1114–1129. [Google Scholar]
- Collins M. Increasing prostate cancer awareness in African American men. Oncology Nursing Forum. 1997;24:91–95. [PubMed] [Google Scholar]
- Ellison CG, Taylor RJ. Turning to prayer: Social and situational antecedents of religious coping among African Americans. Review of Religious Research. 1996;38:111–131. [Google Scholar]
- Ferraro KF, Koch JR. Religion and health among black and white adults: Examining social support and consolation. Journal for the Scientific Study of Religion. 1994;33:362–375. [Google Scholar]
- Forsyth B, Lessler J. Cognitive laboratory methods: A taxonomy. In: Biemer PP, Groves RM, Lyberg LE, Mathiowetz NA, Sudman S, editors. Measurement errors in surveys. New York: Wiley; 1991. pp. 393–418. [Google Scholar]
- Harris TM, Parrott R, Dorgan KA. Talking about human genetics within religious frameworks. Health Communication. 2004;16:105–116. doi: 10.1207/S15327027HC1601_7. [DOI] [PubMed] [Google Scholar]
- Harris AHS, Thoresen CR, McCullough ME, Larson DB. Spiritually and religiously oriented health interventions. Journal of Health Psychology. 1999;4:413–433. doi: 10.1177/135910539900400309. [DOI] [PubMed] [Google Scholar]
- Holt CL, Haire-Joshu DL, Lukwago SL, Lewellyn LA, Kreuter MW. Spirituality and dietary beliefs and behaviors among urban African American women. Cancer Control, Cancer Culture and Literacy Supplement. 2005;12:84–90. doi: 10.1177/1073274805012004S12. [DOI] [PubMed] [Google Scholar]
- Holt CL, Klem PR. As you go, spread the word: Spiritually-based breast cancer education for African American women. Journal of Gynecologic Oncology. 2005;99(Suppl 3):S141–142. doi: 10.1016/j.ygyno.2005.07.066. [DOI] [PubMed] [Google Scholar]
- Holt CL, Kyles A, Wiehagen T, Casey C. Development of a spiritually based breast cancer educational booklet for African American women. Cancer Control. 2003;10(Suppl 5):37–44. doi: 10.1177/107327480301005s06. [DOI] [PubMed] [Google Scholar]
- Holt CL, Lee C, Wright K. A spiritually-based approach to breast cancer awareness: Cognitive response analysis of communication outcomes. Health Communication. 2008;23:13–22. doi: 10.1080/10410230701626919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Lewellyn LA, Rathweg MJ. Exploring religion-health mechanisms among African American parishioners. Journal of Health Psychology. 2005;10:511–527. doi: 10.1177/1359105305053416. [DOI] [PubMed] [Google Scholar]
- Holt CL, Lukwago SN, Kreuter MW. Spirituality, breast cancer beliefs and mammography utilization among urban African American women. Journal of Health Psychology. 2003;8:383–396. doi: 10.1177/13591053030083008. [DOI] [PubMed] [Google Scholar]
- Holt CL, Wynn TA, Darrington J. Religiosity and prostate cancer knowledge, attitudes, and screening among African Americans. American Journal of Men's Health. 2008 July; doi: 10.1177/1557988308318686. [DOI] [PubMed] [Google Scholar]
- Lambert S, Fearing A, Bell D, Newton M. A comparative study of prostate screening health beliefs and practices between African American and Caucasian men. Association of Black Nursing Faculty Journal. 2002;13:61–63. [PubMed] [Google Scholar]
- List MA, Sinner M, Chodak GW. Improving knowledge about prostate cancer: The development of an educational program for African-Americans. Prostate Cancer and Prostatic Diseases. 1999;2:186–190. doi: 10.1038/sj.pcan.4500313. [DOI] [PubMed] [Google Scholar]
- Matthews AK, Berrios N, Darnell JS, Calhoun E. A qualitative evaluation of a faith-based breast and cervical cancer screening intervention for African American women. Health Education and Behavior. 2006;33:643–663. doi: 10.1177/1090198106288498. [DOI] [PubMed] [Google Scholar]
- Meade CD, Calvo A, Rivera MA, Baer RD. Focus groups in the design of prostate cancer screening information for Hispanic farmworkers and African American men. Oncology Nursing Forum. 2003;30:967–975. doi: 10.1188/03.ONF.967-975. [DOI] [PubMed] [Google Scholar]
- Musick MA, Traphagan JW, Koenig HG, Larson DB. Spirituality in physical health and aging. Journal of Adult Development. 2000;7:73–86. [Google Scholar]
- Naguib SM, Geiser PB, Comstock GW. Response to a program of screening for cervical cancer. Public Health Reports. 1968;83:990–998. [PMC free article] [PubMed] [Google Scholar]
- National Institute on Aging. National Institute on Aging. 2000 Strategic Plan [On-line] Available: http://www.nia.nih.gov/AboutNIA/StrategicPlan/
- Potts RG. Spirituality and the experience of cancer in an African-American community: Implications for psychosocial oncology. Journal of Psychosocial Oncology. 1996;14:1–19. [Google Scholar]
- Rogers-Dulan J. Religious connectedness among urban African American families who have a child with disabilities. Mental Retardation. 1998;36:91–103. doi: 10.1352/0047-6765(1998)036<0091:RCAUAA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. What research in motivation suggests for public health. American Journal of Public Health. 1960;50:295–302. doi: 10.2105/ajph.50.3_pt_1.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanford JL, Stephenson RA, Coyle LM, Cerhan L, Correa R, Eley JW, Gilliland F, Hankey B, Kolonel LN, Kosary C, Ross R, Severson R, West D. Prostate cancer trends 1973-1995, SEER Program. Bethesda, MD: National Cancer Institute; 1999. [Google Scholar]
- Sudman S, Bradburn N, Schwartz N. Thinking about answers: The application of cognitive processes to survey methodology. San Francisco: Jossey-Bass, Inc; 1996. [Google Scholar]
- Taylor KL, Shelby R, Kerner J, Redd W, Lynch J. Impact of undergoing prostate carcinoma screening on prostate carcinoma-related knowledge and distress. Cancer. 2002;95:1037–1044. doi: 10.1002/cncr.10781. [DOI] [PubMed] [Google Scholar]
- Taylor RJ. Religion and religious observances. In: Jackson JS, Chatters LM, et al., editors. Aging in black America. Thousand Oaks, CA: Sage Publications, Inc; 1993. pp. 101–123. [Google Scholar]
- Taylor RJ, Chatters LM. Church-based informal support among elderly blacks. Gerontologist. 1986;26:637–642. doi: 10.1093/geront/26.6.637. [DOI] [PubMed] [Google Scholar]
- Tingen MS, Weinrich SP, Heydt DD, Boyd MD, Weinrich MC. Perceived benefits: A predictor of participation in prostate cancer screening. Cancer Nursing. 1998;21:349–357. doi: 10.1097/00002820-199810000-00006. [DOI] [PubMed] [Google Scholar]
- Weinrich SP, Boyd MD, Bradford D, Mossa MS, Weinrich M. Recruitment of African Americans into prostate cancer screening. Cancer Practice. 1998;6:23–30. doi: 10.1046/j.1523-5394.1998.1998006023.x. [DOI] [PubMed] [Google Scholar]
- Weinrich S, Holdford M, Boyd M, Creanga D, Cover K, Johnson A, Frank-Stromborg, Weinrich M. Prostate cancer education in African American churches. Public Health Nursing. 1998;15:188–195. doi: 10.1111/j.1525-1446.1998.tb00338.x. [DOI] [PubMed] [Google Scholar]
- Wilkinson S, List M, Sinner M, Dai L, Chodak G. Educating African-American men about prostate cancer: Impact on awareness and knowledge. Urology. 2003;61:308–313. doi: 10.1016/s0090-4295(02)02144-1. [DOI] [PubMed] [Google Scholar]
- Winett RA, Anderson ES, Whiteley JA, Wojcik JR, Rovniak LS, Graves KD, Galper DI, Winett SG. Church-based health behavior programs: Using social cognitive theory to formulate interventions for at-risk populations. Applied and Preventive Psychology. 1999;8:129–142. [Google Scholar]
- Woods VD, Montgomery SB, Herring RP. Recruiting Black/African American men for research on prostate cancer prevention. Cancer. 2004;100:1017–1025. doi: 10.1002/cncr.20029. [DOI] [PubMed] [Google Scholar]


