Abstract
Objective
To describe the events leading to the epidemic of congenital rubella syndrome in Greece in 1993 after a major rubella epidemic.
Design
Retrospective survey and systematic review.
Setting
Greece (population 10 million), 1950-95.
Subjects
Children, adolescents, and women of childbearing age.
Results
Around 1975 in Greece the measles, mumps, and rubella vaccine started being given to boys and girls aged 1 year without policies to attain high vaccination coverage and to protect adolescents and young women. During the 1980s, vaccination coverage for rubella remained consistently below 50%, and the proportion of pregnant women susceptible to rubella gradually increased. In 1993 the incidence of rubella in young adults was higher than in any previous epidemic year. The epidemic of congenital rubella that followed, with 25 serologically confirmed cases (24.6 per 100 000 live births), was probably the largest such epidemic in Greece after 1950.
Conclusions
With low vaccination coverage, the immunisation of boys and girls aged 1 year against rubella carries the theoretical risk of increasing the occurrence of congenital rubella. This phenomenon, which has not been previously reported, occurred in Greece.
Introduction
Rubella is usually a mild disease, but infection during the first 3-4months of pregnancy can result in spontaneous abortion, stillbirth, and congenital rubella syndrome.1,2
Immunisation programmes to prevent congenital rubella syndrome were introduced in many countries soon after vaccines for rubella and measles, mumps, and rubella became available in 1969 and 1971 respectively.3 The immunisation of boys and girls aged 1 year (“indirect” strategy) aims to protect women of childbearing age from exposure to the rubella virus by interrupting its transmission.4,5 This can lead to a rapid reduction in cases of congenital rubella, but if vaccination coverage is low there is concern that this strategy may increase the incidence of rubella in adolescents and adults thus increasing the incidence of congenital rubella.4,6–9 It has been estimated that in developed countries this could happen in the long term if immunisation uptake was lower than 50%-60%, with wide oscillations in the incidence of congenital rubella in the medium term.4,7,9 In contrast, the immunisation of adolescent girls (“direct” strategy) does not interfere appreciably with the transmission of the virus and aims to protect women of childbearing age from the disease.4,10 Several countries have adopted a two dose vaccination strategy because of its advantages.11–14
Some less developed countries have recently introduced rubella immunisation into their national schedules, or are considering doing so.14,15 The elimination of indigenous congenital rubella syndrome in Europe by the year 2000 is part of the World Health Organisation's health for all strategy.16
In Greece, immunisation of boys and girls aged 1 year with the measles, mumps, and rubella vaccine was introduced in the mid-1970s but not as part of a systematic policy.17 In 1993 a major rubella epidemic took place, which was followed by the birth of a large number of babies with congenital rubella. We hypothesised that this epidemic was related to immunisation practices. As there is no systematic surveillance for rubella in Greece we reviewed relevant information and delineated the events leading to this epidemic.
Methods
We sought all available information on immunisation policies and practices, vaccination coverage, serologically detected immunity, and the occurrence of rubella and congenital rubella in Greece.
We carried out a systematic review of the Greek medical literature by searching electronically the IATROTEK (1980-96) and the Athens Institute of Child Health (1979-96) databases for publications on rubella and congenital rubella, and by hand searching paediatric and other major medical journals published in Greece (1950-97) and proceedings of the annual panhellenic paediatric and medical conferences (1975-97). We also retrieved relevant publications cited in papers identified from these sources. All the studies identified were included, and we systematically evaluated the studies on vaccination coverage and serologically detected immunity, using as criteria the adequacy of documentation of methods, the study population, and the representativeness and size of the sample.
We assessed official documents and unpublished data of the Greek Ministry of Health and other public and private agencies for the period 1970-95. Notifications of rubella cases and mortality from rubella and congenital rubella for the years 1960-95 were examined with data from the National Statistical Service of Greece.18
Results
Immunisation policies
Vaccines against rubella and measles, mumps, and rubella became commercially available in Greece around 1975.19 Since 1977 eminent Greek paediatricians have recommended that children be immunised with the measles, mumps, and rubella vaccine at the age of 15 months.w1 w2 This started in the private sector, which was used by an estimated 56% of children in Athens in the late 1970s.w3Because rubella vaccination was classed as “optional” by the Ministry of Health at this time public services offered rubella immunisation on request only to girls aged 10-14 years.w4 A limited rubella vaccination programme for adolescent girls and special groups of young women was introduced in 1980.w4 In 1975-80 the uptake of vaccination for measles in the second year of life, introduced in the late 1960s, was 1%, 5%, 10% 18%, 19%, and 43% in various groups of children.w3 w5-w8
The national immunisation schedule was revised in 1987, but the new scheme gave doctors the option of vaccinating children aged 15 months with the measles monovalent vaccine or the measles, mumps, and rubella vaccine, and it included no recommendation for the vaccination of adolescent girls or young women for rubella.w9 In 1989 the Ministry of Health declared the immunisation of all children for measles, mumps, and rubella aged 1 “compulsory”w10 and this was extended to the public sector. In 1991 a two dose vaccination scheme (at 15 months and 11-12 years) was adopted for boys and girls.w11 No policy has ever been introduced to vaccinate susceptible women postpartum.
Rubella has been a notifiable disease in Greece since the 1950s, but notification is not comprehensive and the age of cases notified is not reported.18 The introduction of rubella immunisation did not change this nor was any surveillance system for congenital rubella syndrome established.
Vaccination coverage and serologically detected immunity
Vaccination uptake by children is not assessed systematically in Greece. Several studies have been carried out with different methodologies. We identified 18 published studies reporting coverage for rubella vaccination before 1993 (see table A on website).w5-w8 w12-w25 These studies showed that during the late 1970s and the 1980s vaccination coverage for rubella increased only slowly, remaining consistently below 50%, and did not reach 50%-60% before 1990.
Although 17 serological studies on rubella immunity were identified (see table B on website),w17 w26-w41 only five, which studied populations of pregnant women in Athens, are comparable. These show a gradual increase in the proportion of pregnant women susceptible to rubella during the 1980s: 12% (1971-5), 11% (1980), 17% (1981), 24% (1984-9), and 36% (1990-1).w28 w33 w35 w37 w40
Rubella and congenital rubella syndrome
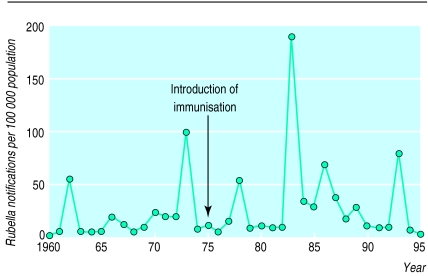
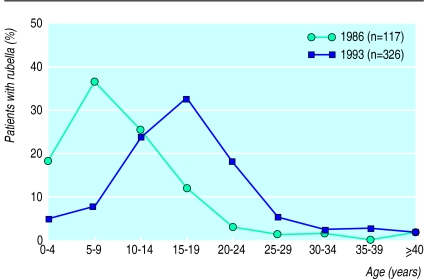
For several years after the introduction of the immunisation of children aged 1 year no substantial changes in the incidence of rubella, as reflected by notified cases, were observed in Greece, and major epidemics continued to occur (fig 1).18 Data on the age distribution of cases are limited. A large study on reported morbidity in the early 1960s in Athens estimated that the mean age at infection was 8.5 years,w42 and a subsequent serological study of immunity to rubella gave accordant results.w26 The age of patients with rubella attending health services in the province of Attiki (Athens and its surrounds) in 1993 and in previous years was studied retrospectively; a shift in the age distribution towards older ages (fig 2) was documented in all the services studied.20,21 In 1993 the mean age of patients with rubella was 17 years and 64% were 15 years or older (n=468), whereas in 1983 and 1986 the age distribution was similar to the prevaccination years.20 Although the number of notified cases was smaller in 1993 than in 1983 the incidence of rubella in people aged 15 years or more was higher in 1993 than in the 1983 epidemic, which was the largest recorded in Greece.20
Figure 1.
Notifications of rubella in Greece, 1960-95. Source: National Statistical Service of Greece18
Figure 2.
Age distribution of patients with rubella attending outpatient departments of general hospital in greater Athens, 1986 and 1993. Source: Panagiotopoulos et al 199620
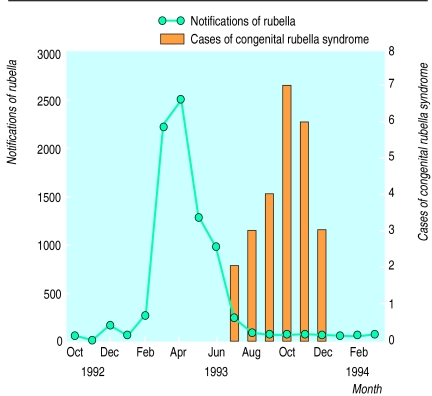
Only sporadic cases of congenital rubella were reported in Greece in 1950-92: 1952 (one case), 1954-5 (five), 1974-8513, 1980 (one), 1983 (three), and 1986-7 (four).w43-w49 A systematic surveillance system for congenital rubella syndrome has never existed, but an investigation of key health services by the Ministry of Health after the 1983 rubella epidemic concluded that “no problems appeared due to infection of pregnant women.”w50 An investigation of babies admitted to hospital with a diagnosis of congenital rubella was made after the 1993 epidemic, in which 25 serologically confirmed cases were recorded (IgM positive)—that is, 24.6 per 100 000 live births in 1993 (table).22 All had serious symptoms and seven were known to have died within the 12 month period of investigation (table).22 The pattern of the congenital rubella epidemic followed closely that of the rubella epidemic, with a lag of approximately 6-7 months (fig 3). Infant mortality from congenital rubella syndrome, as recorded by the National Statistical Service of Greece, was 3.9 per 100 000 live births in 1993 (four deaths), a higher rate than in previous years, but the numbers are small.19
Figure 3.
Notifications of rubella by month of diagnosis, and cases of congenital rubella by month of birth in epidemic in Greece, 1993. Source: National Statistical Service of Greece18 (notifications of rubella) and Panagiotopoulos et al22 (cases of congenital rubella syndrome)
Discussion
In this paper we synthesised the available information on rubella and congenital rubella in Greece, and we provided evidence that the rubella epidemic of 1993 affected young adults at a rate higher than in previous epidemics and led to the birth of an increased number of babies with congenital rubella syndrome, probablythe largest number in Greece after 1950. This increase seems to be due to the inconsistent immunisation policies implemented for about 15 years. From around 1975 boys and girls aged 1 year received the measles, mumps, and rubella vaccine without policies to attain high vaccination coverage and to protect adolescents and women of childbearing age. It has been stressed that such immunisation practices may lead to an increase in the occurrence of congenital rubella,4,6–14 but this phenomenon has not been previously reported.
What is already known on this topic
Vaccinating children aged 1 year against rubella interrupts transmission of the virus and increases the age at infection of non-immunised people
Theoretical concerns exist, backed by evidence from modelling, that if vaccination coverage is low this shift of age at infection can increase rubella incidence among older age groups and lead to an increase in congenital rubella
What this paper adds
The present study provides evidence that this phenomenon occurred in Greece, where immunisation of boys and girls aged 1 year with the measles, mumps, and rubella vaccine was introduced in the mid-1970s without policies to attain high vaccination coverage and to protect adolescents and young women
In 1993 a major rubella epidemic took place, affecting women of childbearing age at a rate higher than in previous epidemics
This was followed by the birth of the largest number of babies with congenital rubella syndrome recorded in the country
The absence of good quality data on rubella activity in Greece is an inherent problem. It is actually a component of the incident described: the introduction of rubella immunisation, not being part of a coherently designed policy, was not accompanied by the establishment of any surveillance system.
Notification data underestimate the true incidence but reflect secular trends and epidemic peaks.19 The shift of the age distribution of cases of rubella in 1993, with an increase in incidence among people aged 15 years or more, is confidently documented, given the magnitude of the effect (fig 2) and its consistency in different studies.20,21 The cases of congenital rubella recorded in 1993 all had serious symptoms, were serologically confirmed, and were diagnosed within 12 months of the end of the rubella epidemic (table).22 Such severe cases are estimated to account for fewer than 50% of all cases of congenital rubella.23 The quality of data from previous years is probably poorer and underreporting even greater (for example, only small numbers of cases of congenital rubella were reported after the major epidemics of 1973 and 1983), but it is unlikely that a major epidemic of congenital rubella, comparable to that of 1993, took place without being mentioned in the published literature or official records. Deaths from congenital rubella syndrome are substantially underreported. Despite the small numbers, the marginal increase of mortality in 1993 compared with previous years is in line with other findings. Not all the studies on vaccination coverage and serologically detected immunity were adequately designed, but as a whole they probably reflect the true trends and order of magnitude of estimates, given the agreement of their results (see tables A and B on website). Exclusion of studies that documented methods inadequately or used non-representative samples does not change the picture (see tables A and B on website). The composite data of this paper, derived from several independent sources, are consistent in portraying different aspects of the same phenomenon.
A comprehensive policy for the prevention of congenital rubella syndrome is a public health priority in Greece. This must include the immunisation of young adults, a large proportion of whom are susceptible to rubella, along with systematic measures to achieve high vaccination coverage of children and adolescents. It must also include competent surveillance systems for rubella and congenital rubella syndrome and evaluation of immunisation programmes. Such a policy has not been adopted to date.
The incident described should serve as a cautionary note on the potential hazards of the introduction of rubella immunisation, especially in countries that have difficulty in assuring high vaccination coverage because of lack of resources or a limited tradition of public health. It is also a reminder of the need to sustain high vaccination coverage in countries with established immunisation programmes, particularly in view of the recent adverse publicity regarding the safety of the measles, mumps, and rubella vaccine.24
Table.
Main characteristics of newborns with confirmed congenital rubella syndrome recorded during epidemic in Greece, 1993*. Modified from Panagiotopoulos et al22
| Month of birth (sex) | Region of residence | Age (months) at diagnosis | Clinical and laboratory manifestations reported† | Died (age)‡ |
|---|---|---|---|---|
| July | ||||
| Male | Aegean islands | <1 | Patent ductus arteriosus, developmental retardation, cryptorchidism | — |
| Male | Greater Athens | <1 | Thrombocytopenic purpura, seizures | — |
| August | ||||
| Female | Greater Athens | 3 | Pulmonary artery stenosis and hypoplasia, patent ductus arteriosus, cataract, hypertonia, intracranial calcifications, failure to thrive | — |
| Unknown | Macedonia | <1 | Hepatosplenomegaly, pigmentary retinopathy, hypotonia, developmental retardation, prematurity | — |
| Unknown | Macedonia | <1 | Hepatosplenomegaly, corneal opacity, petechiae, thrombocytopenia, maculopapular rash, radiographic bone lucencies, hypotonia, intrauterine growth retardation, prematurity, failure to thrive, anaemia | 4 months |
| September | ||||
| Female | Crete | <1 | Patent ductus arteriosus, ventricular septal defect, intrauterine growth retardation | — |
| Male | Greater Athens | <1 | Thrombocytopenic purpura, intrauterine growth retardation, prematurity | — |
| Male | Greater Athens | <1 | Patent ductus arteriosus, petechiae, thrombocytopenia | — |
| Female | Aegean islands | <1 | Patent ductus arteriosus, atrial and ventricular septal defect, microphthalmia, macular rash, jaundice, hypertonia, large anterior fontanelle | 1 month |
| October | ||||
| Male | Rest of Central Greece and Evia§ | <1 | Cataract, glaucoma, ventricular septal defect, intrauterine growth retardation, failure to thrive | — |
| Female | Greater Athens | <1 | Microcephaly, patent ductus arteriosus, atrial septal defect, thrombocytopenic purpura, hepatomegaly, jaundice | <1 month |
| Female | Aegean islands | <1 | Patent ductus arteriosus, cataract, microphthalmia, intracranial calcifications | — |
| Female | Greater Athens | 5 | Tetralogy of Fallot, cataract | — |
| Male | Greater Athens | <1 | Patent ductus arteriosus, atrial and ventricular septal defect, radiographic bone lucencies, intrauterine growth retardation | — |
| Male | Peloponnissos | <1 | Patent ductus arteriosus, tricuspid insufficiency, thrombocytopenic purpura, hepatomegaly, jaundice, hearing loss, prematurity | <1 month |
| Male | Greater Athens | <1 | Cataract, glaucoma, midline cerebral cyst | — |
| November | ||||
| Female | Greater Athens | <1 | Ebstein anomaly, cataract | <1 month |
| Male | Rest of Central Greece and Evia§ | 1 | Patent ductus arteriosus, cataract, microphthalmia, hepatosplenomegaly, thrombocytopenia, anaemia | — |
| Female | Aegean Islands | <1 | Patent ductus arteriosus, cataract, hearing loss | — |
| Female | Crete | <1 | Congenital heart disease (unspecified), cataract, hydrocephalus | <1 month |
| Male | Ipiros | 2 | Patent ductus arteriosus, cataract, petechiae, hepatosplenomegaly, seizures | — |
| Female | Greater Athens | 5 | Hepatosplenomegaly, seizures, hypotonia, intracranial calcifications, intrauterine growth retardation, failure to thrive | 5 months |
| December | ||||
| Female | Rest of Central Greece and Evia§ | <1 | Patent ductus arteriosus, thrombocytopenic purpura, hepatomegaly, hearing loss, intrauterine growth retardation | — |
| Male | Peloponnissos | 1 | Patent ductus arteriosus, jaundice, pneumonitis, hearing loss, developmental retardation, prematurity, failure to thrive | — |
| Male | Thessalia | <1 | Pulmonary artery stenosis, atrial septal defect, cataract | — |
Period of investigation: 1 July 1993 to 31 June 1994. Confirmed cases reported from nine hospitals. †All cases positive for rubella specific IgM antibodies.
Death within period of investigation. §Rest of Central Greece and Evia is one of the 10 regions of Greece.
Acknowledgments
We thank Dr Sheena Nakou (Institute of Child Health, Athens for her assistance, Professor Manolis Kogevinas (Institut Municipal d' Investigació Mèdica, Barcelona), Dr Stuart Logan (Institute of Child Health, London), and Professor Nick Spencer (University of Warwick, Coventry) for their comments on earlier drafts of this paper.
Editorial by King
Footnotes
Funding: Institute of Child Health, Athens, Greece.
Competing interests: None declared.
References
- 1.Cooper LZ. The history and medical consequences of rubella. Rev Infect Dis. 1985;7(suppl 1):2–10S. doi: 10.1093/clinids/7.supplement_1.s2. [DOI] [PubMed] [Google Scholar]
- 2.Miller E, Cradock-Watson JE, Pollock TM. Consequences of confirmed maternal rubella at successive stages of pregnancy. Lancet. 1982;2:781–784. doi: 10.1016/s0140-6736(82)92677-0. [DOI] [PubMed] [Google Scholar]
- 3.Best JM. Rubella vaccines: past, present and future. Epidemiol Infect. 1991;107:17–30. doi: 10.1017/s0950268800048640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knox EG. Theoretical aspects of rubella vaccination. Rev Infect Dis. 1985;7(suppl 1):194–17S. doi: 10.1093/clinids/7.supplement_1.s194. [DOI] [PubMed] [Google Scholar]
- 5.Bart KJ, Orenstein WA, Preblud SR, Hinman AR. Universal immunization to interrupt rubella. Rev Infect Dis. 1985;7(suppl 1):177–84S. doi: 10.1093/clinids/7.supplement_1.s177. [DOI] [PubMed] [Google Scholar]
- 6.Knox EG. Strategy for rubella vaccination. Int J Epidemiol. 1980;9:13–23. doi: 10.1093/ije/9.1.13. [DOI] [PubMed] [Google Scholar]
- 7.Anderson RM, May RM. Vaccination against rubella and measles: quantitative investigation of different policies. J Hyg (Camb) 1983;90:259–325. doi: 10.1017/s002217240002893x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hethcote HW. Measles and rubella in the United States. Am J Epidemiol. 1983;117:2–13. doi: 10.1093/oxfordjournals.aje.a113511. [DOI] [PubMed] [Google Scholar]
- 9.Van Druten JAM, de Boo T, Plantinga AD. Measles, mumps and rubella: control by vaccination. Dev Biol Stand. 1986;65:53–63. [PubMed] [Google Scholar]
- 10.Dudjeon JA. Selective immunization: protection of the individual. Rev Infect Dis. 1985;7(suppl 1):185–90S. doi: 10.1093/clinids/7.supplement_1.s185. [DOI] [PubMed] [Google Scholar]
- 11.Bötiger M, Forsgren M. Twenty years' experience of rubella vaccination in Sweden: 10 years of selective vaccination (of 12-year-old girls and of women postpartum and 13 years of a general two-dose vaccination. Vaccine. 1997;15:1538–1544. doi: 10.1016/s0264-410x(97)00068-6. [DOI] [PubMed] [Google Scholar]
- 12.Center for Disease Control. Rubella prevention. Recommendations of the Immunization Practices Advisory Committee. MMWR Morb Mortal Wkly Rep. 1990;39(RR-15):1–18. [PubMed] [Google Scholar]
- 13.A second dose of MMR vaccine for children in the United Kingdom. Commun Dis Rep CDR Wkly. 1996;6:259. [PubMed] [Google Scholar]
- 14.Robertson SE, Cutts FT, Samuel R, Diaz-Ortega J-L. Control of rubella and congenital rubella syndrome (CRS) in developing countries. Part 2: vaccination against rubella. Bull World Health Organ. 1997;75:69–80. [PMC free article] [PubMed] [Google Scholar]
- 15.Cutts FT, Robertson SE, Diaz-Ortega J-L, Samuel R. Control of rubella and congenital rubella syndrome (CRS) in developing countries. Part 1: burden of disease from CRS. Bull World Health Organ. 1997;75:55–68. [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organisation. Health for all targets. The health policy for Europe. European Health for All Series, No 4. Copenhagen: WHO; 1991. pp. 31–33. [Google Scholar]
- 17.De la Malta I, De Wals P. Policies for immunization against rubella in European countries. Eur J Epidemiol. 1988;4:175–180. doi: 10.1007/BF00144747. [DOI] [PubMed] [Google Scholar]
- 18.National Statistical Service of Greece. Monthly statistical bulletin (years 1960 to 1995). Athens: NSSG.
- 19.Panagiotopoulos T, Antoniadou I, Valassi-Adam E. Major epidemic of congenital rubella in Greece in 1993: a serious public health problem. Report on a study of the Institute of Child Health. Athens: Institute of Child Health; Dec 1995. (In Greek.)
- 20.Panagiotopoulos T, Antoniadou I, Antonopoulou E, Gogoglou V, Taousani S, Lakaki E, et al. Increase of age at infection in Attiki (Greece) during the rubella epidemic of 1993. Arch Hellenic Med. 1996;13:211–219. . (In Greek.) [Google Scholar]
- 21.Panagiotopoulos T, Antoniadou I, Delis D, Giannakos A, Chrysomallou P, Bartsokas C, et al. Increase of age at infection in the childhood population of Athens during the rubella epidemic of 1993. Ann Clin Paediatr Univ Atheniensis. 1995;42:175–180. . (In Greek.) [Google Scholar]
- 22.Panagiotopoulos T, Antoniadou I, Valassi-Adam E. Congenital rubella syndrome epidemic in Greece in 1993. A report of 25 confirmed cases. Paediatriki. 1997;60:582–591. . (In Greek.) [Google Scholar]
- 23.Orenstein WA, Preblud SR, Bart KJ, Hinman AR. Methods for assessing the impact of rubella infection. Rev Infect Dis. 1985;7(suppl 1):22–8S. doi: 10.1093/clinids/7.supplement_1.s22. [DOI] [PubMed] [Google Scholar]
- 24.Wakefield AJ, Murch SH, Anthony A, Linnell J, Casson DM, Malik M, et al. Ileal-lymphoid-nodular hyperplasia, non-specific colitis and pervasive developmental disorder in children. Lancet. 1998;351:637–641. doi: 10.1016/s0140-6736(97)11096-0. [DOI] [PubMed] [Google Scholar]