Abstract
Patients with presenting with left-sided FTLD syndromes sometimes develop a new preoccupation with art, greater attention to visual stimuli, and increased visual creativity. We describe the case of a 53-year-old, right-handed man with a history of bipolar disorder who presented with language and behavior impairments characteristic of FTLD, then developed motor symptoms consistent with a second diagnosis of amyotrophic lateral sclerosis. Though the patient had never created visual art before, he developed a compulsion for painting beginning at the earliest stages of his disease, and continued producing art daily until he could no longer lift a paintbrush because of his motor deficits. Upon autopsy, he was found to have ubiquitin and TDP43-positive inclusions with MND pathology. This case study details the patient’s longitudinal neuropsychological, emotional, behavioral, and motor symptoms, along with structural imaging, neurologic, and neuropathologic findings. Multiple examples of the patient’s art are depicted throughout all stages of his illness, and the possible cognitive, behavioral, and neurologic correlates of his new-onset visual artistry are discussed.
Keywords: frontotemporal lobar degeneration, amyotrophic lateral sclerosis, art, emotion, social behavior
INTRODUCTION
Frontotemporal lobar degeneration is a progressive neurodegenerative disorder disproportionately affecting the frontal and anterior temporal lobes (2). Some clinical subtypes of FTLD help illuminate the nature of artistic creativity. Previous case studies of patients with left-sided FTLD syndromes, whether temporally predominant (semantic dementia) or frontally predominant (progressive non-fluent aphasia) reveal that a new preoccupation with art, greater attention to visual stimuli, and increased visual creativity sometimes occur during the early stages of these kinds of dementia. In contrast, Alzheimer’s disease (AD), which typically first affects the posterior parietal and medial temporal areas, is associated with decreased visuo-constructive ability (7, 19). Of further interest, creativity in FTLD has been observed in visual art, music, mechanics, and mathematics, but not in writing or poetry (1, 17).
A number of other descriptions of artistically creative FTLD patients exist in the literature. In one series of case studies, left-temporal variant FTLD patients, who are known for their severe semantic loss, exhibited a newfound interest in art and preferred making representational drawings of landscapes, animals, and people. Abstract or symbolic art was notably absent (7, 17). In a second study, a 57-year-old right-handed female artist’s left-sided frontal and temporal atrophy correlated with her deteriorating language and social skills but increased creativity in her art-making. Unlike the prior case series, her painting evolved from more traditional landscapes and representational art to freer, more expressive, and abstract forms with the progression of her dementia (9). In a third study, a 56-year-old right-handed businessman with no previous interest in art began painting for the first time with the onset of FTLD. He displayed heightened visual awareness to his environment, especially light and sound, even as his language and behavior deteriorated (10).
While FTLD presents with a variety of clinical syndromes depending on the brain regions affected, these clinical syndromes cannot yet be used to definitively predict the underlying neuropathological subtype. The above reports of increased creativity in FTLD describe patients whose pathological subtype was either unknown or was consistent with one of the pure FTLD pathology types, i.e., either tau positive, or tau-negative ubiquitin and TDP43-positive inclusions with no motor neuron disease (MND) pathology. To our knowledge, no reports of increased creativity in patients with the FTLD-MND pathological subtype (ubiquitin and TDP43-positive inclusions with MND pathology) have yet been published. Clinically, patients with MND can gradually lose limb, bulbar, and respiratory muscle function as a result of gradual degeneration of both upper and lower motor neurons, and up to 50% of these patients manifest some degree of cognitive impairment (3, 23). Patients found to have mixed FTLD-MND pathology can present with clinical features anywhere on the spectrum between typical FTLD (behavior-predominant with few if any motor symptoms) and typical amyotrophic lateral sclerosis (ALS) (motor predominant with few behavior and cognitive changes).
Here we describe the case of a 53-year-old, right-handed man who first presented with the language and behavior impairments characteristic of FTLD, then developed upper and lower motor neuron deficits consistent with a second diagnosis of amyotrophic lateral sclerosis. Upon autopsy, the patient was confirmed to have combined FTLD-MND neuropathology. This case study provides a detailed description of VW’s cognitive, emotional, behavioral, and motor symptoms, which initially enabled but eventually limited his productivity as a visual artist. From another perspective, the evolution of the quality of VWs artwork provides another means of understanding his neurodegenerative decline.
CASE HISTORY
Prior to 2002
Clinical History
VW was a well-educated man whose lifetime work demonstrated a strong commitment to civil rights. After earning his bachelors degree, he dedicated himself to organizing workers’ unions, including among school district bus and taxi cab drivers. VW eventually attended law school, and then started a private practice involving immigration, personal injury, bankrupcy, divorce, and employment rights.
During his twenties, VW was diagnosed with bipolar disorder, type 1, and was hospitalized three times for episodes of mania and bizarre behavior, after which he had no more frank relapses. VW had a history of romantic relationships to drug-addicted women who “used him for housing.” While on vacation in Asia in 1999, at the age of 50, the patient married a woman that he had known for less than one month. The relationship later ended in divorce. VW had a strong family history of mental illness, including twenty-three maternal relatives with bipolar disease. He also had one grandmother who suffered from an unspecified dementia beginning at the age of 73.
In May 2001, at the age of 52, VW suddenly quit his job as a lawyer in southern California and moved to San Francisco. He provided only a vague rationale for his sudden decision to quit his job and change residence. His mother was surprised when she saw that her son “looked like a homeless person” upon arrival in San Francisco, and was simply “not the same person he used to be.” After the move, he was unable to obtain employment, but demonstrated a complete lack of insight into the reasons why, concluding that there is “something bizarre about the city of San Francisco.” After six months, still without work and unable to support himself, he left the city to live with his mother in November 2001.
At this time VW’s behavioral symptoms became evident to his family. They saw that he had begun to exhibit odd, antisocial, and compulsive behaviors. For example, he needed to drink ten glasses of water a day in fifty-minute increments. Lunch and dinner were eaten at exactly 12 noon and 6 pm. He started collecting coins in a compulsive manner, turning over stones to look for pennies, gathering tips from the tip jar at a local restaurant and rifling through others’ purses. No longer wanting to change clothes, bathe, or wear deodorant, his appearance grew increasingly disheveled. His choice of loud shirts and sandals made him look “just a little off.” His mother noticed lapses in his memory, including missed appointments, repetitive questioning, and difficulty remembering remote autobiographical events. Word output diminished and speech became less prosodic. He demonstrated trouble with comprehension and word-finding. While still able to complete most of his activities of daily living, he became unable to perform complex tasks such as writing checks, paying bills, or balancing a checkbook. His visuospatial function, as demonstrated by driving and parking ability, was well-preserved.
Visual Artistry
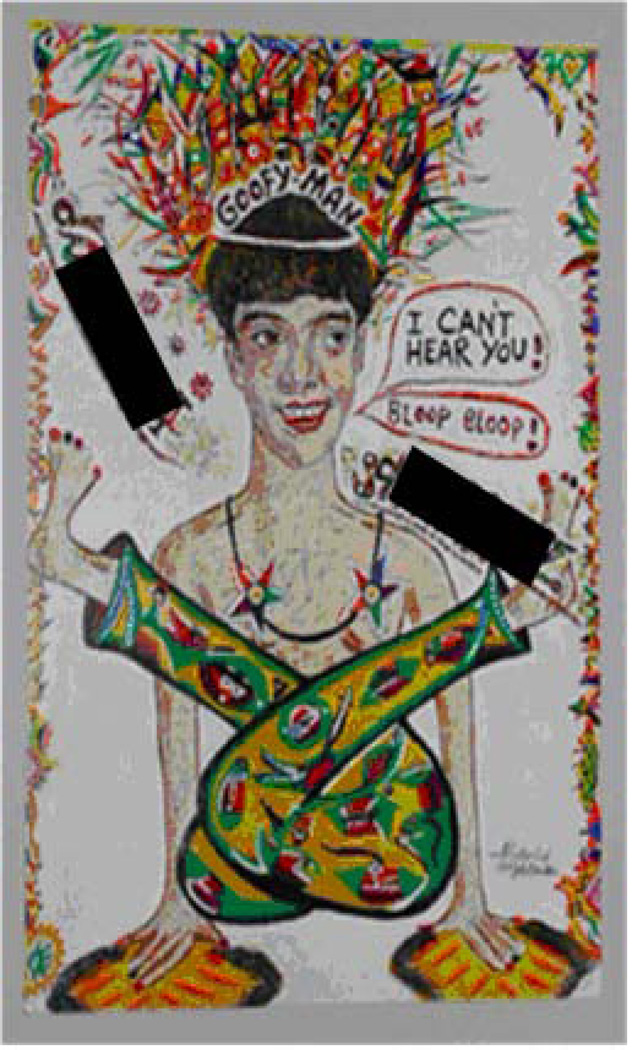
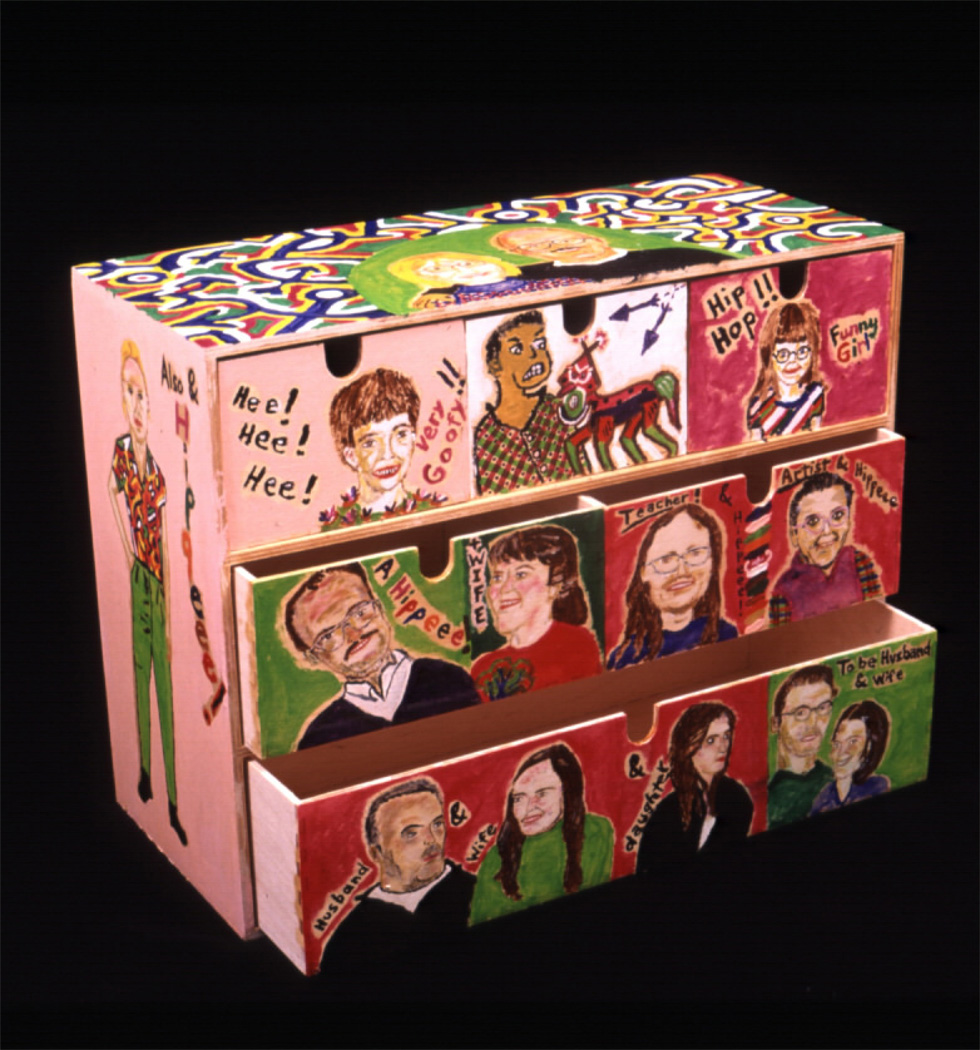
Paradoxically, while his language and behavior were deteriorating, VW immersed himself in painting. Never previously interested in art, he became preoccupied with sculpting and painting in 2000–01. While the expressions on the faces made earlier during the course of his illness are bizarre, they exhibit expressive detail. Figure 1 is an early portrait of his cousin (2001), richly drawn to depict the subject in an impossibly twisted position, dressed in wild clothing, and making odd exclamations. Figure 2 features a box of drawers on which VW painted his family portrait. As reported by his mother, there is enough personal detail that each individual portrait bears a striking resemblance to a family member.
Figure 1.
One of the earliest paintings completed by VW (2001) is a portrait of his cousin (his name was redacted from the picture for purposes confidentiality). He is portrayed as a wildly costumed “Goofy Man” twisted into an impossible pose. His dialogue balloons say “I can’t hear you,” and “Bloop, bloop.”
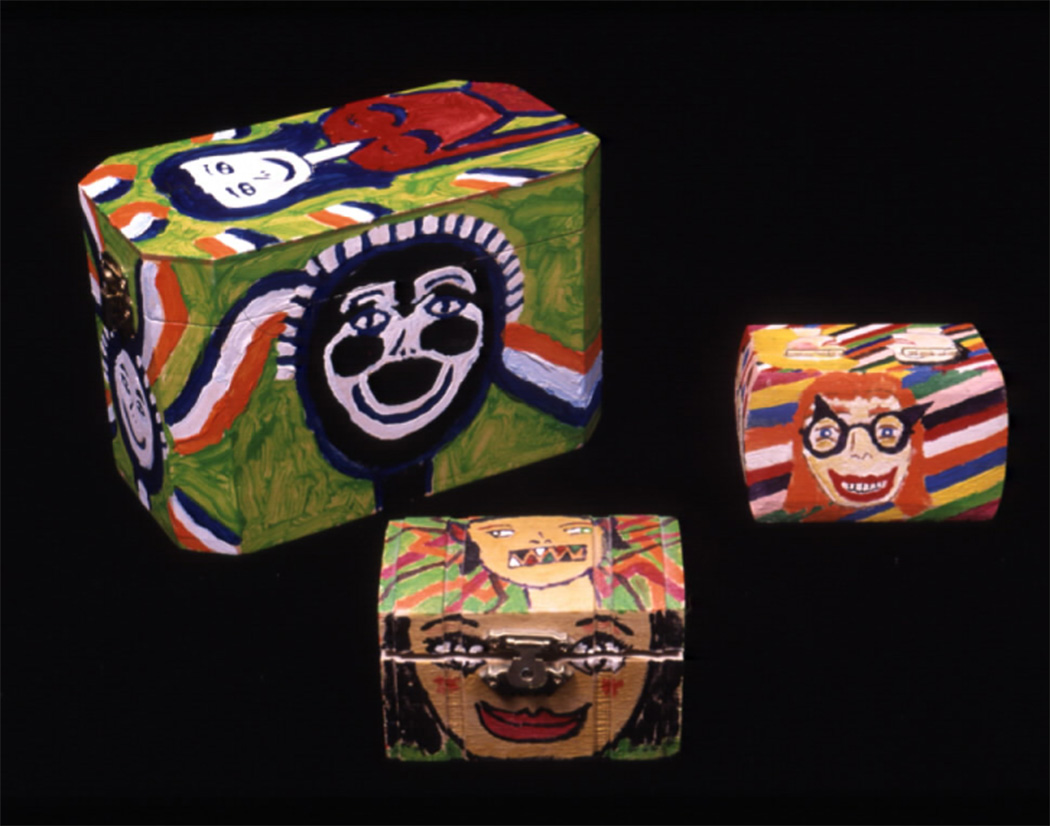
Figure 2.
A box of drawers that VW painted as a family portrait early in his disease. According to family members, the portraits bear a striking resemblance to each family member. VW himself is painted on the left side of the box, his mother and father on the top side, his niece and nephew on the top row, and his siblings and their spouses on the bottom two rows.
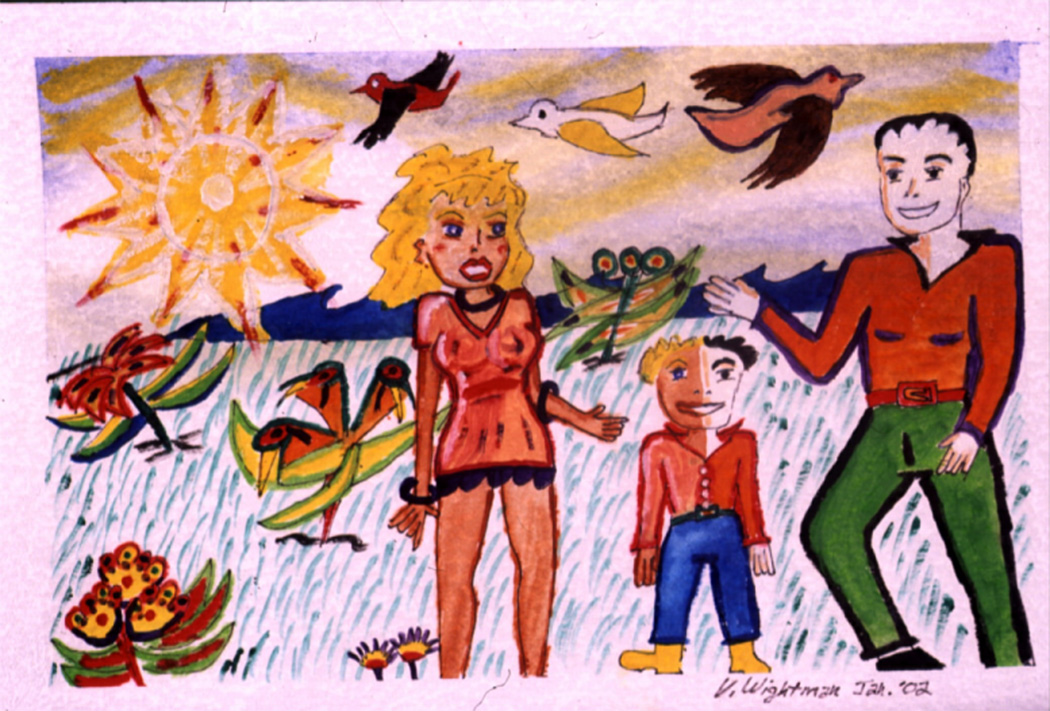
VW brought in a series of colorful paintings to his first visit with a therapist in January 2002 (See Figure 3 and Figure 4). Like his other earlier works, they unmistakably reference the outside world. While the space is relatively flat (no sense of perspective or foreshortening, with equal visual weight assigned to foreground and background), the setting is fairly naturalistic. The people stand, sit, and lie on the green grass; flowers bloom, birds fly, and sky hangs above. These paintings represent a familiar scene of people enjoying themselves at the park on a sunny day. They are engaged in recognizable relationships—pairings of heterosexual couples, oftentimes in sexually suggestive situations. The three people in the painting shown in Figure 3 appear to be a traditional family unit. However, even when the figures are engaged in sex or dance, as in Figure 4, they seemed oddly disconnected.
Figures 3.
These pictures were produced at a time when clear behavioral and neurological changes were occurring in early 2002. They reveal a bright, varied color palette, a variety of brushstrokes, and relatively complex compositions. While the representation of space is relatively flat, VW has staged his characters in a naturalistic environment. However, the figures in many of VW’s drawing often display odd expressions on their faces, many with teeth showing. His characters often appear disinhibited (e.g., sexually provocative).
Figure 4.
These pictures were produced at a time when clear behavioral and neurological changes were occurring in early 2002. They reveal a bright, varied color palette, a variety of brushstrokes, and relatively complex compositions. While the representation of space is relatively flat, VW has staged his characters in a naturalistic environment. However, the figures in many of VW’s drawing often display odd expressions on their faces, many with teeth showing. His characters often appear disinhibited (e.g., sexually provocative).
Compared to his later work, these earlier paintings also manifest a wider variety of mark-making and color. The color palette in VW’s early work uses color from across the entire spectrum. His color choices, while generic, certainly reflect the natural world: the grass and foliage are green, skin tones are light pink or brown, and hair is blond or dark brown. The clothing on his characters is fairly conservative and stereotyped: all of the women wear skirts or dresses while all of the men wear shirts and pants. On closer inspection, however, VW’s characters wear odd expressions on their faces: some show teeth and appear happy, others appear shocked. Besides the fact that VW became newly preoccupied with art, perhaps these characters’ bizarre expressions provided an early visual clue to his dementia.
2002
General & Neurologic Exam
VW first visited the UCSF Memory and Aging Center in May of 2002 at the age of 53. His hair was pulled back into a ponytail and he wore a loud Hawaiian shirt. During the interview, he drank a measured amount of water from a bottle every 15 minutes. Although cooperative, he demonstrated a flat affect interrupted by an occasional smile. He spoke slowly, demonstrating a paucity of spontaneous speech, and responded to questions only after a significant pause. His speech was characterized by a mild stutter and was low in tone and volume. He showed fair comprehension, good repetition, but poor naming of common objects. Motor exam was remarkable for slightly decreased strength (5-/5) in his deltoids and biceps bilaterally, mild atrophy in his arms, and marked fasciculations over the sternocleidomastoid muscle. Reflexes revealed an equivocal Babinski’s sign in the left foot. Otherwise, the cranial nerve exam, sensory exam, and gait were grossly normal. Beginning at this time and over the course of his illness, he was perscribed Zoloft and Zyprexa, and participated in occupational therapy.
A diagnosis of FTLD was made at this time, although VW also had semantic deficits consistent with semantic dementia. Given the fasciculations and weakness noted on initial neurological exam, the patient was referred to UCSF’s ALS center in July 2002. Electromyelogram demonstrated acute and chronic denervation and reinnervation changes in his right arm and chronic partial denervation and reinnervation in the left triceps muscle, consistent with a diagnosis of ALS.
Neuropsychological Exam
VW underwent detailed neuropsychological assessment in August of 2002 (see Table 1). At this initial testing, he already showed severe impairment in most aspects of his language functioning, including significant semantic loss, impaired syntax comprehension, and impaired phonemic and category fluency in response to both phonemic and category cues. In contrast, his visuospatial functioning was consistently in the average to high average range. This dissociation was reflected in his performance on memory testing. He performed within normal limits on tests of spatial memory, but was severely impaired on verbal memory tests, ostensibly because he was unable to comprehend many of the words used as test stimuli, thus could not learn or recall them. His executive functioning was variable, with intact working memory, design fluency, and visuospatial logical reasoning, but impaired set-shifting, rapid oral reading and response inhibition, cognitive flexibility and concept formation, and abstract reasoning. Throughout his illness, he consistently denied any decline in cognitive function, suggesting a general lack of insight.
Table 1.
VW demographic, functional, and neuropsychological data compared to normative data
| August 2002 | July 2003 | |||
|---|---|---|---|---|
| TEST (max possible score): | Score (%ile) | Rating | Score (%ile) | Rating |
| MMSE (30) | 28 (30.8) | Average | 14 (<0.10) | Impaired |
| Geriatric Depression Scale | 11 | WNL | N/A | -- |
| Clinical Dementia Rating | ||||
| Total Score (3.0) | 1.0 | Mild Dementia | 2.0 | Moderate Dementia |
| Total of Box Scores (18) | 4.5 | -- | 9.0 | -- |
| Functional Activities Questionnaire (30) | 11 | 26 | ||
| Neuropsychiatric Inventory Total (144) | 26 | -- | 40 | -- |
| LANGUAGE: | ||||
| Boston Naming Test (60) | 40 (<0.1) | Impaired | 28 (<0.1) | Impaired |
| D-KEFS FAS (SS) | 4 (2.3) | Impaired | 1 (0.1) | Impaired |
| Animal Naming (# words/min) | 6 (0.3) | Impaired | 5 (<0.1) | Impaired |
| Hodges 64 Item Naming | 49 | 39 | ||
| Pyramids and Palm Trees: Words (52) | 40 (<0.1) | Impaired | N/A | -- |
| Pyramids and Palm Trees: Pictures (52) | 30 (<0.1)) | Impaired | N/A | -- |
| CYCLE (55) | 43(<0.1) | Impaired | N/A | -- |
| WAIS-III Information (SS) | 3 (0.9) | Impaired | 1 (0.1) | Impaired |
| VISUOSPATIAL FUNCTIONS: | ||||
| WAIS-III Block Design (SS) | 12 (74.2) | Average | 10 (50.0) | Average |
| WAIS-III Picture Arrangement (SS) | 10 (50.0) | Average | 1 (0.1) | Impaired |
| Modified Rey-O Copy (17)* | 17 (80.2) | High Average | 17 (80.2) | High Average |
| VOSP: Number Location (10) | 7 (1.4) | Impaired | 0 (0.1) | Impaired |
| Florida Affect Battery | ||||
| Face Discrimination (20) | 20 (74.2) | Average | N/A | -- |
| Affect Discrimination (20) | 14 (2.6) | Impaired | “ | -- |
| Name Affect (20) | 17 (36.3) | Average | “ | -- |
| Select Affect (20) | 13 (<0.1) | Impaired | “ | -- |
| Match Affect (20) | 14 (1.6) | Impaired | “ | -- |
| VISUAL MEMORY: | ||||
| WMS-III Visual Reproductions | ||||
| Immediate Delay I (SS) | 6 (8.8) | Borderline | 1 (0.1) | Impaired |
| Long Delay II (SS) | 7 (15.9) | Low Average | 3 (0.9) | Impaired |
| WMS-III Face Recognition | ||||
| Immediate Delay I (SS) | 7 (15.9) | Low Average | N/A | -- |
| Long Delay II (SS) | 8 (25.8) | Average | N/A | -- |
| Modified Rey-O Delay (17)* | 12 (30.8) | Average | 0 (<0.1) | Impaired |
| VERBAL MEMORY: | ||||
| California Verbal Learning Test-MS: | ||||
| 4-Trial Total Correct (36) | 16 (0.8) | Impaired | 10 (<0.1) | Impaired |
| 30” Free Recall (9) | 4 (2.3) | Impaired | 0 (0.1) | Impaired |
| 10’ Free Recall (9) | 3 (15.9) | Low Average | 0 (2.3) | Impaired |
| 10’ Recognition (9) | 6 (0.6) | Impaired | N/A | |
| WORKING MEMORY: | ||||
| WAIS-III Digit Span (SS) | 7 (15.9) | Low Average | 7 (15.9) | Low Average |
| WAIS-III Spatial Span (SS) | 8 (25.8) | Average | 3 (0.9) | Impaired |
| EXECUTIVE FUNCTIONS: | ||||
| WAIS-III Similarities | 1 (0.1) | Impaired | 1 (0.1) | Impaired |
| WAIS-III Matrix Reasoning | 6 (8.8) | Borderline | 6 (8.8) | Borderlin e |
| Wisconsin Card Sorting Test (64 cards) | ||||
| # categories (6) | 0 | Impaired | N/A | -- |
| # perseverative errors | 46 | Impaired | “ | -- |
| # conceptual level responses | 3 | Impaired | “ | -- |
| D-KEFS Design Fluency (SS) | ||||
| Filled Dots | 8 (25.8) | Average | 3 (0.9) | Impaired |
| Empty Dots Only | 7 (15.9) | Low Average | 3 (0.9) | Impaired |
| Set-Shifting | 8 (25.8) | Average | 6 (8.8) | Borderline |
| D-KEFS Trailmaking (SS) | ||||
| Numbers | 3 (0.9) | Impaired | 1 (0.1) | Impaired |
| Letters | 3 (0.9) | Impaired | 1 (0.1) | Impaired |
| Number-Letter Shifting | 1 (0.1) | Impaired | 1 (0.1) | Impaired |
| D-KEFS Color-Word Interference (SS) | ||||
| Color Naming | 1 (0.1) | Impaired | 1 (0.1) | Impaired |
| Word Naming | 1 (0.1) | Impaired | 1 (0.1) | Impaired |
| Color-Word Interference | 1 (0.1) | Impaired | N/A | -- |
Percentiles calculated using normal control data from 30 age-matched (M=56.8, SD=4.11) and education-matched (M=17.4, SD=2.2) normal control subjects; otherwise, published norms were used. SS=scaled scores in which 10=50th %ile.
Emotional Exam
VW also underwent comprehensive testing of his emotional functioning in August 2002. During the testing, his emotional reactivity, emotional understanding, and emotional memory were compared to ten age-matched control participants. VW and the controls were given a wide range of emotion-eliciting stimuli (e.g., viewing emotional film clips, hearing a startling noise, engaging in an embarrassing singing task, reliving emotional memories and engaging in a conversation with his mother regarding an emotionally evocative topic). Participants’ emotional responses were measured continuous via self-reports of emotional experience, coded facial displays of emotion, and measures of autonomic activation1.
Emotional reactivity
Overall, VW’s responses to emotionally evocative stimuli were diminished in comparison to controls. VW displayed little reaction to a loud gunshot-like noise, as measured by his self-reported experience, facial displays and autonomic arousal. In fact, he reported feeling “neutral” upon hearing a highly noxious (115 db) noise. In contrast, the ten controls reported feeling “bad,” “surprised,” and “afraid” upon hearing the noise. Controls were also observed with more surprised facial expressions and greater increases in skin conductance level (SCL), a physiologic indicator of sympathetic nervous system arousal. Furthermore, selected film clips that elicited marked feelings of fear, happiness, sadness, sexual arousal and disgust in the controls barely provoked VW. He reported feeling “good” in response to the happy film, and “bad” in response to the sad film, but felt no specific or nuanced emotion beyond these crude positive and negative states to any of the films. Furthermore, he showed no facial expressions appropriate to the emotional content of the films (e.g., smiles to the happy film, or frowning/tears to the sad film), his SCL was flat and voice monotonous when describing his feelings. In contrast, the controls showed facial expressions that were appropriate to the emotional content of the film clips, and an increased SCL.
VW also showed a marked deficit in self-conscious emotions. When watching a video-tape of himself singing (a task that produced much self-consciousness behavior in controls), VW did not display any signs of self-consciousness (e.g., smiling, blushing, touching his face, and averting his gaze). Rather, he focused on the technical aspects of his voice quality. Finally, when engaging in conversation with his mother about areas of conflict in their relationship (see excerpt below concerning his increasingly abusive treatment of the family dog), he showed no facial expression of emotion, his voice was monotonic, and his SCL remained at baseline levels. In controls, this conflict conversation produced much more emotional behavior and physiological response. In the following excerpt, VW demonstrates his lack of empathy and insight into the cruel behavior he practiced toward his dog.
Mother: When Max barks, do you sometimes squeeze him or put him between your legs and squeeze him…sometimes he squeals because you are hurting him. So I’m wondering, are you doing that because you are angry at him or because you are trying to get him to stop?
VW: I try to get him to stop barking.
Mother: Do you think there could be another way to do that? Sometimes you just talk to him and he stops. But you just keep doing that. This is something that you and I have had an issue with. Do you think you could just talk to him and not squeeze him so that he squeals?
VW: I don’t know what you are talking about.
Mother: Uh-huh. Do you know that you sometimes hurt him?
VW: I don’t believe that he hurts.
Emotional understanding
VW was able to identify some relatively simple emotional displays correctly, but not others. When watching film clips in which the main character experienced a particular emotion, he correctly identified fear, happiness, and sadness, but could not identify sexual arousal or disgust. In comparison, controls were able to identify the character’s emotion in all of the clips. Notably, he was able to recall the factual details of all of the films, even when he when he was not able to identify the emotion correctly. His deficits in emotional understanding were even more dramatically apparent in tasks in which he had to track moment-to-moment changes in another person’s emotions. This was apparent both when attempting to track the emotional valence (positive, neutral or negative) of a character in a film clip and of his mother when watching a video of their earlier interaction. In these more dynamic tasks, compared to controls, he tended to miss the minor fluctuations in the other person’s emotions and to have a positive bias to his ratings, even when the other person’s was clearly experiencing negative emotions2.
Emotional memory
VW appeared to retain some semblance of an inner emotional life. When asked to remember emotional events from his own life, prior to the onset of his illness, he became more impassioned. Specifically, when asked to recall a sad memory, he recalled the time when his wife left him, using appropriate gestures (i.e a somber voice, downcast eyes, sighs). When prompted to recall an angry memory, he recalled an event that occurred during his union organizing days, when he smashed the mirrors of the car owned by an antagonizing CEO. When describing this event, he expressively widened his eyes, furrowed his brow, and elevated his voice. Additionally, while talking about these personal events his skin conductance levels increased. Notably, while VW was more emotionally aroused when recalling these autobiographic memories, his responses were still more subdued and slower to onset compared to control participants.
Visual Artistry
By September 2002, VW was spending most of his time making art. However, he had begun showing signs of increased physical weakness. While previously an avid athlete, running several miles a week, performing pull-ups and pushups on a regular basis, the duration of his workout routines became shorter and lifting heavy objects more strenuous. VW’s mother noticed that his hands trembled and he had fasciculations throughout his body. The patient himself complained about becoming fatigued more easily. He also complained of weakness in his arms, and eventually found it increasingly difficult to hold a paintbrush in his right hand. Figure 5 is a painting that he made in mid-2002 that shows some loss of detail and broader brushstrokes, perhaps partly as a result of his loss of fine motor skills.
Figure 5.
In a picture painted in late 2002, the facial expressions and body types are much more generic and simplified, and their expressions more bizarre. The color palette is notably more simplified, unrealistic, and garish, and the brushstrokes appear somewhat less fine.
2003
Neuropsychological and Neurological Exam
VW was seen again at the MAC clinic in July 2003, and neuropsychological testing and structural MRI were repeated. In June of this year, he had been moved to a care facility. One year after his initial cognitive testing, VW’s performance had worsened in all cognitive domains, and he was unable to perform many of the tests at all due to his failure to comprehend test instructions. Notably, however, he was still able to produce excellent copies of visuospatial stimuli, had normal working memory for verbal stimuli, and performed at the 50th percentile on the Block Design test of 3-dimensional visuospatial logical reasoning (see Table 1).
VW’s second MRI showed clear progression of cortical gray matter loss, particularly in the insular and anterior temporal regions. The atrophy asymmetrically involved the left hemisphere with the most significant involvement seen in the left greater than right amygdala and the left anterior temporal lobe. Other regions of atrophy included the left middle and inferior frontal gyri, left posterior thalamus, bilateral superior temporal gyri and right temporal pole. These same regions tend to be even more atrophied in ALS/FTLD patients when compared to ALS patients, especially in the left hemisphere, suggesting a continuum of disease between ALS and FTLD. There was evidence of an old lacunar infarct in the left lenticular nucleus, but no evidence of other structural abnormalities. A voxel-based morphometry (VBM) analysis was performed on both VW’s structural MRI scan to determine how his regional gray matter volumes compared with a set of fifteen age-matched controls (see Figure 6).
Figure 6.
These voxel-based morphometry renderings of structural MRI scans performed in July, 2002 and July, 2003 demonstrate the selective atrophy of the left-greater-than-right sided temporal regions. Some involvement of the motor and premotor cortex in the distribution of the left middle cerebral artery can also be visualized, particularly regions responsible for R>L upper extremities. The comparison of the 2002 and 2003 images also demonstrates the rapid progression of atrophic changes, particularly in the frontal lobes, left greater than right. Figure threshold was set at p<0.001.
Visual Artistry
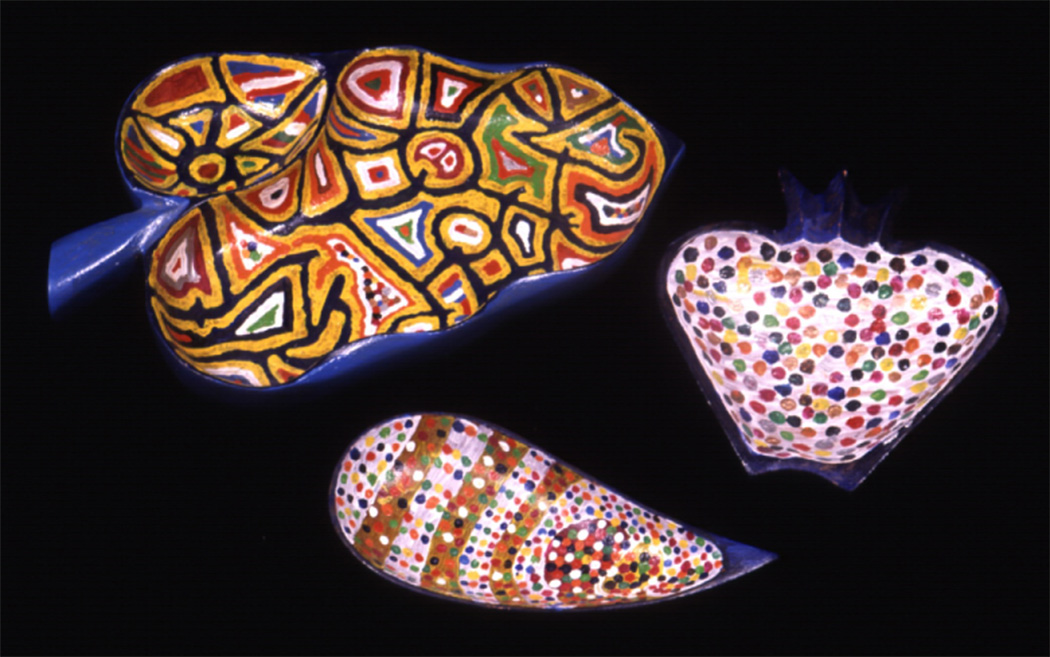
As his illness progressed, VWs artwork evolved from more complex, colorful compositions to simpler geometric designs. By 2003, VW preferred painting on the surfaces of manufactured paper maché and wooden sculptures, using the same coarse linework of richly pigmented, high contrast acrylic. As shown in Figure 7 and Figure 8, there is little composition. Besides the constructed animals and shapes which were not made by subject, there are no recognizable references to the outside world. Instead, he compulsively painted dots, stripes, and other designs. He made approximately twenty copies of the same sculptures and objects at a time.
Figure 7.
These geometrically painted objects represent VW’s typical art in the middle and later periods of his illness (2003–2004). VW compulsively painted these kinds of objects.
Figure 8.
These geometrically painted objects represent VW’s typical art in the middle and later periods of his illness (2003–2004). VW compulsively painted these kinds of objects.
The confluence of VW’s artistic evolution and the progression of his emotion deficits is perhaps best illustrated by his changing representation of faces. Figure 9 and Figure 10 show sets of painted wooden figures that VW made in 2003. In contrast to the faces he painted just two years earlier, these faces and forms are generic, similar, and simplified, and bear little likeness to any real person. The facial expressions are somewhat disturbing, particularly due to their wide-eyed appearance and the prominence of often pointed teeth. Notably, even when he started turning his attention to more geometric, simpler designs, he maintained the use of bizarre facial expressions.
Figure 9.
These represent stock figures emblematic of his later period (2003) that, in contrast to his earlier work in Figure 1–Figure 2, bear no recognizable resemblance to a real person. His depiction of faces has become increasingly bizarre and unrealistic.
Figure 10.
These represent stock figures emblematic of his later period (2003) that, in contrast to his earlier work in Figure 1–Figure 2, bear no recognizable resemblance to a real person. His depiction of faces has become increasingly bizarre and unrealistic.
VW’s methods of working changed as his motor neuron disease progressed. In his later pictures, it is difficult to separate the influence of his FTLD from that of his ALS. Because VW was unable to explain his artistic choices, it is reasonable to assume that his increasing weakness caused at least some part of his simplification. By the end of 2003, he had modified his painting technique by holding his brush at waist level while standing to paint over a table. His later, shakier line paintings reveal his unsteadiness of hand. Figure 11 shows two similar figures he made in 2003 and later in early 2004, and the increasing coarseness of his brushstrokes is evident.
Figure 11.
This figure represents two versions of one of the stock objects painted repeatedly by VW over the course of his last year of life. The deer on the right, painted in 2003, shows finer detail and more precise brushstrokes than the deer on the left, which he painted just before his death in early 2004. The differences can most likely be attributed to his progressive motor weakness and his difficulty holding and maneuvering a brush.
2004
Clinical Exam
By the time of his last clinic visit in February of 2004, VW was passive and withdrawn. His speech output had diminished to single word answers that were oftentimes echolalic. His motor weakness had progressed so that he was unable to comb his hair. Despite this, he continued to make art, holding the brush at waist level. His bulbar symptoms--including dysarthria, gagging, coughing, and dysphagia—continued to worsen. By his last visit, he had lost ten pounds over two weeks from his inability to swallow. VW’s behavior had improved toward the end of his illness—he was calmer, had stopped eloping from his care facility, and was even reported to have helped other residents, smiling and giving a cookie on occasion. In April of 2004, at the age of 55, VW died at his residential care home.
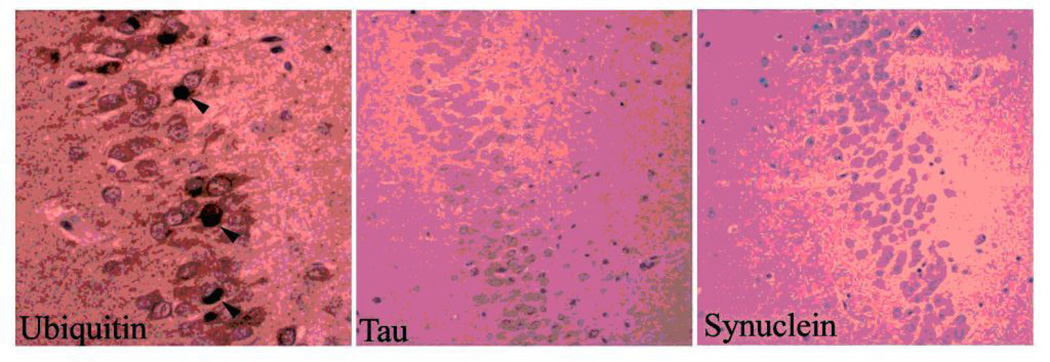
Pathology
On autopsy, VW’s brain weighed only 810 g with diffuse atrophy. Moderate neuronal loss and gliosis was seen in the superficial layers of the cortex and limbic structures. Immunohisto-chemical stains were performed for tau, alpha-synuclein and ubiquitin, along with a thioflavin stain. The predominant pathology was the presence of numerous ubiquitin-positive, tau and alpha-synuclein negative aggregates in the dentate neurons of the hippocampus (Figure 12). Scattered ubiquitin positive aggregates were also seen the limbic cortex and the neocortex. No neuronal loss was seen in the hippocampus or the midbrain. In the spinal cord, there was severe depletion of motor neurons in the anterior horns, more pronounced in the cervical sections. In addition, grossly, two infarcts were seen, one in the left temporal pole (2 cm) and the other in the left orbital frontal cortex (1 cm). Histologically, the frontal infarct showed a cavity with many macrophages and adjacent gliosis. The numerous ubiquitin-positive, tau and alpha-synuclein negative lesions in the hippocampus and elsewhere, along with the loss of spinal motor neurons and the clinical features, is diagnostic for FTLD-MND (frontotemporal lobar degeneration with motor neuron disease).
Figure 12.
The predominant pathology seen in the dentate neurons of the hippocampus were ubiquitin positive, tau and alpha-synuclein negative. Together with the loss of spinal motor neurons (not pictured) and the patient’s clinical picture, a diagnosis of FTLD-MND was confirmed.
DISCUSSION
In many respects, VW presented as a classic FTLD patient with changes in personality and social conduct, with the added component of MND becoming evident in progressive upper motor neuron weakness. However, this case is novel because the deterioration of his emotional and social functioning was illuminated not only though a comprehensive examination of his emotional reactivity, emotional comprehension, and emotional memory, but also through the window of the artwork he generated throughout the course of his illness.
Artistic Creativity in FTLD
Similar to other FTLD patients who have demonstrated new artistic creativity, VW’s visuospatial ability was remarkably preserved on neuropsychiatric testing (10). VW showed no prior interest in art but began painting people and animals in a representative fashion after the onset of his disease. As his illness progressed, his artwork became simpler and incorporated more geometric designs. His repertoire of brushstrokes, color use, and subject matter became more restricted, and less original. Also, he became less likely to depict people and objects in naturalistic settings, instead removing background and context altogether in favor of stylized, geometric designs.
Selective involvement of the temporal regions, with relative sparing of the frontal regions, seems to provide the anatomic rationale for this subset of patients (17). The concept of paradoxical functional facilitation, a term coined by Kapur, suggests that dysfunction in one sphere may allow the development of ability in another sphere because cognitive resources are redirected (1,7, 9). In cases like VW’s, the profound loss of semantic knowledge that results from anterior temporal lobe disease, when paired with preserved visuoperceptual functioning, may create a circumstance in which patients have a heightened sensitivity to the superficial visual features of their environment that is disconnected from the “content” of those elements. In other words, left temporal patients become less aware of the semantic connections surrounding the object they are observing, e.g., “This is a reindeer, it is large and brown, has fur, lives in cold climates with snow and pine trees, etc.”, which may free them to decontextualize the object and focus on its superficial aesthetic properties. This decontextualization seems to progress in some FTLD artists to the point where they project visually stimulating, abstract features onto the art object that are in no way semantically related to it, as is exemplified in VW’s habit of painting wooden reindeer with zigzagging geometric patterns in wild, unnatural color combinations (see Figure 7).
One of the most interesting lines of development in VWs artwork was his progressively more bizarre depiction of the facial features and social interactions of humans and animals. VW’s marked emotional flatness and inability to perceive others’ emotional states may provide at least a partial explanation for these features of his art. He had absent or very subdued responses to laboratory stimuli such as film clips, startle stimuli, his mother talking about difficult topics, and an embarrassing situation (evidenced by his reports of feeling little emotion, flat facial expression, no skin conductance response and monotone voice). Additionally he had difficulty deciphering the emotions of others, especially as the stimuli rapidly fluctuated and became more subtle. It seemed as though VW was cognitively deciphering his emotional world, rather than drawing from intuition about others’ emotional states. Yet the autobiographic relived emotion trials demonstrated that VW possessed remnants of an inner emotional life. He seemed to come alive when talking about past events that were personally relevant to him (e.g., his wife leaving him, his former legal work with unions). VW’s emotional life appeared bound to his past memories of emotional events and internally generated emotions from personally relevant stimuli.
In a comparison of subjects with temporal variant FTLD, Mendez (2004) found that patients with right hemispheric involvement were more likely than left sided patients or normal controls to call computer-distorted faces “human” (30). Thus, there is evidence that the progressive changes in VW’s depictions of humans were due in part to his right temporal lobe degeneration and associated emotional deficits. VW also became much more limited in his ability to lift and move his paintbrush due to his progressing ALS. Did his faces become more generic because he became less attuned to the nuances and meanings of facial expression, or because he could no longer control the brush to produce these likenesses? Both explanations are likely to have contributed to the changing qualities of his art.
The compulsive behaviors commonly seen in FTLD may also play an important role in artistic production, causing patients to obsessively practice and even hone their artistic techniques (17). VW’s compulsive nature appears to have contributed to his artistic process. Indeed, he manifested compulsive behaviors in other realms, including water intake, eating rituals, and coin collecting. Especially in the later years, VW repeatedly painted the same geometric designs on store-bought sculptures and objects twenty to thirty times. Arguably, his increasing compulsion, while causing him to be more prolific, limited the creativity of his artwork.
Bipolar Disorder and Artistic Productivity
Particularly with respect to his novel compulsion to create art on a daily basis, there may have been an interesting interaction between VW’s history of bipolar illness and his dementia. VW had a significant family history of mental illness, including twenty-three relatives on his maternal side with bipolar disease. While he experienced several episodes of mania in his twenties, it is uncertain whether instances of poor judgment as early as three years prior to his diagnosis of FTLD (e.g. deciding to marry unknown woman while on vacation in Asia), were lapses in judgment due to his frontal lobe degeneration or his bipolar disease. Indeed, it is well-established that people with affective disorders tend to be over-represented in the creative artist population (especially those with bipolar disorder (32). Bipolar disorder may carry certain advantages for creativity, especially in those who have milder symptoms (33). Although VW did not seem to be exhibiting symptoms of bipolar disorder (mania or depression) in the years of his progressive dementia and artistic proliferation, his disorder may have contributed to his artistic proliferation and creativity. Indeed, there may be overlap in the brain regions affected in FTLD and bipolar disorder, including the orbitofrontal cortex and the frontal-subcortical loops. Bipolar patients may have diminished frontal regulation of subcortical affective systems involving the amygdala and striatum, which may increase their affective instability as well as their compulsiveness.(34) While it may be impossible to disentangle the effects of the two conditions on VW’s art, his history of bipolar disorder may have laid the neuroanatomic foundation for the artistic creativity that later appeared in the context of FTLD.
FTLD and ALS
VWs case provides not only an informative window into artistry and the brain, but also the natural history of FTLD and ALS. An association between FTLD and MND has been well-established. While some patients with ALS develop FTLD later in their disease course, others begin with FTLD or develop FTLD and MND together. In VW’s case, his FTLD symptoms appear to have preceded the onset of MND.
According to VBM morphometry of VW compared to age matched controls, VW was found to have a relatively atrophied amygdala and temporal cortex (Figure 6). However, there was also some atrophy seen in the left-greater-than right sided premotor and motor cortex Such volumetric findings are consistent with his clinical findings of upper extremity weakness, right-greater-than left. VWs findings are consistent with Chang et al’s (2005) voxel-based morphometry comparison of ALS and ALS/FTLD patients to normal controls, showing that ALS patients demonstrate significant atrophy in the bilateral motor and premotor cortices and anterior portion of the superior frontal gyrus bilaterally (31). Moreover, VW’s brain pathology was classic for the FTLD-MND subtype: moderate density of ubiquitin-positive inclusions in the amygdala, hippocampus, neocortical, and limbic structures; moderate neuronal loss and gliosis of the superficial layers of the cortex and limbic structures; depletion of motor neurons throughout the spinal cord and primary motor cortex (20–22).
CONCLUSIONS
We used data from multiple sources of information, including the patients’ medical record, MRI brain imaging and volumetric analysis, neuropsychology, functional evaluations, laboratory testing of emotional functioning, neuropathology and the patient’s artwork. Not only does this study contribute to the small but growing number of case studies on FTLD patients who develop artistic functioning, but to our knowledge, is the first case study to follow a patient with both FTLD and ALS. While the complicated neuropsychiatric history of this patient makes his examination more rich and interesting, it is also one of the limitations of this case study. Separating the relative contributions of his FTLD, ALS, and bipolar illness is a complex matter.
VW’s newfound interest in art, his evolving technique, choice of subject matter, and changing characterization of faces likely reflect dementia-related changes in cognition and emotional functioning. We propose that future case studies examining the artwork of patients with FTLD also gather information about trajectory of change over time, and that additional studies comparing the natural history of groups of FTLD patients to those with FTLD-MND would be a useful addition to the current case study literature.
Footnotes
Explanation of dependent measures and analyses: Self-reported experience was assessed with an inventory after emotional stimuli was presented. Participants rated whether they felt good, neutral or bad to each stimulus. Then they rated how strongly they felt each of eight specific emotions: afraid, angry, disgusted, embarrassed, happy, sad, sexually aroused, and surprised on a 3-point scale (‘no,’ ‘a little,’ or ‘a lot’) to. For example, for the emotion of happiness to a film clip, participants were asked “Did you feel happy while watching this film?” Target facial expressions were coded based on a modified version of Gross and Levenson’s (1993) Emotional Expressive Behavior coding system. Coders determined whether or not participants displayed specific emotional behaviors including: happiness, sadness, smiling, surprise, anger, fear, amusement, crying, contentment, and interest on a 0 to 3 scale. Autonomic arousal was measured by assessing participants skin conductance levels (SCL) during a baseline period before each emotional task, and during the tasks themselves. SCL responding was determined by subtracting averaged baseline SCL from averaged levels during the emotion eliciting tasks. Analyses were conducted by comparing the mean of VW’s responses to the ten control participant’s means and standard deviations. VW’s responses were considered to be significantly different from controls when his responding differed from the control mean by two standard deviations or more.
A control manipulation ensured the VW possessed the motor skills to use the rating dial in the tracking task. VW’s motor responsivity for the tracking task was slightly slow, and this was accounted for statistically in the analysis with lag-correlations.
REFERENCES
- 1.Mendez MF. Dementia as a window into the neurology of art. Medical Hypotheses. 2004;63:1–7. doi: 10.1016/j.mehy.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Neary, et al. Frontotemporal Lobal Degneration: a consensus on the clinical criteria. Neurology. 1998 December;51(6):1546–1554. doi: 10.1212/wnl.51.6.1546. [DOI] [PubMed] [Google Scholar]
- 3.Strong MJ, Lomen-Hoerth C, Caselli RJ, Bigio EH, Yang W. Cognitive Impairment, Frontotemporal Dementia, and the Motor Neuron Diseases. Annals of Neurology. 2003;Vol 54 suppl 5:S20–S23. doi: 10.1002/ana.10574. [DOI] [PubMed] [Google Scholar]
- 4.Yang WC, Strong MJ. Is the frontemporal dementia of ALS a tauopathy? ALS and other motor neuron disorders. 2002;3 suppl2:50. [Google Scholar]
- 5.Nitrini R, Rosemberg S. Psychotic Symptoms in Dementia Associated with Motor Neuron Disease: A Pathophysiological Hypothesis. Journal of Neuropsychiatry. 1998;10(4):456–458. doi: 10.1176/jnp.10.4.456. [DOI] [PubMed] [Google Scholar]
- 6.Pasquier F, Richard F, Lebert F. Natural history of frontotemporal dementia: comparison with Alzheimer’s disease. Dement Geriatr Cogn DIsord. 2004;17(4):253–257. doi: 10.1159/000077148. * [DOI] [PubMed] [Google Scholar]
- 7.Miller BL, Cummings J, Mishkin F, Boone K, Prince F, Ponton M, Cotman C. Emergence of Artistic Talent in Frontotemporal Dementia. Neurology. 1998;51:978–981. doi: 10.1212/wnl.51.4.978. [DOI] [PubMed] [Google Scholar]
- 8.Kapur N. Paradoxical facilitated function in brain-behaviour research. A critical review. Brain. 1996;119:1775–1790. doi: 10.1093/brain/119.5.1775. [DOI] [PubMed] [Google Scholar]
- 9.Mell JC, Howard SM, Miller BL. Art and the Brain: The Influence of Frontotemporal Dementia on an Accomplished Artist. Neurology. 2003;60:1707–1710. doi: 10.1212/01.wnl.0000064164.02891.12. [DOI] [PubMed] [Google Scholar]
- 10.Miller BL, Ponton M, Benson DF, Cummings JL, Mena I. Enhanced Artistic Creativity with Temporal Lobe Degeneration. Lancet. 1996;348:1744. doi: 10.1016/s0140-6736(05)65881-3. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan JA, Gardner H. Artistry after unilateral brain disease. In: Boller F, Grafman J, editors. Handbook of Neuropsychology. Vol. 2. 1989. pp. 141–155. [Google Scholar]
- 12.Gardner H. New York: Basic Books; 1982. Artistry after brain damage. Art, Mind, and Brain: A Cognitive Approach to Creativity; pp. 318–335. [Google Scholar]
- 13.Knopman DS, Boeve BF, Petersen RC. Essentials on the Proper Diagnoses of Mild Cognitive Impairment, Dementia, and Major Subtypes of Dementia. Mayo Clin Proc. 2003;78:1290–1308. doi: 10.4065/78.10.1290. [DOI] [PubMed] [Google Scholar]
- 14.Rosen HJ, Lengenfelder J, Miller BL. Frontotemporal Dementia. Neurologic Clinics. 2000 November;Vol 18(4):979–992. doi: 10.1016/s0733-8619(05)70235-8. [DOI] [PubMed] [Google Scholar]
- 15.Mychack P, Kramer JH, Boone KB, Miller BL. The influence of right frontotemporal dysfunction on social behavior in frontotemporal dementia. Neurology. 2001 June;56 Suppl 4:S11–S15. doi: 10.1212/wnl.56.suppl_4.s11. [DOI] [PubMed] [Google Scholar]
- 16.Miller BL, Hou CE. Portraits of Artists: Emergence of Visual Creativity in Dementia. Arch Neurology. 2004 June;Vol 61:842–844. doi: 10.1001/archneur.61.6.842. [DOI] [PubMed] [Google Scholar]
- 17.Miller BL, Kyle Boone, Cummerings JL, Read SL, Mishkin F. Functional correlates of musical and visual ability in frontotemporal dementia. British Journal of Psychiatry. 2000;176:458–463. doi: 10.1192/bjp.176.5.458. [DOI] [PubMed] [Google Scholar]
- 18.Mitsuyama Y. Presenile dementia with motor neuron disease in Japan: clinico-pathological review of 26 cases. J Neurol Neurosurg Psychiatry. 1984;47:953–959. doi: 10.1136/jnnp.47.9.953. * [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller BL, Hou CE. Portraits of Artists: Emergence of Visual Creativity in Dementia. Arch Neurol. 2004 June;61:842–844. doi: 10.1001/archneur.61.6.842. [DOI] [PubMed] [Google Scholar]
- 20.Trojanowski JQ, Dickson D. J Update on the neuropathological diagnosis of frontotemporal dementias. Neuropathol Exp Neurol. 2001;60:1123–1126. doi: 10.1093/jnen/60.12.1123. [DOI] [PubMed] [Google Scholar]
- 21.Jackson M, Lennox G, Lowe J. Motor Neurone Disease Inclusion Dementia. Neurodegeneration. 1996;5:339–350. doi: 10.1006/neur.1996.0046. [DOI] [PubMed] [Google Scholar]
- 22.Yoshida M. Amyotrophic lateral sclerosis with dementia: the clinicopathological spectrum. Neuropathology. 2004;24:87–102. doi: 10.1111/j.1440-1789.2003.00544.x. [DOI] [PubMed] [Google Scholar]
- 23.Abrahams S, Goldstein LH, Suckling J, Ng V, Simmons A, Chitnis X, Atkins L, Williams SCR, Leigh PN. Frontotemporal white matter changes in amyotrophic lateral sclerosis. J Neurol. 2005 March 3; doi: 10.1007/s00415-005-0646-x. [DOI] [PubMed] [Google Scholar]
- 24.Abrahams S, Goldstein LH, Al-Chalabi A, Pickering A, Morris RG, Passingham RE, Brooks DJ, Leigh PN. Relation between cognitive dysfunction and pseudobulbar palsy in amyotrophic lateral sclerosis. J Neurol Neur`osurg Psychiatry. 1997;62:464–472. doi: 10.1136/jnnp.62.5.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rakowicz WP, Hodges JP. Dementia and aphasia in motor neuron disease: an underrecognized association? J Neurol Neurosurg Psychiatry. 1998;65:881–889. doi: 10.1136/jnnp.65.6.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saxena S, Rauch SL. Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin North Am. 2000 September;23(3):563–586. doi: 10.1016/s0193-953x(05)70181-7. [DOI] [PubMed] [Google Scholar]
- 27.Stoll AL, Renshaw PF, Yurgelun-Todd DA, Cohen BM. Neuroimaging in Bipolar Disorder: What have We Learned? Biol Psychiatry. 2000;48:505–517. doi: 10.1016/s0006-3223(00)00982-3. [DOI] [PubMed] [Google Scholar]
- 28.Ashburner J, Friston KJ. Voxel-based morphometry—the methods. Neuroimage. 2000;11:805–821. doi: 10.1006/nimg.2000.0582. [DOI] [PubMed] [Google Scholar]
- 29.Good CD, Scahill RI, Fox NC, et al. Automatic differentiation of anatomical patterns in the human brain: validation with studies of degenerative dementias. Neuroimage. 2002;17:29–46. doi: 10.1006/nimg.2002.1202. [DOI] [PubMed] [Google Scholar]
- 30.Mendez MF, Lim, Gerald TH. Alterations of the Sense of “Humanness” in Right Hemisphere Predominant Frontotemporal Dementia Patients. Cognitive & Behavioral Neurology. 2004 September;17(3):133–138. doi: 10.1097/01.wnn.0000136593.21532.16. [DOI] [PubMed] [Google Scholar]
- 31.Chang JL, Eng M, Lomen-Hoerth C, Murphy J, Henry RG, Kramer JH, Miller BL, Gorno-Tempini ML. A Voxel-Based Morphometry Study of Patterns of Brain Atrophy in ALS and ALS/FTD. Neurology. 2005 Jul 12;65(1):75–80. doi: 10.1212/01.wnl.0000167602.38643.29. [DOI] [PubMed] [Google Scholar]
- 32.Richards R, Kinney DK, Lunde I, Benet M, Merzel APC. Creativity in manic-depressives, cyclothymes, their normal relatives and control subjects. Journal of Abnormal Psychology. 1988;97:281–288. doi: 10.1037//0021-843x.97.3.281. [DOI] [PubMed] [Google Scholar]
- 33.Andreasen NC, Glick ID. Bipolar affective disorder and creativity implications and clinical management. Compr Psychiatry. 1988;29(3):207–217. doi: 10.1016/0010-440x(88)90044-2. [DOI] [PubMed] [Google Scholar]
- 34.Strakowski SM, Delbello MP, Adler CM. The functional neuroanatomy of bipolar disorder: a review of neuroimaging findings. Molecular Psychiatry. 2005;10(1):105–116. doi: 10.1038/sj.mp.4001585. [DOI] [PubMed] [Google Scholar]