Abstract
Objective
To determine the impact of an introductory pharmacy practice experience (IPPE) on students' clinical skills during their initial advanced pharmacy practice experience (APPE).
Design
A 4-week First Steps course that focused on students developing pharmacy practice skills, clinical communications skills, and effective use of reference materials was introduced in 2006 at the end of the third-year curriculum, prior to students beginning their APPEs.
Assessment
During the third week of the first APPE, faculty members rated students' demonstration of 9 clinical skills on a 5-point Likert scale (1 being always and 5 being never). The evaluation was performed in 2005 prior to implementation of the course (control group) and again in 2006 after implementation of the course. Students who completed the First Steps course scored better on all 9 skills and had a better average clinical skills value (2.3) compared to the control group (2.6, p < 0.01).
Conclusion
Completion of an IPPE course that focused on critical pharmacy practice aspects, clinical communication skills, and use of reference materials resulted in increased frequency of desired clinical behaviors on a subsequent APPE.
Keywords: introductory pharmacy practice experience, assessment, evaluation, experiential learning, advanced pharmacy practice experience
INTRODUCTION
Introductory pharmacy practice experiences (IPPEs) have been identified as an important opportunity for pharmacy students to practice the provision of patient care early in the curriculum to understand fully and actively apply the information that is being learned.1 Additionally, the Accreditation Council for Pharmacy Education (ACPE) has set specific requirements within Standards 2007 spurring innovation among colleges and schools of pharmacy regarding development of IPPE courses.2
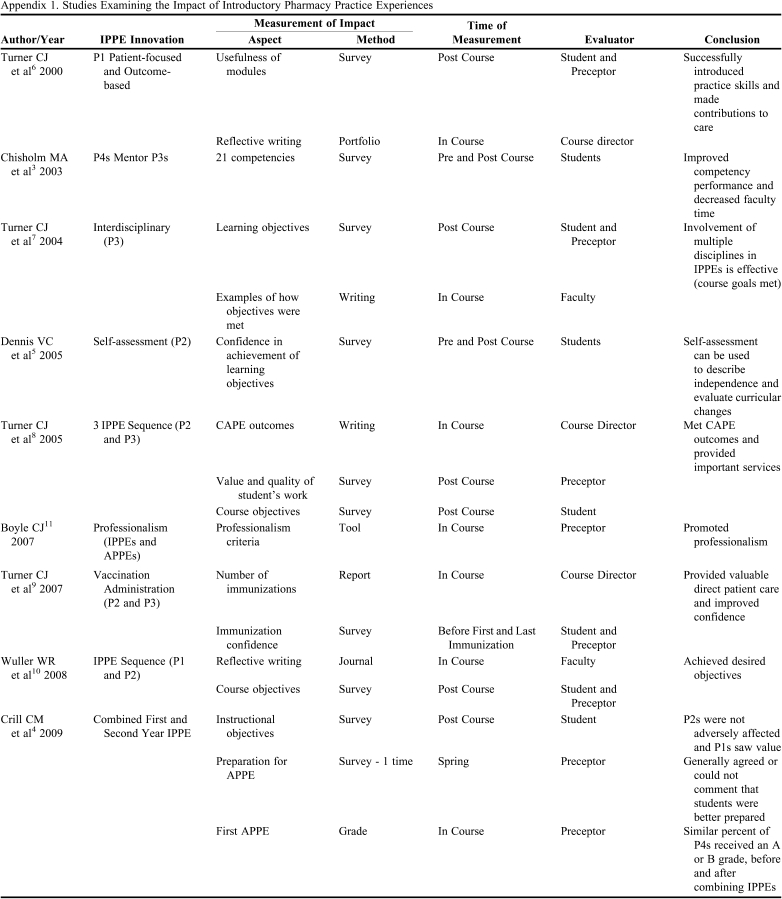
Colleges have used a variety of innovative approaches (eg, interdisciplinary work, vaccination programs, fourth-year mentorship of third-year students) and sites (eg, community, hospital, elementary school, clinic, long-term care) for IPPEs.3-10 The impact of these approaches has been measured in terms of outcome achievement, provision of patient care, and changes in attitudes or behaviors (eg, confidence, professionalism), and typically have been assessed via surveys and student writing.3-11 Appendix 1 contains additional details on these studies. Results have been positive. Assessments of impact occurred either during or at the end of the experience and were completed either by the student or preceptors/faculty members overseeing/teaching the course, creating possible bias about the perceived effect or utility of the IPPE. Only 1 study sought to evaluate subsequent performance, although limitations in design hampered interpretation.4
This project was designed to measure the impact of an IPPE course entitled First Steps on students' skills at the next level of clinical competence (ie, APPE). In addition, the study design minimized the potential bias associated with data obtained from course evaluators by using evaluations from faculty members mentoring students during their first APPE. A control group was also included to ascertain the impact.
The First Steps course was 1 portion of the college's IPPE sequence and served as part of a transitional plan. The transitional plan has since been replaced by a new introductory experiential curriculum that has more hours and is more fully integrated. The course taught basic skills in the provision of pharmacy services, fostered development in clinical communications, and enhanced use of reference materials. This course followed the classroom courses and was designed to prepare students for APPEs through practice experiences, and as such was considered an IPPE. This is consistent with ACPE's Standards 2007 which states IPPEs should “continue in a progressive manner leading to entry into the advanced pharmacy practice experiences.”2 Learning objectives and activities from the First Steps course subsequently have been integrated into IPPEs of the new introductory experiential curriculum that occur throughout the classroom component of the curriculum, due in part to the course's effect on students' performance during APPEs. This paper provides a description of the course and an analysis of its impact on students' skills in an APPE.
DESIGN
Prior to 2006, IPPEs at South Dakota State University's College of Pharmacy were comprised of 135 hours of practice experience distributed within the first, second, and third professional years (P1, P2, P3) of the doctor of pharmacy (PharmD) curriculum. The IPPEs provided students with basic skills in practice, including patient interview techniques, fundamental evaluation of medical literature, and an overall survey of pharmacy practice. Fourth-year APPEs totaled 44 weeks, with each student completing 10 APPEs.
The college implemented the new required First Steps course in 2006 to expand the IPPEs already in place, prepare students for APPEs more quickly, allow for transition to a new curricular structure, and meet evolving accreditation standards. At implementation of the course, the APPE structure changed from 10 APPEs over 44 weeks to 8 APPEs over 40 weeks. No other differences existed between the 2005 and 2006 curricula.
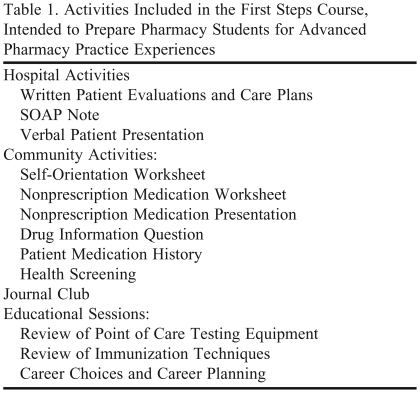
The 4-week course involved 160 hours of practice experience and occurred between the end of the P3 year and the beginning of APPEs. Course activities (Table 1) involved the application of previously learned information to the patient care setting. Nine days were spent at a community site supervised by preceptors and 9 days at a hospital site supervised by faculty members. The coordinator met with the students for 2 days, leading activities such as journal club and reviewing clinical skills such as blood pressure monitoring, patient counseling, and cholesterol and glucose monitoring. Three hospital sites and 14 community sites were involved, with 13 faculty members serving as preceptors at the hospital sites and 1 faculty member overseeing 14 community pharmacist preceptors. Fifty-six students completed the course in 2006. Fifty-seven students were in the 2005 class that preceded the implementation of the First Steps course.
Table 1.
Activities Included in the First Steps Course, Intended to Prepare Pharmacy Students for Advanced Pharmacy Practice Experiences
Abbreviation: SOAP = subjective, objective, assessment, plan
Grading for the course was based on 150 possible points. Approximately a third of the points were completed in the hospital setting, including written patient care plans, patient progress notes, and formal verbal patient presentations. Community assignments included a pharmacy self-orientation checklist, nonprescription medication assignments, patient medication history, and a practice-based drug information question. Designated faculty members graded the community-based activities after assignments were submitted through an online course management system. Students were also required to give a journal club presentation which also was graded by faculty members.
Faculty members' workload for the course included time for preparation, execution, and evaluation. Preparatory time involved scheduling student sites, ensuring classroom availability for group events, creating graded assignments, and developing the course within an online course management system. During the course, faculty members were directly involved with students at each of the 3 hospital sites and worked daily with 2 student groups in consecutive 2-week blocks. The journal club activity required time to schedule, observe, and grade the activity. Finally, 3 faculty members graded students' work submitted online for their community assignments.
Student workload included several assignments and experiential activities within the community setting (Table 1). During their hospital experience, each student formally presented at least 3 patients to faculty and peers and submitted at least 2 written patient care plans. They were also required to perform the literature evaluation necessary to complete the journal club assignment. Students were also expected to perform other tasks assigned by preceptors at the community or hospital sites.
After completing the course, students began their first advanced experience at one of the available APPE sites (excluding some specialty practice experiences), depending on the student's overall schedule. Faculty members served as preceptors for the majority of subspecialty APPEs (eg, internal medicine, ambulatory care, psychiatry, pediatrics, critical care, infectious disease), while practitioners supervised most of the community and hospital APPEs. Only those students in their first APPE with a faculty member were evaluated for this study.
EVALUATION AND ASSESSMENT
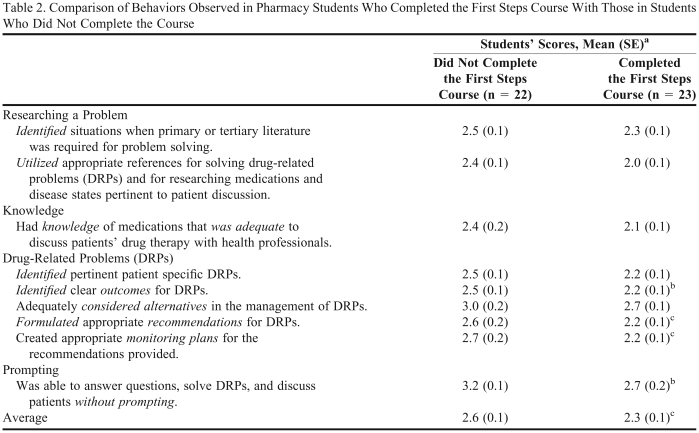
To measure the impact of the First Steps course, an evaluation tool was used that focused on important practice aspects and outcomes specific to the course (eg, provision of pharmaceutical care). The evaluation tool contained 9 statements in the areas of researching a problem (2 statements), sharing knowledge (1 statement), solving drug-related problems (5 statements), and prompting to complete tasks (1 statement). A 5-point Likert scale was used to quantify the frequency with which the student performed the behaviors identified in the evaluation tool: 1 = always, 2 = usually, 3 = half the time, 4 = infrequently, 5 = never. Thus, low numbers reflected more frequent performance of positive behaviors.
The evaluation tool was completed by faculty members for students on their first APPE in 2005, prior to implementation of the course; therefore, this group was used as a control group. The evaluation tool was subsequently completed by faculty members in 2006 for students having taken the First Steps course. All evaluation tools were completed in the third week on the first APPE to allow adequate time for evaluation of the student's skills. Only students who had their first APPE with a faculty member were included in the study to assure consistency and rigor in evaluation. In addition, only the first APPE was included because subsequent APPEs may have been influenced by previous APPEs.
Numeric data were compared via descriptive statistics and a 2-tailed, unpaired t test assuming unequal variance. Approval was obtained from the South Dakota State University Institutional Review Board for this project.
Seventeen faculty members served as preceptors for students in their first APPE for both years. Fourteen faculty members completed evaluation tools in 2005 and 10 in 2006. Between 1 and 3 students were assigned to an individual faculty member. Fifty-seven students were included in the 2005 class and 56 in the 2006 class. Faculty members completed 22 evaluation tools in 2005 and 23 in 2006 (40% of the class in 2005 and 41% in 2006). All of the students in their first APPE with a faculty member had an evaluation tool completed on their performance.
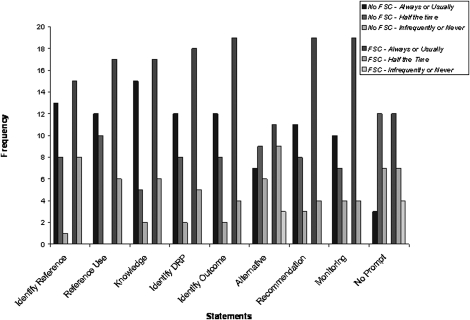
Faculty members perceived that students who took the First Steps course performed the desired clinical behaviors more often than the control group of students who had not taken the course, based on the overall average frequency of the desired behavior (2.6 for 2005 vs. 2.3 for 2006; p < 0.01). More students in 2006 achieved the desired behavior “always or usually” and “over half the time” compared to the control group (Figure 1). Similarly, based on average scores on the 9 items, the 2006 students achieved more frequent occurrence (lower being more frequent) of the desired behaviors. However, the differences in scores on only 4 items were significant (Table 2).
Figure 1.
Distribution of faculty members' evaluation of the frequency of students' behaviors (FSC = First Steps Course).
Table 2.
Comparison of Behaviors Observed in Pharmacy Students Who Completed the First Steps Course With Those in Students Who Did Not Complete the Course
a1 = always, 2 = usually, 3 = half the time, 4 = infrequently, 5 = never
bp ≤ 0.05
cp ≤ 0.01
DISCUSSION
Introductory pharmacy practice experiences are a major curriculum component with the goal of improving performance on subsequent practice experiences. This study analyzed methods to assure this goal was achieved. Other studies have identified positive outcomes from IPPEs but have relied almost exclusively on measures within or upon completion of the course, including students', preceptors', and faculty members' perceptions of achievement, and students' written descriptions of their experiences.3-11 Appendix 1 contains additional details of these studies.
Evaluating the impact of IPPEs on future practice activities is important to assure the effectiveness of these courses. A study by Crill et al4 assessed the effect of integrating 2 IPPEs by measuring preceptors' perception of students' performance on APPEs before and after the change. However, the study involved only 1 survey of preceptors in the spring following implementation of the change. This required that the preceptor remember the students' earlier performance in the academic year and compare it to the performance of students from the previous year. Recalling this information and making the comparison from memory may explain why a large portion of the sample responded “neither agree nor disagree” to the statements (range 37% to 55.6%). While this study advanced the evaluation of IPPEs, additional improvements in study design will provide greater understanding of the IPPE's effectiveness. Our study assessed the impact of an IPPE by comparing faculty members' perceptions of students' performance on their first APPE for a group of students who did not have the First Steps course against students who did. This represents an additional advancement in the measurement of IPPE impact.
The course had a positive impact on students' clinical skills as evidenced by students who took the course exhibiting desired clinical behaviors more often than students who did not. While a greater number of students taking the course exhibited all 9 behaviors more frequently than students not taking the course, significant differences were found for only 4 of the 9 items (Table 2). These results were consistent with the majority of assignments given in the First Steps course. Specifically, identifying and solving drug-related problems was a part of nearly all assignments, and a significant difference was found for 3 of the 5 items in this category. In addition, all activities in the course were designed to prepare students to participate independently in APPE activities, and a significant difference was found between the groups for the item focused on prompting (eg, students taking the class required less prompting). Conversely, behaviors related to knowledge were not significantly different from the control group, perhaps because acquiring new knowledge was not a major component of the course. Researching problems did not improve significantly because it was not a specific focus of any course activities. Requiring additional literature search activities should result in additional improvements in desired literature research behaviors.
The effect of the course should be to challenge students by raising expectations for performance on APPEs. This is especially true in the areas of identifying outcomes, making recommendations, creating monitoring plans, and functioning independently, as students who completed the course demonstrated these skills more frequently than students in the control group. Based on this information, APPE expectations and outcomes may be revised to require higher levels of performance. In addition, students can transition more quickly into practice activities in the APPEs and use more of the APPE time for active learning.
Although credit hours for new IPPEs are usually taken from classroom courses, the 4 credit hours for the First Steps course came from the APPE time block. Thus, the question remains as to whether the addition of 4 credit hours from other types of instruction, or a reduction in classroom coursework affects students' APPE skills. Future research needs to examine not only the effect of adding IPPEs but also the impact of reducing other types of instructional credit hours in the P1 through P3 years in order to create new IPPEs.
In creating the college's new introductory experiential curriculum, attention was given to retaining elements of the First Steps course because these elements have been determined to result in positive outcomes. Improvements with the First Steps course are expected to continue as these activities are integrated into the IPPEs in the new introductory experiential curriculum. The new curriculum contains 2 IPPEs occurring during the summers following the P1 and P2 years, totaling 240 practice hours. In addition, the pharmacy practice sequence during the P1 through P3 academic years involves approximately 80 hours of IPPE time. All activities listed in Table 1 have been included in the new introductory experiential curriculum (ie, pharmacy practice courses and the summer IPPE courses).
While this approach to introductory pharmacy practice involves a significant amount of faculty time and resources, the investment is warranted because of the positive results. This approach ensures a consistent set of skills, allowing students to function at a higher level sooner within the APPE program.
Although this study minimized the biases present in previous IPPE study design, limitations existed. First, the course followed the classroom component, which is not typical of IPPEs. However, these activities are similar to IPPE design to prepare students for APPEs, and are subsequently included in the new introductory experiential curriculum (ie, integrated throughout the P1 through P3 years). The impact of placing these activities after classroom work cannot be determined from this data. Additionally, 3 faculty members designed the course and completed 6 survey instruments (ie, 13% of all surveys); therefore, their investment in the class may have influenced their responses. We feel that the small percentage of surveys potentially impacted would have a minimal effect. Third, all faculty members who completed survey instruments participated in the course, whether their role was overseeing students at their practice site or leading a journal club. This may have influenced their evaluation, although the length of time between surveys would have minimized the effect. Fourth, in this study the credit hours were moved from APPEs to IPPEs, which is an uncommon approach. Future research should evaluate the impact of reducing credit hours of classroom time in P1 through P3 years, as IPPE credits increase. Finally, this study did not evaluate the impact of IPPEs that occur earlier in the curriculum (eg, P1 or P2), and therefore the results cannot be extrapolated to these types of IPPEs. Future research should examine the impact of P1 and P2 IPPEs by measuring skills in subsequent courses.
SUMMARY
This study sought to determine the impact of an IPPE (First Steps course) on students' subsequent practice performance. The course focused on pharmacy practice activities, clinical communication skills, and use of reference materials. The study compared faculty members' evaluations of students not taking the course to students who took the course, and showed that students who completed the course scored better on all 9 skills and had a better average clinical skills value (2.3 versus 2.6, p < 0.01). Improved clinical performance and more rapid acclimation by students to practice situations offset the faculty and preceptor workload requirements for this course. Future research examining the impact of IPPEs should include the reduction in classroom credit hours that typically results from the addition of IPPEs.
REFERENCES
- 1.Nemire RE, Meyer SM. Educating students for practice: educational outcomes and community experience. Am J Pharm Educ. 2006;70(1) doi: 10.5688/aj700120. Article 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American Council on Pharmacy Education Standards 2007. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed January 13, 2010.
- 3.Chisholm MA, DiPiro JT, Fagan SC. An innovative introductory pharmacy practice experience model. Am J Pharm Educ. 2003;67(1) Article 22. [Google Scholar]
- 4.Crill CM, Matlock MA, Pinner NA, Self TH. Integration of first- and second-year introductory pharmacy practice experiences. Am J Pharm Educ. 2009;73(3) doi: 10.5688/aj730350. Article 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dennis VC. Longitudinal student self-assessment in an introductory pharmacy practice experience course. Am J Pharm Educ. 2005;69(1) Article 1. [Google Scholar]
- 6.Turner CJ, Jarvis C, Altiere R. A patient focused and outcomes-based experiential course for first year pharmacy students. Am J Pharm Educ. 2000;64(3):312–319. [Google Scholar]
- 7.Turner CJ, Altiere R, Clark L, Dwinnell B, Barton AJ. An interdisciplinary introductory pharmacy practice experience course. Am J Pharm Educ. 2004;68(1) Article 10. [Google Scholar]
- 8.Turner CJ, Altiere R, Clark L, Maffeo C, Valdez C. Competency-based introductory pharmacy practice experiential courses. Am J Pharm Educ. 2005;69(2) Article 21. [Google Scholar]
- 9.Turner CJ, Ellis S, Giles J, et al. An introductory pharmacy practice experience emphasizing student-administered vaccinations. Am J Pharm Educ. 2007;71(1) doi: 10.5688/aj710103. Article 03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wuller WR, Luer MS. A sequence of introductory pharmacy practice experiences to address the new standards for experiential learning. Am J Pharm Educ. 2008;72(4) doi: 10.5688/aj720473. Article 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boyle CJ, Beardsley RS, Morgan JA. Rodriguez de Bittner M. Professionalism: a determining factor in experiential learning. Am J Pharm Educ. 2007;71(2) doi: 10.5688/aj710231. Article 31. [DOI] [PMC free article] [PubMed] [Google Scholar]