Abstract
Objectives
To assess the breadth, depth, and perceived importance of pharmacogenomics instruction and level of faculty development in this area in schools and colleges of pharmacy in the United States.
Methods
A questionnaire used and published previously was further developed and sent to individuals at all US schools and colleges of pharmacy. Multiple approaches were used to enhance response.
Results
Seventy-five (83.3%) questionnaires were returned. Sixty-nine colleges (89.3%) included pharmacogenomics in their PharmD curriculum compared to 16 (39.0%) as reported in a 2005 study. Topic coverage was <10 hours for 28 (40.6%), 10-30 hours for 29 (42.0%), and 31-60 hours for 10 (14.5%) colleges and schools of pharmacy. Fewer than half (46.7%) were planning to increase course work over the next 3 years and 54.7% had no plans for faculty development related to pharmacogenomics.
Conclusions
Most US colleges of pharmacy include pharmacogenomics content in their curriculum, however, the depth may be limited. The majority did not have plans for faculty development in the area of pharmacogenomic content expertise.
Keywords: pharmacogenomics education, pharmacogenetics education, curriculum
INTRODUCTION
Two policy resolutions passed by the 2008 American Association of Colleges of Pharmacy (AACP) House of Delegates recommended increased focus on the advancement of education in biotechnology. The first pertained to the curricular implications of biotechnology and personalized medicine. It focused on the responsibility of pharmacy curricula to address up-to-date issues associated with biotechnology advances in tailored medicine.1 Specific competencies discussed in this policy are cell and system biology, bioengineering, genetics/genomics, proteomics, nanotechnology, cellular and tissue engineering, bio-imaging, computational methods, and information technologies. The second policy pertained to faculty development in biotechnology areas. This policy stated that “faculty development programs and collaborative research and teaching strategies should be expanded such that faculty at colleges and schools of pharmacy are prepared to lead and contribute significantly to education and research…” in the above areas.
Though colleges and schools of pharmacy (hereafter colleges of pharmacy) are likely working to address the educational needs surrounding the emergence of pharmacogenomics and other biotechnology areas, it appears that AACP members believed policy resolutions might ensure preparation of pharmacy students and faculty members for future roles in the application of biotechnology and pharmacogenomics to patient care. Determining how many colleges of pharmacy already meet the intent or have systems in place to implement these resolutions would provide valuable data for longitudinal assessment of these issues.
Prior to June 2004, Latif and McKay evaluated the depth and extent to which pharmacogenetics and pharmacogenomics content (hereafter referred to as pharmacogenomics) was being taught in colleges of pharmacy in the United States.2 Their investigation was initiated as a result of the Core Competencies in Genetics Essential for all Health-Care Professionals document distributed by the National Coalition for Health Professionals Education in Genetics (NCHPEG) and recommendations from the 2001-2002 AACP Academic Affairs Committee.3,4 The AACP Committee identified the need to include pharmacogenomics content in pharmacy curricula “because most drug effects are determined by the interplay of several gene products that govern the pharmacokinetics and pharmacodynamics of medication.”3 The committee believed that pharmacogenomics would change the practice of pharmacy by using a patient's genotype to guide dosing decisions in order to potentially improve medication effectiveness while reducing toxicity. Latif and McKay's investigation concluded that there was awareness of the need to increase the level of instruction in these areas among the colleges of pharmacy.2
The progress of pharmacogenomics and other biotechnology areas of inquiry over the last 40 years highlight the growing importance of the AACP resolutions. In the 1970s, Robert Smith's work with debrisoquine and Michel Eichelbaum's work with sparteine led to the discovery of a CYP2D6 genetic polymorphism, the frequency of which was enough to make it relevant to the general population and the use of a variety of drugs.5 Over the next decade, drug response was recognized to often be determined by multiple genes as well as other factors. This new information led the focus from pharmacogenetics, the effect of a single gene on drug therapy, to the broader subject of pharmacogenomics, drug treatment based on the effects of many genes.6 The evolution in focus to understand the entire genetic makeup of humans helped lead to the Human Genome Project (HGP).7
Initiated in 1990, the HGP set out to map the entire human genome to gain information regarding the “structure, organization and characteristics of human DNA.”8 The knowledge gained from the HGP has helped to identify individuals and families at risk for disease and can be used to ease the burden of diagnosis and treatments for various diseases. For example, the use of genetic information can be used in determining warfarin dosing when oral anticoagulation is needed. With this information, individuals at risk may avoid the adverse clinical consequences that may arise from underdosing or overdosing when traditional fixed dose approaches are used.9 Other DNA tests have been found useful in identifying patients who would benefit from pharmacogenomic therapies such as those with cancers, deep vein thrombosis, and inflammatory diseases.10
Even with the advancements made in the understanding of pharmacogenomics, many health care providers continue to feel unprepared to speak with their patients regarding the correlation between genetics and their disease.8 The pharmacist's role in the use of pharmacogenomics for application in patient care is evolving and is yet to be elucidated fully, though the profession is active in conducting research and promoting understanding of the variable drug response due to genetics.6 For example, committees formed at the national level have developed core competencies with respect to genetics over the last decade, and colleges of pharmacy have worked to address the educational needs of the emergence of pharmacogenomics.11 Further, the standards and guidelines from the Accreditation Council for Pharmacy Education (ACPE) in the professional programs of pharmacy include requirements for the incorporation of content on the genetic basis of disease and drug action, individualized drug dosages, drug metabolism alteration, and principles of genomics and proteomics in relation to drug development and disease.12
The purpose of this study was to describe the reported breadth and depth of pharmacogenomics instruction in United States colleges of pharmacy, the opinions of survey respondents as to the value of specific course content and sufficiency of education in these area, and the reported level of faculty development relative to these areas: and to compare results to those from an earlier publication.
METHODS
Colleges of pharmacy (n = 109) were eligible to participate if they were in the United States and regular or associate members of AACP in 2008-2009. Colleges that were not on the roster of AACP members were excluded. The authors' Human Subjects Protection Program Institutional Review Board granted exempt status for the study.
This was a descriptive study using a revised and expanded questionnaire from a previous study by Latif and McKay.2 A pretest was conducted by sending the questionnaire to 5 pharmacy faculty members around the country known to be associated with programs where pharmacogenomics and pharmacogenetics content was covered. They were asked for comments on its utility and clarity. Based on their comments, the questionnaire was further refined and then sent to AACP for approval of its use as an endorsed survey. After submission, the authors were notified by AACP of a grant from the CDC for a project called “Pharmacogenomics Education Program (PharmGenEd™): Bridging the Gap between Science and Practice” (http://pharmacogenomics.ucsd.edu). This program aims to build a shared curriculum that meets the needs of US colleges of pharmacy. The appropriate individual from this group was contacted and the questionnaire was revised further, with their assistance, to help identify colleges interested in participation in the development of the curriculum and those interested in using it once completed.
AACP sent an initial e-mail to 109 deans in January 2009 requesting the name of an appropriate member of the faculty for questionnaire completion. Nonresponding deans were contacted 3 weeks after the original e-mail and up to 3 total times by 1 of the investigators via e-mail and/or phone requesting the information. Upon receiving the contact name from the dean, an e-mail was sent to the identified individual stating the purpose of the study and requesting participation. A subject disclosure form was included as an attachment to the e-mail. Contacts who failed to respond were sent a follow-up e-mail 10 and then 20 days after the originating e-mail. A final phone call was also placed to nonrespondents. A message requesting participation and contact information was left if there was no answer.
The questionnaire included requests for descriptive information related to the college, whether pharmacogenomics coursework was taught in the PharmD curriculum, and if so, whether specific topics were covered. Information on the depth (estimated number of hours) of instruction and the respondents' views on the importance of the specific topic areas to the education of doctor of pharmacy candidates were also requested. Respondents were questioned as to the availability of pharmacogenomics research resources, the number and type of faculty involved in teaching, and whether a development plan was in place or being created to provide faculty the opportunity to stay current in the field. Respondents were asked for their perception of their own and other schools' level of pharmacogenomic instruction. Respondents were also asked if they would be interested in having access to and collaborating on the shared pharmacogenomics curriculum. Although this study focused on PharmD curriculum, questions pertaining to pharmacogenomic curriculum for other graduate programs (MS, PhD) and groups (physicians, nurses, students other than those listed) were explored.
The impact of nonresponse error on the questionnaire was determined using approaches to evaluate response trends among subgroups of individuals responding after different contacts to determine whether later respondents differ systematically from earlier respondents and whether this poses problems for generalizing results.13 A p < 0.05 was considered an indicator of significant difference.
To assess the breadth of course content in colleges of pharmacy, 16 topics pertaining to the domains of genetic basis of disease and 9 ethical, social, and economic implication items were described. Respondents were asked to choose between 1 of 3 answers regarding whether the content was covered: yes, no, or unsure. In addition, all respondents were asked to rate the importance of the topics for the curriculum for PharmD candidates. Response options were not important, neutral, important, or unsure.
A password protected Excel (Microsoft, Redmond, Wash) file was maintained to track all communications and progress for the study. Another Excel file was maintained to input questionnaire responses. No direct link was made between the final responses, institution, and/or individual responding. Descriptive statistics were used for reporting the data and for comparisons to previous study results.
RESULTS
Ninety of 109 (82.6%) deans responded with an appropriate contact name. Of the 90 e-mails and instruments then sent, 75 (83.3%) questionnaires (68.8% of total college deans contacted) were returned by e-mail or fax. There were 48 private (44%) and 61 public (56%) colleges of pharmacy among the 109 contacts and the response rate (n = 75) from each was the same, with 33 (44%) private and 42 (56%) public colleges of pharmacy. No significant differences (p = 0.23) were found between responding subgroups using Churchill's approach.13
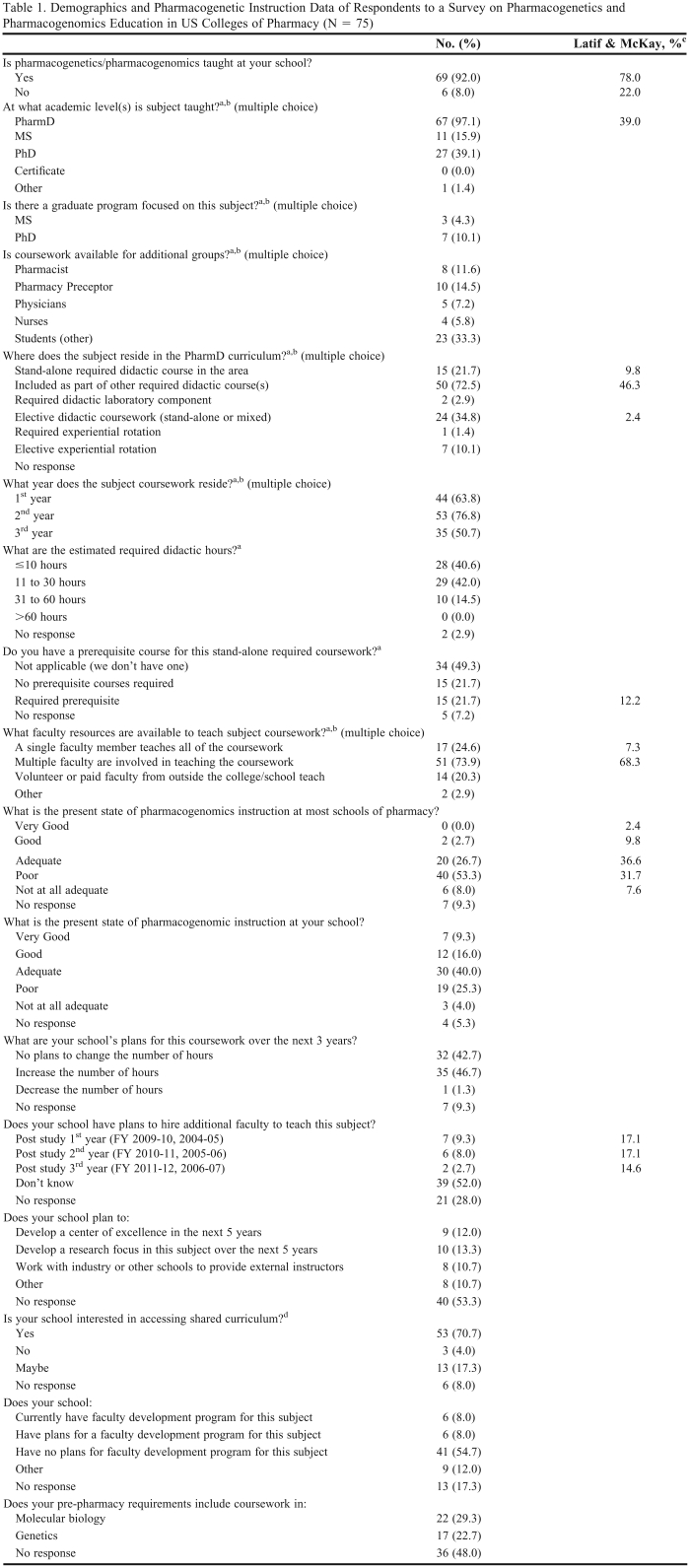
Table 1 provides the summary of relevant demographic and pharmacogenomics teaching-related items along with those of Latif and McKay when similar items existed. Respondents from 69 colleges (92.0%) reported that pharmacogenomics coursework was taught at their institution. Of these, 67 (89.3% of total) taught it at the PharmD level. Graduate programs in 3 (4.3%) of the respondents' colleges in the current study offer MS degrees and 7 (10.1%) colleges offer PhD degrees focused on pharmacogenomics.
Table 1.
Demographics and Pharmacogenetic Instruction Data of Respondents to a Survey on Pharmacogenetics and Pharmacogenomics Education in US Colleges of Pharmacy (N = 75)
aOnly the responses of those colleges/schools that taught pharmacogenomics/pharmacogenetics were included in question 2 (N = 69.)
bSelect all that apply, percentage may be greater than 100.
cPercentage available only for questions asked.
dThe survey was approved by AACP and partially funded by the CDC via a grant to Dr. Grace M. Kuo's (University of California-San Diego) research team. This team is developing the PharmGenEd program (“Pharmacogenomics Education Program: Bridging the Gap between Science and Practice”) for use by colleges and schools around the country.
Multiple faculty members (51, 73.9%) rather than a single individual (17, 24.6%) provided the majority of pharmacogenomic instruction at colleges of pharmacy; 15 (21.7%) colleges were reported to require specific prerequisite course work. Fifteen (21.7%) of the colleges taught this subject matter as a standalone course, 50 (72.5%) included it as part of other required didactic coursework, and 24 (34.8%) taught it as an elective didactic course. Pharmacogenomics subject matter was taught throughout all of the first 3 professional years of the curriculum by 13 (18.8%) of the colleges, but overall the content emphasis appeared to be in the second year, with 53 (76.8%) having taught the coursework in that year. The depth of content coverage for more than 80% (n = 57) of the colleges was less than 30 didactic hours of instruction throughout the entire program.
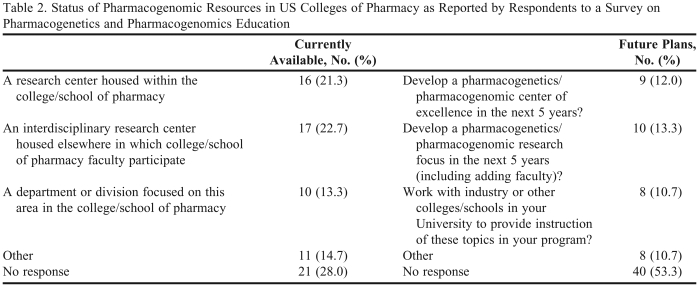
In order to assess the availability of pharmacogenomic resources, respondents were asked to identify current resources and plans for developing new resources over the next 5 years (Table 2). Of the 75 respondents, 33 (44.0%) housed a pharmacogenomics research center within their college, or had an interdisciplinary research center accessible elsewhere; 10 (13.3%) had a department focused on this area in their college. Nineteen were going to develop a center of excellence and/or a research focus in the area in the next 5 years. Respondents from 15 (20.0%) colleges indicated plans to hire additional faculty in this area within the next 3 years. Others did not know (39, 52.0%) or did not respond to the question (21, 28.0%).
Table 2.
Status of Pharmacogenomic Resources in US Colleges of Pharmacy as Reported by Respondents to a Survey on Pharmacogenetics and Pharmacogenomics Education
When asked about the current state of pharmacogenomics instruction, the majority of respondents believed the status at other colleges was poor or not at all adequate (46, 61.3%). However, only 22 (29.3%) believed their own school had a poor or not at all adequate state of instruction in this area.
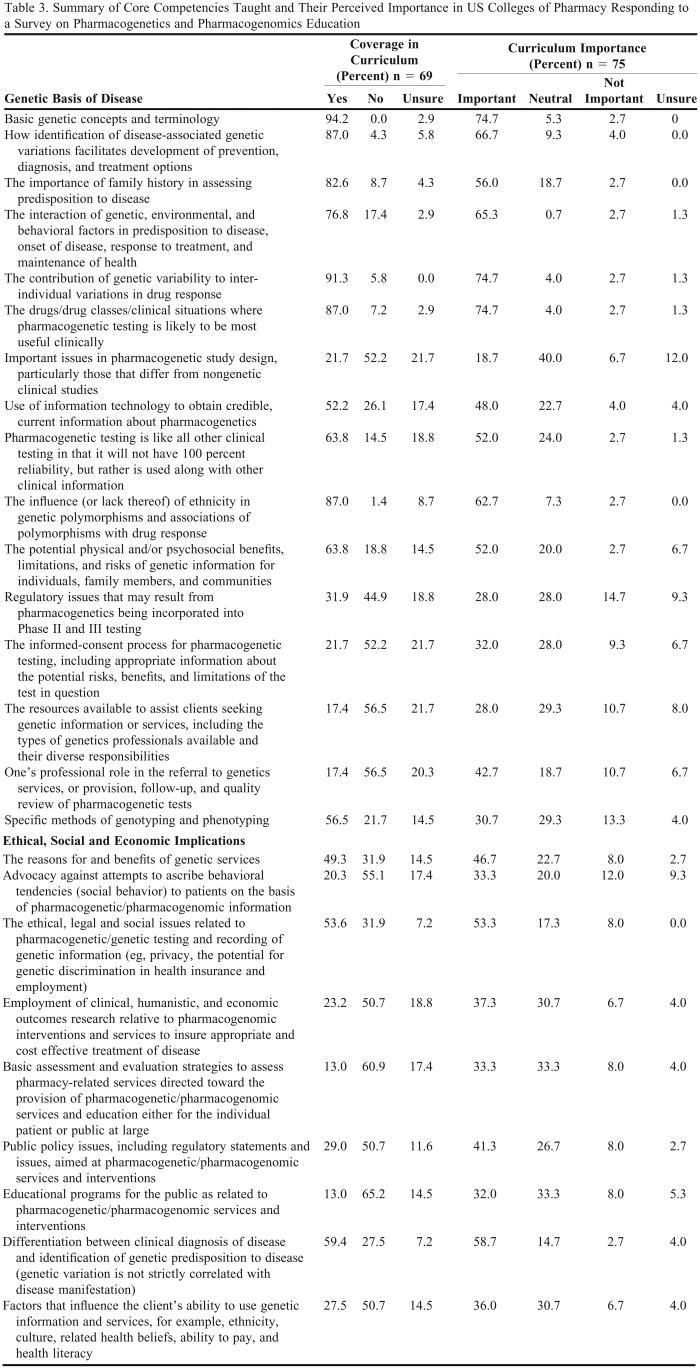
Table 3 provides a summary of the core competencies taught within the curriculum and the level of importance respondents placed on each. The items on the questionnaire pertaining to these competencies were revised slightly from the one used by Latif and McKay to match the September 2007 NCHPEG Core Competencies for all Healthcare Professionals revisions.11 The 20 items for the genetic basis of disease were reduced to 16 items for this study; however, the 9 items under the ethical, social, and economic implications domain remained the same. Eleven (68.8%) of the 16 genetic basis of disease items but only 2 (22.2%) of the 9 ethical, social, and economic implications were being addressed in the majority of colleges.
Table 3.
Summary of Core Competencies Taught and Their Perceived Importance in US Colleges of Pharmacy Responding to a Survey on Pharmacogenetics and Pharmacogenomics Education
Only 9 (56.2%) of the 16 genetic basis of disease topics and the same 2 (22.2%) ethical, social, and economic implication items were considered important for instruction to PharmD students by more than 50% of respondents. The genetic basis of disease domain had 4 topics that were covered in curricula at a 20% higher rate than the percentage of respondents considering the topic area important. These were: (1) how identification of disease-associated genetic variations facilitates development of prevention, diagnosis, and treatment options; (2) the importance of family history in assessing predisposition to disease; (3) the influence (or lack thereof) of ethnicity in genetic polymorphisms and associations of polymorphisms with drug response; and (4) specific methods of genotyping and phenotyping.
Although 35 (46.7%) colleges plan to increase the number of coursework hours dedicated to pharmacogenomic instruction, faculty development was not high on the agenda, with 41 (54.7%) having no current plans for such development programs. The majority of respondents indicated they were interested in having access to (66, 88.0%) and/or collaborating (51, 68.0%) on the shared pharmacogenomics curriculum that is being developed with the CDC grant.
DISCUSSION
The purpose of this study was to assess the breadth and depth of pharmacogenomics content instruction, the importance of these topics as perceived by respondents, and whether faculty development was available relative to these areas in US colleges of pharmacy. The results, where applicable, were also to be compared to those determined previously by Latif and McKay.
In the current study, 69 of 75 (92.0%) colleges were reported to be teaching pharmacogenomics within any their programs, and 67 (89.3%) colleges were teaching it within their current PharmD curriculum. This is up from 78% of programs providing this content in any program found by Latif and McKay, and 39% providing it in the PharmD curriculum.
Findings in this study with regard to who provides instruction is consistent with Latif and McKay's findings of 28 (68.3%) multiple and 3 (7.3%) single faculty members responsible for instruction. Thus, the content tends to be handled in team taught courses rather than provided by a single faculty member with expertise in the areas. There was an increase in the number of colleges requiring specific prerequisite coursework (15, 21.7%) compared to the previous study (5, 12.2%).
In pharmacogenomics, organization of the content was similar to what was found by Latif and McKay where 4 (9.8%) of their responding colleges taught it as a standalone course, 19 (46.3%) included it as part of another didactic course, and 1 (2.4%) taught it as a standalone elective. This is also what would be expected relative to who teaches because incorporation into other courses might lend itself to team teaching.
Latif and McKay found that 20 (49%) colleges of pharmacy planned to hire at least 1 additional faculty member in this area within the 3 years following their survey. Fifteen (20.0%) of the responding colleges planned to hire faculty members in this area within the next 3 years. Though this might indicate a reduction in interest, it might also reflect that more content is already being taught by faculty hired in recent years.
Pharmacogenomics instruction appeared to be provided in roughly similar percentages of postgraduate programs (11, 15.9% MS; 27, 39.1% PhD) as found by Latif and McKay (16, 39% Masters/PhD/other). Graduate programs in 3 (4.9%) of the respondents' colleges in the current study offered MS degrees and 7 (10.1%) colleges offered PhD degrees in pharmacogenomics related areas.
With regard to breadth of content coverage, Latif and McKay evaluated 2 domains of competencies. They found 11 (55%) out of their 20 items of genetic basis of disease and 3 (33.3%) of the 9 items from ethical applications and social and economic implications were being addressed by the majority of the respondents' colleges. In this study, 11 of 16 (69%) of the first domain were covered by more than 50%, but only 2 of 9 of the second domain. Though there is considerable coverage of some pharmacogenomics related topics, many were not covered at all by many colleges. Since the competencies were developed by AACP and a national organization suggesting core competencies for all health care professionals, there is room to expand pharmacogenomics topics taught in the curriculum.3,11
The primary finding of this study is that the majority of colleges of pharmacy are now providing some level of pharmacogenomic instruction within their curriculum, indicating an increased awareness of the need to do so, and thus demonstrating alignment with AACP recommendations about including this material within the PharmD curriculum. The secondary finding is the somewhat limited focus in faculty development for this subject matter.
Increased awareness of pharmacogenomics over the last 5 years, and emphasis on the area from AACP, ACPE, and the NCHPEG core competencies, are likely contributing factors in the differences between the 2 studies. Over the past 5 years, considerable attention to pharmacogenomics-related topics has been given by many journals and the lay press.14 For example, in 2005 Moridani noted the word pharmacogenomics or pharmacogenetics had been included in 5 journal titles.10 This emphasis helps increase the awareness of its potential value to patient care.
On the other hand, perceptions of the respondents relative to the state of instruction at other colleges of pharmacy declined (poor or not at all adequate, 46, 61.3%) compared to those found by Latif and McKay, where almost half of the respondents believed that the level of instruction was average (36.6%) or better (12.2%). Perhaps respondents believe that the quality of instruction is not adequate because of the advances in pharmacogenomics over the last 5 years. Interestingly, the respondents' opinions of their own college were much better, perhaps due to greater knowledge of efforts being made at their campus than elsewhere.
Although colleges plan to increase the number of coursework hours, there appears to be some disconnect between plans to increase coursework hours without preparing, hiring, or developing faculty members to teach this subject. Plans for developing a pharmacogenomic center of excellence and research focus, as well as working with industry, could contribute to a lack of need for faculty development since these options would likely include having faculty members who are knowledgeable on the subjects available for mentoring others as needed. No questions were asked to better understand this disconnect, leaving room for further investigation.
There were several potential limitations to this study. One relates to identification of the most appropriate individual to answer the questionnaire. Though deans would likely know the appropriate contact, it is possible that the selected individual may not have been the best person to provide the most accurate data. Another potential limitation is that some of the responses may have been simply a “best guess.” The survey instrument limitations stated by Latif and McKay hold true for this study as well.2 Since the content areas for the questionnaires in both studies were based on AACP's Academic Affairs Committee recommendations and NCHPEG suggested core competencies, they may have missed content that would be considered important by some college of pharmacy faculty for their curriculum. For example, one respondent suggested that other content such as proteomics, which allows for the bigger picture of discovering biomarkers for diagnosis, prognosis, and treatment of human disease, should be considered in the development of pharmacogenomic curricula. A few respondents provided comments about the way questions were asked. For instance, concern was expressed that the questionnaire may have been geared towards non-integrated teaching and one observed that responses regarding importance of content would vary depending on the type of faculty member responding to the items. Even with these limitations, the results suggest continued progress and academic enhancements in the area of pharmacogenomics.
Though it was not the intent of this study to be prescriptive about course content in the area of pharmacogenomics and pharmacogenetics, the results provide information on what the respondents believe is being taught in their colleges and schools of pharmacy. This information might be useful to committees contemplating content additions or deletions for their curriculum. There are many challenges associated with determining what must and should be in a pharmacy curriculum, and most often these challenges relate to adding more with a relatively fixed number of hours available for teaching. Knowing what other colleges may be teaching and what some faculty consider important may have some utility.
CONCLUSION
This study assessed the breadth, depth, and perceived importance of pharmacogenomics instruction and of faculty development in colleges of pharmacy. In the previous study by Latif and McKay, 32 (78.0%) colleges responding were providing some pharmacogenomic instruction within their programs (PharmD, MS, PhD), though only 39% provide the subject matter to PharmD students. With increased awareness of the need to teach this subject, 69 of 75 (92.0%) of colleges responding to this study were now teaching pharmacogenomics within 1 or more of their programs and 67 (89.3%) colleges were teaching it within their PharmD curriculum. There was a general consensus among the respondents that teaching pharmacogenomics is becoming increasingly important in the practice of pharmacy, but there was limited emphasis on faculty development in the area.
ACKNOWLEDGMENTS
This study was supported in part by the Pharmacogenomics Education Program funded by the Centers for Disease Control and Prevention (No. 1U38GD000070). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC.
REFERENCES
- 1. Final Report of the 2007-2008 Bylaws and Policy Development Committee. American Association of Colleges of Pharmacy. http://www.ajpe.org/view.asp?art=aj7206S16&pdf=yes. Accessed January 13, 2010.
- 2.Latif DA, McKay AB. Pharmacogenetics and pharmacogenomics instruction in colleges and schools of pharmacy in the United States. Am J Pharm Educ. 2005;(2) Article 23. [Google Scholar]
- 3.Johnson JA, Bootman JL, Evans WE, et al. Pharmacogenomics: a scientific revolution in pharmaceutical sciences and pharmacy practice. Report of the 2001-2002 Academic Affairs Committee. Am J Pharm Educ. 2002;66(9) [Google Scholar]
- 4. Core competencies in genetics essential for all health-care professionals. National Coalition for Health Professional Education in Genetics, Lutherville, MD; 2001.
- 5.Caldwell J. Drug metabolism and pharmacogenetics: the British contribution to fields of international significance. Br J Pharmacol. 2006;147(S1):S89–S99. doi: 10.1038/sj.bjp.0706466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Streetman DS. Emergence and evolution of pharmacogenetics and pharmacogenomics in clinical pharmacy over the past 40 years. Ann Pharmacother. 2007;41:2038–2041. doi: 10.1345/aph.1K273. [DOI] [PubMed] [Google Scholar]
- 7. Human Genome Project Information. US Department of Energy Office of Science, Office of Biological and Environmental Research, Human Genome Program. http://www.ornl.gov/sci/techresources/Human_Genome/home.shtml. Accessed November 25, 2009.
- 8.Feetham S, Knisley M, Parker RS, Gallo A, Kenner C. Families and genetics: bridging the gap between knowledge and practice. Newborn Infant Nurs Rev. 2002;2:247–253. [Google Scholar]
- 9.The International Warfarin Pharmacogenetics Consortium. Estimation of the warfarin dose with clinical and pharmacogenetic data. N Engl J Med. 2009;360:753–764. doi: 10.1056/NEJMoa0809329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moridani MY. The significance of pharmacogenomics in pharmacy education and practice. Am J Pharm Educ. 2005;69(2) Article 37. [Google Scholar]
- 11. Core competencies in genetics essential for all health-care professionals. National Coalition for Health Professional Education in Genetics. September 2007. http://www.nchpeg.org/core/Core_Comps_English_2007.pdf. Accessed January 13, 2020.
- 12. Accreditation Standards and Guidelines for the Professional Program in Pharmacy leading to Doctor of Pharmacy Degree. Accreditation Council for Pharmacy Education. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed October 6, 2009.
- 13.Churchill GA, Iacobucci D. Marketing Research: Methodological Foundations. 9th ed. Cincinnati, Ohio: Thomson/South-Western; 2005. [Google Scholar]
- 14. Realizing the promise of pharmacogenomics: Opportunities and challenges. Department of Health & Human Services. March 2007. http://oba.od.nih.gov/oba/SACGHS/reports/SACGHS_PGx_report.pdf. Accessed November 25, 2009.