Abstract
Based on the theory that generalized anxiety disorder (GAD) is maintained through a reactive and fused relationship with one’s internal experiences and a tendency towards experiential avoidance and behavioral restriction, an acceptance based behavioral therapy (ABBT) was developed to specifically target these elements. Since ABBT has been shown to be an efficacious treatment in previous studies, the current study focuses on proposed mechanisms of change over the course of therapy. Specifically, the current study focuses on session-by-session changes in two proposed mechanisms of change: acceptance of internal experiences and engagement in meaningful activities. Overall, clients receiving ABBT reported an increase in the amount of time spent accepting internal experiences and engaging in valued activities. Change in both acceptance and engagement in meaningful activities was related to responder status at post-treatment and change in these two proposed mechanisms predicted outcome above and beyond change in worry. In addition, change in acceptance was related to reported quality of life at post-treatment.
Keywords: Acceptance, values, experiential avoidance, behavioral therapy, generalized anxiety, mechanisms of action
Generalized anxiety disorder (GAD), which is characterized by anxiety, tension, and chronic and persistent worry (American Psychiatric Association, 1994), is associated with significant distress and psychosocial impairment (Kessler, Waters, & Wicchen, 2004). Because of the chronic course of GAD, it is unlike to remit without treatment (Yonkers, Warshaw, Massion, & Keller, 1996). While a variety of efficacious cognitive behavioral treatments exist, only about half of those treated are achieving high end-state functioning (see Waters & Craske 2005, for a review), making GAD one of the least successfully treated anxiety disorders (Brown, Barlow, & Liebowitz, 1994). In an effort to improve the efficacy of treatment for GAD, several promising new treatments have recently been developed (see Heimberg, Turk, & Mennin, 2004, for a review). One of these treatments is an acceptance-based behavioral therapy (ABBT; Roemer & Orsillo, 2005) which, as described in more detail below, specifically aims to help clients become more accepting of their internal experiences and increase their engagement in chosen actions in important life domains. This engagement in behaviors that are congruent with what is personally meaningful to the client has been termed valued action (Wilson & Murrell, 2004).
Drawing from research and theory by Borkovec (e.g., Borkovec, Alcaine, & Behar, 2004), Hayes (e.g., Hayes, Strosahl, & Wilson, 1999), Segal and colleagues (e.g., Segal, Williams, & Teasdale, 2002) and others, Roemer and Orsillo, 2005 propose that GAD is maintained through problematic and reactive relationships with internal experiences and internal and behavioral responses aimed at avoiding and decreasing distress. According to this model, anxiety is maintained in part by a reactive and over-identified relationship with internal experiences (thoughts, feelings, urges, images, bodily sensations, etc.). Through learning, internal experiences can elicit a cascade of negative emotions, judgmental thoughts, and urges to avoid. For example, individuals with symptoms of GAD have been found to report a greater negative reactivity toward their emotions in a clinical sample (Mennin, Heimberg, Turk, & Fresco, 2005) and to view their worrisome thoughts as more dangerous and uncontrollable in an analogue sample (Wells & Carter, 1999) compared to individuals with lower levels of GAD symptomatology. This reactivity towards emotions, coupled with a proposed tendency to experience emotions as all-encompassing and constant, may lead to an experience of internal experiences as unacceptable, intolerable, and threatening, eliciting strong urges to escape or avoid these experiences. However, experiential avoidance, or internal strategies aimed at suppressing our anxious thoughts, feelings, or sensations, decreasing their frequency or changing their form, can paradoxically increase distress (e.g., Hayes, Wilson, Gifford, Follette, & Strosahl, 1996; Salters-Pedneault, Tull, & Roemer, 2004). Higher levels of experiential avoidance have been reported in individuals with GAD compared to those without GAD (Lee, Orsillo, Roemer, & Allen, 2009). Similarly, attempts to avoid events or situations that might elicit anxiety can restrict access to enjoyable and fulfilling activities, severely impacting quality of life and eliciting additional distress. Clients with GAD often report that choices about how to engage in work, relationships and leisure activities are made based on lessening anxiety rather than maximizing satisfaction and that even when they are engaged in potentially meaningful activities they are often distracted by their worries. Additionally, individuals diagnosed with GAD report living less consistently with their values than individuals not diagnosed with GAD (Michelson, Lee, Orsillo, & Roemer, 2008). This may account for the diminished quality of life reported by those with GAD (Henning, Turk, Mennin, Fresco, & Heimberg, 2007). Thus, the internal and behavioral strategies engaged in to avoid anxiety and distress paradoxically increase those responses, eliciting more negative reactions and urges to avoid and escape, reducing engagement in meaningful activities and perpetuating the cycle of anxiety.
If GAD is maintained through problematic and reactive relationships with internal experiences, experiential avoidance, and behavioral restriction, then a treatment that addresses these components should be efficacious. Specifically, treatment should modify one’s relationship with internal experience, decrease avoidance and increase flexibility, and increase action in areas that are of importance to the individual so that the focus is more on engagement than on avoidance. In response, Roemer and Orsillo (2007; see Roemer & Orsillo, 2009 for a more detailed description of the treatment approach) developed an acceptance-based behavioral therapy (ABBT) for GAD. This treatment, which incorporates acceptance and mindfulness strategies with more traditional behavior therapy techniques, draws explicitly from cognitive behavioral interventions for GAD (e.g., Borkovec, Newman, Lytle, & Pincus, 2002) as well as from acceptance and commitment therapy (Hayes et al., 1999), mindfulness-based cognitive therapy (Segal et al., 2002), and dialectical behavior therapy (Linehan, 1993). An assumption underlying ABBT is that it is not the initial worry, feeling, physical sensation, or image that is problematic, but rather the rigid unwillingness to have these internal experiences. In other words, developing an acceptance of, or a willingness to have these internal experiences should reduce distress and interference associated with the internal experiences, thus reducing the negative reactivity and the cycle of anxiety. From this perspective, the focus of treatment is not on eliminating worry, but rather on decreasing the distress and interference associated with this cognitive activity.
ABBT for GAD involves 1) psychoeducation regarding the nature of worry, anxiety, emotion, and experiential avoidance, 2) practice developing mindfulness and acceptance as an alternate response to internal experiences, and 3) identification of valued directions, recognition of obstacles to these actions, and practice engaging in chosen actions nonetheless. The focus is specifically on making choices to act in value-consistent ways rather than in ways that are motivated by avoidance of anxiety. Clients receiving ABBT have shown significant improvements in symptoms in both a small open trial (Roemer & Orsillo, 2007) and a wait list controlled trial (Roemer, Orsillo, & Salters-Pedneault, 2008). In the open trial, the 16 clients who received ABBT reported large and significant changes in GAD severity, worry, and anxiety symptoms from pre to post treatment and at a three month follow-up assessment. Likewise, clients reported a large improvement in quality of life from pre-treatment to both post-treatment and follow-up. In the wait list controlled trial, clients receiving ABBT showed significantly greater improvement on GAD severity, worry, and depression compared to those in the wait list. At post treatment or post waiting list, 75% of participants receiving ABBT were considered treatment responders, compared to 8% on the wait list. Clients also experienced significant changes on a self-report measure of experiential avoidance (Roemer et al., 2008), as well as on a measure of reported anxiety about emotional responses (Treanor, Erisman, Salters-Pedneault, Orsillo, & Roemer, 2009), both are proposed mechanisms of change.
Although further evaluation of the relative efficacy of ABBT of GAD is needed (and a comparative treatment study is currently underway), another important step in treatment development is to assess whether outcome is related to the two hypothesized mechanisms of change: acceptance of internal experiences and engagement in valued action. In the current study, we examine the influence of these proposed mechanisms using data from the open trial and the wait list controlled trial described above. Consistent with the acceptance-based behavioral model, it was expected that clients would report an increase in their acceptance of their internal experiences and an increase in the amount of time they were engaged in valued activities over the course of therapy. It was also hypothesized that these changes in acceptance and engagement in values would predict outcome such that clients who improved more on these dimensions would also be more likely to be treatment responders and would experience more of an increase in quality of life. Finally, based on the focus of treatment in ABBT, we predicted that outcome, including changes in quality of life, would be more closely related to changes in acceptance and engagement in valued action than to changes in the amount of worry since the focus of treatment is not specifically on reducing worry, but rather on changing how one responds to worries.
Method
Data for the current study were collected as part of two treatment outcome trials examining the efficacy of ABBT: a waitlist control trial (Roemer et al., 2008) and an open trial (Roemer & Orsillo, 2007). Complete details of the studies’ methodology and results can be found in the outcome papers. Details relevant to the current study are presented below.
Participants
Participants in this study include 43 clients who received ABBT as either part of a waitlist control trial (n = 27) or an open trial (n = 16). Participants were recruited into the treatment studies from a pool of individuals who sought treatment at the Center for Anxiety and Related Disorders at Boston University and were assessed using the Anxiety Disorders Interview Schedule for DSM-IV-Lifetime version (ADIS-IV-L; DiNardo, Brown, & Barlow, 1994). Participants were included in the outcome studies if they received a principal diagnosis of GAD or major depressive disorder plus GAD, with GAD symptoms causing the most distress and interference; denied current suicidal intent; did not meet criteria for bipolar disorder, substance dependence, or psychotic disorders; and were 18 or older.
Of the 43 clients, 29 (67.4%) were female and 14 (32.6%) were male. The majority (35 or 81.4%) self-identified as being White, 5(11.6%) as Latino(a), 1 (2.3%) as Black, 1 (2.3%) as Asian, and 1 (2.3%%) as Asian and White. On average, clients were 33.72 (SD = 11.97) years old (range 19–66). At the beginning of therapy, clients received an average GAD clinician severity rating of 5.79 (SD = 0.78) from the ADIS-IV-L interview. In this sample, 26 clients received prior psychotherapy for anxiety and 4 for depression. Additionally, 30 had taken prior psychotropic medications for anxiety or mood problems. Of the 43 clients who began therapy, 37 completed the post-treatment assessment.
Measures
Weekly Assessment
The Weekly Assessment, which was designed specifically for the outcome studies, asks respondents to indicate what percentage of time they spent engaged in certain therapy-relevant activities over the preceding week on a scale from 0 to 100. This study focuses on three items from this measure: What percentage of time did you find yourself worrying over the past week?; What percentage of time did you feel accepting of your internal experience (thoughts and feelings) as opposed to trying to push thoughts and feelings away?; and What percentage of the time did you feel you were spending time on the things that are important to you? Participants completed this measure prior to each therapy session.
Action and Acceptance Questionnaire (AAQ; Hayes, Strosahl, et al., 2004)
This 9-item measure was given at pre- and post-treatment to assess experiential avoidance. On this scale, high scores represent experiential avoidance and low scores reflect acceptance. The AAQ has demonstrated adequate internal consistency (α = .70) and test-retest reliability (r = .64) over four months in an undergraduate sample (Hayes et al., 2004). Likewise, scores on the AAQ were moderately correlated with measures of the related construct of cognitive avoidance (r = .50). In the present sample, the AAQ demonstrated adequate internal consistency at pre- (α = .73) and post-treatment (α = .88).
Valued Living Questionnaire (VLQ; Wilson, Sandoz, Kitchens, & Roberts, 2009)
The VLQ is a two-part questionnaire designed to measure aspects of valued living. The first part of the questionnaire assesses the importance of 10 areas that have been identified as valued domains (e.g., family, friendship, work) on a 10 point Likert scale. The second part asks about how consistently the respondent is living according to each of the 10 values using a 10 point Likert scale. A composite score is derived for each area of valued living by multiplying the importance score by the consistency score to indicate the extent to which respondents are living consistently with values that are important to them. The VLQ has demonstrated adequate reliability and is positively correlated with other measures of valued living (Wilson et al., 2009). In this sample, the VLQ consistency subscale demonstrated adequate internal consistency at pre- (α = .77) and post-treatment (α = .90).
Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990)
This 16-item measure of trait worry was completed at pre- and post-treatment. This well-established measure of worry has been shown to have very good reliability (α’s from .86 to .93) and good test-retest reliability (Molina & Borkovec, 1994). The PSWQ has been found to discriminate GAD from other anxiety disorders (Brown, Antony, & Barlow, 1992). In this sample, the PSWQ demonstrated adequate internal consistency at pre- (α = .77) and post-treatment (α = .92).
Quality of Life Inventory (QOLI; Frisch, Cornwell, Villanueva, & Retzlaff, 1992)
This measure, based on an empirically validated model of life satisfaction, assess the importance and satisfaction with 16 areas of life. Respondents indicate the degree of importance and the level of satisfaction in each domain and then these two values are multiplied resulting in a composite score for each domain. In this study, pre- to post-treatment residualized gain scores from a shortened 11-item version of the QOLI were used as a measure of treatment outcome1. The QOLI has demonstrated good internal consistency (α's ranging from .83 to .89 in clinical samples), excellent test-retest reliability (r = .91), and adequate validity through correlations with other measures of well-being and satisfaction (Frisch et al., 1992). In the current sample, the QOLI demonstrated good internal consistency at pre- (α = .83) and post-treatment (α = .80).
Treatment responders
In this study and the outcome studies, participants were considered treatment responders if they demonstrated a 20% or greater reduction from pre- to post-treatment on at least three of four anxiety measures. This procedure was adapted from Borkovec et al. (2002). These measures were the ADIS-IV-L GAD Clinical Severity Rating, the PSWQ, the Depression Anxiety and Stress Scale – Anxiety subscale (Lovibond & Lovibond, 1995), and the Depression Anxiety and Stress Scale – Stress subscale. In this sample, 67.4% of the intent to treat sample were considered treatment responders.
Treatment
All participants in this study received ABBT for GAD. As described above and in the treatment outcome articles, ABBT consisted of 16 sessions of individual psychotherapy. The first four sessions were 90 minutes, and the rest were 60 minutes. ABBT involves increasing clients’ awareness of patterns of anxious responding, the function of emotions, and the role of experiential avoidance using psychoeducation, experiential demonstrations, and between-session monitoring. Clients were also taught a variety of mindfulness practices and were encouraged to establish both formal and informal daily mindfulness practices. Clients also engaged in written exercises about their values. Treatment focused on bringing mindful awareness to valued activities.
Data Analysis
Changes in worry, acceptance of internal experiences, and engagement in valued action over the course of treatment were analyzed using latent growth curve modeling. Latent growth curve modeling describes growth using two parameters, the intercept and the slope. A mean growth curve is estimated for the entire sample so that the intercept is the score at a set time point (second session in this sample) and the linear slope is the average rate of growth between treatment sessions. In addition, individual intercepts and slopes are allowed to vary across individuals via deviations from the mean initial status and slope parameter. The variance of the individual intercepts and slopes can also be estimated, as can the covariance between the intercepts and slopes. Because a separate intercept and slope is estimated for each individual, these parameters can be correlated with each other and with additional outcome measures. For a more detailed description of latent growth curve modeling, please see Preacher, Wichman, MacCallum, and Briggs (2008). Francis, Fletcher, Steubing, Davidson, and Thompson (1991) outline a number of advantages of growth curve analysis over more traditional modes of analysis (i.e., trend analysis using ANOVA) for the study of change. For example, in growth curve analysis, the focus is on individual change. Also, participants can be included in the analysis even if they are missing data through maximum likelihood (ML) estimation techniques.
For the analysis presented here, growth curve models were run using Mplus 3.13 (Muthén & Muthén, 2006), a structural equation modeling software package. Z-tests are used to assess the statistical significance of the model parameters. Z-values greater than 1.96 are statistically significant using an alpha level of .05, and values greater than 2.58 are significant at an alpha level of .01.
Given the small sample size in this study, effect sizes are reported where relevant. For the growth curve analyses, Pearson’s r is reported. Typically, r = 0.1 is considered a small effect size, r = 0.3 medium, and r = 0.5 large (Cohen, 1988). For logistic regression analyses, odds ratios are reported. An odds ratio of 1 indicates that an event is equally likely in both groups, whereas an odds ratio greater than one implies that the event is more likely in the first group. For the linear regression analyses, f2 will be used. By convention, f2 effect sizes of 0.02, 0.15, and 0.35 are considered small, medium, and large, respectively (Cohen, 1988).
Results
Table 1 provides the means, standard deviations, and ranges of scores for the primary variables of interest in this study: percentage of time accepting internal experience, percentage of time engaged in valued actions, and percentage of time worrying. As can be seen in the table, there was a wide range of reported percentages towards the beginning of the therapy.
Table 1.
Mean, Standard Deviation, and Range of for Percentage of Time Engaged in Worry, Acceptance, and Valued Action at Sessions 2
| Mean | SD | Range | |
|---|---|---|---|
| Worry | 56.51 | 22.46 | 30–100 |
| Acceptance | 42.56 | 24.98 | 0–90 |
| Valued Action | 47.67 | 24.96 | 10–100 |
Because these analyses primarily use single item self-report measures of the constructs of interest, it is important to see if these responses correlate with established measures of similar constructs. As expected, the percentage of time spent worrying at the end of therapy was significantly correlated with scores on the PSWQ, an established measure of worry, at the post-treatment assessment [r(36) = .37, p = .02, 95%CI .06-.62]. Similarly, the linear change in percentage of time spent worrying across therapy was close to being significantly correlated with pre to post treatment change on the PSWQ [r(36) = −.31, p = .06, 95%CI −.58-.01]. The percentage of time spent accepting internal experiences at the end of therapy was significantly and negatively correlated with scores on an established measure of experiential avoidance (AAQ) which is conceptualized as the opposite of acceptance [r(36) = −.32, p = .05, 95%CI −.58−.00] and change in acceptance was correlated with pre to post-treatment change on the AAQ [r(36) = .37, p = .02, 95%CI .06−.62]. Likewise, the percentage of time spent engaged in valued actions at the end of therapy was moderately, although not significantly correlated, with scores on the Valued Living Questionnaire (VLQ) [r(33) = .32, p = .06, 95%CI −.01−.60]. Similarly, the linear change in percentage of time spent engaged in valued action was significantly and positively correlated with change on the VLQ [r(33) = .40, p = .03, 95%CI .08−.65].
Trajectories of worry, acceptance, and engagement in valued action
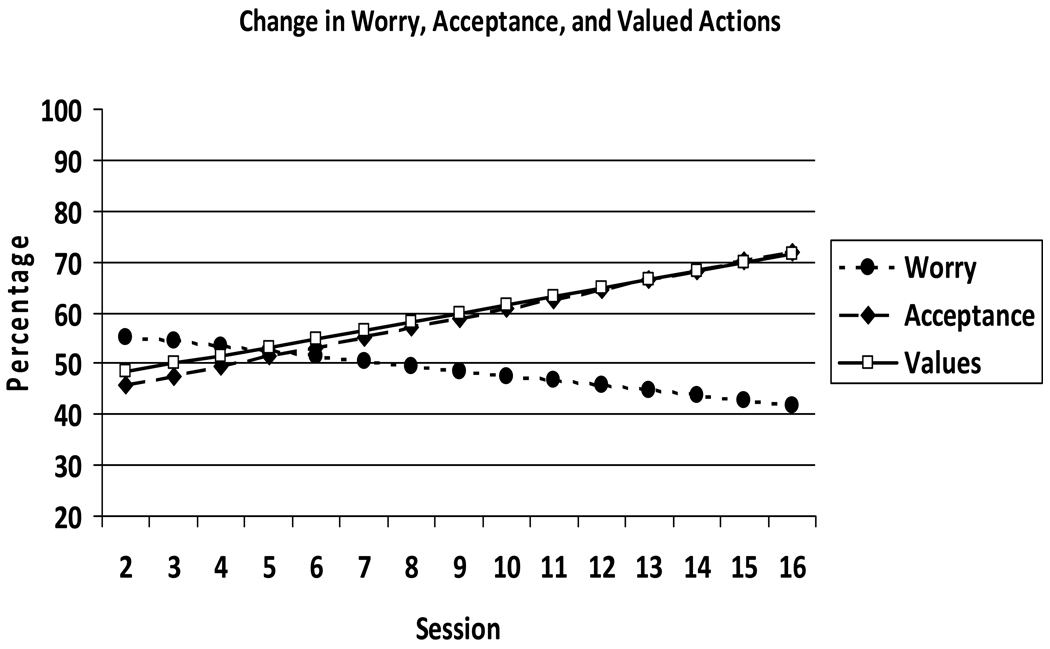
To test the first hypothesis that clients would report significant changes in worry, acceptance, and engagement of valued action over the course of ABBT, a series of linear growth curve models were estimated. A separate model was conducted for session-by-session changes in worry, acceptance, and engagement in valued actions. Figure 1 shows the projected trajectories for each of these three variables. For worry, the intercept, or average worry percentage at session 2, was 55.29 and the slope was −0.96. In other words, on average clients’ reported worry decreased from the 55.29% at session 2 to 41.85% of the time at the end of therapy (0.96 points per sessions from sessions 2 to 16). In terms of the percentage of time that clients reported being accepting of their internal experiences, clients reported being accepting 45.71 percent of the time at session 2, which increased by 1.88 points per session over the course of therapy. In other words, clients reported an increase in their acceptance of internal experiences from 45.71% at session 2 to 72.03% of the time by the end of therapy. Likewise, on average clients reported that they spent 48.31 percentage of time engaged in valued action at session 2, which increased by 1.66 points per session over the course of therapy. In other words, clients’ reports of engaging in valued actions increased from 48.31% to 71.55% over the course of therapy.
Figure 1.
Projected trajectories of change in worry, acceptance, and valued action over the course of ABBT
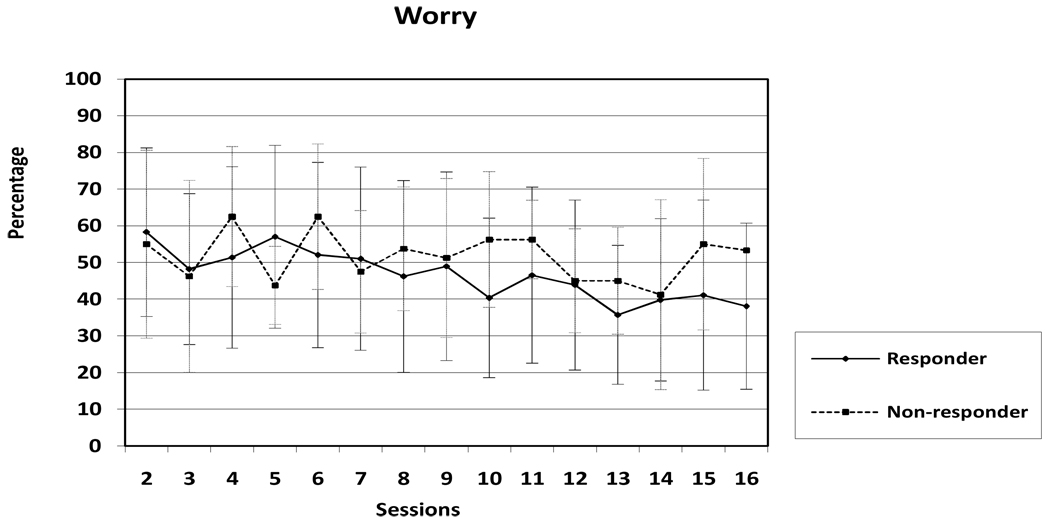
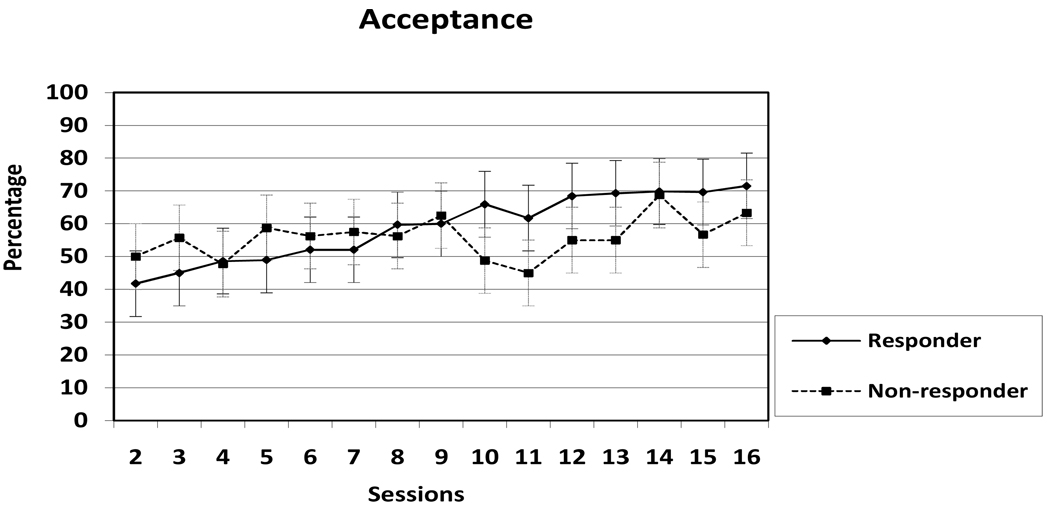
Before examining differences between responders and non-responders on these three variables, we were interested in looking at the mean session by session ratings for worry, acceptance and valued action for responders and non-responders descriptively to better understand the pattern of change. Therefore, Figure 2 through Figure 4 present the mean worry, acceptance, and engagement in valued action percentages for responders and non-responders for each session. For the acceptance means, there appears to be a large difference between responders and non-responders around sessions nine to 14. On the other hand, for valued action, the responders show a steady increase in the amount of time spent engaged in valued actions whereas the non-responders started with a higher percentage than the non-responders, but then do not experience as much movement over the course of therapy.
Figure 2.
Mean percentage of time worrying for responders and non-responders (± 1 standard deviation).
Figure 4.
Mean percentage of time engaged in valued action for responders and non-responders (± 1 standard deviation).
Change in Acceptance and Valued Action Predicting Responder Status and Quality of Life
To better understand the combined effect of change in acceptance and valued action on responder status, a parallel process growth model was run to simultaneously examine change on these two mechanisms of change. Table 2 presents correlations among the parameters. Acceptance scores at the beginning of therapy were significantly correlated with the rate of change in acceptance scores in that the lower the acceptance scores at the beginning of therapy, the more rapidly the percentage of time accepting internal experiences increased. There was also a significant negative correlation between percentage of time spent engaging in valued action at the beginning of therapy and the rate of change in action scores in that the lower valued action percentages at the beginning of therapy were related to a more rapid increase in valued action over the course of therapy. Additionally, the percentage of time accepting internal experiences was positively correlated with the percentage of time engaged in valued action at the beginning of therapy and the rate of change in acceptance was strongly and positively correlated with the rate of change in valued action. Interestingly, acceptance at the beginning of therapy was negatively correlated with the valued action slope in that the lower acceptance scores at the beginning of therapy were associated with more rapid increases in the percentage of time spent engaged in valued action; however the valued action at the beginning of therapy was not significantly correlated with the change in acceptance over the course of therapy.
Table 2.
Correlations between Growth Parameters
| 1. | 2. | 3. | 4. | |
|---|---|---|---|---|
| 1. Acceptance at Session 2 | 1.00 | |||
| 2. Acceptance Slope | −.64* | 1.00 | ||
| 95% Confidence Interval | (−.43 to −.79) | |||
| 3. Valued Action at Session 2 | .56** | −.29 | 1.00 | |
| 95% Confidence Interval | (.31 to .74) | (.01 to −.55) | ||
| 4. Valued Action Slope | −.52* | .78** | −.66* | 1.00 |
| 95% Confidence Interval | (−.27 to −.72) | (.64 to .88) | (−.45 to −.80) | |
Note. p < .05;
p < .01.
Predicting responder status
Responder status was added as a distal outcome variable to each of the three growth models presented above. Table 3 provides the parameter estimates for each of these models. As hypothesized, both change in acceptance and change in valued action significantly predicted post-treatment responder status. In other words, the more increases in acceptance or valued action that a client experienced over the course of therapy, the more likely that they were later considered a treatment responder. Interestingly, clients’ reports of percentage of time accepting internal experience and engaging in valued action at the beginning of therapy did not predict responder status at the end of treatment. Likewise, neither initial worry levels nor change in worry predicted responder status at post-treatment.
Table 3.
Intercept and Slope Predicting Responder Status for the Worry, Acceptance, and Valued Action Models
| Intercept |
Linear Change |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| R2 | Est | SE | Z | r | Est | SE | Z | r | |
| Worry | 5.6% | −0.002 | 0.005 | −0.406 | −.08 | −0.070 | 0.060 | −1.17 | −.27 |
| Acceptance | 21.8% | 0.004 | 0.006 | 0.687 | .15 | 0.157 | 0.067 | 2.346* | .55 |
| Valued Action | 31.1% | 0.001 | 0.005 | 0.141 | .03 | 0.185 | 0.085 | 2.177* | .58 |
Note. R2 = percent of variance in each outcome variable accounted for by intercept and slope. Est = Parameter Estimate; SE = Standard Error; Z = standardized z-score. Z > 1.96 is significant at p < .05; Z > 2.58 is significant at p < .01.
p < .05.
Predicting quality of life
As with responder status, the residualized gain score for quality of life was added as a distal outcome variable to each of the three growth models presented above. Table 4 provides the parameter estimates for each model. Change in acceptance, but not change in valued action significantly predicted post-treatment quality of life while accounting for pre-treatment scores on quality of life. In other words, larger increases in acceptance over the course of therapy were related to more improved quality of life at post treatment. However, neither change in valued action nor change in worry was a significant predictor of quality of life, although both revealed medium-sized effects.
Table 4.
Intercept and Slope Predicting Quality of Life for the Worry, Acceptance, and Valued Action Models
| Intercept |
Linear Change |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| R2 | Est | SE | Z | r | Est. | SE | Z | r | |
| Worry | 8.0% | −0.019 | 0.012 | −1.578 | −.31 | −0.158 | 0.133 | −1.188 | −.26 |
| Acceptance | 23.3% | 0.029 | 0.013 | 2.249* | .48 | 0.419 | 0.151 | 2.776** | .64 |
| Valued Action | 7.1% | 0.005 | 0.013 | 0.381 | .09 | 0.237 | 0.215 | 1.103 | .32 |
Note. R2 = percent of variance in each outcome variable accounted for by intercept and slope. Est = Parameter Estimate; SE = Standard Error; Z = standardized z-score. Z > 1.96 is significant at p < .05; Z > 2.58 is significant at p < .01.
p < .05
p < .01.
Mechanisms predicting change above change in symptoms
In order to determine whether change on the two proposed mechanisms of action predicts responder status over and above change in worry, a series of hierarchical logistic regression models were run to examine the relationships between responder status and the slope parameters from the unconditional worry, acceptance, and valued action growth curves (see Table 5). The model of change in worry predicting responder status was not significantly different from the intercept only model [χ2 (1) = 1.25, p = .26]. However, adding change in acceptance and change in valued action significantly improved the model [χ2 (2) = 9.18, p = .01], making the overall model significant [χ2 (3) = 10.43, p = .02]. Overall, this model correctly classified 83.4% of the individuals. Together, these models indicated that the mechanisms of change predict outcome above and beyond change in worry.
Table 5.
Summary of Logistic Regression Analysis for Variables Predicting Responder Status
| Responder Status |
|||||
|---|---|---|---|---|---|
| Variable | B | SE | Wald Test | OR | 95% CI |
| Step 1 | |||||
| Worry | −0.40 | 0.38 | 1.12 | 0.67 | 0.32−1.40 |
| Step 2 | |||||
| Worry | −0.29 | 0.40 | 0.52 | 0.75 | 0.34−1.65 |
| Acceptance | 0.56 | 0.47 | 1.42 | 1.76 | 0.70−4.42 |
| Values Action | 1.33 | 0.81 | 2.70^ | 3.77 | 0.77−18.33 |
Note. OR = odds ratio; CI = confidence interval.
p < .10.
Likewise, a series of linear regression models were run to predict quality of life from worry, acceptance, and valued action growth curves (see Table 6). In the first model, change in worry was close to significantly predicting quality of life (R2 = .08, F(1, 41) = 3.49, p = .07, f2 = .09). The model was improved upon by a near significant amount by adding the acceptance and valued action linear slopes (R2-change = .13, F-change (2, 39) = 2.50, p = .06, f2 = .15). The combined model significantly predicted quality of life (R2 = .20, F(3, 39) = 3.33, p = .03, f2 = .25).
Table 6.
Summary of Regression Analysis for Variables Predicting Quality of Life
| Quality of Life |
||||
|---|---|---|---|---|
| Variable | B | SE | β | ΔR2 |
| Step 1 | .08 | |||
| Worry | 71.35 | 38.20 | .28^ | |
| Step 2 | .13^ | |||
| Worry | 39.29 | 39.19 | .15 | |
| Acceptance | 83.74 | 46.02 | .30^ | |
| Values Action | −146.39 | 61.93 | −.41* | |
Note. p < .10
p < .05.
Exploratory Analyses
In ABBT for GAD, the first seven sessions are primarily psychoeducational, whereas the remaining sessions are more focused on practicing and implementing mindfulness and valued action practice in everyday life. Therefore, we wanted to examine these two phases separately. Table 7 presents the correlations between responder status and change in worry, acceptance, and engagement in valued action in sessions 2 through 7 and sessions 7 through 16. The data suggest that, for acceptance of internal experiences, change in the second, but not the first half of therapy, is more strongly related to responder status; however, for engagement in valued action, change across the entire course of therapy, as opposed to change in either half of treatment is most highly associated with responder status.
Table 7.
Correlations between Responder Status and Worry, Acceptance, and Engagement in Valued Action by Treatment Segment
| Responder Status | |||
|---|---|---|---|
| First Half |
Second Half |
Total |
|
| Worry | −.03 | −.11 | −.18 |
| 95% Confidence Interval | (−.33 to .28) | (−.40 to .20) | (−.46 to .13) |
| Acceptance | .04 | .34* | .40* |
| 95% Confidence Interval | (−.27 to .34) | (.04 to .58) | (.11 to .63) |
| Valued Action | .09 | .21 | .44** |
| 95% Confidence Interval | (−.22 to .38) | (−.10 to .48) | (.16 to .66) |
p < .05;
p < .01.
Discussion
Based on the theory that GAD is maintained through a reactive and fused relationship with one’s internal experiences and a tendency towards experiential avoidance and behavioral restriction, Roemer and Orsillo (2005) developed a treatment for GAD specifically targeting these elements. This acceptance based behavioral therapy (ABBT) produced favorable outcomes for the majority of clients receiving it in both an open trial and a randomized controlled trial (Roemer & Orsillo, 2007; Roemer et al., 2008). The current study, which involves secondary data analysis from these two previous studies, focused on the relationship between two proposed mechanisms of change and outcome for clients receiving ABBT: acceptance of their internal experiences and engagement in meaningful activities.
Although this preliminary study on the mechanisms of change in ABBT is limited by the use of single item, self-report measures and a small sample size, the findings presented here are largely consistent with the theory underlying ABBT. One challenge in studying longitudinal change is the balance between obtaining frequent assessments that are brief enough that they are acceptable to respondents yet reliable and valid enough that they adequate assess the construct of interest. For pragmatic reasons and concerns about participant burden, brief, single item measures were administered at every therapy session for the clients in this study. Although the use of brief single item measures allowed for a greater frequency of assessment while keeping participant burden low, there are limitations to this approach. For example, single item measures typically have lower reliability and validity than multi-item measures. In this sample, the correlations between the single item measures and their associated longer measures in this study are modest at best. However, because the two measures are intended to measure slightly different constructs, it is difficult to interpret these correlations. Assessments of reliability become even more complicated when, as in this study, there is expected variation from week to week on these measures. In this study, we attempted to address this by utilizing trajectories of change rather than relying on ratings at a single time point. Within the confines of this secondary data analysis, we have attempted to address these limitations by collecting multiple data points from each individual and by reporting effect sizes where possible. However, additional research is needed in which frequent assessments are collected using psychometrically sound measures of these mechanisms of change within a larger sample. Additionally, these results may or may not be specific to ABBT. It is unclear whether the changes in proposed mechanisms of action and their relationship to outcome can be generalized beyond this specific treatment as has been suggested by others (e.g., Segal et al.’s (2002) comments about how decentering may be a mechanisms of change in both cognitive behavioral and mindfulness based cognitive therapy). Given these limitations, these results should be considered preliminary.
Overall, clients reported that they were accepting of internal experiences and engaged in valued action a little less than half of the time at the beginning of therapy. As expected, over the course of therapy, these percentages increased to a little less than three quarters of the time by the end of therapy. This increase in acceptance and engagement in valued action predicted responder status and change in acceptance, but not engagement in valued actions, predicted quality of life. Interestingly, change in these two mechanisms predicted outcome above and beyond change in worry for responder status. In fact, change in the amount of worry was not significantly related to whether or not individuals were considered treatment responders. For quality of life a similar pattern was found. Although the contribution of change in worry approached significance, change in the two mechanisms contributed to a nearly significant increase in the variance in quality of life. However, given the sample size and the size of these effects, power was low (.44) for this analysis. Although this effect did not reach conventional levels of significance, the effect size was in the medium range for this relationship. At first the finding that worry frequency did not predict outcome may seem counter intuitive; however, in an acceptance based model, this finding is consistent with theory. In ABBT, the primary aim is not necessarily to reduce worry, but to change the relationship one has with the worries or other internal experiences, since it appears that attempts to stop worrying paradoxically increase the amount of worry (see Hayes et al., 1996). ABBT instead focuses on finding ways to move forward with meaningful activities regardless of whether or not worry is present. This movement towards engagement in valued actions is aided by and also encourages a greater acceptance of one’s internal experiences. However, as shown in this study, worry often does decrease over therapy. The finding that change in acceptance and engagement in action predict change above and beyond worry provides further support for an acceptance-based behavioral model. However, it should be noted that this may only be true for this specific therapy which directly provides clients with an acceptance-based model of change. It is unclear whether the same would be true in other forms of therapy that are more directly focused on changing the amount of worry. Additionally, future research should also examine whether change in acceptance and valued action contribute to outcome above and beyond other proposed change elements such as the working alliance or knowledge about GAD that are not specific to acceptance or mindfulness based therapies.
In general, clients in ABBT reported changes in acceptance and engagement in valued action that was consistent with the structure of therapy. For example, an examination of the change in means over the course of treatment suggests that clients report fairly consistent percentages of time accepting internal experiences and engaging in valued actions in the first half of therapy and then around session 8, they begin to report larger percentages of times for both acceptance and engagement with valued action. In ABBT, sessions one to seven are conceptualized as providing psychoeducation and an introduction to the main concepts covered in therapy. Then, beginning in session 8, the focus shifts to a more regular application of skills. It will be important to determine whether this apparent pattern is statistically significant in future studies with larger sample sizes. Further, research is needed to determine whether this pattern is actually due to the change in therapy focus or whether it is simply a function of the passage of time. A multiple baseline design where the shift from psychoeducation was varied in time could potentially address this issue.
The strong negative correlation between acceptance and engagement scores at the beginning of therapy and the rate of change raises the question of whether clients who begin at lower levels of these constructs simply have more room to change. Interestingly, in this sample, it is the nonresponders who report higher percentages of time accepting and engaged in valued actions at the beginning of therapy. In fact, this difference is statistically significant for engagement in action. Additionally, the initial levels of acceptance and valued action do not predict outcome. Although it could be the case that ABBT may be more helpful for individuals who do not already feel as engaged in their lives and are beginning with a lower amount of acceptance, this finding may also be an artifact of the difficulty inherent in having individuals self-report difficult to define concepts such as acceptance and engagement in valued actions. Clients who are less aware of what is meant by the terms “acceptance” and “engagement” may be reporting higher levels in the beginning of treatment because they are not aware of what they are missing. It is possible that without this awareness, levels of acceptance and engagement do not change as much over the course of therapy and thus these clients do not show improvement at the end of therapy. Future studies could examine whether constructs such as psychological mindedness are related to how clients respond to self-report measures of these hard to define concepts. Likewise, therapist ratings of either clients’ understanding of these concepts or their sense of clients’ acceptance and engagement in valued actions would allow for examination of whether these clinical impressions predict responder status and quality of life.
Descriptively, it appears that responders and nonresponders differ most from each other in the third quarter of therapy, especially in terms of amount of time accepting internal experiences. Interestingly, nonresponders appear to experience a decrease in their acceptance as they enter the phase of therapy when they are asked to engage in more actions, whereas responders experience a continued increase. This observation, combined with the finding that increased reports of acceptance during the second half of therapy predict responder status, while increased reports during the first half do not, indicates that continued focus on the cultivation of acceptance while engaging in valued action may be a particularly important element of treatment. However, this, as well as the other conclusions drawn regarding the session by session means for responders and non-responders, should be interpreted cautiously as this data is intended to be descriptive only. In this sample, there were not statistically significant differences in these means between responders and non-responders as can be seen by the overlapping error bars in figures two through four. It is also worth noting that the nonresponders appear to be beginning to “catch up” to the responders by the fourth quarter of therapy. Because the number of sessions was fixed in the treatment outcome trial, we cannot determine whether these clients would eventually reach the outcomes seen in the treatment responders if they were seen for more sessions. These suggestions about the course and length of therapy should all be considered conjecture at this point, given that they are based on observations of patterns rather than significance testing. More research is needed in larger samples in order to better elucidate the course of change in ABBT.
These secondary analyses of data from both the open and randomized controlled trials of ABBT are promising in that the treatment seems to decrease the distress and avoidance associated with GAD, a chronic and treatment resistant condition. Further, there is some support for the model of treatment in that the proposed mechanisms of action, increased valued action and acceptance, relate to responder status, above and beyond changes in reported symptoms (i.e., amount of worry). These findings suggest that future research into this approach to treatment may be beneficial both in advancing our understanding of GAD and in helping clients to make meaningful changes in their lives.
Figure 3.
Mean percentage of time accepting internal experiences for responders and non-responders (± 1 standard deviation).
Acknowledgments
This study was supported by National Institute of Mental Health Grants Nos. MH63208 and MH074589.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Unfortunately, due to a clerical error, five domains were omitted from the QOLI (children, relatives [other than children or partners], home, neighborhood, and community), so the scores reflect responses to the 11 remaining domains (health, self-esteem, goals and values, finances, work, recreation, learning, creativity, social/community action, romantic relationship, and friends). In a separate sample of 381 individuals recruited on an urban university campus, the full version of the QOLI was given. Scores were calculated for the full and shortened version of the questionnaire, and these were correlated at .94, suggesting that scores from the version used in the current study can be seen as reliable estimates of full measure scores for this measure. Residualized gain scores were calculated by regressing post-treatment scores on pre-treatment scores.
Portions of this paper were presented at the annual meeting of the Association for Behavioral and Cognitive Therapies, Orlando, FL, November 2008. The authors thank Dave Barlow, Tim Brown, Bonnie Brown and the staff at the Center for Anxiety and Related Disorders for their support of this research. We thank our therapists, Laura Allen, Jenn Block Lerner, Laura Campbell-Sills, Gabrielle Liverant, David Moskovitch, Sue Raffa, LaTanya Rucker Kristi Salters-Pedneault, Yonit Schorr, Jill Stoddard, and Matt Tull, as well as our clients, for sharing their experience and their wisdom with us. Finally, we also thank Laura Allen for her exceptional management of the project and Heidi Barrett-Model, Shannon Erisman, Mike Treanor, and Matt Tull for their invaluable assistance with data management.
Contributor Information
Sarah A. Hayes, University of Massachusetts Boston and Boston University
Susan M. Orsillo, Suffolk University and Boston University
Lizabeth Roemer, University of Massachusetts Boston.
References
- American Psychiatric Association. The diagnostic and statistical manual of mental disorders. 4th edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Borkovec TD, Alcaine OM, Behar E. Avoidance theory of worry and generalized anxiety disorder. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized anxiety disorders: Advances in research and practice. New York: Guilford; 2004. pp. 77–108. [Google Scholar]
- Borkovec TD, Newman MG, Lytle R, Pincus A. A component analysis of cognitive behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70:288–298. [PubMed] [Google Scholar]
- Brown TA, Antony MM, Barlow DH. Psychometric properties of the Penn State Worry Questionnaire in clinical anxiety. Behaviour Research and Therapy. 1992;30:33–37. doi: 10.1016/0005-7967(92)90093-v. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH, Liebowitz MR. The empirical basis of generalized anxiety disorder. American Journal of Psychiatry. 1994;151:1272–1280. doi: 10.1176/ajp.151.9.1272. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences (2nd ed.) Lawrence Erlbaum Associates; 1988. [Google Scholar]
- DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV. Albany NY: Graywind Publications; 1994. [Google Scholar]
- Francis DJ, Fletcher JM, Steubing KK, Davidson KC, Thompson NM. Analysis of change: Modeling individual growth. Journal of Consulting and Clinical Psychology. 1991;59:27–37. doi: 10.1037//0022-006x.59.1.27. [DOI] [PubMed] [Google Scholar]
- Frisch MB, Cornwell J, Villanueva M, Retzlaff PJ. Clinical validation of the Quality of Life Inventory: A measure of life satisfaction of use in treatment planning and outcome assessment. Psychological Assessment. 1992;4:92–101. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York: Guilford Press; 1999. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG, Bissett RT, Pistorello J, Toarmino D, Polusny MA, Dykstra TA, Batten SV, Bergan J, Stewart SH, Zvolensky MJ, Eifert GH, Bond FW, Forsyth JP, Karekla M, McCurry SM. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54:553–578. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VM, Strosahl K. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology. 1996;64:1152–1168. doi: 10.1037//0022-006x.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Turk CL, Mennin DS. Generalized anxiety disorder: Advances in research and practice. New York: Guilford Press; 2004. [Google Scholar]
- Henning ER, Turk CL, Mennin DA, Fresco DM, Heimberg RG. Impairment and quality of life in individuals with generalized anxiety disorder. Depression and Anxiety. 2007;24:342–349. doi: 10.1002/da.20249. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Walters EE, Wittchen H-U. Epidemiology. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized anxiety disorder: Advances in research and practice. New York: Guilford; 2004. pp. 29–50. [Google Scholar]
- Lee J, Orsillo SM, Roemer L, Allen L. The Role of experiential avoidance in generalized anxiety disorder. Manuscript under review. 2009 [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford; 1993. [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney: The Psychology Foundation of Australia; 1995. [Google Scholar]
- Mennin DS, Heimberg RG, Turk CL, Fresco DM. Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behaviour Research and Therapy. 2005;43:1281–1310. doi: 10.1016/j.brat.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Michelson SE, Lee JK, Orsillo SM, Roemer L. The relationship between values in symptom severity, experiential avoidance and quality of life in generalized anxiety disorder; Poster presented at the 42nd Annual Association for Behavioral and Cognitive Therapies Conference; Orlando, Florida. 2008. Nov, [Google Scholar]
- Molina S, Borkovec TD. The Penn State Worry Questionnaire: Psychometric properties and associated characteristics. In: Davey GCL, Tallis F, editors. Worrying: Perspectives on theory, assessment and treatment. Oxford, England: John Wiley & Sons; 1994. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. Los Angeles, CA: Muthén & Muthén; 2006. [Google Scholar]
- Preacher KJ, Wichman AL, MacCallum RC, Briggs NE. Latent growth curve modeling. Los Angeles, CA: Sage Publications; 2008. [Google Scholar]
- Roemer L, Orsillo SM. An acceptance based behavior therapy for generalized anxiety disorder. In: Orsillo SM, Roemer L, editors. Acceptance and mindfulness-based approaches to anxiety: Conceptualization and treatment. New York: Springer; 2005. pp. 213–240. [Google Scholar]
- Roemer L, Orsillo SM. An open trial of an acceptance-based behavior therapy for generalized anxiety disorder. Behavior Therapy. 2007;38:72–85. doi: 10.1016/j.beth.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Roemer L, Orsillo SM. Mindfulness- and acceptance-based behavioral therapies in practice. New York: Guilford Press; 2009. [Google Scholar]
- Roemer L, Orsillo SM, Salters-Pedneault K. Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: Evaluation in a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2008;76:1083–1089. doi: 10.1037/a0012720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salters-Pedneault K, Tull MT, Roemer L. The role of avoidance of emotional material in the anxiety disorders. Applied and Preventive Psychology. 2004;11:95–114. [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford; 2002. [Google Scholar]
- Treanor M, Erisman SM, Salters-Pedneault K, Roemer L, Orsillo SM. An acceptance-based behavioral therapy for GAD: Effects on outcomes from three theoretical models. Submitted for publication. 2009 doi: 10.1002/da.20766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters AM, Craske MG. Generalized anxiety disorder. In: Antony MM, Ledley DR, Heimberg RG, editors. Improving outcomes and preventing relapse in cognitive behavioral therapy. New York: Guilford; 2005. [Google Scholar]
- Wells A, Carter K. Preliminary tests of a cognitive model of generalized anxiety disorder. Behaviour Research and Therapy. 1999;37:585–594. doi: 10.1016/s0005-7967(98)00156-9. [DOI] [PubMed] [Google Scholar]
- Wilson KG, Murrell AR. Values work in acceptance and commitment therapy: setting a course for behavioral treatment. In: Hayes SC, Follette VM, Linehan MM, editors. Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. New York: Guilford; 2004. pp. 120–151. [Google Scholar]
- Wilson KG, Sandoz EK, Kitchens J, Roberts M. The Valued Living Questionnaire: Defining and measuring valued action within a behavioral framework. Manuscript submitted for publication. 2009 [Google Scholar]
- Yonkers KA, Warshaw MG, Massion AO, Keller MB. Phenomenology and course of generalized anxiety disorder. British Journal of Psychiatry. 1996;168:308–313. doi: 10.1192/bjp.168.3.308. [DOI] [PubMed] [Google Scholar]