Abstract
Background/Aims
The risk of venous thromboembolism (VTE), which encompasses deep vein thrombosis and pulmonary embolism (PE), increases in patients with cancer. Anticancer treatment is also associated with an increased risk for VTE. We conducted this study to investigate the clinical characteristics of patients with cancer and PE related to anticancer treatment in a tertiary care hospital in Korea.
Methods
We retrospectively reviewed the clinical data of patients with an underlying malignancy who were diagnosed with PE by chest computed tomography (CT) with or without lower extremity CT angiography between January 2006 and December 2007 at Seoul National University Hospital.
Results
Overall, 95 patients with malignancies among 168 with PE were analyzed. The median age was 64 years. The median time interval from the malignancy diagnosis to the PE diagnosis was 5.5 months. Lung cancer was the most common malignancy (23.0%), followed by pancreatobiliary cancer, stomach cancer, gynecological cancer, breast cancer, and hepatocellular carcinoma. Platinum-containing and pyrimidine analog-containing chemotherapeutic regimens were common.
Conclusions
PE was diagnosed within 1 year after the cancer diagnosis in almost 70% of patients. Lung cancer was the most common underlying malignancy.
Keywords: Drug therapy, Neoplasms, Pulmonary embolism, Radiotherapy
INTRODUCTION
The risk of venous thromboembolism (VTE) now well recognized to increase in patients with cancer. Silverstein et al. [1] reported that the annual incidence of a first episode of deep vein thrombosis (DVT) or pulmonary embolism (PE) in the general population is 117 in 100,000. Cancer alone was associated with a 4.1-fold risk for thrombosis. More recently, Blom et al. [2] reported that the overall risk for venous thrombosis increases 7-fold in patients with a malignancy.
The relationship between VTE and anticancer treatment has been investigated. In a retrospective study in patients who underwent chemotherapy, the annual rate of thromboembolic complications arising within the first 3 months was 11% [3]. In a prospective observational study among 3,003 patients treated with at least one cycle of chemotherapy, VTE occurred in 58 (1.93%) over a median follow-up of 2.4 months [4].
Although DVT and PE encompass one disease entity, important differences exist. The major adverse outcome of DVT alone is the development of postphlebitic syndrome. However, PE can be fatal or cause chronic thromboembolic pulmonary hypertension.
We conducted this study in a single tertiary referral hospital in Korea to investigate the clinical characteristics of cancer patients with PE.
METHODS
Study population
We screened 168 patients who were diagnosed with PE by chest computed tomography (CT) with or without lower extremity CT angiography at Seoul National University Hospital between January 2006 and December 2007. The malignant diseases were diagnosed according to current standards using histological and/or cytological reports. This study was approved by the institutional review board of Seoul National University Hospital, which waived the informed consent requirement for individual patients due to the retrospective nature of the study.
Data collection
Other than patient age and gender, Eastern Cooperative Oncology Group (ECOG) performance scores and comorbidities such as diabetes mellitus, hypertension, congestive heart failure, coronary artery disease, cerebrovascular disease, and chronic renal disease were reviewed. The kind of malignant disease and the various chemotherapeutic agents administered to each patient were recorded. We reviewed the exact dates that chemotherapy was started and stopped. The exact dates the radiotherapy was started and stopped were also recorded for patients given radiotherapy. The exact date of any kind of surgery was also recorded.
We considered that PE diagnosed during the treatment or within 13 weeks after the last treatment was related to treatment, analogous to postsurgical patients [3].
RESULTS
Of the 168 patients who were diagnosed with PE, 99 had an underlying malignancy. Of the 99 patients, four were excluded because no evidence of disease was observed over the 5 years after anticancer treatments had been finished.
Patient characteristics
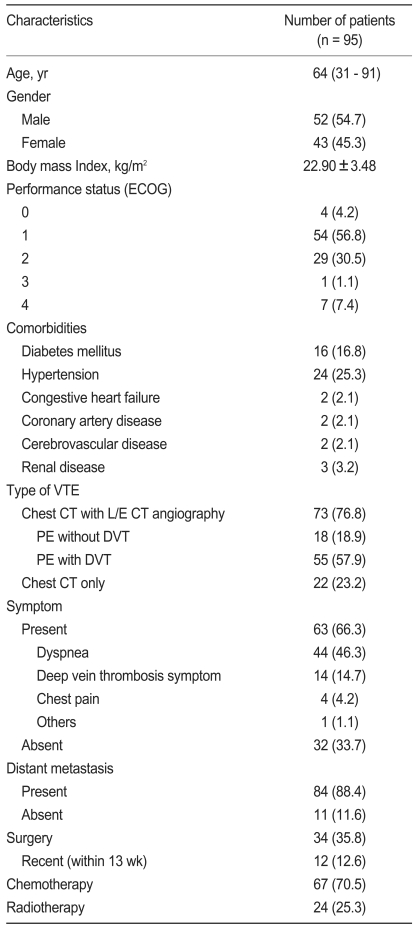
The clinical characteristics of the 95 patients are shown in Table 1. The median age was 64 years. More than half of the patients were in ECOG performance status 0-1, and only 8 patients (8.5%) were in a poor performance status [3,4]. More than 25% of the patients had hypertension and 63 (66.3%) had symptoms associated with PE or DVT. Dyspnea was the most frequent symptom. Eighty-four patients (88.4%) had distant cancer metastasis at the time of PE diagnosis.
Table 1.
Study population characteristics
Values are presented as median (range) or number (%) unless otherwise indicated.
ECOG, Eastern Cooperative Oncology Group; VTE, venous thromboembolism; CT, computed tomography; L/E, lower extremity; PE, pulmonary embolism; DVT, deep vein thrombosis.
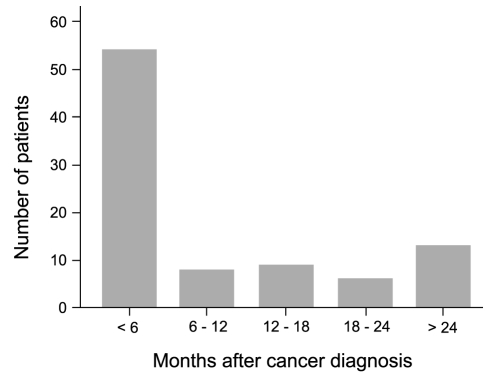
Eleven patients (11.6%) were diagnosed with malignancy after the PE diagnosis. The median time interval from malignancy diagnosis to PE diagnosis was 5.5 months, and PE was diagnosed within 1 year after the malignancy diagnosis in almost 70% of the patients (Fig. 1).
Figure 1.
Interval between cancer and pulmonary embolism diagnoses. A venous thromboembolism was diagnosed within 1 yr after detecting a malignancy in almost 70% of the patients.
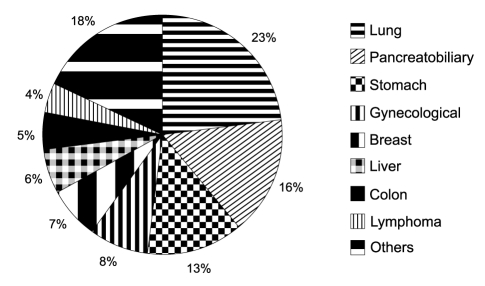
Lung cancer was the most common malignancy (23.0%), followed by pancreatobiliary cancer, stomach cancer, gynecological cancer, breast cancer, and hepatocellular carcinoma (Fig. 2).
Figure 2.
Types of malignancy. Lung cancer was the most common malignancy, followed by pancreatobiliary cancer and stomach cancer.
Chemotherapy / Radiotherapy
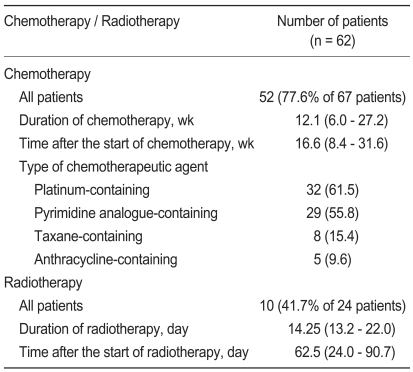
Sixty-seven (70.5%) patients were treated with chemotherapy. Of these, PE was diagnosed during the treatment or within 13 weeks after chemotherapy in 52. The median duration for chemotherapeutic treatment was 12.1 weeks (interquartile range [IQR], 6.0 to 27.2). A platinum-containing regimen (55.8%) was the most common, followed by a pyrimidine analog-containing regimen and a taxane-containing regimen (Table 2).
Table 2.
Details of chemotherapy/radiotherapy related to pulmonary embolism
Values are presented number (%) or median (IQR) unless otherwise indicated.
IQR, interquartile range.
Twenty-five patients were treated with radiotherapy. Of the 25, PE was diagnosed either during the treatment or within 13 weeks after radiotherapy (10 patients). The median radiotherapy duration was 14.3 days (IQR, 13.2 to 22.0; Table 2).
DISCUSSION
The risk for VTE increases in patients with cancer. In the current study, the median time interval from cancer diagnosis to PE diagnosis was 5.5 months, and 70% of the patients were diagnosed with PE within 1 year after the cancer diagnosis. Almost 90% of the patients had metastatic disease. In a previous cohort study including 235,149 patients with cancer [5], the incidence of a thromboembolic event among patients with either metastatic- or regional-stage disease was highest in the first few months after diagnosis, and the incidence decreased over time for most cancers. In a case-control study of patients with acute VTE [2], the incidence of VTE was highest in the first 6 months after the cancer diagnosis. In another lung cancer cohort study [6], the VTE incidence rate was highest in the first 6 months after the cancer diagnosis, averaging 7.2 VTE events/100 patient-years. Patients with distant metastasis are at an increased risk for VTE [2,5-9], and the current study findings are consistent with these previous studies. As noted previously [5], the biological aggressiveness of cancer may be the principal risk factor associated with the development of thromboembolism. However, considering that 52 among 95 patients were diagnosed with PE during or within 13 weeks after chemotherapy in the current study, the possibility also exists that anticancer treatment in the months immediately following the cancer diagnosis may have contributed to the high incidence of thromboembolism.
Among autopsy-proven patients with PE, 83% had DVT in the legs [10]. That is, only 17% of the patients had PE without DVT. In this study, among the 73 patients who were evaluated with both chest CT and lower extremity CT angiography, 18 (24.7%) had no evidence of DVT; however, a direct comparison with previous autopsy data is irrelevant. In a recent Japanese prospective study, patients with PE alone represented 40% of all patients with PE [11]. Due to the retrospective nature of the present study, lower-extremity CT may have been performed on patients who were more likely to have DVT.
In the present study, 11 patients (11.6%) were diagnosed with malignancy after the PE diagnosis. On the basis of results from cohort studies and clinical trials, up to 10% of patients presenting with idiopathic VTE are subsequently diagnosed with an underlying and previously undiagnosed malignancy [12-16]. Although extensive screening of patients with VTE may result in the early identification of hidden cancer, whether the prognosis of the malignancy can be favorably influenced is unknown [17,18].
Gastrointestinal cancer, lung cancer, and hematological cancer are associated with a very high risk for venous thrombosis [2]. In another prospective observational study [4], the highest rates of VTE occurred in patients with upper gastrointestinal cancers (including gastric, pancreatic, and hepatobiliary) and lung cancer. Similarly, lung cancer (23.0%) and upper gastrointestinal cancer (28.0%) were common in the present study. However, this finding may have resulted from the high prevalence of these kinds of cancers, as stomach, lung, colon, liver, and the pancreatobiliary system are the most common sites of malignancy in Korea [19]. As described in Table 2, pancreatobiliary cancers were the second most common underlying malignancy, although pancreatobiliary cancers account for only 5.5% of cancers in Korea [19]. Frequent use of pyrimidine analogs (especially gemcitabine) in these cancers might be one of the possible explanations. In this study, 10 of the 15 patients with pancreatobiliary cancer were treated with a chemotherapeutic regimen containing pyrimidine analogs. The advanced stage of pancreatobiliary cancer diagnosis in most of the patients may be another cause for the relatively high PE incidence.
Chemotherapeutic agents associated with a high risk for VTE are not well known. In a previous prospective study [4], the particular type of chemotherapy regimen was not significantly associated with VTE. Pyrimidine analog-containing and platinum-containing regimens were common in this study (55.8%); however, these agents are widely used as first-line chemotherapy in lung and gastrointestinal cancer, which are the most common cancers in Korea. These kinds of chemotherapeutic agents cannot be concluded to be associated with an increased risk for VTE.
However, in an experimental model, the endothelium of fluorouracil-treated rabbits was badly damaged, leading to intima disruption and denudation of underlying structures with accompanying platelet accumulation and fibrin deposition [20]. A significant increase in fibrinopeptide A levels in patients treated with fluorouracil has been reported [21,22]. Furthermore, VTE was most frequent in patients treated with five daily bolus injections of fluorouracil-leucovorin every months (6 [15%] of these 41 patients had VTE; 95% confidence interval, 6 to 29) [3]. Pyrimidine analogs may be more associated with an increased risk for VTE than other kinds of chemotherapeutic drugs. Further investigation is needed.
Data about the relationship between VTE and radiotherapy are lacking. In a record linkage study, the risk of VTE did not increase for patients who underwent radiotherapy [23]. Further study is needed to investigate the role of radiotherapy in the development of VTE.
This study has several limitations. Because of its retrospective nature, probable or possible patients with PE who did not have chest CT were not been included, and cases of PE diagnosed by lung perfusion/ventilation or pulmonary angiogram were also not included.
In summary, the median time interval from cancer to PE diagnosis was 5.5 months, and almost 90% of the patients had metastatic disease. Lung cancer was the most common underlying malignancy.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Silverstein MD, Heit JA, Mohr DN, Petterson TM, O'Fallon WM, Melton LJ., 3rd Trends in the incidence of deep vein thrombosis and pulmonary embolism: a 25-year population-based study. Arch Intern Med. 1998;158:585–593. doi: 10.1001/archinte.158.6.585. [DOI] [PubMed] [Google Scholar]
- 2.Blom JW, Doggen CJ, Osanto S, Rosendaal FR. Malignancies, prothrombotic mutations, and the risk of venous thrombosis. JAMA. 2005;293:715–722. doi: 10.1001/jama.293.6.715. [DOI] [PubMed] [Google Scholar]
- 3.Otten HM, Mathijssen J, ten Cate H, et al. Symptomatic venous thromboembolism in cancer patients treated with chemotherapy: an underestimated phenomenon. Arch Intern Med. 2004;164:190–194. doi: 10.1001/archinte.164.2.190. [DOI] [PubMed] [Google Scholar]
- 4.Khorana AA, Francis CW, Culakova E, Lyman GH. Risk factors for chemotherapy-associated venous thromboembolism in a prospective observational study. Cancer. 2005;104:2822–2829. doi: 10.1002/cncr.21496. [DOI] [PubMed] [Google Scholar]
- 5.Chew HK, Wun T, Harvey D, Zhou H, White RH. Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch Intern Med. 2006;166:458–464. doi: 10.1001/archinte.166.4.458. [DOI] [PubMed] [Google Scholar]
- 6.Chew HK, Davies AM, Wun T, Harvey D, Zhou H, White RH. The incidence of venous thromboembolism among patients with primary lung cancer. J Thromb Haemost. 2008;6:601–608. doi: 10.1111/j.1538-7836.2008.02908.x. [DOI] [PubMed] [Google Scholar]
- 7.Alcalay A, Wun T, Khatri V, et al. Venous thromboembolism in patients with colorectal cancer: incidence and effect on survival. J Clin Oncol. 2006;24:1112–1118. doi: 10.1200/JCO.2005.04.2150. [DOI] [PubMed] [Google Scholar]
- 8.Blom JW, Osanto S, Rosendaal FR. The risk of a venous thrombotic event in lung cancer patients: higher risk for adenocarcinoma than squamous cell carcinoma. J Thromb Haemost. 2004;2:1760–1765. doi: 10.1111/j.1538-7836.2004.00928.x. [DOI] [PubMed] [Google Scholar]
- 9.Levitan N, Dowlati A, Remick SC, et al. Rates of initial and recurrent thromboembolic disease among patients with malignancy versus those without malignancy: risk analysis using medicare claims data. Medicine (Baltimore) 1999;78:285–291. doi: 10.1097/00005792-199909000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Sandler DA, Martin JF. Autopsy proven pulmonary embolism in hospital patients: are we detecting enough deep vein thrombosis? J R Soc Med. 1989;82:203–205. doi: 10.1177/014107688908200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sakuma M, Nakamura M, Yamada N, et al. Venous thromboembolism: deep vein thrombosis with pulmonary embolism, deep vein thrombosis alone, and pulmonary embolism alone. Circ J. 2009;73:305–309. doi: 10.1253/circj.cj-08-0372. [DOI] [PubMed] [Google Scholar]
- 12.Prandoni P, Lensing AW, Buller HR, et al. Deep-vein thrombosis and the incidence of subsequent symptomatic cancer. N Engl J Med. 1992;327:1128–1133. doi: 10.1056/NEJM199210153271604. [DOI] [PubMed] [Google Scholar]
- 13.Aderka D, Brown A, Zelikovski A, Pinkhas J. Idiopathic deep vein thrombosis in an apparently healthy patient as a premonitory sign of occult cancer. Cancer. 1986;57:1846–1849. doi: 10.1002/1097-0142(19860501)57:9<1846::aid-cncr2820570925>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 14.Monreal M, Fernandez-Llamazares J, Perandreu J, Urrutia A, Sahuquillo JC, Contel E. Occult cancer in patients with venous thromboembolism: which patients, which cancers. Thromb Haemost. 1997;78:1316–1318. [PubMed] [Google Scholar]
- 15.Rajan R, Levine M, Gent M, et al. The occurrence of subsequent malignancy in patients presenting with deep vein thrombosis: results from a historical cohort study. Thromb Haemost. 1998;79:19–22. [PubMed] [Google Scholar]
- 16.Schulman S, Lindmarker P. Incidence of cancer after prophylaxis with warfarin against recurrent venous thromboembolism: Duration of Anticoagulation Trial. N Engl J Med. 2000;342:1953–1958. doi: 10.1056/NEJM200006293422604. [DOI] [PubMed] [Google Scholar]
- 17.Monreal M, Trujillo-Santos J. Screening for occult cancer in patients with acute venous thromboembolism. Curr Opin Pulm Med. 2007;13:368–371. doi: 10.1097/MCP.0b013e3282058b6f. [DOI] [PubMed] [Google Scholar]
- 18.Fennerty A. Venous thromboembolic disease and cancer. Postgrad Med J. 2006;82:642–648. doi: 10.1136/pgmj.2006.046987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Cancer Center. National Cancer Control Program [Internet] Goyang (KR): National Cancer Center; c2000-2009. [cited 2009 Sep 15]. Available from: http://ncc.re.kr/index.jsp. [Google Scholar]
- 20.Kuzel T, Esparaz B, Green D, Kies M. Thrombogenicity of intravenous 5-fluorouracil alone or in combination with cisplatin. Cancer. 1990;65:885–889. doi: 10.1002/1097-0142(19900215)65:4<885::aid-cncr2820650410>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 21.Kinhult S, Albertsson M, Eskilsson J, Cwikiel M. Antithrombotic treatment in protection against thrombogenic effects of 5-fluorouracil on vascular endothelium: a scanning microscopy evaluation. Scanning. 2001;23:1–8. doi: 10.1002/sca.4950230101. [DOI] [PubMed] [Google Scholar]
- 22.Edwards RL, Klaus M, Matthews E, McCullen C, Bona RD, Rickles FR. Heparin abolishes the chemotherapy-induced increase in plasma fibrinopeptide A levels. Am J Med. 1990;89:25–28. doi: 10.1016/0002-9343(90)90093-s. [DOI] [PubMed] [Google Scholar]
- 23.Blom JW, Vanderschoot JP, Oostindier MJ, Osanto S, van der Meer FJ, Rosendaal FR. Incidence of venous thrombosis in a large cohort of 66,329 cancer patients: results of a record linkage study. J Thromb Haemost. 2006;4:529–535. doi: 10.1111/j.1538-7836.2006.01804.x. [DOI] [PubMed] [Google Scholar]