Abstract
Rationale
The long-rejected construct of food addiction is undergoing re-examination.
Objectives
. To evaluate whether a novel carbohydrate food shows abuse potential for rigorously defined carbohydrate cravers, as evidenced by selective self-administration and mood enhancement during double-blind discrimination testing.
Methods
Discrete trials choice testing was performed with 61 overweight (BMI m=27.64, SD=2.59) women (ages 18–45; 19.70% African American) whose diet records showed >4 weekly afternoon/evening emotional eating episodes confined to snacks with carbohydrate:protein ≥ 6:1. After being induced into a sad mood, participants were exposed, double-blind and in counterbalanced order, to taste-matched carbohydrate and protein beverages. They were asked to choose and self-administer the drink that made them feel better.
Results
Women overwhelmingly chose the carbohydrate beverage, even though blinded. Mixed-effects regression modeling, controlling for beverage order, revealed greater liking and greater reduction in dysphoria following the carbohydrate beverage compared to the protein beverage, but no differential effect on vigor.
Conclusion
For women who crave them, carbohydrates appear to display abuse potential, plausibly contributing to overconsumption and overweight.
Keywords: food addiction, addictive behavior, substance-related disorder, carbohydrate craving, food preferences, appetite, eating, eating disorder, women’s health, abuse potential, abuse liability
Introduction
The proposition that foods may have addictive properties has been largely rejected until recently (Haddock and Dill 1999; Hammersley and Reid 1997; Rogers and Smit 2000; Wilson 1999). Criticisms of the food addiction concept were that; 1) alternative psychosocial explanations are plausible (Rogers and Smit 2000); 2) except for the role of striatal dopamine, underlying central nervous system mechanisms are unknown (Hammersley and Reid 1997); 3) effects of substances are often subtle (Haddock and Dill 1999), and 4) evidence of tolerance and withdrawal is lacking (Wilson 1999). As it gradually became recognized that those criticisms applied equally well to many forms of drug addiction, the nature of addiction was reconceptualized (Gifford & Humphreys, 2007; Koob, 2007; Leshner, 1997). Likewise, food addiction is undergoing re-examination as a scientific construct (Avena et al. in press)
Change in prevailing thought about addictions has been an international occurrence. In the past decade in the United States, the National Institutes of Drug Abuse (NIDA), Society of Addiction Medicine (ASAM), and the American Psychiatric Association’s Diagnostic and Statistical Manual (DSM-IV-TR; APA 2000) all re-defined addiction’s core feature as uncontrollable drug seeking and use despite adverse consequences (Holden 2001). Likewise, the World Health Organization’s (WHO) Expert Committee on Drug Dependence and the International Classification of Disease, 10th edition (ICD-10) now emphasize compulsive drug seeking and use as the core feature of addiction, with or without physical signs of dependence (World Health Organization, 1992, 2003). As clinical diagnosis has changed in a manner more open to “behavioral addictions,” evidence suggesting a central nervous system basis for food addiction is accumulating rapidly.
Palatable food and drugs appear to activate the same mesolimbic dopamine reward system circuitry in the brain (Berthoud 2002; Kelley and Berridge 2002). Current thinking is that the manner in which this neural network becomes “hijacked” by exogenous drugs of abuse may resemble and shed light on how the same circuitry can be hijacked by strongly craved foods (Volkow and Wise 2005).
Animal models of binge eating (Corwin and Hajnal 2005) show commonalities with both behavioral and brain substrates of human overeating. Schedule-induced intermittent, excessive intake of sugar has been shown to produce bingeing, withdrawal, and cross-sensitization in rats. In addition to sharing behavioral commonalities with other addictions, neural adaptations including changes in dopamine and opioid receptor binding, and dopamine and acetylcholine release in nucleus accumbens suggest that rats can become sugar dependent (Avena et al. in press). In obese humans, functional magnetic resonance imaging (fMRI) has shown reduced striatal dopamine D2 receptors, like that seen in drug-addicted humans (Wang et al. 2004). It remains unclear whether D2 receptor paucity is causal or consequential in relation to obesity, but one interpretation is that it leads the obese to self-administer excess food rewards to overcome D2 subsensitivity.
Despite increasingly compelling evidence of palatable food dependence in rodents, parallel findings for humans are lacking. We designed the current study to test whether abuse potential for craved foods could be demonstrated in humans under controlled laboratory conditions used to test the abuse potential of drugs (Epstein et al. 2006; Lile and Nader 2003).
We chose to study carbohydrate craving because, arguably, it has the largest empirical evidence base of the putative food addictions (Arbisi et al. 1996; van der Ster Wallin et al. 1994; Spring et al. 1987). Carbohydrate craving has been characterized as an overwhelming drive to compulsively and selectively overconsume carbohydrate-rich, protein-poor foods in response to dysphoric mood, resulting in overweight (Heller and Heller 1993; Wurtman and Wurtman 1995).
The original hypothesis put forward to explain carbohydrate craving posits a phasic (afternoon or evening) functional deficiency in brain serotonin that results in dysphoric mood (Wurtman and Wurtman 1995). Carbohydrate cravers are thought to learn, through experience, that negative mood can be alleviated by self-administering snacks that are high in carbohydrate and low in protein. Such snacks cause an insulin-mediated rise in the ratio of plasma tryptophan to large neutral amino acids, which leads to increased brain tryptophan influx and serotonin synthesis (Fernstrom and Wurtman 1971; Fernstrom and Wurtman 1972), presumably correcting serotonergic hypofunction and dispelling negative mood. Because serotonin neurons inhibit the mesolimbic dopamine pathway, transient serotonergic hypofunction potentiates the dopamine release produced by rewarding substances, likely including palatable foods (Alex and Pehek 2007; Koob and LeMoal 2001; Rothman and Baumann 2006).
There has been some laboratory evidence of acute mood changes after eating carbohydrate (Lieberman et al. 1986; Rosenthal et al. 1989; Spring et al. 1982–1983; Sayegh et al. 1995) with a time course paralleling the predicted change in the plasma tryptophan ratio (Spring et al. 1986; Spring et al. 1989). However, the evidence has not been wholly convincing because of several methodological weaknesses and a few failures to replicate (Toornvliet et al. 1997). Chief methodological flaws have been that most studies lacked a clear operational definition of carbohydrate craving, tested response to foods that were high in fat as well as carbohydrate, offered high-carbohydrate, low-protein choices that were more appealing than the high-protein alternatives, and failed to control for cognitive expectational effects (Fernstrom 1988; Fernstrom 1992; Reid et al. 2007). In addition to implementing a rigorous operational definition of carbohydrate craving, the current research design corrected previous methodological flaws by asking participants to choose between unfamiliar fat-free, carbohydrate-rich, protein-poor, equi-palatable, equi-volumetric protein-rich beverages under double-blind conditions.
The hypothesis was that for women who crave them, carbohydrates would show abuse potential. Specifically, under double-blind conditions, when induced into a negative mood, carbohydrate cravers were expected to: 1) choose to administer a novel carbohydrate beverage over a taste-matched beverage with balanced macronutrient content, 2) report enhanced positive mood and reduced negative mood after drinking the carbohydrate–rich beverage, and 3) possibly, like the carbohydrate beverage more (finding it more palatable). An exploratory aim was to examine evidence suggestive of neuroadaptation: i.e., sensitization or tolerance to the effects of the novel carbohydrate beverage among those who repeatedly chose it.
Materials and Method
Overview
The study was designed to compare the effects of a pure carbohydrate beverage versus a taste-matched beverage balancing protein and carbohydrate on beverage choice, liking and mood in self-reported, overweight, female carbohydrate cravers. The institutional review boards of the University of Illinois – Chicago and Northwestern University approved the protocol. The study was performed in accordance with ethical standards laid down in the 1964 Declaration of Helsinki. All participants gave their informed consent prior to inclusion in the study.
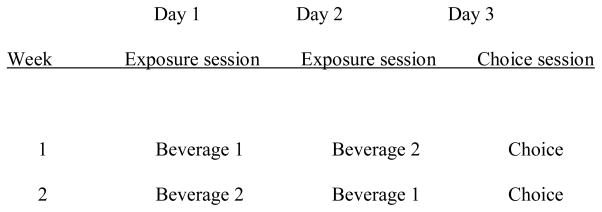
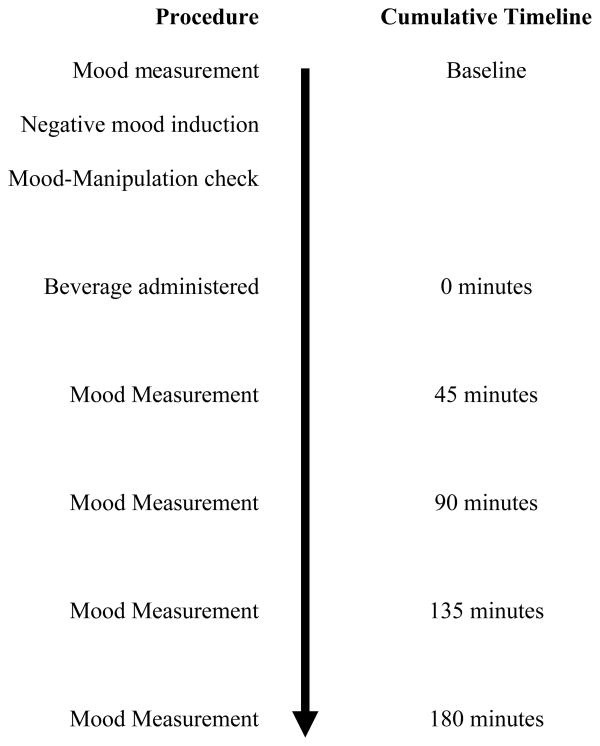
The study time line is shown in Figure 1. After undergoing eligibility screening, participants completed two three-day sets of discrimination trials on consecutive weeks. Each individual laboratory session began with a negative mood induction, after which the participant consumed either a carbohydrate-rich or a balanced beverage under double-blind conditions. The negative mood induction protocol simulated food self-administration to try to dispel a negative mood. The time line of events in each laboratory session is shown in Figure 2.
Figure 1.
Discrete Trials Choice Protocol Timeline.
Figure 2.
Laboratory Session Timeline.
Participants were exposed to each beverage during the initial two days of each three-day discrimination trial sequence. After mood induction, the participant was given one of the beverages in a red-topped cup on one day and the other beverage in a blue-topped cup on the other day. The final day of each three-day sequence served as a testing session: On test days, following the mood induction, the participant was asked to choose and self-administer the beverage that had most improved her mood. Beverage assignment was counterbalanced across cup color, and the order of beverage presentation was counterbalanced across participants. For any given participant, the same beverage appeared in the same cup color across both weeks.
A within subjects design was utilized to test for effects of the repeated measures factors: beverage (carbohydrate versus balanced), week (first versus second), and, for mood assessments, time (baseline, post mood induction and 45, 90, 135 and 180 minutes after beverage consumption). Beverage order (carbohydrate first versus balanced first) was a between subjects factor. Dependent variables were choice of beverage, beverage liking, and beverage effects on positive and negative mood.
Participants
Participants were 61 women from the Chicago metropolitan area who responded to flyers, newspaper advertisements and listserv e-mails offering a $350 honorarium for a paid research study of overweight carbohydrate cravers. Eligibility criteria required participants to be female, between the ages of 20–45 years, and overweight or mildly obese (BMI >24 and <34). The mean age of study participants was 28.02 years (SD = 7.11) and mean BMI was 27.64 (SD = 2.59). The ethnic composition of the sample was 50.80% Caucasian, 19.70% African-American, 13.10% Hispanic, 6.60% Asian/Pacific Islander, 4.90% Multi-Ethnic, 3.3% other; 1.6% were missing ethnicity data.
Carbohydrate Craver Criteria
A comprehensive, rigorous operational definition of carbohydrate craving has not previously been put forth (Fernstrom 1988; Reid et al. 2007). Some prior studies stated entry criteria requiring that carbohydrate snacks comprise at least 30% of total daily caloric intake and more than 40% of daily carbohydrate intake (Wurtman et al. 1993). However, the rationale for those caloric requirements was unclear, and the criteria left unspecified other key features used clinically to identify carbohydrate cravers (Heller and Heller 1993; Wurtman and Wurtman 1995). One important feature is that snacking occurs systematically in the late afternoon or evening hours when phasic dysphoric moods tend to occur. A second is that the craver experiences mood regulatory effects of snacking: dysphoric mood triggers the urge to snack and/or carbohydrate snacking dispels negative mood. A third is that preferred carbohydrate snack foods are very low in protein. That criterion is particularly important because the degree to which a high-carbohydrate food produces mood changes has been shown to be systematically related to its protein content. Foods that are almost purely carbohydrate, containing ≤6% protein, are observed to have the greatest effect on mood (Spring et al. 1989).
To qualify as a carbohydrate craver for the present study, participants needed to describe experiencing an afternoon or evening urge to consume carbohydrate-rich, protein-poor snacks between meals at least four times per week. They also needed to report that on most occasions a negative mood state either preceded carbohydrate snacking or was dispelled by such snacking. This snacking pattern was corroborated by seven-day dietary intake recording. The carbohydrate to protein ratio of the carbohydrate snacks must have been ≥ 6:1, indicating that the chosen snacks supplied insufficient protein to prevent a carbohydrate-induced, insulin-mediated rise the tryptophan ratio (Yokogoshi and Wurtman, 1986). Finally, food diaries, modified to also record mood (i.e., depression, anxiety, anger, boredom) on 7-point scales before and after snacking, needed to demonstrate that at least 50% of afternoon/evening carbohydrate snack occasions either were preceded by dysphoric mood above the scale midpoint or improved negative mood. Eligible carbohydrate snacks were either sweet, savory or bland and either high, medium or low in fat. That is, study participants exhibited a particular macronutrient preference (high carbohydrate, low protein), independent of the taste and independent of the fat content of snacks.
Enrollment Criteria
Study candidates were excluded if they were diabetic, pregnant or lactating, allergic to study beverage ingredients, menopausal, taking antidepressants or other medications affecting mood and/or appetite, very afraid of needles or blood, or currently anorexic or bulimic as assessed via a structured diagnostic interview. Also ineligible were women who were currently dieting, had lost >5% of their total body weight in the past 6 months, smoked > 5 cigarettes per day, had an active drug and/or alcohol problem within the past year, or experienced irregular periods or severe premenstrual disturbances.
Eight percent of study applicants met enrollment criteria. Candidates with current or past major depression, dysthymia, seasonal affective disorder, premenstrual distress, generalized anxiety, or binge-eating were allowed to enroll because those conditions have been reported by overweight carbohydrate cravers. In the final sample, 6.60% of participants met criteria for current major depressive disorder and 26.20% had a history of major depression. The participants’ average Beck Depression Inventory (Beck et al, 1961) score was 8.87 (SD=8.59).
Procedure
Screening Sessions
Study candidates were seen for two screening sessions. During the first screening, they underwent an informed consent process, were weighed with a balance-beam scale, and measured for height and waist/hip ratio. Candidates were interviewed using the Structured Clinical Interview for Diagnosis (SCID-IV; Spitzer et al. 1994), and completed the Beck Depression Inventory (Beck et al. 1961), as well as questionnaires about demographics and medical history.
Candidates also recorded six sad autobiographical memories for use in negative mood inductions (cf., Hernandez et al. 2003). They rated each memory on a 1 to 10 point scale to indicate how sad or upset it made them feel, and how vivid the memory was. Only memories rated ≥6 on both negative mood intensity and vividness were used in laboratory sessions.
Participants were also trained to complete 7-day dietary records. They learned to weigh and measure food portions and to estimate portion sizes when servings could not be measured. Candidates were provided with a food scale, measuring cups, and instruction manual to facilitate accurate recording. To minimize effects of premenstrual hormonal and affective changes on eating, they recorded dietary intake and rated mood before and after eating between days 7 and 21 of the menstrual cycle.
Participants returned the diet records at the second screening session, at which time a phlebotomist drew a blood sample to be assayed for fasting glucose and insulin. Candidates were excluded if the eating pattern shown by their diet records failed to meet entry criteria or if fasting glucose level was ≥ 120 mg/dl, indicating diabetes
Laboratory Sessions
During exposure sessions, participants were given either the carbohydrate or balanced beverage. During choice sessions, they were asked to choose and consume the beverage that most improved their mood during the previous two sessions. Sessions were scheduled between days 7 and 21 of participants’ menstrual cycle, lasted 3.5 hours, and occurred in the afternoon or early evening (at whichever time participant engaged in carbohydrate snacking). To standardize pre-session nutritional status, participants ate a pre-packaged meal three hours prior to the session. The meal was comparable to participant’s usual foods and average lunchtime calorie intake, as derived from her 7-day dietary records.
Upon arrival at the laboratory, adherence with pre-session eating instructions was verified and baseline mood was assessed with the ‘right now’ version of the Profile of Mood States (POMS; McNair et al. 1992). The POMS yields factor-analytically derived scores on vigor-activity, as well as on tension-anxiety, depression-dejection, and anger-hostility, which comprise a composite dysphoria score. Dysphoria has a possible score range from 0 to 144 and showed high internal consistency (Cronbach’s alpha from .92 to .97 across time points), as did vigor (alpha from .86 to .92).
After baseline mood measurement, participants listened via headphones to a recording of Prokofiev’s Russia under the Mongolian Yoke, which has been shown in prior studies to invoke dysphoric mood (Clark and Teasdale 1985; Martin 1990; Hernandez et al. 2003). They were cued to recall one of the sad memories they provided during screening, and asked to remember it for six minutes while listening to the music.
At the end of the music, participants completed the POMS as a manipulation check. Then they consumed one of the beverages in its entirety within 10 minutes following the manipulation check, They rated how much they liked the beverage on a scale of 1–10 (1=tastes bad, 10=tastes good).
Then they engaged in a neutral sedentary activity of their own choosing (e.g. reading), and the POMS was re-administered 45-, 90-, 135-, and 180-minutes after beverage consumption. A positive mood induction (recall a happy memory while listening to Vivaldi’s Four Seasons) was administered at the end of the session to any participant who experienced lingering negative mood.
Beverages
The balanced, protein-rich beverages used in the study had a ratio of carbohydrate:protein less than 6:1. Aminoforce, used for the first 11 participants, contained 23% (22g) protein, 77% (75g) carbohydrates, and 0% fat. After Aminoforce was discontinued by the manufacturer, a comparable beverage, Mass Recovery was used for the remaining 50 participants. Mass Recovery contained 37% (35g) protein (whey), 63% (60g) carbohydrates (maltodextrin, cane syrup, food starch), and 0% fat, and supplied 380 calories. The carbohydrate-rich, protein-poor beverage, Carboforce, was comprised of 100% (109g) carbohydrate (maltodextrin, dextrose, high maltose rice syrup, palantinose, rice oligodextrine, d-ribose), 0% protein, and 0% fat, and supplied 440 calories. Both beverages contained 18 fluid ounces, supplied 400 kcal, and contained the sweetener, sucralose.
Taste-testing panels of 6–10 normal (non-carbohyrate-craving) adults were utilized to equate the carbohydrate and balanced beverages on palatability. Aminoforce was chosen from a selection of alternative balanced sports beverages because taste testers found it as palatable as Carboforce. However, palability ratings from the first six study participants indicated that Carboforce was favored over Aminoforce. Consequently, a new taste testing panel was convened to re-equate the beverages. The second panel found the beverages equipalatable when two additions were made: ½ teaspoon of baking soda was added to Carboforce to thicken its consistency and give the beverage a slightly starchy taste; and ¼ teaspoon of stevia (a noncaloric sweetener) was added to Aminoforce to give the beverage a sweeter taste. After the manufacturer discontinued Aminoforce, a taste panel chose Mass Recovery, as the replacement beverage most similar in taste to Carboforce. In lieu of baking soda, ¼ teaspoon of arrowroot starch was added to Carboforce to equate the two beverages’ consistency, and these beverages were used for the remaining participants. None of these changes significantly altered the taste panel’s overall palatability ratings of the carbohydrate or the balanced beverages.
Data Analysis
Responsiveness to the negative mood induction was operationalized as >4 point increase in POMS dysphoria on at least two of the four laboratory exposure sessions. Four participants failed to meet this criterion; their data were excluded from the analyses. Three participants were missing a 90-minute post-beverage POMS. Only for the analyses that used mood change from manipulation check to 90 minutes post-beverage as a covariate, mean imputation was used to create difference scores for these three missing values.
To determine whether participants chose the carbohydrate beverage more often than the balanced beverage, a logistic regression model for correlated dichotomous responses was estimated by the generalized estimating equations (GEE) method (Liang and Zeger 1986) as implemented in SAS PROC GENMOD. This model characterized the repeated dichotomous classifications (choice week 1 and choice week 2) in terms of choice during week 1 and time-related change in choice from week 1 to week 2 (examining the linear trend over time). Beverage order was included as a covariate. Time and beverage order were centered so that the intercept would reflect the probability of choosing the carbohydrate beverage for the average levels of these covariates.
Mixed-effects regression modeling implemented via SAS PROC MIXED was used to analyze dysphoria and vigor separately across the four time points following the mood induction (45 minutes, 90 minutes, 135 minutes and 180 minutes). The model included random subject effects to account for correlation inherent in the longitudinal data (Verbecke and Molenberghs 2000). Model covariates were: baseline mood (dysphoria or vigor depending on the dependent variable), manipulation check mood (i.e., immediately following mood induction), beverage order (carbohydrate first or balanced first) and week (1 or 2). Both time and time squared terms were included in all analyses to allow for linear and quadratic trends. Specific tests were conducted to determine the effect of beverage (carbohydrate rich versus balanced) on mood at the first post-induction time period (an effect of beverage at 45 minutes) and time-related changes in mood (beverage by time interaction). To create the most parsimonious model, if the latter terms were determined to be non-significant, the model was refit, excluding the non-significant beverage by time interaction terms, in a backwards manner.
Having a majority of carbohydrate cravers choose the carbohydrate beverage at both choice opportunities enabled us to examine these individuals’ data for evidence of sensitization or tolerance to the effects of a newly encountered carbohydrate beverage on liking, vigor and dysphoria over the course of four exposures (1= week 1 administered carbohydrate, 2=week 1 chose carbohydrate, 3=week 2 administered carbohydrate, and 4=week 2 chose carbohydrate). Mixed-effects regression was used to model the effect of time (4 exposures) on liking for the new carbohydrate beverage and on the change that the beverage engendered in vigor and dysphoria from manipulation check to 90 minutes. Beverage order was again included as a covariate. Sensitization would be evidenced by finding that the carbohydrate beverage showed increased liking, increased enhancement of vigor, and decreased reduction of dysphoria over time. Tolerance would be evidenced by finding decreased liking, decreased enhancement of vigor and decreased dysphoria reduction for the carbohydrate beverage over time.
Results
Preliminary Analyses
Manipulation check
The mean increase in POMS dysphoria following mood induction was 18.20 (SD=17.32), indicating that, on average, mood induction was successful. There was no change over the six protocol days in the overall magnitude of dysphoria induced by the mood induction (multivariate F(5,46) = 0.85, p = .52.). The mean increase in POMS dysphoria due to the mood induction varied from 17.77 to 21.15 across the days, with no discernable time trend.
Beverage Liking
Despite recurrent success at matching the palatability of the carbohydrate and balanced beverages for panels of normal adult taste testers, carbohydrate cravers rated the carbohydrate beverage slightly but significantly more palatable (m = 5.90; sd = 2.19) than the balanced beverage (m = 3.68; sd = 2.36), controlling for beverage order [t (170) = 10.02, p < .0001]. Therefore, beverage liking ratings were included as a time-varying covariate in all analyses. For the GEE analyses, beverage liking was centered to be consistent with the other covariates included in the model.
Primary Analyses
Beverage Choice
The analysis of beverage choice revealed a highly significant preference favoring the carbohydrate beverage [z= 3.95, p < .0001, table 1]. The time effect was nonsignificant [z= 0.07, p = .95]: the probability of choosing the carbohydrate beverage was .93 during week 1 and .95 during week 2. 53% of participants chose the carbohydrate beverage on both test days; 33% chose carbohydrate on one day; 9% never chose carbohydrate. Beverage order did not significantly predict choice [z= −0.27, p = .79], but liking ratings for the carbohydrate and balanced beverages both significantly predicted choice [z= 2.76, p = .01 and z= −2.79, p = .01, respectively].
Table 1.
Predictors of Beverage Choice determined by Generalized Estimating Equations.
| Variable | Regression Coefficient | Standard Error | z |
|---|---|---|---|
| Covariates | |||
| Beverage order | −0.13 | .46 | −0.27 |
| Liking-Carbohydrate | 0.38 | .14 | 2.76** |
| Liking-Balanced | −0.33 | .12 | −2.79** |
| Time effects | |||
| Week | 0.01 | .22 | 0.07 |
| Beverage effects | |||
| Intercept | 1.32 | .33 | 3.95**** |
p<.01,
p<.0001
Note. Beverage order reflects the random order in which participants received the two beverages, where −1=carbohydrate beverage presented first and 1=balanced beverage presented first; Beverage choice is coded 0=chose carbohydrate beverage, 1=chose balanced beverage
Dysphoria
The longitudinal analysis of dysphoria showed, as predicted, significant interactions involving beverage by linear time [t (789) = 2.17, p = .03] and beverage by quadratic time [t (789) = −2.12, p = .04] (see Table 2). Figure 3 displays mean dysphoria over time for the carbohydrate and balanced beverages, adjusted for dysphoria at baseline and at manipulation check. Dysphoria declined sharply for the first two hours after the carbohydrate beverage before rising again three hours after intake, whereas dysphoria remained relatively steady after the balanced beverage before finally declining. Neither beverage order [t (789) = −0.95, p = .34], nor beverage liking [t (789) = 0.37, p = .72] significantly influenced dysphoria.
Table 2.
Predictors of Dysphoria from Time 45 minutes through Time 180 minutes, determined by Mixed Effects Regression.
| Variable | Regression Coefficient | Standard Error | t |
|---|---|---|---|
| Covariates | |||
| Baseline dysphoria | .24 | .02 | 10.81*** |
| MC dysphoria | .05 | .02 | 3.33*** |
| Beverage order | −1.24 | 1.30 | −.95 |
| Week | .23 | .48 | .48 |
| Liking | .04 | .11 | .37 |
| Time effects | |||
| Time | −2.10 | .75 | −2.80** |
| (Time)2 | .54 | .24 | 2.31* |
| Beverage effects | |||
| Beverage | −1.14 | .76 | −1.51 |
| Beverage × week | 1.37 | .67 | 2.05* |
| Beverage × time | 2.25 | 1.04 | 2.17* |
| Beverage × time2 | −.70 | .33 | −2.12* |
p < .05,
p < .01,
p < .001
Note. MC = Manipulation Check, Liking is time varying by day; Beverage order reflects the random order in which participants received the two beverages where 0=carbohydrate beverage presented first and 1=balanced beverage presented first; Beverage is coded 0=carbohydrate, 1=balanced; for all t-statistics df = 789, except for time where df = 56.
Figure 3.
POMS Dysphoria* over Time as a Function of Beverage
*adjusted for baseline and manipulation check dysphoria
Vigor
Contrary to the hypothesis, the longitudinal analysis of vigor showed no main effect of beverage [t (790) = 0.91, p = .36] and no beverage by linear time [t (790) = −1.57, p = .12] interaction. Thus, neither beverage significantly altered vigor (see Table 3).
Table 3.
Predictorms of Vigor from time 45 minutes through time 180 minutes, determined by Mixed Effects Regression.
| Variable | Regression Coefficient | Standard Error | t |
|---|---|---|---|
| Covariates | |||
| Baseline vigor | .13 | .03 | 4.61*** |
| MC vigor | .28 | .05 | 6.11*** |
| Beverage order | −.21 | .819 | −.26 |
| Week | −1.18 | .37 | −3.23** |
| Liking | .04 | .07 | .60 |
| Time effects | |||
| Time | −1.01 | .39 | −2.59* |
| (Time)2 | .37 | .11 | 3.35** |
| Time × week | .50 | .20 | 2.57* |
| Beverage effects | |||
| Beverage | .36 | .40 | .91 |
| Beverage × time | −.31 | .20 | −1.57 |
p < .05,
p < .01,
p < .001
Note. MC = Manipulation Check, Liking is time varying by day; Beverage order reflects the random order in which participants received the two beverages where 0=carbohydrate beverage presented first and 1=balanced beverage presented first; Beverage is coded 0=carbohydrate, 1=balanced; for all t-statistics df = 790, except for time where df = 56.
Beverage Choice
We used mixed-effects regression to reexamine whether the preference for carbohydrate remained significant after controlling for beverage effects on liking and dysphoria. Since the major beneficial carbohydrate effect on dysphoria occurred between the manipulation check and 90 minutes post-beverage, we calculated a difference score using these 2 timepoints. Beverage order was again included as a covariate, but did not significantly predict choice [z= −.10, p = .92]. The analysis of beverage choice again revealed a significant carbohydrate preference [z= 4.04, p < .0001, table 4]. Again, liking for both the carbohydrate and balanced beverages significantly predicted choice [z= 2.72, p = .01 and z= −2.78, p = .01, respectively]. However, neither dysphoria change after the carbohydrate beverage [z= −0.90, p = .37] nor dysphoria change after the balanced beverage [z= 1.29, p = .20] significantly predicted beverage choice.
Table 4.
Predictors of Beverage Choice determined by Generalized Estimating Equations.
| Variable | Regression Coefficient | Standard Error | z |
|---|---|---|---|
| Covariates | |||
| Beverage order | −0.19 | .47 | −0.39 |
| Liking-Carbohydrate | 0.40 | .15 | 2.73** |
| Liking-Balanced | −0.34 | .13 | −2.75** |
| Dysphoria:Carbohydrate. (mc-90 min.) | −0.01 | .02 | −0.90 |
| Dysphoria: Balanced (mc-90 min.) | 0.02 | .02 | 1.29 |
| Time effects | |||
| Week | 0.09 | .23 | 0.37 |
| Beverage effects | |||
| Intercept | 1.42 | .35 | 4.04*** |
p<.01,
p<.0001
Note. MC = Manipulation Check. Beverage order reflects the random order in which participants received the two beverages where −1=carbohydrate beverage presented first and 1=balanced beverage presented first; Beverage choice is coded 0=chose balanced beverage, 1=chose carbohydrate beverage.
Secondary Analyses
Sensitization and Tolerance
Mixed-effects regression modeling of the 33 participants who chose carbohydrate on both choice days showed that liking for the carbohydrate beverage increased over time [t (98) = 1.98, p = .05], indicating sensitization. In addition to beverage order, the analyses of vigor and dysphoria controlled for liking. Vigor did not change over the four carbohydrate administrations [t (95) = −1.29, p = .20]. However, the magnitude of reduction in dysphoria produced by the carbohydrate beverage decreased significantly over time [t (95) = −2.82, p = .01], suggesting tolerance to this mood effect of the carbohydrate beverage.
Discussion
In this study, a novel carbohydrate snack displayed indications of abuse potential for rigorously defined carbohydrate cravers, when tested under laboratory conditions used to evaluate abuse liability for drugs,. After being induced into a negative mood, simulating the conditions under which they ordinarily snack on carbohydrates, the carbohydrate cravers we studied chose overwhelmingly to self-administer an unfamiliar carbohydrate-rich, protein-poor beverage in preference to a protein-rich beverage that non-carbohydrate craving taste-testing panels had rated equally palatable. Carbohydrate cravers also showed greater reduction in negative mood after drinking the pure carbohydrate beverage compared to the beverage containing both protein and carbohydrate, and they liked the carbohydrate beverage better (i.e., found it more palatable). The two beverages had no differential effect on positive mood. On three out of four indicators (behavioral choice, self-rated liking, and anti-negative mood effect, but not pro-positive mood effect), therefore, carbohydrate snacks appeared to showed evidence of abuse potential for overweight women who crave them, plausibly contributing to overconsumption and weight gain.
Consistent with contemporary best practice in abuse liability assessment, we applied a multi-method approach that integrates different indicators of abuse potential (Griffiths, Bigelow, & Ator, 2003). Results indicated that the different abuse potential indices were related but non-redundant, as has been observed previously for addictive drugs (Johanson & Uhlenhuth, 1980). The carbohydrate craver’s greater liking for the carbohydrate beverage was not associated with the greater reduction in negative mood produced by that beverage. Nor did the mood effects or the liking for carbohydrate fully explain the behavioral preference for carbohydrate. Interestingly, even though we asked participants to choose and self-administer the beverage that most improved their mood, the effect of the beverages on mood had no significant influence on beverage choice. In contrast, liking ratings for both beverages were associated with beverage preference, even though they did not fully explain the variance in beverage choice.
Positive reinforcing effects of carbohydrate snacks have been found also in other studies of carbohydrate craving populations that used different methodologies and did not use a negative mood induction. For example, women in nicotine withdrawal, a state also associated with carbohydrate craving, overeating and weight gain, worked harder under increasing response requirements, for carbohydrate snacks, relative to money (Spring et al, 2003). Similarly, carbohydrates induced positive mood in several prior studies of different carbohydrate craving populations (Lieberman et al, 1986; Sayegh et al, 1995; Wurtman et al, 1989; Rosenthal et al, 1989), whereas in non-carbohydrate cravers, carbohydrates induced fatigue (Spring et al, 1982, 1989).
A noteworthy finding in the present study was that, among those who consistently preferred carbohydrate, the behavioral response to the novel carbohydrate beverage changed over time in a manner suggestive of neuroadaptation. Interestingly, liking for the carbohydrate beverage grew (sensitized) over time, whereas the beverage’s impact on dispelling negative mood decreased (showed tolerance) over repeated exposures. Gradual recruitment to a pattern of increased liking and self-administration of snacks that progressively lose their potency to dispel (self-medicate) bad moods seems a likely pathway to binge eating. Investigation is warranted to determine whether the observed growing subsensitivity to dysphoria alleviating properties of a food corresponds temporally to the diminution in striatal dopamine D2 receptors that has been observed in substance abuse and obesity (Wang et al. 2004).
We operationalized carbohydrate craving as snacking on high carbohydrate, low protein foods in relation to negative moods at certain characteristic times of day (late afternoon, evening). The carbohydrate snacks that the women routinely consumed were either sweet, savory or bland and either high, medium or low in fat. That is, we studied women who exhibited a particular macronutrient craving (high carbohydrate, low protein), independent of taste and independent of fat content. Study participants ate several different kinds of carbohydrate snacks: sweet, high fat foods (eg., chocolates or cake); sweet, low fat foods (e.g., gummy bears), savory, high fat foods (e.g., potato chips); savory, low fat foods (e.g., pretzels); and bland foods with preparation methods or condiments that made them either high or low in fat (e.g., pasta, bread, potatoes). Given such diversity, it is noteworthy that the pure carbohydrate test beverage lacking any protein was resoundingly preferred by carbohydrate cravers under double-blind conditions, even though both beverages were novel, sweet, lacked any fat, and were liked equally well by non-carbohydrate cravers.
The present study design improved upon prior carbohydrate craving experiments (Wurtman et al. 1981; Wurtman et al. 1987; Wurtman et al. 1993) by using stringent definitional criteria that required a demonstrable pattern on more days than not of snacking on high-carbohydrate, low-protein foods at characteristic afternoon or evening times of day and either preceded by negative mood or followed by improved mood. Additionally, we employed double-blind testing, measured choice in addition to self-reported mood, controlled for intake preceding the session, and assessed self-administration against the relevant dysphoric affective state.
Our sample was highly selected in that participants were required to meet stringent operational criteria for carbohydrate craving. However, participants with psychopathologic comorbidities were included, since those often accompany the carbohydrate craving syndrome. We have no reason to expect results to differ among males or more obese carbohydrate cravers. Females were studied in this initial research because they are believed to comprise the majority of individuals who report carbohydrate craving (Wurtman and Wurtman 1995). Overweight or mildly obese individuals were studied rather than heavier individuals in order to standardize the dose of carbohydrate needed to trigger an insulin response. A sweet rather than a non-sweet carbohydrate snack was studied because we previously found that sweet snacks show heightened reward value among women who exhibit dysphoric mood and overeating (Spring et al. 2003). Liquid rather than solid snacks were studied because liquids permitted greater ease of blinding and expectancy control. Also, the use of beverages allowed for a more efficient protocol, because the time course of plasma tryptophan ratio changes after consuming a liquid is more rapid than that after a solid food.
In designing the experiment, differences in test beverage palatability were regarded as error variance that needed to be controlled. Encapsulating the two beverages to eliminate any difference in taste was not feasible for reasons of practicality and ecological validity. Consequently, we adopted the alternative approach of having adults who did not self-identify as carbohydrate cravers match the beverages as closely as possible on palatability. Interestingly, we observed on repeated occasions that beverages whose palatability was equated carefully for panels of non-carbohydrate craving adults were unmatched for the carbohydrate craving sample. Because the carbohydrate cravers’ difference in liking for the two beverages persisted at the end of the study, liking was treated as a covariate in the analyses. However, the data also reminded us that rated liking for a drug is a well-validated predictor of abuse liability (Epstein et al. 2006). Thus trying to equate liking/palatability for two beverages, one of which has abuse potential for a population and the other of which does not, may prove to be challenging if not impossible. Liking/perceived palatability may be an inherent, integral constituent of a food’s abuse potential.
The reliability and generalizability of the present findings remains to be determined. The results warrant replication, as well as testing to see whether the findings extend to solid foods and non-sweet carbohydrates. Also needed is an examination of whether carbohydrate foods possess apparent abuse potential when tested outside of a context that involves negative mood induction. It is unknown whether self-administration of carbohydrate foods by carbohydrate cravers occurs primarily under conditions of negative affect, or whether preferential self-administration also occurs under conditions of neutral or positive mood. Indeed, elsewhere we have demonstrated that drug effects are integrally related to the affective context in which the substance is self-administered (Spring et al, in press). Another important question is whether the current results have alternative explanations that might have greater scientific and heuristic utility. The study’s most important contribution may be to encourage re-examination of whether a meaningful distinction can be drawn between behavioral addictions and drug addictions, and what methodologies might genuinely differentiate between the two.
These findings should not be interpreted to suggest that obesity is generally attributable to food addiction, or that carbohydrate-rich, protein-poor snacks exhibit abuse potential for the average eater. We think it more plausible that gene by environment interactions convey differential susceptibility to food preferences and cravings involving different nutrients, tastes, textures, etc. (Perusse and Bouchard, 2000). Obesity is likely a heterogeneous syndrome comprised of a number of different behavioral phenotypes. Most likely, different gene by environment interactions give rise to individual differences in susceptibility to specific food cravings and preferences. Although here we have objectively demonstrated the existence of carbohydrate preference, other phenotypes such as fat preference and sweet preference are likely important contributors to obesity. Also important are the other parts of the interaction between genes, environment, and behavior that gives rise to unhealthy eating. As noted, affective triggers, including stress, may play a pivotal role, as may traits like self-control or its converse, impulsivity.
Overconsumption of palatable, energy dense foods has adverse health consequences as severe as those of most drugs of abuse. Early theories of carbohydrate addiction posited that intake of carbohydrate-rich, tryptophan deficient foods corrects serotonergic hypofunction and dispels negative mood via an insulin-mediated rise in the brain tryptophan influx and serotonin synthesis (Fernstrom and Wurtman 1971; Fernstrom and Wurtman 1972). More recently, certain forms of compulsive, excessive food self-administration are being conceptualized as an addiction perpetuated by the rewarding properties of food (Lowe and Butryn 2007) and largely mediated by the mesolimbic dopamine system (Berthoud 2002; Kelley and Berridge 2002), a neural network that is “hijacked” by exogenous substances of abuse (Volkow and Wise 2005). Neither a serotonergic, dopaminergic or other neurobiological pathway for food addiction has been tested directly. The current findings indicate that for those who crave them, carbohydrate snacks display apparent abuse potential on indicators derived from a laboratory protocol that has been used to test the abuse liability of drugs. The possibility of food addiction may warrant reconsideration.
Acknowledgments
Supported by NIH grant HL63307 to Dr. Spring and by NIH grants P30 CA060553 and R25 CA100600. We express appreciation to Jillon Vander Wal and Andrea Kozak for helpful comments.
References
- Alex KD, Pehek EA. Pharmacologic mechanisms of serotonergic regulation of dopamine neurotransmission. Pharmacol Ther. 2007;113:296–320. doi: 10.1016/j.pharmthera.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Arbisi PA, Levine AS, Nerenberg J, Wolf J. Seasonal alteration in taste detection and recognition threshold in seasonal affective disorder: the proximate source of carbohydrate craving. Psychiatry Res. 1996;59:171–182. doi: 10.1016/0165-1781(95)02816-1. [DOI] [PubMed] [Google Scholar]
- Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. doi: 10.1016/j.neubiorev.2007.04.019. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Berthoud HR. Multiple neural systems controlling food intake and body weight. Neurosci and Biobehav Rev. 2002;26:393–428. doi: 10.1016/s0149-7634(02)00014-3. [DOI] [PubMed] [Google Scholar]
- Clark DM, Teasdale JD. Constraints on the effects of mood and memory. J Pers Soc Psychol. 1985;48:1595–1608. [Google Scholar]
- Corwin RL, Hajnal A. Too much of a good thing: neurobiology of non-homeostatic eating and drug abuse. Physiol Behav. 2005;86:5–8. doi: 10.1016/j.physbeh.2005.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit H, Griffiths RR. Testing the abuse liability of anxiolytic and hypnotic drugs in humans. 1990 doi: 10.1016/0376-8716(91)90054-3. [DOI] [PubMed] [Google Scholar]
- Epstein DH, Preston KL, Jasinski DR. Abuse liability, behavioral pharmacology, and physical dependence potential of opioids in humans and laboratory animals: lessons from Tramadol. Biol Psychol. 2006;73:90–99. doi: 10.1016/j.biopsycho.2006.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernstrom JD. Tryptophan, serotonin, and carbohydrate appetite: will the real carbohydrate-craver please stand up! J Nutr. 1988;118:1417–1419. doi: 10.1093/jn/118.11.1417. [DOI] [PubMed] [Google Scholar]
- Fernstrom JD. Brain serotonin, food intake regulation, and obesity. In: Bjorntorp P, Brodoff B, editors. Obesity. Lippincott; Philadelphia: 1992. pp. 411–423. [Google Scholar]
- Fernstrom JD, Wurtman RJ. Brain serotonin content: Increase following ingestion of carbohydrate diet. Science. 1971;174:1023–1025. doi: 10.1126/science.174.4013.1023. [DOI] [PubMed] [Google Scholar]
- Fernstrom JD, Wurtman RJ. Brain serotonin content: Physiological regulation by plasma neutral amino acids. Science. 1972;178:414–416. doi: 10.1126/science.178.4059.414. [DOI] [PubMed] [Google Scholar]
- Gifford E, Humphreys K. The psychological science of addiction. Addiction. 2007;102:352–361. doi: 10.1111/j.1360-0443.2006.01706.x. [DOI] [PubMed] [Google Scholar]
- Griffiths RR, Bigelow G, Ator N. Principles of initial experimental drug abuse liability assessment in humans. Drug and Alcohol Dependence. 2003 June 5;70(3):S41–S54. doi: 10.1016/s0376-8716(03)00098-x. Supplement 1. [DOI] [PubMed] [Google Scholar]
- Haddock CK, Dill PL. The effects of food on mood and behavior: implications for the addictions model of obesity and eating disorders. Drugs Society. 1999;15:17–47. [Google Scholar]
- Hammersley R, Reid M. Are simple carbohydrates physiologically addictive? Addict Res. 1997;5:145–160. [Google Scholar]
- Heller RF, Heller RF. The carbohydrate addict’s diet: the lifelong solution to yo-yo dieting. Signet; New York: 1993. [Google Scholar]
- Hernandez S, Vander Walo J, Spring B. Efficacy of a negative mood induction procedure across repeated administrations. J Psychopathol Behav. 2003;25:49–55. [Google Scholar]
- Holden C. ‘Behavioral’ addictions: do they exist? Science. 2001;294:980–982. doi: 10.1126/science.294.5544.980. [DOI] [PubMed] [Google Scholar]
- Johanson CE, Uhlenhuth EH. Drug preference and mood in humans: d-amphetamine. Psychopharm. 1980;71:275–279. doi: 10.1007/BF00433062. [DOI] [PubMed] [Google Scholar]
- Kelley AE, Berridge KC. The neuroscience of natural rewards: relevance to addictive drugs. J Neurosci. 2002;22:3306–3311. doi: 10.1523/JNEUROSCI.22-09-03306.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF. The neurobiology of addiction: a neuroadaptational view relevant for diagnosis. Addiction. 2007;101(Suppl 1):23–30. doi: 10.1111/j.1360-0443.2006.01586.x. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacol. 2001;24:97–129. doi: 10.1016/S0893-133X(00)00195-0. [DOI] [PubMed] [Google Scholar]
- Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278(5335):45–48. doi: 10.1126/science.278.5335.45. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Lieberman HR, Wurtman JJ, Chew B. Changes in mood after carbohydrate consumption among obese individuals. Am J Clin Nutr. 1986;44:772–778. doi: 10.1093/ajcn/44.6.772. [DOI] [PubMed] [Google Scholar]
- Lile JA, Nader MA. The abuse liability and therapeutic potential of drugs evaluated for cocaine addiction as predicted by animal models. Current Neuropharmacology. 2003;1:21–46. [Google Scholar]
- Lowe MR, Butryn ML. Hedonic hunger: a new dimension of appetite? Physiol Behav. 2007;91:432–439. doi: 10.1016/j.physbeh.2007.04.006. [DOI] [PubMed] [Google Scholar]
- Martin M. On the induction of mood. Clin Psychol Rev. 1990;10:669–697. [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Manuel for the Profile of Mood States (POMS), Revised. San Diego, CA: Educational and Industrial Testing Service; 1992. [Google Scholar]
- Perusse L, Bouchard C. Gene-diet interactions in obesity. Am J Clin Nutr. 2000;72:1285S–1290S. doi: 10.1093/ajcn/72.5.1285s. [DOI] [PubMed] [Google Scholar]
- Reid M, Hammersley R, Hill AJ, Skidmore P. Long-term dietary compensation for added sugar: effects of supplementary sucrose drinks over a 4-week period. Br J Nutr. 2007;97:193–203. doi: 10.1017/S0007114507252705. [DOI] [PubMed] [Google Scholar]
- Rogers PJ, Smit HJ. Food craving and food “addiction:” A critical review of the evidence from a biopsychosocial perspective. Pharmacol Biochem Behav. 2000;66:3–14. doi: 10.1016/s0091-3057(00)00197-0. [DOI] [PubMed] [Google Scholar]
- Rosenthal NE, Genhart MJ, Caballero B, Jacobsen FM, Skwerer RG, Coursey RD, Rogers S, Spring B. Psychobiological effects of carbohydrate- and protein-rich meals in patients with seasonal affective disorder and normal controls. Biol Psychiatry. 1989;25:1029–1040. doi: 10.1016/0006-3223(89)90291-6. [DOI] [PubMed] [Google Scholar]
- Rothman RB, Baumann MH. Balance between dopamine and serotonin release modulates behavioral effects of amphetamine-type drugs. Ann N Y Acad Sci. 2006;1074:245–260. doi: 10.1196/annals.1369.064. [DOI] [PubMed] [Google Scholar]
- Sayegh R, Schiff I, Wurtman J, Spiers P, McDermott J, Wurtman R. The effect of a carbohydrate-rich beverage on mood, appetite, and cognitive function in women with pre-menstrual syndrome. Obstet Gynecol. 1995;86:520–528. doi: 10.1016/0029-7844(95)00246-n. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured Interview for DSM-IV (SCID-IV) New York State Psychiatric Institute, Columbia Presbyterian; New York: 1994. [Google Scholar]
- Spring B, Chiodo J, Bowen DJ. Carbohydrates, tryptophan and behavior: A methodological review. Psychol Bull. 1987;102:234–256. [PubMed] [Google Scholar]
- Spring B, Chiodo J, Harden M, Bourgeois MJ, Mason J, Lutherer L. Psychobiological effects of carbohydrates. J Clin Psychiatry. 1989;50(Suppl):27–33. [PubMed] [Google Scholar]
- Spring B, Lieberman HR, Swope G, Garfield GS. Effects of carbohydrates on mood and behavior. Nutr Rev. 1986;44(Suppl):51–60. doi: 10.1111/j.1753-4887.1986.tb07678.x. [DOI] [PubMed] [Google Scholar]
- Spring B, Maller O, Wurtman J, Digman L, Cozolino L. Effects of protein and carbohydrate meals on mood and performance: Interactions with sex and age. J Psychiatr Res. 1982–1983;17:155–167. doi: 10.1016/0022-3956(82)90017-6. [DOI] [PubMed] [Google Scholar]
- Spring B, Pagoto S, McChargue D, Hedeker D, Werth J. Altered reward value of carbohydrate snacks for female smokers withdrawn from nicotine. Pharmacol Biochem Behav. 2003;76:351–360. doi: 10.1016/j.pbb.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Spring B, Werth Cook J, Appelhans B, Maloney A, Richmond M, Vaughn J, Vanderveen J, Hedeker D. Nicotine Effects on Affective Response in Depression-Prone Smokers. Psychopharm. doi: 10.1007/s00213-007-0977-7. (in press) [DOI] [PubMed] [Google Scholar]
- Toornvliet AC, Pijl H, Tuinenburg JC, Elte-de Wever BM, Pieters MS, Frolich M, Onkenhout W, Meinders A. Psychological and metabolic responses of carbohydrate craving obese patients to carbohydrate, fat, and protein-rich meals. Int J Obes Metab Disorders. 1997;21:860–864. doi: 10.1038/sj.ijo.0800470. [DOI] [PubMed] [Google Scholar]
- van der Ster Wallin G, Norring C, Holmgren S. Binge eating versus nonpurged eating in bulimics: Is there a carbohydrate craving after all? Acta Psychiatr Scand. 1994;89:376–381. doi: 10.1111/j.1600-0447.1994.tb01532.x. [DOI] [PubMed] [Google Scholar]
- Verbecke G, Molenberghs G. Linear mixed models for longitudinal data. Springer; New York: 2000. [Google Scholar]
- Volkow ND, Wise RA. How can drug addiction help us understand obesity? Nat Neurosci. 2005;8:555–560. doi: 10.1038/nn1452. [DOI] [PubMed] [Google Scholar]
- Wang GJ, Volkow ND, Thanos PK, Fowler JS. Similarity between obesity and drug addiction as assessed by neurofunctional imaging: a concept review. J Addict Dis. 2004;23:39–53. doi: 10.1300/J069v23n03_04. [DOI] [PubMed] [Google Scholar]
- Wilson GT. Eating disorders and addiction. Drugs Society. 1999;15:87–101. [Google Scholar]
- World Health Organization. Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization; 1992. The ICD-10 Classification of Mental and Behavioural Disorders. [Google Scholar]
- World Health Organization. WHO Technical Report Series, No. 915. Geneva: World Health Organization; 2003. WHO Expert Committee on Drug Dependence – Thirty-third Report. [PubMed] [Google Scholar]
- Wurtman J, Brzezinski A, Wurtman R, La Ferre B. Effect of nutrient intake on premenstrual depression. Obstetrics & Gynecology. 1989;161:1228–1234. doi: 10.1016/0002-9378(89)90671-6. [DOI] [PubMed] [Google Scholar]
- Wurtman J, Wurtman R, Berry E, Gleason R, Goldberg H, McDermott J, Kahne M, Tsay R. Dexfenfluramine, fluoxetine, and weight loss among female carbohydrate cravers. Neuropsychopharmacology. 1993;9:201–210. doi: 10.1038/npp.1993.56. [DOI] [PubMed] [Google Scholar]
- Wurtman J, Wurtman R, Growdon J, Henry P, Lipscomb A, et al. Carbohydrate craving in obese people: Suppression by treatments affecting serotoninergic neurotransmission. Int J Eat Disord. 1981;1:12–15. [Google Scholar]
- Wurtman JJ, Wurtman RJ, Reynolds S, Tsay R, Chew B. D-fenfluramine suppresses snack intake among carbohydrate-cravers but not among non-carbohydrate-cravers. Int J Eat Disord. 1987;6:687–689. [Google Scholar]
- Wurtman RJ, Wurtman JJ. Brain serotonin, carbohydrate craving, obesity and depression. Obes Res. 1995;3(Suppl 4):477S–480S. doi: 10.1002/j.1550-8528.1995.tb00215.x. [DOI] [PubMed] [Google Scholar]
- Yokogoshi H, Wurtman RJ. Meal composition and plasma amino acid ratios: effect of various proteins or carbohydrates, and of various protein concentrations. Metabolism. 1986;35:837–842. doi: 10.1016/0026-0495(86)90225-8. [DOI] [PubMed] [Google Scholar]