Abstract
Background
Incarceration is associated with increased cardiovascular disease (CVD) mortality, but prospective studies exploring mechanisms of this association are lacking.
Methods
We examined the independent association of prior incarceration with incident hypertension, diabetes, and dyslipidemia using the Coronary Artery Risk Development In young Adults (CARDIA) study--a cohort of young adults aged 18–30 years at enrollment in 1985–86, balanced by sex, race (black and white), and education (high school education or less). We also examined the association of incarceration with left ventricular hypertrophy (LVH) on echocardiography and with barriers to healthcare access.
Results
Of 4350 participants, 288 (7%) reported previous incarceration. Incident hypertension in young adulthood was more common among former inmates (12% versus 7%; odds ratio (OR) 1.7, 95% CI 1.2, 2.6), and this association persisted after adjustment for smoking, alcohol and illicit drug use, and family income (adjusted OR (AOR) 1.6, 95% CI 1.0, 2.6). Incarceration was significantly associated with incident hypertension in those groups with the highest prevalence of prior incarceration - black men (AOR 1.9, 95% CI 1.1, 3.5) and less educated participants (AOR 4.0, 95% CI 1.0, 17.3). Former inmates were more likely to have LVH (AOR 2.7, 95% CI 0.9, 7.9) and to report barriers to healthcare (AOR 2.7, 95% CI 1.5, 5.2). Cholesterol levels and diabetes rates did not differ by history of incarceration.
Conclusions
Incarceration is associated with future hypertension and LVH among young adults. Identification and treatment of hypertension may be important in reducing CVD risk among formerly incarcerated individuals.
INTRODUCTION
Incarceration has become increasingly frequent in the lives of young adults. Between 1987 and 2007, the US prison population tripled, such that currently 1 in 30 men between the ages of 20 and 34 is behind bars and 1 in 9 black men in this age group is incarcerated.1 This rise in incarceration as a normative experience for young men and young black men in particular makes it especially important to understand the implications of incarceration on future health status.
While the health and healthcare of prisoners has received some attention, little is known about the health status of those with a history of incarceration. One large study of recently released prisoners from Washington State demonstrated an increased risk of death immediately following their release from prison.2 The second most common cause of death was from cardiovascular disease (CVD), although the mechanisms of this increased risk were not examined in this study.
Increases in cardiovascular risk factors associated with incarceration may explain part of the increased risk of heart disease in prisoners,3 but to date no prospective study has directly measured such risk factors in either current or former US inmates. The Coronary Artery Risk Development in Young Adults (CARDIA) cohort provides the unique opportunity to explore the development of cardiovascular risk in young adults with a history of incarceration. The objective of this manuscript is to examine prospectively whether a history of incarceration is associated with the development of cardiovascular risk factors, to explore possible mechanisms and outcomes of this association, and to examine access to healthcare among those with prior incarceration.
METHODS
Sample and Setting
The CARDIA study is a longitudinal investigation of CVD risk factors and sub-clinical coronary disease in a population of black and white men and women 18–30 years old at baseline in 1985–1986; it is described in detail in previous publications.4 At baseline, the study enrolled 5115 young adults, who were recruited from 4 US cities (Birmingham, Chicago, Minneapolis, and Oakland). The sampling strategy resulted in a cohort balanced by race (52% black, 48% white), sex (55% male, 45% female), age (45% 18–24 years, 55% 25–30 years) and education level (40% with ≤ 12 years, 60% > 12 years.) Subsequent re-examinations have taken place at years 2 (1987–8), 5 (1990–1), 7 (1992–3), 10 (1995–6), 15 (2000–1) and 20 (2005–6), with high retention rates (91% at year 2, 86% at year 5, 81% at year 7, 79% at year 10, 73% at year 15, and 69% at year 20.) Of the 5115 participants in CARDIA, only those who had complete baseline data and follow-up through the year 5 exam were included in the primary analysis (N=4350).
History of incarceration
To assess history of incarceration, participants at baseline (1985–86) and year 2 (1987–88) were asked this question: “During the past year did any of the following happen to you?” and “Went to jail” was one of the pre-specified responses. In year 2, participants could report any incarceration event occurring since the prior examination. Responses to these two items permitted us to develop an incarceration exposure variable reflecting any jail time during a three year period of young adulthood, extending from one year prior to study entry through the two years preceding the year 2 exam. Since most jail experiences occur during early adult years,1 this measure offers a strong indicator of incarceration in young adulthood.
Cardiovascular risk factors
CVD risk factors were measured at the year 5 exam (1990–91). Trained and certified technicians used a random zero sphygmomanometer to record participants’ blood pressure at year 5 exam and all subsequent CARDIA exams. Measurements of systolic and diastolic blood pressure were taken 3 times at 1-minute intervals. For the purposes of this analysis, we used an average of the second and third blood pressure measurement. Hypertension was defined by systolic blood pressure ≥140 mmHg, diastolic blood pressure ≥90 mmHg, or use of anti-hypertensive medication. Incident hypertension was defined as meeting these criteria by the year 5 exam in persons without hypertension at baseline. Diabetes was defined by use of anti-diabetic medication. Serum total cholesterol and high density lipoprotein (HDL) were measured, and low density lipoprotein (LDL) was calculated using the Friedewald equation.
Potential Confounders
Body mass index (BMI) and smoking history were measured and examined as potential confounders for the association between incarceration and cardiovascular risk factors. Participants’ weight was measured in light clothing using a standard balance beam scale, and height was measured to the nearest 0.5 cm using a wall-mounted stadiometer. BMI was calculated as the ratio of weight (kg) over height (m) squared. Use of cigarettes was ascertained with interviewer- administered questionnaire. For cigarette smoking, participants were categorized as current smokers if they had smoked more than 5 cigarettes per week for the past three months and former smokers if they had ever smoked.
Use of cocaine, amphetamines, and excessive alcohol were also ascertained with interviewer-administered questionnaires. For cocaine or amphetamine use, participants were categorized as current users if they had used in the past month, former users if they had ever used but not in the past month, or never users. For alcohol use, participants were categorized as excessive alcohol consumers based on the at-risk consensus thresholds of the National Institute on Alcohol Abuse and Alcoholism, which were met if a man consumed equal to or greater than 14 drinks per week and a woman more than seven drinks per week, where a drink was counted as 12 ounces of beer, five ounces of wine or 1-1/2 ounces of spirits.5
Socioeconomic status of each participant was approximated using a measure of family income at year 5. Participants were asked: Which of these categories best describes your total combined family income for the past 12 months? This should include income from all sources, wages, veteran’s benefits, help from relatives, rent from properties, and so on (before taxes). Those who responded that their family income was less than $ 24,999 were defined as meeting 200% of the federal poverty line and being of low socioeconomic status.6
Echocardiography Measures
During year 5, all CARDIA participants underwent 2-dimensional-guided M-mode echocardiography described previously.7 Left ventricular mass was measured in grams and indexed to body surface area measured as height in meters squared. We defined left ventricular hypertrophy as left ventricular mass index >90 gm/m2.
Healthcare access
To assess healthcare access barriers, participants were asked three questions: (1) In the past 2 years, have you always had health insurance or other coverage for medical care; (2) Do you have a usual source of care? By that we mean the place you go if you need a checkup or if you are ill; and (3) Was there anytime during the past 2 years when you did not seek medical care because it was too expensive or health insurance did not cover it? Negative answers to question 1 and 2 indicated an insurance barrier and regular care barrier, respectively. An affirmative answer to question 3 was considered an expense barrier.
Realizing that we did not have healthcare access data at or before year 7 (1992–3), we could not perform a formal mediation analysis to test whether healthcare access might explain any associations of incarceration with cardiovascular risk. Instead, we studied potential associations between a history of incarceration and subsequent barriers to healthcare access. If present, such associations might only intensify the increased cardiovascular risk of those with a history of incarceration.
Statistical Analysis
CARDIA participants with and without a history of incarceration in the three year exposure period captured by our data were first compared for baseline sociodemographic characteristics, cardiovascular risk factors, and potential explanatory risk factors of disease using t- and chi-squared tests as appropriate. The primary analyses examined the association of incarceration history in the first three years of CARDIA and CVD risk factors at the year 5 exam, as well as the incidence of these risk factors by year 5. We chose year 5 for an assessment of these outcomes because of the difficulty postulating mechanisms for the effect of incarceration further in the future.
We next examined the independent association between incarceration and the incidence of these risk factors using multivariable logistic regression and explored covariates of the associations using staged models, first accounting for demographics, clinical risk factors, and behavioral risk factors (illicit drug use and excessive alcohol consumption) and then adding a measure of socioeconomic status. P-values < 0.05 were considered statistically significant. Because those incarcerated were mostly male, black, and with limited education (and because these were sampling strata within the original CARDIA design), we repeated our analyses within subgroups defined by sex, race, and education, and tested for interactions between incarceration and these factors. Because of differential drop-out across these strata, we also ran models using inverse probability-of-censoring weights to reduce bias potentially resulting from differential dropout.8
In secondary analyses, we examined whether measures of left ventricular mass index and left ventricular hypertrophy differed by prior incarceration using Fisher exact, t- and chi-squared tests as appropriate and in multivariable logistic regression models. Finally, among persons with hypertension evident by year 5, we investigated the association between incarceration and a barrier to accessing healthcare in year 7 using multivariable logistic regression.
RESULTS
Of the 4350 participants included in this analysis, 288 (7%) reported having been incarcerated during the three year period of young adulthood captured in the first two surveys. Black men and less educated participants were most likely to have history of prior incarceration (Table 1). Within these subgroups, former inmates were more likely to report family earnings below 200% of the federal poverty line, smoking, illicit drug use, and excess alcohol consumption compared to those without incarceration history.
Table 1.
Sociodemographic and clinical characteristics of 4350 black and white men and women by history of incarceration before 1987
| Prior Incarceration | No Prior Incarceration | p-value | |
|---|---|---|---|
| N (%)* or Mean ± SD | |||
| All participants, N=4350 | 288 | 4062 | |
| Age, y | 24.0± 3.7 | 25.1± 3.6 | <0.001 |
| Income below 200% federal poverty line | 173 (60) | 1462 (36) | <0.001 |
| Body mass index (kg/m2) | 26 ± 5 | 26 ± 6 | 0.59 |
| Tobacco use (current or former) | 182 (63) | 1269 (31) | <0.001 |
| Cocaine use (current or former) | 153 (55) | 1386 (35) | <0.001 |
| Amphetamine use (current or former) | 86 (30) | 1030 (26) | 0.05 |
| Alcohol use (excessive) | 99 (34) | 549 (13) | <0.001 |
| Black Men, N=905 | 154 (53) | 751 (18) | |
| Age, y | 23.8± 0.3 | 24.4± 0.1 | 0.08 |
| Income below 200% federal poverty line | 104 (68) | 317 (43) | <0.001 |
| Body mass index (kg/m2) | 25.8± 0.4 | 26.6± 0.2 | 0.12 |
| Tobacco use (current or former) | 98 (64) | 288 (39) | <0.001 |
| Cocaine use (current or former) | 83 (55) | 224 (30) | <0.001 |
| Amphetamine use (current or former) | 33 (22) | 99 (13) | 0.008 |
| Alcohol use (excessive) | 67 (50) | 171 (28) | <0.001 |
| White Men, N=1054 | 62 (22) | 992 (24) | |
| Age, y | 24.2± 0.5 | 25.6± 0.1 | 0.002 |
| Income below 200% federal poverty line | 25 (40) | 263 (27) | 0.02 |
| Body mass index (kg/m2) | 25.1± 0.6 | 25.6± 0.1 | 0.37 |
| Tobacco use (current or former) | 39 (63) | 296 (30) | <0.001 |
| Cocaine use (current or former) | 39 (63) | 448 (45) | <0.001 |
| Amphetamine use (current or former) | 34 (55) | 377 (38) | 0.03 |
| Alcohol use (excessive) | 23 (40) | 210 (23) | 0.004 |
| Black Women, N=1214 | 49 (17) | 1165 (29) | |
| Age, y | 23.9± 0.5 | 24.5± 0.1 | 0.27 |
| Income below 200% federal poverty line | 32 (67) | 589 (51) | 0.03 |
| Body mass index (kg/m2) | 27.7± 1.1 | 28.1± 0.2 | 0.66 |
| Tobacco use (current or former) | 38 (78) | 388 (33) | <0.001 |
| Cocaine use (current or former) | 21 (44) | 238 (21) | <0.001 |
| Amphetamine use (current or former) | 6 (12) | 125 (11) | 0.74 |
| Alcohol use (excessive) | 8 (19) | 8 (1) | 0.03 |
| White Women, N=1177 | 23 (8) | 1154 (28) | |
| Age, y | 24.7± 0.8 | 25.6± 0.1 | 0.004 |
| Income below 200% federal poverty line | 12 (52) | 293 (25) | 0.45 |
| Body mass index (kg/m2) | 25.4± 1.0 | 24.3± 0.2 | 0.36 |
| Tobacco use (current or former) | 7 (30) | 297 (26) | 0.61 |
| Cocaine use (current or former) | 13 (57) | 472 (41) | 0.24 |
| Amphetamine use (current or former) | 13 (57) | 429 (38) | <0.001 |
| Alcohol use (excessive) | 1 (5) | 94 (9) | 0.63 |
| High school education or less, N=1640 | 182 (63) | 1458 (36) | |
| Age, y | 23.3± 0.3 | 24.1± 0.1 | 0.02 |
| Male | 144 (79) | 625 (43) | <0.001 |
| Black | 137 (75) | 913 (63) | 0.001 |
| Income below 200% federal poverty line | 121 (67) | 784 (54) | 0.001 |
| Body mass index (kg/m2) | 25.8± 0.4 | 26.8± 0.2 | 0.05 |
| Tobacco use (current or former) | 129 (71) | 660 (45) | <0.001 |
| Cocaine use (current or former) | 96 (54) | 477 (33) | <0.001 |
| Amphetamine use (current or former) | 49 (27) | 336 (23) | 0.29 |
| Alcohol use (excessive) | 72 (45) | 256 (22) | <0.001 |
| More than high school, N=2710 | 106 (37) | 2604 (64) | |
| Age, y | 25.1± 0.3 | 25.6± 0.1 | 0.11 |
| Male | 72 (68) | 1118 (43) | <0.001 |
| Black | 66 (13) | 1003 (39) | <0.001 |
| Income below 200% federal poverty line | 52 (49) | 678 (26) | <0.001 |
| Body mass index (kg/m2) | 26.3± 0.6 | 25.8± 0.1 | 0.37 |
| Tobacco use (current or former) | 53 (50) | 609 (23) | <0.001 |
| Cocaine use (current or former) | 60 (57) | 909 (35) | <0.001 |
| Amphetamine use (current or former) | 37 (35) | 694 (27) | 0.10 |
| Alcohol use (excessive) | 27 (30) | 293 (13) | <0.001 |
Percents are column percents; for each covariate, the percentages indicate percents within strata.
By the year 5 examination, persons with incarceration history had higher mean systolic blood pressures and were more likely to have hypertension (Table 2). Among participants without hypertension at baseline, former inmates were more likely to have developed incident hypertension by the year 5 examination (12% vs. 7%, unadjusted odds ratio (OR) 1.7, 95% confidence interval (CI) 1.2, 2.6). Among black men and less educated individuals, subgroups of the CARDIA sample where incarceration was more common, the relationship between incarceration and hypertension was particularly pronounced and statistically significant. Cholesterol levels (LDL, 108 mg/dL: vs. 108 mg/dL, p=0.9; HDL, 53 mg/dL vs. 53 mg/dL p=0.5) and diabetes (2% vs. 3%, p=0.7) did not differ between participants with and without a history of incarceration, even in subgroup analyses.
Table 2.
Blood pressure and hypertension among CARDIA cohort in 1990–91 at age 23–35, by history of incarceration before 1987
| Prior Incarceration |
No Prior Incarceration | p-value | |
|---|---|---|---|
| N (%) or Mean ± SD | |||
| All participants (N=4350) | |||
| Systolic blood pressure (mmHg) | 111 ± 13 | 108 ± 11 | <0.001 |
| Diastolic blood pressure (mmHg) | 70± 11 | 69 ± 10 | 0.42 |
| Hypertension | 65 (23) | 650 (16) | 0.006 |
| Incident Hypertension 1 | 29 (12) | 254 (7) | 0.007 |
| Black men (N=905) | |||
| Systolic blood pressure (mmHg) | 114 ± 12 | 114 ± 11 | 0.73 |
| Diastolic blood pressure (mmHg) | 71± 11 | 73 ± 10 | 0.10 |
| Hypertension | 43 (23) | 155 (20) | 0.05 |
| Incident Hypertension1 | 22 (17) | 75 (11) | 0.08 |
| White men (N=1054) | |||
| Systolic blood pressure (mmHg) | 111 ± 12 | 110 ± 11 | 0.57 |
| Diastolic blood pressure (mmHg) | 70± 10 | 71 ± 9 | 0.33 |
| Hypertension | 10 (16) | 149 (15) | 0.81 |
| Incident Hypertension1 | 4 (7) | 39 (4) | 0.35 |
| Black women (N=1214) | |||
| Systolic blood pressure (mmHg) | 106 ± 14 | 107 ± 11 | 0.39 |
| Diastolic blood pressure (mmHg) | 67± 13 | 69 ± 10 | 0.09 |
| Hypertension | 8 (16) | 235 (20) | 0.51 |
| Incident Hypertension1 | 2 (5) | 96 (9) | 0.29 |
| White women (N=1177) | |||
| Systolic blood pressure (mmHg) | 102 ± 10 | 101 ± 10 | <0.001 |
| Diastolic blood pressure (mmHg) | 67± 13 | 65 ± 8 | 0.42 |
| Hypertension | 4 (17) | 123 (10) | 0.30 |
| Incident Hypertension1 | 1 (5) | 44 (7) | 0.84 |
| High school education or less (N=1640) | |||
| Systolic blood pressure (mmHg) | 111 ± 12 | 109 ± 12 | 0.01 |
| Diastolic blood pressure (mmHg) | 70± 12 | 70 ± 10 | 0.84 |
| Hypertension | 46 (25) | 279 (19) | 0.05 |
| Incident Hypertension 1 | 22 (14) | 111 (9) | 0.02 |
| More than high school education (N=2710) | |||
| Systolic blood pressure (mmHg) | 110 ± 13 | 107 ± 11 | 0.006 |
| Diastolic blood pressure (mmHg) | 70± 12 | 69 ± 10 | 0.49 |
| Hypertension | 19 (18) | 383 (14) | 0.83 |
| Incident Hypertension 1 | 7 (7) | 143 (6) | 0.58 |
458 participants with baseline hypertension were excluded in this analysis (N=3892).
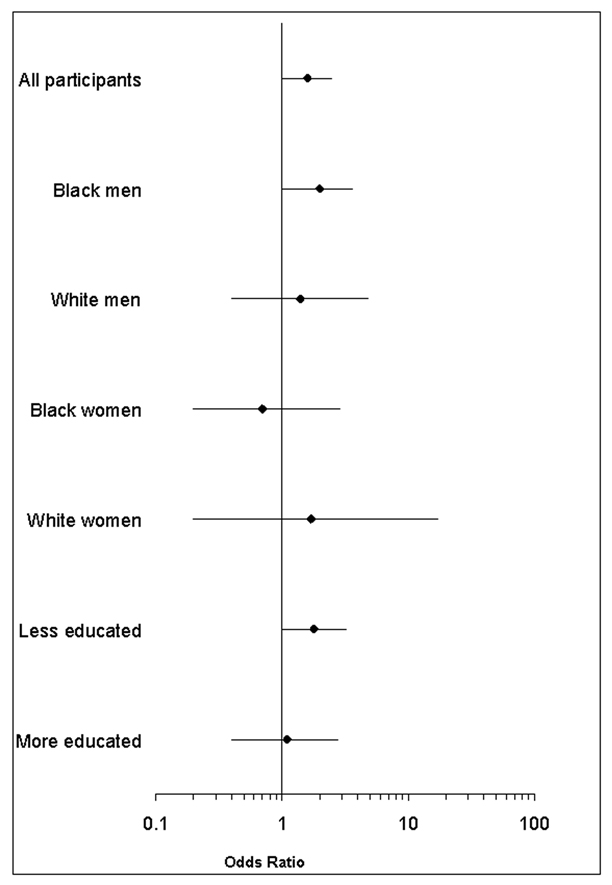
Because of the association of incarceration with hypertension, we examined several potential explanatory factors for the observed association of prior incarceration and incident hypertension. Adjustment for age, sex race, drugs and alcohol use did not alter this association (AOR 1.6 95% CI 1.0, 2.5), nor did additional adjustment for poverty (AOR 1.6, 95% CI 1.0, 2.6). Although the statistical tests for interaction between incarceration and race, sex, and education were not significant we ran these models within the sampling strata of CARDIA (Figure 1). Subgroups with the highest rate of incarceration – black men and less educated participants –showed significant associations between incarceration and incident hypertension in adjusted models; associations in subgroups that had lower rates of incarceration were not significant, but had wide confidence intervals. Although black men and less educated individuals were more likely to have been lost to follow up by year 5, our results were no different in analyses using inverse probability weights to reduce bias due to differential dropout (all participants AOR 1.5, 95% CI 0.9–2.2; black men AOR 1.9, 95% CI 1.0–3.6; less educated participants AOR 1.6, 95% CI 0.9–2.7).
Figure 1.
Association of incarceration history before 1987 with subsequent incident hypertension (1990–91) at age 23–35
*Adjusted for traditional clinical risk factors for hypertension including body mass index, smoking, excessive alcohol consumption, and illicit drug use, including cocaine and amphetamine use. The areas under the curve for models including all participants ranged from 0.52–0.68. The interaction terms between incarceration and race (p=0.77), incarceration and sex (p=0.15), and incarceration and educational level (p=0.22) are not statistically significant.
We examined whether incarceration might be associated with end organ damage related to hypertension. Persons with incarceration history had higher mean left ventricular mass index (54.0 ±14.1 gm/m2 vs. 50.3 ±14.1 gm/m2, p<0.001) and were more likely to have left ventricular hypertrophy (2% vs. 0.6%, p=0.005). Prior incarceration was associated with left ventricular hypertrophy in unadjusted analyses, and we observed a trend for an association even after accounting for potential confounders (Table 4). In analyses restricted to black men and less educated individuals, prior incarceration was also associated with left ventricular hypertrophy in both unadjusted and adjusted models.
Table 4.
Association of incarceration history with subsequent access to care at among the 650 CARDIA participants with hypertension
| No regular source of care | No health insurance | Limited medical care | ||||
|---|---|---|---|---|---|---|
| Adjusted Odds Ratio* (95% CI) |
P-value | Adjusted Odds Ratio (95% CI) |
P-value | Adjusted Odds Ratio (95% CI) |
P-value | |
| All participants (N=650) | 2.5 (1.3, 4.8) | 0.005 | 2.5 (1.4, 4.7) | 0.003 | 4.3 (2.1, 8.7) | <0.001 |
| Black men (N=170) | 2.9 (1.2, 6.6) | 0.01 | 2.4 (1.1, 5.4) | 0.03 | 6.5 (2.2, 18.8) | <0.001 |
|
Participants with high school education or less (N=287) |
2.5 (1.1, 5.5) | 0.03 | 3.3 (1.5, 6.9) | 0.02 | 5.1 (2.0, 13.2) | <0.001 |
Adjusted for sex, race, age, and socioeconomic status
Among participants with hypertension at the year 5 exam, those with a history of incarceration had an increased odds of reporting a barrier to healthcare at the next follow-up visit two years later (Table 5). This association persisted after adjustment for age, race, sex, and socioeconomic status and was more pronounced in black males and less educated participants. Former inmates were also more likely to lack treatment for their hypertension at the Year 7 exam (17% vs. 41%, unadjusted OR 3.3, 95% CI 1.3, 9), and in each of the follow-up visits over the entire 20 year duration of the CARDIA study (unadjusted OR 2.0, 95% CI 1.3, 3.0 at year 20). Incarceration prior to 1987 was associated with a 5.7 mmHg higher mean systolic blood pressure at the Year 20 examination (95% CI: 0.2–11.2), but not a higher diastolic blood pressure at Year 20 (1.1 mmHg (95% CI −0.6, 2.8) in analyses adjusting for the age, sex, and race of these participants.
DISCUSSION
In a well characterized US cohort of black and white young adults, we found that a history of incarceration is associated with a significantly elevated risk of future hypertension and with left ventricular hypertrophy. Over the three to five year period that followed incarceration, we found a cumulative incidence of hypertension of 12% among these young adults age 23–35 years, compared with 7% among those without incarceration. This association was strongest in those groups most likely to be incarcerated – black men and those with limited education - and was independent of alcohol and illicit drug use. Prior incarceration was also significantly associated with future barriers to healthcare access. Improving access to healthcare among former inmates, as well as screening for hypertension and other modifiable hypertension risk factors may be important in reducing the risk of cardiovascular death among individuals with a history of incarceration.
The mechanisms by which incarceration may lead to hypertension are not known. Several mechanisms have been postulated in prior studies, including higher use of drugs and alcohol, increased obesity, or lower socioeconomic status.9–12 Our data suggest that these mechanisms do not entirely explain the hypertension risk among former inmates, as we observed significant residual effect even after accounting for these factors. Other possible explanations include increased hostility or stress among individuals with prior incarceration that has been shown to increase the risk for hypertension and ultimately atherosclerosis.13–15 The stress of incarceration may increase catecholamines or stress hormones which lead to hypertension, or incarceration may cause lasting dysregulation of these hormones that might lead to the development of hypertension later in life at faster rates.
Although exploring these mechanisms whereby incarceration may contribute to hypertension is beyond the scope of this current study, our results suggest that hypertension and associated left ventricular hypertrophy in young former inmates may contribute to the previously observed increased risk of CVD death after their release. Left ventricular hypertrophy is a well-established independent risk factor for the development of heart failure and mortality.16, 17 Further study is needed to explore this relationship between incarceration, hypertension and left ventricular hypertrophy, both to establish whether the association is causal and if so, to elucidate how a history of incarceration might lead to hypertension and cardiovascular damage, and whether this is related to the type and duration of incarceration exposure.
While incarceration is not a traditional risk factor for cardiovascular risk factors, our results suggest that a history of incarceration should be understood as part of the risk profile for development of hypertension and left ventricular hypertrophy in young adults. Physicians working in communities where incarceration is highly prevalent should consider screening for a history of incarceration, as it may provide information about the future risk of hypertension and associated end-organ damage, as well as the risk of discontinuity in healthcare or medical treatment. Moreover, detention in jail, where healthcare is constitutionally guaranteed, may present a prime opportunity to screen soon-to-be released inmates for hypertension and to link inmates with chronic conditions to healthcare services in the community upon release.
We find that hypertensive individuals with a history of incarceration were less likely to have insurance, access to healthcare, or be on anti-hypertensive medications. Current and former inmates with chronic diseases such as hypertension typically fall at the intersection of two poorly functioning healthcare systems: the correctional healthcare system and the public safety net healthcare system. Neither healthcare system is well equipped to take care of the growing population of individuals with chronic medical conditions who cycle in and out of both systems. Ninety percent of those released from jail are uninsured and lack financial resources to pay for their medical care in the community.18 Most state correctional systems do not provide discharged inmates with a state identification card, thereby rendering such individuals ineligible for care in the major county hospitals that exist to serve the indigent upon release from correctional facilities.19 With access to regular outpatient care sharply constrained, formerly incarcerated individuals are more likely to seek care in the emergency department, rather than the primary care office.19, 20 The resulting discontinuity and irregularity of service may lead to poor health outcomes and/or duplication of services. Improved continuity of care between correctional facilities and the community could protect the health of inmates with hypertension and other chronic conditions, but assuring such continuity would require reconfiguration of correctional services and modest interventions such as the provision of referrals and identification cards to speed re-entry.
There are several limitations in our study. History of incarceration was only measured in the first two CARDIA examinations, and the single binary question item captured the preceding year events that would have included both a brief jail stay after arrest as well as longer periods of imprisonment. Because the CARDIA questionnaire asked specifically about jail, we can also not exclude the possibility that those in prisons would not have answered affirmatively. We therefore lack accurate information about the duration, frequency, or nature of the incarceration exposure, or exposure that might have occurred well before the baseline examination. Such information would be useful for understanding the true effect of the type, frequency and intensity of incarceration on the development of hypertension, especially given the high rates of recidivism nationwide.21 Measurement of important confounders in this study, including illicit drug use, was based on self-report. There may have been social desirability and recall bias at play in this study, especially in the reporting of illicit drugs.22, 23 Nonetheless, the prevalence of illicit drug use observed in this study approximates that in other studies in both incarcerated and non-incarcerated populations.23, 24 Finally, we initially chose to examine three types of cardiovascular risk factors and only found an association of incarceration with hypertension, thus raising the possibility of Type 1 error. However, the strength of this analysis is the consistency of the association we observe across the population subgroups in the US at highest risk of incarceration, as well as the association of incarceration with the end-organ manifestations of hypertension.
In conclusion, we found that prior incarceration predicts future hypertension and left ventricular hypertrophy among young adults. For the more than 7 million people that pass through US jails and prison each year,25 incarceration may be an independent risk factor for the development of hypertension and left ventricular hypertrophy, both of which put such persons at higher risk for clinical CVD. Incarceration may be both a cause for hypertension and cardiovascular disease, as well as an underutilized opportunity for intervention and improving health and access to healthcare.
Table 3.
Association of incarceration history before 1987 with left ventricular hypertrophy in 1990–91 at age 23–35*
| Unadjusted | Adjusted for demographic characteristics, clinical risk factors and illicit drug use† |
Adjusted for demographic characteristics, clinical risk factors, illicit drug use, and measure of socioeconomic status‡ |
||||
|---|---|---|---|---|---|---|
| Odds Ratio (95% CI) |
P- value |
Odds Ratio (95% CI) |
P-value | Odds Ratio (95% CI) |
P-value | |
|
All Participants (N=3688) |
3.8 (1.4, 10.1) |
0.009 | 2.5 (0.8, 7.3) |
0.1 | 2.7 (0.9, 7.9) |
0.08 |
|
Black men (N=760) |
2.6 (0.6–10.6) |
0.2 | 4.3 (0.9–20.0) |
0.07 | 6.0 (1.2–31.0) |
0.03 |
|
Participants with high school education or less (N=1364) |
4.8 (1.6, 14.4) |
0.006 | 4.3 (1.0, 17.3) |
0.04 | 4.3 (1.0, 17.3) |
0.04 |
This analysis included only participants who were not hypertensive at baseline. The areas under the curve for models including all participants ranged from 0.69–0.82.
Traditional clinical risk factors for hypertension include body mass index, smoking, and excessive alcohol consumption; illicit drugs includes cocaine and amphetamine use.
Socioeconomic status is defined by family income.
ACKNOWLEDGMENTS
E. A. Wang originated this research question and participated in the analysis of data and writing of the article. M.J. Pletcher, F. Lin, E. Vittinghoff, and S Kertesz participated in the analysis of data and writing of the article. C. Kiefe originated the study and participated in the analysis of data and writing of the article. K. Bibbins-Domingo originated this research question and participated in the analysis of the data and writing of the article. K. Bibbins-Domingo and E.A. Wang had full access to all of the data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. No potential conflict of interest relevant to this article was reported.
Work on this manuscript was supported (or partially supported) by contracts: University of Alabama at Birmingham, Coordinating Center, N01-HC-95095; University of Alabama at Birmingham, Field Center, N01-HC-48047; University of Minnesota, Field Center and Diet Reading Center (Year 20 Exam), N01-HC-48048; Northwestern University, Field Center, N01-HC-48049; Kaiser Foundation Research Institute, N01-HC-48050; University of California, Irvine, Echocardiography Reading Center (Year 5 & 10), N01-HC-45134; Harbor-UCLA Research Education Institute, Computed Tomography Reading Center (Year 15 Exam) N01-HC-05187; Wake Forest University (Year 20 Exam), N01-HC-45205; New England Medical Center (Year 20 Exam), N01-HC-45204 from the National Heart, Lung and Blood Institute. E. Wang was supported by the National Research Service Award Training Grant in General Internal Medicine to University of California, San Francisco (grant T32 HP19025). K. Bibbins-Domingo is supported by grants from the Robert Wood Johnson Amos Faculty Development Program, a diversity supplement to the CARDIA contract to the University of Alabama Coordinating Center (N01-HC-95095), and the UCSF Hellman Family Faculty Award.
We gratefully acknowledge the administrative assistance of Tekeshe Mekonnen, MS in the resubmission of this manuscript.
REFERENCES
- 1.Trust TPC. One in 100: Behind Bars in America. 2008 [Google Scholar]
- 2.Binswanger IA, Stern MF, Deyo RA, et al. Release from prison--a high risk of death for former inmates. N Engl J Med. 2007 Jan 11;356(2):157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Olubodun J. Prison life and the blood pressure of the inmates of a developing community prison. J Hum Hypertens. 1996 Apr;10(4):235–238. [PubMed] [Google Scholar]
- 4.Cutter GR, Burke GL, Dyer AR, et al. Cardiovascular risk factors in young adults. The CARDIA baseline monograph. Control Clin Trials. 1991 Feb;12 1 Suppl:1S–77S. doi: 10.1016/0197-2456(91)90002-4. [DOI] [PubMed] [Google Scholar]
- 5.Alcoholism NIoAAa. National Institute on Alcohol Abuse and Alcoholism, Helping Patients Who Drink Too Much: A Clinician's Guide. 2008 http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm.
- 6.Services UDoHaH. US Department of Health and Human Services. [Accessed: October 15, 2008]; http://aspe.hhs.gov/POVERTY/figures-fed-reg.shtml.
- 7.Gardin JM, Wong ND, Bommer W, et al. Echocardiographic design of a multi-center investigation of free-living elderly subjects: the Cardiovascular Health Study. J Am Soc Echo. 1992;5:63–72. doi: 10.1016/s0894-7317(14)80105-3. [DOI] [PubMed] [Google Scholar]
- 8.Alonso A, Segui-Gomez M, de Irala J, Sanchez-Villegas A, Beunza JJ, Martinez-Gonzalez MA. Predictors of follow-up and assessment of selection bias from dropouts using inverse probability weighting in a cohort of university graduates. Eur J Epidemiol. 2006;21(5):351–358. doi: 10.1007/s10654-006-9008-y. [DOI] [PubMed] [Google Scholar]
- 9.Hajjar IKT. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003;290(51):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 10.Control CoD. State-specific trends in self-reported blood pressure screening and high blood pressure---United States, 1991–1999. MMWR. 2002;51:456–460. [PubMed] [Google Scholar]
- 11.Control CfD. State-specific prevalence of selected health behaviors, by race and ethnicity--Behavioral Risk Factor Surveillance System, 1997. MMWR. 2000;49 (No. SS-2) [PubMed] [Google Scholar]
- 12.Policy OoNDC. Drug Data Summary. [Accessed April 20];2008 http://www.whitehousedrugpolicy.gov/publications/factsht/drugdata/index.html.
- 13.Yan LL, Liu K, Matthews KA, Daviglus ML, Ferguson TF, Kiefe CI. Psychosocial factors and risk of hypertension: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Jama. 2003 Oct 22;290(16):2138–2148. doi: 10.1001/jama.290.16.2138. [DOI] [PubMed] [Google Scholar]
- 14.Carroll D, Davey Smith G, Sheffield D, Shipley MJ, Marmot MG. The relationship between socioeconomic status, hostility, and blood pressure reactions to mental stress in men: data from the Whitehall II study. Health Psychol. 1997 Mar;16(2):131–136. doi: 10.1037//0278-6133.16.2.131. [DOI] [PubMed] [Google Scholar]
- 15.Iribarren C, Sidney S, Bild DE, et al. Association of hostility with coronary artery calcification in young adults: the CARDIA study. Coronary Artery Risk Development in Young Adults. Jama. 2000 May 17;283(19):2546–2551. doi: 10.1001/jama.283.19.2546. [DOI] [PubMed] [Google Scholar]
- 16.Koren MJDR, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Annals of Internal Medicine. 1991;114:345–352. doi: 10.7326/0003-4819-114-5-345. [DOI] [PubMed] [Google Scholar]
- 17.Levy DGR, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Study. New England Journal of Medicine. 1990;322:1561–1566. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 18.Lee J, Vlahov D, Freudenberg N. Primary care and health insurance among women released from New York City jails. J Health Care Poor Underserved. 2006 Feb;17(1):200–217. doi: 10.1353/hpu.2006.0028. [DOI] [PubMed] [Google Scholar]
- 19.Mallik-Kane K. Returning Home Illinois Policy Brief: Health and Prison Reentry [Google Scholar]
- 20.Conklin TJ, Lincoln T, Tuthill RW. Self-reported health and prior health behaviors of newly admitted correctional inmates. Am J Public Health. 2000 Dec;90(12):1939–1941. doi: 10.2105/ajph.90.12.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prison sentence and time served for violence. Bureau of Justice Statistics. 1995 NCJ 153858. [Google Scholar]
- 22.Kim TaH MN. Validity of self-report of illicit drug use in young hypertensive urban African-American males. Addictive Behaviors. 2003:795–802. doi: 10.1016/s0306-4603(01)00277-5. [DOI] [PubMed] [Google Scholar]
- 23.Hill MN, Bone LR, Kim MT, Miller DJ, Dennison CR, Levine DM. Barriers to hypertension care and control in young urban black men. Am J Hypertens. 1999 Oct;12(10 Pt 1):951–958. doi: 10.1016/s0895-7061(99)00121-1. [DOI] [PubMed] [Google Scholar]
- 24.Mumola C. Substance abuse and treatment, State and Federal prisoners, 1997. Bureau of Justice Statistics Bulletin. 1997 NCJ 172871. [Google Scholar]
- 25.William J Sobol TDM, Harrison Paige M. Prisons and Jails at Midyear 2006. Washington, DC: Bureau of Justice Statistics; 2006. [Google Scholar]