Abstract
Context:
Debate remains regarding the dose of physical activity that will facilitate weight loss maintenance.
Objective:
To examine the dose and intensity of physical activity (PA) in the context of a 24-month behavioral intervention on weight loss, anthropometric measures, fitness, PA, and eating behaviors.
Design:
Data collection and intervention were conducted between December 1999 and January 2003. Participants were assigned to one of four behavioral weight loss intervention groups, with randomization based on PA energy expenditure and intensity.
Setting:
A hospital-based weight loss research center.
Participants:
201 overweight and obese women (BMI: 27 to 40 kg/m2; Age: 21 to 45 years) with no contraindications to weight loss or physical activity.
Interventions:
Recommended to reduce intake to 1,200 to 1,500 kcal/d and to increase PA based on dose (1,000 or 2,000 kcal/wk) and intensity (moderate or vigorous). Content was delivered in a combination of in-person and telephone contacts delivered across 24 months.
Main Outcome Measures:
The primary outcome was weight loss.
Results:
Weight loss did not differ between the randomized groups at 6 months (approximately 8-10% weight loss) or 24 months (approximately 5% weight loss). Post-hoc analysis showed that individuals sustaining ≥10% weight loss at 24 months reported more PA (1,835 kcal/wk or 275 min/wk) compared to those sustaining <10% weight loss (p<0.001).
Conclusions:
The addition of 275 min/wk of PA, in combination with a reduction in energy intake, is important for sustaining ≥10% weight loss for overweight women. Interventions to facilitate this level of PA are needed.
Keywords: physical activity, obesity, overweight, fitness, weight control
Introduction
In excess of 65% of adults in the United States are overweight 1. This is a public health concern because of the association with numerous chronic diseases 2. Long-term weight loss and prevention of weight regain have been less than desirable 3, 4, and therefore, there is a need for more effective interventions.
Behavioral interventions result in weight loss of approximately 10% of initial body weight within 6 months, with intervention recommendations including both a reduction in energy intake (diet) and an increase in energy expenditure (exercise/physical activity) 5. The importance of physical activity may be heightened in the maintenance of this clinically significant magnitude of weight loss 6-9.
The consensus public health recommendation for physical activity is a minimum of 30 minutes of moderate intensity activity on most days of the week (150 min/wk) 10, 11. There is growing consensus that a higher level of exercise may be necessary to enhance long-term weight loss 12-15. Few studies exceeding 12 months in duration have been conducted to examine the optimal amount of exercise to enhance weight loss. In secondary analyses, Jakicic et al. 6 reported that exercise ≥200 min/wk over a 12-month period enhanced weight loss, and data are now available over a period of 24-months.
This study examined the 24-month effect of exercise of varying duration and intensity on weight loss and fitness in overweight adult women. Secondary analyses examine the level of exercise necessary to sustain varying levels of weight loss at 24 months.
Methods
Subjects
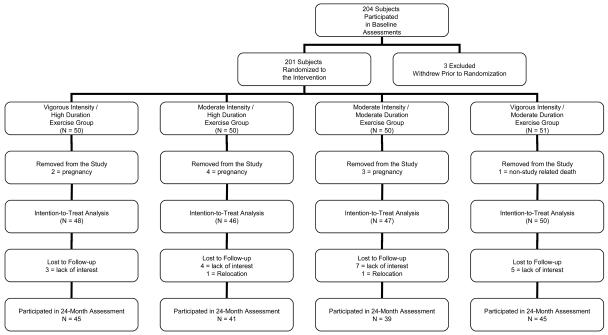
Data collection and the intervention for this study were conducted from December 1999 until January 2003. Participants included 201 women (Table 1 and Figure 1). Eligibility criteria included BMI of 27 to 40 kg/m2, 21 to 45 years of age, and sedentary at baseline defined as reporting exercising <3 days per week for <20 minutes per day over the previous 6 months. Exclusionary criteria included history of myocardial infarction, taking medication that would alter the heart rate response during exercise, taking medication that would impact metabolism or weight loss, being treated for psychological conditions, currently pregnant, pregnant within the previous 6 months, or planning to become pregnant during the intervention period, a medical condition that impacts metabolism or body weight, a medical condition that would limit exercise participation. A medical history and physical activity readiness questionnaire (PAR-Q) were completed, and the subject's personal physician indicated that the proposed intervention was not contraindicated. Written informed consent was obtained, and the protocol was approved by the Institutional Review Boards of the Miriam Hospital (Providence, RI) and the University of Pittsburgh (Pittsburgh, PA).
Table 1.
Baseline Characteristics of Subjects Randomly Assigned to Treatment and of Those Completing the Study.
| Intervention Groups | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Vigorous Intensity/ High Duration |
Moderate Intensity / High Duration |
Moderate Intensity / Moderate Duration |
Vigorous Intensity / Moderate Duration |
Total | ||||||
| Number of Subjects | ||||||||||
| Randomly Assigned | 50 | 50 | 50 | 51 | 201 | |||||
| Intention-to-Treat Analysis | 48 | 46 | 47 | 50 | 191 | |||||
| Completers Analysis | 45 | 41 | 39 | 45 | 170 | |||||
| Age (years) | ||||||||||
| Randomly Assigned | 38.8±5.5 | 37.4±5.4 | 37.2±6.1 | 36.4±5.7 | 37.5±5.7 | |||||
| Intention-to-Treat Analysis | 39.2±5.3 | 38.1±5.0 | 37.8±5.6 | 36.3±5.6 | 37.8±5.5 | |||||
| Completers Analysis | 39.6±5.1 | 38.7±4.7 | 38.7±5.5 | 36.4±5.8 | 38.3±5.4 | |||||
| Weight (kg) | ||||||||||
| Randomly Assigned | 87.3±11.2 | 86.8±14.6 | 87.2±13.1 | 88.1±14.6 | 87.4±13.3 | |||||
| Intention-to-Treat Analysis | 87.4±10.7 | 87.9±14.4 | 87.4±13.3 | 87.9±14.7 | 87.6±13.3 | |||||
| Completing Treatment | 87.6±10.8 | 85.9±13.4 | 88.1±13.2 | 88.4±15.3 | 87.5±13.2 | |||||
| Body Mass Index (kg/m2) | ||||||||||
| Randomly Assigned | 32.8±3.9 | 32.2±3.9 | 32.8±4.3 | 32.8±4.6 | 32.6±4.2 | |||||
| Intention-to-Treat Analysis | 32.7±3.8 | 32.4±3.9 | 32.8±4.3 | 32.7±4.6 | 32.7±4.1 | |||||
| Completing Treatment | 32.8±3.9 | 32.0±3.8 | 33.1±4.4 | 32.8±4.7 | 32.7±4.2 | |||||
| Ethnicity * | ||||||||||
| American Indian or Alaska Native |
1 | (1) | 0 | (0) | 0 | (0) | 0 | (0) | 1 | (1) |
| Asian | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
| Black or African-American | 3 | (3) | 3 | (2) | 8 | (7) | 2 | (2) | 16 | (14) |
| Hispanic, Latino, Portuguese, or Cape Verdean |
1 | (1) | 1 | (1) | 5 | (5) | 9 | (9) | 16 | (16) |
| Native Hawaiian or Other Pacific Islander |
0 | (0) | 1 | (1) | 0 | (0) | 0 | (0) | 1 | (1) |
| White | 42 | (39) | 41 | (37) | 33 | (26) | 38 | (33) | 154 | (135) |
| Mixed Ethnicity | 0 | (0) | 0 | (0) | 1 | (1) | 1 | (1) | 2 | (2) |
| Not Specified or Missing | 1 | (1) | 0 | (0) | 0 | (0) | 0 | (0) | 1 | (1) |
indicates that numbers are based on the intent-to-treat analysis (N=191) and numbers in parentheses are based on subjects completing 24 months (N = 170).
Figure 1.
Flow chart of subject randomization and follow-up.
Intervention
Group Meetings
Subjects attended group meetings weekly during months 1-6, twice per month during months 7-12, once per month during months 13-18, with no group sessions conducted during months 19-24. Sessions focused on strategies for modifying both eating and exercise behaviors.
Telephone calls
Subjects received brief (approximately 10 minutes) telephone calls periodically from a member of the intervention team. A standard script was used to conduct these calls. Telephone calls occurred twice per month during months 7-12, once per month during months 13-18, and twice per month during months 19-24.
Diet
Subjects weighing <200 pounds at baseline were prescribed 1200 kcal/d, with subjects weighing ≥200 pounds at baseline prescribed 1500 kcal/d. Prescription of dietary fat intake was 20-30% of total energy intake. Subjects were instructed to maintain these dietary recommendations throughout the duration of the study unless they achieved a BMI of <25 kg/m2, at which time energy intake was adjusted.
Exercise
Subjects were randomized to one of four exercise conditions based on estimated energy expenditure (moderate = 1000 kcal/wk versus vigorous = 2000 kcal/wk) and exercise intensity (moderate versus vigorous) 6. Randomization, based on a computer program, was to moderate intensity/moderate energy expenditure (MOD/MOD), moderate intensity/high energy expenditure (MOD/HIGH), vigorous intensity/moderate energy expenditure (VIG/MOD), or vigorous intensity/high energy expenditure (VIG/HIGH). Energy expenditure was converted to minutes per week based on the average body weight of participants in this study, and therefore weekly goals were expresses as minutes per week for subjects. Subjects were encouraged to spread the exercise over 5 days per week, and for each exercise bout to be a minimum of 10 minutes in duration. Intensity was prescribed as percent of age-predicted maximal heart rate (Moderate = 50 to 65%; Vigorous = 70 to 85%) and rating of perceived exertion (RPE) (Moderate = 10 to 12; Vigorous = 13 to 15) 16. Subjects were taught how to monitor their heart rate using the palpation method and how to regulate intensity using RPE. Exercise was not supervised on-site, but a treadmill was provided to each subject to use at home as a strategy to enhance participation 7.
Assessment of Outcomes
Height and Weight
Height was measured at 0 months to the nearest 0.1 centimeter. Subjects were weighed at 0, 6, 12, 18, and 24 months in undergarments while wearing a cloth hospital gown to the nearest 0.25 pounds. BMI was computed as kg/m2.
Anthropometry
Waist circumference (horizontally at the umbilicus), hip circumference (widest portion of the buttocks), and sagittal diameter of the abdomen (iliac crest in a supine position) were measured at 0, 6, and 24 months. Measures were accepted when two measures ≤2.0 cm apart were obtained.
Fitness
A submaximal graded exercise treadmill test to 85% of age-predicted maximal heart rate (computed as 220 minus age) was performed at 0, 6, and 24 months. Speed was 80.4 m/min (3.0 mph); grade was initiated at 0% and progressed by 2.5% at 3-minute intervals until termination heart rate was achieved. A metabolic cart (Vmax Spectra, SensorMedics, Yorba Linda, CA) was used to assess oxygen consumption.
Leisure-Time Physical Activity (LTPA)
LTPA was assessed using a questionnaire 17. This questionnaire was completed by participants a 0, 6, and 24 months. However, a sub-sample of participants also completed this questionnaire at 12 and 18 months. Energy expenditure was computed using previously published scoring algorithms 17 and classifications based on the compendium of physical activity 18. This questionnaire queried subjects about the amount of walking (12 city blocks equivalent to 1 mile, and 1 mile equivalent to 20 minutes), along with time spent per week in sport, fitness, or recreational activity performed for the purpose of exercise. These data were used to represent time (min/wk) and energy expenditure (kcal/wk) for participation in LTPA. Subjects also reported flights of steps walked per day; however, data from the flights of steps reported were not used in the computation of LTPA for this study.
Energy Intake
Energy intake was assessed at 0, 6, and 24 months using the previously validated 1998 version of the food frequency questionnaire developed by Block and colleagues 19.
Weight Control Eating Behaviors
Eating behavior was assessed at 0, 6, and 24 months using the Eating Behavior Inventory (EBI) 20. A higher score is indicative of engagement in more eating behaviors recommended for weight control.
Statistical Analysis
A power calculation was computed based on expected changes in body weight between the randomized groups. Randomization of 40 subjects per group provided 70% power to detect a moderate effect size (0.50) for differences in weight loss between the groups at an alpha level of 0.05 assuming moderate intraclass correlations (0.40 – 0.60) among the repeated measures (time effect). Assuming a 15 to 20 percent attrition increased the sample to 50 subjects per randomized group.
Statistical analyses were performed using SAS (version 9.1) and SPSS (version 15.0), with the type I error rate fixed at p≤0.05 (two-tailed). Separate mixed effect models were performed to examine the change in selected outcomes across the 24 month study period. These were intention-to-treat analyses with baseline data carried forward for missing data at subsequent assessment periods.
This study randomly assigned 201 subjects to the intervention. However, 10 subjects were excluded from follow-up analyses due to pregnancy (N=9) and non-study related death (N=1). Thus, 191 subjects were included in the primary analyses that were performed to examine the a priori aims of this study.
Secondary analyses were performed with subjects grouped based on the percent weight loss achieved at 24-months, and included 170 subjects who provided objective weight loss data at 24-months. Weight loss groups included <0% (N=54), 0-4.9% (N=33), 5.0-9.9% (N=36), and ≥10% (N=47) weight loss.
Results
Results by Randomized Group Assignment
Baseline characteristics did not differ between subjects randomly assigned to the four exercise groups (Table 1). Excluding individuals removed from the study, 170 of the 191 (89%) randomized subjects completed the 24 month study (Figure 1). There were no serious adverse events related to the interventions in this study. Chi-square analysis revealed no significant difference in completion rates between groups (MOD/MOD = 83%, MOD/HIGH = 89%, VIG/MOD = 90%, VIG/HIGH = 94%). Subjects who completed the study were significantly older than those who dropped out of this study (38.3±5.4 years vs. 33.8±4.3 years; p<0.001), with no other differences observed at baseline.
Intervention Contact
Subjects attended 79.1±19.5% of group sessions during months 1-6, with attendance at group sessions being 67.8±22.0% across the entire 24 months. 67.7±23.7% of telephone calls were completed during the intervention period. There were no significant differences between intervention groups for sessions attended or telephone calls completed.
LTPA, Energy Intake, and Eating Behaviors
The significant time effect for LTPA reflects an increase of 1235±1815 kcal/wk from baseline to 6 months (Table 2). This increase was not sustained, with the increase at 24 months being 720±1189 kcal/wk above baseline. The non-significant Group X Time Interaction indicated that this pattern for LTPA was consistent across intervention groups. Eating behavior and dietary intake data are presented in Table 2.
Table 2.
Physical Activity, Eating Behaviors, and Energy Intake Across 24 months by Randomized Group Assignment.
| Randomized Groups Assignment (N=191) |
|||||||
|---|---|---|---|---|---|---|---|
| Vigorous Intensity/ High Duration (N=48) |
Moderate Intensity / High Duration (N=46) |
Moderate Intensity / Moderate Duration (N=47) |
Vigorous Intensity / Moderate Duration (N=50) |
Intervention Group Effect |
Time Effect |
Group × Time Effect |
|
| LTPA* (kcal/wk) | |||||||
| Baseline | 295±861 | 351±539 | 456±930 | 366±590 | 0.64 | <0.001 | 0.42 |
| 6 mo. | 1583±1446 | 2035±2807 | 1462±1241 | 1354±1356 | |||
| 24 mo. | 1182±1310 | 1080±1268 | 1020±1180 | 1066±869 | |||
| LTPA* (min/wk) | |||||||
| Baseline | 54.9±154.9 | 70.5±110.5 | 84.9±144.9 | 70.8±110.0 | 0.10 | <0.001 | 0.06 |
| 6 mo. | 297.6±263.6 | 387.1±482.5 | 238.9±208.4 | 254.7±239.6 | |||
| 24 mo. | 220.3±238.6 | 213.1±257.0 | 124.6±162.6 | 192.8±175.6 | |||
| Eating Behavior Inventory | |||||||
| Baseline | 69.8±9.3 | 71.2±9.6 | 66.7±9.9 | 69.5±10.4 | 0.05 | <0.001 | 0.74 |
| 6 mo. | 90.4±12.5 | 87.7±13.9 | 83.8±14.2 | 87.6±12.1 | |||
| 24 mo. | 79.8±12.6 | 79.0±12.9 | 73.8±13.3 | 77.5±11.1 | |||
| Energy Intake (kcal/d) | |||||||
| Baseline | 2096±805 | 2147±978 | 2039±754 | 2200±875 | 0.79 | <0.001 | 0.67 |
| 6 mo. | 1454±688 | 1551±495 | 1551±525 | 1551±560 | |||
| 24 mo. | 1454±771 | 1553±711 | 1689±776 | 1628±993 | |||
| Dietary Fat Intake (%) | |||||||
| Baseline | 38.7±6.7 | 39.0±8.8 | 38.4±6.4 | 36.8±5.2 | 0.50 | <0.001 | 0.38 |
| 6 mo. | 30.1±5.6 | 28.3±8.1 | 30.7±8.1 | 29.7±6.5 | |||
| 24 mo. | 34.7±6.0 | 33.7±8.0 | 34.9±6.6 | 32.9±5.8 | |||
LTPA = Leisure-Time Physical Activity
Weight
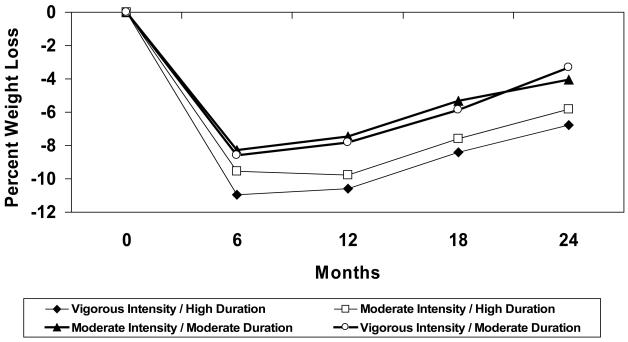
Weight loss data are shown in Table 3 and Figure 2. There was a significant time effect (p<0.001) for change in body weight; with a non-significant Group Effect and Group X Time Interaction Effect. Weight loss was 8.1±5.0 kg (9.3±5.6%) at 6 months, 7.8±6.8 kg (8.9±7.8%) at 12 months, 5.9±7.0 kg (6.8±8.1%) at 18 months, and 4.2±7.2 kg (5.0±8.5%) at 24 months. Anthropometric data are presented in Table 3.
Table 3.
Differences in Body Weight, Regional Adiposity, and Fitness Between Intervention Groups (N=191).
| Vigorous Intensity/ High Duration (N=48) |
Moderate Intensity / High Duration (N=46) |
Moderate Intensity / Moderate Duration (N=47) |
Vigorous Intensity / Moderate Duration (N=50) |
Intervention Group Effect |
Time Effect |
Group × Time Effect |
|
|---|---|---|---|---|---|---|---|
| Body Weight (kg) | |||||||
| Baseline | 87.4±10.7 | 87.9±14.4 | 87.4±13.3 | 87.9±14.7 | 0.85 | <0.001 | 0.43 |
| 6 mo. | 77.9±11.5 | 79.7±15.7 | 80.1±12.4 | 80.4±14.4 | |||
| 12 months | 78.3±12.9 | 79.6±16.9 | 80.9±13.6 | 81.0±14.3 | |||
| 18 months | 80.1±12.6 | 81.5±17.0 | 82.7±14.4 | 82.6±14.3 | |||
| 24 mo. | 81.6±13.1 | 83.2±18.3 | 83.9±14.8 | 85.0±15.2 | |||
| Body Mass Index(kg/m2) | |||||||
| Baseline | 32.7±3.8 | 32.4±3.9 | 32.8±4.3 | 32.7±4.6 | .72 | <0.001 | 0.38 |
| 6 mo. | 29.2±4.1 | 29.4±4.5 | 30.1±4.3 | 29.9±4.6 | |||
| 12 months | 29.3±4.6 | 29.3±4.8 | 30.3±4.6 | 30.2±4.6 | |||
| 18 months | 30.0±4.5 | 30.0±4.8 | 31.0±4.9 | 30.8±4.6 | |||
| 24 mo. | 30.6±4.8 | 30.6±5.3 | 31.5±5.0 | 31.7±5.0 | |||
| Waist Circumference(cm) | |||||||
| Baseline | 100.7±10.5 | 100.6±13.5 | 97.1±11.4 | 99.6±11.3 | 0.94 | <0.001 | 0.11 |
| 6 mo. | 93.0±11.2 | 92.4±15.5 | 93.0±10.4 | 94.3±11.5 | |||
| 24 mo. | 95.6±12.4 | 95.9±16.2 | 96.2±13.3 | 97.0±13.3 | |||
| Hip Circumference (cm) | |||||||
| Baseline | 115.8±7.9 | 116.6±9.7 | 115.9±9.2 | 115.7±8.1 | 0.92 | <0.001 | 0.36 |
| 6 mo. | 107.8±8.8 | 109.8±11.1 | 109.2±8.1 | 109.4±8.9 | |||
| 24 mo. | 112.5±10.1 | 113.0±12.9 | 114.0±9.9 | 114.2±9.2 | |||
| Waist-to-Hip Ratio | |||||||
| Baseline | 0.87±0.07 | 0.86±0.07 | 0.84±0.06 | 0.86±0.07 | 0.56 | 0.03 | 0.09 |
| 6 mo. | 0.86±0.08 | 0.84±0.08 | 0.85±0.07 | 0.86±0.07 | |||
| 24 mo. | 0.85±0.07 | 0.85±0.08 | 0.84±0.07 | 0.85±0.07 | |||
| Sagittal Diameter | |||||||
| Baseline | 23.5±3.1 | 23.5±2.8 | 22.9±3.1 | 23.0±2.9 | 0.98 | <0.001 | 0.35 |
| 6 mo. | 21.3±2.4 | 21.5±3.2 | 21.5±2.8 | 21.3±2.4 | |||
| 24 mo. | 22.0±3.1 | 22.1±3.8 | 22.6±3.1 | 22.2±3.0 | |||
| Fitness (ml/kg/min) | |||||||
| Baseline | 20.2±3.0 | 19.4±3.2 | 19.8±3.7 | 19.7±3.1 | 0.21 | <0.001 | 0.11 |
| 6 mo. | 23.7±4.3 | 21.8±3.8 | 21.5±3.9 | 22.2±3.8 | |||
| 24 mo. | 23.2±4.5 | 22.1±4.6 | 22.1±3.9 | 22.1±4.1 | |||
| Fitness (L/min) | |||||||
| Baseline | 1.8±0.3 | 1.7±0.4 | 1.7±0.3 | 1.7±0.3 | 0.72 | <0.001 | 0.68 |
| 6 mo. | 1.8±0.3 | 1.7±0.4 | 1.7±0.3 | 1.8±0.3 | |||
| 24 mo. | 1.9±0.3 | 1.8±0.4 | 1.8±0.3 | 1.8±0.4 | |||
| Time to Achieve 85% of Maximal Heart Rate (min.) | |||||||
| Baseline | 11.5±3.1 | 10.9±4.1 | 10.9±3.8 | 11.4±3.3 | 0.56 | <0.001 | 0.002 |
| 6 mo. | 16.0±4.4 | 14.3±3.3 | 14.0±3.8 | 15.1±4.5 | |||
| 24 mo. | 13.1±4.1 | 13.3±3.0 | 12.9±3.8 | 12.5±3.6 | |||
Figure 2.
Percent weight loss based on randomized group assignment (N = 191).
Fitness
At baseline, 184 subjects provided valid oxygen consumption data, which allowed for change in oxygen consumption to be analyzed for these individuals. There was a significant increase (p<0.001) in fitness from baseline to 6 months of 13.4±15.9% (2.5±3.0 ml/kg/min), with a 13.9±18.3% (2.5±3.4 ml/kg/min) increase from baseline to 24 months. There was no significant Group Effect or Group X Time Interaction for fitness expressed as ml/kg/min or L/min (Table 3).
Results by Percent Weight Loss Achieved at 24 Months
Weight
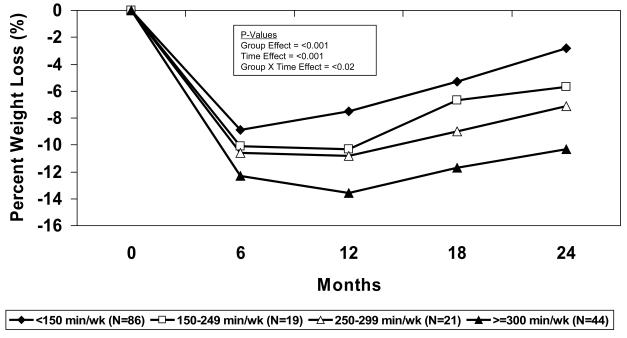
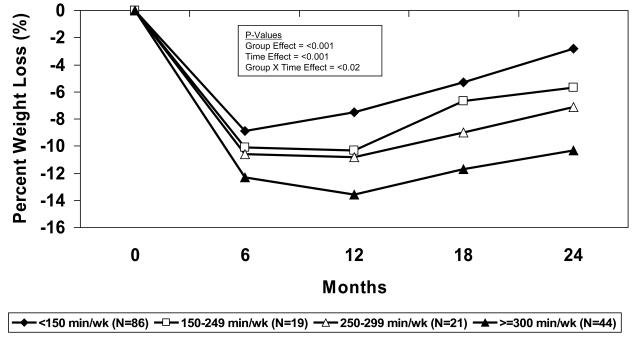
There was a significant Group X Time interaction (p<0.001) for weight change measured at 6 and 24 months between the weight loss categories (Table 4). Weight change from baseline to 24 months was +3.0±2.6 kg (+3.5±3.1%) for the <0% category, −2.2±1.3 kg (−2.5±1.3%) for the 0-4.9% category, −6.4±1.3 kg (−7.4±1.3%) for the 5.0-9.9% category, and −14.2±5.2 kg (−16.8±6.2%) for the ≥10% category. Percent weight loss with subjects group on varying levels of physical activity (min/wk and kcal/wk) are presented in Figures 4 and 5. Anthropometric data are presented in Table 5.
Table 4.
Physical Activity, Eating Behaviors, and Energy Intake Based on Weight Loss at 24 Months (N=170).
| Groups Based on Weight Loss at 24 Months (N=170) |
|||||||
|---|---|---|---|---|---|---|---|
| <0% (N=54) | 0-4.9% (N=33) | 5.0-9.9% (N=36) | >10% (N=47) | Intervention Group Effect |
Time Effect |
Group × Time Effect |
|
| Subjects by Randomized Group Assignment N (% of subject in group)* |
|||||||
| Vigorous Intensity / High Duration |
12 (26.7%) | 5 (11.1%) | 11 (24.4%) | 17 (37.8%) | |||
| Moderate Intensity / High Duration |
14 (34.1%) | 9 (22.0%) | 5 (12.2%) | 13 (31.7%) | |||
| Moderate Intensity / Moderate Duration |
12 (30.8%) | 10 (25.6%) | 9 (23.1%) | 8 (20.5%) | |||
| Vigorous Intensity / Moderate Duration |
16 (35.6%) | 9 (20.0%) | 11 (24.4%) | 9 (20.0%) | |||
| LTPA** (kcal/wk) | |||||||
| Baseline | 232±422 | 547±1117 | 336±545 | 299±459 | 0.06 | <0.001 | <0.001 |
| 6 mo. | 1602±2590 | 1586±1342 | 1939±1668 | 1761±1297 | |||
| 24 mo. | 703±808 | 1024±1087 | 988±1010 | 1848±1329 | |||
| LTPA** (min/wk) | |||||||
| Baseline | 53.7±95.4 | 104.4±202.4 | 60.1±102.9 | 63.6±95.8 | 0.06 | <0.001 | <.001 |
| 6 mo. | 297.6±421.7 | 289.9±229.6 | 370.0±337.2 | 317.2±241.6 | |||
| 24 mo. | 127.3±154.1 | 194.3±200.4 | 184.9±189.4 | 338.2±249.0 | |||
| Eating Behavior Inventory | |||||||
| Baseline | 68.4±10.2 | 66.6±11.8 | 72.8±8.4 | 70.3±8.3 | <0.0001 | <0.001 | 0.002 |
| 6 mo. | 87.1±13.8 | 83.8±14.4 | 92.6±10.0 | 91.9±10.1 | |||
| 24 mo. | 74.4±12.1 | 73.8±11.7 | 80.2±9.8 | 85.6±11.7 | |||
| Energy Intake (kcal/d) | |||||||
| Baseline | 2329±1025 | 2272±888 | 2042±643 | 2028±760 | 0.02 | <0.001 | 0.93 |
| 6 mo. | 1711±692 | 1506±489 | 1398±474 | 1384±446 | |||
| 24 mo. | 1809±1142 | 1638±802 | 1452±640 | 1365±474 | |||
| Dietary Fat Intake (%) | |||||||
| Baseline | 38.3±8.1 | 37.4±6.9 | 39.0±6.2 | 38.8±4.9 | 0.38 | <0.001 | 0.04 |
| 6 mo. | 31.2±8.7 | 28.4±5.3 | 28.7±5.4 | 27.8±5.8 | |||
| 24 mo. | 34.5±6.8 | 34.8±5.6 | 33.8±5.7 | 32.1±6.8 | |||
No significant difference between randomization groups based on Chi-Square analysis.
LTPA = Leisure-Time Physical Activity
Figure 4.
Percent Weight Loss for Categories of 24-Month Physical Activity (min/wk) (N=170).
Figure 5.
Percent Weight Loss for Categories of 24-month Physical Activity (kcal/wk) (N = 170).
Table 5.
Differences in Body Weight, Regional Adiposity, and Fitness Subjects Based on Weight loss at 24 Months (N=170).
| Weight Loss at 24 Months |
|||||||
|---|---|---|---|---|---|---|---|
| <0% (N=54) |
0-4.9% (N=33) |
5.0-9.9% (N=36) |
≥10% (N=47) |
Intervention Group Effect |
Time Effect |
Group × Time Effect |
|
| Body Weight (kg) | |||||||
| Baseline | 89.6±12.5 | 88.9±12.9 | 87.0±14.6 | 84.6±12.8 | <0.0001 | <0.001 | <0.001 |
| 6 months | 83.7±11.8 | 81.8±12.5 | 77.4±13.5 | 72.1±12.4 | |||
| 12 months | 86.4±12.2 | 83.3±12.3 | 77.0±13.5 | 69.2±12.1 | |||
| 18 months | 89.5±11.9 | 84.5±11.8 | 79.0±13.6 | 70.2±12.0 | |||
| 24 months | 92.6±12.4 | 86.7±12.4 | 80.6±13.9 | 70.5±12.5 | |||
| Body Mass Index(kg/m2) | |||||||
| Baseline | 33.1±3.9 | 33.1±4.5 | 32.6±4.6 | 32.0±4.1 | <0.0001 | <0.001 | <0.001 |
| 6 months | 30.9±3.6 | 30.4±4.4 | 29.0±4.3 | 27.2±4.3 | |||
| 12 months | 31.9±3.7 | 31.0±4.4 | 28.8±4.3 | 26.2±4.1 | |||
| 18 months | 33.1±3.7 | 31.4±4.2 | 29.6±4.3 | 26.5±4.1 | |||
| 24 months | 34.3±3.9 | 32.2±4.4 | 30.2±4.4 | 26.6±4.2 | |||
| Waist Circumference(cm) | |||||||
| Baseline | 102.0±11.4 | 101.7±10.5 | 99.2±11.7 | 96.9±11.9 | <0.0001 | <0.001 | <0.001 |
| 6 months | 96.1±11.5 | 96.0±11.7 | 92.9±11.6 | 87.3±12.2 | |||
| 24 months | 104.4±11.9 | 100.7±11.6 | 94.3±11.5 | 85.0±11.4 | |||
| Hip Circumference (cm) | |||||||
| Baseline | 117.8±7.8 | 115.5±7.7 | 116.3±10.4 | 114.1±8.9 | <0.0001 | <0.001 | <0.001 |
| 6 months | 112.0±7.0 | 109.5±7.3 | 108.0±10.3 | 103.7±9.4 | |||
| 24 months | 120.1±8.0 | 115.1±7.9 | 112.6±10.4 | 104.0±9.0 | |||
| Waist-to-Hip Ratio | |||||||
| Baseline | 0.86±0.07 | 0.88±0.06 | 0.85±0.07 | 0.85±0.08 | 0.02 | 0.02 | 0.03 |
| 6 months | 0.86±0.08 | 0.87±0.07 | 0.86±0.08 | 0.84±0.07 | |||
| 24 months | 0.87±0.08 | 0.87±0.06 | 0.84±0.07 | 0.82±0.07 | |||
| Sagittal Diameter | |||||||
| Baseline | 23.3±2.6 | 23.1±2.9 | 23.6±3.3 | 23.0±3.1 | <0.0001 | <0.001 | <0.001 |
| 6 months | 22.1±2.3 | 21.7±2.4 | 21.0±2.8 | 20.1±2.8 | |||
| 24 months | 24.3±2.6 | 23.0±2.7 | 21.8±2.5 | 19.2±2.7 | |||
| Fitness (ml/kg/min) | |||||||
| Baseline | 18.8±3.2 | 20.6±3.3 | 19.8±2.5 | 20.0±3.1 | <0.0001 | <0.001 | <0.001 |
| 6 months | 20.8±3.5 | 22.6±3.0 | 22.6±3.4 | 24.0±4.7 | |||
| 24 months | 19.9±2.9 | 22.3±3.9 | 22.8±3.5 | 25.6±4.3 | |||
| Fitness (L/min) | |||||||
| Baseline | 1.8±0.3 | 1.7±0.4 | 1.7±0.3 | 1.7±0.3 | 0.72 | <0.001 | 0.68 |
| 6 mo. | 1.8±0.3 | 1.7±0.4 | 1.7±0.3 | 1.8±0.3 | |||
| 24 mo. | 1.9±0.3 | 1.8±0.4 | 1.8±0.3 | 1.8±0.4 | |||
| Time to Achieve 85% of Maximal Heart Rate (min.) | |||||||
| Baseline | 10.9±3.7 | 12.2±4.3 | 11.1±3.1 | 10.8±3.3 | 0.03 | <0.001 | <0.001 |
| 6 mo. | 13.7±3.4 | 15.8±4.6 | 15.4±3.9 | 15.8±4.0 | |||
| 24 mo. | 11.5±3.3 | 13.5±3.6 | 13.3±3.4 | 14.6±3.5 | |||
Intervention Contact
Attendance at intervention sessions did not differ between the groups. Completion of telephone contacts was significantly higher for the ≥10% weight loss category (81.5±17.0%) compared to the <0% (66.8±18.8%) and 0-4.9% (68.8±13.9%) weight loss categories (p<0.05), but not significantly different than the 5.0-9.9% weight loss category (75.9±13.0%).
LTPA
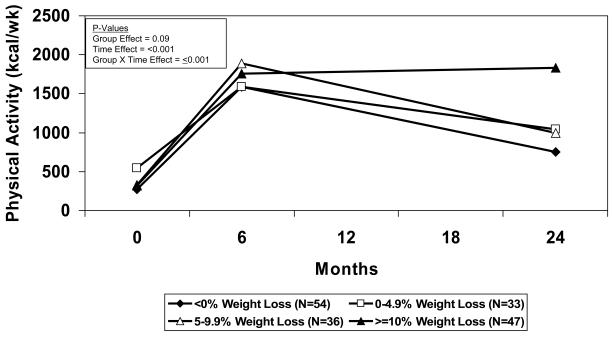
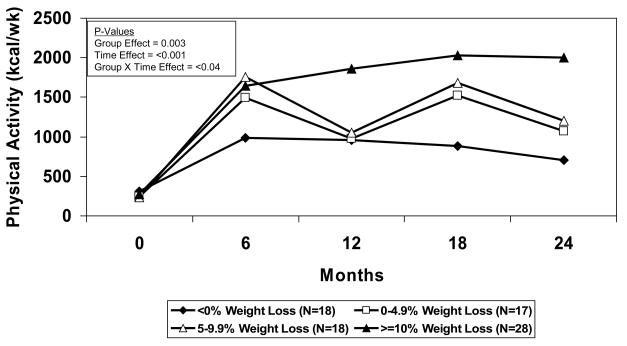
LTPA increased from baseline to 24 months by 1515±1357 kcal/wk in the ≥10% category compared to the 480±779 kcal/wk in the <0% category, 494±1377 kcal/wk in the 0-4.9% category, and 668±1146 kcal/wk in the 5-9.9% category (Group X Time interaction: p≤0.001; Table 4 and Figure 3a and 3b).
Figure 3.
Figure 3a. Physical activity (0, 6, and 24 months) for categories of 24-month weight loss (N = 170).
Figure 3b. Physical activity (0, 6, 12, 18, and 24 months) for categories of 24-month weight loss (N = 81).
Fitness
There was a significant Group X Time interaction (p<0.001) for change in oxygen consumption (ml/kg/min) attained at 85% of age-predicted maximal heart rate between the weight loss categories (Table 4) (N=165). Compared to baseline, the 24 month increase in oxygen consumption was 5.6±3.6 ml/kg/min, 2.9±2.3 ml/kg/min, 1.7±2.8 ml/kg/min, and 1.1±2.9 ml/kg/min in the ≥10%, 5-9.9%, 0-4.9%, and <0% weight loss categories, respectively. There was a significant increase in fitness when expressed in L/min, with no significant difference between groups based on weight loss achieved at 24 months (Table 5).
Energy Intake and Weight Control Eating Behaviors
There was no significant difference between weight loss categories for the pattern of change in energy intake as determine by a non-significant Group X Time interaction (p=0.93). There was a significant Group X Time interaction (p<0.05) for change in weight loss eating behaviors measured by the EBI (Table 4). All groups improved in eating behavior from 0 to 6 months. However, scores at 24 months were 85.6±11.7 in the ≥10% category, 80.2±9.8 in the 5-9.9% category, 73.8±11.7 in the 0-4.9% category, and 74.4±12.1 in the <0% category.
Discussion
Exercise is an important component of weight loss interventions 5, 14. However, few studies examining the specific dose and intensity of exercise that may be required to enhance long-term weight loss have been conducted that exceed 6 to 12 months in duration. Previous results from this study reported that weight loss at 12 months was approximately 10% of initial body weight in response to energy restriction combined with prescription of a high dose of exercise (~2,000 kcal/wk), whereas approximately 8% weight loss was observed in response to energy restriction combined with prescription of a moderate dose of exercise (~1,000 kcal/wk); however, these differences were not statistically significant 6. Prescribed intensity (moderate versus vigorous) did not influence weight loss outcomes, but this may have been a result of lack of adherence to the prescribed intensity over the duration of this study. Unfortunately, the results presented here show that this level of weight loss was not maintained, with a mean weight loss of 5% sustained at 24 months regardless of prescribed dose or intensity of exercise (Figure 2).
Weight regain in this study was approximately 50% of the weight that was achieved following the initial 6 months of the intervention. This approximates the weight regain previously reported in the literature. Wing 4 concluded that weight regain was approximately 43% across a 40 month period following initial weight loss, and similar results have been reported by Perri and Corsica 3.
Analysis based on randomized group assignment did not portray a favorable contribution of exercise on weight loss maintenance. LTPA increased by 1235 kcal/wk from baseline to 6 months; however, only a 720 kcal/wk increase above baseline was sustained at 24 months (Table 2). Moreover, the randomized groups did not sustain the prescribed differences in LTPA, which may have contributed to the non-significant differences in weight loss between these groups. Studies of a similar duration have shown comparable results, with physical activity initially increasing before gradually decreasing over time 7, 21. Thus, the inability to sustain weight loss appears to mirror the inability to sustain physical activity.
When subjects were categorized based on the magnitude of weight loss achieved at 24 months, the importance of physical activity to sustain weight loss became more apparent. Individuals achieving and maintaining a weight loss ≥10% of their initial body weight reported participating in approximately 1800 kcal/wk of LTPA at both 6 and 24 months (Figures 3a, 3, 4, 5). This is approximately 1500 kcal/wk, which corresponds to 275±254 min/wk (55 min/d on 5 d/wk), above the baseline level of LTPA. This level of physical activity is consistent with our previous findings 6, 7, and supports the levels of physical activity that should be targeted for successful weight loss12,14,15,11. The 338 min/wk reported at 24 months approximates 68 min/d on 5 days per week. This would suggest that the level of physical activity that may be necessary to sustain weight loss for as long as 24 months is approximately twice the minimum consensus public health recommendation for physical activity 10, 22. This appears to be consistent with the amount of energy expenditure reported by Schoeller et al. 9 and recommended in the US Dietary Guidelines for prevention of weight regain 11. However, it is important to highlight that this is approximately 1,500 kcal/wk, or 275 min/wk, above baseline activity levels for relatively sedentary overweight adults.
Forty-seven of the 191 subjects (25%) were able to sustain a weight loss of ≥10% at 24 months. In addition to sustaining relatively high levels of LTPA, individuals sustaining ≥10% weight loss at 24 months completing more telephone contacts with the intervention team during months 6-24 (81.5% of contacts completed) compared to individuals achieving <5% weight loss at 24 months (<69% of contacts completed). The ability to sustain a higher level of contact may have contributed to the higher level of LPTA and greater engagement in eating behaviors consistent with weight control reported by these participants (Table 4). Perri and Corsica 3 have recommended that weight loss interventions follow a chronic-care model that sustains contact between the interventionists and participants. The results from this study support this recommendation; however, this contact may not need to be in-person. Wing et al. 23 reported that delivering an 18-month weight loss maintenance intervention via in-person or internet contact significantly reduced the proportion of participants gaining ≥2.3 kg. Marcus et al. 24 reported that non-in-person contact (i.e., internet, print) can be effective at increasing physical activity in sedentary adults.
Compliance to dietary recommendations may also have contributed to improved weight loss at 24 months. Individuals sustaining ≥10% weight loss at 24 months reported engaging in more weight loss eating behaviors, as measured by the EBI, and lower intake of dietary fat compared to individuals sustaining lower levels of weight loss (see Table 4). The failure to detect a difference in total energy intake between those individuals sustaining and not sustaining a 10% weight loss at 24 months may be a result of limitations when using a food frequency questionnaire. Howard et al. 25 reported that compliance to dietary guidelines facilitated the maintenance of a 2.2 kg weight loss over a period of 7.5 years, supporting the importance of also targeting this aspect of energy balance. However, the greater magnitude of weight loss achieved in this current study may be a result of a greater emphasis on reduction in energy intake along with the inclusion of physical activity, both of which were not included in the study conducted by Howard et al. 25.
A potential limitation is that physical activity was based on self-report and not objective techniques to quantify physical activity, which may partially explain the high variability in physical activity reported in this study. Thus, objective assessment of physical activity should be included in future studies which examine this important research question. Moreover, this study did not include a diet only comparison, which prohibits the ability to examine the additive effect of different doses of physical activity above what can be achieved with diet alone. However, this study tested an intervention approach that is recommended by both the National Institutes of Health 5 and the 2005 US Dietary Guidelines 11, which recommends the combination of changes in both eating and physical activity behaviors to reduce body weight. The results of this study are clinically relevant and provide guidance to health-care professionals regarding the magnitude of physical activity that needs to be included in behavioral interventions for weight loss and weight loss maintenance.
An intensive intervention was implemented that required regular contact via in-person or telephone over a period of 24 months. While higher amounts of contact were predictive of long-term weight loss, this amount of contact may not translate to what is permissible in clinical and community interventions. The optimal frequency of contact that can reasonably be provided in these settings to enhance weight loss outcomes needs to be addressed, and this may involve the integration of alternative modes of contact.
This study demonstrated the difficulty in sustaining weight loss of ≥ 10% of initial body weight, with approximately 30% of individuals in this study meeting this criterion at 24 months. However, relatively high levels of physical activity appear to contribute sustained weight loss. In excess of 1,800 kcal/wk of LTPA, which is 1,500 kcal/wk (275 min/wk) above the baseline level for sedentary individuals, appears to be important for sustaining ≥10% weight loss. This clarifies the dose of physical activity that should be targeted for achieving and sustaining this magnitude of weight loss, but also demonstrated the difficulty of sustaining this level of physical activity. Research is needed to improve long-term compliance to this targeted level of physical activity. Moreover, continued contact with the intervention staff and the ability to sustain recommended eating behaviors also may be important contributing factors to sustaining weight loss, suggesting that physical activity does not function independently of these other behaviors for enhancing maintenance of significant weight loss that exceeds 10% of initial body weight.
Acknowledgements
This study was supported by a grant from the National Institutes of Health and the National Heart, Lung and Blood Institute (HL64991). Dr. Jakicic had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The authors also recognize the contribution of staff of the Weight Control and Diabetes Research Center and the Centers for Behavioral and Preventive Medicine at the Miriam Hospital (Providence, RI) and the Physical Activity and Weight Management Research Center at the University of Pittsburgh (Pittsburgh, PA) for their assistance with the intervention, data management, and statistical analysis for this study.
Footnotes
Trial Registration: ClinicalTrial.gov, identifier: NCT00006315
Financial Disclosures:
Dr. Jakicic is on the Scientific Advisory Board for BodyMedia, Inc. and the Calorie Control Council (caloriescount.com). Dr. Marcus, Dr. Lang, and Ms. Janney have no financial interests to disclose.
List of References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophsiology, evaluation, and effect of weight loss. An update of the 1997 American Heart Assocation Scientific Statement of Obesity and Heart Disease from the Obesity Committee on the Council of Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]
- 3.Perri MG, Corsica JA. Improving the maintenance of weight lost in behavioral treatment of obesity. In: Wadden T, Stunkard AJ, editors. Handbook of Obesity Treatment. The Guilford Press; New York: 2002. pp. 357–379. [Google Scholar]
- 4.Wing RR. Behavioral Weight Control. In: Wadden TA, Stunkard AJ, editors. Handbook of Obesity Treatment. The Guilford Press; New York: 2002. pp. 301–316. [Google Scholar]
- 5.National Institutes of Health Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults - The Evidence Report. Obes. Res. 1998;6(suppl.2) [PubMed] [Google Scholar]
- 6.Jakicic JM, Marcus BH, Gallagher KI, Napolitano M, Lang W. Effect of exercise duration and intensity on weight loss in overweight, sedentary women. A randomized trial. JAMA. 2003;290:1323–1330. doi: 10.1001/jama.290.10.1323. [DOI] [PubMed] [Google Scholar]
- 7.Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women: a randomized trial. JAMA. 1999 October 27;282(16):1554–1560. doi: 10.1001/jama.282.16.1554. 1999. [DOI] [PubMed] [Google Scholar]
- 8.Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr. 1997;66:239–246. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- 9.Schoeller DA, Shay K, Kushner RF. How much physical activity is needed to minimize weight gain in previously obese women. Am J Clin Nutr. 1997;66:551–556. doi: 10.1093/ajcn/66.3.551. [DOI] [PubMed] [Google Scholar]
- 10.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the Centers for Disease and Prevention and the American College of Sports Medicine. JAMA. 1995;273(5):402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 11.Department of Health and Human Services and US Department of Agriculture Dietary Guidelines for Americans. 2005 www.healthierus.gov/dietaryguidelines
- 12.Buse JB, Ginsberg HN, Bakris GL, et al. Primary prevention of cardiovascular disease in people with diabetes mellitus. A scientific statement from the American Heart Assocation and the American Diabetes Association. Circulation. 2007;115:114–126. doi: 10.1161/CIRCULATIONAHA.106.179294. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine . Dietary Reference Intakes for Energy, Carbohydrates, Fiber, Fat, Protein and Amino Acids (Macronutrients): A Report of the Panel on Macronutrients, Subcommittees on Upper Reference Levels of Nutrients and Interpretation and Uses of Dietary Reference Intakes, and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. The National Academies Press; Washington, DC: 2002. [Google Scholar]
- 14.Jakicic JM, Clark K, Coleman E, et al. American College of Sports Medicine Position Stand: Appropriate Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults. Med Sci Sports Exerc. 2001;33(12):2145–2156. doi: 10.1097/00005768-200112000-00026. [DOI] [PubMed] [Google Scholar]
- 15.Saris WHM, Blair SN, van Baak MA, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obesity Reviews. 2003;4:101–114. doi: 10.1046/j.1467-789x.2003.00101.x. [DOI] [PubMed] [Google Scholar]
- 16.American College of Sports Medicine . Guidelines for exercise testing and prescription. Lippincott, Williams and Wilkins; Phildelphia, PA: 2005. [Google Scholar]
- 17.Paffenbarger RS, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 18.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25(1):71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 20.O'Neil PM, Currey HS, Hirsch AA, et al. Development and validation of the eating behavior inventory. Journal of Behavioral Assessment. 1979;1(2):123–132. [Google Scholar]
- 21.Dunn A, Marcus B, Kampert J, Garcia M, Kohl H, III, Blair S. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness. JAMA. 1999;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 22.US Department of Health and Human Services . Physical Activity and Health: A Report of the Surgeon General. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; Atlanta: GA: 1996. [Google Scholar]
- 23.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006;355:1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 24.Marcus BH, Lewis BA, Williams DM, et al. A comparison of internet and print-based physical activity interventions. Arch Intern Med. 2007;167:944–949. doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- 25.Howard BV, Manson JE, Stephanick ML, et al. Low-fat dietary program and weight change over 7 years. The Women's Health Initiative Dietary Modification Trial. JAMA. 2006;295(1):39–49. doi: 10.1001/jama.295.1.39. [DOI] [PubMed] [Google Scholar]