Abstract
We report a case of under treated necrotizing fasciitis (NF) in a 65-year-old woman with diabetes misdiagnosed as Mycobacterium ulcerans infection. She came to the Institut Médical Evangélique (IME) with an extensive painful edematous ulcerated lesion on the dorsum of the right foot and ankle. The diagnosis of Buruli ulcer (BU) was based initially on clinical findings and place of residence (Songololo Territory, the largest known focus of BU in Bas-Congo province). Tissue specimens gave negative results for acid-fast bacilli (AFB), culture, and polymerase chain reaction (PCR) for M. ulcerans. Histopathologic analysis revealed marked necrosis of the lower dermis and subcutaneous tissue. No AFB was found. Later, scattered foci of intracellular gram-positive cocci typical of streptococci were seen. Clinicopathologic correlation of these findings strongly supported the diagnosis of NF. This patient shows the difficulties that may be encountered even in known endemic areas in recognizing BU cases purely on clinical findings.
Mycobacterium ulcerans infection, popularly known as Buruli ulcer (BU), has been identified by the World Health Organization (WHO) as a rapidly re-emerging disease.1 The disease often afflicts people who live or work in riverine areas, wetlands, and stagnant bodies of water.2,3 Penetrating trauma to skin is believed by many authorities to introduce the etiologic agent from M. ulcerans-contaminated skin surface, or the penetrating object itself is similarly contaminated.4,5 The trauma may be as slight as a hypodermic injection or as severe as a gunshot or landmine wound. Following inoculation into the skin, M. ulcerans proliferates and elaborates a toxin that causes necrosis of the dermis, panniculus, and fascia.6,7 The usual incubation period of BU ranges from 2 months to several years.5 As required by the Medical Committee of IME, all patients or their responsible relative or guardian must provide informed consent for all diagnostic and treatment procedures and publication of any or all images derived from the management of the patient, including clinical photographs that might reveal patient identity. We report here a case of under-treated necrotizing fasciitis (NF) misdiagnosed on admission to the hospital as an ulcerated edematous lesion of M. ulcerans infection. Onset of disease followed well-documented local trauma to the skin of a resident of Songololo Territory, the largest known focus of BU in the Democratic Republic of Congo (DRC).8
Case Report
A 65-year-old woman with diabetes from the village of Luvuvamu (Songololo Territory, Bas-Congo Province, DRC) came to the hospital of the Institut Médical Evangélique (IME), on September 9, 2002, with an extensive painful edematous ulcerated lesion on the dorsum of the right foot and ankle. Seven days before admission (September 2, 2002), while tilling the soil, a thorn had pierced the skin deeply at this site. The day after this trauma the site of penetration was surrounded by warm and tender swelling. Her daughter, a nurse, immediately took her to the nearby peripheral health center, where she received analgesic and ampicillin therapy for 6 days.
On admission to the hospital laboratory, tests showed neutrophilia, increased erythrocyte sedimentation rate (ESR), and hyperglycemia. Cefoxitin, metronidazole, and ciprofloxacin were administrated for 10 days, with surgical exploration and debridement of devitalized tissue on September 19, 2002. Response to therapy was favorable (Figure 1). A split skin graft was performed 4 weeks later and the patient was discharged from the hospital 58 days after admission (Figure 2).
Figure 1.

Wound after surgical excision and daily wound care several days after admission. This figure appears in color at www.ajtmh.org.
Figure 2.
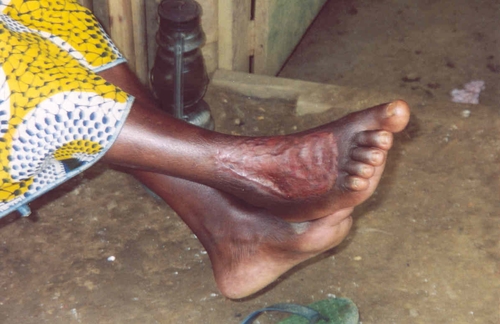
Patient in her village several weeks after discharge from hospital. Note good healing without cicatricial retraction. This figure appears in color at www.ajtmh.org.
The diagnosis of BU was based initially on clinical findings, place of residence, and of the report of rare acid-fast bacilli (AFB) in the Ziehl-Neelsen (ZN) stained smears. Culture and polymerase chain reaction (PCR) tests for M. ulcerans were not available locally. Cultivation for bacteria was not performed because the patient had already received antibiotics. Tissue specimens, however, were submitted to the Mycobacteriology laboratory of the Institute of Tropical Medicine (ITM), in Antwerp. Smears, culture, and PCR for M. ulcerans were tested and gave negative results for AFB and M. ulcerans.9 Histopathologic analysis of formalin-fixed tissue performed at the Armed Forces Institute of Pathology (AFIP) revealed marked necrosis of the lower dermis and subcutaneous tissue, with numerous acute and a few chronic inflammatory cells (Figure 3). No AFB was found.
Figure 3.
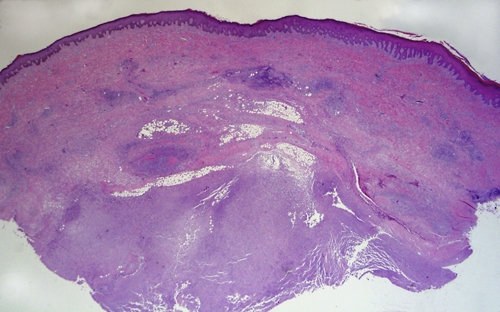
Full thickness section of skin from near the edge of the ulcer, showing inflammation and necrosis, most marked in the deep areas of the panniculus. H&E, ×3. This figure appears in color at www.ajtmh.org.
Initially, the histopathologic findings were interpreted as nonspecific acute and chronic inflammation with necrosis (Figure 4). Buruli ulcer was not ruled-out. Later, the specimen was studied exhaustively and scattered foci of intracellular gram-positive cocci were seen in Brown-Brenn stained sections (Figure 5). Silver staining showed numerous carcasses of coccal forms (Figure 6). In the lower dermis and panniculus there was vasculitis of small vessels, with dense neutrophilic infiltrates, a few lymphocytes, and thrombi (Figure 7). Clinicopathologic correlation of these findings strongly supported the diagnosis of NF. The morphology of the bacteria was interpreted as typical of streptococci.
Figure 4.
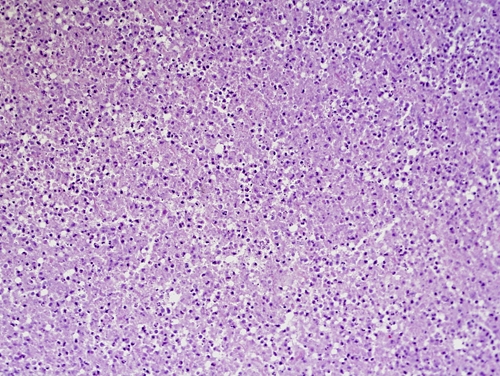
Parallel section of panniculus of specimen in Figure 3. Note heavy infiltration of neutrophils mixed with a few lymphocytes, and necrosis. H&E, ×75. This figure appears in color at www.ajtmh.org.
Figure 5.
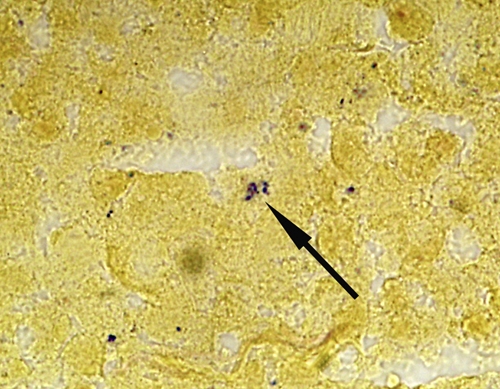
Brown-Brenn stained parallel section of area in Figure 4, showing gram-positive cocci in a small cluster (arrow). There were similar cocci, singly and in clusters, widely scattered in the panniculus (see Figure 6), ×330. This figure appears in color at www.ajtmh.org.
Figure 6.
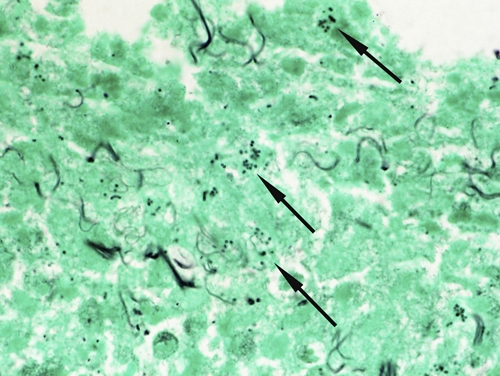
Gomori's methenamine-silver stained parallel section of area in Figure 6 showing many silvered bodies interpreted as carcasses of cocci (arrows). GMS, ×330. This figure appears in color at www.ajtmh.org.
Figure 7.
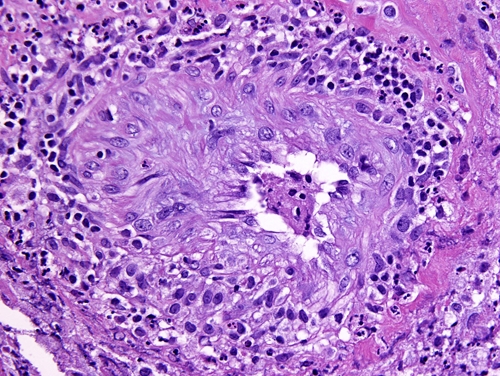
Vasculitis of small vessels in a parallel section of Figure 3. Note dense neutrophilic infiltrates, a few lymphocytes and thrombus. H&E, ×75. This figure appears in color at www.ajtmh.org.
Discussion
The initial BU diagnosis was suspected on clinico-epidemiological features. The patient lived in an endemic region, and the lesion was extensive, located on a lower limb, minimally painful, edematous, and ulcerated, whereas NF classically presents acutely with pain, fever, and systemic toxicity, often with minimal clinical cutaneous findings. Necrotizing fasciitis can extend to cutaneous structures, causing vasculitis and thrombosis, skin discoloration, crepitus, anesthesia, and bulla formation.10 Erythema and edema frequently appear early. Pain disproportionate to local findings may be present and should be a clue to consider NF.11–14 In our patient, ampicillin therapy prescribed in the village probably significantly modified the initial clinical picture. Moreover, we presume that antibiotic therapy had rendered many gram-positive organisms nonstainable by the Brown-Brenn method. Common features of M. ulcerans infection and NF are compared in Table 1. We also have added features of tropical phagedenic ulcer (TPU), an acute or chronic skin disease frequently seen in BU endemic areas15,16 and misdiagnosed as BU.17 Tropical phagedenic ulcer, mostly solitary,18 is characterized by necrosis of the epidermis and underlying superficial tissue.16,19
Table 1.
Comparison of common features of Buruli ulcer, necrotizing fasciitis, and tropical phagedenic ulcer (TPU)*
| Buruli ulcer | Necrotizing fasciitis | Tropical phagedenic ulcer | |
|---|---|---|---|
| Epidemiology | Focal in the tropics | Cosmopolitan | Mostly tropical |
| Most frequent, host age, and comorbidities | More frequent in children 15 or younger | All ages, diabetes, HIV, immunosuppression, and peripheral vascular diseases | Children and young adults malnutrition, anemia, poor hygiene |
| Clinical features | |||
| Body distribution | More frequent on limbs | Non-selective | Most commonly on lower limbs (mostly lateral malleolus) |
| Trauma related | Frequently | Frequently | Frequently |
| Odor | No | Malodorous | Strongly malodorous |
| Onset | |||
| Slow (2–3 months) | Rapid (1–2 days) | Relatively rapid (2 weeks to 1–2 months) | |
| Lesion type | Nodule, or plaque, or edema ulcer | Swelling, ulcer | Ulcer, red violaceous in color |
| Pain | Non-tender, relatively painless | Tender, painful | Tender, painful |
| Skin temperature | Normal | Warm | Normal |
| Erythema | No | Yes | No |
| Systemic signs | None | Systemic toxicity fever ® shock | None |
| Etiology | Mycobacterium ulcerans | Polybacterial | Polybacterial |
HIV = human immunodeficiency virus.
On admission to the hospital, the BU diagnosis was also based on the ZN staining done at IME, which showed rare AFB. These results, however, could not be confirmed on tissue specimens analyzed at the ITM. Other studies on smear microscopy in tuberculosis concluded that a smear result of ≤ 3 AFB is unreliable20 and that single smear-positive results require confirmation by another examination. We therefore believe the IME report of AFB was a false-positive result.
A study done on BU patients hospitalized at IME from May 2002 to August 2004 showed that the median delay in seeking medical attention was 60 days for all clinical forms.21 Often BU patients do not remember the time of onset of the disease. However, those who have had specific trauma at the site where the lesion developed are often able to recall the circumstances more precisely. Published data from such patients indicate that incubation periods range from 2 weeks to 3 years with a mean of 2 to 3 months.4,5,22,23
A study of six patients diagnosed with NF and treated in the Department of Surgery, University College Hospital, in Ibadan, Nigeria, between January 1998 and December 2001, showed that the duration of symptoms ranged between 3 and 14 days.24 The 7 day delay for our patient between the skin trauma and presentation to IME medical center is therefore more compatible with NF than with BU, as well as the reported edema on the day after this trauma. Diabetes, trauma, and old age frequently play a role in the rapid spread of NF.
Necrotizing fasciitis is commonly caused by a group A streptococcus, (Streptococcus pyogenes), but a variety of aerobic and anaerobic organisms have been reported.10–14,25
Abnormal inflammatory tests are frequent in cases of NF. Laboratory tests in our case showed a neutrophilia and increased ESR. In Bas-Congo, superinfection of skin ulcers by other bacterial species was found in 52.8% of BU patients, with similar abnormal inflammatory tests.21
It is generally believed that in endemic areas, the experienced health worker usually can make an accurate presumptive diagnosis of BU on clinical grounds alone, or by using a combination of clinical features and a positive ZN staining.9 Laboratory confirmation of clinically suspected BU cases, however, is highly recommended. Indeed, several studies on the microbiological confirmation of clinically suspected cases of BU showed that up to 70% of clinically suspected cases cannot be confirmed by microbiological tests.9,26 Moreover, clinicians must remember that misdiagnosis of BU can require the patient to receive 8 weeks of antibiotic therapy with a combination of oral rifampicin and an intramuscular aminoglycoside (usually streptomycin) under direct observation.27
Our patient healed well with a combination of antibiotics, surgery, and daily wound dressings followed by skin graft (Figure 2). Our case illustrates the importance of early detection and adequate management of NF, and any other significant tropical skin disease such as TPU or BU. Effective collaboration between peripheral health centers and reference hospitals is of utmost importance.
In conclusion, this patient shows the difficulties that may be encountered, even in known endemic areas, in recognizing BU cases purely on clinical findings.
Acknowledgments
We thank the staff of the Institut Médical Evangélique in Kimpese and the staff of the Mycobacteriology Unit of the Institute of Tropical Medicine in Antwerp for patient care and microbiologic analyses. We also thank Esther K Meyers for her outstanding work in preparation of the manuscript.
Footnotes
Financial support: This study was supported by the European Commission (International Science and Technology Cooperation Development Program), Project No. INCO-CT-2005-05-051476-BURULICO.
Authors' addresses: Mavinga D. Phanzu, Aombe E. Bafende, and Bofunga B. D. Imposo, Institut Médical Evangélique (IME), Kimpese, Bas-Congo, Democratic Republic of Congo, E-mails: dmavingaphanzu@yahoo.fr, eric.bafende@sam-ame.org, and imposodesire@yahoo.fr. Wayne M. Meyers, Armed Forces Institute of Pathology (AFIP), Washington, DC, E-mail: wmekmeyers@comcast.net. Françoise Portaels, Institute of Tropical Medicine (ITM), Antwerp, Belgium, E-mail: portaels@itg.be.
References
- 1.World Health Organization . In: Buruli ulcer: Mycobacterium ulcerans infection. Asiedu K, Scherpbier R, Raviglione M, editors. Geneva: World Health Organization; 2000. [Google Scholar]
- 2.Walsh DS, Portaels F, Meyers WM. Review: Buruli ulcer (Mycobacterium ulcerans infection) Trans R Soc Trop Med Hyg. 2008;102:969–978. doi: 10.1016/j.trstmh.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 3.Aiga H, Amano T, Cairncross S, Domako JA, Nanas OK, Coleman S. Assessing water-related risk factors for Buruli ulcer: a case-control study in Ghana. Am J Trop Med Hyg. 2004;71:387–392. [PubMed] [Google Scholar]
- 4.Debacker M, Zinsou C, Aguiar J, Meyers WM, Portaels F. First case of Mycobacterium ulcerans disease (Buruli ulcer) following a human bite. Clin Infect Dis. 2003;36:e67–e68. doi: 10.1086/367660. [DOI] [PubMed] [Google Scholar]
- 5.Meyers WM, Shelly WM, Connor DH, Meyers EK. Mycobacterium ulcerans infections developing at sites of trauma to skin. Am J Trop Med Hyg. 1974;23:919–923. doi: 10.4269/ajtmh.1974.23.919. [DOI] [PubMed] [Google Scholar]
- 6.Abalos FM, Aguiar J, Guédénon A, Portaels F, Meyers WM. Mycobacterium ulcerans infection (Buruli ulcer): a case report of the disseminated nonulcerative form. Ann Diagn Pathol. 2000;4:386–390. doi: 10.1053/adpa.2000.19372. [DOI] [PubMed] [Google Scholar]
- 7.Portaels F, Silva MT, Meyers WM. Buruli ulcer. Clin Dermatol. 2009;27:291–305. doi: 10.1016/j.clindermatol.2008.09.021. [DOI] [PubMed] [Google Scholar]
- 8.Meyers WM, Connor DH, McCullough B, Bourland J, Moris R, Proos L. Distribution of Mycobacterium ulcerans infection in Zaïre, including the report of new foci. Ann Soc Belg Med Trop. 1974;54:147–157. [PubMed] [Google Scholar]
- 9.World Health Organization . In: Buruli Ulcer: Diagnosis of Mycobacterium ulcerans disease. Portaels F, Johnson P, Meyers WM, editors. Geneva: World Health Organization. WHO/CDS/CPE/BBUI/2001.4; 2001. [Google Scholar]
- 10.Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL. 15th Edition Harrison's Manual of Medicine. Vol. 176. New York: McGraw-Hill; 2001. pp. 180–378. [Google Scholar]
- 11.Dahl PR, Perniciaro C, Holmkvist KA, O'Connor MI, Gibson LE. Fulminant group A streptococcal necrotizing fasciitis: clinical and pathological findings in 7 patients. J Am Acad Dermatol. 2002;47:489–492. doi: 10.1067/mjd.2002.120536. [DOI] [PubMed] [Google Scholar]
- 12.Hasham S, Matteucci P, Stanley PR, Hart NB. Necrotising fasciitis. Br Med J. 2005;330:830–833. doi: 10.1136/bmj.330.7495.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smeets L, Bous A, Heymans O. Necrotizing fasciitis: case report and review of literature. Acta Chir Belg. 2007;107:29–36. doi: 10.1080/00015458.2007.11680007. [DOI] [PubMed] [Google Scholar]
- 14.Angoules AG, Kontakis G, Drakoulakis E, Vrentzos G, Granick MS, Giannoudis PV. Necrotising fasciitis of upper and lower limb: a systematic review. Injury. 2007;38S:S18–S25. doi: 10.1016/j.injury.2007.10.030. [DOI] [PubMed] [Google Scholar]
- 15.Fleming RA. The causes, pathologic aspects and treatment of phagedenic ulcer in West Africa. J Int Coll Surg. 1962;38:120–128. [PubMed] [Google Scholar]
- 16.Robinson DC, Adriaans B, Hay RJ, Yesudian P. The clinical and epidemiologic features of tropical ulcer (tropical phagedenic ulcer) Int J Derm. 1988;27:49–53. doi: 10.1111/j.1365-4362.1988.tb02339.x. [DOI] [PubMed] [Google Scholar]
- 17.Janssens P, Pattyn S, Meyers WM, Portaels F. Buruli ulcer: an historical overview with updating to 2005. Bull Seances Acad R Sci Outre Mer. 2005;51:265–299. [Google Scholar]
- 18.Bulto T, Maskel FH, Fisseha G. Skin lesions in resettled and indigenous populations in Gambela, with special emphasis on the epidemiology of tropical ulcer. Ethiop Med J. 1993;31:75–82. [PubMed] [Google Scholar]
- 19.Tumwine JK, Dungare PS, Tswana SA, Maoneke WR. Tropical ulcers in a remote area in Zimbabwe. Cent Afr J Med. 1989;35:413–416. [PubMed] [Google Scholar]
- 20.Van Deun A, Hamid Salim A, Cooreman E, Daru P, Das AP, Aung KJ, Rieder HL. Scanty AFB smears: what's in a name? Int J Tuberc Lung Dis. 2004;8:816–823. [PubMed] [Google Scholar]
- 21.Phanzu MD, Bafende AE, Imposo BB, Dunda KB, Nsiangana ZS, Kibadi KA, Singa NJ, Meyers WM, Portaels F. Mycobacterium ulcerans disease (Buruli ulcer) in a rural hospital in Bas-Congo, Democratic Republic of Congo, 2002–2004. Am J Trop Med Hyg. 2006;75:311–314. [PubMed] [Google Scholar]
- 22.Debacker M, Aguiar J, Steunou C, Zinsou C, Meyers WM, Guédénon A, Scott JT, Dramaix M, Portaels F. Mycobacterium ulcerans disease (Buruli ulcer) in a rural hospital, Southern Benin, 1997–2001. Emerg Infect Dis. 2004;10:1391–1398. doi: 10.3201/eid1008.030886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van der Werf TS, van der Graaf WTA, Tappero JW, Asiedu K. Mycobacterium ulcerans infection. Lancet. 1999;354:1013–1018. doi: 10.1016/S0140-6736(99)01156-3. [DOI] [PubMed] [Google Scholar]
- 24.Ogundiran TO, Akute OO, Oluwatosin OM. Necrotising fasciitis. Trop Doct. 2004;34:175–178. doi: 10.1177/004947550403400320. [DOI] [PubMed] [Google Scholar]
- 25.Cox NH. Streptococcal necrotizing fasciitis and the dermatologist. Br J Dermatol. 1999;141:613–614. doi: 10.1046/j.1365-2133.1999.03097.x. [DOI] [PubMed] [Google Scholar]
- 26.Siegmund V, Adjei O, Nitschke J, Thompson W, Klutse E, Herbinger KH, Thompson R, van Vloten F, Racz P, Fleischer B, Loescher T, Bretzel G. Dry reagent-based polymerase chain reaction compared with other laboratory methods available for the diagnosis of Buruli ulcer disease. Clin Infect Dis. 2007;45:68–75. doi: 10.1086/518604. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization . Provisional guidance on the role of specific antibiotics in the management of Mycobacterium ulcerans disease (Buruli ulcer) Geneva: World Health Organization; 2004. WHO/CDS/CPE/GBUI/2004.10. [Google Scholar]


