Abstract
Objective
The purpose of this study was to assess the feasibility of a standardized test of gaze stabilization as an indicator of vestibular function in community-dwelling older adults and to examine the relationship between gaze stabilization and physical performance.
Design
Descriptive, Cross-sectional.
Setting
Tertiary Medical Center.
Subjects
Eighty-six healthy older adults (22 males) of mean (SD) age 76.8 (5.8) years were recruited from the Pittsburgh community.
Main Outcome Measures
Performance on the gaze stabilization test (GST), measures of physical performance (standing balance, chair rises, and gait speed individually and combined into the Short Physical Performance Battery (SPPB)) and self-reported balance.
Results
While over 90% of participants completed testing in the pitch and yaw planes, only 85% (73/86) had interpretable scores, due to prolonged perception time, independent of VOR. The mean (SD) head movement velocity in the pitch plane was 94.5 (26.7) degrees per second and in the yaw plane was 95.5 (29.3) degrees per second. There was a strong association between age and GST performance in the pitch and yaw planes (r=0.68, p<0.001). Poor GST performance in the yaw plane was associated with balance capacity with eyes closed. Additionally, there was a trend toward an association between self-reported balance and GST performance in both pitch (p=0.08) and yaw planes (p=0.10).
Conclusions
While most older adults completed GST testing, estimates were not interpretable in almost 15% due to prolonged perception time. GST in the yaw plane was worse than previously reported in healthy older adults and was associated with poor ability to balance with eyes closed. Self-reported balance tended to be associated with an objective assessment of VOR in this population of older adults.
INTRODUCTION
Balance declines with increasing age, contributes to increased risk of falls (1), and is consequently a frequent source of morbidity and mortality in older adults (2,3). While large studies of balance in older adults have assessed measures of vision and standing balance, none have used a performance-based functional test of vestibulo-ocular function. Numerous studies have identified a decline of vestibulo-ocular function with aging, but have not studied associations between vestibular functional decline and physical performance measures of mobility and balance (4–9). This decline in vestibular function appears to occur without symptoms of disequilibrium (6).
The gaze stabilization test (GST) was designed as a clinical test of vestibular function. The test assesses how quickly the head can be moved while maintaining focus on a computer-based target, thus theoretically providing an estimate of vestibulo-ocular reflex (VOR) function. Prior work using the gaze stabilization test has focused on its potential as a diagnostic tool for vestibular disorders (10–13). Patients with vestibular dysfunction have been shown to have reduced scores on the GST, requiring slower head movements to correctly identify an optotype of the same size as compared to healthy controls (10). The GST has been found to be highly reliable for diagnosing patients with unilateral vestibular deficits (10).
While the use of the GST in patients with unilateral vestibular loss has been explored, less is known about the role of the GST in healthy older adults. While vestibular function is known to decrease with age, the relationship between vestibular function decline and physical performance is not clear. The purpose of this study is to assess the feasibility of a standardized test of gaze stabilization as an indicator of vestibular function in community-dwelling older adults and to examine the relationship between gaze stabilization and physical performance. The authors hypothesized that physical performance measures of standing balance would correlate with performance on the GST.
MATERIALS AND METHODS
Subjects
Subjects were recruited to a parent study of physical performance measure from a registry of older adult volunteers. Of 120 subjects who were in the parent study, 86 attempted the gaze stabilization test. The study was approved by the institutional review board at the University of Pittsburgh and all participants provided consent.
For inclusion in the parent study, participants had to be age 65 or older, self-report an ability to tolerate a 5-hour battery of performance measures, and ability to walk 50 feet with or without an assistive device. Exclusion criteria for this study included neuromuscular disorders that impair movement (such as Parkinson Disease, stroke, or multiple sclerosis), cancer with active treatment, severe pulmonary disease, or chest pain or cardiac event within the last 6 months.
Physical Performance Measures
Measures from the parent study that were used in this substudy include the Short Physical Performance Battery (SPPB) and separate tests of balance, gait speed, and chair rises. The SPPB consists of: 1) the ability to maintain stance for 10 seconds in three progressively more difficulty foot positions, 2) a timed 4 meter walk and 3) time to rise from a chair 5 times. Each of the three tasks is scored 0–4, for an overall score range of 0–12 points (14). The test-retest reliability of the SPPB is excellent, with Intraclass correlation coefficients (ICC) ranging from 0.88 to 0.92 (15).
More detailed performance tests were performed for standing balance, gait speed and chair rise. The standing balance test of the SPPB was expanded from 10 to 30 second tests, assessments of all positions with eyes closed and added one foot standing. An overall score for standing balance with eyes closed was calculated by summing the maximum stance time in seconds in each of the four balance tasks (tandem, side-by-side, left foot only and right foot only). Walking speed was performed just as for the SPPB, but calculated as velocity in meters per second rather than the 0 to 4 score. The chair rise test was assessed as number of stands completed in 15 seconds, with arms folded across the chest. In addition, participants were asked to rate their balance as a categorical variable such as “excellent,”“very good,” “good,” “fair,” and “poor”.
Gaze Stabilization Test
Participants completed tests of static visual acuity, minimum perception time and the Gaze Stabilization test (GST) in both pitch and yaw planes. Participants were seated 1.5m from a computer screen and allowed to wear their glasses during testing. Static visual acuity was determined by presenting optotypes (letter E) on the computer screen of varying sizes based on the participant’s accuracy on the most recent trial. An optotype E was presented on the computer screen oriented in one of four directions (up, down, left, right). Participants declared the direction the optotype was pointing. Visual acuity was defined as the smallest optotype that was correctly identified twice. The minimum perception time is the minimum time an optotype can be presented on the screen so that the participant can still accurately identify it. Participants focused on a box that would appear in the center of the computer screen for 2 s. The box disappeared and after 200 ms, an ‘E’ optotype 0.2 logMAR or two lines of visual acuity above the subject’s SVA appeared in its place for a variable amount of time. Participants were asked to identify the orientation of the optotype. The gaze stabilization test (GST) is a functional test of the vestibulo-ocular reflex (VOR). A 3-axis integrating gyro that determines head turning velocity is mounted on a headband and worn by participants. Participants rotate their head horizontally (in the yaw plane) or vertically (in the pitch plane) while maintaining a fixed gaze on the computer screen. When the participant’s head movement meets the required minimum head velocity for the trial, an optotype E is presented on the computer screen oriented in one of four directions. The subject is required to identify the direction the optotype is pointing. The optotype size is fixed at 0.2 logMAR or two lines of visual acuity above the participant’s SVA. The duration of presentation is set at 35 ms longer than the subject’s minimum perception time performance if the minimum perception time is at least 40 ms. If the minimum perception time is less than 40 ms, the maximum duration of presentation is set at 75 ms. The outcome recorded for the GST is the mean of the three fastest head velocities at which the participant can move their head and still correctly identify a transient optotype target (letter E).
Statistical Analysis
Cross-sectional analyses of baseline data were conducted using STATA (version 9, STATA corp., College Station, Texas). Gaze stabilization test scores were examined as a continuous variable using the average score in degrees/second for left and right to determine horizontal scores and up and down to determine vertical scores. Short physical performance battery, age, 15-second sit to stand, standing balance tasks, and gait speed were also assessed as continuous variables. Scatter plots were examined to assess associations. Pearson correlation coefficients were used to determine the association between physical performance measures and the gaze stabilization test. Multiple linear regression models were used to assess the effect of GST performance on physical performance measures after adjusting for age and gender. Spearman correlation coefficients were used to assess the relationship between self-reported balance and GST performance in pitch and yaw planes. A p-value of 0.05 was used to determine significance.
RESULTS
Of the 120 participants in the parent study, 86 attempted gaze stabilization testing. Their mean age (SD) was 76 (5.8) years with a range of 65–92 years, and 22 were men. Mean (SD) GST performance in the pitch plane was 94.5 (26.7) degrees per second and in the yaw plane was 95.5 (30.5) degrees per second. Women tended to have faster GST scores than men in the pitch plane, but these differences were not significant. The participants had a mean SPPB total score of 10.1 (2.03), indicating relatively good physical function. Mean (SD) gait speed for this population was 0.99 (0.2) m/s (Table 1).
Table 1.
Characteristics of the Study Participants
| Characteristics | Interpretable GST scores (n=73) |
GST scores <90 degrees/second in either plane (n=39) |
All (n = 86) | |
|---|---|---|---|---|
| Age, y (SD) | *76.5 (5.7) | *78.3 (5.7) | 76.8 (5.8) | |
| GST (yaw), deg/s (SD) | 98.8 (29.7) | 77. 8 (20.8) | 95.5 (29.3) | |
| GST(pitch), deg/s (SD) | 96. 9 (26.9) | 78. 4 (19.2) | 94.5 (26.7) | |
| SPPB (Total) (SD) | 10. 2 (1.9) | 9. 8 (2.3) | 10.1 (2.0) | |
| Gait speed, s (SD) | 0.98 (0.2) | 0.95 (0.2) | 0.98 (0.2) | |
| 15-second chair rises, number (SD) | 6.9 (2.1) | 6. 5 (1.7) | 7.0 (2.0) | |
| Standing balance, s (SD) | 71.3 (27.6) | 68.2 (26.7) | 69.2 (27.8) | |
| Romberg, s (SD) | 29.3 (3.8) | 29. 6 (2.4) | 29.3 (3.7) | |
| Tandem, s (SD) | 22.8 (11.1) | 21.9 (12.4) | 22.3 (11.2) | |
| Single leg stance (left), s (SD) | 10. 4 (10.6) | 9.9 (10.6) | 10.0 (10.4) | |
| Single leg stance (right), s (SD) | 8.8 (9.7) | 6.6 (7.7) | 8.4 (9.6) | |
| Self-reported balance (SD) (‘1’ is excellent, ‘5’ is poor) |
3.2 (0.9) | 3.4 (1.0) | 3.2 (0.9) | |
GST = gaze stabilization test, SPPB = short physical performance battery
indicates statistical significance at p < 0.05
Of 86 participants, 81 (94%) completed testing in the yaw plane and 78 (91%) completed testing in the pitch place. One subject could not achieve the minimum head velocity required for the gaze stabilization test. GST scores were considered not interpretable if the minimum perception time exceeded 80 milliseconds, because scores above this threshold would lead to dwell times that would allow the subject to make a corrective saccade and therefore would no longer isolate VOR performance (16). Twelve subjects were defined as having unreliable GST scores in the yaw and pitch planes due to prolonged minimum perception time. Therefore, 73 out of 86 participants were included in the analysis.
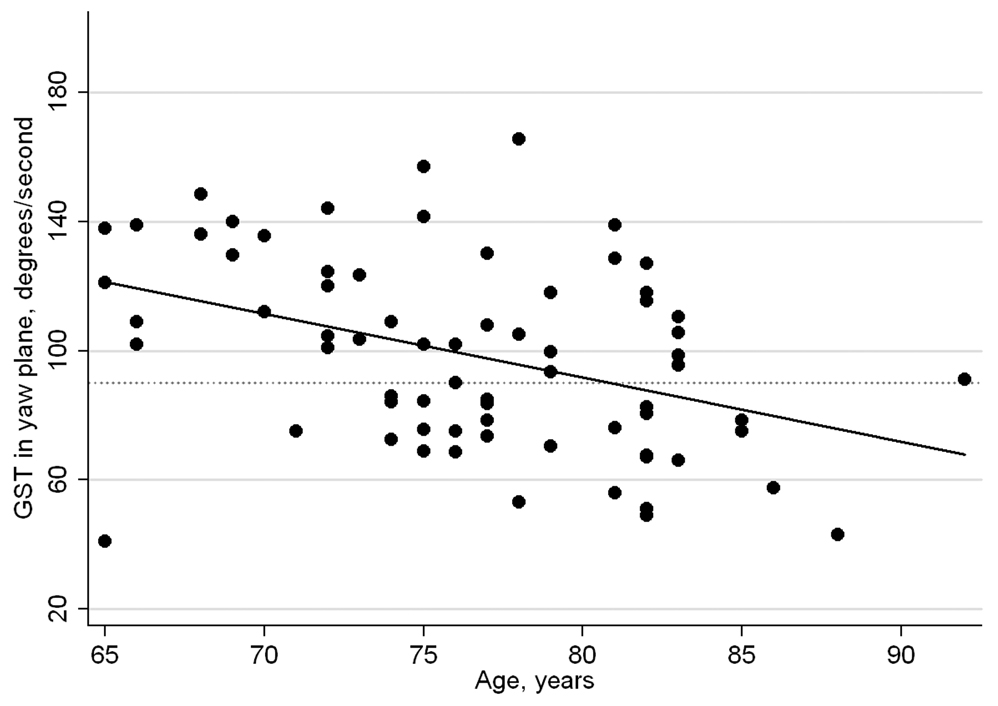
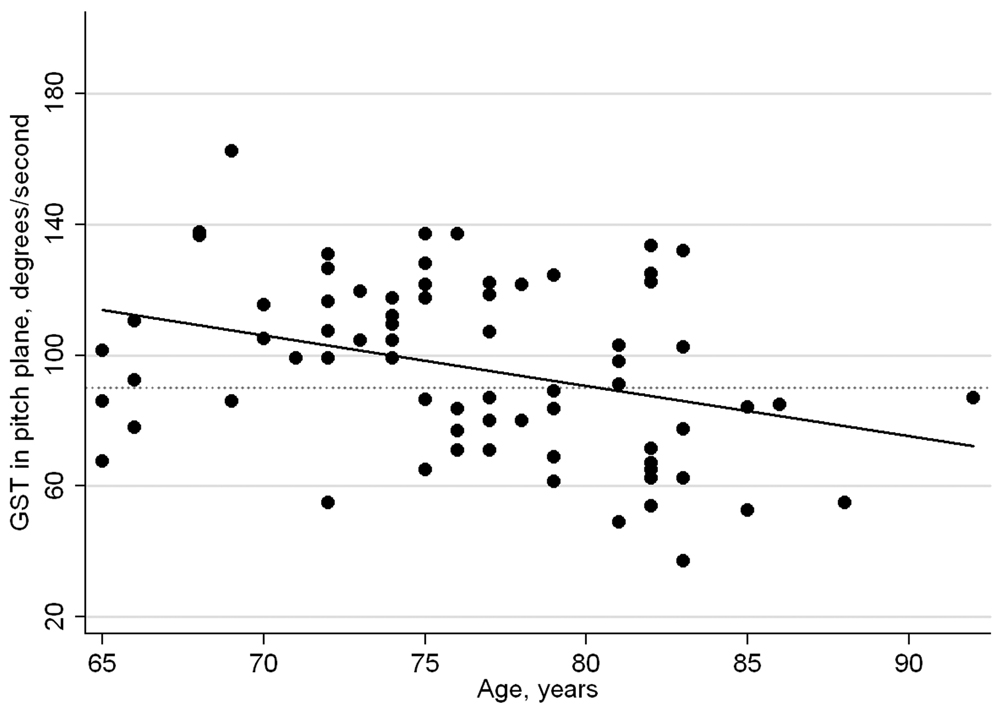
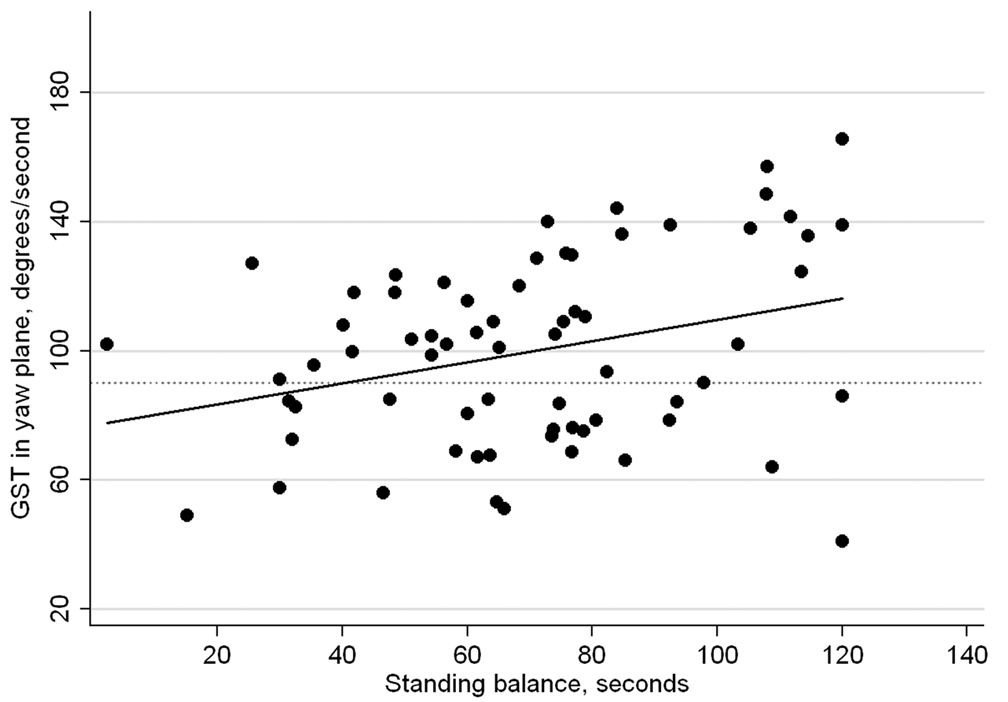
Table 1 demonstrates results from the GST in the 73 subjects. GST scores in both the pitch and yaw planes were significantly correlated with each other (r=0.68, p<0.001) and were significantly inversely associated with age (p<0.001), indicating poorer performance with increasing age. The distribution of GST performance in the pitch and yaw planes by age is shown in Figures 1A and 1B. In univariate analyses, GST performance in the yaw plane was significantly associated with the SPPB (p<0.05), gait speed (p<0.05), 15-second sit to stand and standing balance (p<0.01). After adjusting for age and gender, only standing balance remained significant (p<0.01) (Figure 1C). GST in the pitch plane was associated only with 15-second sit to stand (p=0.01) and this relationship remained significant after adjusting for age and gender (p=0.01).
Figure 1.
A, B, and C, Scatter Plots of Gaze Stabilization Test (GST) performance in yaw and pitch planes by age and GST performance in the yaw plane by standing balance. A reference line is drawn at a GST score of 90 degrees per second.
Thirty-three of 86 subjects (38%) were unable to generate an average GST score in either the pitch or the yaw plane greater than 90 degrees/second (Table 2). Those who were unable to generate this minimum head velocity in either plane were significantly older (79.4 years vs. 75.2 years), had a slower gait speed (0.92 m/s vs. 1.02 m/s) and worse SPPB (9.5 vs. 10.5) than those able to achieve this threshold (p<0.05).
Table 2.
Physical Performance in older adults with normal and reduced GST scores in either the pitch or yaw planes.
| Above 90deg/s | Below 90deg/s | |
|---|---|---|
| Age, years (SD) | 75.2 (5.9)* | 79.4 (4.8)* |
| SPPB (0–12) (SD) | 10.5 (1.6)* | 9.5 (2.5)* |
| Gait Speed, m/s (SD) | 1.02 (0.2)* | 0.92 (0.2)* |
| 15-second sit to stand, # (SD) |
7.1 (2.1) | 6.6 (2.1) |
| Standing Balance, s (SD) | 72.2 (28.0) | 66.2 (25.3) |
| Self-Reported balance (SD) | 3.0 (0.8)* | 3.4 (1.0) * |
indicates statistical significance at p < 0.05
Of the 73 subjects with interpretable GST scores, there was a trend toward an association between self-reported balance and GST performance in both pitch (p=0.08) and yaw planes (p=0.10). Participants with higher GST scores tended to report better balance than those with lower scores.
DISCUSSION
This study suggests that the ability to see clearly during head rotation is significantly reduced in some older adults, and that those with reduced GST performance also have reduced mobility and balance. Maximum VOR demands during walking in healthy younger adults have been reported at 90 degrees per second; therefore, a significant proportion of older adults may have difficulty with visual stabilization during usual ambulation (17,18). Since there are no studies of the VOR demands of older adults during routine tasks, this threshold may overestimate the VOR requirements in this age group. Nevertheless, older adults who scored below this threshold in one or more directions in this study had more physical performance impairments than those who exceeded this value.
The GST performance of older adults in this study is worse than that reported in prior studies of healthy adults or older adults (10,12,13). In 14 healthy adults with a mean age of 45.8 years, Goebel et al. (10) reported average GST scores in the yaw plane of 147 degrees/second. In 20 healthy older adults (mean age 70) Whitney et al. (12) noted average GST scores in the yaw plane of 126 degrees/second and 101 degrees/second in the pitch plane. Our findings of GST scores in the yaw plane of 95.5 degrees per second are considerably lower than those reported in these prior studies, while our findings of 94.5 in the pitch plane are somewhat similar to Whitney et al (12). We believe that the worse performance is attributable to the more advanced age and diverse health status of our population.
This study has shown an association between standing balance times with eyes closed and GST performance after adjusting for age and gender. This relationship indicates that the GST is likely assessing vestibular function. With eyes closed, only proprioceptive and vestibular input would be contributing to maintenance of standing balance. Since performing the GST involves little proprioceptive function, we assume that this association indicates that the GST is therefore measuring vestibular function.
In addition, the association seen between GST performance in the pitch plane and number of chair rises in a 15 second period may be attributed to an age-related decrement in physical performance measures not assessed by this study. An alternative, but less likely explanation is that head rotation during sit-to-stand movements may cause images to slip on the retina or oscillopsia. Both GST assessments in the pitch plane and sit to stand movements stimulate the otolith organs and posterior and anterior semicircular canals. Since subjects were asked to rise from a seated position as many times as possible in 15 seconds, those whose maximum pitch head velocity was exceeded by the required rapid vertical movements may have experienced oscillopsia and a subjective feeling of dizziness, leading to decreased motivation to rise quickly from the seated position. While this explanation is less likely than a multi-system decline associated with aging, subjective symptoms of visual blurring and dizziness may be assessed in future studies to better identify subjective reasons for poorer physical performance.
This study did detect a trend toward a relationship between self-reported balance and GST performance in older adults. Those older adults who rated their balance as ‘excellent’ tended to have higher GST scores as compared to those who rated their balance as ‘fair’ or ‘poor’. While this study was unable to determine causality, a decline in VOR function as measured by the GST may be interpreted by the participant as a loss of balance. Future studies could further explore this relationship over time with more rigorous balance surveys.
In their recent study using the GST in a population of healthy older adults and adults with vestibular dysfunction, Whitney et al. (12) noted a correlation between the ‘Timed Up and Go’ test and Dynamic Gait Index (DGI) scores and GST performance only in those with vestibular disorders, but not healthy older adults. Our cross-sectional study also found only limited relationships between GST and physical performance. There are several possible explanations for this observation. First, it is possible that a strong age-related VOR effect causes reduced physical performance, so that age explains both the vestibular and performance deficits, and adjusting for age causes an overadjustment phenomenon. Second, since there are multiple systems that contribute to physical performance, we may have failed to detect the vestibular component because we did not account for other system deficits, such as peripheral neuropathy or lower extremity weakness. Third, it is possible that our performance tests did not challenge head velocity or visual stabilization.
Since older adults with poor GST performance may have difficulty with visual stabilization during movement, vestibular rehabilitation may be beneficial. An example of a therapy that simulates the GST and may enhance VOR adaptation is VOR x1 as described by Herdman et al. (19) in which a subject views a stationary object while rotating their head to the point of oscillopsia. Vestibular rehabilitation has been shown to improve GST scores in the yaw plane of unilateral vestibular patients (11). Additionally, vestibular rehabilitation has been shown to be effective in older adults with dizziness (20–23), but has never been assessed for its ability to improve gaze stabilization in older adults without symptoms but with poor performance. Since poor VOR function could contribute to poor visual acuity during motion, and increase the risk of falls, it is possible that vestibular rehabilitation could be a treatment option for older fallers with poor GST scores. Further work to establish head velocity demands during basic tasks such as walking or climbing stairs could provide treatment targets for VOR function to be used in rehabilitation.
Vestibular dysfunction appears to make up a relatively small, but significant percentage of physical performance disability in this population of older adults with few vestibular complaints. Although there are myriad potential causes of falls in older adults that often are associated with age-related functional decline, vestibular dysfunction has often been overlooked as a contributor (2,3). A recent study by Agrawal, et al. (24) estimates the presence of vestibular impairment in US adults at approximately 35%, 32% of whom reported no prior symptoms of dizziness. Other recent studies of fall risk in older adults have identified a high rate of subjective vestibular impairment (25) and abnormal standing balance (26) among fallers, but have not assessed objective vestibular dysfunction. In part, this has been a result of the lack of a clinical test that can be easily administered. The GST may be a useful measure to identify those older adults at risk for falls due to vestibular reasons.
This is the first study in which the gaze stabilization test has been successfully performed by research technicians previously unfamiliar with the device. Older tests of VOR function like rotational chair testing are expensive and cumbersome and therefore difficult to apply to community practices or large epidemiologic studies. This study has shown that the GST may be more generally applicable in the community and additionally may be a valid test of isolated vestibular function in balance studies of older adults.
In conclusion, we believe GST performance in the yaw plane is associated with vestibular function as indicated by the correlation with standing balance; however, it is not associated with other tests of physical performance in this population of older adults. Average GST performance in the pitch plane was associated with chair rises and this may be attributed to oscilopsia when moving from a seated to standing position.
Acknowledgements
The authors would like to thank Subashan Perera, PhD and Gregory Marchetti, PhD, PT for statistical support. This project was supported in part by funding from the National Institutes of Health via K23 DC005384 and P30 AG024827 (Pittsburgh Claude D. Pepper Center for Older Americans Independence Center).
References
- 1.Stevens KN, Lang IA, Guralnik JM, Melzer D. Epidemiology of balance and dizziness in a national population: findings from the English Longitudinal Study of Ageing. Age Ageing. 2008;37:300–305. doi: 10.1093/ageing/afn019. [DOI] [PubMed] [Google Scholar]
- 2.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 3.Nevitt MC, Cummings SR, Hudes ES. Risk factors for injurious falls: a prospective study. J Gerontol. 1991;46:M164–M170. doi: 10.1093/geronj/46.5.m164. [DOI] [PubMed] [Google Scholar]
- 4.Paterka RJ, Black FO, Schoenhoff MB. Age-related changes in human vestibulo-ocular reflexes: sinusoidal rotation and caloric tests. J Vestib Res. 1990;1:49–59. [PubMed] [Google Scholar]
- 5.Paige GD. Senescence of human visual-vestibular interactions. 1. Vestibulo-ocular reflex and adaptive plasticity with aging. Exp Brain Res. 1992;2:133–151. [PubMed] [Google Scholar]
- 6.Baloh RW, Enrietto J, Jacobson KM, Lin A. Age-related changes in vestibular function: A longitudinal study. Ann N Y Acad Sci. 2001;942:210–219. doi: 10.1111/j.1749-6632.2001.tb03747.x. [DOI] [PubMed] [Google Scholar]
- 7.Baloh RW, Ying SH, Jacobson KM. A Longitudinal Study of Gait and Balance Dysfunction in Normal Older People. Arch Neurol. 2003;60(6):835–839. doi: 10.1001/archneur.60.6.835. [DOI] [PubMed] [Google Scholar]
- 8.Furman JM, Redfern MS. Visual-vestibular interaction during OVAR in the elderly. J Vest Res. 2001;11(6):365–370. [PubMed] [Google Scholar]
- 9.Furman J, Muller ML, Redfern M, Jennings JR. Visual-Vestibular Stimulation Interferes with Information Processing in Young and Older Humans. Exp Brain Res. 2003;152:383–392. doi: 10.1007/s00221-003-1560-z. [DOI] [PubMed] [Google Scholar]
- 10.Goebel JA, Tungsiripat N, Sinks B, Carmody J. Gaze stabilization test: a new clinical test of unilateral vestibular dysfunction. Otol Neurotol. 2007;28(1):68–73. doi: 10.1097/01.mao.0000244351.42201.a7. [DOI] [PubMed] [Google Scholar]
- 11.Badaracco C, Labini FS, Meli A, De Angelis E, Tufarelli D. Vestibular rehabilitation outcomes in chronic vertiginous patients through computerized dynamic visual acuity and gaze stabilization test. Otol Neurotol. 2007;28(6):809–817. doi: 10.1097/MAO.0b013e3180cab73f. [DOI] [PubMed] [Google Scholar]
- 12.Whitney SL, Marchetti GF, Pritcher M, Furman JM. Gaze stabilization and gait performance in vestibular dysfunction. Gait Posture. 2009;29(2):194–198. doi: 10.1016/j.gaitpost.2008.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pritcher MR, Whitney SL, Marchetti GF, Furman JM. The influence of age and vestibular disorders on gaze stabilization: a pilot study. Otol Neurotol. 2008;29(7):982–988. doi: 10.1097/MAO.0b013e31818457fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home placement. J Gerontol. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 15.Ostir GV, Volpato S, Fried LP, Chaves P, Guralnik JM. Reliability and sensitivity to change assessed for a summary measure of lower body function: results from the Women’s Health and Aging Study. J Clin Epidemiol. 2002;55(9):916–921. doi: 10.1016/s0895-4356(02)00436-5. [DOI] [PubMed] [Google Scholar]
- 16.Leigh RJ, Zee DS. The neurology of eye movements. New York: Oxford University Press; 1999. [Google Scholar]
- 17.Grossman GE, Leigh RJ, Abel LA, Lanska DJ, Thurston SE. Frequency and velocity of rotational head perturbations during locomotion. Exp Brain Res. 1988;70:470–476. doi: 10.1007/BF00247595. [DOI] [PubMed] [Google Scholar]
- 18.Pozzo T, Berthoz A, Lefort L. Head stabilization during various tasks in humans, I: normal subjects. Exp Brain Res. 1990;82:97–106. doi: 10.1007/BF00230842. [DOI] [PubMed] [Google Scholar]
- 19.Herdman SJ, Whitney SL. Treatment of vestibular hypofunction. In: Herdman SJ, editor. Vestibular Rehabilitation (Contemporary Perspectives in Rehabilitation) 2nd ed. USA: F A Davis; 2000. pp. 387–423. [Google Scholar]
- 20.Whitney SL, Wrisley DM, Marchetti GF, Furman JM. The effect of age on vestibular rehabilitation outcomes. Laryngoscope. 2002;112(10):1785–1790. doi: 10.1097/00005537-200210000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Zanardini FH, Zeigelboim BS, Jurkiewiz AL, Marques JM, Martins-Bassetto J. Vestibular rehabilitation in elderly patients with dizziness. Braz J Otorhinolaryngol. 2005;71(1):38–46. [Google Scholar]
- 22.Macias JD, Massingale S, Gerkin RD. Efficacy of vestibular rehabilitation therapy in reducing falls. Otolaryngol Head Neck Surg. 2005;133(3):323–325. doi: 10.1016/j.otohns.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 23.Ribeiro Ados, Pereira JS. Balance improvement and reduction of likelihood of falls in older woman after Cawthorne and Cooksey exercises. Gait Posture. 2006;24(1):62–69. doi: 10.1016/S1808-8694(15)31283-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agrawal Y, Carey JP, Della Santina CC, et al. Disorders of balance and vestibular function in US adults: data from the National Health and Nutrition Examination Survey, 2001–2004. Arch Intern Med. 2009;169(10):938–944. doi: 10.1001/archinternmed.2009.66. [DOI] [PubMed] [Google Scholar]
- 25.Pothula V, Chew F, Lesser T, Sharma A. Falls and vestibular impairment. Clin Otolaryngol Allied Sci. 2004;29:179–182. doi: 10.1111/j.0307-7772.2004.00785.x. [DOI] [PubMed] [Google Scholar]
- 26.Murray KJ, Hill K, Phillips B, Waterston J. A pilot study of falls risk and vestibular dysfunction in older fallers presenting to hospital Emergency Departments. Disabil Rehabil. 2005;27(9):499–506. doi: 10.1080/09638280400018486. [DOI] [PubMed] [Google Scholar]