Abstract
Background
The relationship between coronary endothelial function and coronary calcification is not well established.
Methods
Forty-six patients (17 men [37%]; age, 47.4±11.4 years prospectively underwent testing for coronary endothelial function and measurement of coronary artery calcification (CAC).
Results
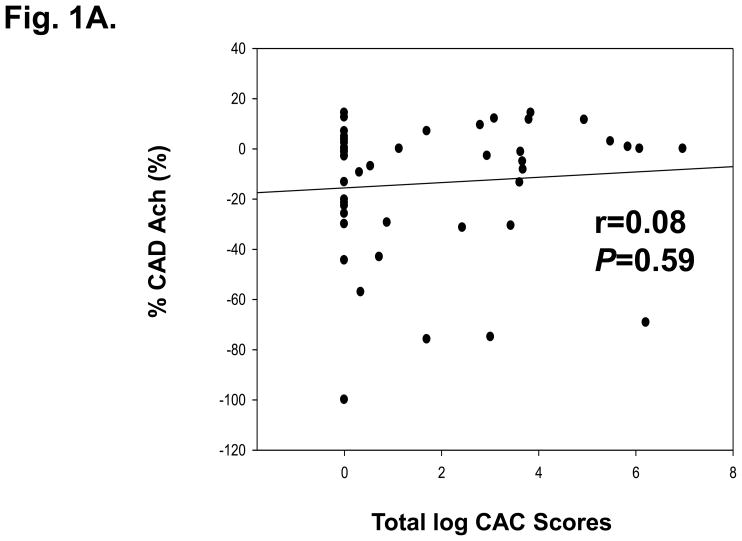
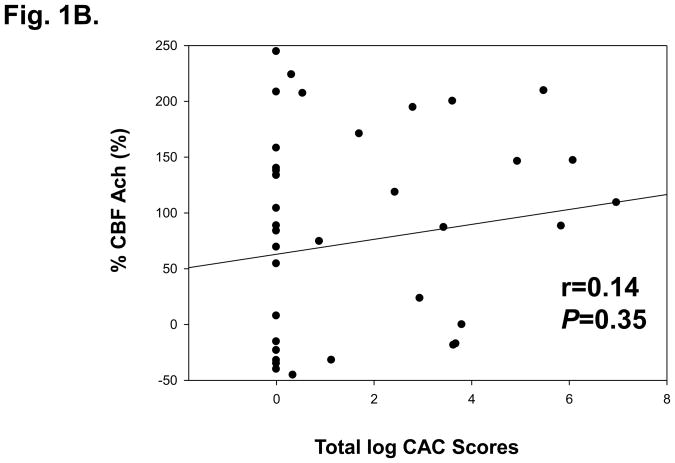
Log CAC scores were not significantly different between patients with normal (n=31) and abnormal (n=15) response of epicardial coronary artery diameter to acetylcholine (%CADAch) (median (25, 75 percentile) (1.1 (0.0, 3.7) vs 0.3 (0.0, 2.4), P=.32) and with normal (n=28) and abnormal (n=18) response of coronary blood flow to acetylcholine (%CBFAch) (0.5 (0.0, 3.6) vs 0.5 (0.0, 3.2), P=.76). Log CAC scores did not correlate with %CADAch (r=0.08, P=.59), %CBFAch (r=0.14, P=.35).
Conclusions
In patients without significant coronary artery disease, coronary endothelial dysfunction showed no apparent association with coronary calcification. Our findings suggest that these 2 markers may represent separate, independent processes in the progression of coronary atherosclerosis.
Keywords: coronary calcification, early coronary atherosclerosis, electron beam computed tomography, endothelial dysfunction
Introduction
Among the markers of subclinical atherosclerosis that have proved predictive of future cardiac events are coronary endothelial dysfunction and coronary artery calcification (CAC) [1.2]. These are attractive measures in that they both directly examine the vascular bed at risk and do not rely on concordance between coronary artery disease and non-coronary atherosclerosis.
Functional abnormalities could be expected to precede structural abnormalities in the pathogenesis of atherosclerosis; for example, previous studies could not identify a relationship between coronary plaque on intravascular ultrasound and coronary endothelial dysfunction [3]. A noninvasive, inexpensive technique such as cardiac CT might be preferable over an invasive, expensive procedure such as cardiac catheterization for the assessment of cardiovascular risk if both tests provided concordant information.
Hence, the goal of our study was to explore the relationship between coronary endothelial dysfunction and CAC.
Methods
Patients
We prospectively enrolled patients referred by independent physicians for the assessment of coronary endothelial function. Patients had recurrent chest pain and/or positive cardiac stress testing and negative findings thorough evaluation of lungs and gastrointestinal tract. Patients with early atherosclerosis (coronary artery luminal narrowing <30%) were underwent coronary endothelial function test and the procedure for CAC scanning within 2 weeks of the coronary catheterization procedure. Exclusion criteria were described previously [4]. The Mayo Clinic Institutional Review Board approved the study, and informed consent was obtained from all participants.
Endothelial Function Assessment and Coronary Flow Reserve
Coronary angiography was performed in standard technique [4]. Coronary endothelial function of the LAD was assessed as previously described [4]. To evaluate endothelium-independent, microvascular coronary flow reserve (CFR), intracoronary bolus injections of adenosine (Fujisawa Healthcare Inc., Deerfield, IL) were administered and CFR was calculated [4].
To assess endothelium-dependent function, acetylcholine (Iolab Pharmaceuticals, Claremont, CA) was selectively infused into the LAD for 3 minutes at increasing concentrations (10−6, 10−5, and 10−4 mol/L) respectively. Coronary artery diameter and average peak velocity were measured and coronary blood flow was calculated from the Doppler-derived time velocity integral and vessel diameter [4].
The percent change of coronary artery diameter in response to acetylcholine (%CADAch) was measured in the mid LAD 5 mm distal to the tip of the Doppler wire after each infusion. The degree of endothelial function in the coronary microcirculation was defined by the percent change of coronary blood flow in response to acetylcholine (%CBFAch). The %CBFAch was calculated by dividing the coronary blood flow after infusing acetylcholine (concentration, 10−4 M; 18.2 μg/mL) by the blood flow at baseline.
Definitions of Abnormal Endothelial Function
Abnormal coronary epicardial endothelial function was defined as a decrease in %ΔCADAch by >20% [4]. Abnormal endothelium-dependent function in the coronary microcirculation was defined as %ΔCBFAch by <50%, or a ratio between measurements before and after acetylcholine <1.5. Impaired endothelium-independent function of the coronary microcirculation was defined as a CFR of 2.5 or lower [4].
Electron Beam Computed Tomography
The procedure for CAC scanning with electron beam CT (Imatron; GE Healthcare, Milwaukee, WI) was performed as previously described [5]. Forty to 60 tomograms were acquired to cover the entire heart in all patients. The field of view was 26 cm with a 512 × 512 pixel matrix (resolution, 0.51 × 0.51 mm/pixel). Presence of CAC on EBCT tomograms was defined as 2 or more contiguous pixels with a brightness of at least 130 Hounsfield units. Regions of interest surrounding areas of CAC were traced by trained technicians using custom software. CAC scores were calculated following previously described methods [6] for the entire coronary tree (total) and for the LAD only. CAC scores were not normally distributed, log CAC scores were used for statistical analysis.
Statistical Analysis
Continuous variables were presented as mean±SD or as median (interquartile range). Discrete data were presented as frequencies and percentages. Associations between 2 continuous variables were measured with the Spearman rank correlation test. Associations between 2 discrete variables were tested using the Pearson χ2 test. Group differences in continuous measures were made by Mann-Whitney U-test. All hypothesis tests were 2-tailed with a significance level of 0.05.
Results
Study Patients
Forty-six patients (17 men [37%]; age, 47±11 years) were prospectively enrolled in the study.
Analysis by Presence or Absence of Coronary Artery Calcium
Patients with detectable CAC (n=26) were significantly older (P=.04) and had a higher body mass index (P=.02) and fasting glucose level (P=.02). Other baseline characteristics, in particular the serum lipids profiles, were not different between groups. No significant differences between groups were present for %ΔCADAch, %ΔCBFAch, CFR (Supplementary data Table 2).
Analysis by Presence or Absence of Abnormal Coronary Physiology
Total log CAC scores and log CAC scores of LAD were not different between groups by the results of endothelial function and CFR (Table 1).
Table 1.
Calcium score in the entire coronary tree and in the LAD grouped by type and result of coronary physiologic testing
| Total log CAC scores | P | Log CAC scores of LAD | P | ||
|---|---|---|---|---|---|
| %ΔCADAch | Normal (n=31) | 1.1 (0.0,3.7) | 0.32 | 0.0 (0.0, 3.5) | 0.63 |
| Abnormal (n=15) | 0.3 (0.0, 2.4) | 0.0 (0.0, 1.6) | |||
| %ΔCBFAch | Normal (n=28) | 0.5 (0.0, 3.6) | 0.76 | 0.0 (0.0, 3.5) | 0.98 |
| Abnormal (n=18) | 0.5 (0.0, 3.2) | 0.0 (0.0, 1.7) | |||
| Maximal CFR | Normal (n=35) | 1.0 (0.0, 3.6) | 0.44 | 0.0 (0.0, 3.5) | 0.37 |
| Abnormal (n=11) | 0.0 (0.0, 3.6) | 0.0 (0.0, 1.2) | |||
Values are median (25%, 75% percentile). LAD= Left anterior desencding coronary artery, CAC: coronary artery calcification, %ΔCADAch= Percent change of coronary artery diameter in response to acetylcholine, %ΔCBFAch = Percent change of coronary blood flow in response to acetylcholine, CFR= Coronary flow reserve.
Correlation Between Coronary Endothelial Dysfunction and Coronary Calcification
Total log CAC scores was not significantly correlated with %ΔCADAch (r=0.08, P=.59), %ΔCBFAch (r=0.14, P=.35), CFR (r=0.15, P=.32) (Fig 1). Similarly, log CAC scores of LAD also was not significantly correlated with these parameters (0.05≤r≤0.14, all P=NS). Of interest, even after adjusting for age, body mass index, fasting glucose level, and mean arterial pressure, total log CAC scores was not significantly correlated with %ΔCADAch (r=0.006, P=.97), %ΔCBFAch (r=0.24, P=.19), CFR (r=0.27, P=.12). This lack of correlation does not appear to be related to skewing of the data by the many subjects who had no CAC. Among the 26 patients with detectable CAC, no significant association was identified between these measures of coronary endothelial function (%ΔCADAch, %ΔCBFAch, CFR) and total log CAC scores (−0.17<r<0.39, all P=NS) or log CAC scores of LAD (−0.003<r<0.24, all P=NS).
Figure 1.
A, B There was no significant correlation between %CADAch and total log CAC scores (A) and %CBFAch and total log CAC scores (B) in the overall study group.
%CADAch, percent change of coronary artery diameter in response to acetylcholine, %CBFAch, percent change of coronary blood flow in response to acetylcholine, CAC, coronary artery calcification
Discussion
Previous studies of the relationship between endothelial function in various vascular beds assessed noninvasively and CAC have shown conflicting results [7,8]. We, for the first time, demonstrated that, in patients with chest pain in the absence of significant CAD, there is no appreciable relationship between CAC scores and quantitative or qualitative measures of coronary endothelium-dependent or independent function.
The lack of correlation between coronary endothelial function and CAC in our study may have several explanations. First, these two markers may well represent separate processes in the development of coronary atherosclerosis. Previous experimental studies suggest that osteopontin-mediated vascular calcification may originate from an osteoprogenitor cell population in the adventitia [9] and occur independently of atheroma formation associated with endothelial injury.
Second, CAC may represent structural changes of the endothelium, media, and adventitia that reflect mechanisms of atherosclerosis progression unrelated to endothelial function, such as plaque rupture, or intraplaque hemorrhage associated with immature neovascularization [10]. Studies that examined CAC patterns with intravascular ultrasound or CT showed that the culprit coronary lesions in patients with acute coronary syndromes had less or spotty calcification when compared with stable plaques in other vessels, and also are less likely to be calcified than the plaques of patients with chronic stable angina [11]. Importantly, CAC is usually not present in the earliest fatty streak atherosclerotic lesions and adverse cardiac events may occur in the absence of CAC [2]. A recent in vitro study [12] showed that CAC quantity assessed by CT was not related to morphologic predictors of likelihood of rupture such as intraplaque hemorrhage, lipid content, inflammation, or plaque size.
Third, the relationship between markers of subclinical inflammation and CAC is tenuous [7]. This lack of a relationship between inflammation and CAC is yet another likely partial explanation of our findings.
The main limitations of coronary endothelial function assessment as a measure of early atherosclerosis are its invasive nature and the fact that it assesses the functional interaction between the endothelium and the media but cannot address the atherosclerotic process at the level of the adventitia. However, the clinical importance of detecting coronary endothelial dysfunction is suggested by a previous study which demonstrated that the treatment of endothelial function can reduce the incidence of cardiac events [13]. Conversely, although high quantities of CAC can be present without evidence for advanced CAD in the form of myocardial perfusion abnormalities on Tc-99m single-photon emission CT [14], randomized, prospective studies to date have not shown an effect of risk factor modification on the progression of CAC or on clinical outcomes [15].
The considerations on the pathophysiology of atherosclerosis discussed above suggest that endothelial dysfunction and CAC may represent two distinct and separate processes in the development of coronary atherosclerosis at least at the early stage, and may provide complementary information in the assessment of subclinical coronary artery disease.
The main limitations of our study are the small number of study patients and the likely presence of referral bias. Further study for this topic in patients with higher CAC and early atherosclerosis or in patients with coronary artery disease are needed in the future.
Conclusions
Our results support the concept that coronary endothelial dysfunction and CAC may be separate phenomena in the development of atherosclerosis, especially at the early stage. These two phenomena may contribute differently to plaque biology and provide complementary information on future risk of cardiac events.
Supplementary Material
Abbreviations
- CAC
coronary artery calcification
- %CADAch
percent change of coronary artery diameter in response to acetylcholine
- %CBFAch
percent change of coronary blood flow in response to acetylcholine
- CFR
coronary flow reserve
- CT
computed tomography
- LAD
left anterior descending coronary artery
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lerman A, Zeiher AM. Endothelial Function: Cardiac Events. Circulation. 2005;111:363–68. doi: 10.1161/01.CIR.0000153339.27064.14. [DOI] [PubMed] [Google Scholar]
- 2.Greenland P, Bonow RO, Brundage BH, et al. American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography); Society of Atherosclerosis Imaging and Prevention; Society of Cardiovascular Computed Tomography. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. Circulation. 2007;115:402–26. doi: 10.1161/CIRCULATIONAHA..107.181425. [DOI] [PubMed] [Google Scholar]
- 3.Nishimura RA, Lerman A, Chesebro JH, et al. Epicardial vasomotor responses to acetylcholine are not predicted by coronary atherosclerosis as assessed by intracoronary ultrasound. J Am Coll Cardiol. 1995;26:41–9. doi: 10.1016/0735-1097(95)00142-m. [DOI] [PubMed] [Google Scholar]
- 4.Han SH, Bae JH, Holmes DR, Jr, et al. Sex differences in atheroma burden and endothelial function in patients with early coronary atherosclerosis. Eur Heart J. 2008;29:1359–69. doi: 10.1093/eurheartj/ehn142. [DOI] [PubMed] [Google Scholar]
- 5.Kaufmann RB, Sheedy PF, 2nd, Breen JF, et al. Detection of heart calcification with electron beam CT: interobserver and intraobserver reliability for scoring quantification. Radiology. 1994;190:347–52. doi: 10.1148/radiology.190.2.8284380. [DOI] [PubMed] [Google Scholar]
- 6.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardio. 1990;15:827–32. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 7.Ramadan MM, Mahfouz EM, Gomaa GF, et al. Evaluation of coronary calcium score by multidetector computed tomography in relation to endothelial function and inflammatory markers in asymptomatic individuals. Circ J. 2008;72:778–85. doi: 10.1253/circj.72.778. [DOI] [PubMed] [Google Scholar]
- 8.Kullo IJ, Malik AR, Bielak LF, Sheedy PF, 2nd, Turner ST, Peyser PA. Brachial artery diameter and vasodilator response to nitroglycerine, but not flow-mediated dilatation, are associated with the presence and quantity of coronary artery calcium in asymptomatic adults. Clin Sci (Lond) 2007;112:175–82. doi: 10.1042/CS20060131. [DOI] [PubMed] [Google Scholar]
- 9.Towler DA, Bidder M, Latifi T, Coleman T, Semenkovich CF. Diet-induced diabetes activates an osteogenic gene regulatory program in the aortas of low density lipoprotein receptor-deficient mice. J Biol Chem. 1998;273:30427–34. doi: 10.1074/jbc.273.46.30427. [DOI] [PubMed] [Google Scholar]
- 10.Langheinrich AC, Michniewicz A, Sedding DG, et al. Quantitative X-ray imaging of intraplaque hemorrhage in aortas of apoE(−/−)/LDL(−/−) double knockout mice. Invest Radiol. 2007;42:263–73. doi: 10.1097/01.rli.0000258085.87952.ea. [DOI] [PubMed] [Google Scholar]
- 11.Beckman JA, Ganz J, Creager MA, Ganz P, Kinlay S. Relationship of clinical presentation and calcification of culprit coronary artery stenosis. Arterioscler Thromb Vasc Biol. 2001;21:1618–22. doi: 10.1161/hq0901.095554. [DOI] [PubMed] [Google Scholar]
- 12.Pham PH, Rao DS, Vasunilashorn F, Fishbein MC, Goldin JG. Computed tomography calcium quantification as a measure of atherosclerotic plaque morphology and stability. Invest Radiol. 2006;41:674–80. doi: 10.1097/01.rli.0000233325.42572.08. [DOI] [PubMed] [Google Scholar]
- 13.Ceconi C, Fox KM, Remme WJ, et al. EUROPA Investigators; PERTINENT Investigators and the Statistical Committee. ACE inhibition with perindopril and endothelial function. Results of a substudy of the EUROPA study: PERTINENT. Cardiovasc Res. 2007;73:237–46. doi: 10.1016/j.cardiores.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 14.Berman DS, Wong ND, Gransar H, et al. Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomograpy. J Am Coll Cardiol. 2004;44:923–30. doi: 10.1016/j.jacc.2004.06.042. [DOI] [PubMed] [Google Scholar]
- 15.Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol. 2005;46:166–72. doi: 10.1016/j.jacc.2005.02.089. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.