Abstract
Objective
Prolonged emergency department (ED) wait time and length of visit reduce quality of care and increase adverse events. Previous studies have not examined hospital-level performance on ED wait time and visit length in the United States. The purpose of this study is to describe hospital-level performance on ED wait time and visit length.
Methods
We conducted a retrospective cross-sectional study of a stratified random sampling of 35,849 patient visits to 364 non-Federal U.S. hospital EDs in 2006, weighted to represent 119,191,528 visits to 4,654 EDs. Measures included EDs' median wait times and visit lengths, EDs' median proportion of patients seen by a physician within the time recommended at triage, and EDs' median proportion of patients dispositioned within 4 or 6 hours.
Results
In the median ED, 78.3% (interquartile range [IQR], 63.2%, 89.5%) of all patients, and 66.9% (IQR, 52.0%, 81.9%) of patients who were triaged to be seen within one hour were seen by a physician within the target triage time. A total of 30.5% of EDs achieved the triage target for more than 90% of their patients; 13.8% of EDs achieved the triage target for 90% or more of patients triaged to be seen within an hour. In the median ED, 76.3% (IQR 54.4%, 93.9%) of patients were admitted within 6 hours. A total of 47.7% of EDs admitted more than 90% of their patients within 6 hours, but only 24.5% of EDs admitted more than 90% of their patients within 4 hours.
Conclusions
A minority of hospitals consistently achieved recommended wait times for all ED patients, and fewer than half of hospitals consistently admitted their ED patients within 6 hours.
Introduction
Background
Emergency department (ED) crowding in the United States has become so severe that the Institute of Medicine calls it a “national epidemic.”1 Across the nation, an ambulance is diverted away from an overcrowded ED approximately once every minute.1 Patients who do arrive in the ED have faced increasingly long average wait times and ED visit lengths over the past decade.2, 3 Most importantly, these increases have been most pronounced for patients with the most acute illnesses.2–4 In 2006, the average wait time for emergent patients to see an ED provider was 37 minutes, well above the recommended maximum of 15 minutes.4
Importance
Prolonged ED wait time and length of visit reduce quality of care and increase adverse events for patients with serious illnesses.5–9 For example, patients presenting with non-ST-elevation myocardial infarction (MI) who have an ED stay of more than 8 hours are more likely to have recurrent in-hospital MI than patients with an average ED stay.8 Prolonged wait time and length of visit also decrease patient satisfaction10–12 and increase the number of patients who leave before being seen.13, 14 Therefore, ED wait time and length of visit are important measures of the timeliness, efficiency, safety and patient-centeredness of emergency care.
Several studies have examined wait time and visit length across the nation in aggregate,2, 3, 15, 16 including a recent comprehensive report from the United States Government Accountability Office (GAO).4 However, none of these studies examined hospital-level variability. The GAO report argues that hospital-level conditions such as the availability of inpatient beds are the most important determinants of crowding and delayed care.4 Consequently, from a policy and quality improvement perspective, it is most appropriate to consider these metrics from a hospital rather than patient viewpoint.
Goals of this investigation
The National Quality Forum (NQF) recently endorsed 10 voluntary consensus standards for emergency care quality, including measures of ED wait time, visit length for admitted patients, and visit length for discharged patients.17 If widely adopted, these measures would be reported at the hospital level. While one study has examined hospital-level performance on visit length for black patients,16 there have been no studies of variation in hospital-level performance on these metrics for all patients. National data on hospital-level performance, which would allow EDs to benchmark themselves against peers and distinguish targets for improvement, are needed.18 Accordingly, we sought to characterize the variation in ED performance in wait times and visit lengths nationally using data from 2006 National Hospital Ambulatory Medical Care Survey (NHAMCS).
Materials and Methods
Theoretical model of the problem
The central tenet of quality improvement is that “quality is a system property.”19 ED wait time and length of visit have been observed to differ systematically according to race, ethnicity, site of care and a variety of other immutable patient-level factors.2, 15, 16 Using, instead, the quality improvement model, we examine ED wait time and length of visit at the system (hospital) level. Describing hospital-level rather than patient-level performance allows for benchmarking, characterization of variation, recognition of positive and negative outliers, and assessment of effective care practices: activities necessary for sustainable quality improvement.
Study design, setting and participants
We conducted a cross-sectional study of patient visits to 364 United States EDs in 2006, using NHAMCS data. The NHAMCS is a 4-stage probability sample of visits to emergency departments of United States general and short-stay hospitals, excluding Federal, military, and Veterans Administration hospitals. Each hospital abstracts data from a systematic random sample of emergency department visits during a randomly assigned 4-week period. Data collection, abstraction and cleaning procedures have been fully described elsewhere.20 The dataset includes weights to facilitate estimation of national results.
Methods of measurement, outcome measures
Outcome variables
We examined median ED performance on 1) wait time, defined as number of minutes between the time the patient arrived at the ED and the time the patient was seen by a provider, and 2) length of visit, defined as the number of minutes between the time the patient arrived at the ED and the time the patient was discharged from the ED. These medians correspond to the NQF measures for wait time and length of visit. The dataset includes a five-level triage assessment variable: immediate (see in 0 minutes), emergent (see in 1–14 minutes), urgent (see in 15–60 minutes), semi-urgent (see in 61 minutes to 2 hours), and non-urgent (see in 121 minutes to 24 hours). Because 5-level triage systems are not yet universal in the U.S.,21 we collapsed the first two categories into one emergent category (see in 0–14 minutes). For each ED, we calculated the percentage of patients that were seen within their triage target timeframe,4 and repeated this analysis restricting the dataset to acutely ill patients (those triaged as emergent or urgent). For each ED, we also calculated the percentage of patients with a visit less than 4 hours, based on United Kingdom standards,22 and the percentage with a visit less than 6 hours, based on Canadian standards.23
Independent variables
Our independent variables included visit characteristics, patient sociodemographic factors, and hospital characteristics. Visit characteristics included triage category (emergent, urgent, semi-urgent, non-urgent); level of pain at presentation; admission to intensive care; number of medications given in ED (0, 1–3, ≥3); season of visit and day of visit. Because research suggests that ED tests lengthen ED stays,15 we included binary dummy variables for presence of any laboratory test, any plain film, any ultrasound, any computed tomography (CT) scan, any magnetic resonance imaging (MRI) scan or any electrocardiogram for the length of visit analyses. We also created two dummy variables for procedures: one for any emergent procedure (cardiopulmonary resuscitation, endotracheal intubation and/or thrombolysis) and one for any non-emergent procedure (all others).
Patient sociodemographic factors included age, self-reported race and ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), gender, method of payment, arrival by ambulance, quartile of poverty rate in the patient's zip code (<5%, 5–9.99%, 10–19.99%, ≥ 20%), quartile of median household income in the patient's zip code (<$32,793; $37,794–$40,626; $40,627–$52,387; ≥$52,388), and quartile of bachelor's degree or higher in the patient's zip code (<12.8%, 12.8–19.7%, 19.7–31.7%, ≥ 31.7%).
Hospital characteristics included urban status (mode of patients' zip code locations: large central metro; large fringe metro; medium metro; small metro; non-metro), ownership, proportion of uninsured patients (<10%, 10–19.9%, 20–29.9%, ≥30%), geographic region (Northeast, Midwest, South, West), teaching status (any patients seen by a trainee versus none), and use of electronic medical records (EMR) (all electronic; part paper, part electronic; all paper).
Primary data analysis
We used standard descriptive statistics to characterize the sample of patients and hospitals. To describe EDs' median performance on wait time and length of visit, we reported the median of ED medians, with interquartile ranges. We also constructed histograms of EDs' median results for wait time by triage category and length of visit for admitted and for non-admitted patients. We then calculated the weighted percent of EDs seeing a given percent of their patients within triage targets or within length of visit goals (e.g., half their patients, 75% of their patients, 90% of their patients).
We estimated linear models with a separate random intercept for each ED to identify the percent of variation in log-transformed wait time and in log-transformed length of visit that was present within hospitals and between hospitals. Next, we estimated hospital random-effects regressions with a separate random intercept for each hospital with one of the hospitals excluded as the reference group, and reported the percent of overall variation explained by the model (R2).26, 27 This approach allowed us to account for the clustering of patients within hospitals while including hospital-level predictors of wait time performance. Multivariate analyses were conducted using Stata version 10.0 (Stata Corp, College Station, TX), and all other analyses were conducted using SAS version 9.1.2 (SAS Institute, Cary, NC). To account for the complex sampling design and survey weights, procedures surveyfreq and surveymeans were used in SAS. All statistical tests were two-tailed and we used a P-value of 0.05 to determine statistical significance.
Results
Characteristics of study subjects
The 2006 NHAMCS dataset comprised data about 35,849 patient visits at 364 EDs, weighted to represent 119,191,528 visits to 4,654 EDs. The wait time analysis included 24,889 patient visits to 354 EDs; the length of visit analyses included 33,339 patient visits to 363 EDs. Descriptive statistics for the sample of patients and hospitals are shown in Table 1.
Table 1.
Weighted characteristics of study sample
| Visit Level Characteristics | Percentage of total sample* | Hospital level characteristics | Percentage of total sample* |
|---|---|---|---|
| Arrival by ambulance | 16.0 | Region | |
| Triage Assessment | Northeast | 13.9 | |
| Non-urgent (see in >2 hrs – 24 hrs) | 12.1 | Midwest | 28.7 |
| Semi-urgent (see in >1 hr – 2 hrs) | 22.0 | South | 38.9 |
| Urgent (see in 15–60 min) | 36.6 | West | 18.5 |
| Emergent (see in 0–14 min) | 15.9 | Urban status | |
| No/unknown triage | 13.4 | Large central metro | 17.9 |
| Pain | Large fringe metro | 15.7 | |
| No pain | 19.6 | Medium metro | 20.0 |
| Mild pain | 13.9 | Small metro | 13.3 |
| Moderate pain | 25.9 | Non-metro | 33.2 |
| Severe pain | 21.1 | Ownership | |
| Unknown pain | 19.5 | Voluntary non-profit | 67.6 |
| Any blood test or EKG | 41.0 | Government, non-Federal | 22.0 |
| Any radiology | 44.2 | Proprietary | 10.4 |
| Any emergent procedure | 0.5 | Teaching Status | |
| Any non-emergent procedure | 47.5 | Teaching hospital | 47.7 |
| Number of medications given in ED | Proportion of uninsured patients | ||
| 0 | 44.6 | 0–9.9% | 32.1 |
| 1–3 | 49.3 | 10–19.9% | 34.0 |
| >3 | 6.0 | 20–29.9% | 25.1 |
| Admitted to hospital | 12.8 | ≥30% | 8.9 |
| Season | Electronic medical records | ||
| Winter | 26.4 | All electronic | 16.1 |
| Spring | 24.0 | Part paper, part electronic | 30.4 |
| Summer | 25.6 | None electronic | 53.5 |
| Autumn | 24.0 | ||
| Day of week | |||
| Weekend | 28.9 | ||
| Age, mean years | 36.8 | ||
| Female | 54.5 | ||
| Race/Ethnicity | |||
| White, non-Hispanic | 60.3 | ||
| Black, non-Hispanic | 23.6 | ||
| Hispanic | 12.5 | ||
| Other | 3.7 | ||
| Payment type | |||
| Private insurance | 35.3 | ||
| Medicare | 14.8 | ||
| Medicaid/SCHIP | 26.7 | ||
| Self-pay | 18.5 | ||
| Other pay type | 4.7 | ||
| Percent with bachelor's degree or higher in patient's zip code | |||
| <12.84% | 32.9 | ||
| 12.84–19.66% | 26.6 | ||
| 19.67–31.68% | 22.2 | ||
| ≥31.69% | 18.3 | ||
| Median household income of patient's zip code | |||
| <$32,793 | 33.7 | ||
| $32,794–40,626 | 27.0 | ||
| $40,627–52,387 | 21.3 | ||
| ≥52,388 | 18.1 | ||
| Median poverty rate of patient's zip code | |||
| <5% | 13.2 | ||
| 5–9.99% | 25.8 | ||
| 10–19.99% | 37.4 | ||
| ≥20% | 23.6 | ||
| Median wait time, minutes (IQR) | 33 (15, 69) | ||
| Median wait time, by triage category, minutes (IQR) | |||
| Emergent (see within 15 min) | 15 (6, 38) | ||
| Urgent (see in 16–60 min) | 32 (17, 60) | ||
| Semi-urgent (see in 60–120 min) | 48 (23, 90) | ||
| Nonurgent (see in 2–24 hrs) | 44 (20, 95) | ||
| No triage or unknown | 33 (14, 74.5) | ||
| Median length of visit, patients ultimately admitted, hours (IQR) | 4.4 (2.8, 6.7) | ||
| Median length of visit, patients ultimately discharged, hours (IQR) | 2.3 (1.3, 3.8) |
unless otherwise specified in table
SEM: standard error of the mean; IQR: interquartile range
Weighted visit N = 119,191,528
Weighted ED N = 4654
Main results: Hospital wait time performance
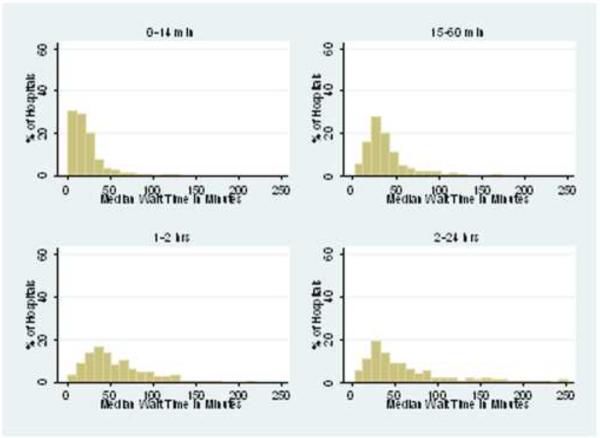
Median ED wait times are shown in Table 2. Among acutely ill (emergent and urgent) patients, the median ED wait time was 27.5 minutes with wide variability across hospitals (IQR 19 min, 40 min). Variation in EDs' median wait times was apparent at every level of triage urgency (Table 2 and Figure 1).
Table 2.
Hospital performance on wait time and length of ED visit
| Mean of hospital means (SE) | Median of hospital medians (IQR) | Median hospital proportion within target (IQR) | |
|---|---|---|---|
| Wait time, all patients, minutes | 52.4 (7.3) | 34.0 (22.5, 47.8) | 78.3% (63.2, 89.5) |
| Wait time by triage category, minutes | |||
| Immediate and emergent (see within 15 min) | 31.8 (4.6) | 16.0 (9.5, 28.0) | 48.4% (23.1, 66.7) |
| Urgent (see in 16–60 min) | 45.2 (3.0) | 32.0 (23.0, 45.0) | 80.0% (63.3, 92.2) |
| Semi-urgent (see in 60–120 min) | 58.6 (3.4) | 45.0 (30.0, 75.0) | 91.7% (77.4, 100.0) |
| Nonurgent (see in 2–24 hrs) | 68.6 (6.7) | 45.0 (27.0, 83.0) | 100% (100, 100) |
| No triage or unknown | 60.9 (13.2) | 36.0 (21.0, 63.0) | N/A |
| Length of visit, patients ultimately admitted, hours | 4.93 (0.65) | 4.3 (3.3, 5.6) | 76.3% (54.4, 93.9)* 60.0% (35.3, 87.5)† |
| Length of visit, patients ultimately discharged, hours | 3.0 (0.45) | 2.3 (1.9,2.9) | 93.0% (87.1, 97.3)* 86.8% (75.5, 94.3)† |
SE: standard error; IQR: interquartile range
proportion within 6 hour target
proportion within 4 hour target
Figure 1.
Distribution of hospital median wait time, by triage assessment
The median ED evaluated 78.3% of its patients within the triage target time (IQR 63.2%, 89.5%). Performance for acutely ill patients was lower. The median ED evaluated 66.9% of its acutely ill patients within the triage target time (IQR 52.0%, 81.9%). While 80.3% of EDs evaluated at least half of their acutely ill patients within the triage target time, only 13.8% achieved this target for at least 90% of their patients (Table 3). Overall, 82.7% of the variation in wait time was due to within-hospital (patient-level) variation, and 17.3% of the variation was due to between-hospital (hospital-level) variation. The multivariate model explained 15.0% of the total variation (R2=0.15).
Table 3.
Weighted percent of hospitals meeting performance measure for a given proportion of their patients
| Wait time within triage target | Length of visit less than 6 hours | Length of visit less than 4 hours | ||||
|---|---|---|---|---|---|---|
| All patients | Immediate, emergent and urgent patients* | Patients discharged home | Patients admitted | Patients discharged home | Patients admitted | |
| (Weighted hospital N = 4,402) | (Weighted hospital N = 4,380) | (Weighted hospital N = 4,653) | (Weighted hospital N= 4,015) | (Weighted hospital N= 4,653) | (Weighted hospital N= 4,015) | |
| At least half of patients, % (SE) | 91.7 (2.0) | 80.3 (2.9) | 98.6 (1.3) | 90.3 (2.0) | 96.1 (1.5) | 62.7 (5.0) |
| At least 75 percent of patients, % (SE) | 64.9 (4.2) | 37.1 (3.9) | 95.7 (1.6) | 69.6 (4.5) | 75.5 (3.8) | 41.6 (5.7) |
| At least 90 percent of patients, % (SE) | 30.5 (4.3) | 13.8 (3.3) | 79.0 (3.3) | 47.7 (5.1) | 41.1 (5.2) | 24.5 (5.5) |
SE: Standard error
Main results: Hospital length of visit performance
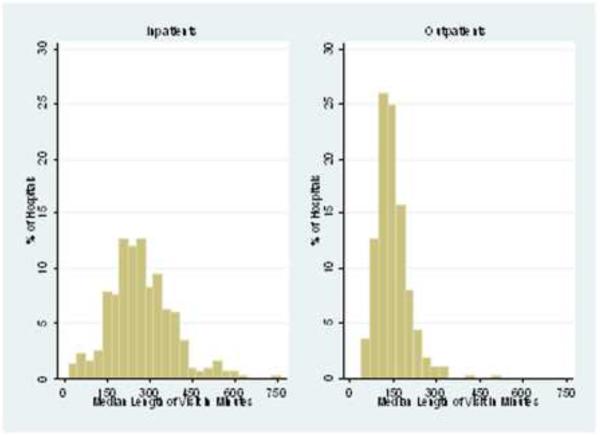
The median ED length of visit was 4.3 hours (IQR 3.3, 5.6) for admitted patients and 2.3 hours (IQR 1.9, 2.9) for discharged patients (Table 2). Figure 2 illustrates ED variation in length of visit by showing the distribution of EDs' median lengths of visit for admitted and discharged patients, separately.
Figure 2.
Distribution of hospital median length of visit, by discharge disposition
The median ED admitted 76.3% (IQR, 54.4%, 93.9%) of its patients within 6 hours and 60.0% (IQR, 35.3%, 87.5%) of its patients within 4 hours. This outcome, too, varied substantially among EDs: 90.3% of EDs admitted at least 50% of their patients within 6 hours, while 47.7% of EDs admitted at least 90% of their patients within 6 hours (Table 3). Similar variation was found for 4 hour visit lengths (Table 3). Overall, 66.8% of the variation in visit length for admitted patients was within hospitals, and 33.2% of the variation was between hospitals. The multivariate model explained 6.9% of the total variation (R2=0.069).
The median ED discharged 93.0% (IQR, 87.1%, 97.3%) of its patients within 6 hours and 86.8% (75.5%, 94.3%) of its patients within 4 hours. As shown in Table 3, EDs had better performance and were more consistent on this outcome for their discharged patients. A total of 98.6% of EDs discharged at least 50% of their patients within 6 hours, and 96.1% of EDs discharged at least 50% of their patients within 4 hours. A total of 79.0% of EDs discharged at least 90% of their patients within 6 hours, but only 41.1% of EDs discharged at least 90% of their patients within 4 hours. Overall, 82.6% of the variation in visit length for discharged patients was within hospitals, and 17.4% of the variation was between hospitals. The multivariate model explained 28.7% of the total variation (R2=0.287).
Limitations
Our study has some limitations. Data are abstracted from charts by each hospital and may not reflect actual practice, particularly for the most emergent patients, who might be examined first and documented later. Between 7–31% of the sample was excluded from various analyses because triage assessment or outcome data were missing. However, these visits did not differ systematically from included visits. Triage assessment reliability has been reported to be fair to excellent depending on the triage method used,28–32 and may have varied among hospitals. Finally, our dataset lacked information about visit volume, crowding, hospital occupancy and processes of care, so the effect of these variables could not be directly determined.
Discussion
In this study we found that hospital emergency departments perform fairly poorly in seeing acutely ill patients within the time recommended by the triage nurse, and in keeping ED visits for admitted patients within 4 or 6 hours. Less than one fifth of EDs were able to see at least 90% of their emergent or urgent patients (those triaged to be seen in an hour or less) within an hour; only half kept the ED visit under 6 hours for at least 90% of their admitted patients.
Performance was not only deficient at the median, it was highly variable across EDs. The median wait time at the slowest 25% of EDs was at least twice as long as the median wait time of the fastest quartile of EDs, and patients admitted from the slowest quartile of EDs spent a median of at least 2.3 more hours in the ED than patients admitted from the quartile with shortest visit length. EDs were most variable in their care of their most acutely ill patients. There was a three-fold difference between the bottom and top quartiles of EDs in median wait times of patients triaged to be seen within 15 minutes.
The reasons for the wide disparity in these outcomes among EDs are likely several, including factors both within and outside a hospital's control. First, hospitals differ in patient, visit and hospital characteristics. However, together these factors explained only a portion of the variability in wait time and length of visit, leaving most of the variability unexplained. Second, higher-volume EDs may be more crowded, increasing wait times and visit lengths.33 These are factors that not often under the control of the ED and reflect the larger social and economic features of the hospital's environment.
It has recently been suggested, however, that the largest contributors to ED crowding and delays in care are not these immutable “input” factors, but rather “throughput” and “output” factors that are at least partially modifiable.4, 34 Numerous studies have shown improved wait time or length of visit after improvements in ED throughput, including changes in triage,35–37 registration,38 work assignment,39 laboratory testing,40–42 staffing,43, 44 physical plant37 or combinations thereof.12, 18, 37, 45–48 Perhaps most important is “output”: the availability of inpatient beds into which to move patients.4 For example, ED length of visit increases as hospital occupancy rates rise.49–53
Our study provides new evidence for the importance of these hospital-level effects, particularly for patients with more severe illness.4 For admitted patients, we found that 33.2% of the variability in length of visit was attributable to the hospital level (between-hospital effect), suggesting that hospital-level factors may be an important driver of visit length for admitted patients. Furthermore, our multivariate models for admitted patients explained only 6.9% of the total variation. This finding implies that the hospital-level data available to us (e.g., region, urban status, ownership, proportion of uninsured patients) are not the major determinants of hospital variability for admitted patients' length of visit. Rather, output factors at each hospital, such as inpatient occupancy, transport availability, housekeeping practices, admitting procedures and prioritization of non-ED admissions, are likely also important determinants of hospital-level variability in ED length of stay.4
Performance measures for ED patient flow have not yet been widely adopted in the United States.17, 25 In this study we report several measures, including median performance and percent performance within goals. Medians are useful to describe the range of performance across EDs, identify benchmark values, and define outliers,25 and have been endorsed by the NQF.17 For wait time, however, reporting an overall median is imperfect since the clinically acceptable wait time varies markedly by patient acuity. Instead, the GAO has reported the proportion of patients overall in the U.S. who are seen within the time recommended by triage assessment.4 Therefore, we also measured the proportion of patients at each ED seen within the time recommended by the triage assessment. For length of visit, we reported both ED median, and the proportion of patients exceeding a predetermined “excess” length of visit. Excess length of visit has variously been defined as 4 hours in the United Kingdom,54 4–6 hours in Canada,23 and 8 hours in Australia.55 The NQF has not defined a target length of visit in the U.S. In this study, we examined performance relative to both 4- and 6-hour visit length targets.
Should ED wait time and visit length be national quality measures, as the NQF proposes? Our findings of marked variability in wait time and visit length across EDs highlight the potential of these quality measures to prompt fundamental changes in ED processes. To achieve improvements in their performance, hospitals would have to focus attention on a wide range of institutional practices involving triage, registration, patient flow, physical environment, laboratory testing, admission processes and policies, workload assignment, staffing and others. Because these measures are correlated with patient outcomes such as leaving before being seen,13, 14 satisfaction,10–12 receipt of recommended care,6, 8 adverse events7–9 and in-hospital length of stay,5 improving performance in wait time and visit length could have a large impact on quality of care for all patients seen in the ED. An example of the implementation of these measures is the United Kingdom, where public reporting of ED visit length has been linked to substantial reduction in ED visit lengths, reduced variability and improved patient outcomes without evidence of “gaming” the measure.56 In 2008, 98% of ED visit lengths in the U.K. were 4 hours or less.57 However, some have complained that the focus on the four hour target has come at the expense of professionalism, collegiality and morale.58, 59
Although apparently successful in the UK, there are several reasons these performance measures should be piloted before widespread adoption in this country. A focus on short wait times might have the unintended consequence of distracting attention from patients already in the ED unless visit length was also simultaneously tracked. Furthermore, a focus on time might prompt EM physicians to prioritize efficiency over accuracy, thoroughness and perhaps safety. Time-based measures are quite susceptible to “gaming” by altering practice and documentation patterns, and have been observed to some degree in the UK.60 Finally, the “optimal” length of visit for an admitted ED patient is unclear. Excessive length of visit is detrimental, but premature discharge or transfer to an inpatient unit may also have adverse consequences.
In summary, we found that United States hospital emergency departments have relatively poor performance in wait time and length of ED visit for their most acutely ill patients, and furthermore, that hospitals themselves vary widely in performance. Attention to these outcomes on a hospital level may provide insight into hospital practices that could improve the quality and efficiency of emergency department care.
Acknowledgements
This publication was made possible by the CTSA Grant UL1 RR024139 and KL2 RR024138 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NCRR or NIH.
Funding Dr. Horwitz is supported by Yale-New Haven Hospital and by the National Center for Research Resources (NCRR). No funding source had any role in the design and conduct of the study; collection, management, analysis and interpretation of the data; or preparation, review and approval of the manuscript.
Funding/support: This publication was made possible by the CTSA Grant UL1 RR024139 and KL2 RR024138 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NCRR or NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial disclosures: No author reports any conflicts of interest relating to this paper.
Role of the sponsor: No funding source had any role in the design and conduct of the study; collection, management, analysis and interpretation of the data; or preparation, review and approval of the manuscript.
REFERENCES
- 1.Institute of Medicine . Hospital-based emergency care: At the breaking point. National Academy of Sciences; Washington, DC: 2006. [Google Scholar]
- 2.Wilper AP, Woolhandler S, Lasser KE, et al. Waits to see an emergency department physician: U.S. trends and predictors, 1997–2004. Health Aff (Millwood) 2008 Mar-Apr;27(2):w84–95. doi: 10.1377/hlthaff.27.2.w84. [DOI] [PubMed] [Google Scholar]
- 3.Herring A, Wilper A, Himmelstein DU, et al. Increasing Length of Stay Among Adult Visits to U.S. Emergency Departments, 2001–2005. Acad Emerg Med. 2009 Jun 15; doi: 10.1111/j.1553-2712.2009.00428.x. DOI:10.1111/j.1553-2712.2009.00428.x. [DOI] [PubMed] [Google Scholar]
- 4.United States Government Accountability Office Hospital emergency departments; crowding continues to occur, and some patients wait longer than recommended time frames. 2009;Vol GAO-09-347 [Google Scholar]
- 5.Liew D, Liew D, Kennedy MP. Emergency department length of stay independently predicts excess inpatient length of stay. Med J Aust. 2003 Nov 17;179(10):524–526. doi: 10.5694/j.1326-5377.2003.tb05676.x. [DOI] [PubMed] [Google Scholar]
- 6.Pines JM, Hollander JE, Localio AR, Metlay JP. The association between emergency department crowding and hospital performance on antibiotic timing for pneumonia and percutaneous intervention for myocardial infarction. Acad Emerg Med. 2006 Aug;13(8):873–878. doi: 10.1197/j.aem.2006.03.568. [DOI] [PubMed] [Google Scholar]
- 7.Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006 Mar 6;184(5):208–212. doi: 10.5694/j.1326-5377.2006.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 8.Diercks DB, Roe MT, Chen AY, et al. Prolonged emergency department stays of non-ST-segment-elevation myocardial infarction patients are associated with worse adherence to the American College of Cardiology/American Heart Association guidelines for management and increased adverse events. Ann Emerg Med. 2007 Nov;50(5):489–496. doi: 10.1016/j.annemergmed.2007.03.033. [DOI] [PubMed] [Google Scholar]
- 9.Ackroyd-Stolarz S, Guernsey J, MacKinnon N, Kovacs G. Is a prolonged stay in the emergency department associated with adverse events in older patients? Acad Emerg Med. 2008 May;15(S1):S67. [Google Scholar]
- 10.Rodi SW, Grau MV, Orsini CM. Evaluation of a fast track unit: alignment of resources and demand results in improved satisfaction and decreased length of stay for emergency department patients. Qual Manag Health Care. 2006 Jul-Sep;15(3):163–170. doi: 10.1097/00019514-200607000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Taylor C, Benger JR. Patient satisfaction in emergency medicine. Emerg Med J. 2004 Sep;21(5):528–532. doi: 10.1136/emj.2002.003723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spaite DW, Bartholomeaux F, Guisto J, et al. Rapid process redesign in a university-based emergency department: Decreasing waiting time intervals and improving patient satisfaction. Annals of Emergency Medicine. 2002 Feb;39(2):168–177. doi: 10.1067/mem.2002.121215. [DOI] [PubMed] [Google Scholar]
- 13.Fernandes CM, Price A, Christenson JM. Does reduced length of stay decrease the number of emergency department patients who leave without seeing a physician? J Emerg Med. 1997 May-Jun;15(3):397–399. doi: 10.1016/s0736-4679(97)00030-9. [DOI] [PubMed] [Google Scholar]
- 14.Goldman RD, Macpherson A, Schuh S, Mulligan C, Pirie J. Patients who leave the pediatric emergency department without being seen: a case-control study. Cmaj. 2005 Jan 4;172(1):39–43. doi: 10.1503/cmaj.1031817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gardner RL, Sarkar U, Maselli JH, Gonzales R. Factors associated with longer ED lengths of stay. Am J Emerg Med. 2007 Jul;25(6):643–650. doi: 10.1016/j.ajem.2006.11.037. [DOI] [PubMed] [Google Scholar]
- 16.Pines JM, Russell Localio A, Hollander JE. Racial Disparities in Emergency Department Length of Stay for Admitted Patients in the United States. Acad Emerg Med. 2009 Feb 24; doi: 10.1111/j.1553-2712.2009.00381.x. [DOI] [PubMed] [Google Scholar]
- 17.National Quality Forum National Voluntary Consensus Standards for Emergency Care. http://www.qualityforum.org/projects/ongoing/emergency/. Accessed 22 June, 2009.
- 18.Hoffenberg S, Hill MB, Houry D. Does sharing process differences reduce patient length of stay in the emergency department? Ann Emerg Med. 2001 Nov;38(5):533–540. doi: 10.1067/mem.2001.119426. [DOI] [PubMed] [Google Scholar]
- 19.Institute of Medicine . Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press; Washington, D.C.: 2001. [PubMed] [Google Scholar]
- 20.National Center for Health Statistics National Hospital Ambulatory and Medical Care Survey Description. http://www.cdc.gov/nchs/about/major/ahcd/nhamcsds.htm. Accessed 10 August, 2008.
- 21.American College of Emergency Physicians ACEP Policy Statement: Triage Scale Standardization. http://www.acep.org/practres.aspx?id=29828. Accessed 15 April, 2009.
- 22.National Health Service The NHS Plan: a plan for investment, a plan for reform. 2000:103. [Google Scholar]
- 23.Canadian Association of Emergency Physicians CAEP Position Statement on Emergency Department Overcrowding. http://www.caep.ca/template.asp?id=37C951DE051A45979A9BDD0C5715C9FE. Accessed 2008, 10 August.
- 24.Solberg LI, Asplin BR, Weinick RM, Magid DJ. Emergency department crowding: consensus development of potential measures. Ann Emerg Med. 2003 Dec;42(6):824–834. doi: 10.1016/S0196064403008163. [DOI] [PubMed] [Google Scholar]
- 25.Welch S, Augustine J, Camargo CA, Jr., Reese C. Emergency department performance measures and benchmarking summit. Acad Emerg Med. 2006 Oct;13(10):1074–1080. doi: 10.1197/j.aem.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 26.Normand S-LT, Glickman ME, Gatsonis CA. Statistical Methods for Profiling Providers of Medical Care: Issues and Applications. J Am Statistical Assoc. 1997;92(439):803–814. [Google Scholar]
- 27.Bryk AS, Raudenbush SW. Hierarchical Linear Models: Applications and Data Analysis. Sage; Newbury Park, CA: 1992. [Google Scholar]
- 28.Brillman JC, Doezema D, Tandberg D, et al. Triage: limitations in predicting need for emergent care and hospital admission. Ann Emerg Med. 1996 Apr;27(4):493–500. doi: 10.1016/s0196-0644(96)70240-8. [DOI] [PubMed] [Google Scholar]
- 29.Fernandes CM, Tanabe P, Gilboy N, et al. Five-level triage: a report from the ACEP/ENA Five-level Triage Task Force. J Emerg Nurs. 2005 Feb;31(1):39–50. doi: 10.1016/j.jen.2004.11.002. quiz 118. [DOI] [PubMed] [Google Scholar]
- 30.Parenti N, Ferrara L, Bacchi Reggiani ML, Sangiorgi D, Lenzi T. Reliability and validity of two four-level emergency triage systems. Eur J Emerg Med. 2009 Mar 11; doi: 10.1097/MEJ.0b013e328310b594. [DOI] [PubMed] [Google Scholar]
- 31.Tanabe P, Gimbel R, Yarnold PR, Kyriacou DN, Adams JG. Reliability and validity of scores on The Emergency Severity Index version 3. Acad Emerg Med. 2004 Jan;11(1):59–65. doi: 10.1197/j.aem.2003.06.013. [DOI] [PubMed] [Google Scholar]
- 32.Wuerz RC, Milne LW, Eitel DR, Travers D, Gilboy N. Reliability and validity of a new five-level triage instrument. Acad Emerg Med. 2000 Mar;7(3):236–242. doi: 10.1111/j.1553-2712.2000.tb01066.x. [DOI] [PubMed] [Google Scholar]
- 33.Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA., Jr. A conceptual model of emergency department crowding. Ann Emerg Med. 2003 Aug;42(2):173–180. doi: 10.1067/mem.2003.302. [DOI] [PubMed] [Google Scholar]
- 34.Newton MF, Keirns CC, Cunningham R, Hayward RA, Stanley R. Uninsured adults presenting to US emergency departments: assumptions vs data. Jama. 2008 Oct 22;300(16):1914–1924. doi: 10.1001/jama.300.16.1914. [DOI] [PubMed] [Google Scholar]
- 35.Choi J, Claudius I. Decrease in emergency department length of stay as a result of triage pulse oximetry. Pediatr Emerg Care. 2006 Jun;22(6):412–414. doi: 10.1097/01.pec.0000221340.26873.2f. [DOI] [PubMed] [Google Scholar]
- 36.Partovi SN, Nelson BK, Bryan ED, Walsh MJ. Faculty triage shortens emergency department length of stay. Acad Emerg Med. 2001 Oct;8(10):990–995. doi: 10.1111/j.1553-2712.2001.tb01099.x. [DOI] [PubMed] [Google Scholar]
- 37.Fernandes CM, Christenson JM, Price A. Continuous quality improvement reduces length of stay for fast-track patients in an emergency department. Acad Emerg Med. 1996 Mar;3(3):258–263. doi: 10.1111/j.1553-2712.1996.tb03430.x. [DOI] [PubMed] [Google Scholar]
- 38.Gorelick MH, Yen K, Yun HJ. The effect of in-room registration on emergency department length of stay. Ann Emerg Med. 2005 Feb;45(2):128–133. doi: 10.1016/j.annemergmed.2004.08.041. [DOI] [PubMed] [Google Scholar]
- 39.Hirshon JM, Kirsch TD, Mysko WK, Kelen GD. Effect of rotational patient assignment on emergency department length of stay. J Emerg Med. 1996 Nov-Dec;14(6):763–768. doi: 10.1016/s0736-4679(96)00199-0. [DOI] [PubMed] [Google Scholar]
- 40.Singer AJ, Ardise J, Gulla J, Cangro J. Point-of-care testing reduces length of stay in emergency department chest pain patients. Ann Emerg Med. 2005 Jun;45(6):587–591. doi: 10.1016/j.annemergmed.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 41.Holland LL, Smith LL, Blick KE. Reducing laboratory turnaround time outliers can reduce emergency department patient length of stay: an 11-hospital study. Am J Clin Pathol. 2005 Nov;124(5):672–674. doi: 10.1309/E9QP-VQ6G-2FBV-MJ3B. [DOI] [PubMed] [Google Scholar]
- 42.Lee-Lewandrowski E, Corboy D, Lewandrowski K, Sinclair J, McDermot S, Benzer TI. Implementation of a point-of-care satellite laboratory in the emergency department of an academic medical center. Impact on test turnaround time and patient emergency department length of stay. Arch Pathol Lab Med. 2003 Apr;127(4):456–460. doi: 10.5858/2003-127-0456-IOAPSL. [DOI] [PubMed] [Google Scholar]
- 43.Bucheli B, Martina B. Reduced length of stay in medical emergency department patients: a prospective controlled study on emergency physician staffing. Eur J Emerg Med. 2004 Feb;11(1):29–34. doi: 10.1097/00063110-200402000-00006. [DOI] [PubMed] [Google Scholar]
- 44.Gerbeaux P, Ledoray V, Liauthaud H, et al. Medical student effect on emergency department length of stay. Ann Emerg Med. 2001 Mar;37(3):275–278. doi: 10.1067/mem.2001.111709. [DOI] [PubMed] [Google Scholar]
- 45.Yen K, Gorelick MH. Strategies to improve flow in the pediatric emergency department. Pediatric Emergency Care. 2007 Oct;23(10):745–749. doi: 10.1097/PEC.0b013e3181568efe. [DOI] [PubMed] [Google Scholar]
- 46.Cardin S, Afilalo M, Lang E, et al. Intervention to decrease emergency department crowding: does it have an effect on return visits and hospital readmissions? Ann Emerg Med. 2003 Feb;41(2):173–185. doi: 10.1067/mem.2003.50. [DOI] [PubMed] [Google Scholar]
- 47.Urgent Matters . Bursting at the seams: Improving patient flow to help America's emergency departments. The George Washington University; Washington, D.C.: 2004. [Google Scholar]
- 48.Welch SJ, Allen TL. Data-driven quality improvement in the Emergency Department at a level one trauma and tertiary care hospital. J Emerg Med. 2006 Apr;30(3):269–276. doi: 10.1016/j.jemermed.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 49.Forster AJ, Stiell I, Wells G, Lee AJ, van Walraven C. The effect of hospital occupancy on emergency department length of stay and patient disposition. Acad Emerg Med. 2003 Feb;10(2):127–133. doi: 10.1111/j.1553-2712.2003.tb00029.x. [DOI] [PubMed] [Google Scholar]
- 50.Rathlev NK, Chessare J, Olshaker J, et al. Time series analysis of variables associated with daily mean emergency department length of stay. Ann Emerg Med. 2007 Mar;49(3):265–271. doi: 10.1016/j.annemergmed.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 51.Cooke MW, Wilson S, Halsall J, Roalfe A. Total time in English accident and emergency departments is related to bed occupancy. Emerg Med J. 2004 Sep;21(5):575–576. doi: 10.1136/emj.2004.015081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bagust A, Place M, Posnett JW. Dynamics of bed use in accommodating emergency admissions: stochastic simulation model. BMJ. 1999 Jul 17;319(7203):155–158. doi: 10.1136/bmj.319.7203.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lucas R, Farley H, Twanmoh J, et al. Emergency Department Patient Flow: The Influence of Hospital Census Variables on Emergency Department Length of Stay. Acad Emerg Med. 2009 May 11; doi: 10.1111/j.1553-2712.2009.00397.x. [DOI] [PubMed] [Google Scholar]
- 54.Department of Health Clinical exceptions to the 4 hour emergency care target. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndG uidance/DH_4091871. Accessed 10 Jan, 2009.
- 55.Australasian College for Emergency Medicine Access block and overcrowding in emergency departments. http://www.acem.org.au/media/Access_Block1.pdf. Accessed 8 Jan, 2009.
- 56.Kelman S, Friedman JN. Performance improvement and performance dysfunction: an empirical examination of distortionary impacts of the Emergency Room wait-time target in the English NHS. Journal of Public Administration Research and Theory. 2009 doi:10.1093/jopart/mun028. [Google Scholar]
- 57.Department of Health Total time spent in A&E from arrival to admission, transfer or discharge, NHS organisations in England, 2008–09, July to September (Q2) http://www.dh.gov.uk/en/Publicationsandstatistics/Statistics/Performancedataandstatistics/AccidentandEmergency/DH_079085. Accessed 22 Jan, 2009.
- 58.Hughes G. The four hour target; problems ahead. Emerg Med J. 2006 Jan;23(1):2. doi: 10.1136/emj.2005.031948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mortimore A, Cooper S. The “4-hour target”: emergency nurses' views. Emerg Med J. 2007 Jun;24(6):402–404. doi: 10.1136/emj.2006.044933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Locker TE, Mason SM. Are these emergency department performance data real? Emerg Med J. 2006 Jul;23(7):558–559. doi: 10.1136/emj.2005.032748. [DOI] [PMC free article] [PubMed] [Google Scholar]