Abstract
The use of a DNA immunization approach to deliver protective antigens against Yersinia pestis (Y. pestis) has been successful in previously reported studies. In the current study, the gene designs for V and F1, two well-studied virulent factors serving as main targets for vaccine development, were altered to explore additional options in hopes of improving the protective immunity of DNA vaccines expressing these two antigens. Compared to the wild type V gene DNA vaccines, the use of codon optimized V gene sequences was effective in improving the antigen expression, titers of anti-V antibody responses, and survival against a mucosal lethal challenge. For the F1 DNA vaccine, removal of the N-terminal hydrophobic region was able to improve protective immunity. However, adding a mammalian signal peptide sequence to F1 actually led to reduced protection despite it inducing slightly higher anti-F1 antibody responses. The F1 gene can be fused with a gene coding for YscF, a newly confirmed partial protective antigen for Y. pestis, to produce DNA vaccines that express fused F1 and YscF antigens. One design, in particular, that had YscF fused to the downstream sequence of F1, produced better protection than separate F1 or YscF DNA vaccines, suggesting a potential synergistic effect between these two antigens. Findings from the above studies indicated that there are multiple approaches to optimize the protective immunity for plague DNA vaccines. Most importantly, proper antigen engineering to produce optimal antigen gene inserts in DNA vaccines can clearly play a major role in the future designs of a wide range of DNA vaccines.
1. Introduction
Plague, caused by the bacterium, Yersinia pestis (Y. pestis), still remains a potential public health threat in many parts of the world and is also a serious concern as a potential bioterrorism agent. There are two main forms of plague: the bubonic plague, resulting from transmission of the bacteria via the bite of an infected flea, and the pneumonic plague, which is caused by the subsequent spread of the bacteria to the lungs. The pneumonic plague is also transmissible from person to person via airbone transmission and is almost 100% fatal when left untreated. Although vaccines are useful in the prevention of infection by Y. pestis and a number of killed whole-cell (KWC) vaccines and a live attenuated vaccine (EV76) have been developed over the years, various shortcomings and drawbacks have limited their wide use in the prevention of plague in humans [1–4]. Two Y. pestis proteins, fraction 1 capsular protein (F1) and LcrV (V) protein, are known to be protective antigens. In the last decade, subunit vaccines based on F1 and V recombinant proteins have been shown to be immunogenic and protective in various animal studies against plague challenges [5–13]. Subunit vaccines comprising recombinant F1 and V proteins have shown to be immunogenic in a phase I clinical trial but the levels of protective antibody responses are not impressive and may not persist for an extended period [14]. The search for additional protective antigens has only achieved limited progress. A third protective antigen, YscF, was recently reported in several independent studies but the level of protection was only partial when tested in lethal challenge studies in animal models [15–17].
Recently, DNA vaccination has emerged as a novel approach of immunization and is beginning to show promising signs of its utility in humans [18–21]. Previous studies, including our own, have demonstrated that DNA vaccines expressing F1 or V antigens were able to elicit antigen-specific antibody responses and protected animals against lethal plague challenges via mucosal route [22–25]. At the same time, experience accumulated in the studies of DNA vaccines against other pathogens has indicated that the efficacy of DNA vaccines can be further improved from its prototypic design in which the original gene sequence from a pathogen antigen is directly cloned into a DNA vaccine vector. Several well-established strategies including antigen engineering, signal peptide selection, and codon usage optimization can all affect the optimal expression of antigens encoded in DNA vaccines [17, 25–29]. One unique consideration for DNA vaccines that express bacterial antigens is codon usage. If DNA vaccines are developed for human applications, high level expression in mammalian cells is required. However, expression of proteins coded by bacterial genes in mammalian cells can be hampered as codon usage for bacterial genes may not be optimal for protein expression in mammalian cells. Previous studies have shown that codon optimization was effective in improving antigen expression and/or the immunogenicity of DNA vaccines against a wide range of viral pathogens such as Human Immunodeficiency Virus Type 1 (HIV-1) [26–28], influenza [30], and papillomavirus (HPV) [31], and, in limited studies, against bacterial pathogens such as anthrax [32] and tetanus [33].
In the current study, three approaches were taken to further improve plague DNA vaccines. First, for the DNA vaccine expressing the V antigen, there is a previous report showing that a codon optimized V DNA vaccine was not more effective than the wild type V gene DNA vaccine in eliciting anti-V antibodies in mice; however, no attempts were made to determine whether this vaccine was able to increase levels of protection [22]. In the current study, we synthesized a new codon optimized DNA sequence coding for the Y. pestis V antigen with synonymous codon alternation based on the wild type lcrV gene sequences. Mouse studies were conducted to examine whether codon optimization can improve the ultimate protection even if there is no effect on the levels of antibody responses.
Second, a different optimization approach was employed for the F1 antigen in the current study. Recombinant F1 protein is very immunogenic, as are previously developed F1 DNA vaccines [24, 25]. Our previous study also demonstrated that adding a leader sequence of human tissue plasminogen activator (tPA) was able to improve the immunogenicity of an F1 DNA vaccine [25]. However, the other study showed that simple removal of the putative F1 leader sequence was more protective than a modified F1 insert using a signal-bearing E3 polypeptide of Semliki Forest Virus [24]. In order to reconcile this difference, we combined designs from the above two studies by using the leader of tPA in these studies. More significantly we tested the final protection outcome in addition to antibody responses as biomarkers to evaluate different F1 DNA vaccines.
Our previous studies have shown that although F1 and newly confirmed protective antigen YscF-based DNA vaccines were able to elicit protection against mucosal lethal challenge in a mouse model, the protection levels elicited by either of these two antigens were low when compare to that elicited by the V antigen-based DNA vaccines. Therefore, the final approach in the current study was to fuse these two genes into one large DNA vaccine insert to see whether F1 and YscF antigens can work synergistically in this fusion protein design.
2. Materials and Methods
2.1 Bacterial strains
Y. pestis strain KIM 1001 was prepared by growing inocula for 18 h at 37°C on Tryptose Blood Agar Base (Difco) supplemented with 2.5 mM CaCl2 but without the addition of blood. Bacteria were removed from the plate with an inoculating loop and resuspended in injection-grade PBS. The bacteria count in the suspension was correlated to its optical density (OD600). The numbers of bacteria in the final inocula were confirmed by colony counts.
2.2 Construction of DNA vaccine plasmids expressing wild type and codon optimized V DNA vaccines
The codon optimized full length lcrV gene sequence from Y. pestis Kim strain was designed with McVector computer software according to the codon preference in human genes (shown in Table 1) and chemically synthesized by Geneart, Inc. (Germany). The wild type lcrV gene was amplified with pfu DNA polymerase (Strategene, CA) from the virulent plasmid pCD1 of Y. pestis KIM5 with primers V-1 and V-2, as previous described [25]. Either the wild type or codon optimized lcrV gene was individually cloned into the DNA vaccine vector, pSW3891 [34] at PstI and BamHI sites downstream of Cytomegalovirus (CMV) Immediate Early (IE) promoter and its adjacent Intron A. The final DNA plasmids were prepared by using Mega DNA purification kit (QIAGEN, Valencia, CA) for in vitro expression and animal immunization studies.
Table 1.
Primers used in the study
| Primers | Oligonucleotide sequence* | Description |
|---|---|---|
| F1-1 | gtcgctcc AAGCTTHindIII GCTAGC NheI ATGAAAAAAATCAGTTCCGTTATCGCC | caf1, sense |
| F1-2 | agtcac GGATCCBamHI TTATTGGTTAGATACGGTTACGG | caf1, sense |
| F1-3 | ctagtc CTGCAGPstI ATG GATTTAACTGCAAGCACCACTG | caf1, sense |
| F1-4 | accagtcac GTCGACSalI TTG GTT AGA TAC GGT TAC GG | caf1, sense |
| F1-5 | gtcgctcc GCTAGCNheI GATTTAACTGCAAGCACCACTG | caf1, sense |
| F1-7 | atgg ACTAGTSpeI ggcggc GATTTAACTGCAAGCACCACTG | caf1, sense |
| YscF-2 | agtcac GGATCCBamHI TTATGGGAACTTCTGTAGGATGCC | yscF, anti-sense |
| YscF-3 | gtcgctcc GCTAGCNheI AGTAACTTCTCTGGATTTACG | yscF, sense |
| YscF-4 | atgg ACTAGTSpeI ggcggc TGGGAACTTCTGTAGGATGCC | yscF, anti-sense |
| YscF-5 | accagtcac GTCGACSalI ATGAGTAACTTCTCTGGATTTACG | yscF, sense |
The lower case letters indicate the non-specific sequences; the upper case letters indicate the specific sequences matching the target genes. The underlined sequences are the restriction enzyme sites.
2.3 Construction of DNA vaccine plasmids expressing modified F1 DNA vaccines
While there is a hydrophobic region at the N-terminus of F1 protein, it may represent a putative natural signal peptide. Four versions of F1 DNA vaccines were constructed both with and without removing this N-terminal hydrophobic region. The wild type F1 (wt-F1) and tPA-F1 DNA vaccines was constructed, as previously described [25]. The d-F1 gene, following removal of the natural signal peptide, was amplified with primer pairs F1-3/F1-2 or F1-5/F1-2 (Table 1), respectively. Each of the above gene inserts were directly sub-cloned into the previously described DNA vaccine vector pJW4303 PstI-BamHI cloning sites or NheI-BamHI cloning sites immediately downstream of the tPA leader sequence [25, 35], which is in-frame with such sub-cloned inserts. Two DNA vaccines expressing F1 and YscF fusion proteins were constructed: dF1-YscF or YscF-dF1, both with a tPA leader sequence. For dF1-YscF, the dF1 gene fragment with deletion of stop codon was amplified using primers F1-5/F1-4 and the YscF gene was amplified with primers YscF-5/YscF-2, then these two fragments were ligated together by inducing a SalI site and a linker (Val-Asp) in the junction. For YscF-dF1, the YscF gene with deletion of stop codon was amplified with primers YscF-3/YscF-4 and the dF1 gene was amplified with F1-7/F1-2, then these two fragments were ligated together by inducing a SpeI site and a linker (Ala-Ala-Thr-Ser-Gly-Gly) in the junction. The DNA vaccine constructs were verified by restriction digestion and gene sequencing. Sufficient amounts of the DNA vaccines were prepared by the Qiagen Mega plasmid purification kit (Valencia, CA) for in vitro transfection and animal immunization applications.
2.4 In vitro expression of V and F1 antigens
The expression of DNA vaccine constructs was examined by transient transfection of 293T cells [36]. Transfection was done when cells were at approximately 50% confluence on 60-mm dishes by calcium phosphate co-precipitation, using 10 μg of plasmid DNA per dish. The supernatants and cell-lysates were harvested 72 hours after transfection. The V and F1 antigen expressions were confirmed by Western blot. In this system, pooled mouse sera specific to V or F1 antigen were used as detecting antibodies. A homemade quantitative ELISA was used to measure the amounts of V antigen produced from each V DNA vaccine construct. A known amount of recombinant V antigen was used to establish the standard curve.
2.5 DNA Immunization
Female Balb/C mice of 6–8 weeks old were purchased from Taconic Farms (Germantown, NY) and housed in the animal facility managed by the Department of Animal Medicine at the University of Massachusetts Medical School in accordance with IACUC approved protocol. The animals received three biweekly DNA immunizations at Week 0, 2 and 4 by a Bio-Rad Helios gene gun (Bio-Rad, Hercules, CA) and were boosted at Week 8 (one week prior to Y. pestis challenge). The V or F1 DNA vaccines or the empty vector plasmids were coated onto the 1.0-micron gold beads at 2 μg of DNA/mg of gold. Each shot delivered 1 μg of DNA and a total of six non-overlapping shots were delivered to each mouse at the shaved abdominal skin after animals were anesthetized. The serum samples were collected at Week 0, 2, 4, 6, 8 and 9 (prior to challenge).
2.6 ELISA (enzyme-linked immunosorbent assay)
Mouse sera were tested for V or F1-specific IgG antibody responses. Microtiter plates were coated with 100 μl/well of recombinant V or F1 antigen (1 μg/ml in PBS, pH7.2) at 4°C overnight and then washed five times with washing buffer (PBS at pH 7.2 with 0.1% Triton X-100). Blocking was done with 200 μl/well of 4% milk-whey blocking buffer for 1 hour at room temperature. After removal of the blocking buffer and another five washes, 100 μl of serially diluted mouse sera were added and incubated for 1 hour. The plates were washed five times and incubated with 100 μl of biotinylated anti-mouse IgG (Vector Laboratories, Burlingame, CA) diluted at 1:1000 for 1 hour followed with washes. Then, horseradish peroxidase-conjugated streptavidin (Vector Laboratories) diluted at 1:2000 was added (100 μl/well) and incubated for 1 hour. After the final washes, 100 μl of fresh TMB substrate (Sigma) was added per well and incubated for 3.5 min. The reaction was stopped by adding 25 μl of 2 M H2SO4, and the optical density (OD) of the plate was measured at 450 nm.
2.7 Western blot analysis
Plague antigens transiently expressed from 293T-cell supernatants and cell lysates were subjected to denaturing SDS-PAGE and blotted onto PVDF membrane (BioRad). Blocking was done with 0.1% I-Block (Tropix, Bedford, MA). V or F1-specific mouse sera were used as the detecting antibody at 1:500 dilution and incubated for 45 minutes. Subsequently, the membranes were washed with blocking buffer and then reacted with AP-conjugated goat anti-rabbit (Tropix) at 1:5000 dilution. After final wash, Western-light substrate was applied to the membranes for 5 minutes. Once the membranes were dry, Kodak films were exposed to the membrane and developed with an X-Omat processor.
2.8 Animal challenges
Challenge was performed by an intranasal instillation of 50 μl saline containing lethal doses of Y. pestis (KIM strain) into the nostril of ketamine-anesthetized mice. This method leads to rapid infection and is lethal to 100% of non-immunized mice in 3–4 days. The LD50 (median lethal dose) of this challenge model was determined by a previous study (data not shown): 5,000 and 80,000 cfu equals to approximately 15 LD50 and 240 LD50, respectively. Individual mice were challenged two weeks after the fourth immunization and observed twice daily to monitor both morbidity and mortality. All of the studies were conducted in a Biosafety Level 3 containment facility at the Department of Animal Medicine, UMMS.
2.9 Statistical analysis
Statistical analysis was done with the Student’s t-test for significance of differences regarding antibody responses and Fisher’s exact test for percent of protections.
3. Results
3.1 Antigen expression, immunogenicity, and protection efficacy of codon optimized V DNA vaccines
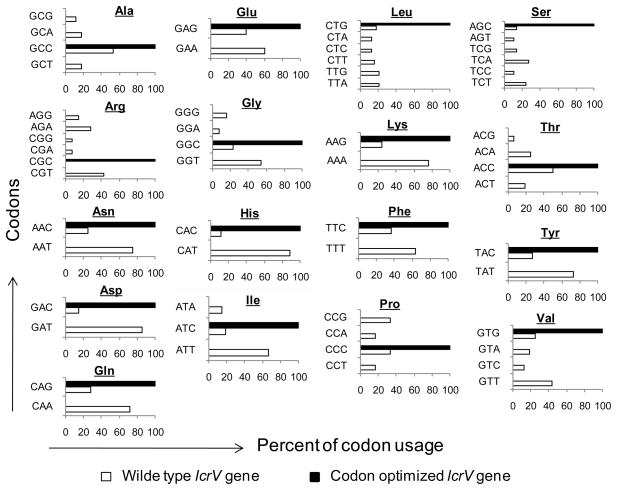
To explore whether codon usage on the lcrV gene can cause any difference in V antigen expression and/or its immunogenicty, we designed and chemically synthesized a codon optimized sequence for the lcrV gene. In the synthetic lcrV gene, most of the codons in the original wild type lcrV gene were alternated with the new codons preferred for its expression in mammalian cells. Some deviations from strict adherence to mammalian cell-preferred codon were made to avoid both changes on certain restriction enzyme sites for subcloning use and any potential inhibitory effects from the secondary RNA structures. Figure 1 shows the codon usages in the wild type and codon optimized lcrV genes. As the results of codon optimization, a dominant codon was used for most amino acids. The DNA sequence analysis showed that the “G+C” content was 63% in the codon optimized lcrV gene and 40% in the wild type lcrV gene. Both wild type (wt) and codon optimized (opt) lcrV genes were individually subcloned into pSW3891 vector, as described in Materials and Methods.
Fig 1.
Comparison of codon usage frequency (%) for each amino acid between the wild type and codon optimized lcrV genes.
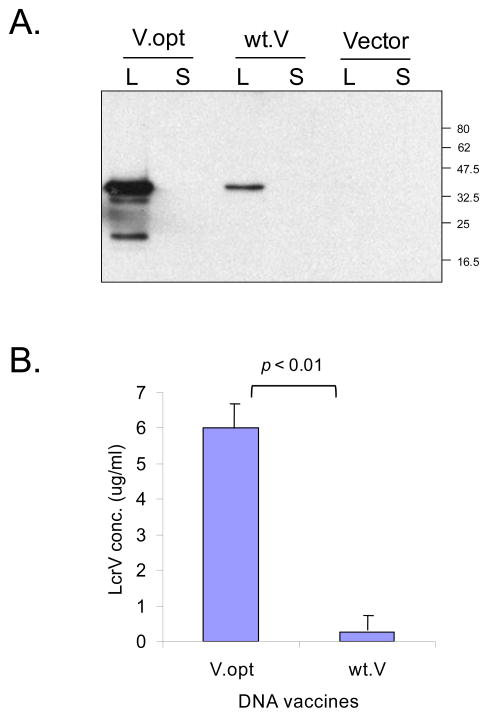
To evaluate the relative potency of the wild type and codon optimized lcrV coding sequence, we compared V antigen expression by these two types of V DNA vaccines in transiently transfected 293T cells. As shown in Figure 2A, V antigen was expressed at a very high level in the 293T cell lysate by the codon optimized V DNA vaccine (V.opt) compared to the wild type V DNA vaccine, based on Western blot analysis. The expression level of V.opt increased over 20-fold, as determined by ELISA (Fig 3B). Since there was no leader sequence in either the wt.V or V.opt DNA constructs, the V antigen was mostly expressed intracellularly in the transfected 293T cell lysate, as predicted.
Fig 2.
Analyses V protein expression by the wild type (wt.V) or codon optimized (V.opt) LcrV DNA vaccine. A. Western-blot analysis of V protein expression by V.opt or wt.V DNA vaccines, or empty vector in supernatant (S) and lysate (L) of transfected 293T cells. B. V protein amount was determined by a quantitative ELISA in 293T cell lysate transfected with either V.opt or wt.V DNA vaccines. The V protein concentration in 293T cell lysate was calculated based on a standard curve of a control recombinant V protein. V-specific mouse sera were used as the detection antibody for Western blot (1:500 dilution) or ELISA (1:1000 dilution).
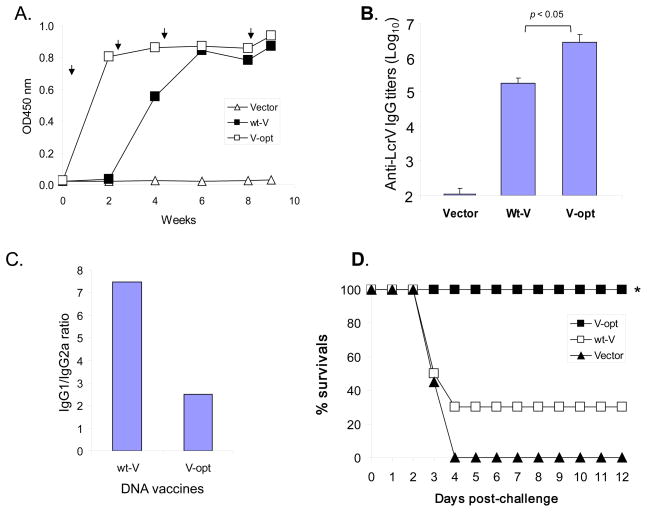
Fig 3.
V-specific immune protection induced by V DNA vaccines. A. Temporal V-specific antibody responses of group-pooled sera at 1:500 serum dilution. The arrows indicate the time-points of DNA immunizations. B. Peak levels of V-specific antibody titers after the 4th DNA immunization. The data show mean titers with standard deviations of 10 Balb/C mice in each group. Statistical difference is indicated between V.opt and wt.V DNA immunization groups. C. The IgG1/IgG2a ratios in V.opt and wt.V DNA immunized mice at peak antibody responses. D. In vivo protections of mice immunized with different V DNA vaccines as indicated. The Balb/C mice were challenged with a lethal dose of 80000 cfu Y. pestis by intranasal inoculation at one week after the 4th DNA immunization. The percent of survival of each group of 10 Balb/C mice is shown. * indicates the significant difference (p < 0.05) of survival rates between V.opt and wt.V DNA immunization groups.
In order to analyze whether high level in vitro expression of V antigen could be translated into stronger immune responses in vivo, groups of Balb/C mice (20 per group) were immunized with either wt.V or V.opt DNA vaccines, in addition to empty DNA vector pSW3891 as the negative control, by a gene gun at Weeks 0, 2, 4 and 8. The antibody responses were measured by ELISA with the sera pooled from animals in the same group over different time points. Consistent with the in vitro expression results, the codon optimized V DNA vaccine induced quicker and higher antibody responses than the wt.V DNA vaccine (Fig. 3). Serum V-specific IgG responses induced by V.opt were detected even after the first DNA immunization. In contrast, the antibody response induced by the wt.V DNA vaccine was only detected after the second DNA immunization at a relatively low level. Peak-level V-antigen specific IgG titers were measured with individual mouse sera within each group and the mean titers for each group were compared between two V DNA vaccines (Fig. 3B). At Week 9, one week after the 4th DNA immunization, the mean V-specific IgG titer in the V.opt DNA vaccine group was about 10-fold higher than that observed in the wt.V immunized group. Further analysis showed that both wt.V and V.opt elicited a Th2-type antibody response with the ratio of IgG1/IgG2a responses being greater than 1 (Fig 3C).
Mice immunized with the above described DNA vaccines were challenged at Week 10. Each animal was inoculated with a highly lethal challenge of Y. pestis Kim strain at 80,000 cfu (equivalent to 240 LD50) by the intranasal route. Animals that received the DNA vector control quickly developed easily observable signs of infection, such as rough coats, hunched or huddled postures, shivering, labored breathing, and lethargy, within the first 24–36 hours and all 20 mice died within 4 days (Fig 3D). Partial protection was generated by the wt.V DNA vaccine with 6 out of 20 mice (30%) surviving at two weeks after challenge (Fig 3D). Full protection was achieved by V.opt DNA vaccine with 100% (20 of 20 mice) of animals surviving at the two weeks of the study period (Fig 3D). All of non-protected mice exhibited signs of sickness shortly after the challenge and usually died within 3- 4 days. No obvious sickness was observed among the surviving animals. The difference in survival between wt.V and V.opt was statistically significant (p<0.005).
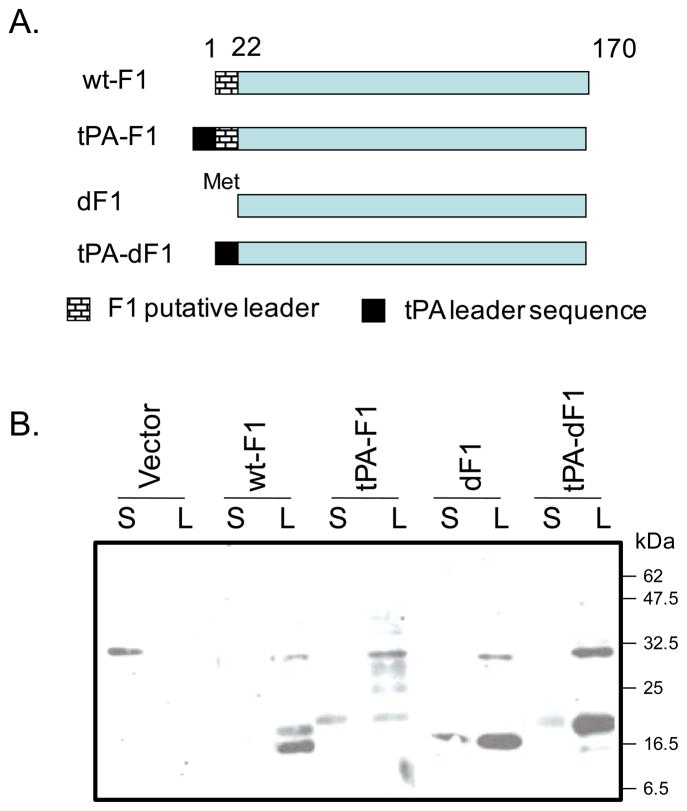
3.2 Expression, immunogenicity, and protection efficacy of F1 DNA vaccines with different N-terminal sequences
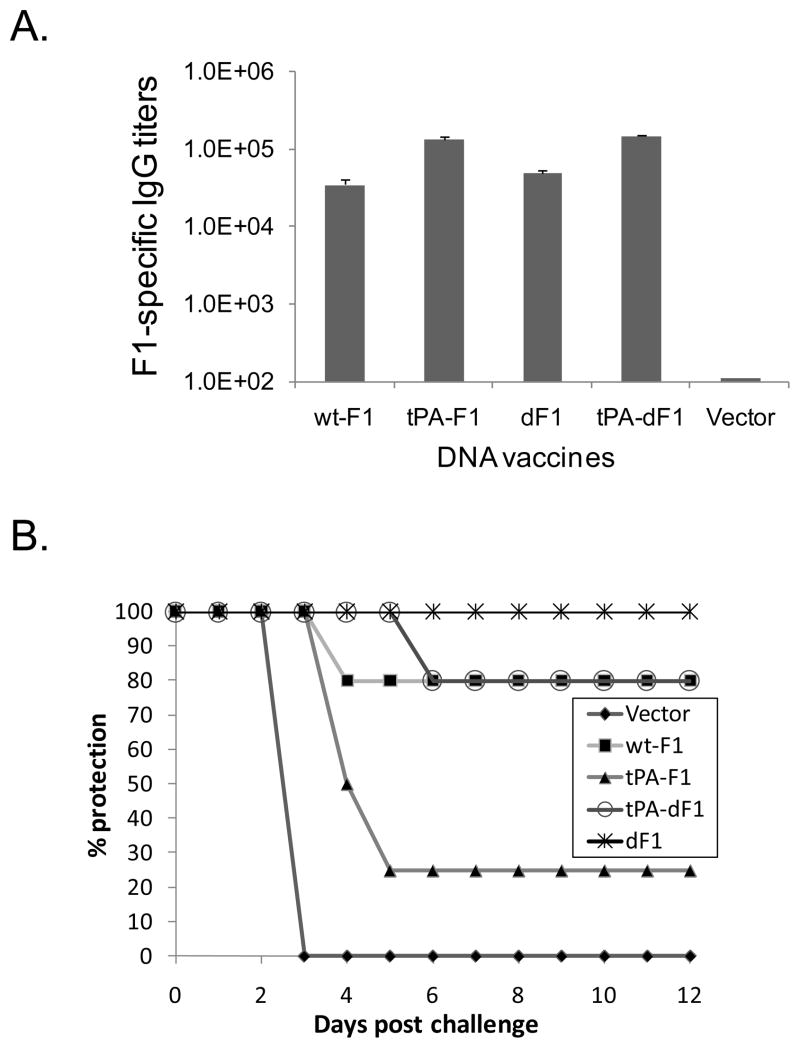
Four versions of F1 antigen inserts were designed for F1 DNA vaccines in the current study (Fig 4A). Our previous studies demonstrated that DNA vaccines with the full length F1 gene (wt-F1), with or without a tPA leader sequence upstream of the full length F1 gene (tPA-F1), could produce partial protection against intranasal challenge with Y. pestis in mice [24, 25]. Although the addition of a tPA leader to the full length F1 sequence was able to achieve more detectable secretion of F1 protein in the supernatant of transiently transfected 293T cells (Fig 4B) and a moderate increase in antibody responses (Fig 5A), the tPA-F1 DNA vaccine was not effective in generating better protection against Y. pestis challenge than the full length F1 DNA vaccine. The level of protection in animals that were immunized with tPA-F1 DNA vaccine was significantly reduced to only 25% of survival against intranasal challenge of 5,000 cfu (~15 LD50) while the wt-F1 DNA vaccine was able to protect about 80% of the mice receiving the same intranasal challenge (Fig 5B), (p < 0.05).
Fig 4.
A. Schematic diagram of gene inserts in F1 DNA vaccine constructs. The numbers indicate the amino acid positions. The weaved or solid boxes represent the putative F1 natural leader or tPA-leader sequence, respectively. (b) Western-blot analysis of the F1 protein expression by different F1 DNA vaccines in supernatant (S) or lysate (L) of transfected 293T cells.
Fig 5.
A. F1-specific IgG responses induced by different F1 DNA vaccines in Balb/C mice. The F1-specific IgG titers were measured by ELISA. Results shown were mean titers of each group (5 mice per group) after the 4th DNA immunization. B. Protection of mice immunized with different F1 DNA vaccines. The Balb/C mice were challenged with a lethal dose of 5000 cfu Y. pestis by intranasal inoculation at one week after the 4th DNA immunization. Cumulative survival curves were plotted to show the protection for each group as indicated. Vector control group was included as the negative control.
Two additional F1 DNA inserts were tested in the current study by removing a short segment of gene sequences at the N-terminus of F1 that codes for 21 hydrophobic amino acid residues. It is not clear whether this segment has the similar function as the putative leader sequence usually associated with many mammalian proteins. Two versions of this modified F1 gene without the N-terminal hydrophobic segment were produced, one with a starting codon ATG (dF1) and the other with an extra leader sequence from the human tissue plasminogen activator (tPA) protein (tPA-dF1) (Fig 4A). Transient expression of F1 demonstrated that both versions of the dF1 DNA vaccine were able to express F1 antigen in transfected 293T cells, not only in lysate but also in supernatant (Fig 4B). Both dF1 and tPA-dF1 DNA vaccines induced good levels of antibody responses (ranging 104 ~105) but not significantly different from those induced by wt-F1 and tPA-F1 DNA vaccines (Fig 5A). However, the dF1 DNA vaccine induced clear protection benefit with 100% survival against intranasal challenge (Fig. 5B). While the tPA-dF1 DNA was less effective in eliciting protection than the dF1 DNA vaccine, it still achieved the same level of protection (80% survival) as did the wt-F1 DNA vaccine (Fig 5B).
Combining the protection results from each of the four F1 DNA vaccines made it clear that adding a tPA leader to either the wild type F1 or the dF1 that had the N-terminal hydrophobic segment removed was counterproductive and elicited lower levels of protection than their counterparts without the tPA leader. Due to the small difference in survival rate (~20%), it was not statistically significant between dF1 (or wt-F1) and tPA-dF1 groups by Fisher’s exact test although each group already included 10 mice per group.
3.3 Expression, immunogenicity, and protection efficacy of F1 and YscF fusion DNA vaccines
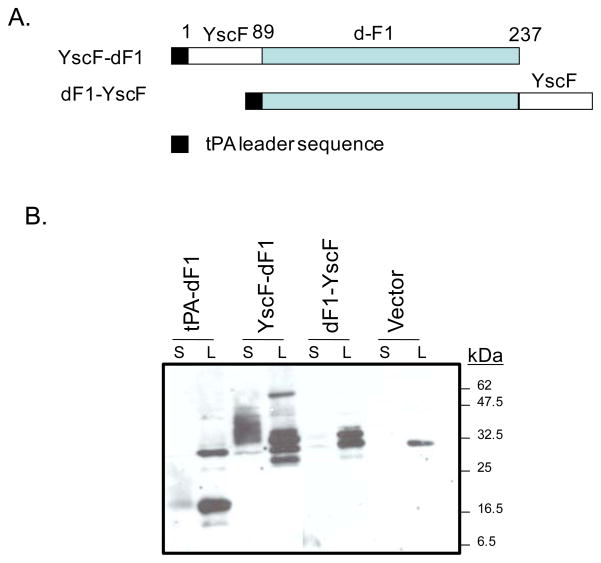
YscF, a recently identified, third protective antigen against plague, has very small molecular weight (~6.7 kDa) without any putative leader sequence. We have demonstrated in a previous study that YscF, like F1, could only produce partial protection against plague in mice and its effect was not as powerful as the V antigen [17, 25]. In order to determine whether there is any synergistic effect if a fusion protein containing both F1 and YscF antigen components is constructed, we designed two versions of DNA vaccines expressing both F1 and YscF antigens (Fig 6A). Depending on whether the YscF antigen is fused to the N- or C- terminus of dF1 antigen, they are called YscF-F1 and F1-YscF, respectively. Both YscF-F1 and F1-YscF DNA vaccines were produced by cloning one of the two inserts into the DNA vaccine vector pJW4303 downstream of a tPA leader sequence. The expression of F1 and YscF components by these two fusing antigen DNA vaccines was examined in transiently transfected 293T cells, followed by Western blot analysis. Both fusion antigen DNA vaccines expressed their antigens very well when probed by an F1-specific rabbit serum (Fig 6B). YscF-dF1 had higher overall protein expression and improved secretion of YscF-dF1 in the supernatant (Fig 6B). Similarly, in a separate Western blot analysis, anti-YscF antibody was able to identify both fusion protein antigens but not dF1 antigen alone (data not shown).
Fig 6.
A. Schematic diagram of caf1 and yscF fusion gene inserts in DNA vaccines. The numbers indicate the amino acid positions. The black, open or grey boxes represent the tPA-leader sequence, YscF and dF1 genes, respectively. B. Western-blot analysis of the YscF-dF1 or dF1-YscF fusion proteins using supernatant (S) and lysate (L) from 293T cells transiently transfected with different DNA vaccines or empty vector. dF1 DNA vaccine and vector was used as positive and negative controls. F1-specific mouse sera were used as detection antibody at 1:500 dilution.
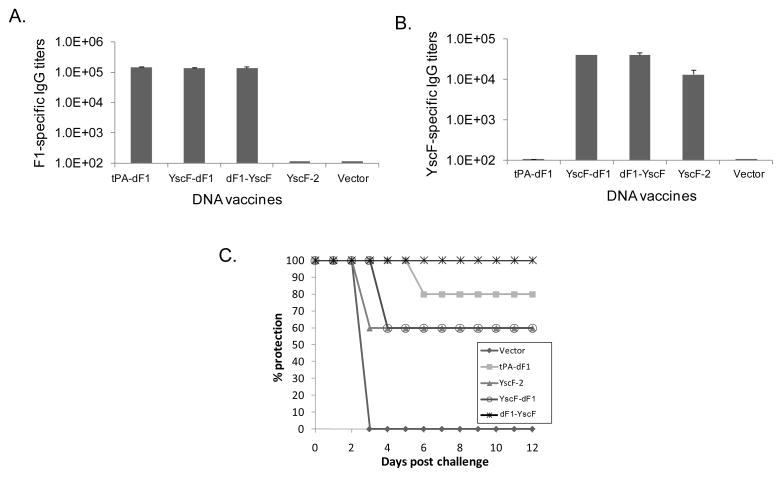
Immunogenicity of these two novel F1 and YscF fusion protein antigens were studied. YscF-F1 and F1-YscF DNA vaccines induced similar titers of F1 antigen-specific antibody responses (~105) to that elicited by the tPA-dF1 DNA vaccine (Fig 7A). The same immune sera can also recognize YscF-2 antigen with equal strength (titers ~104), similar to that elicited by the YscF-2 DNA vaccine (Fig. 7B). Control DNA vaccines expressing either F1 or YscF antigens could only elicit antibody responses against one but not both antigens (Fig 7a and 7B). These results indicated that both F1 and YscF fusion DNA vaccines are immunogenic in eliciting antibodies against both F1 and YscF antigens.
Fig 7.
Antigen-specific responses and in vivo protection induced by YscF-dF1 and dF1-YscF DNA vaccine in Balb/C mice. YscF-2 and tPA-F1 DNA vaccines or empty vector were used as positive or negative controls, respectively. A. F1-specific IgG titers in immunized mouse sera. B. YscF-specific IgG titers in mouse immunized sera. The F1- or YscF-specific IgG titers were measured by ELISA using F1 or YscF-2 as coating antigen, respectively. Results shown here were mean titers of each group (5 mice per group) after the 4th DNA immunization. B. In vivo protections of the Balb/C mice against intranasal challenge with a lethal dose of 5000 cfu Y. pestis at one week after the 4th DNA immunization. Cumulative survival curves were plotted to show the protection for each group as indicated.
Immunized animals were subsequently challenged with 5,000 cfu of Y. pestis by intranasal inoculation. A 100% protection was achieved in the group immunized with the F1-YscF DNA vaccine (Fig 7c), which was better than groups immunized with either the F1 alone (tPA-dF1, 80% survivals) or YscF-2 alone (60% survivals) DNA vaccines. Interestingly, only 60% of the mice survived in the other group that received fusion antigen YscF-F1 DNA vaccine, which was the same as the YscF-2 DNA vaccine group but lower than tPA-dF1 DNA vaccine group (Fig 7C). The mock DNA immunization group (received empty DNA vector without a Y. pestis antigen insert) quickly developed easily observable signs of sickness and died within the first 3 days post-challenge (Fig. 7C).
4. Discussion
In the current report, we used different approaches to further improve the immunogenicity and protection efficacy of plague DNA vaccines expressing V or F1 alone, or F1 fused with YscF. The results showed that immunogenicity of bacterial antigens can be improved by using either a well-established approach, such as codon optimization or some other less studied approaches, such as antigen engineering.
The Y. pestis genome harbors three plasmids necessary for full virulence of the bacterium besides the chromosome. Based on the analysis of genes with coding sequence equal to or larger than 300 bps, the overall “G+C” content was 47.64% in the whole Y. pestis genome [37]. The synonymous codon usage pattern of these genes was different. Gene expression levels are strongly related to the frequency of “G+C” at the third position of synonymous codon usage [37]. Sequence analysis for the Y. pestis gene coding for V protein, lcrV, as part of the 70-kb low calcium response (lcr) plasmid, showed a “G+C” content of only 37.71%. Because codon usage is directly linked to preferred tRNA usage in a given cell type, it is conceivable that codon optimization for LcrV gene is important for its high level expression of this bacterial protein in mammalian cells [38]. However, in a previous report, codon optimization for the V gene based on murine codon preference did not make any difference in a DNA vaccine vector pVAX1-CMV-TE when it was tested in mice and the peak anti-V antibody titers were measured [22]. Results in the current study showed that codon optimization is very effective in not only eliciting higher antibody responses but also in improving protection when compared to the wild type V gene-based DNA vaccine.
There are several differences between these two studies. First, the exact levels of codon changes may be different, however, since no sequence information is available for the previous study, it is hard to compare the exact sequence difference between the two studies. In our study, we also made sure to minimize sequence changes that may generate inhibitory secondary RNA structures. It is not known whether a similar analysis was incorporated in the previous study. It is quite unusual that in the previous report that one group of mice immunized with the codon optimized V gene DNA vaccine had worse immune responses than the wild type V gene DNA vaccine. It appeared that some changes in the codon optimized V gene had a negative effect on the otherwise immunogenic wild type V gene. Second, the study approaches were different in these two reports. In the study conducted by Garmory et al., the comparison between the codon optimized and the wild type V DNA vaccines was done in mice using only intramuscular (im) immunization and mice required up to five im immunizations before any positive anti-V antibody titers could be detected [22]. However, in our previous [25] and current studies, strong positive anti-V IgG responses can be easily detected within two DNA immunizations delivered by a gene gun. It was shown recently that both the physical DNA delivery methods (gene gun or electroporation) were much more effective than the intramuscular needle injection method [39]. Because the overall antibody levels were so low in the previous report [22], a protein boost had to be given in order to detect any difference between codon optimized and wild type V genes when they were used as a prime immunization, which may bring more variables to the final measurement. Finally, in the current study, the protection results from the challenge study provide more definitive evidence to support the survival benefit of codon optimized V DNA vaccine while the previous study did not test such a difference in challenge studies between the vaccine formulations with different codon usages.
A different optimization approach was employed for the F1 antigen in the current study. F1 is a 17.5 kDa protein which is considered an important but not essential virulence factor unique to Y. pestis. The reason for this is because the F1-negative mutant bacterial strains do not abolish virulence of Y. pestis but lead to a delay in onset of the disease in animal models [40, 41]. Recombinant F1 protein is very immunogenic as are F1 DNA vaccines [24, 25]. Our previous study also demonstrated the addition of the leader sequence of human tissue plasminogen activator (tPA) in front of the entire original coding sequence for F1 was able to improve the immunogenicity of F1 DNA vaccine [25], but a study from another group showed that the removal of a putative F1 leader sequence from the F1 coding sequence was more protective than adding a signal-bearing E3 polypeptide of Semliki Forest Virus [24]. In order to reconcile such differences, we combined designs from the above two studies by using the leader of tPA in these studies.
The leader sequence of tPA has been shown in multiple DNA vaccine studies to produce more secreted downstream protein in mammalian expression systems. As a result, immunogenicity of many DNA vaccines with a tPA leader is also improved as shown by higher antibody responses including the envelope protein of HIV-1 [26] and LcrV protein of Y. pestis [25]. Because the original F1 gene has a short hydrophobic segment in its N-terminus, which may serve as a putative leader sequence for a bacterial protein, we tested the effect of adding a tPA leader to the F1 gene, with and without the removal of this putative F1 leader.
Adding a tPA leader to both types of F1 genes was able to increase the secretion of F1 protein, as shown by increased detection of F1 in culture supernatant, and to improve the levels of anti-V IgG responses. However, the protection results showed that the addition of a tPA leader led to lower protection when compared to counterparts without a tPA leader. This was the case between either the tPA-F1 and F1 pair or the tPA-dF1 and dF1 pair, i.e., removal or not of the putative F1 leader did not make the addition of a tPA leader more effective. This finding was further confirmed by the data that the protection levels for F1 (keeping the original putative leader) and tPA-dF1 (replacing the putative leader with a new tPA leader) were similar. The worst among the four F1 DNA vaccine designs was tPA-F1, which basically had two leaders (one from tPA plus the putative F1 leader). The most effective design was dF1, F1 without any N-terminal leader sequence. It is not clear why a “leader-less” F1 is more protective, given the finding that this design did not lead to the highest anti-F1 IgG responses. Future studies should analyze additional bacterial proteins to understand whether bacterial proteins have any unique sequences that may affect their expression in the mammalian system and, more importantly, their functional conformation in eliciting protective immune responses. This knowledge is important not only to DNA vaccines but also to recombinant protein-based bacterial vaccines, which only started to enter the vaccine development pipeline in recent years. DNA vaccine studies, as presented in the current report, can certainly be used as very valuable tools to any subunit-based vaccine studies.
Bacteria vaccines can take advantage of the large number of proteins associated with this type of pathogen by including multiple antigens in one vaccine formulation to improve the efficacy of a vaccine or to minimize the escape of vaccine-induced protection. However, technically, a polyvalent subunit-based vaccine can be challenging because of the cost and technical complexity associated with the production of multiple protective vaccine components. In the past, a V-F1 fusion protein was proposed to minimize such issues associated with physically separate, bivalent V and F1 protein vaccines. In the current report, we tested the same concept by making F1 and YscF fusion antigens, which were then tested by DNA immunization.
Our results indicate that DNA vaccines expressing F1 and YscF fusion proteins could induce antigen-specific antibody responses against both F1 and YscF antigens. Two versions of fusion antigens were produced, either F1 upstream of YscF or YscF upstream of F1, and both were immunogenic as evidenced by their ability to generate similar levels of antigen-specific antibody responses. However, improved protection was observed only when the YscF was fused downstream of F1 protein (F1-YscF design) while the other fusion antigen design (YscF-F1) had reduced protection when the tPA-F1 DNA vaccine was used as the baseline control for the protection studies using both fusion antigens. In our previous study, we demonstrated that YscF in its dimer form, but not in the monomer form, was protective [17]. Therefore, we did not include a YscF monomer as the control in the current study. Even with the dimer form of YscF, the protection level was only partial (60% protection against intranasal challenge with 15 LD50 of Y. pestis).
It is also interesting to observe that the YscF-F1 design had much higher levels of secreted antigens than the F1-YscF1, but could not induce better protective immunity than the latter. When the F1 antigen alone was included, we found that it was most protective when it had no leader sequence and did not require high level of secretion, as examined by in vitro assays. Therefore, it may not be a total surprise that a mainly intracellularly expressed F1-YscF fusion protein is more protective than the easily secreted YscF-F1 fusion protein. However, this finding, along several other results presented in the current report, points to the importance of antigen engineering in the next phase of DNA vaccine research. In the past, given the gene-based nature of DNA vaccines, optimization of the DNA vaccine vector and delivery of DNA vaccines have been the main focus of research being conducted. The findings that changes to the coding sequence itself can significantly affect not only the immunogenicity but also protection will bring more attention to the designs of antigen inserts which may affect a wide range of considerations, including antigen conformation, antigen expression, post-translational antigen modification, and ultimately the fate of antigen processing and presentation in vivo which remains largely unknown to DNA vaccines. Results reported here using Y. pestis proteins as model antigens should make antigen engineering the first step of the above complicated process as we previously noted [42].
Acknowledgments
Work presented in this report was partially supported by the NIH/NIAID grant 1U01AI078073.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Meyer KF, Cavanaugh DC, Bartelloni PJ, Marshall JD., Jr Plague immunization. I. Past and present trends. J Infect Dis. 1974 May;129(Suppl):S13–8. doi: 10.1093/infdis/129.supplement_1.s13. [DOI] [PubMed] [Google Scholar]
- 2.Reisman RE. Allergic reactions due to plague vaccine. J Allergy. 1970 Jul;46(1):49–55. doi: 10.1016/0021-8707(70)90061-4. [DOI] [PubMed] [Google Scholar]
- 3.Marshall JD, Jr, Bartelloni PJ, Cavanaugh DC, Kadull PJ, Meyer KF. Plague immunization. II. Relation of adverse clinical reactions to multiple immunizations with killed vaccine. J Infect Dis. 1974 May;129(Suppl):S19–25. doi: 10.1093/infdis/129.supplement_1.s19. [DOI] [PubMed] [Google Scholar]
- 4.Williams JE, Altieri PL, Berman S, Lowenthal JP, Cavanaugh DC. Potency of killed plague vaccines prepared from avirulent Yersinia pestis. Bull World Health Organ. 1980;58(5):753–6. [PMC free article] [PubMed] [Google Scholar]
- 5.Heath DG, Anderson GW, Jr, Mauro JM, Welkos SL, Andrews GP, Adamovicz J, et al. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine. 1998 Jul;16(11–12):1131–7. doi: 10.1016/s0264-410x(98)80110-2. [DOI] [PubMed] [Google Scholar]
- 6.Williamson ED, Eley SM, Griffin KF, Green M, Russell P, Leary SE, et al. A new improved sub-unit vaccine for plague: the basis of protection. FEMS Immunol Med Microbiol. 1995 Dec;12(3–4):223–30. doi: 10.1111/j.1574-695X.1995.tb00196.x. [DOI] [PubMed] [Google Scholar]
- 7.Williamson ED, Eley SM, Stagg AJ, Green M, Russell P, Titball RW. A sub-unit vaccine elicits IgG in serum, spleen cell cultures and bronchial washings and protects immunized animals against pneumonic plague. Vaccine. 1997 Jul;15(10):1079–84. doi: 10.1016/s0264-410x(96)00303-9. [DOI] [PubMed] [Google Scholar]
- 8.Williamson ED, Eley SM, Stagg AJ, Green M, Russell P, Titball RW. A single dose sub-unit vaccine protects against pneumonic plague. Vaccine. 2000 Oct 15;19(4–5):566–71. doi: 10.1016/s0264-410x(00)00159-6. [DOI] [PubMed] [Google Scholar]
- 9.Glynn A, Roy CJ, Powell BS, Adamovicz JJ, Freytag LC, Clements JD. Protection against aerosolized Yersinia pestis challenge following homologous and heterologous prime-boost with recombinant plague antigens. Infect Immun. 2005 Aug;73(8):5256–61. doi: 10.1128/IAI.73.8.5256-5261.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glynn A, Freytag LC, Clements JD. Effect of homologous and heterologous prime-boost on the immune response to recombinant plague antigens. Vaccine. 2005 Mar 14;23(16):1957–65. doi: 10.1016/j.vaccine.2004.10.025. [DOI] [PubMed] [Google Scholar]
- 11.Leary SE, Williamson ED, Griffin KF, Russell P, Eley SM, Titball RW. Active immunization with recombinant V antigen from Yersinia pestis protects mice against plague. Infect Immun. 1995 Aug;63(8):2854–8. doi: 10.1128/iai.63.8.2854-2858.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones SM, Griffin KF, Hodgson I, Williamson ED. Protective efficacy of a fully recombinant plague vaccine in the guinea pig. Vaccine. 2003 Sep 8;21(25–26):3912–8. doi: 10.1016/s0264-410x(03)00379-7. [DOI] [PubMed] [Google Scholar]
- 13.Eyles JE, Williamson ED, Spiers ID, Alpar HO. Protection studies following bronchopulmonary and intramuscular immunisation with yersinia pestis F1 and V subunit vaccines coencapsulated in biodegradable microspheres: a comparison of efficacy. Vaccine. 2000 Aug 1;18(28):3266–71. doi: 10.1016/s0264-410x(00)00128-6. [DOI] [PubMed] [Google Scholar]
- 14.Williamson ED, Flick-Smith HC, Lebutt C, Rowland CA, Jones SM, Waters EL, et al. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect Immun. 2005 Jun;73(6):3598–608. doi: 10.1128/IAI.73.6.3598-3608.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matson JS, Durick KA, Bradley DS, Nilles ML. Immunization of mice with YscF provides protection from Yersinia pestis infections. BMC microbiology. 2005;5:38. doi: 10.1186/1471-2180-5-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swietnicki W, Powell BS, Goodin J. Yersinia pestis Yop secretion protein F: purification, characterization, and protective efficacy against bubonic plague. Protein expression and purification. 2005 Jul;42(1):166–72. doi: 10.1016/j.pep.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 17.Wang S, Joshi S, Mboudjeka I, Liu F, Ling T, Goguen JD, et al. Relative immunogenicity and protection potential of candidate Yersinia Pestis antigens against lethal mucosal plague challenge in Balb/C mice. Vaccine. 2008 Mar 20;26(13):1664–74. doi: 10.1016/j.vaccine.2008.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang S, Kennedy JS, West K, Montefiori DC, Coley S, Lawrence J, et al. Cross-subtype antibody and cellular immune responses induced by a polyvalent DNA prime-protein boost HIV-1 vaccine in healthy human volunteers. Vaccine. 2008 Jul 23;26(31):3947–57. doi: 10.1016/j.vaccine.2007.12.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu S, Wang S, Grimes-Serrano JM. Current progress of DNA vaccine studies in humans. Expert review of vaccines. 2008 Mar;7(2):175–91. doi: 10.1586/14760584.7.2.175. [DOI] [PubMed] [Google Scholar]
- 20.Lu S. Immunogenicity of DNA vaccines in humans: it takes two to tango. Human vaccines. 2008 Nov–Dec;4(6):449–52. doi: 10.4161/hv.4.6.6179. [DOI] [PubMed] [Google Scholar]
- 21.Harari A, Bart PA, Stohr W, Tapia G, Garcia M, Medjitna-Rais E, et al. An HIV-1 clade C DNA prime, NYVAC boost vaccine regimen induces reliable, polyfunctional, and long-lasting T cell responses. The Journal of experimental medicine. 2008 Jan 21;205(1):63–77. doi: 10.1084/jem.20071331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garmory HS, Freeman D, Brown KA, Titball RW. Protection against plague afforded by immunisation with DNA vaccines optimised for expression of the Yersinia pestis V antigen. Vaccine. 2004 Feb 25;22(8):947–57. doi: 10.1016/j.vaccine.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 23.Grosfeld H, Bino T, Flashner Y, Ber R, Mamroud E, Lustig S, et al. Vaccination with plasmid DNA expressing the Yersinia pestis capsular protein F1 protects mice against plague. Adv Exp Med Biol. 2003;529:423–4. doi: 10.1007/0-306-48416-1_84. [DOI] [PubMed] [Google Scholar]
- 24.Grosfeld H, Cohen S, Bino T, Flashner Y, Ber R, Mamroud E, et al. Effective protective immunity to Yersinia pestis infection conferred by DNA vaccine coding for derivatives of the F1 capsular antigen. Infect Immun. 2003 Jan;71(1):374–83. doi: 10.1128/IAI.71.1.374-383.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang S, Heilman D, Liu F, Giehl T, Joshi S, Huang X, et al. A DNA vaccine producing LcrV antigen in oligomers is effective in protecting mice from lethal mucosal challenge of plague. Vaccine. 2004 Sep 3;22(25–26):3348–57. doi: 10.1016/j.vaccine.2004.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang S, Farfan-Arribas DJ, Shen S, Chou TH, Hirsch A, He F, et al. Relative contributions of codon usage, promoter efficiency and leader sequence to the antigen expression and immunogenicity of HIV-1 Env DNA vaccine. Vaccine. 2006 May 22;24(21):4531–40. doi: 10.1016/j.vaccine.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 27.Andre S, Seed B, Eberle J, Schraut W, Bultmann A, Haas J. Increased immune response elicited by DNA vaccination with a synthetic gp120 sequence with optimized codon usage. J Virol. 1998 Feb;72(2):1497–503. doi: 10.1128/jvi.72.2.1497-1503.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haas J, Park EC, Seed B. Codon usage limitation in the expression of HIV-1 envelope glycoprotein. Curr Biol. 1996 Mar 1;6(3):315–24. doi: 10.1016/s0960-9822(02)00482-7. [DOI] [PubMed] [Google Scholar]
- 29.Kutzler MA, Weiner DB. DNA vaccines: ready for prime time? Nature reviews. 2008 Oct;9(10):776–88. doi: 10.1038/nrg2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang S, Taaffe J, Parker C, Solorzano A, Cao H, Garcia-Sastre A, et al. Hemagglutinin (HA) proteins from H1 and H3 serotypes of influenza A viruses require different antigen designs for the induction of optimal protective antibody responses as studied by codon-optimized HA DNA vaccines. J Virol. 2006 Dec;80(23):11628–37. doi: 10.1128/JVI.01065-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheung YK, Cheng SC, Sin FW, Xie Y. Plasmid encoding papillomavirus Type 16 (HPV16) DNA constructed with codon optimization improved the immunogenicity against HPV infection. Vaccine. 2004 Dec 16;23(5):629–38. doi: 10.1016/j.vaccine.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 32.Herrmann JE, Wang S, Zhang C, Panchal RG, Bavari S, Lyons CR, et al. Passive immunotherapy of Bacillus anthracis pulmonary infection in mice with antisera produced by DNA immunization. Vaccine. 2006 Jul 26;24(31–32):5872–80. doi: 10.1016/j.vaccine.2006.04.065. [DOI] [PubMed] [Google Scholar]
- 33.Stratford R, Douce G, Zhang-Barber L, Fairweather N, Eskola J, Dougan G. Influence of codon usage on the immunogenicity of a DNA vaccine against tetanus. Vaccine. 2000 Nov 22;19(7–8):810–5. doi: 10.1016/s0264-410x(00)00246-2. [DOI] [PubMed] [Google Scholar]
- 34.Wang S, Chou TH, Sakhatskyy PV, Huang S, Lawrence JM, Cao H, et al. Identification of two neutralizing regions on the severe acute respiratory syndrome coronavirus spike glycoprotein produced from the mammalian expression system. J Virol. 2005 Feb;79(3):1906–10. doi: 10.1128/JVI.79.3.1906-1910.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lu S, Wyatt R, Richmond JF, Mustafa F, Wang S, Weng J, et al. Immunogenicity of DNA vaccines expressing human immunodeficiency virus type 1 envelope glycoprotein with and without deletions in the V1/2 and V3 regions. AIDS research and human retroviruses. 1998 Jan 20;14(2):151–5. doi: 10.1089/aid.1998.14.151. [DOI] [PubMed] [Google Scholar]
- 36.Pear WS, Nolan GP, Scott ML, Baltimore D. Production of high-titer helper-free retroviruses by transient transfection. Proceedings of the National Academy of Sciences of the United States of America. 1993 Sep 15;90(18):8392–6. doi: 10.1073/pnas.90.18.8392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hou ZC, Yang N. Factors affecting codon usage in Yersinia pestis. Sheng Wu Hua Xue Yu Sheng Wu Wu Li Xue Bao (Shanghai) 2003 Jun;35(6):580–6. [PubMed] [Google Scholar]
- 38.Lindler LE, Plano GV, Burland V, Mayhew GF, Blattner FR. Complete DNA sequence and detailed analysis of the Yersinia pestis KIM5 plasmid encoding murine toxin and capsular antigen. Infect Immun. 1998 Dec;66(12):5731–42. doi: 10.1128/iai.66.12.5731-5742.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang S, Zhang C, Zhang L, Li J, Huang Z, Lu S. The relative immunogenicity of DNA vaccines delivered by the intramuscular needle injection, electroporation and gene gun methods. Vaccine. 2008 Apr 16;26(17):2100–10. doi: 10.1016/j.vaccine.2008.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sebbane F, Jarrett C, Gardner D, Long D, Hinnebusch BJ. The Yersinia pestis caf1M1A1 fimbrial capsule operon promotes transmission by flea bite in a mouse model of bubonic plague. Infect Immun. 2009 Mar;77(3):1222–9. doi: 10.1128/IAI.00950-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Davis KJ, Fritz DL, Pitt ML, Welkos SL, Worsham PL, Friedlander AM. Pathology of experimental pneumonic plague produced by fraction 1-positive and fraction 1-negative Yersinia pestis in African green monkeys (Cercopithecus aethiops) Archives of pathology & laboratory medicine. 1996 Feb;120(2):156–63. [PubMed] [Google Scholar]
- 42.Lu S, Manning S, Arthos J. Antigen engineering in DNA immunization. In: Lowrie DaW R, editor. Methods in Molecular Medicine DNA Vaccines. Humana Press; 1999. pp. 355–74. [DOI] [PubMed] [Google Scholar]