Abstract
D-cyclin proteins play a central role in cell cycle regulation and are involved in the pathogenesis of lymphomas. In mantle cell lymphoma, the t(11;14) translocation leads to the overexpression of cyclin D1, in addition to which cyclin D1-negative mantle cell lymphoma that overexpress cyclin D2 or D3 have also been described. Although cyclins D2 and D3 have been implicated in the prognosis of specific lymphoma subtypes, a thorough characterization of D-cyclin protein expression in human hematolymphoid neoplasia has not been reported. To evaluate the tissue expression patterns of D-cyclins, particularly D2 and D3, in normal and neoplastic hematolymphoid tissues, we optimized commercially available antibodies for D-cyclins for use on paraffin-embedded tissue and stained tissue microarrays of over 700 patient samples. Our results show that cyclin D2 and D3 proteins are expressed in many more lymphoma subtypes than cyclin D1. Cyclins D1, D2 and D3 were expressed in 100%, 22% and 6% of mantle cell lymphoma and 2%, 49% and 20% of diffuse large B-cell lymphoma. Fluorescence in situ hybridization studies confirmed the presence of the CCND1/IGH translocation in the majority of mantle cell lymphoma but not in diffuse large B-cell lymphoma that expressed cyclin D1 protein. In addition, a subset of follicular, marginal zone, lymphoplasmacytic, lymphoblastic, classical Hodgkin, mature T- and Natural Killer cell lymphomas and acute myeloid leukemias also expressed cyclins D2 and D3. These data support the hypothesis that dysregulation of cell cycle control by D-cyclins contribute to the pathogenesis of hematolymphoid neoplasia, and suggest a potential role for these proteins in the prognostic and therapeutic aspects of these diseases. For diagnostic purposes, however, the expression of D-cyclin proteins should be interpreted with caution in the subclassification of lymphoma types.
Keywords: Cyclin D2, cyclin D3, CCND2, CCND3, diffuse large B-cell lymphoma, tissue microarray, immunohistochemistry, FISH
INTRODUCTION
Cyclins are an evolutionarily conserved family of proteins that play an important role in the regulation of the cell cycle by binding cyclin-dependent kinases. They are synthesized and destroyed in a precise manner and this periodicity enables specific cyclin-dependent kinase-cyclin complexes to facilitate the sequential events that take place during cell cycle progression.1 D-cyclins (D1, D2, and D3) are structurally and functionally similar proteins that bind and activate cyclin-dependent kinases 4 and 6 during the G1 phase of the cell cycle as the cell prepares to initiate DNA synthesis.1–3 In mammalian cells, deregulation of these proteins lead to significantly increased cell proliferation and turnover.
Overexpression of D-cyclins has been implicated in the pathogenesis of lymphomas.4 Translocation t(11;14)(q13;q32) at the cyclin D1 locus is the hallmark of mantle cell lymphoma.5,6 Although cyclin D1 is overexpressed in the majority of mantle cell lymphoma, recent studies using gene expression profiling have identified cyclin D1-negative mantle cell lymphoma that overexpress cyclin D2 or cyclin D3.7 Additional studies have revealed specific translocations involving the CCND2 and CCND3 loci that lead to the overexpression of their cognate cyclin D2 or D3 proteins in cyclin D1-negative mantle cell lymphoma.8–10 In a multivariate model correlating the expression of six genes (as measured by quantitative RT-PCR) that predicts outcome in patients with diffuse large B-cell lymphoma, we had previously identified CCND2 as a marker of poor prognosis.11,12 Overexpression of the cyclin D2 protein was also found to be an independent predictor of inferior 5-year overall survival in diffuse large B-cell lymphoma patients.13 The overexpression of cyclin D3 protein in indolent lymphomas has been associated with adverse clinical features including a high-intermediate or high-risk International Prognostic Index, and poor overall and relapse-free survival.14
The role of D-cyclins in hematolymphoid neoplasms is becoming increasingly recognized. Although the tissue distribution pattern of cyclin D1 protein has been previously documented, there are limited data for cyclin D2 and D3 proteins. Because cyclin D2 and D3 immunostaining is likely to be employed for differentiating cyclin D1-negative mantle cell lymphoma from other lymphoma subtypes, and cyclin D2 may have clinical utility as a prognostic marker in diffuse large B-cell lymphoma, it is of importance to know their tissue distribution pattern and reactivity in hematopoietic neoplasms. Therefore, our aim in this study was to characterize the expression profiles of D-cyclin proteins, particularly cyclins D2 and D3, in a wide variety of normal and neoplastic tissue samples obtained from formalin-fixed and paraffin-embedded patient biopsies. We document the differential expression patterns of D-cyclins and explore the utility of immunohistogic staining for D-cyclins in the diagnostic setting.
MATERIALS AND METHODS
Tissue Samples
Formalin-fixed, paraffin-embedded tissue samples of normal and neoplastic hematolymphoid cases were obtained from the archives of the Departments of Pathology, Stanford University Medical Center, Stanford, California. Institutional Review Board (IRB) approval was obtained for these studies. The cases were studied by immunohistochemistry and fluorescence in situ hybridization (FISH) on tissue microarrays, and on whole sections wherever detailed evaluation was deemed necessary. For expression in normal hematopoietic tissues, 3–5 examples each of tonsil, lymph node, thymus, spleen and bone marrow core biopsies were used. Hematolymphoid neoplasia were classified according to the current World Health organization (WHO) scheme.6 Tissue microarray (TMA) construction has been described previously.15,16
To screen for the expression of D-cyclin proteins in non-hematopoietic tissue, TMAs containing 100 samples of various tissues (neoplastic and non-neoplastic) were used. Two samples each of the following normal tissue samples were analyzed: adrenal, bladder, brain, breast, colon, kidney, liver, lung, muscle (heart and skeletal), ovary, pancreas, prostate, stomach, testis, thyroid and uterus. Neoplastic tissue samples included carcinomas of the adrenal cortex (2), bladder (2), breast (8), colon (6), head and neck squamous cell (2), liver (4 hepatocellular and 4 cholangiocarcinoma), lung (4 adenocarcinoma and 4 squamous cell carcinoma), ovary (6), parathyroid (4), prostate (3), stomach (2), thyroid (2) and uterus (4) as well as glioblastoma multiforme (2), seminoma (2), and soft tissue sarcomas (13).
Immunohistochemistry
Serial 4 μM-thick sections from paraffin-embedded whole tissue sections and tissue microarray blocks were deparaffinized in xylene and hydrated in a series of graded alcohols. Antibodies directed against D-cyclins were used at a dilution of 1:100 for anti-cyclin D1 (clone SP4, Thermo Fisher Scientific, Fremont, CA), 1:400 for anti-cyclin D2 (clone M-20, Santa Cruz Biotechnology, Santa Cruz, CA), and 1:30 for anti-cyclin D3 (clone DCS-22, Santa Cruz Biotechnology, Santa Cruz, CA). DAKO citrate retrieval and detection using the DAKO Envision method was carried out (DAKO Corporation, Carpinteria, CA).
Staining for cyclin D2 and D3 proteins was optimized on normal paraffin-embedded tonsil sections. Cyclin D2 staining was primarily localized to the nucleus although a combination of nuclear and cytoplasmic staining was frequently seen in positive cell types. Weak cytoplasmic staining without corresponding nuclear staining was not considered positive. Cyclin D3 staining was crisply localized to the nucleus and resembled cyclin D1 staining. A cut-off of staining in greater than 20% of lymphoma cells was assigned a positive score. This cut-off was based on the need for using a non-ambiguous threshold for scoring TMAs and does not reflect differences in staining intensity between normal and neoplastic tissue or among different diagnoses. The cut-off was chosen before correlation with other immunohistologic markers. The distinction between positive and negative cases was relatively straightforward using standard light microscopy. Two pathologists (RM and YN) independently scored all cases and any discrepancies were resolved by re-scoring over a double-headed microscope.
Double-immunohistochemical labeling for both cyclin D2 (1:60 dilution) and cyclin D3 (1:30 dilution) was carried out using the DAKO EnVision G2 doublestaining system (DAKO, Carpinteria, CA). Heat-induced antigen retrieval was performed using the Decloaking Chamber (Biocare Medical, Concord, CA) in Tris/EDTA buffer (50mM TRIS/20mM EDTA, pH 9.0). Antibodies directed against the following markers were used in combination with cyclin D2 or cyclin D3: CD20 (1:1000 dilution, DAKO), CD3 (1:100 dilution, Cell Marque Corp., Rocklin, CA), CD34 (1:10 dilution, BD Biosciences, San Jose, CA), myeloperoxidase (1:8000 dilution, DAKO, Carpinteria, CA), and glychophorin (1:100 dilution, DAKO).
Fluorescence in situ hybridization (FISH)
Formalin-fixed, paraffin-embedded thin tissue sections were pretreated by standard protocol using the VP2000™ slide pretreatment instrument (Abbott Molecular, Abbott Park, IL). Briefly, slides were deparaffinized with CitroSolv™ (Fisher Scientific, Pittsburg, PA), digested with a 10% pepsin solution at 37°C (Protease I, VP2000™ Protease Buffer; Abbott Molecular), pre-treated with a sodium thiocyanate solution at 80°C (VP2000™ Pretreatment Solution; Abbott Molecular), re-fixed in 10% buffered formalin, and dehydrated in an ethanol series.
Dried, dehydrated slides were denatured with a Vysis® HYBrite instrument at 73°C for six minutes and hybridized for 48 hours at 37°C with the CCND1(BCL1)/IGH dual-color, dual-fusion probe (Abbot Molecular). Slides were washed with 2xSSC/0.3% NP-40 at 73°C for two minutes, counterstained with DAPI and analyzed with an Olympus BX51 microscope equipped with an 100x oil immersion objective, appropriate fluorescent filters and CytoVision® imaging software (Applied Imaging, San Jose, CA).
Two hundred interphase nuclei were analyzed for each specimen. Nuclei demonstrating single CCND1 (red) and IGH (green) signals and two CCND1/IGH fusion signals (yellow) were scored as positive for CCND1/IGH gene rearrangement. Nuclei with two CCND1, two IGH signals and no fusion signals were scored as negative. Specimens with greater than 30% of nuclei demonstrating CCND1/IGH fusion signal patterns were considered positive for CCND1/IGH gene rearrangement.
TMA data analysis and visualization
The stained lymphoma TMA slides were scanned and stored as high resolution images using an automated scanner (Bacus Laboratories, Inc., Slide Scanner (BLISS) http://www.bacuslabs.com). The “Deconvoluter” algorithm (custom WBS macro, Excel, Microsoft) with appropriate layout for use in the Cluster software was used for hierarchical clustering to integrate all immunohistologic staining results as previously described (http://genome-www.stanford.edu/TMA/).17 A total of 2784 TMA images generated from cyclin D2 and cyclin D3 staining are displayed on the following freely accessible website: http://tma.stanford.edu/tma_portal/cyclins.
RESULTS
Immunohistochemistry for cyclin D1 on normal hematopoietic and non-hematopoietic tissues was not carried out as part of the current study as this marker has been in routine use for a number of years and its tissue distribution pattern is well documented. For purposes of comparison, cyclin D1 expression was studied only in hematopoietic tumors (Table 1), and detailed characterization of the cyclin D2 and D3 proteins is presented. All three D-cyclins were expressed in endothelial cells, which allowed for excellent internal positive controls for comparisons among the three stains in paraffin tissue biopsies and tissue microarray cores.
Table 1.
Summary of Immunohistochemistry for D-Cyclin Expression
| Lymphoma subtype | Cyclin D1 | Cyclin D2 | Cyclin D3 |
|---|---|---|---|
| Diffuse large B-cell lymphoma, NOS | 4/204 (2) | 95/194 (49) | 44/220 (20) |
| Follicular lymphoma, grades 1 and 2 | 0/87 (0) | 24/79 (30) | 6/93 (6) |
| Follicular lymphoma, grade 3 | 0/69 (0) | 21/61 (34) | 10/71 (14) |
| Extranodal Marginal zone lymphoma | 0/21 (0) | 4/17 (24) | 0/24(0) |
| Nodal Marginal zone lymphoma | 0/5 (0) | 1/4 (25) | 1/5 (20) |
| Splenic Marginal zone lymphoma | 0/5 (0) | 0/4 (0) | 0/5 (0) |
| Mantle cell lymphoma | 18/18 (100) | 3/18 (22) | 1/18 (6) |
| Mantle cell lymphoma, blastoid variant | 5/5 (100) | 1/5 (20) | 0/5 (0) |
| Chronic lymphocytic leukemia/SLL | 0/36 (0) | 11/36 (31) | 2/38 (5) |
| Lymphoplasmacytic lymphoma | 0/5 (0) | 3/5 (60) | 0/5 (0) |
| Plasma cell myeloma | 0/2 (0) | 0/2 (0) | 1/2 (50) |
| Burkitt lymphoma | 0/3 (0)* | 1/2 (50) | 1/3 (33) |
| B lymphoblastic lymphoma/leukemia | 0/7 (0) | 4/7 (57) | 3/14 (21) |
| T lymphoblastic lymphoma | 0/12 (0) | 10/11 (91) | 3/12 (25) |
| Peripheral T-cell lymphoma, NOS | 0/18 (0)* | 10/18 (56) | 1/20 (5) |
| Adult T-cell lymphoma | 0/1 (0) | 0/1 (0) | 0/1 (0) |
| Angioimmunoblastic T-cell lymphoma | 0/3 (0) | 1/3 (33) | 0/3 (0) |
| Anaplastic large cell lymphoma, ALK+ | 0/7 (0) | 3/5 (60) | 2/8 (25) |
| Extranodal NK/T cell lymphoma, nasal type | ND | ND | 3/63 (5) |
| Classical Hodgkin lymphoma | ND | 76/101 (75) | 21/125 (17) |
| Acute myeloid leukemia | ND | 6/6 (100) | 6/6 (100) |
The proportion of cases of each diagnostic category that stained positive is shown in parentheses.
indicates that occasional cells (<20% of lymphoma cells) showed staining in one Burkitt and two peripheral T cell lymphoma, NOS.
Cyclin D2 protein shows widespread expression among normal tissues and in hematopoietic and non-hematopoietic neoplasms
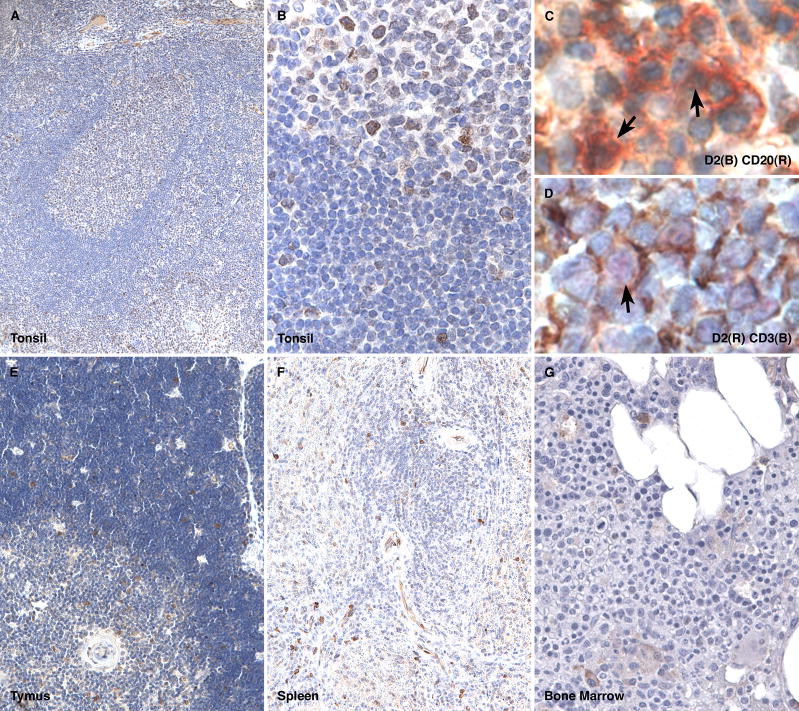
Cyclin D2 staining in normal tonsil and lymph node tissue showed a range of staining from weak to strong in a subset of cells within germinal centers, mantle and marginal zones and in the paracortex (Figure 1A and B). Plasma cells typically showed cytoplasmic localization of the stain with only weak nuclear staining. In tonsils, a subset of intraepithelial lymphocytes also showed staining. Double immunohistochemical labeling of tonsil sections with CD20 and CD3 showed that a proportion of both B- and T-cells stain for this marker (Figure 1C and D). In normal thymi, there was staining in scattered cortical and medullary cells (Figure 1E). Double immunohistochemical labeling of thymic sections showed a similar staining pattern to that seen in tonsils with co-localization of the stain in a proportion of CD20-positive B-cells and CD3-positive T-cells. In normal spleen, staining for cyclin D2 was confined to scattered lymphoid cells and plasma cells but was absent from splenic marginal zone cells within the white pulp (Figure 1F). In addition, staining was prominent in endothelial cells (splenic littoral cells). Sections of normal bone marrow showed cyclin D2 staining in scattered lymphoid cells; however, the majority of myeloid and erythroid precursors and megakaryocytes lacked staining, except for weak staining in occasional myeloid precursors (Figure 1G). Double-labeling of cyclin D2 with myeloperoxidase (specific for myeloid and monocytic lineages), glycophorin (specific for erythroid lineage) and CD34 (immature blasts) did not show significant co-expression (data not shown).
Figure 1. Cyclin D2 expression in normal hematopoietic tissue.
Cyclin D2 staining is found in a subset of cells in the germinal center, mantle and marginal zones and in the paracortex of a normal tonsil (A and B); double immunohistochemical labeling for cyclin D2 (brown) and CD20 (red) show co-localization of staining in a subset of B-cell (arrows, C); double immunohistochemical labeling for cyclin D2 (red) and CD3 (brown) show co-localization of staining in a subset of T-cell (arrow, D); scattered cells in the cortex and medulla of the normal thymus show cyclin D2-positive cells (E); the normal spleen shows staining in scattered lymphoid cells in the red and white pulp and in endothelial cells but is lacking in splenic marginal zones (F); the normal bone marrow shows staining in scattered lymphoid and plasma cells but is not found in a significant proportion of erythroid or myeloid precursors or megakaryocytes (G).
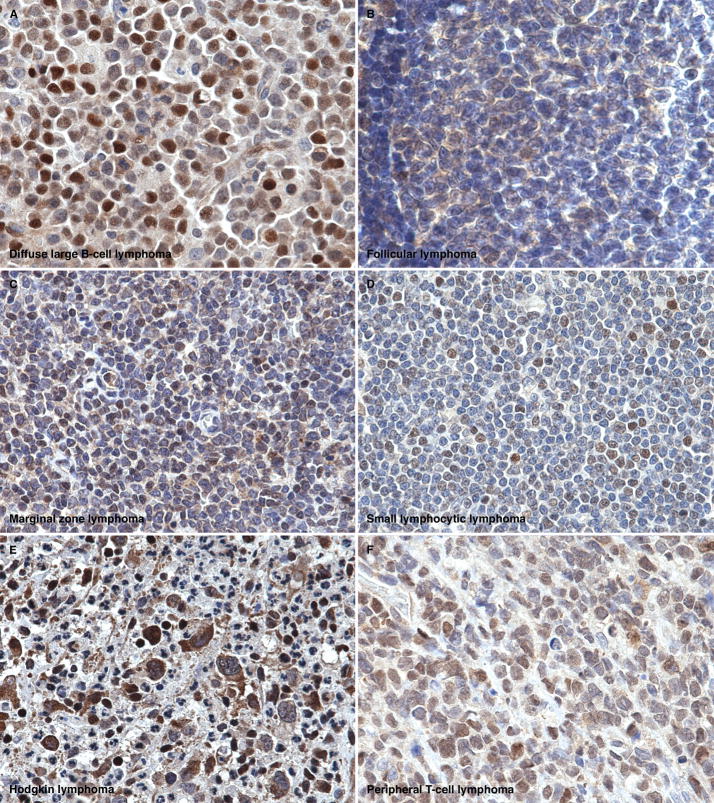
Among hematopoietic neoplasms, staining for cyclin D2 was present in nearly half of diffuse large B-cell lymphoma (95/194, 49%) (Figure 2A), along with a significant proportion of all histologic grades of follicular lymphoma (45/140, 32%) (Figure 2B), marginal zone lymphoma (5/25, 25%) (Figure 2C), mantle cell lymphoma (typical 3/18, 17% and blastoid variant 1/5, 20%), lymphoplasmacytic lymphoma (3/5, 60%), chronic lymphocytic leukemia/small lymphocytic lymphoma (11/36, 31%) (Figure 2D), B lymphoblastic lymphoma (4/7, 57%), T lymphoblastic lymphoma (10/11, 91%), peripheral T-cell lymphoma (10/18, 56%) (Figure 2F), anaplastic large cell lymphoma (3/5, 60%) and classical Hodgkin lymphoma (76/101, 75%) (Figure 2E). All six cases of acute myeloid leukemia showed cyclin D2 staining in the blast population. These cases included two acute myeloid leukemia, not otherwise specified, two acute myeloid leukemia with associated multilineage dysplasia, one acute myeloid leukemia with a 11q23 deletion and one acute myeloid leukemia arising as a result of blast transformation from t(9;22)-positive chronic myeloid leukemia (Table 1).
Figure 2. Cyclin D2 expression in hematopoietic neoplasia.
Cyclin D2 staining is shown in examples of diffuse large B-cell lymphoma (A), follicular lymphoma (B), marginal zone lymphoma (C), small lymphocytic lymphoma (D), classical Hodgkin lymphoma (E), and peripheral T-cell lymphoma (F). In all cases, the staining is primarily localized to the nucleus, although associated cytoplasmic staining is also seen in some instances.
Seventy-three samples of non-hematolymphoid tissues from various adult organs and corresponding neoplasms were stained for cyclin D2. The majority of the cases (53/73, 73%) showed nuclear staining or a combination of nuclear and cytoplasmic staining for cyclin D2 (Table 2). Only staining in the relevant lesional cells or tissue compartment was scored positive; in the case of malignancies, the neoplastic infiltrate was evaluated. Cyclin D2 staining was present in endothelial cells in most of the tissue cores and full sections examined.
Table 2.
Summary of Immunohistochemistry for Cyclins D2 and D3 Expression in Non-hematopoietic Tissue and Tumor Types
| Tissue/Tumor | Cyclin D2 | Cyclin D3 |
|---|---|---|
| Adrenal, normal | 1/1 | 0/1 |
| Adrenocortical carcinoma | 0/1 | 0/1 |
| Bladder mucosa, normal | 1/1 | 0/1 |
| Bladder, urothelial carcinoma | 1/2 | 0/1 |
| Brain, normal | 1/1 | 0/1 |
| Brain, GBM | 2/2 | 0/2 |
| Breast, normal | 0/1 | 0/1 |
| Breast carcinoma | 4/13 | 2/13 |
| Colon, normal | 2/2 | 0/1 |
| Colon, adenocarcinoma | 2/2 | 0/3 |
| ENT, squamous cell carcinoma | 1/1 | 1/1 |
| Heart, normal | 1/1 | 0/1 |
| Kidney, normal | 2/2 | 1/1 |
| Kidney, renal cell carcinoma | 2/2 | 0/2 |
| Liver, normal | 1/1 | 1/1 |
| Liver, hepatocellular carcinoma | 2/2 | 0/2 |
| Lung, normal | 1/2 | 0/1 |
| Lung, carcinoma | 2/2 | 2/2 |
| Ovary, normal | 1/1 | 0/1 |
| Ovary, carcinoma | 0/2 | 0/3 |
| Pancreas, normal | 1/1 | 0/1 |
| Pancreas, adenocarcinoma | 0/2 | 0/1 |
| Parathyroid, normal | 3/3 | 0/3 |
| Prostate, normal | 1/1 | 0/1 |
| Prostate, carcinoma | 3/3 | 0/3 |
| Salivary gland, normal | 1/1 | 0/1 |
| Skin, melanoma | 1/1 | 1/1 |
| Soft tissue fibromatosis | 1/1 | 0/1 |
| Soft tissue sarcomas | 6/6 | 2/6 |
| Stomach, normal | 1/1 | 0/1 |
| Stomach, adenocarcinoma | 1/1 | 0/1 |
| Testis, normal | 1/1 | 0/1 |
| Testis, seminoma | 1/1 | 0/1 |
| Thyroid, normal | 1/1 | 0/1 |
| Thyroid, carcinoma | 2/3 | 0/3 |
| Uterus, normal | 2/2 | 0/2 |
| Uterus, endometrial carcinoma | 0/2 | 0/2 |
| TOTAL | 53/73 (73%) | 10/70 (14%) |
Cyclin D3 protein shows a restricted pattern of expression among normal tissues and in hematopoietic and non-hematopoietic neoplasms
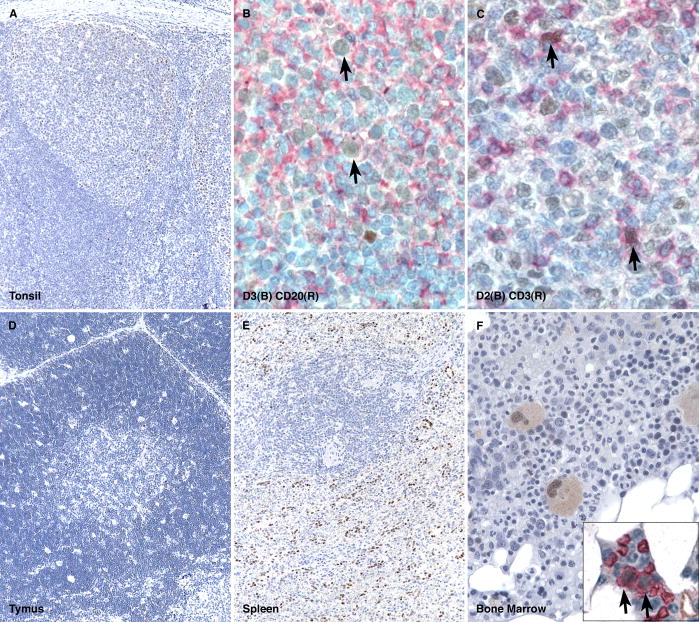
Cyclin D3 staining in normal tonsil and lymph node tissue showed intense and crisply localized nuclear staining in a subset of lymphoid cells within germinal centers and in the paracortex; only rare cells were appreciated within the mantle and marginal zones (Figure 3A). The overall distribution of the stained cells was similar to that of cyclin D2 staining but fewer cells stained for cyclin D3 than for the cyclin D2 protein within each compartment. Occasional plasma cells showed a combination of nuclear (weak) and cytoplasmic (strong) staining. In tonsils, a few intraepithelial lymphocytes also showed staining. Double immunohistochemical labeling of tonsil sections with CD20 and CD3 showed that the vast majority of B- and T-cells lacked cyclin D3-staining; however, cyclin D3 staining was seen in occasional B- and T-cells (Figure 3B and C). In normal thymi, there was staining in scattered cortical and medullary cells in a pattern similar to cyclin D2 staining (Figure 3D). Double-immunohistochemical labeling of thymic sections again showed co-localization of cyclin D3 staining in subsets of CD20-positive B-cells and CD3-positive T-cells. In the normal spleen, staining for cyclin D3 was confined to scattered lymphoid cells and plasma cells in the red pulp and endothelial cells; lymphoid cells of the splenic marginal zone lacked staining (Figure 3E). Sections of normal bone marrow showed prominent cyclin D3 staining in megakaryocytes (nuclear and cytoplasmic) and in a subset of erythroid precursors, which was confirmed by double immunohistochemical labeling for glycophorin (Figure 3F and inset). Myeloid precursors and blasts lacked staining for cyclin D3, which was confirmed by double labeling for myeloperoxidase and CD34 (data not shown).
Figure 3. Cyclin D3 expression in normal hematopoietic tissue.
Cyclin D3 staining is found in a subset of cells in the germinal center, and rarely in the mantle and marginal zones and paracortex of a normal tonsil (A); double immunohistochemical labeling for cyclin D3 (brown) and CD20 (red) show co-localization of staining in occasional B-cell (arrows, B); double immunohistochemical labeling for cyclin D3 (red) and CD3 (brown) show co-localization of staining in a subset of T-cell (arrow, C); scattered cells in the cortex and medulla of the normal thymus shows cyclin D3-positive cells (E); the normal spleen shows staining in scattered lymphoid cells in the red and white pulp and in endothelial cells but is lacking in splenic marginal zones (F); the normal bone marrow shows staining in scattered lymphoid and plasma cells, megakaryocytes and in a subset of erythroid precursors (G). Double immunohistochemical labeling of erythroid precursors with glycophorin (red) and cyclin D3 (brown) shows co-localization of the staining in erythroid cells (inset and arrows).
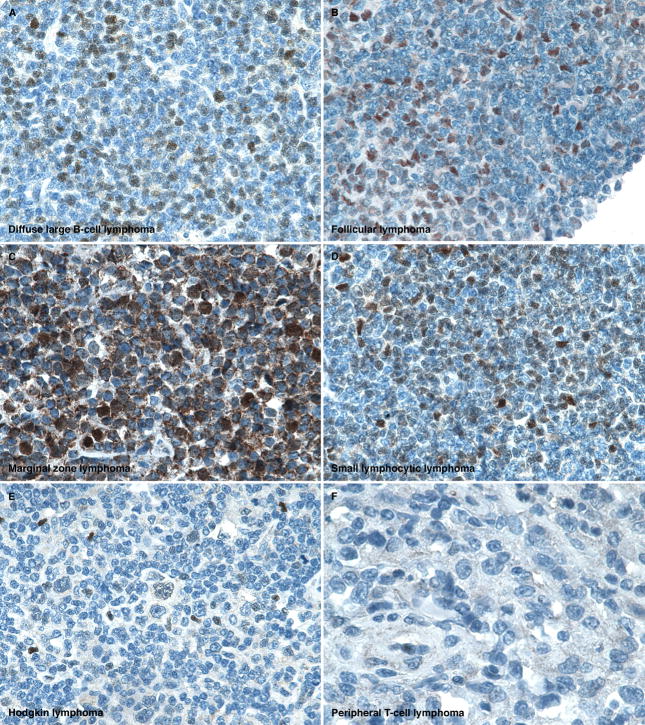
Cyclin D3 immunostaining highlighted a minority of cases of nearly all subtypes of hematopoietic tumors (Table 1). In contrast to cyclin D2, cyclin D3 staining was found in a smaller proportion of diffuse large B-cell lymphoma (44/220, 20%) (Figure 4A). Cyclin D3 staining was seen in a small number of all grades of follicular lymphoma (Figure 4B), although the proportion of cases that stained positive increased with the grade of the tumor: grade 1 (1/37, 3%), grade 2 (5/55, 9%), and grade 3 (10/72, 14%). A small minority of marginal zone lymphoma (2/35, 6%) (Figure 4C), mantle cell lymphoma (typical 1/18, 6% and blastoid variant 0/5, 0%), chronic lymphocytic leukemia/small lymphocytic lymphoma (2/38, 5%) (Figure 4D), peripheral T-cell lymphoma (1/20, 5%) (Figure 4F), and extranodal NK/T cell lymphomas, nasal type (4/83, 5%) were positive. Additionally, a slightly higher proportion of classical Hodgkin lymphoma (21/125, 17%) (Figure 4E), B lymphoblastic lymphoma (3/14, 21%), T lymphoblastic lymphoma (3/12, 25%) and anaplastic large cell lymphoma (2/8, 25%) expressed cyclin D3. All 6 cases of acute myeloid leukemia showed cyclin D3 staining in a small subset of blasts although four of the six cases showed expression in only rare clusters of cells. The one case of megakaryoblastic leukemia (acute myeloid leukemia, not otherwise specified or French-American-British classification, subtype M7) showed staining in the atypical megakaryoblasts.
Figure 4. Cyclin D3 expression in hematopoietic neoplasia.
Cyclin D3 staining is shown in examples of diffuse large B-cell lymphoma (A), follicular lymphoma (B), marginal zone lymphoma (C), small lymphocytic lymphoma (D), classical Hodgkin lymphoma (E), and peripheral T-cell lymphoma (F). In all cases, except in the peripheral T-cell lymphoma, the staining is primarily localized to the nucleus, although associated cytoplasmic staining is also seen in some instances. The case of peripheral T-cell lymphoma lacked staining for cyclin D3.
Seventy samples of non-hematolymphoid tissues from various adult organs and corresponding tumors were stained for cyclin D3. In contrast to cyclin D2, only a small minority of cases (10/70, 14%) expressed cyclin D3 and included a ductal carcinoma of the breast, a lobular carcinoma of the breast, a squamous cell carcinoma of the head and neck, a lung squamous cell carcinoma, a lung adenocarcinoma, a melanoma, a gastrointestinal stromal tumor and a malignant fibrous histiocytoma (Table 2). Of the normal tissues, liver and kidney showed staining for cyclin D3. As described for cyclin D2, staining in the relevant lesional cells or tissue compartment was scored positive; in the case of malignancies, the neoplastic infiltrate was evaluated.
Cyclin D1 (BCL1) protein expression is limited to mantle cell lymphoma and rare diffuse large B-cell lymphoma
To facilitate comparison between cyclin D1, D2 and D3 staining across lymphoma subtypes, immunohistochemistry for cyclin D1 was carried out in the same set of hematopoietic tumors as used for the study of cyclin D2 and D3 (Table 1). All eighteen cases of typical mantle cell lymphoma and five cases of blastoid mantle cell lymphoma showed nuclear staining for cyclin D1. One mantle cell lymphoma showed relatively weak staining in comparison to the others; however, the majority of the nuclei in the lymphoma cells showed the presence of cyclin D1. Four cases of diffuse large B-cell lymphoma (of 204 studied) showed nuclear staining for cyclin D1 in the majority of tumor cells. In addition, one case of Burkitt lymphoma (1/3) and two cases of peripheral T-cell lymphoma (2/18) showed occasional lymphoma cells with nuclear staining. These latter cases did not meet the threshold defined for a positive score in this study. All remaining lymphoma subtypes lacked staining for cyclin D1 (Table 1).
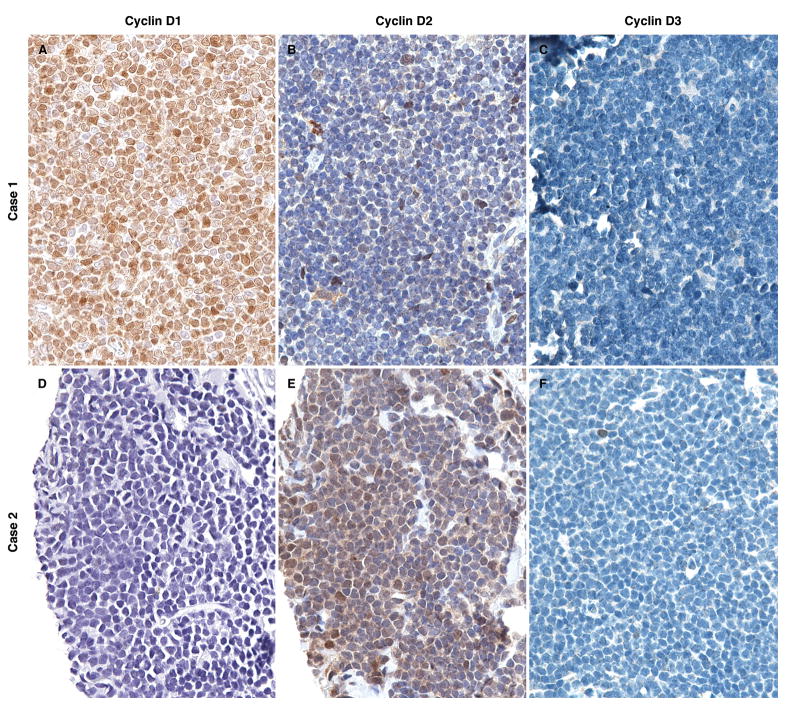
Among the 18 typical mantle cell lymphoma cases, 17 expressed strong staining for cyclin D1 (representative case illustrated in Figures 5A – C), three cases expressed cyclin D2 and a single case expressed cyclin D3. The case that was weakly positive for cyclin D1 showed strong staining for cyclin D2 (Figures 5D – F). Two of the three cases that stained for cyclin D2, and the case that stained for cyclin D3, also harbored the CCND1/IGH translocation by FISH analysis. All five cases of blastoid mantle cell lymphoma showed strong staining for cyclin D1, in addition to which one case showed weak expression of cyclin D2. None of the cases showed staining for all three D-cyclins.
Figure 5. The expression of D-cyclins in mantle cell lymphoma.
The differential expression of D-cyclin staining in two case examples of mantle cell lymphoma is shown. Case 1 shows intense cyclin D1 and weak cyclin D2 staining. Case 2 shows weak cyclin D1 and strong cyclin D2 staining. Both cases lack staining for cyclin D3.
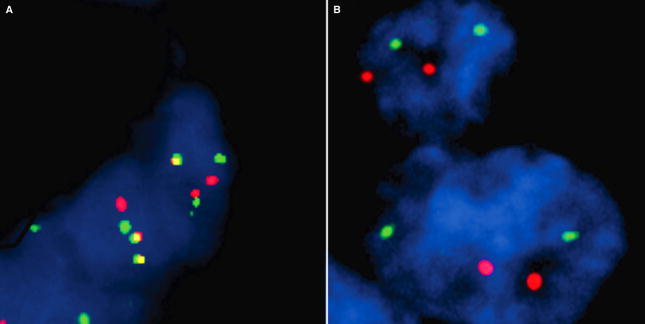
We performed FISH analysis on TMAs and whole sections for the CCND1/IGH translocation to assess whether the cases positive for cyclin D1 by immunohistochemistry also harbored the translocation. Sixteen of eighteen cases of mantle cell lymphoma showed the presence of the CCND1/IGH translocation (Figure 6A). However, the translocation was lacking in the two cyclin D1-positive diffuse large B-cell lymphoma cases that were tested (Figure 6B). Material was not available for the other two diffuse large B-cell lymphoma cases. FISH analysis did not demonstrate the CCND1/IGH translocation in the Burkitt and peripheral T-cell lymphoma cases that showed cyclin D1 staining in scattered cells. The translocation was also absent in all other hematopoietic tumor types analyzed on our TMA (a total of 477 lymphomas).
Figure 6. FlSH for CCND1/IGH in mantle cell and diffuse large B-cell lymphoma.
An example of mantle cell lymphoma shows the dual fusion signal associated with the CCND1/IGH translocation in numerous lymphoma cells (A); an example of cyclin D1-positive diffuse large B-cell lymphoma shows no dual fusion signals within lymphoma cells indicating the lack of the CCND1/IGH translocation (B).
Protein Expression Profiles of Cyclin D2 and D3 in diffuse large B-cell lymphoma
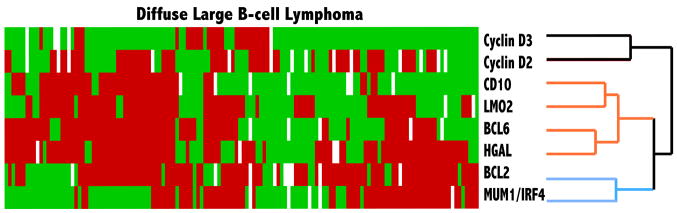
In prior studies, CCND2 mRNA and the cyclin D2 protein have been found to correlate with an inferior outcome in patients with diffuse large B-cell lymphoma.11–13 The significance of cyclin D3 expression in diffuse large B-cell lymphoma has not been previously explored. Therefore, we compared the relationship of cyclin D2 and D3 protein expression in 143 cases of diffuse large B-cell lymphoma on which we had previously analyzed the expression of CD10, BCL6, HGAL, LMO2, BCL2 and MUM1/IRF4.15,18 Hierarchical cluster analysis of immunohistologic data showed that the expression patterns of cyclins D2 and D3 were closely related to each other and clustered on one branch of the dendrogram but was distinct from both the germinal center and non-germinal center markers (Figure 7).
Figure 7. Hierarchical cluster analysis of immunohistologic data in diffuse large B-cell lymphoma.
Hierarchical cluster analysis shows that the expression profiles of cyclin D2 and D3 proteins are similar to each other across the 143 cases of diffuse large B-cell lymphoma, but are distinct from that of germinal center-associated markers CD10, BCL6, HGAL and LMO2, and from non-germinal center markers, BCL2 and MUM1/IRF4.
The expression of D-cyclins is variably associated with the degree of proliferation in lymphoma subtypes
To address whether the expression of D-cyclins was associated with the degree of proliferation in lymphoma subtypes, we performed Ki-67 staining on the lymphoma tissue microarrays. On 61 diffuse large B-cell lymphoma cases data for all four markers (cyclins D1, D2, D3 and Ki-67) was available; we found no specific correlation among D-cyclin expression and proliferation as measured by Ki-67 (Table 3). In addition, in 24 cases of diffuse large B-cell lymphoma that did not express any of the three D-cyclins, the proliferation index ranged from 10 to 70%. In low-grade lymphomas, no correlation was seen between the expression of D-cyclins, particularly cyclins D2 and D3, and the degree of proliferation. For example, grade 1 follicular lymphomas with increased proliferation (three cases with 30% and one case with 80% Ki-67 positivity) did not express cyclins D2 or D3. In high grade lymphomas including lymphoblastic lymphoma and subtypes of T-cell lymphoma with >50% proliferation rate as measured by Ki-67, the proliferation index was highly correlated with the expression of cyclins D2 and D3: In B- and T-lymphoblastic lymphomas 10/11 (90%) cases expressed high levels of cyclin D2 and three cases expressed high levels of cyclin D3; the single case that expressed moderate amounts of cyclin D2 showed high levels of cyclin D3 expression. Similarly, the degree of proliferation in T-cell lymphoma subtypes were closely associated with increased levels of cyclin D2 expression: peripheral T-cell lymphoma 7/10 (70%), anaplastic large cell lymphoma 2/2 (100%) and extranodal NK/T-cell lymphoma, nasal type 2/2 (100%). Six of the T-cell lymphomas also showed moderate expression of cyclin D3.
Table 3.
Proliferation Index (Ki-67) and Expression of D-Cyclins in Diffuse Large B-Cell Lymphomas
| Proliferation Index (Ki-67 Staining) | Cyclin D1 | Cyclin D2 | Cyclin D3 |
|---|---|---|---|
| Low (<30%) | 0/9 (0%) | 6/9 (66.6%) | 0/9 (0%) |
| Intermediate (30 – <50%) | 1/28 (3.5%) | 16/28 (57.1%) | 2/28 (7.1%) |
| High (>50%) | 0/24 (0%) | 15/24 (62.5%) | 4/24 (16.6%) |
DISCUSSION
D-cyclins are cell cycle regulatory proteins whose expression and distribution in human tissue types and neoplasms are incompletely characterized. In the current work, we show that among the three D-cyclin proteins, cyclin D1 has the most restricted pattern of expression, whereas cyclin D2 exhibits more widespread expression in a variety of hematopoietic and non-hematopoietic tissues. The expression pattern of cyclins D2 and D3 is in sharp contrast to the known tissue distribution of cyclin D1, which is not found in normal hematopoietic cells. Our findings are in keeping with studies in mouse splenic B-cells that showed cyclins D2 and D3 but not D1 as crucial for the proliferative capacity of mitogen-stimulation of B cells.19 In normal hematopoietic tissues, cyclins D2 and D3 were expressed in a proportion of B- and T- cell subsets as ascertained by double-labeling experiments. Although cyclin D3 was found in fewer lymphoid cells than cyclin D2, the pattern of expression in different lymphoid cell compartments in normal hematopoietic organs (tonsil, lymph node, thymus and spleen) was similar to each other. Most importantly, a significant proportion of germinal center B-cells lacked cyclin D2 and D3 staining. Although cyclin D2 is essential for B-cell receptor-mediated signaling and proliferation of naive B-cells20,21, its low abundance in germinal center B-cells is supported by prior gene expression profiling studies.22 The mechanism of how some germinal center B-cells proliferate in the absence of these key cell cycle regulators of the G1/S transition that controls cell proliferation, is as yet unknown.
The expression of cyclin D2 and D3 proteins in normal hematopoietic tissues was mirrored by their expression across the hematopoietic neoplasms studied, with some exceptions. Cyclin D2 was the most widely expressed D-cyclin and was found in almost all subtypes of lymphomas including a subset of classical Hodgkin lymphoma. Although normal myeloid precursors and blasts in the bone marrow did not show significant amount of staining for cyclin D2, all acute myeloid leukemias and subsets of B- and T- lymphoblastic lymphoma/leukemias showed staining for cyclin D2 in a subset of blasts. Cyclin D3 staining was detected in erythroid precursors and in megakaryocytes in the normal bone marrow, and its overexpression was also detected in a subset of the blasts in all acute myeloid leukemias and in B- and T- lymphoblastic lymphoma/leukemias. Given that cyclin D2 and D3 expression is minimal or absent in normal marrow precursors, these findings raise the possibility that their expression may be activated during leukemogenesis and are overexpressed in acute leukemias. Since a significant proportion of acute leukemias showed overexpression of both cyclins D2 and D3, these results suggest the possibility of coordinate regulation of cyclin D2 and D3 in these leukemias.
Translocation t(11;14) (q13;q32) at the cyclin D1 locus results in the overexpression of the cyclin D1 protein which accelerates lymphoma cells through the G1/S transition of the cell cycle leading to dysregulated proliferation.5,6 In cyclin D1-negative mantle cell lymphomas, there is overexpression of cyclin D2 or D3 proteins.7 Furthermore, knockdown of cyclin D1 mRNA in mantle cell lymphoma cell lines have shown a modest compensatory increase in the expression of cyclin D2 mRNA and protein, suggesting the possibility for coordinate regulation of the expression of D-cyclins.23 This finding is in keeping with gene targeting experiments in mice deficient in D-cyclins that suggested the presence of functional redundancy among mammalian D-cyclins.24 Several recent reports have described translocations targeting the CCND2 or CCND3 loci in cyclin D1-negative mantle cell lymphomas: t(12;14)(p13;q32)/IGH-CCND2, t(2;12)(p11;p13)/IGK-CCND2 and t(6;14)(p21;q32)/IGH-CCND3.8–10 We performed FISH analysis to further interrogate our cohort of mantle cell lymphoma cases: 16 of 18 cases harbored the CCND1/IGH translocation and all expressed the cyclin D1 protein. The single case in our series that showed weak cyclin D1 but strong cyclin D2 staining was found to harbor the CCND1/IGH translocation. Therefore, we did not pursue additional cytogenetic analyses as our cases would be unlikely to yield a known or novel translocation involving CCND2 or CCND3. However, it would be of interest to characterize the cytogenetic abnormalities of additional cyclin D1-negative mantle cell lymphomas to better understand the spectrum of chromosomal defects acquired by this rare type of lymphoma.
Apart from mantle cell lymphoma, cyclin D1 expression was detected in a four cases (2%) of diffuse large B-cell lymphoma. These cases showed intense nuclear staining in the vast majority of lymphoma cells. In two cases where material was available for cytogenetic/FISH studies, neither the CCND1/IGH translocation nor abnormalities associated with the CCND1 locus was detected. Complete karyotypic analysis was not performed due to the lack of fresh tissue. Rare cases of cyclin D1-positive diffuse large B-cell lymphoma have been previously reported.25,26 In a series of 231 cases of diffuse large B-cell lymphoma, Ehinger and colleagues described 10 cases (4%) that showed staining for cyclin D1; the majority of these cases showed aberrancies involving the CCND1 locus and one case showed the CCND1/IGH translocation.25 In a single case reported by Rodrigues-Justo and colleagues, aberrancies involving the CCND1 locus but not the translocation were detected.26 Our findings are in keeping with these prior observations that cyclin D1 is expressed in rare cases of diffuse large B-cell lymphoma. These findings underscore the importance of using an integrated approach to diagnosis that involves morphologic assessment, clinical input and a panel of immunostains (including BCL2, BCL6, IgM, and IgD in addition to cyclin D1) to distinguish among large cell or blastoid variants of mantle cell and diffuse large B-cell or other high grade B-cell lymphomas.
Our results in a variety of lymphoma subtypes show that immunostaining for cyclin D2 and D3 lacks specificity with regard to a particular subtype of lymphoma; staining for cyclin D2 and D3 was found in a subset of almost all types of B- and T- cell lymphomas including lymphoblastic and classical Hodgkin lymphomas. As important cell cycle regulatory molecules, the overexpression of cyclin D2 and D3 proteins in lymphomas and leukemias with a propensity for increased proliferation is not unexpected. This is reflected in our data on lymphoblastic lymphoma and T and NK-cell lymphoma subtypes where all cases that showed a high degree of proliferation (>50% by Ki-67 staining) also showed high levels of expression of cyclin D2 and/or D3. Of particular interest is that a significant proportion of low grade B-cell lymphomas also express cyclins D2 and D3. In these cases, the expression of D-cyclins did not correlate with increased proliferation. This finding is particularly relevant to grade 1 follicular lymphomas with increased proliferation, a group of lymphomas reported to follow a more aggressive clinical course.27 The four cases in our cohort that belong to this category showed no expression of D-cyclin proteins. These findings may be suggestive of additional as yet unidentified cyclins that may be involved in the regulation of proliferation in lymphoma subtypes or other mechanisms of cell cycle regulation at play. Therefore, it should be emphasized that the presence of cyclin D2 or D3 staining in a low grade B cell lymphoma should not be interpreted as compatible with a diagnosis of cyclin D1-negative mantle cell lymphoma. This latter entity is a rare diagnosis and as such, morphologic features, other immunohistologic markers (CD5, IgM, IgD), and FISH studies for abnormalities involving the CCND1 locus should be correlated before the diagnosis of this rare entity is rendered. In addition, since cyclin D2 and D3 proteins are expressed in lymphoid and myeloid leukemias, caution should be exercised in utilizing these stains for bone marrow diagnosis. Potential pitfalls include cases in which the marrow is replaced by a diffuse proliferation of intermediate cell size where a concurrent aspirate smear is not available for sufficient morphologic assessment; this proliferation could potentially lead to confusion of a lymphoblastic or myeloid leukemia with mantle cell lymphoma. Therefore, given the expression of cyclins D2 and D3 in a variety of lymphoid subtypes, it is necessary for careful assessment of these markers in the context of other findings.
The overexpression of cyclin D2 and D3 proteins in a variety of subsets of lymphomas raises the possibility that dysregulation of specific biological pathways associated with the cell cycle may play a role in their pathogenesis and prognosis. For example, we found that among ALK-positive anaplastic large cell lymphomas, 60% overexpressed cyclin D2 and 25% overexpressed cyclin D3. This result corresponds with previous gene expression profiling studies that identified the expression of cyclin D3 in ALK-positive but not in ALK-negative ALCL.28 These findings further suggest that ALK-positive anaplastic large cell lymphoma may exploit a different mechanism of promoting G1/S transition than its ALK-negative counterpart. Given the significant difference in clinical outcome between these entities, the overexpression of cyclin D3 may prove to be a marker of superior outcome in this disease. However, further work on sufficiently well-characterized ALK-positive and ALK-negative anaplastic large cell lymphoma cases is needed to formally prove this hypothesis.
We previously identified CCND2 as the best predictor of inferior survival in diffuse large B-cell lymphoma patients in a multivariate model based on the expression of six-genes as measured by quantitative RT-PCR.11,12 Immunohistochemical staining for cyclin D2 was also found to be associated with an inferior outcome in patients with diffuse large B-cell lymphoma treated with anthracycline-containing chemotherapy.13 In a set of 143 cases of diffuse large B-cell lymphoma that we have previously evaluated for markers of germinal center and non-germinal center derivation,15,16,18,29 hierarchical cluster analysis showed that cyclins D2 and D3 staining exhibit protein expression profiles that are similar to each other across the diffuse large B-cell lymphoma cases. This pattern of expression of cyclins D2 and D3 in diffuse large B-cell lymphoma suggests that the relationship of these proteins to prognostic stratification may be associated with cell cycle control rather than the cell of origin. However, in our cohort of diffuse large B-cell lymphoma cases the degree of proliferation as measured by Ki-67 staining and the expression of D-cyclins did not yield a significant correlation. In addition, cases that did not express any of the three D-cyclins showed a range of proliferation from 10 to 70%. Therefore, the proliferative capacity of diffuse large B-cell lymphomas is likely governed by complex and as yet unknown mechanisms that may not be restricted to cell cycle control. Of note, prior gene expression profiling studies showed low abundance of cyclin D2 in germinal center B-cells,22 although our data shows variable expression of cyclin D2 protein in germinal center B-cells. Our findings also differ from a previous report that found that cyclin D3 but not cyclin D2 was expressed in germinal center B-cells.30 Whether the differential expression of cyclins D2 and D3 proteins is associated with patient outcome warrants further investigation in a cohort of diffuse large B-cell lymphoma patients uniformly treated with Rituximab-based immunochemotherapy as these regimens have been shown to be of improved benefit in patients with diffuse large B-cell lymphoma.31–34
Acknowledgments
NIH CA34233, NIH CA109335 and the Dwoskin Family Foundation
We would like to thank Edward Gilbert for technical assistance with immunohistochemistry and Thelma Santa Maria for administrative support.
Footnotes
DISCLOSURES
The authors report no conflicts of interest associated with this work.
References
- 1.Malumbres M, Barbacid M. Cell cycle, CDKs and cancer: a changing paradigm. Nat Rev Cancer. 2009;9:153–166. doi: 10.1038/nrc2602. [DOI] [PubMed] [Google Scholar]
- 2.Malumbres M, Sotillo R, Santamaria D, et al. Mammalian cells cycle without the D-type cyclin-dependent kinases Cdk4 and Cdk6. Cell. 2004;118:493–504. doi: 10.1016/j.cell.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Sherr CJ. G1 phase progression: cycling on cue. Cell. 1994;79:551–555. doi: 10.1016/0092-8674(94)90540-1. [DOI] [PubMed] [Google Scholar]
- 4.Suzuki R, Kuroda H, Komatsu H, et al. Selective usage of D-type cyclins in lymphoid malignancies. Leukemia. 1999;13:1335–1342. doi: 10.1038/sj.leu.2401485. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg CL, Wong E, Petty EM, et al. PRAD1, a candidate BCL1 oncogene: mapping and expression in centrocytic lymphoma. Proc Natl Acad Sci U S A. 1991;88:9638–9642. doi: 10.1073/pnas.88.21.9638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swerdlow SH, Campo E, Harris NL, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon: IARC; 2008. [Google Scholar]
- 7.Fu K, Weisenburger DD, Greiner TC, et al. Cyclin D1-negative mantle cell lymphoma: a clinicopathologic study based on gene expression profiling. Blood. 2005;106:4315–4321. doi: 10.1182/blood-2005-04-1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gesk S, Klapper W, Martin-Subero JI, et al. A chromosomal translocation in cyclin D1-negative/cyclin D2-positive mantle cell lymphoma fuses the CCND2 gene to the IGK locus. Blood. 2006;108:1109–1110. doi: 10.1182/blood-2006-01-0015. [DOI] [PubMed] [Google Scholar]
- 9.Herens C, Lambert F, Quintanilla-Martinez L, Bisig B, Deusings C, de Leval L. Cyclin D1-negative mantle cell lymphoma with cryptic t(12;14)(p13;q32) and cyclin D2 overexpression. Blood. 2008;111:1745–1746. doi: 10.1182/blood-2007-10-120824. [DOI] [PubMed] [Google Scholar]
- 10.Wlodarska I, Dierickx D, Vanhentenrijk V, et al. Translocations targeting CCND2, CCND3, and MYCN do occur in t(11;14)-negative mantle cell lymphomas. Blood. 2008;111:5683–5690. doi: 10.1182/blood-2007-10-118794. [DOI] [PubMed] [Google Scholar]
- 11.Lossos IS, Czerwinski DK, Alizadeh AA, et al. Prediction of survival in diffuse large-B-cell lymphoma based on the expression of six genes. N Engl J Med. 2004;350:1828–1837. doi: 10.1056/NEJMoa032520. [DOI] [PubMed] [Google Scholar]
- 12.Malumbres R, Chen J, Tibshirani R, et al. Paraffin-based 6-gene model predicts outcome in diffuse large B-cell lymphoma patients treated with R-CHOP. Blood. 2008;111:5509–5514. doi: 10.1182/blood-2008-02-136374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hans CP, Weisenburger DD, Greiner TC, et al. Expression of PKC-beta or cyclin D2 predicts for inferior survival in diffuse large B-cell lymphoma. Mod Pathol. 2005;18:1377–1384. doi: 10.1038/modpathol.3800434. [DOI] [PubMed] [Google Scholar]
- 14.Moller MB, Nielsen O, Pedersen NT. Cyclin D3 expression in non-Hodgkin lymphoma. Correlation with other cell cycle regulators and clinical features. Am J Clin Pathol. 2001;115:404–412. doi: 10.1309/8KF0-0Y0C-2F4L-UHXL. [DOI] [PubMed] [Google Scholar]
- 15.Natkunam Y, Lossos IS, Taidi B, et al. Expression of the human germinal center-associated lymphoma (HGAL) protein, a new marker of germinal center B-cell derivation. Blood. 2005;105:3979–3986. doi: 10.1182/blood-2004-08-3112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Natkunam Y, Warnke RA, Montgomery K, Falini B, van De Rijn M. Analysis of MUM1/IRF4 protein expression using tissue microarrays and immunohistochemistry. Mod Pathol. 2001;14:686–694. doi: 10.1038/modpathol.3880373. [DOI] [PubMed] [Google Scholar]
- 17.Marinelli RJ, Montgomery K, Liu CL, et al. The Stanford Tissue Microarray Database. Nucleic Acids Res. 2008;36:D871–877. doi: 10.1093/nar/gkm861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Natkunam Y, Zhao S, Mason DY, et al. The oncoprotein LMO2 is expressed in normal germinal-center B cells and in human B-cell lymphomas. Blood. 2007;109:1636–1642. doi: 10.1182/blood-2006-08-039024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Su TT, Rawlings DJ. Transitional B lymphocyte subsets operate as distinct checkpoints in murine splenic B cell development. J Immunol. 2002;168:2101–2110. doi: 10.4049/jimmunol.168.5.2101. [DOI] [PubMed] [Google Scholar]
- 20.Solvason N, Wu WW, Parry D, et al. Cyclin D2 is essential for BCR-mediated proliferation and CD5 B cell development. Int Immunol. 2000;12:631–638. doi: 10.1093/intimm/12.5.631. [DOI] [PubMed] [Google Scholar]
- 21.Jena N, Deng M, Sicinska E, Sicinski P, Daley GQ. Critical role for cyclin D2 in BCR/ABL-induced proliferation of hematopoietic cells. Cancer Res. 2002;62:535–541. [PubMed] [Google Scholar]
- 22.Alizadeh AA, Eisen MB, Davis RE, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature. 2000;403:503–511. doi: 10.1038/35000501. [DOI] [PubMed] [Google Scholar]
- 23.Klier M, Anastasov N, Hermann A, et al. Specific lentiviral shRNA-mediated knockdown of cyclin D1 in mantle cell lymphoma has minimal effects on cell survival and reveals a regulatory circuit with cyclin D2. Leukemia. 2008;22:2097–2105. doi: 10.1038/leu.2008.213. [DOI] [PubMed] [Google Scholar]
- 24.Chiles TC. Regulation and function of cyclin D2 in B lymphocyte subsets. J Immunol. 2004;173:2901–2907. doi: 10.4049/jimmunol.173.5.2901. [DOI] [PubMed] [Google Scholar]
- 25.Ehinger M, Linderoth J, Christensson B, Sander B, Cavallin-Stahl E. A subset of CD5-diffuse large B-cell lymphomas expresses nuclear cyclin D1 with aberrations at the CCND1 locus. Am J Clin Pathol. 2008;129:630–638. doi: 10.1309/42CQ0HU7XEY9QMQX. [DOI] [PubMed] [Google Scholar]
- 26.Rodriguez-Justo M, Huang Y, Ye H, et al. Cyclin D1-positive diffuse large B-cell lymphoma. Histopathology. 2008;52:900–903. doi: 10.1111/j.1365-2559.2008.03042.x. [DOI] [PubMed] [Google Scholar]
- 27.Wang SA, Wang L, Hochberg EP, Muzikansky A, Harris NL, Hasserjian RP. Low histologic grade follicular lymphoma with high proliferation index: morphologic and clinical features. Am J Surg Pathol. 2005;29:1490–1496. doi: 10.1097/01.pas.0000172191.87176.3b. [DOI] [PubMed] [Google Scholar]
- 28.Thompson MA, Stumph J, Henrickson SE, et al. Differential gene expression in anaplastic lymphoma kinase-positive and anaplastic lymphoma kinase-negative anaplastic large cell lymphomas. Hum Pathol. 2005;36:494–504. doi: 10.1016/j.humpath.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 29.Natkunam Y, Farinha P, Hsi ED, et al. LMO2 protein expression predicts survival in patients with diffuse large B-cell lymphoma treated with anthracycline-based chemotherapy with and without rituximab. J Clin Oncol. 2008;26:447–454. doi: 10.1200/JCO.2007.13.0690. [DOI] [PubMed] [Google Scholar]
- 30.Teramoto N, Pokrovskaja K, Szekely L, et al. Expression of cyclin D2 and D3 in lymphoid lesions. Int J Cancer. 1999;81:543–550. doi: 10.1002/(sici)1097-0215(19990517)81:4<543::aid-ijc7>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 31.Sehn LH, Donaldson J, Chhanabhai M, et al. Introduction of combined CHOP plus rituximab therapy dramatically improved outcome of diffuse large B-cell lymphoma in British Columbia. J Clin Oncol. 2005;23:5027–5033. doi: 10.1200/JCO.2005.09.137. [DOI] [PubMed] [Google Scholar]
- 32.Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med. 2002;346:235–242. doi: 10.1056/NEJMoa011795. [DOI] [PubMed] [Google Scholar]
- 33.Habermann TM, Weller EA, Morrison VA, et al. Rituximab-CHOP versus CHOP alone or with maintenance rituximab in older patients with diffuse large B-cell lymphoma. J Clin Oncol. 2006;24:3121–3127. doi: 10.1200/JCO.2005.05.1003. [DOI] [PubMed] [Google Scholar]
- 34.Pfreundschuh M, Trumper L, Osterborg A, et al. CHOP-like chemotherapy plus rituximab versus CHOP-like chemotherapy alone in young patients with good-prognosis diffuse large-B-cell lymphoma: a randomised controlled trial by the MabThera International Trial (MInT) Group. Lancet Oncol. 2006;7:379–391. doi: 10.1016/S1470-2045(06)70664-7. [DOI] [PubMed] [Google Scholar]