Abstract
While it is well known that the widowed suffer increased mortality risks, the mechanism of this survival disadvantage is still under investigation. In this article, we examine the quality of health care as a possible link between widowhood and mortality using a unique data set of 475,313 elderly couples who were followed up for up to nine years. We address whether the transition to widowhood affects the quality of care that individuals receive and explore the extent to which these changes mediate the elevated mortality hazard for the widowed. We analyze six established measures of quality of health care in a fixed-effect framework to account for unobserved heterogeneity. Caregiving and acute bereavement during the transition to widowhood appear to distract individuals from taking care of their own health care needs in the short run. However, being widowed does not have long-term detrimental effects on individuals’ ability to sustain contact with the formal medical system. Moreover, the short-run disruption does not mediate the widowhood effect on mortality. Nevertheless, long after spousal death, men suffer from a decline in the quality of informal care, coordination between formal and informal care, and the ability to advocate and communicate in formal medical settings. These findings illustrate women’s centrality in the household production of health and identify important points of intervention in optimizing men’s adjustment to widowhood.
Losing one’s spouse is one of the most traumatic transitions during the life course (Hatch 2000; Thompson et al. 1984). It has been well documented that individuals suffer increased mortality risks following spousal death (Elwert and Christakis 2006; Hu and Goldman 1990; Lillard and Panis 1996; Lillard and Waite 1995; Martikainen and Valkonen 1996). While the survival disadvantages of becoming widowed conform to broader findings on the role of social support and social ties on mortality (Berkman and Syme 1979; House, Landis, and Umberson 1988), the specific mechanism of this effect remains elusive. The bereavement literature has suggested that an array of biological and psychosocial factors may mediate the effect of spousal loss on mortality (Brown, House, and Smith 2006; Irwin and Pike 1993; Kim and Jacobs 1993; Williams 2004). However, studies that directly investigate the precise social and biological mechanisms of the survival disadvantages of becoming widowed are rare.
Here, we examine quality of health care as a potential link between widowhood and survival. It has been suggested that becoming widowed may alter individuals’ patterns of interaction with the formal medical system, which in turn may affect individuals’ health and survival (Elwert and Christakis 2006; Iwashyna and Christakis 2003; Litwak 1985; Litwak and Messeri 1989), but this conjecture has not been rigorously evaluated. We use a unique longitudinal data set of 475,313 elderly couples and ask two sets of related questions. First, do the patterns of health care use and the quality of health care individuals receive change when individuals lose their spouses? Moreover, how does the quality of health care vary at different stages of the transition to widowhood? Second, to what extent do these changes, if any, contribute to the elevated mortality risks among the widowed?
Investigating the patterns of changes in quality of health care surrounding the transition to widowhood and their effects on survival has significant theoretical and practical implications. It illustrates how the marital relationship, as one of the most prevalent and strongest dyadic ties in individuals’ informal social networks (McPherson, Smith-Lovin, and Brashears 2006), regulates individuals’ interactions with a macro-social institution, namely the formal medical system, and, as a result, affects important aspects of life chances, such as health and survival. Formal institutions and primary groups serve complementary and substitutive functions to fulfill individual needs (Litwak and Messeri 1989). The loss in one realm affects the functioning of the other. The bereavement literature has so far tended to focus on the effects of spousal loss on bereaved individuals and their primary groups but has paid little attention to the interplay of individuals and formal institutions.1 Practically, to the extent that quality of health care serves as a link between the transition to widowhood and survival, this investigation provides insights into the timing and methods of interventions that may attenuate the harmful consequences of widowhood.
In the following sections, we first discuss theoretical perspectives on how becoming widowed may alter patterns of health care use and quality of health care that individuals receive. Gender differences are an intrinsic focus of the research on marriage and health and are therefore considered. The link between quality of health care and survival in older adults is also discussed. We introduce the data and statistical methods and then present and discuss the findings.
QUALITY OF HEALTH CARE DURING THE TRANSITION TO WIDOWHOOD
The Effects of Becoming Widowed on Quality of Health Care
The married typically enjoy better health than the unmarried (Lillard and Panis 1996; Waite and Gallagher 2000). Two causal explanations, which emphasize the marital benefits and the crisis of marital disruption, have been proposed to account for the marital advantages and can be applied to understand the quality of health care during the transition to widowhood (Wade and Pevalin 2004; Williams and Umberson 2004).
First, the marital-benefits perspective suggests that social control and social integration provided by the marital relationship discourage risky behavior and encourage healthful behavior (Laub et al. 1998; Umberson 1987, 1992). To the extent that maintaining regular interaction with health care providers, following medical regimens, and performing self-care and self-monitoring are seen as fostering health, the married may be particularly motivated to engage in such activities. As a result, the married may be better able to enjoy appropriate use of health care and better coordination of formal and informal care than the unmarried.
Spouses also provide instrumental support that enables appropriate use of health care. Spouses may serve as conduits of information for each other. Marriage generally expands one’s social network; consequently, the married may have access to a larger and better referral network and may obtain more and better information on health and health care, which they can use to assess their own health conditions and evaluate treatment options (Iwashyna and Christakis 2003). Spouses may also serve as advocates for their partners during interactions with health care providers. Spouses may facilitate communication with health care providers and help evaluate treatment options during interactions in the formal medical system. This function is especially important when the partners are incapacitated.
When spouses die, the benefits conferred by the marital relationship may be at least partially lost (Umberson 1992), though the depletion of marital benefits may start before the actual death of the spouse (Prokos and Keene 2005; Utz et al. 2004). Among older adults, spousal death is typically preceded by episodes of serious illnesses. The declining health of the ailing spouse may render him or her incapable of providing instrumental support or motivating his or her spouse to maintain healthful behavior (Christakis and Allison 2006).
Second, the crisis perspective argues that the process of transitioning to widowhood redistributes household resources (Dunkin and Anderson-Hanley 1998; Shaw, Patterson, and Semple 1997). Spousal illness prior to death diverts household resources away from the surviving spouse, who typically also bears the burden of caregiving. As a result, the surviving spouse’s interaction with the formal medical system may be disrupted. The literature on bereavement adjustment of caregivers after the death of recipients of caregiving provides two opposite predictions. The relief model suggests that the death of the ailing spouse may relieve the surviving spouse of the burden of caregiving and thus refocus household resources on his or her own health care needs (Bernard and Guarnaccia 2003; Mullan 1992). On the other hand, the complicated grief model suggests that accumulated stress compromises the coping abilities of the surviving spouse (Bernard and Guarnaccia 2003; Stroebe and Stroebe 1993). Complicated grief, coupled with the strain of adjustment to new roles and reconfiguration of the household, may distract the surviving spouse from taking care of his or her health care needs.
The arguments of the loss of marital benefits and the disruption caused by spousal death converge in their predictions regarding the trajectories of changes in health care use at some stages during the transition to widowhood. For example, the burden of caregiving and the incapacitation of the dying spouse typically occur at the same time; the acute bereavement and the loss of marital benefits due to spousal death coincide as well. The negative effects of these distinctive processes on quality of health care are hard to distinguish. On the other hand, Lopata (1996) found that after two years of bereavement, most widows and widowers were able to adjust to their new roles. The crisis model predicts that the detrimental effects of spousal death on quality of care diminishes and disappears in the long term; the explanation of loss of martial benefits suggests that these detrimental effects persist. By examining the trajectories of changes in quality of care, it is therefore possible to make some inferences regarding the independent effects of the loss of marital benefits and crisis of spousal death.
Gender Differences
Gender differences are a traditional focus of the research on marriage. In the household division of labor, wives are traditionally charged with taking care of the health needs of household members (Harrison 1978; Stolzenberg 2001; Umberson 1992). In addition, wives are more likely than husbands to do the emotional work of maintaining the couples’ social network (di Leonardo 1987; Hagestad 1986; Powers and Bultena 1976). It follows that husbands may suffer a greater loss in marital benefits than wives in terms of quality of health care when they become widowed. Husbands also have a more difficult time adjusting to the reconfiguration of the household and the management of daily tasks after becoming widowed (Gupta 1999; Utz et al. 2004).
Indeed, the bereavement literature has generally found that widowers suffered worse health outcomes than widows (Gove 1973; Helsing and Szklo 1981; Martikainen and Valkonen 1996; Stroebe and Stroebe 1983). Our work here focuses on elderly couples—for whom the traditional gender roles are more salient than for their younger counterparts (Rogers and Amato 2000)—and we expect that the transition to widowhood will have more detrimental effects on quality of care for men than for women. On the other hand, a few studies have failed to find gender differences in different dimensions of life after widowhood (Elwert and Christakis 2006; Schaefer, Quesenberry, and Wi 1995). Therefore, it needs to be empirically verified whether men would be worse off in terms of obtaining appropriate health care than women after spousal loss.
Quality of Health Care as a Mediator of the Widowhood Effect
In the United States, 74% of all deaths occur in the population aged 65 or older (Hoyert, Kung, and Smith 2005). The elderly are more likely to suffer from chronic illness, or often a combination of several chronic illnesses, than the younger population (Bos Van Den 1995; Wolff, Starfield, and Anderson 2002). With the development of effective medical therapies in the past few decades, appropriate utilization of health care has become crucial in maintaining health for the elderly (Christakis and Iwashyna 2003; Cutler 2004; Rowe 1985; Wang et al. 2007). If individuals tend to neglect their health care needs during the time surrounding the transition to widowhood, it is natural to ask whether and to what extent this neglect contributes to the adverse health outcomes and elevated mortality suffered by the widowed. Hence, a second goal of the present research is discovering whether any observed decrement in health care quality as a result of having a sick or dead spouse plays a role in a person’s elevated mortality risk during the period after becoming widowed.
With a few exceptions (Iwashyna and Christakis 2003; Prigerson, Maciejewski, and Rosenheck 1999), there has not been systematic research on how marriage or widowhood per se influences individuals’ interactions with the health care system. To our knowledge, no studies have examined quality of health care as a mediator between widowhood and mortality. Prior work has explored cross-sectional correlations between marital status and health care utilization and has suggested that married individuals enjoy better quality of health care than the widowed (Chin and Goldman 1997; Goodwin et al. 1987; Iwashyna and Christakis 2003; Lannin et al. 1998; Mark and Paramore 1996; Prigerson et al. 1999; Sox et al. 1998). However, the causal direction and mechanisms are less than clear in these cross-sectional studies. In particular, married couples tend to share a similar living environment and lifestyle. To the extent that characteristics of the shared environment or lifestyle lead to both low quality of health care and spousal death, we might observe a correlation between low quality of health care and being widowed if we compare the use of health care of those who do and those who do not experience spousal death. That is, the potential selection process out of marriage, rather than the casual effects of becoming widowed, might account for the observed correlation. Moreover the same selection process might also confound the assessment of the widowhood effect on the mortality of the surviving spouse. Therefore, in this article, we take a fixed-effects approach that compares the same individuals before and after spousal death, which accounts for all observed and unobserved traits that are stable over time.
DATA AND METHODS
Data
We compiled Medicare claims data to obtain a very large cohort of elderly couples. First, we used the Medicare Denominator File, which captures 96% of all elderly Americans, to identify Medicare beneficiaries who were 65 years of age or older as of January 1, 1993. Specially developed algorithms were then used to identify married couples (Iwashyna et al. 2002; Iwashyna et al. 1998); out of an estimated 6.6 million couples in which both spouses were older than 65, we identified 5,496,444 couples (83%). Past research has shown that these couples were representative of all U.S. married couples who were 65 years of age or older in terms of sociodemographic characteristics (Iwashyna et al. 2002). Eighty-nine percent of these were between the ages of 65 and 98 and resided in the United States. From this group, we drew a random sample of 518,240 couples (11%). Individuals enrolled in Medicare managed care plans were excluded from the analytical sample because the data on health care utilization are not complete for these individuals. Our primary analytical sample consisted of 475,313 couples.
We combined multiple data sets provided by the Center for Medicare and Medicaid Services. The Vital Status File provided complete, daily follow-up of mortality status through January 1, 2002; this information allowed us to construct precise time-dependent measures of widowhood and mortality status. We obtained inpatient and outpatient claims for our sample for a nine-year period from 1993 to 2001, which provided diagnostic details and information on health care use. We used these data to construct time-varying measures of health care use and quality; the construction of these measures is discussed in more detail below. The Denominator File provided information on baseline demographic characteristics.
Quality-of-Care Measures
Quality of care is a multidimensional concept (Brook, McGlynn, and Cleary 1996). We focus on two types of quality-of-care measures that are sensitive to patient agency and advocacy. These measures of quality are consequential to health outcomes in and of themselves (Smith-Bindman et al. 2006; Wang et al. 2007). Here, in keeping with past work, we also take them to be indicators of various aspects of a broader concept of quality of health care (Cutler 2004).
The first type of measures indicates whether certain processes of care are performed. We examine whether individuals received each of four recommended measures of preventive care and chronic care management at appropriate frequencies, including diabetic monitoring (hemoglobin A1c testing2 and diabetic eye examination), cancer screening (mammogram), and vaccinations (influenza vaccination). These measures do not typically involve medically urgent situations, and patients therefore have more control over their occurrence. Their occurrence indicates the ability of the patients to maintain appropriate and desirable contact with their health care providers. Consensus in the medical community has established relatively unequivocal recommendations as to the frequency of delivery of these services in eligible populations (Pham et al. 2005). Table 1 reports the eligibility criteria and expected annual rates of performance of these quality-of-care measures. For example, it has been recommended that women between ages 65 and 74 should have annual mammograms; the expected annual rate is therefore 100%. Medicare claims data have been used with great success to identify eligible populations and to detect and time the delivery of these services. The methods used to identify the occurrences of these services have been previously evaluated and validated by other investigators (Pham et al. 2005).
Table 1.
Eligibility Criteria for Quality-of-Care (QOC) Indicators, Expected Rates of QOC Indicators in One Year, Observed Rates of QOC Indicators in 2001, and Cohort Sizes at Baseline
| Quality Measures | Eligibility Criteria | Expected Rates of QOC Indicators in One Year, %a | Observed Rates of QOC Indicators in One Year, %a | Cohort Size at Baseline |
|
|---|---|---|---|---|---|
| Nonwidowed | Widowed | ||||
| Influenza Vaccination | Age ≥ 65 years | 100 | 40 | 657,693 | 292,933 |
| Mammograms | Women aged 65–74 years, excluding those with cancer diagnoses or surgery of the breast | 100 | 37 | 160,165 | 91,153 |
| Diabetic Eye Examinations | Medicare beneficiaries ≥ 65 years diagnosed with diabetes | 100 | 44 | 94,354 | 37,892 |
| Hemoglobin A1c Monitoring | Medicare beneficiaries ≥ 65 years diagnosed with diabetes | 100 | 56 | 94,354 | 37,892 |
| Preventable Hospitalizations | Age ≥ 65 years | 0 | 6.7 | 657,693 | 292,933 |
| Early Readmissions | Age ≥ 65 years | 0 | 1.4 | 657,693 | 292,933 |
Rates are for the eligible populations.
The second type of measure examines the outcomes of health care provision. We use two measures of this type: the occurrence of preventable hospitalizations and early readmission after hospitalization. Preventable hospitalizations are hospitalizations for so-called ambulatory care–sensitive (ACS) conditions, such as asthma, diabetes, and hypertension (Billings, Anderson, and Newman 1996; Bindman et al. 1995; Blustein, Hanson, and Shea 1998). Hospitalization for ACS conditions is generally considered avoidable because if the patient’s care had been better organized as an outpatient, the disease process could have been headed off at an earlier point, and thus the patient would not have had to be hospitalized for these conditions. The Agency for Healthcare Research and Quality provides a set of criteria to identify ACS-related conditions, which we applied to the diagnosis codes associated with inpatient claims to identify associated hospitalizations (Agency for Healthcare Research and Quality 2003). An early readmission is defined as an admission for the same principal diagnosis less than two weeks after the discharge of an earlier admission. If a patient is given good care in the hospital, he or she should not need to be readmitted for the same diagnosis within two weeks of discharge. It is generally argued that early readmissions are an indicator of suboptimal care in the hospital (Ashton et al. 1997). Taken together, the occurrence of preventable hospitalizations and early readmissions signal patients’ inability to communicate with health care providers, provide complementary informal care at home, and coordinate formal and informal care. These measures may be particularly responsive to the presence of another individual in the household, such as a spouse, who can serve these functions. These six measures of quality of health care have been widely used to assess the performance of physicians and health plans (National Committee for Quality Assurance 2006).
The unit of our analysis is person-month. We generated a record for each month a person was alive during the study period; a person who survived until the end of the nine-year study period contributed 108 records to the analysis. For a given month, in terms of preventive services and chronic care management, a person may be in one of three mutually exclusive states. Mammograms can serve as an example. In a given month, a woman between 65 and 74 years of age may have had a mammogram in the previous 12 months and therefore did not need to get a mammogram in that month. Conversely, she may not have had a mammogram in the previous 12 months and thus needed one that month; she may or may not have gotten one. For each preventive measure, we generated two time-varying variables. The first variable indicates, in a given month, whether patients were “up-to-date” in terms of a preventive service, that is, whether they received the recommended service in the previous 12 months. Among the patients who were not “up-to-date” and therefore were “at risk” for receiving that service, we generated a second variable indicating whether the patients received the service that month. The two variables are complementary, with one indicating the cumulative effect of accessing preventive services during a fixed period and the other indicating the action of the patient in a particular point in time. For the occurrence of preventable hospitalizations and early readmissions, we constructed time-varying variables indicating whether such an event occurred in a given month.
Statistical Methods
Our analysis proceeded in two steps. In the first step, we examined the effects of the transition to widowhood on indicators of the quality of health care. The dependent variables are whether an individual received a preventive service in a given month, given that he or she did not receive the service in the previous 12 months, or whether an individual had a preventable hospitalization or an early readmission in a given month. We used conditional logit models to obtain fixed-effect estimates. The equations used to model the occurrence of these events take the form
where P(yjit = 1) is subject i’s probability of having event j (e.g., mammogram) in month t. Wit is a vector of 15 dummy variables indicating the amount of time preceding and succeeding spousal death (3 or more years, 2 years, 1 year, 7–12 months, 3–6 months, 2 months, and 1 month before spousal death; the month of the death; and the same time intervals after spousal death). The coefficients of Wit, δj, capture the trend in changes of quality-of-care indicators before and after spousal death for those who experienced spousal death.
Zi and αi represent observed and unobserved time-invariant individual traits (e.g., gender); both Zi and αi were eliminated in the fixed-effect estimation. To assess gender differences in the effects of transition to widowhood on the use of health care, we examined the interaction terms between Wit and gender.
Xit is a group of time-varying control variables. We included dummy variables representing each of the nine years during the study period to account for the secular time trend. As individuals age, their consumption of health care in general increases; we accounted for the age effect by including dummy variables indicating incremental age grouped into two-year intervals. Age is measured in months; as a result, both age and year were identified in the fixed-effect models. Serious health conditions can distract individuals from paying attention to routine and preventive services; severity of illness has also been shown to be correlated with early readmission (Holloway, Medendorp, and Bromberg 1990). We therefore controlled for time-varying indicators of health status. We used two years of inpatient claims prior to a given month to construct a Charlson index,3 which summarizes the illness burden in the month (Charlson et al. 1987). For this reason, individuals have to be at least 67 years of age as of 1993 in the analytical sample because younger persons did not have claims data for the entire period from 1991 to 1992. We also calculated the number of days an individual spent in the hospital in the year prior to a given month and the number of days an individual spent in the hospital in a given month as indicators of health status. For patients with diabetes, we also constructed and controlled for variables indicating whether an individual suffered from four types of diabetes-related complications in a given month, since diabetic monitoring typically intensifies as these complications emerge. The analysis of the occurrence of influenza vaccination is limited to the months between October and February because the vast majority of the elderly are “at risk” for influenza vaccination only in these months. We included in this analysis dummy variables indicating the calendar month because the probability of having an influenza vaccination varies a great deal over the months. It is also possible that as the frequency of hospitalizations increases, preventable hospitalizations are more likely to occur, other things being equal. We therefore controlled for the occurrence of hospitalizations that were not related to ACS conditions in a given month.
In the second step of our analysis, we tackled the question of whether quality of health care, as measured by our standard indicators, mediates the link between widowhood and elevated mortality risks. To examine whether quality-of-care indicators are mediators, we first needed to establish that they are associated with both the mortality risks and being widowed. We therefore first evaluated the link between becoming widowed and quality-of-care indicators. We then assessed the mediating effect of quality-of-care indicators. To do that, we estimated the widowhood effect on mortality in models with and without indicators of quality of care and compared the estimates of widowhood effect on mortality in these nested models. To the extent that the widowhood effect decreases or disappears, we would detect a mediating effect (Clogg, Petkova, and Haritou 1995). We used measures of preventive service delivery as markers of quality of care in the second step of the analysis. We used lagged and cumulative measures of quality of care in these analyses; that is, we used whether an individual obtained particular preventive services in the year prior to a given month as quality indicators in this step of the analysis.4 We did not include measures of preventable hospitalizations and early readmissions because these measures also tend to indicate health status.5
We applied a novel approach that estimates fixed-effect survival models of non-repeatable events, such as death. Two layers of confounding are not accounted for in conventional survival models. First, shared environment and behavior in a couple may affect the mortality of both the husband and wife. Mortality of the partner following spousal death may then be attributed to the shared traits rather than the death itself. Second, intrinsic individual traits, such as the ability to maintain a healthy lifestyle, may lead to both appropriate use of health care and low mortality risks. An observed relationship between the appropriate use of health care and low mortality risks may at least partially reflect the confounding effect of individuals’ intrinsic tendency, rather than the protective effects of high quality of health care.
To account for these potential unobserved confounders, we would ideally want to compare the mortality risk for the same individual over time; that is, we would want to perform a fixed-effect analysis of the mortality risk. However, death is a nonrepeatable event. It always takes place at the end of the observation period, and therefore, the survival status is a monotonic function of time. Conventional fixed-effects models cannot provide valid estimates in this context. Hence, we employed the case-time-control method, which reverses the dependent and independent variables in the estimation of conditional logistic regressions (Allison and Christakis 2006). This method takes advantage of the fact that when both the dependent and independent variables are dichotomous, the odds ratio is symmetric. Therefore, reversing the dependent and independent variables produces the same result. Again, the data are organized into a person-month format.
In the analysis of the effect of quality-of-care indicators on mortality, the dependent variable is a time-varying indicator of health care quality; the independent variable is the survival status in a given month, and its coefficient indicates the effect of health care quality on mortality. In the analysis of the mediating effect of the quality of health care on the effect of widowhood on mortality, the dependent variable is a time-varying indicator of whether the spouse died during a specific interval of time (e.g., 1 month, 2 months, 3 months, 6 months, and 1 year) before a given month. The independent variable is again the survival status in a given month, and its coefficient denotes the effect of widowhood on mortality. We applied the case-time-control method with and without the time-varying quality-of-care indicators and assessed the changes in the widowhood effect on mortality in these nested models. Time-varying covariates can be introduced in these models. We controlled for the time trend and age.
RESULTS
Cohort Attributes and Descriptive Statistics
Table 1 shows the eligibility criteria for receiving the preventive services and the size of the cohorts that met the eligibility criteria at the inception of the study, stratified by whether the subject became widowed during the study period. Only those diagnosed with diabetes were eligible for diabetic monitoring; about 13% of the sample had diabetes at baseline. An annual mammogram is recommended for women between 65 and 74 years old. As they became older than 74 years of age during the follow-up period, they became ineligible for annual mammograms and were dropped from the analysis. We excluded anyone who had breast cancer or surgery of the breast at any time during 1991 to 2001. Table 1 also shows the rates of occurrences of quality indicators in 2001, which were well below the expected annual rates (100%).
Table 2 displays summary statistics for select covariates at three levels: the person-month (for time-varying covariates), the individual, and the residential context. The first three columns show the summary statistics for the entire sample, the nonwidowed, and the widowed. The last two columns display the summary statistics for diabetes patients and women who were eligible for annual mammograms.
Table 2.
Descriptive Statistics for Select Variables by Widowhood Status and Cohorts
| All | Widowhood Status |
Mammography Cohort | Diabetes Cohort | ||
|---|---|---|---|---|---|
| Nonwidowed | Widowed | ||||
| Person-Month Level | |||||
| Hospital days in the past year (mean) | 8.9 | 8.4 | 9.9 | 7.0 | 8.1 |
| Hospital days in the past month (mean) | 4.6 | 4.4 | 4.9 | 3.8 | 3.2 |
| Charlson index (mean) | 1.3 | 1.3 | 1.3 | 0.99 | 1.3 |
| Number of diabetic complications (mean) | –– | –– | –– | –– | 0.78 |
| Individual Level | |||||
| Age, in years (mean) | 75 | 74 | 75 | 70 | 75 |
| Women (%) | 49 | 41 | 67 | 100 | 48 |
| African American (%) | 9.1 | 9.0 | 9.1 | 8.8 | 14.0 |
| Poor (%) | 5.4 | 4.8 | 6.7 | 5.6 | 9.5 |
| Residential Context | |||||
| Urbanization index | 68 | 68 | 68 | 68 | 67 |
| % African American | 8.9 | 8.8 | 9.4 | 9.1 | 11.0 |
| Median home value ($) | 91,641 | 92,961 | 88,679 | 90,168 | 84,067 |
| Median income ($) | 30,383 | 30,658 | 29,765 | 30,318 | 29,229 |
| Male unemployment rate | 4.4 | 4.4 | 4.5 | 4.5 | 4.8 |
| % Poor | 13 | 13 | 13 | 13 | 14 |
| % Less than high school | 24 | 24 | 25 | 25 | 26 |
Trajectories of Changes in Quality-of-Care Indicators Surrounding the Transition to Widowhood
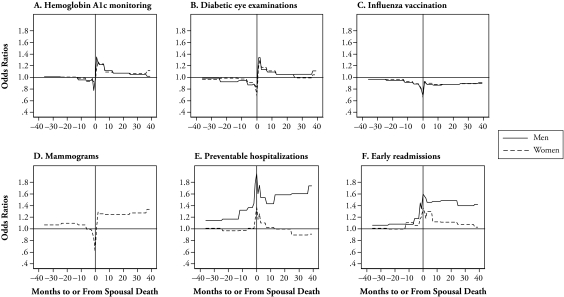
We first addressed the question of whether quality of care changed around the transition to widowhood. The average rates of diabetic eye exam and hemoglobin A1c monitoring among eligible diabetes patients in a given month were 3.6% and 2.5%, respectively. On average, 13% of the individuals who were “at risk” for influenza vaccination got the vaccination in a given month6; 3.5% of the women eligible for a mammogram got it in a given month. The average monthly rates of preventable hospitalizations and early readmissions were 1.3% and 0.09%, respectively. We explored the trajectories of changes in quality indicators by examining the coefficients of the dichotomized variables indicating the time intervals before and after spousal death. We hypothesized that the process of becoming widowed has a more negative impact on the quality of health care for men than for women. To facilitate the visualization of the trajectories of the changes, Panels A–F of Figure 1 graph the estimated odds ratios of the occurrence of quality-of-care indicators relative to the baseline period (three years prior to spousal death) during various time intervals before and after spousal death for men and women separately (except for mammograms, which are applicable only to women). Appendix A presents these odds ratios and their statistical significance, as well as the likelihood ratio chi-square tests for the overall statistical significance of the interaction terms between gender and the series of dichotomized variables indicating the time intervals before and after spousal death. The horizontal axis in Panels A–F in Figure 1 represents the months before or since spousal death; the vertical axis represents the odds ratio of event occurrence in a given month. The horizontal line in the graphs shows the baseline level, and the vertical line marks the month of spousal death.
Figure 1.
Trajectories of Changes in Quality-of-Care Indicators During the Transition to Widowhood, by Gender
Notes: The odds ratios of the occurrence of quality-of-care indicators in a given month within various time intervals before and after spousal death for men and women are shown, including hemoglobin A1c testing (Panel A), diabetic eye exams (Panel B), influenza vaccination (Panel C), mammograms (Panel D), preventable hospitalizations (Panel E), and early readmissions (Panel F). These estimates were generated in conditional logit models in populations eligible for the quality-of-care indicators. The horizontal line in the figures represents the baseline level, and the vertical line represents the month of spousal death.
Panels A–C suggest little gender difference in the trajectories of changes in influenza vaccination or diabetic monitoring (A1c test and eye exam).7 At approximately 7–12 months before spousal death, the likelihood of receiving these services decreased significantly, which was then followed by a precipitous drop as spousal death approached; the nadir typically happened in the month when the death occurred. In the months immediately after spousal death, the rates of obtaining these services shot up; except for influenza vaccination, the rates rose significantly higher than the baseline rates. These trajectories diverged beyond the first three months following spousal death. The likelihood of obtaining influenza vaccination fell after the initial rise and remained slightly lower than the baseline. The likelihood of obtaining diabetic monitoring decreased steadily after the initial rise and either returned to the baseline level (dilated eye exams) or was slightly higher than the baseline (hemoglobin A1c tests) two years after spousal death.
Similar to influenza vaccination or diabetic monitoring, the likelihood of obtaining mammograms for women between ages 65 and 74 decreased as spousal death approached, reached the bottom in the month of spousal death, and started to increase in the months following spousal death (Panel D of Figure 1). Unlike the other measures, the likelihood of mammogram occurrence remained high after the initial rise and steadily increased as the amount of time lapsed since spousal death.
Panels E–F show large gender differences in the rates of preventable hospitalizations and early readmissions. In terms of preventable hospitalizations, the rates increased significantly about one year before spousal death for men but remained unchanged for women. During the month of spousal death, the rates of preventable hospitalizations spiked for both men and women and then gradually declined in the months immediately after spousal death. About six months after spousal death, the rates returned to the baseline level and became even lower than the baseline level after about two years into widowhood for women. For men, the rates remained much higher than the baseline level and started to increase steadily at about six months after spousal death. In other words, only the short-term shock of becoming widowed increased the risks of having preventable hospitalizations for women; however, men’s risks increased during the whole process of transitioning to widowhood and remained higher than the baseline level long after spousal death (Panel E).
Similarly, widowed men were much more likely than widowed women to experience early readmissions. The rates of early readmissions spiked for both men and women at the time of spousal death, but for women, these rates declined steadily and returned to the baseline level three years after becoming widowed. For men, the rates declined at a much slower pace and remained much higher than the baseline level three years after spousal death (Panel F).
The Quality of Health Care and Widowhood Effect on Mortality
We consistently observed a decline in quality of health care before and at the time of spousal death, when the crisis caused by the pending death of the spouse was presumably unfolding. Moreover, the mortality risk for the newly bereaved was especially high; for example, a recent study found that the hazard of death increased 52% for men and 62% for women during the first month of bereavement (Elwert and Christakis 2006). Our question was whether neglecting one’s health care needs when one’s spouse was dying or after spousal death contributed to the subsequent elevated mortality risks during bereavement. Table 3 displays the survival status at the end of the follow-up period by gender and widowhood for each of the cohorts that met the inclusion criteria for different quality measures.8
Table 3.
Survival at the End of Follow-up, by Gender and Widowhood Status in Eligible Cohorts (N, with % in parentheses)
| Nonwidowed |
Widowed |
|||||||
|---|---|---|---|---|---|---|---|---|
| Dead | Alive | Dead | Alive | |||||
| Men | ||||||||
| All | 219,074 | (56) | 169,771 | (44) | 48,932 | (50) | 49,191 | (50) |
| Diabetes cohort | 40,361 | (71) | 16,186 | (28) | 7,828 | (62) | 4,896 | (38) |
| Women | ||||||||
| All | 105,021 | (39) | 168,827 | (61) | 63,437 | (33) | 131,373 | (67) |
| Diabetes cohort | 23,234 | (61) | 14,573 | (39) | 11,794 | (47) | 13,374 | (53) |
| Mammography cohort | 46,096 | (29) | 114,069 | (71) | 18,773 | (21) | 72,380 | (79) |
To assess the mediating effect of the quality-of-care indicators, we first examined the relationship between quality-of-care indicators and mortality. We then compared estimates of the hazard of death during various time intervals after spousal death in fixed-effect models of mortality without and with quality-of-care indicators. We found a negative relationship between the occurrence of quality-of-care indicators and mortality. Appendix B displays the odds ratios of death in a given month associated with being “up-to-date” on receiving a specific preventive service. The effects of preventive service on the mortality risk are quite large, as we argued that obtaining these preventive services is a marker of health care quality (Appendix B). A recent study of influenza vaccination in an elderly population also found large effects of the vaccination on cause-specific and all-cause mortality (Wang et al. 2007).
Table 4 presents odds ratios of death of the surviving spouse during different time intervals after becoming widowed. Consistent with previous studies, individuals’ risks of death increased significantly after the deaths of their spouses and remained elevated for up to two years. Odds ratios estimated from the base models (without the quality-of-care indicators) are similar in magnitude to those estimated from models with quality-of-care indicators at all time intervals. That is, adding the quality-of-care indicators had little effect on the estimates of the widowhood effect on mortality for both men and women. Our investigation therefore suggests that the quality of health care, as we measured it, has little effect on the relationship between being widowed and the mortality risk.
Table 4.
Odds Ratios of Death in a Given Month Within Various Time Intervals After Spousal Death Estimated in Models With and Without Quality-of-Care Indicatorsa
| Time After Spousal Death | Men |
Women |
||
|---|---|---|---|---|
| Base Modelb | + Quality-of-Care Indicatorsc | Base Modelb | + Quality-of-Care Indicatorsc | |
| 1 Month | 1.384 | 1.381 | 1.437 | 1.433 |
| 2 Months | 1.328 | 1.325 | 1.315 | 1.311 |
| 3–6 Months | 1.222 | 1.219 | 1.180 | 1.176 |
| 7–12 Months | 1.255 | 1.253 | 1.159 | 1.157 |
| 2 Years | 1.416 | 1.413 | 1.244 | 1.242 |
Estimates are generated by case-time-control models (fixed-effect models for nonrepeatable events). All estimated odds ratios are statistically significant at p < .001 (two-tailed tests).
The base models control for time trend and age.
Quality-of-care indicators are added to the base models.
DISCUSSION
The transition to widowhood does indeed influence the quality of health care that individuals receive. Past work suggests that the loss of marital benefits and the crisis caused by spousal death may combine to negatively affect individuals’ abilities to maintain contact with health providers, advocate for themselves in the formal medical system, and coordinate formal and informal care (Umberson 1987; Williams 2004; Williams and Umberson 2004).
Our analyses support the crisis model: the occurrences of quality-of-care indicators experienced significant fluctuation during the months surrounding spousal death. During the time leading up to spousal death, all quality indicators experienced a gradual but significant decline. This decline is likely indicative of the burden of spousal caregiving and/or the loss of marital benefits due to spousal incapacitation. In the month when spousal death occurred, all quality indicators experienced a sharp drop, which may be attributed to acute bereavement and the need to manage the urgent and practical matters associated with the passing of a spouse.
In the months immediately after spousal death, the quality indicators improved, especially the rates of preventive service delivery and diabetic monitoring. At this time, newly widowed individuals intensified their interaction with the formal medical system; the rates and numbers of visits to both primary care physicians and specialists reached the highest point (results not shown). Consistent with the relief model, these trends may reflect a tendency of the newly widowed to compensate for earlier neglect of their health care needs. In addition, spousal death might remind them of their own vulnerability (Walter 2003). Or they might feel particularly unwell and think that health care providers can offer comfort and help; the physical manifestation of grief might lead the widowed to seek the assistance of medical professionals, who might take the opportunity to perform routine and preventive services (Stroebe et al. 2001). Regardless of their motives, the newly widowed appear to have had enough resources to sustain a high level of contact with the formal medical system. Spousal death may have freed up household resources, in particular the time of the surviving spouse that used to be devoted to caring for the dying spouse. It is also very likely that during the time following spousal death, the widowed experienced a surge of attention and support from their family and friends (Ha 2008). Future work will need to explore which of the foregoing mechanisms were operational.
Whether our findings support the argument regarding the positive impact of marriage with respect to interaction with the formal medical system is more ambiguous. First, being widowed proved not to have long-term detrimental effects on individuals’ abilities to obtain preventive services. That is, losing one’s spouse does not have sustained negative effect on one’s abilities to maintain contact with the formal medical system. However, these findings do not imply that there are no marital benefits. It is plausible that internalized values and habituated behaviors acquired during the marriage continued to function without external sanction or motivation after spousal death. These findings also do not preclude the possibility that the marital benefits were partially lost after spousal death but the surviving spouses were able to compensate for the loss and gradually regain their ability to maintain contact with the formal medical system. This scenario is consistent with the trajectory of changes in the likelihood of receiving influenza vaccination; after the precipitous drop at the time of spousal death and a large rise immediately after, the rate of influenza vaccination remained lower than the baseline level but gradually increased and approached the baseline level three years after spousal death. On the other hand, the rates of breast cancer screening and diabetic monitoring rose well above the baseline level following spousal death. In these cases, the depletion of marital benefits, if the depletion took place at all, seems to have been overwhelmed by the intention to seek medical help and the availability of additional resources.
On the other hand, for men, the rates of preventable hospitalizations and early readmissions remained higher than the baseline level three years after spousal death. We suggest that whereas obtaining appropriate preventive services can be achieved through sustained outpatient interaction with the health care providers, more factors are involved in avoiding preventable hospitalizations and early readmissions. Preventable hospitalizations may be headed off with both sustained interaction with health care providers and adequate home and self-care, as well as coordination between the formal and informal care. Early readmissions may be prevented by good communication between the patient and doctor, competent discharge planning, and again adequate home and self-care after discharge. As a result, avoiding these undesirable events may be more sensitive to spousal inputs.
We argue that the elevated risks for these undesirable outcomes suffered by men after they became widowed signal the loss of marital benefits provided by the wives. What kind of marital benefits are lost? Our data do not allow us to tease out precisely whether the loss was tied to the wives’ role in helping to maintain contact with the formal medical system, supporting self-care and providing informal care at home, or helping coordinate formal and informal care. However, we observed that men did not differ from women in obtaining preventive services after becoming widowed. This suggests that when men became widowed, they lost help with self-care and informal care as well as help with coordinating care needs; possibly, they may have had to substitute that loss with formal care provided in the institutional settings of the health care system. The loss of marital benefits probably does not lie in promoting contact with the formal medical system, but in spouses’ role as advocates, caregivers, and coordinators of health care. These gender differences highlight women’s centrality in the household production of health (di Leonardo 1987; Powers and Bultena 1976). These findings may have practical implications since they identify important points of intervention for friends, family, and social services in optimizing men’s adjustment to widowhood.
The trajectories of changes in preventive service delivery generally suggest that there is little decline in the likelihood of obtaining these services after spousal death. But the long-term effects of being widowed on the rates of obtaining different preventive services did vary, which merits further consideration. Although vaccination, cancer screening, and diabetic monitoring are subsumed under the heading of preventive services, they serve different functions, and patients and doctors may attach different salience and urgency to different services. For example, practices of diabetic monitoring are associated with a chronic disease that has already occurred; they are preventive in the sense that they may slow the progression of the disease and prevent acute symptoms. Patients with diabetes may have adopted diabetic monitoring as a routine practice, and this routine may be reinforced by interactions with their doctors. The routine nature of diabetic monitoring could explain why, after the shock and aftermath of spousal death, the rates of diabetic monitoring stabilized at a level close to that before the onset of the process of transitioning to widowhood.
Cancer screening may become particularly salient to the widowed who were made acutely aware of their own mortality with the experience of spousal death (Walter 2003:15); we may therefore observe an increase in the occurrence of post-widowhood mammograms. As a sensitivity analysis, we examined the trajectory of prostate cancer screening during the transition to widowhood for men between ages 65 and 74 and similarly observed an upward trend in the occurrence of prostate cancer screening after spousal death (results not shown).9 The idiosyncrasy of the mammogram trajectory therefore cannot be attributed to female gender. Among the preventive services under examination, only influenza vaccinations are generally applicable to both spouses. The fact that influenza vaccinations are actually relevant to both spouses might add to the importance of having a spouse to obtaining influenza vaccinations; for example, spouses may obtain these shots together. This may explain why the rates of influenza vaccination lingered slightly below the baseline level long after spousal death.10
We offer the foregoing explanations for why the long-term effects of being widowed varied across different measures of preventive service delivery. However, our ability to use the available data to test the validity of these explanations is limited. More measures of different types of quality indicators would help differentiate the effects of being widowed from the nature of measures under examination.
Our second goal here was to examine whether the changes in quality of health care surrounding the transition to widowhood mediate the much-documented relationship between widowhood and elevated mortality risks. Although we found that quality of care fluctuated around spousal death and that the quality indicators were predictive of the mortality risk of the surviving spouse, our analysis did not detect any mediating effects of health care quality on the widowhood effect on mortality. This finding does not conform to the speculation in the literature about the detrimental effect of a decline in the quality of health care due to widowhood. However, this study first shows that the pattern of changes in quality of health care surrounding spousal death is more complicated than that of a simple decline. Quality of care did experience a decline prior to and at the time of spousal death. But some quality indicators, in particular the use of preventive services, quickly recovered in the months following spousal death; in the long run, being widowed did not exert a strong negative influence on these indicators. Conceptually, this relatively short-term fluctuation in quality of care due to spousal death may still harm the health and survival of the surviving spouse. Empirical examination, however, suggests that this is not the case. Indeed, the mechanism of the widowhood effect may be a fundamentally biosocial one that transcends the mere access to health care.
To our knowledge, this article provides the most complete evidence regarding whether and how marriage confers a survival advantage by promoting quality of health care. However, quality of care is a multidimensional concept, and our study is limited by the number and types of quality-of-care indicators in the available data. Further studies using measures of other dimensions of quality of health care are needed to confirm and extend the findings of this study. Nevertheless, the measures we used are known to be markers of health care quality more generally and, as such, should be taken as markers. We therefore conclude that changes in quality of health care during the transition to widowhood, as we measure it, do not have discernible impact on the elevated mortality suffered by the widowed.
Acknowledgments
We thank Laurie Meneades for the expert data programming required to build the analytic data set. We thank Paul Allison, Jack Iwashyna, Kathleen Mullen, and the participants of the core seminar of the Robert Wood Johnson Scholars in Health Policy Program at Harvard University for helpful discussions and advice.
Appendix Table A1.
Odds Ratios of Occurrences of Quality-of-Care Indicators in a Given Month Within Various Time Intervals Before and After Spousal Deatha
| Hemoglobin A1c Monitoring | Diabetic Eye Examinations | Influenza Vaccination | Mammograms | Preventable Hospitalizations | Early Readmissions | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Women | Men | Women | Men | Women | |
| Months Before Spousal Death | |||||||||||
| 25–36 | 1.02 | 1.01 | 0.99 | 0.97 | 0.97*** | 0.97*** | 1.07*** | 1.15*** | 0.99 | 1.06 | 1.01 |
| 13–24 | 1.00 | 1.00 | 0.93* | 0.98 | 0.95*** | 0.96*** | 1.10*** | 1.20*** | 0.97 | 1.08 | 1.00 |
| 7–12 | 0.96 | 0.98 | 0.95 | 0.97 | 0.91*** | 0.93*** | 1.08** | 1.37*** | 1.01 | 1.08 | 1.11* |
| 3–6 | 0.95 | 0.93 | 0.88** | 0.91* | 0.89*** | 0.89*** | 1.01 | 1.49*** | 1.05 | 1.18* | 1.06 |
| 2 | 0.97 | 0.95 | 0.89 | 0.88* | 0.84*** | 0.85*** | 0.95 | 1.49*** | 1.09 | 1.45*** | 1.18* |
| 1 | 0.78** | 0.92 | 0.87 | 0.83** | 0.78*** | 0.80*** | 0.86** | 1.89*** | 1.20*** | 1.33** | 1.20* |
| 0 | 0.97 | 0.92 | 0.83* | 0.68*** | 0.68*** | 0.65*** | 0.63*** | 2.00*** | 1.49*** | 1.59*** | 1.37*** |
| Months After Spousal Death | |||||||||||
| 1 | 1.35*** | 1.15* | 1.35*** | 1.16** | 0.93** | 0.95** | 1.03 | 1.67*** | 1.25*** | 1.56*** | 1.30** |
| 2 | 1.25** | 1.27*** | 1.35*** | 1.30*** | 0.90*** | 0.89*** | 1.31*** | 1.79*** | 1.25*** | 1.52*** | 1.18** |
| 3–6 | 1.23* | 1.23*** | 1.15** | 1.17*** | 0.87*** | 0.90*** | 1.30*** | 1.61*** | 1.06 | 1.45*** | 1.30*** |
| 7–12 | 1.12** | 1.09* | 1.10* | 1.11** | 0.87*** | 0.88*** | 1.27*** | 1.61*** | 1.04 | 1.45** | 1.12* |
| 13–24 | 1.07 | 1.07 | 1.06 | 1.05 | 0.88*** | 0.88*** | 1.30*** | 1.64*** | 1.02 | 1.47*** | 1.11* |
| 25–36 | 1.06 | 1.06 | 1.06 | 0.99 | 0.90*** | 0.89*** | 1.33*** | 1.64*** | 0.92* | 1.39*** | 1.08 |
| > 36 | 1.03 | 1.11* | 1.12* | 1.04 | 0.91*** | 0.89*** | 1.40*** | 1.89*** | 0.92* | 1.41*** | 1.03 |
| Likelihood Ratio χ2 Test for Gender Differencesb | 12.14 | 23.44 | 16.22 | –– | 323.8 | 49.22 | |||||
| df | 14 | 14 | 14 | 14 | 14 | ||||||
| p > χ2 | .60 | .05 | .30 | < .001 | < .001 | ||||||
Estimates are generated by conditional logit models; all models control for time, age, and indicators of health status.
Likelihood ratio chi-square test for the overall significance of the interaction terms between gender and the series of dichotomized variables representing various time intervals before and after spousal death.
p < .05;
p < .01;
p < .001 (two-tailed tests)
Appendix Table B1.
Odds Ratios of Death in a Given Month Associated With Being “Up-to-Date” on Receiving Specific Preventive Services
| Preventive Service | Men | Women |
|---|---|---|
| Hemoglobin A1c Monitoring | 0.753 | 0.731 |
| Diabetic Eye Examinations | 0.650 | 0.615 |
| Influenza Vaccination | 0.698 | 0.736 |
| Mammograms | –– | 0.722 |
Notes: Estimates are generated in case-time-control models (fixed-effect models for nonrepeatable events). All models control for time trend, age, and indicators of time-varying health status. All estimated odds ratios are statistically significant at p < .001 (two-tailed tests).
Footnotes
Support for this research was provided by a grant to Nicholas A. Christakis from NIH (R-01 AG17548-01). Lei Jin was supported by the Robert Wood Johnson Scholars in Health Policy Program.
Entry into marriage has been shown to deter crime (Laub, Nagin, and Sampson 1998). Research in this vein illustrates the effects of micro-level social networks on individuals’ interactions with macro-social institutions. However, aside from research on the criminal justice system, little has been done to examine how marriage affects individuals’ interactions with other formal institutions. In addition, not much is know about the effects of spousal loss.
A hemoglobin A1c test is a lab test that measures the average amount of sugar (also called glucose) that has been in a person’s blood over the previous two to three months.
The Charlson index is a weighted sum of 17 conditions that have been shown to be predictive of mortality (Charlson et al. 1987).
Because the quality indicators are applicable to specific populations, for the person-months in which individuals are not eligible for a certain quality indicator, the quality indicator was set as 0. For the person-months in which individuals are eligible, the quality indicator was set as 0 if the individual obtained a particular preventive service in the year prior to a given month; otherwise it was set as 1.
Measures of obtaining preventive services may also be affected by health status. As a sensitivity analysis, we examined the mediating effects of quality-of-care indicators on the widowhood effect on mortality with and without controlling for time-varying indicators of health status. Controlling for indicators of health status does not affect the mediating effect of the quality-of-care indicators.
The monthly rate of influenza vaccination is higher than other preventive services because we considered only the flu season, between October and February each year, in our analysis. The occurrence of influenza vaccination is typically concentrated in these months.
The likelihood ratio chi-square tests for the gender difference in trajectories of changes in hemoglobin A1c testing and influenza vaccination are not statistically significant (p = .60 and p = .30, respectively; two-tailed test). The test for the gender difference in diabetic eye examinations approaches statistical significance (p = .053; two-tailed tests). However, given that we worked with very large samples, it is likely that we would have found statistical significance even when the magnitudes of the differences were quite small (as shown in Figure 1 and Appendix A). These tests for statistical significance should therefore be interpreted with caution. Despite the relatively small p value from the likelihood ratio chi-square test for the gender difference in diabetic eye exams, the findings suggest that the transition to widowhood had similar effects on the likelihood of obtaining these preventive services for elderly men and women.
The widowed in general were more likely to survive until the end of the follow-up period than the non-widowed because, by definition, the widowed had to survive their spouses. Conditional on survival to a certain time point, however, the hazard of subsequent death is in fact higher for the widowed than the nonwidowed.
It has been suggested that men between the ages of 65 and 74 should have annual prostate cancer screenings. However, this suggestion has been highly controversial (Barry 2001). We therefore did not use this measure as a quality-of-care indicator in the article, but used it only to corroborate the findings regarding mammograms.
To test this explanation indirectly, we separated a group of diabetes patients whose spouses also suffered from diabetes and compared the widowhood effects on the practices of diabetic monitoring for this group and for diabetes patients whose spouses were free of diabetes. The rates of diabetic monitoring practices were higher for the diabetic couples at the baseline, but the trajectories of change during the transition to widowhood for the two groups paralleled each other (results not shown here). Perhaps the diabetic couples were able to help each other obtain appropriate services and were able to retain that advantage after becoming widowed; or perhaps the higher rates of diabetic monitoring among the diabetic couples are due to unobserved differences between the two groups. These findings do not offer evidence to support our speculation for the post-widowhood decline of rates of influenza vaccinations.
Contributor Information
LEI JIN, RM 431, Sino Building, Department of Sociology, Chung Chi College Campus, The Chinese University of Hong Kong, Shatin, Hong Kong SAR, China; e-mail:ljin@cuhk.edu.hk..
NICHOLAS A. CHRISATAKIS, Departments of Sociology and Health Care Policy, Harvard University.
REFERENCES
- Agency for Healthcare Research and Quality 2003“Monitoring the Healthcare Safety Net: Preventable/Avoidable Hospitalizations (Ambulatory Care Sensitive Conditions)”Agency for Healthcare Research and Quality, Washington, DC. Available online at http://www.ahrq.gov/data/safetynet/billappb.htm
- Allison PD, Christakis NA. “Fixed-Effects Methods for the Analysis of Nonrepeated Events”. Sociological Methodology. 2006;36:155–72. [Google Scholar]
- Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. “The Association Between the Quality of Inpatient Care and Early Readmission: A Meta-analysis of the Evidence”. Medical Care. 1997;35:1044–59. doi: 10.1097/00005650-199710000-00006. [DOI] [PubMed] [Google Scholar]
- Barry MJ. “Prostate-Specific Antigen Testing for Early Diagnosis of Prostate Cancer”. New England Journal of Medicine. 2001;344:1373–77. doi: 10.1056/NEJM200105033441806. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Syme SL. “Social Networks, Host Resistance, and Mortality: A Nine-Year Follow-up Study of Alameda County Residents”. American Journal of Epidemiology. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Bernard LL, Guarnaccia CA. “Two Models of Caregiver Strain and Bereavement Adjustment: A Comparison of Husband and Daughter Caregivers of Breast Cancer Hospice Patients”. The Gerontologist. 2003;43:808–16. doi: 10.1093/geront/43.6.808. [DOI] [PubMed] [Google Scholar]
- Billings J, Anderson GM, Newman LS. “Recent Findings on Preventable Hospitalizations”. Health Affairs. 1996;15:239–49. doi: 10.1377/hlthaff.15.3.239. [DOI] [PubMed] [Google Scholar]
- Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, Billings J, Stewart A. “Preventable Hospitalizations and Access to Health Care”. Journal of American Medical Association. 1995;274:304–11. [PubMed] [Google Scholar]
- Blustein J, Hanson K, Shea S. “Preventable Hospitalizations and Socioeconomic Status”. Health Affairs. 1998;17:177–89. doi: 10.1377/hlthaff.17.2.177. [DOI] [PubMed] [Google Scholar]
- Bos Van Den GAM. “The Burden of Chronic Diseases in Terms of Disability, Use of Health Care and Healthy Life Expectancies”. European Journal of Public Health. 1995;5:29–34. [Google Scholar]
- Brook RH, McGlynn EA, Cleary PD. “Measuring Quality of Care—Part Two of Six”. New England Journal of Medicine. 1996;335:966–70. doi: 10.1056/NEJM199609263351311. [DOI] [PubMed] [Google Scholar]
- Brown SL, House JS, Smith DM. “Interpersonal and Spiritual Connections Among Bereaved Older Adults.”. In: Carr DS, Nesse RM, Wortman CB, editors. Spousal Bereavement in Late Life. New York: Springer Publishing Company; 2006. pp. 143–66. [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. “A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation”. Journal of Chronic Diseases. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Chin MH, Goldman L. “Correlates of Early Hospital Readmission or Death in Patients With Congestive Heart Failure”. American Journal of Cardiology. 1997;79:1640–44. doi: 10.1016/s0002-9149(97)00214-2. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Allison PD. “Mortality After the Hospitalization of a Spouse”. New England Journal of Medicine. 2006;354:719–30. doi: 10.1056/NEJMsa050196. [DOI] [PubMed] [Google Scholar]
- Christakis NA, Iwashyna TJ. “The Health Impact of Health Care on Families: A Matched Cohort Study of Hospice Use by Decedents and Mortality Outcomes in Surviving, Widowed Spouses”. Social Science & Medicine. 2003;57:465–75. doi: 10.1016/s0277-9536(02)00370-2. [DOI] [PubMed] [Google Scholar]
- Clogg CC, Petkova E, Haritou A. “Statistical Methods for Comparing Regression Coefficients Between Models”. American Journal of Sociology. 1995;100:1261–93. [Google Scholar]
- Cutler DM. Your Money or Your Life: Strong Medicine for America’s Health Care System. New York: Oxford University Press; 2004. [Google Scholar]
- di Leonardo M. “The Female World of Cards and Holidays: Women, Family, and the Work of Kinship”. Signs. 1987;12:440–53. [Google Scholar]
- Dunkin J, Anderson-Hanley C. “Dementia Caregiver Burden: A Review of the Literature and Guidelines for Assessment and Intervention”. Neurology. 1998;51(Suppl):S53–S60. doi: 10.1212/wnl.51.1_suppl_1.s53. [DOI] [PubMed] [Google Scholar]
- Elwert F, Christakis NA. “Widowhood and Race”. American Sociological Review. 2006;71:16–41. [Google Scholar]
- Goodwin JS, Hunt WC, Key CR, Samet JM. “The Effect of Marital Status on Stage, Treatment, and Survival of Cancer Patients”. Journal of the American Medical Association. 1987;258:3125–130. [PubMed] [Google Scholar]
- Gove WR. “Sex, Marital Status, and Mortality”. American Journal of Sociology. 1973;79:45–67. doi: 10.1086/225505. [DOI] [PubMed] [Google Scholar]
- Gupta S. “The Effects of Transitions in Marital Status on Men’s Performance of Housework”. Journal of Marriage and the Family. 1999;61:700–11. [Google Scholar]
- Ha J-H. “Changes in Support From Confidants, Children, and Friends Following Widowhood”. Journal of Marriage and Family. 2008;70:306–18. [Google Scholar]
- Hagestad GO.1986“The Aging Society as a Context for Family Life” Daedalus 115119–39.11611945 [Google Scholar]
- Harrison J. “Warning: The Male Sex Role May Be Dangerous to Your Health”. Journal of Social Issues. 1978;34:65–86. [Google Scholar]
- Hatch LR. Beyond Gender Differences: Adaptations to Aging in Life Course Perspective. Amityville, NY: Baywood; 2000. [Google Scholar]
- Helsing KJ, Szklo M. “Mortality After Bereavement”. American Journal of Epidemiology. 1981;114:41–52. doi: 10.1093/oxfordjournals.aje.a113172. [DOI] [PubMed] [Google Scholar]
- Holloway JJ, Medendorp SV, Bromberg J.1990“Risk Factors for Early Readmission Among Veterans” Health Services Research 25(1, Pt. 2):213–37. [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. “Social Relationships and Health”. Science. 1988;241:540–45. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hoyert DL, Kung H-C, Smith BL. National Vital Statistics Reports. No. 15. Vol. 53. Hyattsville, MD: National Center for Health Statistics; 2005. “Deaths: Preliminary Data for 2003.”. [PubMed] [Google Scholar]
- Hu Y, Goldman N. “Mortality Differentials by Marital Status: An International Comparison”. Demography. 1990;27:233–50. [PubMed] [Google Scholar]
- Irwin M, Pike J. “Bereavement, Depressive Symptoms, and Immune Function.”. In: Stroebe MS, Stroebe W, Hansson RO, editors. Handbook of Bereavement: Theory, Research, and Intervention. New York: Cambridge University Press; 1993. pp. 160–74. [Google Scholar]
- Iwashyna TJ, Brennan G, Zhang JX, Christakis NA. “Finding Married Couples in Medicare Claims Data”. Health Services and Outcomes Research Methodology. 2002;3:75–86. [Google Scholar]
- Iwashyna TJ, Christakis NA. “Marriage, Widowhood, and Health Care Use”. Social & Science Medicine. 2003;57:2137–47. doi: 10.1016/s0277-9536(02)00546-4. [DOI] [PubMed] [Google Scholar]
- Iwashyna TJ, Zhang JX, Lauderdale D, Christakis NA. “A Methodology for Identifying Married Couples in Medicare Data: Mortality, Morbidity, and Health Care Use Among the Married Elderly”. Demography. 1998;35:413–19. [PubMed] [Google Scholar]
- Kim K, Jacobs S. “Neuroendocrin Changes Following Bereavement.”. In: Stroebe MS, Stroebe W, Hansson RO, editors. Handbook of Bereavement: Theory, Research, and Intervention. New York: Cambridge University Press; 1993. pp. 143–59. [Google Scholar]
- Lannin DR, Mathews HF, Mitchell J, Swanson MS, Swanson FH, Edwards MS. “Influence of Socioeconomic and Cultural Factors on Racial Differences in Late-Stage Presentation of Breast Cancer”. Journal of the American Medical Association. 1998;279:1801–807. doi: 10.1001/jama.279.22.1801. [DOI] [PubMed] [Google Scholar]
- Laub JH, Nagin DS, Sampson RJ. “Trajectories of Change in Criminal Offending: Good Marriages and the Desistance Process”. American Sociological Review. 1998;63:225–38. [Google Scholar]
- Lillard LA, Panis C. “Marital Status and Mortality: The Role of Health”. Demography. 1996;33:313–27. [PubMed] [Google Scholar]
- Lillard LA, Waite LJ. “‘Til Death Do Us Part: Marital Disruption and Mortality”. American Journal of Sociology. 1995;100:1131–56. [Google Scholar]
- Litwak E. Helping the Elderly: The Contemporary Roles of Informal and Formal Systems. New York: Guilford Press; 1985. [Google Scholar]
- Litwak E, Messeri P. “Organizational Theory, Social Support, and Mortality Rates: A Theoretical Convergence”. American Sociological Review. 1989;54:49–66. [Google Scholar]
- Lopata HZ. Current Widowhood: Myths and Realities. Thousand Oaks, CA: Sage Publications; 1996. [Google Scholar]
- Mark TL, Paramore LC. “Pneumococcal Pneumonia and Influenza Vaccination: Access to and Use by Hispanic Medicare Beneficiaries”. American Journal of Public Health. 1996;86:1545–50. doi: 10.2105/ajph.86.11.1545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martikainen P, Valkonen T. “Mortality After the Death of a Spouse: Rates and Causes of Death in a Large Finnish Cohort”. American Journal of Public Health. 1996;86:1087–93. doi: 10.2105/ajph.86.8_pt_1.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson M, Smith-Lovin L, Brashears ME. “Social Isolation in America: Changes in Core Discussion Networks Over Two Decades”. American Sociological Review. 2006;71:353–75. [Google Scholar]
- Mullan JT. “The Bereaved Caregiver: A Prospective Study of Changes in Well-being”. The Gerontologist. 1992;32:673–83. doi: 10.1093/geront/32.5.673. [DOI] [PubMed] [Google Scholar]
- National Committee for Quality Assurance 2006HEDIS® 2006 Summary Table of Measures and Product LinesNational Committee for Quality Assurance, Washington, DC. Available online at http://www.ncqa.org/Portals/0/HEDISQM/Archives/2006/MeasuresList.pdf
- Pham HH, Schrag D, Hargraves JL, Bach PB. “Delivery of Preventive Services to Older Adults by Primary Care Physicians”. Journal of American Medical Association. 2005;294:473–81. doi: 10.1001/jama.294.4.473. [DOI] [PubMed] [Google Scholar]
- Powers EA, Bultena GL. “Sex Differences in Intimate Friendships of Old Age”. Journal of Marriage and the Family. 1976;38:739–47. [Google Scholar]
- Prigerson HG, Maciejewski PK, Rosenheck RA. “The Effects of Marital Dissolution and Marital Quality on Health and Health Service Use Among Women”. Medical Care. 1999;37:858–73. doi: 10.1097/00005650-199909000-00003. [DOI] [PubMed] [Google Scholar]
- Prokos AH, Keene JR. “The Long-Term Effects of Spousal Care Giving on Survivors’ Well-being in Widowhood”. Social Science Quarterly. 2005;86:664–82. [Google Scholar]
- Rogers SJ, Amato PR. “Have Changes in Gender Relations Affected Marital Quality?”. Social Forces. 2000;79:731–53. [Google Scholar]
- Rowe JW. “Health Care of the Elderly”. New England Journal of Medicine. 1985;312:827–35. doi: 10.1056/NEJM198503283121305. [DOI] [PubMed] [Google Scholar]
- Schaefer C, Quesenberry CP, Wi S. “Mortality Following Conjugal Bereavement and the Effects of a Shared Environment”. American Journal of Epidemiology. 1995;141:1142–52. doi: 10.1093/oxfordjournals.aje.a117387. [DOI] [PubMed] [Google Scholar]
- Shaw W, Patterson T, Semple S. “Longitudinal Analysis of Multiple Indicators of Health Decline Among Spousal Caregivers”. Annals of Behavioral Medicine. 1997;19:101–109. doi: 10.1007/BF02883326. [DOI] [PubMed] [Google Scholar]
- Smith-Bindman R, Miglioretti DL, Lurie N, Abraham L, Barbash RB, Strzelczyk J, Dignan M, Barlow WE, Beasley CM, Kerlikowske K. “Does Utilization of Screening Mam-mography Explain Racial and Ethnic Differences in Breast Cancer?”. Annals of Internal Medicine. 2006;144:541–53. doi: 10.7326/0003-4819-144-8-200604180-00004. [DOI] [PubMed] [Google Scholar]
- Sox CM, Swartz K, Burstin HR, Brennan TA. “Insurance or a Regular Physician: Which Is the Most Powerful Predictor of Health Care”. American Journal of Public Health. 1998;88:364–70. doi: 10.2105/ajph.88.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolzenberg R. “It’s About Time and Gender: Spousal Employment and Health”. American Journal of Sociology. 2001;101:61–100. doi: 10.1086/323151. [DOI] [PubMed] [Google Scholar]
- Stroebe MS, Hansson RO, Stroebe W, Schut H, editors. Handbook of Bereavement Research: Consequences, Coping, and Care. Washington, DC: American Psychological Association; 2001. [Google Scholar]
- Stroebe MS, Stroebe W. “Who Suffers More? Sex Differences in Health Risks of the Widowed”. Psychological Bulletin. 1983;93:279–301. [PubMed] [Google Scholar]
- Stroebe W, Stroebe MS. “Determinants of Adjustment to Bereavement in Younger Widows and Widowers.”. In: Stroebe MS, Stroebe W, Hansson RO, editors. Handbook of Bereavement: Theory, Research, and Intervention. New York: Cambridge University Press; 1993. pp. 208–26. [Google Scholar]
- Thompson LW, Breckenridge JN, Gallagher D, Peterson J. “Effects of Bereavement on Self-perceptions of Physical Health in Elderly Widows and Widowers”. Journal of Gerontology. 1984;39:309–14. doi: 10.1093/geronj/39.3.309. [DOI] [PubMed] [Google Scholar]
- Umberson D. “Family Status and Health Behaviors: Social Control as a Dimension of Social Integration”. Journal of Health and Social Behavior. 1987;28:306–19. [PubMed] [Google Scholar]
- Umberson D. “Gender, Marital Status and the Social Control of Health Behavior”. Social & Science Medicine. 1992;34:907–17. doi: 10.1016/0277-9536(92)90259-s. [DOI] [PubMed] [Google Scholar]
- Utz R, Reidy EB, Carr D, Nesse R, Wortman C. “The Daily Consequences of Widowhood: The Role of Gender and Intergenerational Transfers on Subsequent Housework Performance”. Journal of Family Issues. 2004;25:683–712. [Google Scholar]
- Wade TJ, Pevalin DJ. “Marital Transitions and Mental Health”. Journal of Health and Social Behavior. 2004;45:155–70. doi: 10.1177/002214650404500203. [DOI] [PubMed] [Google Scholar]
- Waite LJ, Gallagher M. The Case for Marriage: Why Married People Are Happier, Healthier, and Better Off Financially. New York: Doubleday; 2000. [Google Scholar]
- Walter CA. The Loss of a Life Partner. New York: Columbia University Press; 2003. [Google Scholar]
- Wang C-S, Wang S-T, Lai C-T, Lin L-J, Chou P. “Impact of Influenza Vaccination on Major Cause-Specific Mortality”. Vaccine. 2007;25:1196–203. doi: 10.1016/j.vaccine.2006.10.015. [DOI] [PubMed] [Google Scholar]
- Williams K. “The Transition to Widowhood and the Social Regulation of Health: Consequences for Health and Health Risk Behavior”. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2004;59B:S343–S349. doi: 10.1093/geronb/59.6.s343. [DOI] [PubMed] [Google Scholar]
- Williams K, Umberson D. “Marital Status, Marital Transitions, and Health: A Gendered Life Course Perspective”. Journal of Health and Social Behavior. 2004;45:81–98. doi: 10.1177/002214650404500106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff JL, Starfield B, Anderson G. “Prevalence, Expenditures, and Complications of Multiple Chronic Conditions in the Elderly”. Archives of Internal Medicine. 2002;162:2269–76. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]