Abstract
In this article, we examine changes in life expectancy free of disability using longitudinal data collected from 1984 through 2000 from two cohorts who composed the Longitudinal Studies of Aging I and II. Life expectancies with and without ADL and/or IADL disability are calculated using a Markov-based multistate life table approach. At age 70, disability-free life expectancy increased over a 10-year period by 0.6 of a year in the later cohort, which was the same as the increase in total life expectancy, both increases marginally statistically significant. The average length of expected life with IADL and ADL disability did not change. Changes in disability-free life expectancy resulted from decreases in disability incidence and increases in the incidence of recovery from disability across the two survey cohorts. Age-specific mortality among the ADL disabled declined significantly in the later cohort after age 80. Mortality for the IADL disabled and the nondisabled did not change significantly. Those with ADL disability at age 70 experienced substantial increases in both total life expectancy and disability-free life expectancy. These results indicate the importance of efforts both to prevent and delay disability and to promote recovery from disability for increasing life expectancy without disability. Results also indicate that while reductions in incidence and increases in recovery work to decrease population prevalence of disability, declining mortality among the disabled has been a force toward increasing disability prevalence.
Studies from recent years have provided evidence of a decline in the prevalence of disability among the older population over more than two decades (Freedman, Crimmins, et al. 2004; Manton, Gu, and Lamb 2006). First, less severe disability declined beginning in the 1980s, and then more severe disability declined beginning in the 1990s (Crimmins 2004; Freedman, Crimmins, et al. 2004).
Most of our knowledge about trends in disability is based on changes in the prevalence of disability. However, the prevalence of disability is the outcome of several dynamic processes, including disability onset and recovery as well as mortality (Crimmins, Hayward, and Saito 1994; Hayward, Crimmins, and Saito 1998). Understanding the dynamic forces affecting the prevalence of disability is important in interpreting prevalence changes and projecting the likelihood of continued change. One cannot conclude from reductions in the prevalence of disability in old age whether disability has been postponed through decreases in incidence, through increases in recovery, or through changes in the mortality of the disabled or nondisabled (Leveille et al. 2000; Melzer et al. 2001). Changes in any or all of these dynamic forces could be the explanation.
Although we have less information on changes in incidence and recovery, several studies have reported reductions in the onset of disability or movement to more severe disability over the 1980s to the early 2000s (Cai and Lubitz 2007; Crimmins, Saito, and Reynolds 1997; Manton, Corder, and Stallard 1993; Wolf, Mendes de Leon, and Glass 2007). Three of these studies are based on nationally representative data sets, the Longitudinal Study of Aging (Crimmins, Saito, and Reynolds 1997), the Medicare Current Beneficiary Survey (Cai and Lubitz 2007), and the National Long Term Care Survey (NLTCS; Manton et al. 1993); the fourth is based on the New Haven Populations for Epidemiologic Studies of the Elderly (Wolf et al. 2007). These studies, however, provide conflicting information on change in age-specific recovery rates. The Crimmins et al. study reported some improvement in disability recovery rates from 1984–1986 to 1988–1990; the Cai and Lubitz study also reported an increase in recovery from disability from 1992 to 2002; the Manton et al. study reported that all recovery rates were lower in the 1984–1989 period than the 1982–1984 period; and Wolf et al. found decreases in recovery among older persons in New Haven from 1982 to 1994.
Trends in disability prevalence as well as the length of time lived with disability will be affected by each of these processes as well as mortality trends among the disabled and the nondisabled. The prevalence of disability can increase if survival of the disabled increases, even though the likelihood of becoming disabled stays the same (Hayward et al. 1998). In recent decades, mortality in the United States has been declining among the old, but not at a steady pace. Decline was very rapid from 1968 up to 1980, with a slowing in the early 1980s and a resumption of faster decline in the 1990s (Crimmins 2004; White 2002). We do not have evidence on the trends in mortality among the disabled and the nondisabled.
While it is important to link these processes to the observed prevalence of disability in the population, it is difficult to know how all of these trends interact to affect the average lifetime experience with disability for older persons or how many years an older person lives with disability. Life-cycle changes, rather than population changes, may be important for individual planning. For instance, it is possible to have declines in disability onset but increases in life expectancy among the disabled that would lead to longer lives with disability even in the face of reductions in age-specific incidence of disability.
This article provides an assessment of changes in disabled and nondisabled life expectancy from experiences covering the period from 1984 through 2000 for the population 70 years of age and older in the United States. It provides a unique assessment of changes in healthy life expectancy based on repeated longitudinal surveys of the older population that cover more than a decade. We examine not only change in the length of disabled and nondisabled life expectancy but also change in the age-specific rates of onset and recovery from disability, as well as change in death rates for the disabled and nondisabled segments of the population. In addition, we examine the implications of these changes for the future disability status of the older U.S. population. This article extends current knowledge about disability by indicating the source of observed changes in prevalence of disability, clarifying the effect of mortality and disability processes on the average life course of older persons, and estimating the effect of continuation of current rates on future disability prevalence.
DISABILITY
Verbrugge and Jette (1994) are credited with clarifying the placement of disability in the process of health change that they termed the disablement process. Disability is an inability to perform expected social roles within a given environment (Freedman 2006; Verbrugge 1989). For populations, disability is downstream of the onset of diseases and functioning loss; in contrast to other dimensions of health, such as disease and functioning loss, which are characteristics of individuals, disability is affected by factors operating both internally and externally to individuals. Change in disability can reflect change in innate ability of individuals or change in the challenges to performance presented by the environment to those individuals. The level of disability is thus affected by the social roles used to define disability and the environment in which it is measured.
For older people, disability has often been viewed as ability to perform activities needed for independent living and personal care and has been operationalized as ability to perform activities of daily living (ADLs) and instrumental activities of daily living (IADLs; Bandeen-Roche et al. 2006; Freedman, Aykan, et al. 2004; Manton et al. 2006; Schoeni et al. 2005). These disability indicators have been used not only in research on trends in the older population but in determining eligibility for participation in publicly funded health care programs (Centers for Medicare and Medicaid Services 2005; U.S. Department of Health and Human Services 2000).
DISABILITY-FREE LIFE EXPECTANCY
With increasing emphasis on improving quality as well as quantity of life, both length of nondisabled life and total life expectancy have become useful indicators of population well-being. Based on estimates from cross-sectional approaches, disability-free life expectancy appears to have been increasing in the United States since the 1980s (Crimmins and Saito 2001; Crimmins, Saito, and Ingeneri 1997), as well as in France (Robine, Mormiche, and Sermet 1998), while England has experienced longer life with less severe disability (Bone et al. 1995).
The reliance on cross-sectional data and methods provides a picture of life cycle implications of the current structure of disability in the population but does little to clarify how this status came about. Because the prevalence of disability used in these analyses reflects all disability events occurring throughout the lifetime of the subjects, life expectancy changes based on cross-sectional data can reflect events that happened decades ago (Laditka and Hayward 2003). Another constraint of the application of this method is that mortality is usually assumed to be invariant by disability status, which could potentially lead to biased estimates of disabled and nondisabled life expectancy if mortality actually differs markedly by disability state. A further limitation is that this approach cannot show the consequences of current conditions for future disability prevalence (Laditka and Hayward 2003).
In contrast, the multistate life table approach used in this study allows for the possibility that individuals may traverse back and forth between disability states, and that mortality might vary according to disability status. Recent changes in disability and the occurrence of mortality are captured using longitudinal data to estimate incidence rates, which are the inputs to multistate life tables. The multistate life table modeling approach provides a wealth of summary information, such as the length of disabled life, the ways in which the transition rates determine disabled life expectancy, and the future structure of population disability (e.g., age-specific prevalence) if current transition rates of disability onset and recovery continue indefinitely (Jagger et al. 2003; Laditka and Laditka 2006; Manton and Land 2000; Minicuci et al. 2004; Reynolds, Saito, and Crimmins 2005). Thus, a multistate life table approach is conceptually preferable to the traditional prevalence-based approach, and it offers methodological advantages that increase understanding of the forces responsible for changes in the prevalence of disability. The longitudinal data from multiple cohorts necessary to examine historical changes in the process underlying disability-free life expectancy have only recently become available. Recent estimates of change in disabled life expectancy based on longitudinal data and life table methods suitable for such data have reinforced the findings of cross-sectional studies with findings that disability-free life has been increasing along with total life expectancy; they also indicate that some types of disabled life have decreased (Cai and Lubitz 2007; Manton, Gu, and Lowrimore 2008). These studies have not, however, fully described the change in the processes causing changes in life expectancy.
MEASURES, DATA AND METHODS
Measures
Disabled life in this older population can be viewed as the inability, because of a health or physical problem, to do at least one of the tasks required for either self-care or independent living (Spector and Fleishman 1998). In this analysis, we define two disability states. Inability to perform one of the five activities of daily living (ADLs) is inability to perform self-care: bathing, dressing, eating, getting in/out of a bed or chair, and toileting. Inability to do one of the five instrumental activities of daily living (IADLs: preparing meals, shopping for groceries, managing money, using the telephone, and doing light housework) is inability to live independently. Such definitions of disability are commonly used with the older population (Lynch, Brown, and Harmsen 2003; Wu, Leu, and Li 1999). We choose to define disability using “inability” to do a task rather than “difficulty” in doing a task because “inability” has a clearer meaning for respondents and implications for societal needs.
Four states are used in this analysis: able to perform all ADLs and IADLs, unable to perform one or more of the ADLs, able to perform all ADLs but unable to perform one or more IADLs, and deceased. Institutionalized persons are assumed to be ADL disabled. The age-specific transition schedules that determine disabled and disability-free life expectancy are determined by changes across these states: the onset of either type of disability, recovery from disability, change of disability state, and death from either of the disabled states or the nondisabled state.
Data
Our life table models of active life expectancy are based on information from two longitudinal surveys of the U.S. community-dwelling population collected from 1984 through 2000. The Longitudinal Study of Aging (LSOA I) began in 1984 with interviews of 7,527 respondents who formed a representative sample of the noninstitutionalized population aged 70 and older. Most respondents were reinterviewed three times: 1986, 1988, and 1990. The Second Longitudinal Study of Aging II (LSOA II), which was designed to replicate LSOA I, began in 1994, with 9,447 respondents who were reinterviewed twice: in 1996–1997 and 1999–2000.1 The periods covered by these surveys thus center 10 years apart: 1987 and 1997. We assume that the results represent change in synthetic cohorts over a 10-year period. Sample weights are used in all analyses.
Both LSOA surveys were supplements to the annual National Health Interview Survey (NHIS): LSOA I in 1984 and LSOA II in 1994. Questions in the two surveys are identical because they were designed to be used to evaluate change in disability over time. There were some differences in survey procedures between the two surveys that need to be considered in evaluating time trends. For instance, the first interview of LSOA II was done between 7 and 17 months after the main survey, rather than at the time of the main survey as in LSOA I. As a result, the response rate at the initial wave was somewhat lower in the second cohort (87.4% versus 93.2%; National Center for Health Statistics [NCHS] 2002). Although similar questions on disability were asked in the two surveys, there were more follow-up questions in the somewhat longer interviews of the second cohort. There were also some survey design changes between the two cohorts: an oversample of blacks in LSOA II and a change in the number of primary sampling units used (NCHS 2002). These design changes and differential response rates at the first interview are reflected in the weights used for analysis, so we believe that the surveys can be compared to indicate change over time. An additional difference between the two surveys is that respondents of LSOA I were followed through the National Death Index (NDI), so the exact dates of death have been recorded and made publicly available. NDI records were not available in a public-use file for LSOA II, so they cannot be used with the estimation program used here. However, respondents in LSOA II were followed with a survivors’ survey to record information about death.
Not all respondents in LSOA I were eligible for all interviews. Of the 7,527 respondents in the first wave of LSOA I, 7,496 were included in the analysis; however, because of budgetary constraints, not all subjects were eligible for the 1986 interview (N = 5,151), but ineligible subjects were included in the later interviews. For LSOA II, this analysis is based on a sample of 9,409 respondents, since 38 cases were eliminated because they had missing information on all ADL and IADL questions in the first interview.
In the LSOA I data set, sample attrition was 11.2% by the end of the four waves. In the LSOA II data set, attrition was higher by the third wave (16.9%). For every observation, disability status is known at Wave 1; for the 1984 sample, we have the results of the NDI search to provide information on vital status at the end of the interview period; for the 1994 sample, we have information on vital status from exit interviews with survivors for those who die. If people are interviewed only once and no other status is known, they will not be included in the estimates without imputation. We cannot ignore attrition because those who are lost are likely to differ from those who are interviewed. Missing data for cases known alive, but not interviewed, were assigned values for disability status based on the proportion of the sample with the same observed health state patterns for known waves. If vital status was not known, death was also considered as a possible alternative state and assignment was based on observed health states, including mortality.
We impute a health state for those who have a “terminal” missing value because missing values are not likely to be random but rather represent the selectivity of attrition. Attrition is likely to have an important effect on estimates of life expectancy. When a case ends in a missing value—which can mean that a person was missing at all interviews (and is not known to be deceased) after the first interview or only at the last interview—we impute a state based on observed data with similar prior disability patterns. We do not impute data for cases in which the information is missing for an “internal interview” or an interview between two known states. The imputations are performed for 877 people in the 1984 cohort and 1,642 in the 1994 cohort (of whom 53 are imputed to death). For 1984, the results with no imputations are similar to those with imputations (no differences great than 0.1 years); but for the 1994 cohort, there is a difference. We imputed 53 deaths in the 1994 cohort because we did not know about the vital status of all respondents at the last interview. If we did not impute, the values of each life expectancy state would be lower in the 1994 cohort: disability-free would be 0.5 lower, IADL disabled would be 0.2 lower, and ADL disabled would be 0.3 lower, leading to a lower total of .9.2
Because we rely on an interpolated Markov chain approach to estimate the multistate life table models, we are able to take advantage of the approach’s capabilities of handling observation intervals of unequal length and missing data. Where date of death was not known, we assumed that death occurred at the midpoint of the interval.
Both the LSOA I and the LSOA II samples originally omitted the institutional population but followed participants after baseline into institutions. At the last interview of the 1984 cohort in 1990, 6.8% of those for whom interview information was supplied lived in institutions; in 2000, the figure was 5.5%. In our analyses, all institutionalized persons are assumed to be ADL disabled. Our estimates reflect the change in life expectancy for the initially community-dwelling cohorts. Over the period, there was a small drop in the percentage of the older population in institutions (Manton et al. 2006).
Table 1 provides the distribution of the almost 16,000 intervals of observation used in each of the studies by status at the beginning and end of the intervals. Most intervals at both times began and ended disability-free. By the date of the last scheduled interview, more than 2,400 LSOA I respondents had died; this was true for about 2,300 respondents in LSOA II. While we show these intervals to provide a rough indication of the amount of state change in the two surveys, a more accurate assessment of change is provided by our multistate life table results.
Table 1.
Distribution of Observations by State at Beginning and End of Intervals
| States at Beginning and End | LSOA I |
LSOA II |
||
|---|---|---|---|---|
| N | % | N | % | |
| Disability-Free at Both Interviews | 9,856 | 62.8 | 9,727 | 65.8 |
| Disability-Free to IADL Disabled | 865 | 5.5 | 738 | 5.0 |
| Disability-Free to ADL Disabled | 710 | 4.5 | 572 | 3.9 |
| Recovered From IADL Disability | 266 | 1.7 | 283 | 1.9 |
| Recovered From ADL Disability | 99 | 0.6 | 113 | 0.8 |
| Remained IADL Disabled | 479 | 3.1 | 279 | 1.9 |
| Remained ADL Disabled | 501 | 3.2 | 406 | 2.7 |
| From IADL Disabled to ADL Disabled | 346 | 2.2 | 233 | 1.6 |
| From ADL Disabled to IADL Disabled | 121 | 0.8 | 102 | 0.7 |
| Died From Disability-Free State | 1,457 | 9.3 | 1,481 | 10.0 |
| Died From IADL Disabled | 403 | 2.6 | 354 | 2.4 |
| Died From ADL Disabled | 579 | 3.7 | 490 | 3.3 |
| Total | 15,682 | 100.0 | 14,778 | 100.0 |
Methods
We employ the interpolated Markov chain approach (IMaCh) developed by Brouard and Liévre, following work by Laditka and Wolf (1998), to estimate the transition probabilities and the expectancies implied by the transition probabilities. Given data on a sequence of health states at various time points, as in this study, IMaCh estimates the likelihood of what was observed in terms of the higher probabilities of the embedded Markov chain (Liévre, Brouard, and Heathcote 2003:212). The inputs to the IMaCh model are state-space indicators, and the outputs are a “model” of transition probabilities, hpxij, indicating the likelihood of changing health states over a time period h at age x, which are the “inputs” to the active-life expectancy calculation. The four states are able (coded 1), ADL disabled (coded 2), IADL disabled (coded 3), and deceased (coded 4). The transition probabilities are estimated based on a series of 4 × 4 matrices:
The top row of the matrix represents transitions for individuals who begin the interval nondisabled; the second row represents transitions for individuals who begin the interval ADL disabled; the third row represents individuals who begin the interval IADL disabled; and the final row represents death, the absorbing state. The transition probabilities are then parameterized using a multinomial logit implying that the dependence on age x is log-linear with a time interval h:
Because a maximum likelihood estimation approach is used to estimate the transition probabilities, the method provides standard errors for the model parameters, which are then used to derive standard errors for the life expectancies derived from the transition probabilities (Liévre et al. 2003).
IMaCh is based on a logistic regression model that assumes that all changes in disability state occur at the end of the interval, which results in different estimates of life expectancy from programs that assume central rates (Crimmins et al. 1994). IMaCh’s ability to provide standard errors for the expectancies is an important improvement over recent hazard-based approaches to estimate multistate life tables (Hayward and Grady 1990; Land, Guralnik, and Blazer 1994). The standard errors allow the assessment of whether group differences in expectancies are statistically meaningful. Note that the life expectancies are a summary of interacting processes, which makes it difficult to draw inferences from the statistical tests of the individual parameters making up the interacting processes.3 We should note that we are unable to correct our estimates of the standard errors for the complex sample designs used in the LSOA surveys.4 Other advantages of the IMaCh approach include, as noted above, that it is flexible in handling survey intervals that differ in length; it can incorporate cases that have missing data; and it theoretically allows for multiple transitions in an interval (Jagger et al. 2003). The approach also provides estimates of the health distribution in the life table population implied by the transition rates. We use IMaCh with a time between events of 24 months, which means that the interval on which transition rates are calculated closely matches the interval observed in the data.5
RESULTS
Changes in Transition Rates
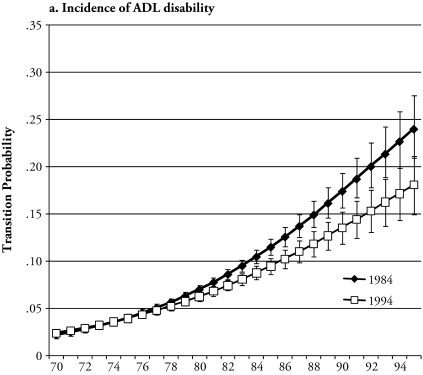
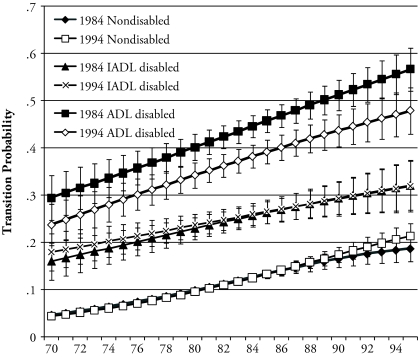
We begin our results by examining changes over time in the age-specific onset of each type of disability and the change from IADL to ADL disability (Figure 1). First, the age pattern indicates, not surprisingly, that at both dates, older persons are more likely than younger persons to become disabled and to move to the state of greater disability. The probability of ADL disability onset is significantly lower in the 1994 cohort than in 1984 cohort at the older end of the age range. The onset rates of IADL disability and of ADL disability among the IADL impaired are also somewhat lower at the older ages, but the differences are not significant. This outward shift of the onset curve represents some delay in the onset of disability in the more recent cohort.
Figure 1.
Probability of Becoming Disabled by Age: LSOA I and LSOA II
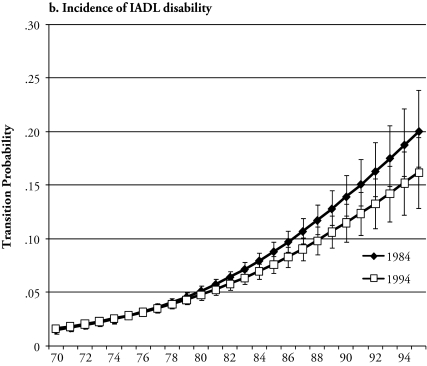
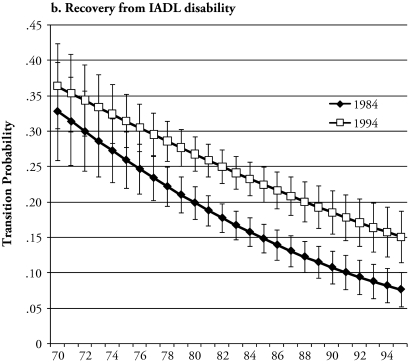
The rates of recovering from disability—that is, changing to nondisabled from a disabled state or of becoming less disabled by moving from ADL to IADL disability—are shown in Figure 2 for the two samples. Here, not surprisingly, the age pattern is negative and opposite to the previous one; older persons are less likely to recover. There is a greater likelihood of recovery at many ages from both types of disability in the 1994 cohort than in the 1984 cohort. The rates of changing from ADL disabled to IADL disabled do not differ in the cohorts. Thus, it appears that the probabilities of both disability onset and recovery improved somewhat over the 10-year period.
Figure 2.
Probability of Recovery From Disability by Age: LSOA I and LSOA II
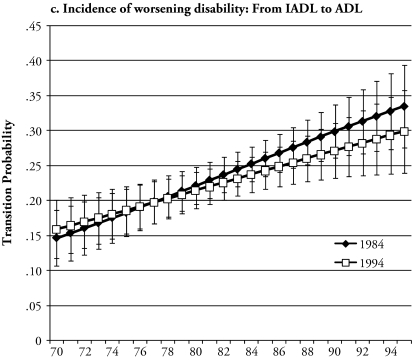
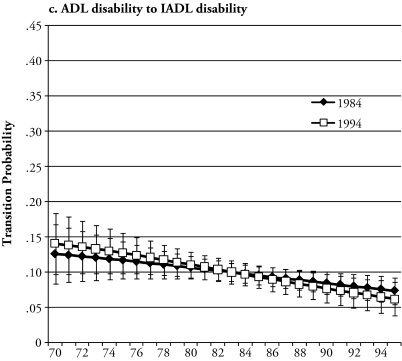
Figure 3 shows the probability of dying from the three states in the two time periods. The probability is highest from the ADL-disabled state; mortality from the IADL-disabled state is lower; and mortality in the nondisabled state is the lowest. The probability of death among the ADL disabled is significantly lower in the later cohort at older ages than in the earlier cohort (Figure 3). There is no difference in the mortality of the IADL disabled and nondisabled in the two cohorts.
Figure 3.
Death Rates by Age for the ADL and IADL Disabled and the Nondisabled
Life Expectancy
Total life expectancy, disability-free life expectancy, and disabled life expectancy implied by the age-specific transition rates are shown in Table 2. Calculations of total life expectancy made using the survey data are very close to those published by the National Center for Health Statistics (NCHS). Life expectancy at age 70 from the vital statistics for the U.S. population in 1987 (the midpoint of the LSOA I data collection) is 13.6 years (NCHS 1990), and the total life expectancy in the LSOA I from the multistate life table is 13.7 years. Life expectancy at age 70 for the U.S. population in 1997 (the midpoint of the LSOA II data collection) is 14.3 years (Anderson 1999), which is the same as that in the multistate life table for the 1994 cohort.
Table 2.
Total, Disability-Free, and Disabled Life Expectancy by Age (with confidence intervals): LSOA I and LSOA II
| Age | Total Life Expectancy |
Disability-Free Life Expectancy |
IADL-Disabled Life Expectancy |
ADL-Disabled Life Expectancy |
||||
|---|---|---|---|---|---|---|---|---|
| 1984 | 1994 | 1984 | 1994 | 1984 | 1994 | 1984 | 1994 | |
| 70 | 13.69 | 14.30 | 10.92 | 11.55 | 1.32 | 1.22 | 1.45 | 1.54 |
| Confidence Interval | 13.37–14.00 | 13.98–14.63 | 10.64–11.19 | 11.26–11.83 | 1.23–1.42 | 1.13–1.31 | 1.35–1.55 | 1.42–1.65 |
| 80 | 8.18 | 8.78 | 5.19 | 5.88 | 1.36 | 1.19 | 1.63 | 1.71 |
| Confidence Interval | 7.92–8.44 | 8.49–9.08 | 5.00–5.38 | 5.66–6.09 | 1.26–1.47 | 1.09–1.29 | 1.51–1.75 | 1.56–1.87 |
| 90 | 4.75 | 5.32 | 1.71 | 2.30 | 1.23 | 1.06 | 1.81 | 1.96 |
| Confidence Interval | 4.47–5.04 | 4.97–5.67 | 1.51–1.91 | 2.07–2.53 | 1.07–1.40 | 0.90–1.22 | 1.60–2.02 | 1.68–2.24 |
In the 1994 cohort, at age 70, the total life expectancy of 14.30 is divided as follows: nondisabled life expectancy was 11.55 years and total disabled life expectancy was 2.76 years, with 1.22 years spent with IADL disability and 1.54 years spent with ADL disability. In the 1984 cohort, these values are 13.69, 10.92, and 2.77, of which 1.32 is IADL impaired and 1.45 is ADL impaired.6 Both total and disability-free life expectancy at age 70 were somewhat longer in the later cohort, but only the difference in disability-free life is significant at age 70. At age 80, both increase significantly in the later cohort (total from 8.18 to 8.78 and disability-free from 5.19 to 5.88). There is no significant change over the 10-year period in life expectancy with ADL disability or IADL disability. More of the disabled life expectancy at every age is ADL disability than IADL disability (52% in 1984 and 56% in 1994 at age 70). The length of IADL life expectancy is similar both over time and across ages, with some decrease at the older ages. ADL disability, although similar over time, increases with age.
The proportion of expected life free of disability stayed roughly constant between the two dates at age 70, going from 80% to 81%. Disability-free life increased proportionally at the older ages, from 63% to 67% at age 80 and from 36% to 43% at age 90.
As noted above, these two cohorts originally represented only the community-dwelling population at the first wave, but in later waves, people were interviewed in institutions. If we weight our sample observed in institutions at Wave 2 to reflect the age-specific proportions observed institutionalized in the NLTCS, it becomes evident how our results are likely to be affected by limiting our analysis to those initially noninstitutionalized (Manton et al. 2006). This is not a total solution: using these weights, we do not completely reflect the cohort’s institutional experience in the period, and the short-term institutionalized are better represented than the long-term institutionalized.7 However, when this is done, the conclusions about life expectancy change are essentially the same even though the levels of estimated life expectancy are somewhat changed. The level of total life expectancy is 0.1 lower for each cohort, while the level of disability-free life expectancy is 0.2 lower in 1984 and 0.3 lower in 1994, resulting in essentially the same change as in the estimates in Table 2. At the same time, there is more ADL-impaired life expectancy: 0.15 more in the 1984 cohort and 0.16 more in the 1994 cohort.
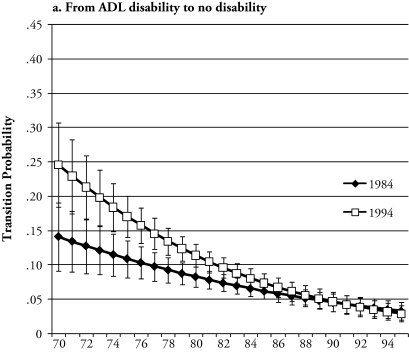
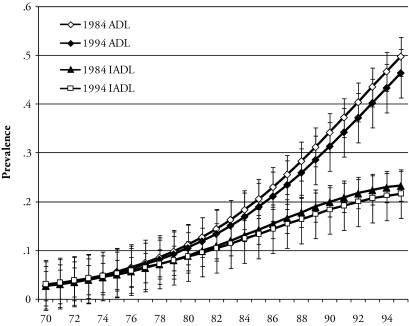
Implied Prevalence
The prevalence of ADL and IADL disability in the stationary population implied by continuing the rates of disability onset, recovery, and death is shown in Figure 4. This population disability distribution is independent of initial health state distribution or the prevalence of disability state and age structure and provides an indication of the long-term impact of the continuation of current processes. The implication of continuation of these rates is some slight—and nonsignificant—reduction in ADL disability, especially at the older ages. There is no change in IADL prevalence predicted by the differences in rates. Another way of understanding the long-term impact of continuing the rates is to examine the shift in the age at which a given level of prevalence would occur. For example, if the rates for the 1984 cohort continued, an ADL disability prevalence of 40% would occur at roughly age 92. If the rates for the 1994 cohort were continued, this prevalence would occur at age 93. Thus, the shift in the incidence rates implies a very small and nonsignificant decline in disability at advanced ages.
Figure 4.
Implied Prevalence of Disability if Rates Remain Constant
Status-Based Life Tables
To this point, we have focused on population-based life tables, which represent the expected average length of life by disability state for the entire population. However, individuals arrive at old age either disabled or not, and their disability status at a particular age can have profound implications for their overall life expectancy and life free of disability. To understand the implications of surviving to a given age with or without ADL or IADL disability for the two cohorts, we use status-based life tables to look at change in the expected lives of those who are free of ADL or IADL disability at age 70 and those with each type of disability at age 70.
As shown in Table 3, for those free of disability at age 70, life expectancy increased by 0.6 years (13.92 to 14.53) and almost all of this increase (0.63 of a year) was in disability-free life expectancy. The levels of life expectancy for the nondisabled are fairly similar to those for the entire population; on the other hand, people who are IADL disabled at age 70 have lower life expectancy by 3.5 years, and those with ADL disability are 5 to 6 years lower. For those who were IADL-disabled at age 70, total life expectancy increased by about half a year (0.53), but the increase was not significant. This group experienced increases in disability-free life expectancy (0.83) and decreases in IADL disabled life expectancy (0.35), but neither of these changes was significant. The changes were larger for the ADL disabled, with total life expectancy increasing from 7.7 to 9.6, with a gain of 1.9 years in nondisabled life expectancy, both of which were significant. These results show a tendency for greater improvement over this period in length of life free of disability as well as a decrease in time with a disability among those who arrive at old age with a disability.
Table 3.
Status-Based Life and Health Expectancies at Age 70 by Year and Initial Health Status (with confidence intervals)
| Status | Initial Disability State at Age 70 |
|||||
|---|---|---|---|---|---|---|
| Disability-Free |
IADL Disabled |
ADL Disabled |
||||
| 1984 | 1994 | 1984 | 1994 | 1984 | 1994 | |
| Total | 13.92 | 14.53 | 10.45 | 10.98 | 7.70 | 9.64 |
| Confidence Interval | 13.62–14.22 | 14.20–14.85 | 9.63–11.26 | 10.19–11.78 | 6.73–8.66 | 8.66–10.63 |
| Disability-Free | 11.24 | 11.87 | 5.72 | 6.55 | 3.29 | 5.20 |
| Confidence Interval | 11.00–11.50 | 11.61–12.13 | 4.94–6.50 | 5.84–7.27 | 2.52–4.08 | 4.33–6.08 |
| IADL Disabled | 1.28 | 1.17 | 3.03 | 2.68 | 1.15 | 1.23 |
| Confidence Interval | 1.19–1.37 | 1.09–1.26 | 2.74–3.32 | 2.45–2.92 | 0.89–1.42 | 1.00–1.46 |
| ADL Disabled | 1.40 | 1.49 | 1.70 | 1.75 | 3.25 | 3.21 |
| Confidence Interval | 1.30–1.49 | 1.37–1.60 | 1.49–1.92 | 1.53–1.96 | 2.87–3.62 | 2.90–3.52 |
SUMMARY AND CONCLUSIONS
Evidence from these two longitudinal surveys indicates that increases in life expectancy after age 70 were concentrated in years of life expectancy without ADL or IADL disability, meaning that later cohorts can expect a longer disability-free period of life. This was accomplished through some delay in the onset of disability and an increase in the likelihood of recovery from disability. While life expectancy overall increased in the population, it was because of decreases in mortality among the ADL disabled and some shift of the population over the time period into the lower mortality and less disabled group.
As life expectancy at older ages has increased, a question has arisen as to whether life is being extended only for those with severe impairment. Here we observe a pattern of greater mortality decline among the ADL disabled than either the IADL or nondisabled over this time period. This change would actually lead to an increase in disability in the population without compensating changes in other processes, such as the lower likelihood of becoming and remaining disabled. Our analysis indicates that declines in incidence and increases in recovery from disability must be the reinforcing forces responsible for observed decreases in the prevalence of ADL and IADL disability in the older population reported in numerous studies in the literature. This indicates not only the importance of disability processes in determining life expectancy free of disability or life cycle disability, but also how preventing and delaying disability and promoting recovery from disability interacts with mortality change in determining the prevalence of disability in the population. The long-run effect of the combination of more recent transition forces compared with the earlier set of transitions is for only small declines in ADL disability prevalence at the oldest ages because some changes in transition rates are a force for increases in disability prevalence (i.e., the reduction in mortality among the disabled), while the reductions in incidence and increase in recovery are a force for reductions in prevalence.
While we find that both mortality and disability processes have changed, we are not able to do more than speculate about the reasons for change. The decrease in the onset of disability could be linked to the fact that some diseases have become less disabling over time (Crimmins, Reynolds, and Saito 1999; Cutler 2001). This may reflect earlier diagnosis of disease and better disease management. Recent cohorts may arrive at a given age with less physical damage—which would result in a lower likelihood of ADL/IADL disability (Soldo et al. 2006)—possibly resulting from the fact that they have had a lifetime advantage from more education and less physically demanding jobs. However, a recent analysis showed little effect of improving education on reduction in ADL disability (Freedman, Crimmins, et al. 2004). It is also possible that new housing environments result in less environmental challenge in newer cohorts of older persons. The growth of alternatives to traditional housing could result in better ability/environmental fit for some persons. Technological and market changes may offer better opportunities for self-maintenance in more recent years and reduce the disability associated with functional loss. Increasing recovery from disability may also reflect changes in housing and technological conditions if people have become more likely to move or to change the way they accomplish tasks such as meal preparation to ameliorate a disability. Direct attempts to remediate loss of function and disability may also have improved. For instance, it is also possible that changes in ability to treat stroke have resulted in better return to functioning as well as reduced mortality for people who have an acute cerebrovascular event. Greater use of physical and occupational therapy may have enabled people to better regain ability to provide self-care.
Our findings are similar to those in the earlier analysis of LSOA I (Crimmins, Saito, and Reynolds 1997) and the recent analysis of the Medicare Current Beneficiary Survey (Cai and Lubitz 2007) in that a trend toward increased recovery is found. One of the reasons that trends based on these surveys may differ from those based on earlier analysis of the NLTCS is that disability in the NLTCS is limited to that which has lasted, or is expected to last, 90 days. It is possible that eliminating disability lasting less than three months changes the results of trend analysis; we know that recovery is more likely from short-term disability or shortly after onset of disability (Cai and Lubitiz 2007; Crimmins and Saito 1993). Our results also point to some decreased incidence of disability onset observed in other studies. We should note that a recent analysis of cohorts from the NLTCS that computed life expectancy at different ages using very different methods has drawn conclusions very similar to ours: “ALE increases faster than morbidity dependence, with the rate of improvement declining (faster) at higher levels of disability and at later ages” (Manton et al. 2008). Our examination of the changes in transitions indicates more change at ages over 80 and at younger ages.
We recognize several limitations to our analysis arising from differences between the two LSOA surveys that threaten the validity of our estimates. The somewhat lower initial response rate and the greater rate of loss over the period in the second survey means our results rest more on the weights used to compensate for these effects. Because the inputs to the estimates are transition rates rather than prevalence rates, the effect of initial prevalence, or distribution of the population at the radix, is quickly eliminated (Crimmins et al. 1994). The greater loss over the survey is addressed with imputations that assume that those who are lost will experience change similar to those who stay who have had the same history. If we did not impute any data, the results of this analysis would change because neither life expectancy nor disability-free life expectancy would increase significantly. This change in the estimates results mainly from the need to close the interval for people who are observed only once and who are most likely to be healthy, because even though the rates of non-follow-up will be higher for the disabled, the numbers are higher for the able. The fact that we cannot use results from an NDI search for the LSOA II with the IMaCh program has resulted in our imputing some deaths in the later cohort but not the earlier cohort. If we did not impute some cases to death, life expectancy would be even longer in the later period. The fact that our estimates of total life expectancy for both cohorts so closely match the estimates from U.S. vital statistics provides some assurance about our imputation procedures. Without imputations in LSOA II, our estimate of total life expectancy would be approximately a year lower than that reported in the vital statistics.
As we indicated above, we are not able to adjust for complex sample design, and given that many of the results are only marginally statistically significant, such adjustment might change our assessment of the results. Finally, we have not included gender in our analysis, and determining gender differences in trends is an important first step in understanding the process of change. In spite of these problems, there are very few nationally representative longitudinal cohorts available for assessment of change in incidence, recovery, and mortality. For instance, the NLTCS has repeated interviews with only a small portion of its sample after a five-year interval, making it difficult to use to study the range of individual trajectories. The Medicare Current Beneficiary Survey has yearly intervals but does not go back to the decade covered by the LSOA I.
We cannot compare the years of disability-free life estimated here to those developed using different definitions of disability-free life expectancy and based on methods with different assumptions; there is no reason to expect the numbers to be identical with different definitions of disability or different methods. However, the conclusion that most of the recent increase in life expectancy at the older ages has been concentrated in nondisabled years is the same using multiple methodological approaches and multiple definitions of disability. The richness of the multistate method is obvious because one is able to clarify the processes underlying this conclusion: a decrease in the rate or disability onset and an increase in the rate of recovery. This approach also allows us to understand the processes that have resulted in the observed decreases in disability.
Footnotes
Support for this research was provided by NIH Grants P30 AG017265 and R01AG11235.
There is heterogeneity in the length of the intervals between interviews in both surveys. In LSOA I, the mean length between Waves 1 and 2 for those interviewed was 26.42 months (SD = 3.30); but taking into account the fact that 32% of the sample was not interviewed at Wave 2, the actual time interval between the first observation and the second observation for the sample was, on average, 35.01 months (SD = 3.37). Combining all intervals in the LSOA I data, the average time interval between observations was 28.27 months (SD = 2.16). In LSOA II, the mean length between interviews for those interviewed at Waves 1 and 2 was 24.85 months (SD = 3.48), but the average time between the first and second observations was 26.64 months (SD = 3.63). Combining all observed intervals in the LSOA II data, the average time interval between observations was 27.94 months (SD = 4.37).
More details on the imputation can be found in supplemental material on Demography’s Web page (http://www.soc.duke.edu/resources/demography).
The standard errors do not correct for clustering at the individual level, which is often called the “repeat measures” problem.
Cai et al. (2008) estimated the design effect using a bootstrap approach and the SPACE (Stochastic Population Analysis for Complex Events) method of computing active-life expectancy. Comparing variance estimates from the bootstrap approach with those from IMaCh estimates shows the design effect for males and females both active and disabled ranging from about 1.3 to 1.8, and the differences in the standard errors of the life expectancies estimated using the two methods ranging from about .04 for non-Hispanic males to .01 for females. These differences are found in the cross section using data from the Medicare Current Beneficiary Survey.
We used the stepm of 24 in the IMaCh program for efficiency, tantamount to assuming only one event in a 24-month period, but examined alternatives of 12, 6, and 1 month. Varying stepm makes no significant differences in our estimates of life expectancy, as reported earlier by Gill et al. 2005. Using the data for LSOA I as an example, disabled life is identical using values of 24 and 1 for stepm (in both cases IADL and ADL are 1.32 and 1.4, respectively). Estimates of total life are 13.69 and 13.53, and active life expectancy is 10.92 and 10.76. The higher values are based on the stepm of 24 and the lower on a stepm of 1 month. Results were similar for 1994 except that the program would not converge with a stepm of 1.
An earlier multistate analysis of life expectancy without ADL/IADL impairment based on LSOA I produced a similar estimate of years of ADL/IADL disabled life at age 70 (2.9 versus 2.8 years) but quite different estimates of total life expectancy (12.2 versus 13.7 years; Crimmins et al. 1994). The use of the IMaCh method produces the longer estimates of total life expectancy because it is based on a logistic model, whereas the more traditional multistate life table applied in the earlier analysis uses central death rates. Another difference between the two estimates is that the traditional method of estimation could not accommodate different interval lengths, resulting in the elimination of many data points used in this analysis.
Percentages of the population aged 75–84 and 85 and older in institutions in the 1984 and 1989 NLTCS were used to produce estimates for 1986; NLTCS data for 1994 and 1997 were used for estimates for 1997. The ratios of the NLTCS institutionalized samples to those in LSOA I at Wave 2 were 1.87 for those aged 74–84 and 3.07 for those aged 85 and older; and for LSOA II at Wave 2, 2.33 for those aged 75–84 and 2.40 for those aged 85 and older.
Contributor Information
EILEEN M. CRIMMINS, Andrus Gerontology Center, University of Southern California, Los Angeles, CA 90089-0191; e-mail:crimmin@usc.edu.
MARK D. HAYWARD, Population Research Center and Department of Sociology, University of Texas at Austin.
AARON HAGEDORN, Andrus Gerontology Center, University of Southern California..
YASUHIKO SAITO, Advanced Research Institute for the Sciences and Humanities..
NICOLAS BROUARD, Institut National d’Etudes Démographiques, Paris..
REFERENCES
- Anderson RN. National Vital Statistics Reports. No. 28. Vol. 47. National Center for Health Statistics; Hyattsville, MD: 1999. “United States Life Tables, 1997”. Available online at http://www.cdc.gov/nchs/data/nvsr/nvsr47/nvs47_28.pdf. [PubMed] [Google Scholar]
- Bandeen-Roche K, Xue QL, Ferrucci L, Walston J, Guralnik JM, Chaves P, Zeger SL, Fried LP. “Phenotype of Frailty: Characterization in the Women’s Health and Aging Studies”. Journals of Gerontology: Biological Sciences & Medical Sciences. 2006;6:262–66. doi: 10.1093/gerona/61.3.262. [DOI] [PubMed] [Google Scholar]
- Bone MR, Bebbington AC, Jagger C, Morgan K, Nicolaas G. Health Expectancy and Its Uses. London: HMSO; 1995. [Google Scholar]
- Cai L, Lubitz J. “Was There a Compression of Disability for Older Americans From 1992 to 2003?”. Demography. 2007;44:479–95. doi: 10.1353/dem.2007.0022. [DOI] [PubMed] [Google Scholar]
- Cai L, Lubitz J, Hayward M, Saito Y, Hagedorn A, Crimmins E. “Using the Bootstrap Method to Estimate Variances of Multi-State Life Table Functions.”. Paper presented at the annual meeting of the Population Association of America; April 17–19; New Orleans. 2008. [Google Scholar]
- Centers for Medicare and Medicaid Services 2005“Medicare Part A Skilled Nursing Facility (SNF) Prospective Payment System (PPS) Price Update and Health Insurance Prospective Payment System (HIPPS) Coding Update Effective January 1, 2006.”MLN Matters No. MM3962. Available online at http://www.cms.hhs.gov/MLNMattersArticles/downloads/MM3962.pdf
- Crimmins EM. “Trends in the Health of the Elderly”. Annual Review of Public Health. 2004;25:79–98. doi: 10.1146/annurev.publhealth.25.102802.124401. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Hayward M, Saito Y. “Changing Mortality and Morbidity Rates and the Health Status and Life Expectancy of the Older U.S. Population”. Demography. 1994;31:159–75. [PubMed] [Google Scholar]
- Crimmins EM, Reynolds S, Saito Y. “Trends in Health and Ability to Work Among the Older Working-Age Population”. Journals of Gerontology Series B: Psychological Sciences & Social Sciences. 1999;54:S1–S10. doi: 10.1093/geronb/54b.1.s31. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y. “Getting Better and Getting Worse: Transitions in Functional Status Among Older Americans”. Journal of Aging and Health. 1993;5:3–36. [Google Scholar]
- Crimmins EM, Saito Y. “Trends in Disability-Free Life Expectancy in the United States, 1970–1990: Gender, Racial, and Educational Differences”. Social Science and Medicine. 2001;52:1629–41. doi: 10.1016/s0277-9536(00)00273-2. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y, Ingegneri D. “Trends in Disability-Free Life Expectancy in the United States, 1970–1990”. Population and Development Review. 1997;23:555–72. [Google Scholar]
- Crimmins EM, Saito Y, Reynolds S. “Further Evidence on Recent Trends in the Prevalence and Incidence of Disability Among Older Americans From Two Sources: The LSOA and the NHIS”. Journal of Gerontology Series B: Psychological Sciences & Social Sciences. 1997;52B:S59–S71. doi: 10.1093/geronb/52b.2.s59. [DOI] [PubMed] [Google Scholar]
- Cutler DM. “The Reduction in Disability Among the Elderly”. Proceedings of the National Academy of Sciences USA. 2001;98:6546–47. doi: 10.1073/pnas.131201698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA.2006“Late-Life Disability Trends: An Overview of Current Evidence.” 101–12.Workshop on Disability in America: A New Look—Summary and Background Papers Field MJ, Jette AM, Martin L.Washington, DC: National Academies Press; Also available online at http://www.nap.edu/catalog/11579.html [Google Scholar]
- Freedman VA, Aykan H, Wolf DA, Marcotte JE. “Disability and Home Care Dynamics Among Older Unmarried Americans”. Journals of Gerontology: Psychological Sciences & Social Sciences. 2004;59B:S25–S33. doi: 10.1093/geronb/59.1.s25. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Crimmins EM, Schoeni RF, Spillman BC, Aykan H, Kramarow E, Land K, Lubitz J, Manton KG, Martin LG, Shinberg D, Waidmann TA. “Resolving Inconsistencies in Trends in Old-Age Disability: Report From a Technical Working Group”. Demography. 2004;41:417–41. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- Gill TM, Allore H, Hardy SE, Holford TR, Han L. “Estimates of Active and Disabled Life Expectancy Based on Different Assessment Intervals”. Journal of Gerontology: Biological Sciences & Medical Sciences. 2005;60:1013–16. doi: 10.1093/gerona/60.8.1013. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Crimmins EM, Saito Y. “Cause of Death and Active Life Expectancy in the Older Population of the United States”. Journal of Aging and Health. 1998;10:192–213. [Google Scholar]
- Hayward MD, Grady WR. “Work and Retirement Among a Cohort of Older Men in the United States, 1966–1983”. Demography. 1990;27:337–56. [PubMed] [Google Scholar]
- Jagger C, Goyder E, Clarke M, Brouard N, Arthur A. “Active Life Expectancy in People With and Without Diabetes”. Journal of Public Health Medicine. 2003;25:42–46. doi: 10.1093/pubmed/fdg009. [DOI] [PubMed] [Google Scholar]
- Laditka SB, Hayward MD. “The Evolution of Demographic Methods to Calculate Health Expectancies.”. In: Robine J-M, Jagger C, Mathers CD, Crimmins EM, Suzman RM, editors. Determining Health Expectancies. Chichester, UK: Wiley; 2003. pp. 221–34. [Google Scholar]
- Laditka SB, Laditka JN. “Effects of Diabetes on Healthy Life Expectancy: Shorter Lives With More Disability for Both Women and Men.”. In: Yi Zeng, Crimmins EM, Carriere Y, Robine J-M., editors. Longer Life and Healthy Aging. Dordrecht, The Netherlands: Springer; 2006. pp. 71–90. [Google Scholar]
- Laditka SB, Wolf D. “New Methods for Analyzing Active Life Expectancy”. Journal of Aging and Health. 1998;10:214–41. [Google Scholar]
- Land K, Guralnik J, Blazer D. “Estimating Increment-Decrement Life Tables With Multiple Covariates From Panel Data: The Case of Active Life Expectancy”. Demography. 1994;31:289–319. [PubMed] [Google Scholar]
- Leveille SG, Penninx BWJH, Melzer D, Izmirlian G, Guralnik JM. “Sex Differences in the Prevalence of Mobility Disability in Old Age: The Dynamics of Incidence, Recovery, and Mortality”. Journal of Gerontology: Psychological Sciences & Social Sciences. 2000;55B(1):S41–S50. doi: 10.1093/geronb/55.1.s41. [DOI] [PubMed] [Google Scholar]
- Liévre A, Brouard N, Heathcote C. “The Estimation of Health Expectancies From Cross-Longitudinal Surveys”. Mathematical Population Studies. 2003;10:211–48. [Google Scholar]
- Lynch SM, Brown JS, Harmsen KG. “The Effect of Altering ADL Thresholds on Active Life Expectancy Estimates for Older Persons”. Journals of Gerontology: Psychological Sciences & Social Sciences. 2003;58B:S171–S178. doi: 10.1093/geronb/58.3.s171. [DOI] [PubMed] [Google Scholar]
- Manton KG, Corder L, Stallard E. “Estimates of Change in Chronic Disability and Institutional Incidence and Prevalence Rates in the U.S. Elderly Population From the 1982, 1984, and 1989 National Long Term Care Survey”. Journals of Gerontology: Psychological Sciences & Social Sciences. 1993;48:S153–S166. doi: 10.1093/geronj/48.4.s153. [DOI] [PubMed] [Google Scholar]
- Manton KG, Gu X, Lamb VL. “Change in Chronic Disability From 1982 to 2004/2005 as Measured by Long-Term Changes in Function and Health in the U.S. Elderly Population”. Proceedings of the National Academy of Sciences of the United States of America. 2006;103(48):18374–79. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton KG, Gu X, Lowrimore GR. “Cohort Changes in Active Life Expectancy in the U.S. Elderly Population: Experience From the 1982–2004 National Long-Term Care Survey”. Journals of Gerontology: Psychological Sciences & Social Sciences. 2008;63B:S269–S281. doi: 10.1093/geronb/63.5.s269. [DOI] [PubMed] [Google Scholar]
- Manton KG, Land K. “Active Life Expectancy Estimates for the U.S. Elderly Population: A Multidimensional Continuous Mixture Model of Functional Change Applied to Completed Cohorts, 1982–1996”. Demography. 2000;37:253–65. [PubMed] [Google Scholar]
- Melzer D, Izmirlian G, Leveille SG, Guralnik JM. “Educational Differences in the Prevalence of Mobility Disability in Old Age: The Dynamics of Incidence, Mortality, and Recovery”. Journals of Gerontology: Psychological Sciences & Social Sciences. 2001;56B:S294–S301. doi: 10.1093/geronb/56.5.s294. [DOI] [PubMed] [Google Scholar]
- Minicuci N, Noale M, Pluijm SMF, Zunzunegui MV, Blumstein T, Deeg DJH, Bardage C, Jylha M. “Disability-Free Life Expectancy: A Cross-National Comparison of Six Longitudinal Studies on Aging. The CLESA Project”. European Journal of Ageing. 2004;1:37–44. doi: 10.1007/s10433-004-0002-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics (NCHS) 1990Vital Statistics of the United States, 1987 IISection 6, “Life Tables.” DHHS Publication No. (PHS) 90-1104.Washington, DC: Public Health Service; Available online athttp://www.cdc.gov/nchs/data/lifetables/life87_2acc.pdf [Google Scholar]
- National Center for Health Statistics (NCHS) 2002The 1994–2000 Second Longitudinal Study of Aging: Wave 3 Survivor File, version SF 2.1, October 2002 National Center for Health Statistics, Centers for Disease Control Available online at http://www.cdc.gov/nchs/about/otheract/aging/w3sf.htm
- Reynolds SL, Saito Y, Crimmins EM. “The Impact of Obesity on Active Life Expectancy in Older American Men and Women”. The Gerontologist. 2005;45:438–44. doi: 10.1093/geront/45.4.438. [DOI] [PubMed] [Google Scholar]
- Robine J-M, Mormiche P, Sermet C. “Examination of the Causes and Mechanisms of the Increase in Disability-Free Life Expectancy”. Journal of Aging and Health. 1998;10:171–91. [Google Scholar]
- Schoeni RF, Martin LG, Andreski PM, Freedman VA. “Persistent and Growing Socioeconomic Disparities in Disability Among The Elderly: 1982–2002”. American Journal of Public Health. 2005;95:2065–70. doi: 10.2105/AJPH.2004.048744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldo BJ, Mitchell OS, Tfaily R, McCabe JF.2006“Cross-Cohort Differences in Health on the Verge of Retirement.”PRC WP 2006-17 Pension Research Council Working Paper Pension Research Council, The Wharton School, University of Pennsylvania. Available online athttp://www.pop.upenn.edu/rc/parc/aging_center/2006/PARCwps06-13.pdf
- Spector WD, Fleishman JA. “Combining Activities of Daily Living With Instrumental Activities of Daily Living to Measure Functional Disability”. Journals of Gerontology: Psychological Sciences and Social Sciences. 1998;53B:S46–S57. doi: 10.1093/geronb/53b.1.s46. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services 2000“Cost-Effectiveness of Home and Community-Based Long-Term Care Services.”Background paper. USHHS/ASPE Office of Disability, Aging and Long-Term Care Policy, Washington, DC. Available online at http://aspe.hhs.gov/daltcp/reports/costeff.htm
- Verbrugge LM. “Recent, Present, and Future Health of American Adults”. Annual Review of Public Health. 1989;10:333–61. doi: 10.1146/annurev.pu.10.050189.002001. [DOI] [PubMed] [Google Scholar]
- Verbrugge LM, Jette AM. “The Disablement Process”. Social Science & Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- White KM. “Longevity Advances in High-Income Countries, 1955–96”. Population and Development Review. 2002;28:59–76. [Google Scholar]
- Wolf DA, Mendes de Leon C, Glass T. “Trends in Rates of Onset of and Recovery From Disability at Older Ages: 1982–1994”. Journals of Gerontology: Psychological Sciences & Social Sciences. 2007;62B:S3–S10. doi: 10.1093/geronb/62.1.s3. [DOI] [PubMed] [Google Scholar]
- Wu SC, Leu SY, Li CY. “Incidence of and Predictors for Chronic Disability in Activities of Daily Living Among Older People in Taiwan”. Journal of the American Geriatric Society. 1999;47:1082–86. doi: 10.1111/j.1532-5415.1999.tb05231.x. [DOI] [PubMed] [Google Scholar]