Abstract
The experience of stressful social interactions, negative causal attributions, and the use of maladaptive coping efforts help maintain depression over time in the general population. We investigated whether a similar experience occurs among adults with mild intellectual disability. We compared the frequency and stress impact of such interactions, identified causal attributions for these interactions, and determined the coping strategies of 47 depressed and 47 nondepressed adults with mild intellectual disability matched on subject characteristics. The depressed group reported a higher frequency and stress impact of stressful social interactions, more negative attribution style, and more avoidant and less active coping strategies did than the nondepressed group. Findings have implications for theory building and development of psychotherapies to treat depression.
Depression is one of the most frequent psychiatric disorders in adults with intellectual disability (Borthwick-Duffy, 1994; Linna et al., 1999; Richards et al., 2001). The point prevalence of depression among adults with intellectual disability is estimated to be 4% (Cooper & Bailey, 2001; Cooper, Smiley, Morrison, Williamson, & Allan, 2007; Deb, Thomas, & Bright, 2001), and the period prevalence is thought to be notably higher (Smiley & Cooper, 2003). Adults with mild intellectual disability, therefore, experience depression at greater rates than do their peers with average intelligence. Unlike depression in the general population, however, there has been little systematic research regarding the processes that contribute to the onset or persistence of depression in an intellectual disability population. Given the enormous cost and emotional burden of caring for individuals with depression (Lakin, Doljanic, & Taub, 2007; Minnes, Woodford, & Passey, 2007), research is needed to understand the mechanisms contributing to depression in adults with intellectual disability. This information would be beneficial to theorists and those who design interventions to treat depression in this population. We designed this study to address the methodological limitations of previous studies and determine whether a clinical diagnosis of depression is related to stressful social interactions, negative causal attributions, and maladaptive coping in adults with mild intellectual disability as it is in the general population.
In the general population, people who are depressed report experiencing a high rate of stressful events, and this is purported to maintain depression over time (Davila, Hammen, Burge, Paley, & Daley, 1995; Hammen, 1991). Depressed persons are particularly vulnerable to experiencing stressful social interactions (e.g., Davila et al., 1995; Joiner & Coyne, 1999; Joiner & Metalsky, 1995). Studies have shown that depressed persons often behave in ways that elicit criticism, rejection, and interpersonal conflict (e.g., Davila et al., 1995; Hammen, 1991; Joiner & Metalsky, 1995). Moreover, maladaptive cognitive processing has been shown to make depressed persons more sensitive to these negative interactions and accentuates their impact (e.g., Gotlib & Hammen, 1992; Sacco, 1999).
Preliminary evidence suggests that depressed persons with mild intellectual disability similarly experience a high rate of stressful social interactions. Nezu, Nezu, Rothenberg, DelliCarpini, and Groag (1995) found that the depressive symptoms of adults with mild intellectual disability were associated with an increased frequency of negative social interactions. Lunsky and colleagues found that stress surrounding negative social interactions was positively correlated with concurrently assessed depressive symptoms. Further, interpersonal stress predicted depressive symptoms that were evident 6 months later (Lunsky & Benson, 2001; Lunsky & Havercamp, 1999). Similarly, Hartley and MacLean (2005) examined the subjective perceptions of stress among 88 adults with mild intellectual disability and found that both the frequency and stress impact of stressful social interactions predicted symptoms of depression.
In many of these studies, the association between stressful social interactions and depressive symptoms was investigated in adults with mild intellectual disability who did not have a depressive disorder (Hartley & MacLean, 2005; Lunsky & Benson, 2001; Lunsky & Havercamp, 1999). This strategy does not allow for a direct test of whether perceptions of stress are related to a clinical diagnosis of depression. Perceptions of stressful social interactions in adults with mild intellectual disability who have a depressive disorder were examined in only one study. Nezu and colleagues (1995) found that 16 adults with mild intellectual disability who had a depressive diagnosis reported more stress surrounding social relationships than did 16 adults with mild intellectual disability who were not depressed and who were matched on age, gender, and IQ. One of our purposes in conducting the present study was to build on this research by using a larger sample of depressed adults with mild intellectual disability.
In addition, we designed the present study to ensure that subject characteristic differences, other than age, gender, and IQ, between the depressed and nondepressed groups could not account for findings. Adults with mild intellectual disability who have more independent self-help abilities may be better able to avoid stressful social interactions than are adults with limited everyday living skills. In addition, studies suggest that adults with intellectual disability living in group homes with several other clients and staff have more negative social interactions than do adults with intellectual disability living alone or with only a few others (Felce, Lowe, & Blackman, 1995). Thus, in our study we controlled for adaptive behavior and living status in addition to IQ, gender, and age to understand the relation between stressful social interactions and a clinical diagnosis of depression in adults with mild intellectual disability.
Causal Attributions
In the general population, dysfunctional cognitive patterns of depressed persons have been shown to increase susceptibility to experiencing frequent and severe stressful social interactions. One of the most widely recognized cognitive processes critical to maintaining depression is a tendency to make negative attributions or causal explanations for negative stressful events (Abramson, Seligman, & Teasdale, 1978; Abramson, Metalsky, & Alloy, 1989). People who are depressed make global, stable, and internal causal explanations for negative events (e.g., Firth & Brewin, 1982; Nolen-Hoeksema, Girgus, & Seligman, 1986; Robins, 1988).
A growing body of research suggests that many of the same faulty cognitive patterns seen in the general population (e.g., having a low self-concept, making negative social comparisons, and more frequent automatic negative thoughts) also occur in depression among persons with intellectual disability (Benson & Ivins, 1992; Dagnan & Sandhu, 1999; Esbensen & Benson, 2006; Glenn, Bihm, & Lammers, 2003; Lunsky, 2003; Nezu et al., 1995). However, there is only one published study on whether depression is related to negative causal attributions for stressful events in an intellectual disability population. Esbensen and Benson (2005, 2006) examined attributions for negative and positive events through the Children’s Attribution Style Questionnaire (Seligman et al., 1984) in 73 adults with mild intellectual disability. They found that negative attributions (i.e., more internal, stable, and global) for negative events were correlated with depressed mood. Esbensen and Benson also found a greater rate of negative attributions among 12 adults with intellectual disability diagnosed with major depression than among a matched comparison group of 12 non-depressed adults. Conclusions from their study are limited, however, by the small sample size and methodological problems with the questionnaire. They examined attribution styles for hypothetical negative events through a self-report measure designed for the general population. Poor internal consistency (.39) was reported for the Children’s Attribution Style Questionnaire in this sample. Although Esbensen and Benson (2006) pointed out that poor internal consistency has also been reported for this questionnaire among typically developing children, inadequate reliability raises questions about the soundness of study findings. Moreover, test–retest reliability and construct validity for use of this questionnaire in an intellectual disability population has not been assessed.
Self-report measures using Likert-type response options, such as the Children’s Attribution Style Questionnaire, are vulnerable to poor reliability among adults with intellectual disability if pretest procedures are not employed to screen out participants who demonstrate response bias (Finlay & Lyons, 2002; Hartley & MacLean, 2006). Measures designed to determine complex meta-cognitive content, such as causal explanations for hypothetical negative events, may be particularly prone to response problems. Use of open-ended questions can avoid these difficulties and offer a method for assessing the spontaneously generated causal explanations for actual stressful social interactions experienced by adults with intellectual disability. Therefore, we designed the present study to build on previous research by assessing causal attributions through open-ended questions to actual stressful social interactions in a large sample of adults with mild intellectual disability and diagnosed with a depressive disorder.
Coping Strategies
Depressed persons in the general population have difficulty effectively coping with stressful negative situations. Depression is related to a lack of active coping aimed at altering the stressful situation or negative emotions surrounding the situation and increased use of avoidant coping intended to avoid or ignore the stressful situation and negative affect surrounding it (e.g., Aldwin & Revenson, 1987; Endler & Parker, 1990; Moos, 1991; Sigmon et al., 2007). A high rate of avoidant coping may not only prolong and exacerbate the stressful situation but also intensify negative emotions surrounding it (Holahan & Moos, 1987; Wegner, 1994; Wegner & Wenzloff, 1996). In this way, maladaptive coping efforts are also thought to contribute to the persistence of depressed affect over time.
In recent research investigators have suggested that coping may similarly be related to depression in adults with mild intellectual disability (Hartley & MacLean, 2005; Lunsky, 2003). Lunsky found that depressed women with mild intellectual disability reported fewer coping strategies than did nondepressed women. To date, there has been only one study in which researchers questioned whether depressed adults with intellectual disability use different types of coping strategies to deal with stressful events than do nondepressed adults with intellectual disability. Hartley and MacLean (2005) found that depressive symptoms among adults with mild intellectual disability were related to an infrequent use of active coping. However, most participants in this study did not have a clinical diagnosis of depression. Therefore, another purpose in the present study was to determine whether adults with mild intellectual disability diagnosed with a depressive disorder have difficulty adaptively coping with stressful social interactions.
We examined the experience of stressful social interactions among 47 depressed and 47 non-depressed adults with mild intellectual disability who were matched on various subject characteristics by (a) comparing the frequency and stress impact of stressful social interactions, (b) identifying causal attributions for these interactions, and (c) determining the coping strategies used to deal with these interactions and the negative emotions evoked. We hypothesized that depressed adults with mild intellectual disability would report a higher frequency and stress impact of stressful social interactions, more negative attribution style, and more avoidant and less active coping strategies than would nondepressed adults.
Method
Participants
Fifty-two adults with mild intellectual disability (IQ = 55–70, concomitant impairments in adaptive behavior, and who had met criteria for a diagnosis of mental retardation according to the Diagnostic and Statistical Manual, Fourth Edition Text Revision–DSM-IV-TR (American Psychiatric Association, 2000) were recruited from 10 disability service providers in the Rocky Mountain region of the United States. They also had a current diagnosis of a depressive disorder (i.e., Major Depressive Disorder, Dysthymia, or Depression–Not Otherwise Specified) according to their disability service providers. All participants had adequate oral communication skills (i.e., could orally communicate without the aid of another person). The majority of them were taking medication to manage their depression. Previous studies of the interpersonal or cognitive processes among depressed adults with intellectual disability have not limited etiology of intellectual disability (Benson & Ivins, 1992; Dagnan & Sandu, 1999; Nezu et al., 1995). To be consistent with this approach, we chose participants who had a range of etiologies for intellectual disability, the most common being unknown etiology. Four participants were unable to pass the pretest outlined in the Procedure section and were excluded. An additional participant demonstrated response bias during actual testing (i.e., endorsed same response option on all items) and was also excluded. Forty-seven adults with mild intellectual disability without a depressive disorder matched on age (within 5 yrs), gender, IQ (within 5 points), ethnicity (Caucasian vs. not Caucasian), impairments in adaptive behavior (within 10 points), and living status served as a comparison group. In the depressed group, 6 adults had a reported psychiatric disorder diagnosis in addition to depressive disorder noted by their disability service provider (3 anxiety disorder, 2 personality disorder, and 1 sleep disorder). Ten adults with mild intellectual disability in the non-depressed group had a nondepressive psychiatric disorder diagnosis (2 adjustment disorder, 4 anxiety disorder, 3 personality disorder, and 1 sexual disorder). Table 1 presents the characteristics of the depressed and nondepressed groups. All participants and their guardians were given a description of the nature and requirements of the study prior to deciding to participate and informed consent was obtained.
Table 1.
Characteristics by Group
| Depressed |
Nondepressed |
|||
|---|---|---|---|---|
| Characteristic | Mean/n | SD | Mean/n | SD |
| Mean age | 42.62 | 12.87 | 41.74 | 12.03 |
| Gender (n) | ||||
| Male | 24 | – | 24 | – |
| Female | 23 | – | 23 | – |
| Ethnicity (n) | ||||
| Caucasian | 42 | – | 42 | – |
| Not Caucasian | 5 | – | 5 | |
| Mean Composite IQ | 62.94 | 5.64 | 61.19 | 5.73 |
| Mean adaptive behavior | 67.26 | 12.67 | 67.19 | 12.66 |
| Living status (n) | ||||
| Group home | 31 | – | 31 | – |
| Family/host family | 4 | – | 4 | – |
| Alone or with roommate/partner | 12 | – | 12 | – |
Note. Groups were matched on age (5 years), gender, ethnicity, Composite IQ (5 points), adaptive behavior (10 points), and living status.
Measures
Participant characteristics
The age, gender, living status, and ethnicity of each participant was obtained from their disability service provider. The Kaufman Brief Intelligence Test, 2nd Edition–KBIT-2 (Kaufman & Kaufman, 2004), a brief test of verbal and nonverbal cognitive abilities, was individually administered to participants. The Composite IQ, which was used in this study. has satisfactory internal consistency (.86 to .96), test–retest reliability (.88 to .92), and concurrent validity (Kaufman & Kaufman, 2004). To assess adaptive behavior, we asked staff from each participant’s disability service provider who had at least weekly contact with the participant to complete the Adaptive Behavior Assessment System-2nd Edition–ABAS-II (Harrison & Oakland, 2006). We also administered the General Adaptive Composite (GAC) score, which has satisfactory internal consistency (.97 to .99), test–retest reliability (.86 to .99), and concurrent validity (Harrison & Oakland, 2006).
Depression
We conducted a diagnostic interview with the adults who had mild intellectual disability using the Diagnostic Criteria for Psychiatric Disorders for Use with Adults with Learning Disabilities/Mental Retardation–DC-LD (Royal College of Psychiatrists, 2001). The DC-LD was specifically designed for people with intellectual disability and offers operationalized diagnostic criteria for psychiatric disorders. Field trials indicated that diagnoses based on the DC-LD had a 96.3% agreement with clinical opinion (Smiley & Cooper, 2003; Royal College of Psychiatrists, 2001). In the present study, participants in the depressed group also had to meet criteria for a current depressive diagnosis using the DC-LD, and participants in the matched comparison group could not meet criteria for a depressive diagnosis on the DC-LD.
The Birleson Depressive Short form Self-Rating Scale–hereafter called the Depressive Self-Rating Scale (Birleson, 1981) was used to verify that adults in the depressed group reported more symptoms of depression than did those in the nondepressed group. The scale has 18 items and three response categories (never, sometimes, and most of the time). Among typically developing children, the scale has adequate test–retest reliability, internal consistency, and concurrent and criterion validity (Birleson, 1981). Among adults with mild intellectual disability, the Depressive Self-Rating Scale was significantly correlated with informant ratings of depressive symptoms (Benson & Ivins, 1992). In the present study, a paired sample t test indicated that the depressed group had a significantly higher Depressive Self-Rating Scale total score (M = 19.59, SD = 6.34) than did the nondepressed group (M = 10.78, SD = 6.80), t(46) = 18.38, p < .01.
Stressful social interactions
The Inventory of Negative Social Interactions (Lakey, Tardiff, & Drew, 1994) is a 40-item self-report measure of negative social situations. Sample items include “Said bad things about you” and “Friends spent less time with you.” Among adults with mild intellectual disability, this inventory has satisfactory reliability and is predictive of somatic complaints and depressive symptoms reported 6 months later (Lunsky & Benson, 2001; Lunsky & Bramston, 2006).
The Lifestress Inventory (Bramston & Bostock, 1994) is a self-report measure of daily situations or life events previously reported to be stressful by adults with intellectual disability. The Lifestress Inventory has satisfactory test–retest reliability, internal consistency, and concurrent validity (Bramston & Bostock, 1994; Bramston & Fogarty, 1995; Fogarty, Bramston, & Cummins, 1997; Lunsky & Bramston, 2006). Only the 13-item Negative Interpersonal Relations dimension was used in this study. This dimension was designed to elicit the experience of stressful social interactions. Sample items include “Have you had any arguments with anyone?” and “Do people tease you or call you names” A composite measure of stressful social interactions was created by summing scores from the 40-item Inventory of Negative Social Interactions and 13-item Negative Interpersonal Relations dimension of the Life-stress Inventory. Our decision to use a composite measure of stressful social interactions was based the (a) moderate correlation between the Total Frequency and Total Severity, rs = .48 and .53, respectively, ps < .01, of the Negative Interpersonal Relations dimension of the Lifestress Inventory and Inventory of Negative Social Interactions; and (b) finding similar results when these measures were separately analyzed.
The same response format was used for the Lifestress Inventory and Inventory of Negative Social Interactions. In the frequency rating, participants indicated whether they had experienced the stressful situation in the past 2 weeks. The total frequency score is the total number of stressful social interactions experienced across both measures. In the Stress Impact rating, participants rated the severity of stress incurred using a 4-point Likert-type scale (verbal descriptors [no, a little, medium, and a lot] and numbers [1–4]). Consistent with Fogarty et al.’s (1997) findings, Stress Impact ratings were rescored such that stressful social interactions not experienced or experienced but rated as having no stress impact were scored 0, interactions rated as causing a little stress impact were scored 1, interactions rated as causing medium stress impact were scored 2, and those rated as causing a lot of stress impact were scored 3. Stress Impact ratings were summed to create the Total Stress Impact score. In the present study, there was satisfactory internal consistency for the Total Frequency and Total Severity of the Life-stress Inventory, α = .72, .77 and Inventory of Negative Social Interactions, α = .81, .88.
Causal attribution
The open-ended question “What caused that event to occur?” was used to assess causal attributions for each stressful social interaction endorsed. Two undergraduate students who were naïve to the group assignments (i.e., depressed vs. nondepressed) rated the Internality, Stability, and Globility of these responses using a content analysis of verbatim explanations, a content analytic technique to assess explanatory styles. This technique has been shown to result in reliable and valid assessments of explanatory styles in the typically developing population (Gray, Pumphrey, & Lombardo, 2003; Kamen-Siegel, Rodin, Seligman, & Dwyer, 1991; Schulman, Castellon, & Seligman, 1989). The two undergraduates were trained according to the guidelines developed by Schulman et al. (1989) to use 7-point Likert scales: Internality (1–7: external to internal), Stability (1–7: unstable to stable), and Globility (1–7: specific to global).
Participants endorsed varying numbers of stressful social interactions. Moreover, many participants were unable to identify or describe causal explanations for every stressful social interaction endorsed. Therefore, the Internality, Stability, and Globality scores were summed and then divided by the number of causal attributions provided. In order to assess interrater reliability, we defined agreement as the two coders being within 1 point in their independent content analysis of verbatim explanations ratings. The percentage agreement between the raters for the Internality (89.4%), Stability (86.0%), and Globality (84.4%) dimensions indicated adequate interrater reliability. These dimension scores were then summed to create the Composite Negative score. Cronbach’s alpha coefficient was .71 for the Composite Negative scale, which is consistent with alpha coefficients reported for this technique when used in the general population (Gray et al., 2003; Kamen-Siegel et al., 1991; Schulman et al., 1989).
Coping strategies
Open-ended responses to the sentence stem “When I have this problem, I —” were used to assess coping efforts for each stressful social interaction endorsed. Previous studies have shown that this procedure successfully elicits coping responses among adults with intellectual disability (Hartley & MacLean, 2005; Lunsky, 2003; Wayment & Zetlin, 1989). Two undergraduate students who were naïve to the hypotheses of the study were trained to code responses as active and avoidant coping strategies defined by Ayers and colleagues (Ayers et al., 1989; Program for Prevention Research, 1999). Active coping was defined as a cognitive or behavioral effort to manage the stressful event itself through directly altering the event, seeking solutions to alter it, or by altering one’s emotional response to the event by focusing directly on it in an active and constructive fashion. Avoidant coping was defined as a behavioral or cognitive effort to avoid the stressful event or to repress, not think about, or wish away the problem. Responses that involved verbal or physical actions to implicitly or explicitly hurt or threaten others, venting feelings with no intention of altering these feelings, or lack of efforts to alter or avoid the problem were coded as noncoping efforts.
Participants often reported using multiple coping strategies to deal with a single stressful event. When this occurred, all coping strategies were coded. To account for differences in total number of coping responses reported by participants, the ratio of coping responses in each dimension in comparison to the total number of coping responses was used in all analyses. Satisfactory interrater reliability was achieved for coding responses into coping (.87) versus noncoping efforts (.90) and for active (.83) and avoidant coping (.85).
Procedure
Participants were informed that their responses would be confidential and that they could withdraw from the study at any time. To help participants feel comfortable, a caregiver was present during interviews if requested but did not assist the participant in responding. A 2-step pretest was used to assess participants’ ability to reliably use a 4-point Likert-type scale and understand the meaning of stressful events. In Step 1, participants were asked to arrange a set of four clear containers with varying amounts of colored water by quantity of water. Participants were then asked to match these containers to written descriptors (no, a little, medium, and a lot) and a numerical scale (1 to 4). Finally, participants were asked to use the containers, written descriptors, or numbers to indicate where their most favorite and least favorite food would fall on a scale of preference. In Step 2, participants were asked to provide an example of a stressful event. Only participants who successfully passed both steps of the pretest were included in the study. In a previous study using this pretest to screen out participants, a low rate of response bias was found for Likert-type scales in actual testing (Hartley & MacLean, 2005).
A researcher unaware of participants’ group membership (i.e., depressed vs. nondepressed) administered assessments. Participants were first given the KBIT-2. They were then read the Lifestress Inventory and Inventory of Negative Social Interactions and asked to rate the Frequency and Stress Impact of each stressful social interaction. Clear containers with varying amounts of colored water were paired with the Likert-type scale responses to provide a visual representation of response options. For each stressful social interaction endorsed, participants were asked, “What caused that event?” One participant was unable to provide any causal explanations for stressful social interactions and, thus, was not included in analyses of causal attributions. Participants were also asked to complete the word stem “When I have this problem I —.” If they were confused or did not describe coping efforts, the statement prompt “People do different things to solve their problems or to make themselves feel better; What do you do when you have this problem?” (Program for Prevention Research, 1999) was read. The clarifying question “Tell me more about it” was employed to confirm understanding of answers and seek further information when needed. The Depressive Self-Rating Scale was read aloud. The procedure was conducted in a single session, with breaks, and took 60 to 90 min.
Results
Independent samples t tests were conducted to ensure that the subject characteristics (age [years], IQ [Composite IQ standard score], and adaptive behavior [ABAS]) of the depressed and nondepressed group were comparable. There was no significant difference between the matched pairs in age, t(93) = −.34, p = .74, IQ, t(93) = −1.02, p = .31, or adaptive behavior, t(93) = −.02, p = .98. As shown in Table 1, the depressed and nondepressed groups were successfully paired on gender, ethnicity, and living status. We examined paired sample correlations for the stressful social interaction, causal attributions, and coping variables. Correlations were positive for all variables and significant for Total Frequency of stressful social interactions, r = .29, p = .03. This find-ing supports the importance of matching the groups on subject characteristics, and the use of paired sample t tests in the remaining analyses. Cohen’s d calculations based on the original SDs (or between group t-test values) were used to estimate effect size (Dunlop, Cortina, Vaslow, & Burke, 1996).
The depressed group had a significantly higher Total Frequency of stressful social interactions than did the nondepressed group (Ms = 20.15, SD = 7.07, and 14.04, SD = 7.90, respectively), t(46) = 3.86, p = .001, d = .82 (95% confidence interval .39 to 1.23). The depressed group (M = 42.72, SD = 8.73) also had a significantly higher Total Stress Impact of stressful social interactions than did the nondepressed group (M = 23.84, SD = 7.02), t(46) = 4.39, p = .001, d = .90 (95% confidence interval .47 to 1.32).
Figure 1 displays the means and SDs for Internality, Stability, and Globality of causal attributions reported for stressful social interactions incurred by the depressed and nondepressed groups. The depressed group was significantly higher (i.e., more internal) on the Internality dimension than was the nondepressed group (Ms = 5.11, SD = 1.19 and 3.07, SD = 1.00, respectively), t(45) = 7.88, p < .001, d = 1.86 (95% confidence interval 1.35 to 2.33). The depressed group was significantly higher (i.e., more stable) on the Stability dimension than was the nondepressed group (Ms = 5.00, SD = 1.02, and 4.53, SD = 1.06), t(45) = 2.16, p = .04, d = .45 (95% confidence interval .03 to .86). The depressed group was significantly higher (i.e., more global) on the Globality dimension than was the nondepressed group (Ms = 4.00, SD = 0.90, and 3.19, SD = 1.06, respectively), t(45) = 3.72, p = .001, d = .82 (95% confidence interval .39 to 1.24). On the Composite Negative score, the depressed group was significantly higher (i.e., more internal/stable/global) than was the nondepressed group (Ms = 14.10, SD = 2.70, and 10.86, SD = 1.99, respectively), t(45) = 6.03, p < . 001, d = 1.37 (95% confidence interval .90 to 1.81). Table 2 presents examples of attributions and coping efforts of the depressed and nondepressed group.
Figure 1.
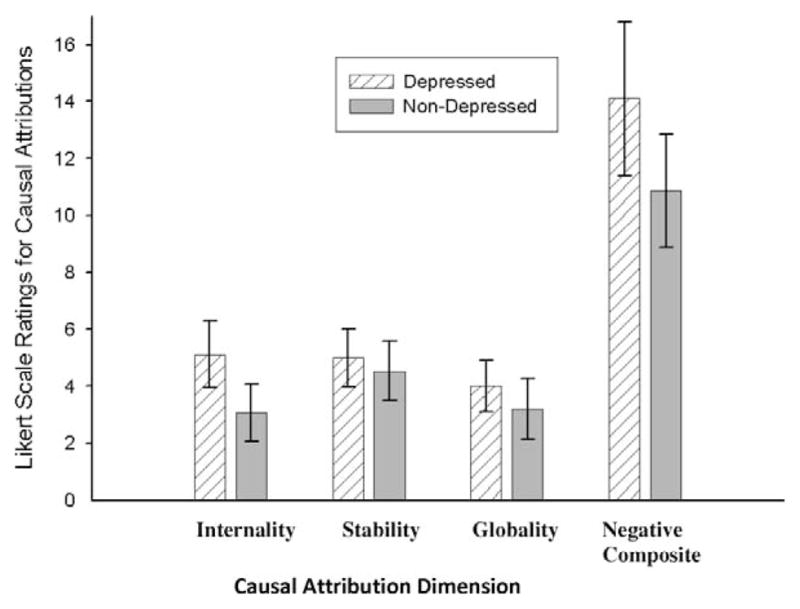
Means and SDs for Likert-scale content analysis of verbatim explanations (CAVE) ratings of causal attributions reported by group. Note that higher scores mean more internal/stable/global ratings.
Table 2.
Examples of Attributions and Coping Responses by Group
| Group/Negative event | Attributiona | Coping |
|---|---|---|
| Depressed | ||
| Acted bossyb | Cause I don’t stand up to him enough. (Internality = 6, Stability = 5, Globality = 5) | Pretend he isn’t thered or go in my roomc |
| People don’t like talking to youc | Cause I’m not as good as my sisters are. They are making lots of money and never get in trouble. (Internality = 7, Stability = 7, Globality = 7) | I get real mad and tell him off.e |
| Friends spent less time with youb | I don’t know. I think they don’t like what I do or the way I laugh. (Internality = 5, Stability = 6, Globality = 6) | I just be by myself and ignore them.d |
| Arguments with anyonec | I’m just always asking people questions and they get mad cause I’m a pest. (Internality = 6, Stability = 6, Globality = 6) | I don’t know what to do. I ask them why they angry,f but they don’t tell. |
| Not enough friendsc | Cause they don’t want to be my friend. No friends. Never. (Internality = 5, Stability = 7, Globality = 5) | Can’t do nothing. Never have no friends.e |
| Nondepressed | ||
| Get on well with your familyc | They just busy is all. (Internality = 2, Stability = 2, Globality = 2) | I call them and we talk on the phone.f When I’m lonely I call my [girlfriend] and we talk on the phone and we talk and she makes me feel better about it.f |
| Not enough friendsc | It’s because all my friends are other places and I can’t get there. (Internality = 3, Stability = 4, Globality = 3) | Write ’em letters and can call sometimesf |
| Not enough privacy/time to yourselfc | — [client] just wants attention so he comes to my room. (Internality = 2, Stability = 3, Globality = 1) | I tell him he can’t be in my room.f If he doesn’t leave, I tell staff and they make him go.f |
| When you are busy, people get in the way or interruptc | They don’t know no better. (Internality = 1, Stability = 6, Globality = 3) | Oh, I try to pretend they aren’t there.d Sometimes I tell — [boss] and she gets them to move.f |
| Went back on their wordb | They thought that I didn’t need a ride, but I really did need one. (Internality = 2, Stability = 1, Globality = 1) | We talked about it and got a plan. Now I’m going to get a ride on Mondays and Tuesdays.f |
Attribution ratings are based on a 7-point scale, with higher values meaning more Internal/Stable/Global ratings.
From the Inventory of Negative Social Interactions.
From the Lifestress Inventory.
Avoidant copy.
Noncoping.
Active coping.
Analyses were first conducted to compare the relative use of coping as opposed to noncoping efforts for stressful social interactions by the depressed and nondepressed groups. Figure 2 presents that relative percentage of responses coded as coping efforts in the depressed and nondepressed groups. The depressed group reported a significantly lower percentage of coping efforts than did the nondepressed group (Ms = 68.31, SD = 22.31, and 86.29, SD = 18.12, respectively), t(46) = −3.58, p = .001, d = −.88 (95% confidence interval −1.30 to −.45). Figure 2 also displays the relative percentage of coping efforts coded as active and avoidant coping strategies for the depressed and nondepressed groups. The depressed group reported significantly fewer active coping strategies than did the nondepressed group (Ms = 54.20, SD = 20.41, and 69.22, SD = 26.14, respectively), t(44) = 3.30, p = .001, d = −.64 (95% confidence interval −1.06 to −.21). The depressed group reported significantly more avoidant coping strategies than did the nondepressed group (Ms = 46.39, SD = 20.03, and 30.36, SD = 25.08, respectively), t(44) = −3.48, p = .001, d = .71 (95% confidence interval .27 to 1.13).
Figure 2.
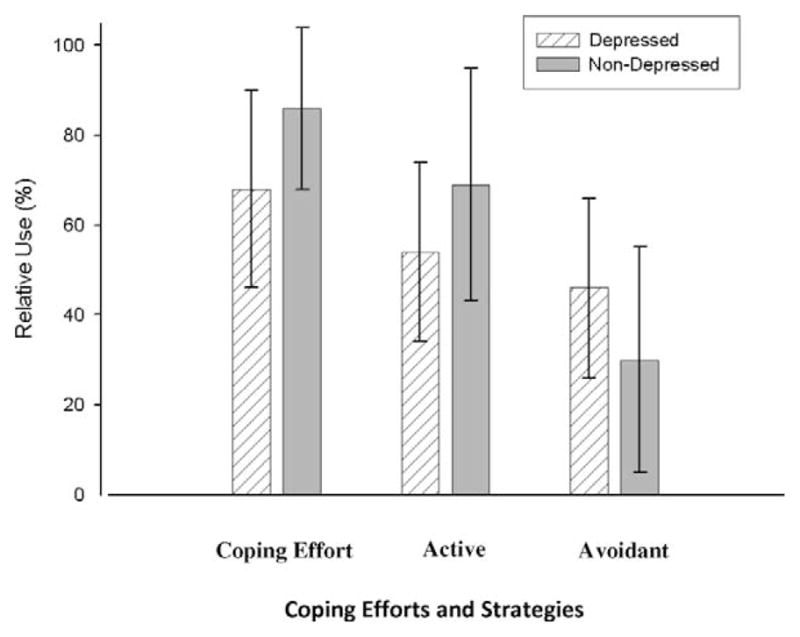
Relative percentage of responses coded as coping efforts and as active and avoidant coping strategies.
Discussion
Depressed persons in the general population experience a high rate of stressful social interactions, demonstrate a negative attribution style for these interactions, and use maladaptive coping strategies to deal with these interactions (Abraham et al., 1978; Daley et al., 1997; Hammen, 1991; Seligman et al., 1984). In this way, the experience of stressful social interactions is believed to maintain depression over time. The present study was designed to address the methodological limitations of previous studies to determine whether a clinical diagnosis of depression is related to a similar experience of stressful social interactions, negative causal attributions, and coping in adults with mild intellectual disability.
In this study, depressed adults with mild intellectual disability reported experiencing a greater frequency and stress impact of stressful social interactions than did nondepressed adults with mild intellectual disability matched on various subject characteristics. This confirms past studies (Hartley & MacLean, 2005; Lunsky & Benson, 2001; Lunsky & Havercamp, 1999; Nezu et al., 1995) and adds to the literature by showing that people who are diagnosed with a depressive disorder experience more frequent and severe interpersonal conflict than do nondepressed adults matched on age, gender, IQ, ethnicity, adaptive behavior, and living status. This suggests that the experience of stressful social interactions may serve to sustain depressed affect in an intellectual disability population as it is purported to do in the general population (Hammen, 1991; Joiner & Coyne, 1999).
As with the general population, cognitive and interpersonal deficits likely interact such that depressed adults with mild intellectual disability elicit negative interactions from their environment and are more aware of and sensitive to interpersonal criticism and rejection (Gotlib & Hammen, 1992; Joiner & Coyne, 1999; Joiner & Metalsky, 1995). The extent to which the heightened experience of stressful social interactions reported by depressed adults with mild intellectual disability reflects an actual increase in negative stressful social interactions versus dysfunctional cognitive processes cannot be determined in this study. Future researchers need to determine whether depressed adults with mild intellectual disability exhibit an increased self-focus and vigilance to criticism and rejection from others. Informant reports by people interacting with depressed adults with mild intellectual disability are also needed to determine the extent to which depressed adults elicit criticism and rejection from others and generate their own stressful social situations. An investigation of the specific interpersonal skill deficits (e.g., self-disclosure, reassurance seeking, and poor interpersonal problem-solving skills) contributing to this generation is also necessary.
Depressed adults with mild intellectual disability reported a more negative attribution style for stressful social interactions than did the matched nondepressed comparison group. This finding supports an earlier study by Esbensen and Benson (2006) conducted with adults who had mild intellectual disability using self-report measures developed for the general population. As in the general population (e.g., Abraham et al., 1978; Seligman et al., 1984), causal attributions for negative events are involved in depression among adults with mild intellectual disability. Further research is needed to determine whether other faulty cognitive patterns associated with depression in the general population are seen in depressed persons with intellectual disability. For instance, effortful information processing is impaired and biases in attention and memory are seen in depression in the general population (e.g., Gotlib et al., 2004). Research is needed to determine whether persons with intellectual disability experience similar information processing errors.
The finding that negative attribution styles are involved in depression among adults with mild intellectual disability suggests that cognitive techniques aimed at changing these faulty cognitive processes may be appropriate intervention strategies. Aside from medication, which is frequently prescribed for people with intellectual disability, behavioral therapies have primarily been used to manage psychiatric symptoms among people in this population (Grey & Hastings, 2005; Kiernan, Reeves, & Alborz, 1995). The possibility of cognitive–behavioral therapies (CBT) for psychopathology among adults with intellectual disability has been largely neglected (e.g., Stenfert-Kroese, 1997; Sturmey, 2004). CBT therapies may appear inappropriate for people with intellectual disability because they rely on complex cognitive skills, such as the ability to weigh evidence, recognize distortions in thinking, and identify more adaptive thoughts. Yet, a growing number of researchers have begun to adapt CBT techniques and teach adults with intellectual disability to understand connections between their affect, thoughts, and behavior (Dagnan, Chadwick, & Proudlove, 2000; Joyce, Globe, & Moody, 2006; Stenfert Kroese, 1997; Whitehouse, Tudway, Look, & Kroese, 2006). Preliminary studies suggest that CBT can be beneficial among people with intellectual disability when these training procedures and modifications are used (e.g., Clare & Murphy, 1998; Lindsay, Neilson, & Lawrenson, 1997; Taylor, 2002). Researchers will need to examine the feasibility and effectiveness of CBT techniques to challenge and modify negative causal attributions for stressful social interactions in an intellectual disability population.
Depressed adults with mild intellectual disability reported using fewer coping strategies (i.e., more noncoping efforts) than did the nondepressed group. Moreover, of the coping strategies generated, the depressed group reported fewer active coping strategies and more avoidant coping strategies for stressful social interactions than did nondepressed adults with mild intellectual disability. This result supports past findings among adults with intellectual disability (Hartley & MacLean, 2005) and research in the general population (Aldwin & Revenson, 1987; Endler & Parker, 1990) that depressed persons have difficulty generating adaptive coping efforts. Interventions aimed at helping depressed adults with mild intellectual disability utilize more active coping to deal with their experience of frequent and severe social conflict may be an important strategy for treating depression.
There are several limitations to this study. Several adults with mild intellectual disability in the depressed and nondepressed group had a non-depressive psychiatric disorder diagnosis reported by their disability service provider. The contribution of these comorbid psychiatric diagnoses to the findings is not known. Moreover, the experience of stressful social interactions among depressed adults with mild intellectual disability was examined at only one time point. This methodology does not permit an assessment of the time-order causal role of the experience of stressful social interactions, negative attributions, and mal-adaptive coping efforts in reinforcing or prolonging depressed affect. Future research in which investigators utilize a longitudinal methodology is required to better understand the likely bidirectional relations between cognitive and interpersonal problems and depression.
This study is also limited in that it provides a preliminary look at the active and avoidant coping efforts generated by depressed adults with mild intellectual disability through open-ended questions. Observational studies would help ensure that the coping strategies reported by depressed and nondepressed adults with mild intellectual disability are the coping strategies actually utilized in stressful social situations. In the present study we also examined a limited array of coping efforts. Further research is necessary to examine additional coping efforts found to be important in maintaining depression in the general population. For instance, research in the general population suggests that depressed persons often exhibit reassurance-seeking behaviors, in which they seek reassurance from others to reduce their perceptions of low self-worth, when faced with negative stressful events and that this strategy contributes to the generation of additional social conflict (Joiner & Metalsky, 1995; Joiner, Metalsky, Katz, & Beach, 1999). Further research is needed to investigate the importance of reassurance-seeking for maintaining negative affect and generating stressful social interactions among people with intellectual disability.
In summary, we found that depressed adults with mild intellectual disability experience more stressful social interactions, have a more negative attribution style for these interactions, and use more maladaptive coping strategies to deal with these interactions than do nondepressed adults with mild intellectual disability. These findings suggest that interpersonal behaviors, thinking styles, and problem-solving skills are important mechanisms through which depression is maintained in adults with mild intellectual disability. Interventions aimed at improving interpersonal functioning and challenging dysfunctional thought processes may be useful in treating depressed adults with mild intellectual disability. Moreover, coping interventions aimed at helping such adults better deal with stressful social interactions and the negative emotions that they evoke may also be important treatment strategies for depression.
Acknowledgments
This work was supported by a grant from the National Institutes of Health R03 MH 076124 to William MacLean, Jr. We are grateful to the participants and the following agencies for their continued support of our research: Circle C Resources; Envision-Creative Support for People with Developmental Disabilities; Goodwill Industries; Love, Care, & Dignity; Magic City Enterprises, Inc.; Mosaic; Mountain Regional Services, Inc.; and NOWCAP.
References
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory-based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Abramson LY, Seligman ME, Teasdale JD. Learned helplessness in humans: Critique and reformulation. Journal of Abnormal Psychology. 1978;87:49–74. [PubMed] [Google Scholar]
- Aldwin CM, Revenson TA. Does coping help? A reexamination of the relation between coping and mental health. Journal of Personality and Social Psychology. 1987;53:337–348. doi: 10.1037//0022-3514.53.2.337. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- Ayers TS, Sandler IN, Bernzweig JA, Harrison RJ, Wampler TW, Lustig LL. Handbook for the content analysis of children’s coping responses. Tempe: Arizona State University, Program for Prevention Research; 1989. [Google Scholar]
- Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale: A research report. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1981;22:73–88. doi: 10.1111/j.1469-7610.1981.tb00533.x. [DOI] [PubMed] [Google Scholar]
- Benson BA, Ivins J. Anger, depression, and self-concept in adults with mental retardation. Journal of Intellectual Disability Research. 1992;36:169–175. doi: 10.1111/j.1365-2788.1992.tb00492.x. [DOI] [PubMed] [Google Scholar]
- Borthwick-Duffy SA. Epidemiology and prevalence of psychopathology in people with mental retardation. Journal of Consulting and Clinical Psychology. 1994;62:17–27. doi: 10.1037//0022-006x.62.1.17. [DOI] [PubMed] [Google Scholar]
- Bramston P, Bostock J. Measuring stress in people with intellectual disabilities: The development of a new scale. Australian and New Zealand Journal of Developmental Disabilities. 1994;19:149–157. [Google Scholar]
- Bramston P, Fogarty G. Measuring stress in the mildly intellectually handicapped: The factorial structure of the Subjective Stress Scale. Research in Developmental Disabilities. 1995;16:117–131. doi: 10.1016/0891-4222(95)00003-8. [DOI] [PubMed] [Google Scholar]
- Clare IC, Murphy GH. Working with offenders or alleged offenders with intellectual disability. In: Emerson E, Hatton C, Bromley J, Caine A, editors. Clinical psychology and people with intellectual disabilities. New York: Wiley; 1998. pp. 154–176. [Google Scholar]
- Cooper SA, Bailey NM. Psychiatric disorders amongst adults with learning disabilities: Prevalence and relationship to ability level. Irish Journal of Psychological Medicine. 2001;18:45–53. doi: 10.1017/S0790966700006315. [DOI] [PubMed] [Google Scholar]
- Cooper SA, Smiley E, Morrison J, Williamson A, Allan L. An epidemiological investigation of affective disorders with a population-based cohort of 1023 adults with intellectual disabilities. Psychological Medicine. 2007;37:873–882. doi: 10.1017/S0033291707009968. [DOI] [PubMed] [Google Scholar]
- Dagnan D, Chadwick P, Proudlove J. Toward an assessment of suitability of people with mental retardation for cognitive therapy. Cognitive Therapy and Research. 2000;24:627–636. [Google Scholar]
- Dagnan D, Sandhu S. Social comparison, self-esteem, and depression in people with intellectual disability. Journal of Intellectual Disability Research. 1999;43:372–380. doi: 10.1046/j.1365-2788.1999.043005372.x. [DOI] [PubMed] [Google Scholar]
- Davila J, Hammen C, Burge D, Paley B, Daley SE. Poor interpersonal problem solving as a mechanism of stress generation in depression among adolescent women. Journal of Abnormal Psychology. 1995;104:592–600. doi: 10.1037//0021-843x.104.4.592. [DOI] [PubMed] [Google Scholar]
- Deb S, Thomas M, Bright C. Mental disorder in adults with intellectual disability I: Prevalence of functional psychiatric illness among a community-based population aged between 16 and 64 years. Journal of Intellectual Disability Research. 2001;45:495–505. doi: 10.1046/j.1365-2788.2001.00374.x. [DOI] [PubMed] [Google Scholar]
- Dunlop WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- Endler NS, Parker JDA. State and trait anxiety depression and coping styles. Australian Journal of Psychology. 1990;42:207–220. [Google Scholar]
- Esbensen AJ, Benson BA. Cognitive variables and depressed mood in adults with intellectual disability. Journal of Intellectual Disability Research. 2005;49:481–489. doi: 10.1111/j.1365-2788.2005.00710.x. [DOI] [PubMed] [Google Scholar]
- Esbensen AJ, Benson BA. Diathesis-stress and depressed mood among adults with mental retardation. American Journal on Mental Retardation. 2006;111:100–112. doi: 10.1352/0895-8017(2006)111[100:DADMAA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Felce D, Lowe K, Blackman D. Resident behavior and staff interaction with people with intellectual disabilities and seriously challenging behavior in residential services. Mental Handicap Research. 1995;8:272–295. [Google Scholar]
- Finlay WM, Lyons E. Acquiescence in interviews with people who have mental retardation. Mental Retardation. 2002;40:14–29. doi: 10.1352/0047-6765(2002)040<0014:AIIWPW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Firth J, Brewin C. Attributions and recovery from depression: A preliminary study using cross-lagged correlational analysis. British Journal of Clinical Psychology. 1982;21:229–230. doi: 10.1111/j.2044-8260.1982.tb00559.x. [DOI] [PubMed] [Google Scholar]
- Fogarty GJ, Bramston P, Cummins RA. Validation of the Lifestress Inventory for People With a Mild Intellectual Disability. Research in Developmental Disabilities. 1997;18:435–456. doi: 10.1016/s0891-4222(97)00021-8. [DOI] [PubMed] [Google Scholar]
- Glenn E, Bihm EM, Lammers WJ. Depression, anxiety, and relevant cognitions in persons with mental retardation. Journal of Autism and Developmental Disorders. 2003;33:69–76. doi: 10.1023/a:1022282521625. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Hammen CL. Psychological aspects of depression: Toward a cognitive-interpersonal integration. New York: Wiley; 1992. [Google Scholar]
- Gray MJ, Pumphrey E, Lombardo TW. The relationship between dispositional pessimistic attributional style versus trauma-specific attributions and PTSD symptoms. Journal of Anxiety Disorders. 2003;17:289–303. doi: 10.1016/s0887-6185(02)00205-0. [DOI] [PubMed] [Google Scholar]
- Grey IM, Hastings RP. Evidence-based practices in intellectual disability and behaviour disorders. Current Opinion in Psychiatry. 2005;18:469–475. doi: 10.1097/01.yco.0000179482.54767.cf. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Harrison P, Oakland R. Adaptive Behavior Assessment System. 2. San Antonio, TX: Harcourt Assessment; 2006. ABAS–II. [Google Scholar]
- Hartley SL, MacLean WE., Jr Perceptions of stress and coping strategies among adults with mild mental retardation: Insight into psychological adjustment. American Journal on Mental Retardation. 2005;110:285–297. doi: 10.1352/0895-8017(2005)110[285:POSACS]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Hartley SL, MacLean WE., Jr A review of the reliability and validity of Likert-type scales for people with intellectual disability. Journal of Intellectual Disability Research. 2006;50:813–827. doi: 10.1111/j.1365-2788.2006.00844.x. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH. Personal and contextual determinants of coping strategies. Journal of Personality and Social Psychology. 1987;52:946–955. doi: 10.1037//0022-3514.52.5.946. [DOI] [PubMed] [Google Scholar]
- Joiner T, Coyne J, editors. The interactional nature of depression: Advances in interpersonal approaches. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- Joiner TE, Jr, Metalsky GI. A prospective test of an integrative interpersonal theory of depression: A naturalistic study of college roommates. Journal of Personality and Social Psychology. 1995;69:778–788. doi: 10.1037//0022-3514.69.4.778. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr, Metalsky GI, Katz J, Beach S. Depression and excessive reassurance-seeking. Psychological Inquiry. 1999;10:269–278. [Google Scholar]
- Joyce T, Globe A, Moody C. Assessment of the component skills for cognitive therapy in adults with intellectual disability. Journal of Applied Research in Intellectual Disabilities. 2006;19:17–23. [Google Scholar]
- Kamen-Siegel L, Rodin J, Seligman ME, Dwyer J. Explanatory style and cell-mediated immunity in elderly men and women. Health Psychology. 1991;10:229–235. doi: 10.1037//0278-6133.10.4.229. [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. KBIT-2: Kaufman Brief Intelligence Test. 2. Shoreview, MN: American Guidance Service; 2004. [Google Scholar]
- Kiernan C, Reeves D, Alborz A. The use of anti-psychotic drugs with adults with learning disabilities and challenging behaviour. Journal of Intellectual Disability Research. 1995;39:264–274. doi: 10.1111/j.1365-2788.1995.tb00518.x. [DOI] [PubMed] [Google Scholar]
- Lakey B, Tardiff TA, Drew JB. Negative social interactions: Assessment and relations to social support, cognitions, and psychological distress. Journal of Social and Clinical Psychology. 1994;13:42–62. [Google Scholar]
- Lakin CK, Doljanic R, Taub S. Adults with dual diagnoses of intellectual and psychiatric disability receiving Medicaid home and community-based services (HCBS) and ICF/MR recipients in six states. Mental Health Aspects of Developmental Disabilities. 2007;10:78–90. [Google Scholar]
- Lindsay W, Neilson C, Lawrenson H. Cognitive-behaviour therapy for anxiety in people with learning disabilities. In: Stenfert Kroese B, Dagnan D, Loumidis K, editors. Cognitive-behaviour therapy for people with learning disabilities. New York: Brunner–Routledge; 1997. pp. 124–140. [Google Scholar]
- Linna SL, Moilanch I, Ebeling H, Piha J, Kumpulainenk K, Tumminen T, et al. Psychiatric symptoms in children with intellectual disability. European Child and Adolescent Psychiatry. 1999;8:77–82. doi: 10.1007/pl00010704. [DOI] [PubMed] [Google Scholar]
- Lunsky Y. Depressive symptoms in intellectual disability: Does gender play a role? Journal of Intellectual Disability Research. 2003;47:417–428. doi: 10.1046/j.1365-2788.2003.00516.x. [DOI] [PubMed] [Google Scholar]
- Lunsky Y, Benson BA. Association between perceived social support and strain, and positive and negative outcomes for adults with mild intellectual disability. Journal of Intellectual Disability Research. 2001;45:106–114. doi: 10.1046/j.1365-2788.2001.00334.x. [DOI] [PubMed] [Google Scholar]
- Lunsky Y, Bramston P. A preliminary study of perceived stress in adults with intellectual disabilities according to self-report and informant ratings. Journal of Intellectual and Developmental Disability. 2006;31:20–27. doi: 10.1080/13668250500488660. [DOI] [PubMed] [Google Scholar]
- Lunsky Y, Havercamp SM. Distinguishing low levels of social support and social strain: Implications for dual diagnosis. American Journal on Mental Retardation. 1999;104:200–204. doi: 10.1352/0895-8017(1999)104<0200:DLLOSI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Minnes P, Woodford L, Passey J. Mediators of wellbeing in ageing family carers of adults with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities. 2007;20:539–552. [Google Scholar]
- Moos RH. Life stressors, social resources, and the treatment of depression. In: Becker J, Kleinman A, editors. Psychosocial aspects of depression. Hillsdale, NJ: Erlbaum; 1991. pp. 187–214. [Google Scholar]
- Nezu CM, Nezu AM, Rothenberg JL, DelliCarpini L, Groag I. Depression in adults with mild mental retardation: Are cognitive variables involved? Cognitive Therapy and Research. 1995;19:227–239. [Google Scholar]
- Nolen-Hoeksema S, Girgus JS, Seligman ME. Learned helplessness in children: A longitudinal study of depression, achievement and explanatory style. Journal of Personality and Social Psychology. 1986;51:435–442. doi: 10.1037//0022-3514.51.2.435. [DOI] [PubMed] [Google Scholar]
- Program for Prevention Research. Manual for the Children’s Coping Strategies Checklist and the How I Coped Under Pressure Scale. Arizona State University; PO Box 876005, Tempe, AZ 85287–6005: 1999. [Google Scholar]
- Richards M, Maughan B, Hardy R, Hall I, Strydon A, Wadsworth M. Long-term affective disorders in people with mild learning disability. British Journal of Psychiatry. 2001;179:523–527. doi: 10.1192/bjp.179.6.523. [DOI] [PubMed] [Google Scholar]
- Robins CJ. Attributions and depression: Why is the literature so inconsistent? Journal of Personality and Social Psychology. 1988;54:880–889. doi: 10.1037//0022-3514.54.5.880. [DOI] [PubMed] [Google Scholar]
- Royal College of Psychiatrists. DC–LD [Diagnostic Criteria for Psychiatric Disorders for Use With Adults With Learning Disabilities/Mental Retardation] London: Gaskell Press; 2001. [Google Scholar]
- Sacco WP. A social-cognitive model of interpersonal processes in depression. In: Joiner T, Coyne JC, editors. Advances in interpersonal approaches: The interactional nature of depression. Washington DC: American Psychological Association; 1999. pp. 329–362. [Google Scholar]
- Schulman P, Castellon C, Seligman ME. Assessing explanatory style: The content analysis of verbatim explanations and the Attributional Style Questionnaire. Behaviour Research and Therapy. 1989;27:505–512. doi: 10.1016/0005-7967(89)90084-3. [DOI] [PubMed] [Google Scholar]
- Seligman MEP, Peterson C, Kaslow NJ, Tanenbaum RL, Alloy LB, Abrahmanson LY. Explanatory style and depressive symptoms among school children. Journal of Abnormal Psychology. 1984;93:235–238. doi: 10.1037//0021-843x.93.2.235. [DOI] [PubMed] [Google Scholar]
- Sigmon ST, Pells TJ, Schartel JG, Hermann BA, Edenfield TM, LaMattina SM, et al. Stress reactivity and coping in seasonal and nonseasonal depression. Behavior Research and Therapy. 2007;45:965–975. doi: 10.1016/j.brat.2006.07.016. [DOI] [PubMed] [Google Scholar]
- Smiley E, Cooper SA. Intellectual disability, depressive episode, diagnostic criteria and Diagnostic Criteria for Psychiatric Disorders for Use With Adults With Learning Disability/Mental Retardation (DC–LD) Journal of Intellectual Disability Research. 2003;47:62–71. doi: 10.1046/j.1365-2788.47.s1.26.x. [DOI] [PubMed] [Google Scholar]
- Stenfert-Kroese B. Cognitive-behaviour therapy for people with learning disabilities: Conceptual and contextual issues. In: Stenfert Kroese B, Dagnan D, Loumidis K, editors. Cognitive–behaviour therapy for people with learning disabilities. New York: Brunner-Routledge; 1997. pp. 1–15. [Google Scholar]
- Sturmey P. Cognitive therapy with people with intellectual disabilities: A selective review and critique. Clinical Psychology and Psychotherapy. 2004;11:222–232. [Google Scholar]
- Taylor JL. A review of assessment and treatment of anger in offenders with intellectual disabilities. Journal of Intellectual Disability Research. 2002;46:57–73. doi: 10.1046/j.1365-2788.2002.00005.x. [DOI] [PubMed] [Google Scholar]
- Wayment HA, Zetlin AG. Coping responses of adolescents with and without mild learning handicaps. Mental Retardation. 1989;27:311–316. [PubMed] [Google Scholar]
- Wegner D. Ironic processes of mental control. Psychological Review. 1994;101:34–52. doi: 10.1037/0033-295x.101.1.34. [DOI] [PubMed] [Google Scholar]
- Wegner DM, Wenzlaff RM. Mental control. In: Higgins ET, Kruglanski AW, editors. Social psychology: Handbook of basic principles. New York: Guilford; 1996. pp. 466–492. [Google Scholar]
- Whitehouse RM, Tudway JA, Look R, Kroese BS. Adapting individual psychotherapy for adults with intellectual disabilities: A comparative review of the cognitive-behaviour and psychodynamic literature. Journal of Applied Research in Intellectual Disabilities. 2006;19:55–65. [Google Scholar]


