Abstract
As long as a wound is infected, the healing process cannot begin. The indication for wound antiseptic is dependent on the interaction between the wound, the causative micro-organisms, and the host immune system. An uncritical colonisation is a condition whereby micro-organisms on a wound will proliferate, yet the immune system will not react excessively. Wound antiseptic is most often not necessary unless for epidemiologic reasons like colonisation with multi-resistant organisms. In most instances of a microbial contamination of the wound and colonisation, thorough cleaning will be sufficient.
Bacterial counts above 105 to 106 cfu per gram tissue (critical colonisation) might decrease wound healing due to release of toxins, particularly in chronic wounds. Traumatic and heavily contaminated wounds therefore will require anti-infective measures, in particular wound antiseptic. In such situations, even a single application of an antiseptic compound will significantly reduce the number of pathogens, and hence, the risk of infection. If a wound infection is clinically manifest, local antiseptics and systemic antibiotics are therapeutically indicated.
The prophylactic and therapeutic techniques for treatment of acute and chronic wounds (chemical antiseptics using xenobiotics or antibiotics, biological antiseptic applying maggots, medical honey or chitosan, physical antiseptic using water-filtered infrared A, UV, or electric current) mostly have been empirically developed without establishing a fundamental working hypothesis for their effectiveness.
The most important aspect in controlling a wound infection and achieving healing of a wound is meticulous debridement of necrotic material. This is achieved by surgical, enzymatic or biological means e.g. using maggots. However, none of these methods (with some exception for maggots) is totally gentle to vital tissue and particularly chemical methods possess cytotoxicity effects.
Derived from the general principles of antiseptic wound treatment, the following working hypothesis is postulated: the most ideal constellation for treatment of wounds is the superficial destruction of microbial layers without deep tissue alteration, like it is caused by antiseptics, in order not to endanger the regenerative granulation tissue. At the same time, it is desirable to support and increase cell proliferation and granulation capacities. These two aspects might be achieved by using low temperature plasma technology.
Abstract
Solange eine Wunde infiziert ist, kommt der Heilungsprozess nicht zum Abschluss. Die Indikation zur Wundantiseptik ist abhängig von der Wechselwirkung Wunde – Mikroorganismus – Wirt: Bei mikrobieller Kontamination bzw. Kolonisation ist die wirksame Reinigung der Wunde ausreichend. Bei größeren traumatischen kontaminierten Wunden kann durch einmalige präventive Antiseptik eine Reduzierung postoperativer Infektionen erreicht werden. Bei unkritischer Kolonisation handelt es sich um die Vermehrung von auf die Wunde gelangten Erregern ohne klinische Wirtsreaktion. Auch hier ist keine Antiseptik erforderlich, außer aus epidemiologischer Indikation (multiresistente Erreger).
Bakterienzahlen in der Wunde >105-106 KBE/g hemmen die Wundheilung durch Toxinfreisetzung (kritische Kolonisation) speziell bei chronischen Wunden bis zum Stillstand der Heilung. Hier ist eine „milde Antiseptik“ mit gleichzeitiger Endotoxinabsorption oder -inaktivierung indiziert. Bei klinisch manifester Infektion mit lokaler und/oder systemischer Wirtsreaktion (Sepsis) ist die therapeutische Anwendung von Antiseptika indiziert, andernfalls kommt zur Defektheilung und im ungünstigen Fall zur Sepsis.
Die Verfahren zur antiseptischen Behandlung akuter und chronischer Wunden (chemische Antiseptik mit Xenobiotika oder Antibiotika, biologische Antiseptik mit Maden, Bienenhonig oder Chitosan, physikalische Antiseptik mit wIRA, UV, Elektrostimulation) wurden empirisch ohne Zugrundelegung einer übergeordneten Arbeitshypothese eingeführt.
Voraussetzung für die Wundheilung und Beherrschung einer Wundinfektion ist das effektive Debridement. Dieses erfolgt chirurgisch, enzymatisch oder mittels Maden. Zur Erregerinaktivierung werden chemische oder biologische Antiseptika sowie physikalische Verfahren eingesetzt. Diesen Verfahren gemeinsam ist eine mehr oder weniger ausgeprägte Zytotoxizität.
Aus der Verallgemeinerung der Wirkprinzipien zur antiseptischen Wundbehandlung wird folgende Arbeitshypothese abgeleitet: Die ideale Konstellation zur Wundbehandlung ist die oberflächliche Zerstörung des mikrobiellen Biofilms auf der Wunde ohne antiseptische Tiefenwirkung, um das sich regenerierende Gewebe nicht zu hemmen. Gleichzeitig soll durch das Behandlungsprinzip die Wundheilung (Zellproliferation, Granulozytenleistung) im sich regenerierenden Gewebe stimuliert werden. Niedertemperaturplasma soll so konfiguriert werden, dass es die Anforderungen der Arbeitshypothese erfüllt.
Introduction
The adverse effects of bacterial contamination and in particular infection on wound healing are well known [1], [2], [3], [4], [5]. First descriptions of infection and inflammation and empirical local antiseptic therapies date back to ancient times. Today, much is known about the mechanisms of wound healing and infection, but the actual options for antiseptic treatment of acute and especially chronic problem wounds within the concept for wound treatment are purely empirical. The consequence is the absence of a fundamental working hypothesis for effectiveness and risks of antiseptics and the lack of evidence based integration of wound antisepsis into wound therapy standards.
Therefore, today we are facing a situation with an ever increasing number of options but without a common system to access their effectiveness, which leads to a polypragmasia in the therapy of infected wounds. This article will discuss the accepted principles in wound therapy and summarises conclusions drawn from the perspectives of low temperature plasma technology.
Basic principles of wound therapy: algorithm of therapeutic steps
The basic principle of wound therapy is to create and maintain an optimal situation for wound healing. This involves the absence of infection or critical microbial contamination and (hyper)-inflammation, includes optimal perfusion, oxygenation and nutrition, protection from internal (necrotic material, debris, toxins) and external (mechanical, chemical, physical) irritations and an optimal “climate” (humidity, temperature) for the regenerating tissue (milieu of moist wound healing).
Currently, there is no single wound treatment available addressing all these factors at the same time. Therapies differ in the number of aspects they deal with simultaneously and in their effect/side effect ratio or damage they do to the wound. Therefore, therapies should not only be rated by their effect on a specific aspect, but by their overall impact on wound healing. Furthermore, a strict division of therapies in terms of aspects they deal with is impossible.
Each wound needs the same algorithm of therapy with the following steps:
cleansing
debridement
antisepsis if wound infected
elimination of wound inhibiting healing factors
stimulation of wound healing especially important for chronic wounds
moist wound healing for secondarily healing traumatic or chronic wounds by suitable wound dressings
First step: Debridement
The first main aspect to achieve healing indisputably is meticulous debridement of necrotic tissue [6], [7]. Necrotic tissue impairs wound healing in many ways: It detains the building of granulation tissue, becomes easily colonised with micro-organisms and maintains inflammation by liberating cellular debris and toxins from dead cells. Debridement is achieved by surgical, physical, enzymatic or biological means, e.g., using maggots. However, none of these methods (with some exception for maggot therapy) is absolutely gentle to non-necrotic tissue and particularly enzymatic methods possess cytotoxic effects combined with increased infection risk.
After surgical debridement the use of low temperature plasma could be a new option for fine-tuning the debridement by detachment of the non-visible part of necrotic tissue connected with inactivation of released toxins by necrotic cells as well as by bacteria.
Second step: Cleansing and optional antisepsis
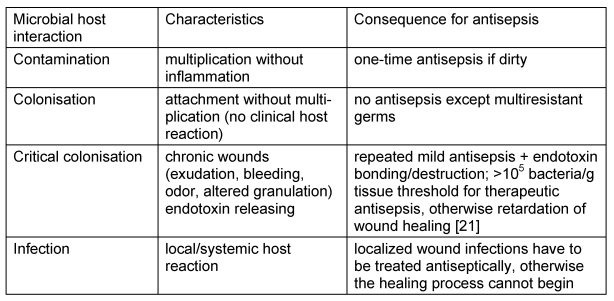
Mechanical cleansing by rinsing is important for wound healing, because factors like dirt, bacteria, toxins, and dead cells, which impair wound closure, must be removed [8]. In case of infection risk, the control of microbiological colonisation or infection, respectively, of the wound is necessary, because the infected wound cannot heal (Table 1 (Tab. 1)). After cleansing and antisepsis, the recontamination of the healing wound must be prevented.
Table 1. Bacteria and wound healing.
Pertaining to the first aspect, antisepsis is the method of choice, whereas the wound protection is realized by mechanical protection (wound dressing).
The indication of wound antisepsis depends upon the interaction between microorganism and host. Bacterial counts above 105 to 106 cfu per gram tissue (so-called critical colonisation) might decrease wound healing due to release of toxins, particularly in chronic wounds. In this situation and for dirty traumatic as well as infected wounds antiseptic treatment is indicated (Table 1 (Tab. 1)).
Antiseptics should be used only after careful risk benefit assessment; otherwise impaired wound healing can result. The following indications are commonly accepted [9]:
dirty, contaminated injuries incl. bite-, cut-, shot wounds and high soft tissue trauma
clinically infected acute or chronic wounds
burns
surgically opened abscesses and phlegmons
intra-operative wound contamination wound colonisation with multi-resistant bacteria (i.e. MRSA, VRE)
Optional indications are:
rinsing of the prepared area before alloplastic implantation
final antiseptic rinsing after long time surgical interventions with large opened areas before wound closure
once antisepsis after excision of chronically inflamed foci
No indications for wound antisepsis are:
aseptic wound conditions
non-critical wound colonization
dried surgical wounds (2nd postoperative day)
uncomplicated healing of trivial wounds
after mesh-graft transplants, respectively, fresh skin graft
Except for infected acute or chronic wounds and burns, a single application of a wound antiseptic is in most cases sufficiently effective and will significantly reduce the number of pathogens, and hence, the risk of infection [10].
If there are no signs for systemic infections, antiseptic therapy is to be used, because modern antiseptics do not have systemic side effects and do not lead to antimicrobial resistance. But in situations, when the clinically manifested wound infection is associated with systemic spread of infection, antisepsis and antibiosis are indicated parallel.
Antiseptic agents: Options for local antiseptic therapy are mainly xenobiotic agents. The ideal antiseptic should be strong enough to kill bacteria within an adequate exposure time without harming host cells and tissues. Nowadays, highly effective xenobiotic agents with low toxic or irritative potential are available [11], [12].
To calculate the difference between microbicidal activity and cytotoxicity, the combined assessment of cytotoxicity and antimicrobial activity allows the assessment of appropriate dilution of antiseptic agents, which is both biocompatible to host tissue and effective against bacteria. The resulting dimensionless so-called biocompatibility index (BI) is the ratio of the concentration at which 50% of murine fibroblasts are damaged, and the microbicidal effect, i.e., the concentration at which the baseline burden of the test microorganisms is reduced by at least 3 log (99.9%). Under the present normally used antiseptics only polihexanide and octenidine have a BI>1, for triclosan, chlorhexidin, PVP iodine and silver compounds the BI is <1 [13], [14]. Therefore, only polihexanide and octenidine are of further scientific and practical interest (Table 2 (Tab. 2)).
Table 2. Characteristics of octenidin and polihexanide.
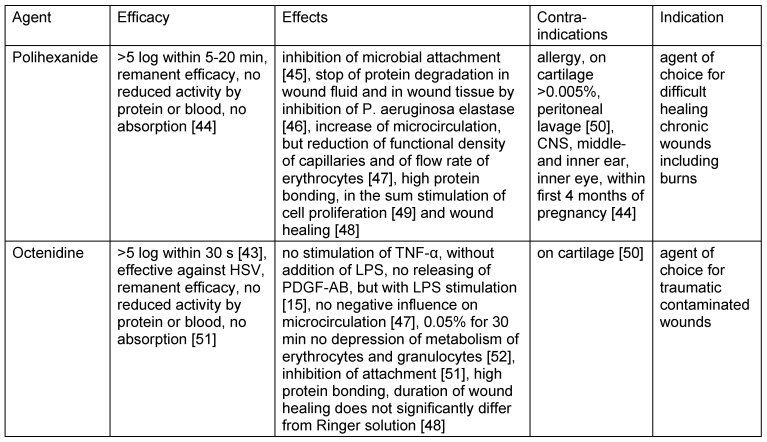
The efficacy and safety of polihexanide and octenidine was shown in numerous studies [10], [15], [16], [17], [18], [19], [20].
Physical methods for wound therapy
To control the microbial burden of wounds it can distinguish between methods with indirect or direct antimicrobial efficacy [21].
The constant decontamination by vacuum dressing generates a mechanical wound cleansing [22].
At any investigated time, the amount of colonisation under therapy with water-filtered infrared-A (wIRA) in combination with visible light (VIS) was lesser compared with the group using wIRA+VIS+dexpanthenol cream, which was interpreted as more suppression of the flora due to the stimulation of wound healing by wIRA. wIRA produces a therapeutically usable field of heat in the tissue and increases tissue temperature, tissue oxygen partial pressure, and tissue perfusion. These three factors are decisive for a sufficient tissue supply with energy and oxygen and, consequently, also for wound healing and infection defence by attraction of macrophages, activation of phagocytosis, etc. wIRA can considerably alleviate pain, diminish elevated wound exudation and inflammation, and also show positive immunomodulatory effects [23], [24].
In addition to reduction of oedema, stimulation of wound clearance by attraction of macrophages, neutrophilic granulocytes, reduction of mast cells, acidifying, stimulation of epithelisation, increase of neogenenesis of capillaries, oxygen- and energy supply as well as stimulation of proliferation of fibroblasts and synthesis of collagen, electric stimulation is direct microbicidal effective [25]. The sum results show an increased healing capacity, which is demonstrated for chronic wounds as well as for skin transplants and myocutaneous flaps [26], [27].
Consequences for usability of low temperature plasma: Low temperature plasma is microbicidal active [28] and could be a valuable addition for wound treatment, because it can be specifically targeted on the superficial layers of the wound and on attached micro-organisms and microbial bio-films without a negative effect on the deeper layers of vital and regenerating tissue.
Natural agents
Recently, natural agents such as medical honey or chitosan and the so-called bio-surgery with maggots have become increasingly interesting.
Medical honey is microbicidal as effective as xenobiotic antiseptics and is also effective against HSV [29], [30]. The mode of action causes a non-invasive debridement of avitalic parts of the wound by its osmolarity, production of H202 in a non-cytotoxic concentration by glucose oxidase and other unidentified components [30], [31], [32], [33], [34]. Indications are herpes labialis (same efficacy as acyclovir without resistance development), high immuno-suppressed patients with chemotherapy induced disturbance of wound healing, infected wounds of newborns, by irradiation induced mucositis and 2nd degree burns [35], [36], [37] .
Chitosan is the deacetylated compound of chitin [38] and can be extracted from the shells of aquatic animals (crabs, shrimps). The amino group in the C-2 position of the cationic glucosamine provides its antimicrobial activity [39], [40] by binding to the bacterial cells [41]. Chitosan shows only bacteriostatic activity [42]. From the theoretical point of view, heavily contaminated wounds would benefit from an early renewal of the wound dressing.
Third step: Control of inflammation and stimulation of wound healing
The third main aspect in wound therapy is the control of inflammation and the maintenance of an optimal “climate” (humidity, temperature), perfusion, oxygenation and nutrition for the regenerating tissue. The so-called moist wound healing is identified as essential factor for the healing process and can realise by modern wound dressings.
No single therapy can address all these factors. Beside efforts to optimise systemic factors and diseases (e.g. metabolic diseases like diabetes mellitus) and regional factors (e.g. peripheral arterial disease), local therapies are of great importance. These therapies cover pharmaceutical and immunological therapies (e.g., anti-inflammatory therapies, special dressings) as well as physical therapies.
Derived hypothesis for the use of low temperature plasma
Wound healing is an extremely energy exhausting process. Physical therapies, especially wIRA aim to warm tissue with low thermal load to the skin surface. Warming improves capillary circulation with increased oxygen supply and leads secondarily to an accelerated metabolism and faster regeneration. While wIRA consists of a broad spectral range and effects are summation effects, low temperature plasma is much more controllable and is expected to be much more adaptable to the individual wound and stage of regeneration.
Electric stimulation controls the inflammation and stimulates the wound healing and even the regeneration of damaged nervous cells. Low temperature plasma possesses electrical activity, which can support the wound healing, comparable with electric stimulation.
The first step of wound therapy, the debridement, can support by low temperature plasma, because the superficial layer of the wound together with attached micro-organisms and microbial bio-films will be detached. On the other hand, low temperature plasma acts antiseptically, which can be used for antiseptic treatment of dirty, critical colonised and infected wounds.
In conclusion, we postulate the following working hypothesis for general principles of wound treatment:
The first step is the surgical debridement, supported by superficial destruction and detachment of attached micro-organisms.
The critically colonised (microbial bio-film) or infected wound can be antiseptically treated with low temperature plasma combined with degradation of bacterial endotoxins.
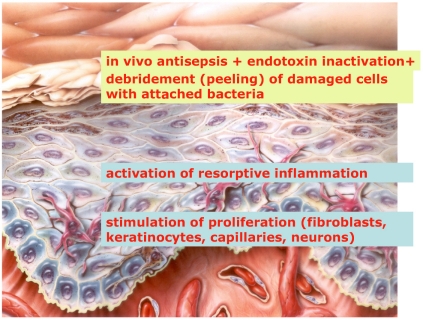
By configuration of the low temperature plasma, it is possible that the plasma penetrates only into the superficial layer of the wound without any toxic effects on deeper layers of regenerative granulation tissue, and the reduced energy in the deeper layers can regulate inflammation on a reparative level and support cell proliferation and cell functions (phagocytosis, releasing of growth factors) with the consequence of stimulation on wound healing. No current treatment covers all these requirements and most therapies deal only with a limited number of aspects of wound healing (Figure 1 (Fig. 1)).
Figure 1. Targets for plasma wound therapy.
Of course, the thorough risk benefit assessment of plasma wound therapy with low temperature plasma must be performed with the following main points:
analysis of stability of produced radicals, exclusion of their penetration into living tissue
limited stimulation of proliferation with exclusion of mutagenic or carcinogenic potency (one marker is the missing induction of metallo-proteinases)
no induction of apoptotic processes
Low temperature plasma could be, as shown above, an innovative, well controllable approach for wound treatment with a broad range of positive effects and very limited side effects.
References
- 1.Kramer A, Heeg P, Harke HP, Rudolph H, Koch S, Jülich WD, Hingst V, Merka V, Lippert H. Wundantiseptik. In: Kramer A, Gröschel D, Heeg P, Hingst V, Lippert H, Rotter M, Weuffen W, editors. Klinische Antiseptik. 1993. [Google Scholar]
- 2.Assadian O, Kramer A, Piatek S, Schulz H-U, Tautenhahn J. Lokalbehandlung sekundär heilender Wunden. In: Lippert H, editor. Wundatlas. 2. Aufl. Stuttgart: Thieme; 2006. [Google Scholar]
- 3.Assadian O, Kramer A. Wundinfektionen. In: Lippert H, editor. Wundatlas. 2. Aufl. Stuttgart: Thieme; 2006. [Google Scholar]
- 4.Assadian O, Kramer A. Wundantiseptik. In: Lippert H, editor. Wundatlas. 2. Aufl. Stuttgart: Thieme; 2006. [Google Scholar]
- 5.Kramer A, Assadian O, Müller G, Brauer V, Stier A, Hübner NO. Aktuelle Erkentnisse zu Indikationen und zur Auswahl von Mitteln bzw. Verfahren zur Wundantiseptik. In: Eikmann T, Christiansen B, Exner M, Herr C, Kramer A, editors. Hygiene in Krankenhaus und Praxis. (Loseblattsammlung. 5. Ergänzungslieferung) Landsberg: Ecomed Medizin; 2007. [Google Scholar]
- 6.Baharestani M. The clinical relevance of debridement. In: Baharestani M, Goltrup F, Holstein P, Vanscheidt W, editors. The Clinical Relevance of Debridement. Berlin: Springer; 1999. [Google Scholar]
- 7.Eisenbeiß W. Therapie der infizierten Verbrennungswunde. GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc64. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000097.shtml. [Google Scholar]
- 8.Hübner NO, Assadian O, Müller G, Kramer A. Anforderungen an die Wundereinigung mit Wasser. GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc61. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000094.shtml. [Google Scholar]
- 9.Hübner NO, Assadian O, Kramer A. Indikationen zur Wundantiseptik. GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc60. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000093.shtml. [Google Scholar]
- 10.Roth B, Assadian O, Wurmitzer F, Kramer A. Wundinfektionen nach antiseptischer Primärversorgung kontaminierter traumatischer Wunden mit Polihexanid, PVP-Iod bzw. Wasserstoffperoxid. GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc58. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000091.shtml. [Google Scholar]
- 11.Kramer A, Daeschlein G, Kammerlander G, Andriessen A, Aspöck C, Bergemann R, Eberlein T, Gerngross H, Görtz G, Heeg P, Jünger M, Koch S, König B, Laun R, Peter RU, Roth B, Ruef Ch, Sellmer W, Wewalka G, Eisenbeiß W. Konsensusempfehlung zur Auswahl von Wirkstoffen für die Wundantiseptik. Hyg Med. 2004;5:147-57. ZfW. 3:110–120. [Google Scholar]
- 12.Kramer A, Assadian O, Hrsg . Wallhäußers Praxis der Sterilisation, Desinfektion, Antiseptik und Konservierung. In: Kramer A, Assadian O, editors. Qualitätssicherung der Hygiene in medizinischen und industriellen Bereichen. Stuttgart: Thieme; 2008. [Google Scholar]
- 13.Müller G, Kramer A, Karkour Y. Biokompatibilitätsindex silberhaltiger Wundantiseptika. GMS Krankenhaushyg Interdiszip. 2006;1(1):Doc31. Available from: http://www.egms.de/en/journals/dgkh/2006-1/dgkh000031.shtml. [Google Scholar]
- 14.Müller G, Kramer A. Biocompatibilty index of antiseptic agents by parallel assessment of antimicrobial activity and cellular cytotoxicity. JAC. doi: 10.1093/jac/dkn125. [DOI] [PubMed] [Google Scholar]
- 15.Menke H, Pelzer M, Raff T, Siebert J, Germann G. Ein neues lokales Antiseptikum zur Oberflächenbehandlung bei Schwerstverbrannten. Akt Traumotol. 2001;31:211–215. [Google Scholar]
- 16.Daeschlein G, Assadian O, Bruck JC, Meinl C, Kramer A, Koch S. Feasibility and clinical applicability of polihexanide for treatment of second-degree burn wounds. Skin Pharmacol Physiol. 2007;20:292–296. doi: 10.1159/000107577. [DOI] [PubMed] [Google Scholar]
- 17.Vanscheidt W, Baur M, May TW, Siebert J. Beeinflussung der Wundheilung bei chronischen Beinulzera durch ein lokales Octenidin-dihydrochloridhaltiges Wundantiseptikum. Hyg Med. 2005;30(5):153–158. [Google Scholar]
- 18.Mulder GD, Cavorsi JP, Lee DK. Feature: Polyhexamethylene Biguanide (PHMB): An addendum to current topical antimicrobials. Wounds. 2007;19(7):173–182. [PubMed] [Google Scholar]
- 19.Behrens-Baumann W, Kramer A. Anti-Infectives against Amebic Keratitis. In: Kramer A, Behrens-Baumann W, editors. Antiseptic Prophylaxis and Therapy in Ocular Infections. Principles, Clinical Practice and Infection Control. Basel: Karger; 2002. pp. 297–303. [Google Scholar]
- 20.Wiedmann M, Hagendorff A, Bohm R, Schulz T, Mossner J. Caca K. Malignant oesophago-pleuro-pericardial fistula in a patient with oesophageal carcinoma. Z Kardiol. 2005;94(6):411–414. doi: 10.1007/s00392-005-0235-0. [DOI] [PubMed] [Google Scholar]
- 21.Drosou A, Falabella A, Kirsner RS. Antiseptics on wounds: an area of controversy. Wounds. 2003;15(5):149–166. [Google Scholar]
- 22.Fleischmann W. Die V.A.C.-Instill zur Behandlung der akuten Wundinfektion. GMS Krankenhaushyg Interdiszip. 2006;1(1):Doc28. Available from: http://www.egms.de/en/journals/dgkh/2006-1/dgkh000028.shtml. [Google Scholar]
- 23.Hoffmann G. Principles and working mechanisms of water-filtered infrared-A (wIRA) in relation to wound healing. GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc54. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000087.shtml. [PMC free article] [PubMed] [Google Scholar]
- 24.Hartel M, Illing P, Mercer JB, Lademann J, Daeschlein G, Hoffmann G. Therapy of acute wounds with water-filtered infrared-A (wIRA) GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc53. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000086.shtml. [PMC free article] [PubMed] [Google Scholar]
- 25.Daeschlein G, Assadian O, Kloth LC, Meinl C, Ney F, Kramer A. Antibacterial activity of positive and negative polarity low-voltage pulsed current (LVPC) on six typical Gram-positive and Gram-negative bacterial pathogens of chronic wounds. Wound Repair Regen. 2007;15(3):399–403. doi: 10.1111/j.1524-475X.2007.00242.x. [DOI] [PubMed] [Google Scholar]
- 26.Kloth LC. Electrical stimulation for wound healing: a review of evidence from in vitro studies, animal experiments, and clinical trials. Int J Low Extrem Wounds. 2005;4(1):23–44. doi: 10.1177/1534734605275733. [DOI] [PubMed] [Google Scholar]
- 27.Bayat M, Asgari-Moghadam Z, Maroufi M, Rezaie FS, Bayat M, Rakhshan M. Experimental wound healing using microamperage electrical stimulation in rabbits. J Rehabil Res Dev. 2006;43(2):219–226. doi: 10.1682/jrrd.2005.05.0089. [DOI] [PubMed] [Google Scholar]
- 28.Brandenburg R, Ehlbeck J, Stieber M, von Woedtke T, Zeymer J, Schluter O, Weltmann KD. Antimicrobial treatment of heat sensitive materials by means of atmospheric pressure rf-driven plasma jet. Contrib Plasma Phys. 2007;47(1-2):72–79. [Google Scholar]
- 29.Cooper R. Honey in wound care: antibacterial properties. GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc51. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000084.shtml. [PMC free article] [PubMed] [Google Scholar]
- 30.Igelbrink D, Koburger T, Simon A, Kramer A. Mikrobiozide Wirksamkeit von Medihoney™. GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc50. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000083.shtml. [Google Scholar]
- 31.Brudzynski K. Effect of hydrogen peroxide on antibacterial activities of Canadian honeys. J Microbiol. 2006;52(12):1228–1237. doi: 10.1139/w06-086. [DOI] [PubMed] [Google Scholar]
- 32.Al-Waili NS. Investigating the antimicrobial activity of natural honey and its effects on the pathogenic bacterial infections of surgical wounds and conjunctiva. J Med Food. 2004;7(2):210–222. doi: 10.1089/1096620041224139. [DOI] [PubMed] [Google Scholar]
- 33.Al-Waili NS, Akmal M, Al-Waili FS, Saloom KY, Ali A. The antimicrobial potential of honey from United Arab Emirates on some microbial isolates. Med Sci Monit. 2005;11(12):BR433–BR438. [PubMed] [Google Scholar]
- 34.Mercan N, Guvensen A, Celik A, Katircioglu H. Antimicrobial activity and pollen composition of honey samples collected from different provinces in Turkey. Nat Prod Res. 2007;21(3):187–195. doi: 10.1080/14786410600906277. [DOI] [PubMed] [Google Scholar]
- 35.Mphande AN, Killowe C, Phalira S, Jones HW, Harrison WJ. Effects of honey and sugar dressings on wound healing. J Wound Care. 2007;16(7):317–319. doi: 10.12968/jowc.2007.16.7.27053. [DOI] [PubMed] [Google Scholar]
- 36.Simon A. Medihoney. In: Kramer A, Assadian O, editors. Wallhäußers Praxis der Sterilisation, Desinfektion, Antiseptik und Konservierung. Stuttgart: Thieme; 2008. [Google Scholar]
- 37.Simon A, Sofka K, Wiszniewsky G, Blaser G, Bode U, Fleischhack G. Wound care with antibacterial honey (Medihoney) in pediatric hematology-oncology. Support Care Cancer. 2006;14:91–97. doi: 10.1007/s00520-005-0874-8. [DOI] [PubMed] [Google Scholar]
- 38.Lim SH, Hudson SM. Synthesis and antimicrobial activity of a water-soluble chitosan derivative with a fiber-reactive group. Carbohydr Res. 2004;339(2):313–319. doi: 10.1016/j.carres.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 39.Chen YM, Chung YC, Wang LW, Chen KT, Li SY. Antibacterial properties of chitosan in waterborne pathogen. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2002;37:71379–71390. doi: 10.1081/ese-120005993. [DOI] [PubMed] [Google Scholar]
- 40.Al-Bahra MM. Darstellung von Chitinderivaten zur antimikrobiellen Ausrüstung von Textilien [Diss.] Rheinisch-Westfälische Technische Hochschule Aachen; 2004. [Google Scholar]
- 41.Takai K, Ohtsuka T, Senda Y, Nakao M, Yamamoto K, Matsuoka J, Hirai Y. Antibacterial properties of antimicrobial-finished textile products. Microbiol Immunol. 2002;46(2):75–81. doi: 10.1111/j.1348-0421.2002.tb02661.x. [DOI] [PubMed] [Google Scholar]
- 42.Heisig P, Claußen T, Mayer G. Nachweis der antibakteriellen Aktivität von Chitosan. GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc39. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000072.shtml. [Google Scholar]
- 43.Pitten FA, Werner HP, Kramer A. A standardized test to assess the impact of different organic challenges on the antimicrobial activity of antiseptics. J Hosp Infect. 2003;55(2):108–115. doi: 10.1016/s0195-6701(03)00260-3. [DOI] [PubMed] [Google Scholar]
- 44.Kramer A, Roth B. Polihexanid. In: Kramer A, Assadian O, editors. Wallhäußers Praxis der Sterilisation, Desinfektion, Antiseptik und Konservierung. Stuttgart: Thieme; 2008. [Google Scholar]
- 45.Rosin M, Welk A, Bernhardt O, Ruhnau M, Pitten FA, Kocher T, Kramer A. Effect of a polyhexamethylene biguanide mouthrinse on bacterial counts and plaque. J Clin Periodontol. 2001;28(12):1121–1126. doi: 10.1034/j.1600-051x.2001.281206.x. [DOI] [PubMed] [Google Scholar]
- 46.Schmidtchen A, Davoudi M, Andersson E. Abstracts 13th Conf Europ Wound Manag Assoc. Pisa. 2003. Potent antibacterial effects of polyhexamethylenebbiguanide on common chronic ulcer-derived bacteria; p. 70. [Google Scholar]
- 47.Langer S, Sedigh Salakdeh M, Goertz O, Steinau HU, et al. The impact of topical antiseptics on skin microcirculation. Europ J Med Res. 2004;9(9):449–454. [PubMed] [Google Scholar]
- 48.Kramer A, Roth B, Müller G, Rudolph P, Klöcker N. Influence of the antiseptic agents polihexanide and octenidine on FL-cells and on healing of experimental superficial aseptic wounds in piglets. A double-blind, randomised, stratified, controlled, parallel-group study. Skin Pharmacol Physiol. 2004;17:141–146. doi: 10.1159/000077241. [DOI] [PubMed] [Google Scholar]
- 49.Wiegand C, Abel M, Kramer A, Müller G, Ruth P, Hipler UC. Proliferationsförderung und Biokompatibilität von Polihexanid. GMS Krankenhaushyg Interdiszip. 2007;2(2):Doc43. Available from: http://www.egms.de/en/journals/dgkh/2007-2/dgkh000076.shtml. [Google Scholar]
- 50.Müller G, Kramer A. Effect of selected wound antiseptics on adult articular cartilage (bovine sesamoid bone) in the presence of Escherichia coli and Staphylococcus aureus. J Orthop Res. 2005;23:127–133. doi: 10.1016/j.orthres.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 51.Kramer A, Müller G. Octenidindihydrochlorid. In: Kramer A, Assadian O, editors. Wallhäußers Praxis der Sterilisation, Desinfektion, Antiseptik und Konservierung. Stuttgart: Thieme; 2008. [Google Scholar]
- 52.Wagner KH, Jurss A, Zarembach B, Elmadfa I. Impact of antiseptics on radical metabolism, antioxidant status and genotoxic stress in blood cells: povidone-iodine versus octenidine dihydrochloride. Toxicol In Vitro. 2004;18(4):411–418. doi: 10.1016/j.tiv.2003.12.001. [DOI] [PubMed] [Google Scholar]