Abstract
Bovine serum albumin (BSA), which is present in bovine plasma, is one of the major allergens affecting patients with food allergies induced by milk and meat. It is also commonly used in research laboratories. Although some reports have documented food allergies associated with BSA, BSA-induced occupational asthma has not been reported. We report a case of occupational asthma and rhinitis in a laboratory worker caused by the inhalation of BSA powder, in which an IgE-mediated response was suggested as the pathogenic mechanism.
Keywords: occupational asthma, bovine serum albumin (BSA), milk allergy
INTRODUCTION
Occupational asthma is a respiratory disease characterized by bronchial hyper-reactivity caused by specific agents inhaled during work.1 Although the inhalation of various substances, such as animal dander and some chemicals, has been implicated in the etiology of occupational asthma,1 occupational asthma induced by the inhalation of bovine serum albumin (BSA) powder has not been reported. BSA, a protein purified from bovine blood, is commonly used for enzyme-linked immunosorbent assays (ELISA), immunoblotting, and immunohistochemistry in research laboratories.2 This is the first case of occupational asthma and rhinitis caused by the inhalation of BSA powder that has been confirmed by an inhalation challenge test and immunologic studies.
CASE REPORT
A 25-yr-old nonsmoking male who suffered from mild seasonal allergic rhinitis from childhood had been employed as a laboratory researcher for 1 yr. Although he had worked in a laboratory for 4 yr when he was a university student, he did not notice any allergy symptoms. Five months earlier, when the patient was directly exposed to 100% BSA powder in the workplace, he suddenly developed rhinorrhea, nasal itching, nasal obstruction, and chest discomfort, which improved when he worked far from the BSA power. Subsequently, he began to experience laryngeal swelling, abdominal pain, and diarrhea after drinking milk, but never experienced any other food allergies, including meat allergies.
At presentation, the blood differential count, serum biochemistry, and chest radiograph were normal. He refused skin prick testing. The serum total IgE was 314 KU/L (range 0-114 KU/L). Serum specific IgE levels for common inhalant allergens and milk measured using ImmunoCAP (Pharmacia-Upjohn, Uppsala, Sweden) showed 7.49 KU/L for Dermatophagoides pteronyssinus, 8.03 KU/L for D. farinae, negative results for alder, ragweed, and mugwort pollens, and 14.60 KU/L for milk. Lung function was normal; the forced expiratory volume in one second (FEV1) was 3.75 L, 86.93% of predicted, but the threshold of methacholine producing a 20% decrease in the FEV1 was 10 mg/mL.
The clinical history suggested that he had occupational asthma and rhinitis resulting from the inhalation of BSA powder, and milk allergy associated with BSA. First, for bronchial provocation and immunologic studies, BSA (Sigma, St. Louis, MO, USA) and milk extracts (Difco, Michigan, USA) were prepared in our laboratory according a method described elsewhere.3,4 To evaluate the patient's bronchial sensitization, we performed a bronchial provocation test with BSA solution. Two minutes after starting exposure to 0.1 mg/mL BSA solution, the patient experienced severe systemic reactions, including eye itching, conjunctivitis, rhinorrhea, nasal obstruction, sneezing, shortness of breath, bronchospasm with a 30% fall in FEV1 (52.43% of predicted), and decreased blood pressure. After bronchodilator inhalation, his symptoms and FEV1 had improved, and no late reaction was observed.
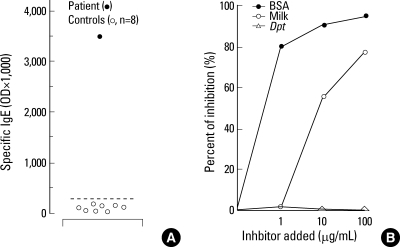
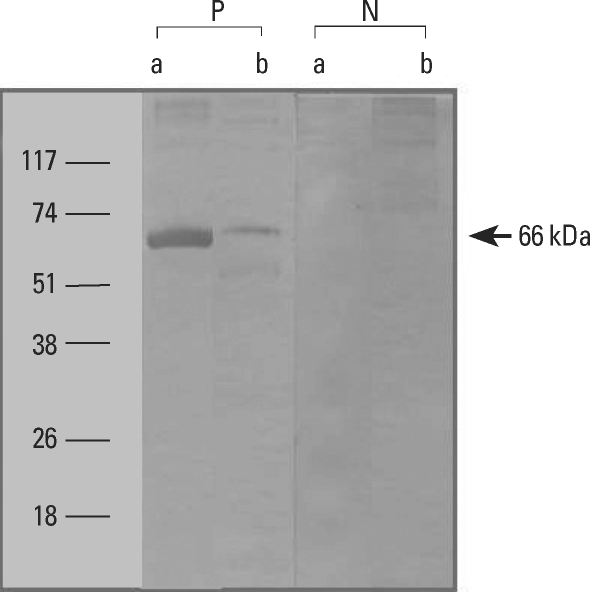
To investigate the pathogenic mechanisms involved, serum specific IgE antibody to BSA extract was measured using an enzyme-linked immunosorbent assay (ELISA). The positive cutoff value for a high level of serum-specific IgE antibody was defined as the mean±3 standard deviations (SD) of the absorbance value for 8 non-atopic healthy controls. The patient had a high level of specific IgE to BSA (Fig. 1A). We performed competitive ELISA inhibition tests to determine the specificity of IgE binding to BSA and possible cross-reactivity with milk antigen, because BSA is one of the major milk allergens. Significant inhibition was noted with the addition of both BSA and milk antigens in a dose-dependent manner, whereas inhibition with D. pteronyssinus antigen was minimal (Fig. 1B). To identify the specific IgE binding component within BSA, we performed an IgE immunoblot analysis. One IgE-binding protein band with a molecular weight of 66 kDa was detected in both BSA and milk extracts (Fig. 2). As a result, the patient was diagnosed with occupational asthma and rhinitis due to the inhalation of BSA powder combined with food allergy induced by milk, which is derived from BSA present within milk. It was recommended that he avoid BSA exposure in his workplace and BSA-containing foods and that he take anti-asthmatic and rhinitis medication.
Fig. 1.
(A) Specific IgE binding to BSA based on ELISA with serum from the patient (•) and unexposed healthy controls (◦). Horizontal bars indicate the positive cutoff value determined from the mean±3 SD of the absorbance value of normal controls. (B) IgE-ELISA inhibition results for BSA-coated wells with the serial additions of BSA (•), milk (◦), and Dermatophagoides pteronyssinus (Dpt, ▵) extracts. The patient had a high level of specific IgE to BSA and showed significant BSA IgE-ELISA inhibition with the addition of BSA and milk extracts in a dose-dependent manner, while minimal inhibition to Dpt antigen was noted.
Fig. 2.
IgE-immunoblot analysis of BSA and milk in serum from the sensitized patient (P) and non-atopic control (N). A 66 kDa IgE-binding BSA band was detected from both BSA and milk extracts. a, BSA; b, Milk
DISCUSSION
Bovine serum albumen (BSA) is a protein widely used in research labs because it stabilizes some enzymes during the digestion of DNA and prevents the non-specific binding of proteins. This case demonstrates that occupational asthma and rhinitis can develop in laboratory workers after dealing with BSA powder. In general, the major pathogenic mechanism of occupational allergies induced by high-molecular-weight antigens is mediated by IgE responses.1 Our patient had a high serum-specific IgE level to BSA, and a 66 kDa IgE-binding component was detected within the BSA extract on immunoblot analysis. In addition, the bronchial provocation test with BSA solution produced immediate bronchoconstriction. These findings suggest that the IgE-mediated response was the major mechanism leading to the development of occupational asthma and rhinitis induced by BSA inhalation.
BSA is involved in milk-induced food allergy.5,6 Although it is present at low concentrations in milk, it is one of the major milk allergens, in addition to casein, as demonstrated by in vivo and in vitro assays.5,7,8 Our patient also had food allergy symptoms with milk ingestion. In addition, using immunoblot analysis, we confirmed an IgE-binding component within the milk extract that was identical to that of BSA. Furthermore, the BSA ELISA inhibition test demonstrated significant inhibition with the serial addition of milk antigens similar to that with BSA. Milk allergy is commonly sensitized via the oral route. However, this study suggested that milk-induced food allergy symptoms can start with sensitization via the respiratory route with the inhalation of BSA in the workplace, as our patient had sufficient time to develop sensitization via the inhalation route in his workplace and he did not experience any allergic symptoms to milk until he experienced severe respiratory symptoms after dealing with BSA powder directly.
BSA, the most abundant blood plasma protein, is one of the important proteins leading to the development of beef-induced food allergy,9 which may be why milk and beef allergies frequently coexist.3,6 It has been also reported that beef may have cross-reactivity with other meats, such as pork, chicken, and mutton, due to the similar structure of mammalian serum albumins.10 Our patient never experienced food allergy symptoms on exposure to beef, pork, or chicken meat.
In conclusion, we report the first case of occupational asthma and rhinitis caused by the inhalation of BSA powder. The case presented as a milk-induced food allergy, which was demonstrated to be an IgE-mediated response.
ACKNOWLEDGMENTS
This study was supported by a grant of the Korean Health 21 R&D Project, Ministry For Health, Welfare and Family Affairs, Republic of Korea (A03001).
Footnotes
There are no financial or other issues that might lead to conflict of interest.
References
- 1.Dykewicz MS. Occupational asthma: current concepts in pathogenesis, diagnosis, and management. J Allergy Clin Immunol. 2009;123:519–528. doi: 10.1016/j.jaci.2009.01.061. [DOI] [PubMed] [Google Scholar]
- 2.Restani P, Ballabio C, Cattaneo A, Isoardi P, Terracciano L, Fiocchi A. Characterization of bovine serum albumin epitopes and their role in allergic reactions. Allergy. 2004;59:21–24. doi: 10.1111/j.1398-9995.2004.00568.x. [DOI] [PubMed] [Google Scholar]
- 3.Vicente-Serrano J, Caballero ML, Rodriguez-Perez R, Carretero P, Perez R, Blanco JG. Sensitization to serum albumins in children allergic to cow's milk and epithelia. Pediatr Allergy Immunol. 2007;18:503–507. doi: 10.1111/j.1399-3038.2007.00548.x. [DOI] [PubMed] [Google Scholar]
- 4.Choi SJ, Hur GY, Shin SY, Park HS. A case of adult onset cow's milk allergy presenting beef and pork meat allergy. Korean J Asthma Allergy Clin Immunol. 2007;27:200–203. [Google Scholar]
- 5.Wal JM. Cow's milk proteins/allergens. Ann Allergy Asthma Immunol. 2002;89:3–10. doi: 10.1016/s1081-1206(10)62115-1. [DOI] [PubMed] [Google Scholar]
- 6.Martelli A, De Chiara A, Corvo M, Restani P, Fiocchi A. Beef allergy in children with cow's milk allergy; cow's milk allergy in children with beef allergy. Ann Allergy Asthma Immunol. 2002;89:38–43. doi: 10.1016/s1081-1206(10)62121-7. [DOI] [PubMed] [Google Scholar]
- 7.Goldman AS, Anderson DW, Jr, Sellers WA, Saperstein S, Kniker WT, Halpern SR. Milk allergy. I. Oral challenge with milk and isolated milk proteins in allergic children. Pediatrics. 1963;32:425–443. [PubMed] [Google Scholar]
- 8.Goldman AS, Sellars WA, Halpern SR, Anderson DW, Jr, Furlow TE, Johnson CH., Jr Milk allergy. II. Skin testing of allergic and normal children with purified mild proteins. Pediatrics. 1963;32:572–579. [PubMed] [Google Scholar]
- 9.Han GD, Matsuno M, Ito G, Ikeucht Y, Suzuki A. Meat allergy: investigation of potential allergenic proteins in beef. Biosci Biotechnol Biochem. 2000;64:1887–1895. doi: 10.1271/bbb.64.1887. [DOI] [PubMed] [Google Scholar]
- 10.Restani P, Beretta B, Fiocchi A, Ballabio C, Galli CL. Cross-reactivity between mammalian proteins. Ann Allergy Asthma Immunol. 2002;89:11–15. doi: 10.1016/s1081-1206(10)62116-3. [DOI] [PubMed] [Google Scholar]