Abstract
Background
The prevention of head injuries in alpine activities has focused on helmets. However, no systematic review has examined the effect of helmets on head and neck injuries among skiers and snowboarders.
Methods
We searched electronic databases, conference proceedings and reference lists using a combination of the key words “head injury or head trauma,” “helmet” and “skiing or snowboarding.” We included studies that used a control group; compared skiers or snowboarders with and without helmets; and measured at least one objectively quantified outcome (e.g., head injury, and neck or cervical injury).
Results
We included 10 case–control, 1 case–control/case-crossover and 1 cohort study in our analysis. The pooled odds ratio (OR) indicated that skiers and snowboarders with a helmet were significantly less likely than those without a helmet to have a head injury (OR 0.65, 95% confidence interval [CI] 0.55–0.79). The result was similar for studies that used controls without an injury (OR 0.61, 95% CI 0.36–0.92), those that used controls with an injury other than a head or neck injury (OR 0.63, 95% CI 0.52–0.80) and studies that included children under the age of 13 years (OR 0.41, 95% CI 0.27–0.59). Helmets were not associated with an increased risk of neck injury (OR 0.89, 95% CI 0.72–1.09).
Interpretation
Our findings show that helmets reduce the risk of head injury among skiers and snowboarders with no evidence of an increased risk of neck injury.
Skiing and snowboarding are popular winter activities.1 Estimates from numerous countries indicate that head injuries account for 9% to 19%, and neck injuries for 1% to 4%, of all injuries reported by ski patrols and emergency departments.2–11 Rates of head and neck injuries have been reported between 0.09 and 0.46 per 1000 outings.12 Head and neck injuries are disproportionately represented in cases of severe trauma, and traumatic brain injury is the leading cause of death and serious injury among skiers and snow-boarders.13 As far back as 1983, Oh and Schmid recommended mandatory helmet use for children while skiing.14
Many studies of the relation between helmet use and head injuries among skiers and snowboarders have found a protective effect.15–24 It has been suggested that the use of helmets may increase the risk of neck injury in a crash or fall.25 This may be more evident among children because they have a greater head:body ratio than adults, and the additional size and weight of the helmet may increase the risk of neck injury in an otherwise routine fall.26 We conducted a systematic review of the effect of helmets on head and neck injuries among skiers and snowboarders.
Methods
Literature search
We conducted comprehensive literature searches of the following electronic databases: MEDLINE (1950 to November 2008), Academic Search Complete (1948 to November 2008), SPORTDiscus (1982 to November 2008), Embase (1980 to November 2008), ERIC (Education Resources Information Center; 1965 to October 2008), PubMED (1948 to November 2008), the Cochrane Central Register of Controlled Trials (CENTRAL; 1991 to November 2008) and SafetyLit (1870 to November 2008). We manually searched the proceedings of the 1st to 16th annual conferences of the International Society of Skiing Safety. We also reviewed the reference lists of included studies. The search strategy is described in Appendix 1 (available at www.cmaj.ca/cgi/content/full/cmaj.091080/DC1). Both published and unpublished studies were considered. We included only English-language studies in the review.27
Selection of studies
Two of us (J.C. and K.R.) screened the titles, and abstracts when available, of potentially relevant studies. The same reviewers independently assessed the full text if the study met the following inclusion criteria: (a) cohort, case–control or case-crossover study design; (b) comparison of snowboarders or skiers with and without helmets; and (c) measurement of at least one objectively quantified outcome (e.g., head injury, neck injury, or severity of head or neck injury). Disagreements were resolved by consensus.
Assessment of methodologic quality
Two of us (J.C. and K.R.) independently assessed the methodologic quality of the studies using the Downs and Black checklist.28 This 28-point checklist assesses biases related to reporting, external validity, internal validity and power. Disagreements were resolved by consensus.
Data extraction and analysis
Three of us (J.C., K.R. and V.W.) extracted the following information from the studies: study design, demographic characteristics, data source and results (type and severity of injury and adverse events). The data were checked for completeness and accuracy; disagreements were resolved by consensus.
Agreement on inclusion and methodologic quality of studies was measured with use of the kappa statistic. We used random-effects modelling to generate pooled estimates of effect. When available, adjusted results were extracted over crude results. The effect of helmet use was expressed as odds ratios (ORs) with accompanying 95% confidence intervals (CIs). To explore heterogeneity, we conducted subgroup analyses for age, sex, experience, and snowboarding versus skiing. For age, we grouped studies if they used consistent categories. We used the I2 statistic to measure statistical heterogeneity.29 We conducted a sensitivity analysis of studies of high (Downs and Black score ≥ 18) and low methodologic quality. We assessed publication bias by examining the estimated measures of effect (i.e., odds ratios) against their standard errors.
Results
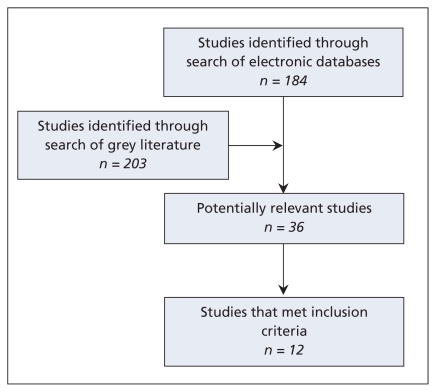
Of the 36 potentially relevant studies, we included 12 in our analysis (kappa = 0.87, 95% CI 0.70–1.00) (Figure 1). We excluded the other 24 studies for the following reasons: the study design was inappopriate (15 studies); the study did not examine skiers or snowboarders with and without helmet use (5); and the data were not reported by exposure and outcome (4).
Figure 1.
Results of literature search.
Of the 12 included studies, 10 were case–control studies, 1 was a case–control/case-crossover study, and 1 was a cohort study (Table 1).2,15–24,30 Five studies were conducted in Europe, one in Asia and six in North America. In the 10 studies from which the data could be obtained, 9829 participants wore helmets and 36 735 did not.2,15–17,19–21,23,24,30 Criteria for selection of cases included self-reported injuries, reports from ski patrols, insurance registrations and patients reporting to an emergency department. Eleven studies examined head injuries; five of them also examined neck injuries.15–17,19,21 The twelfth study examined neck injuries only.30 No study reported deaths. No study described the design, quality or fit of the helmets.
Table 1.
Description of studies included in a systematic review of the effect of helmets on the risk of head and neck injuries among skiers and snowboarders
| Study (country) | Study design | Study population | Sex and age | Snowboarders | Ability | Definition used for head or neck injury | Verification of head or neck injury |
|---|---|---|---|---|---|---|---|
| Mueller et al.17 (United States) | Case–control | 21 375 injured skiers and snowboarders reported by ski patrol; 4779 with helmet, 16 855 without helmet | Cases (head/neck/face injury): male 69% (2904/3701) Controls (no injury): male 57% (10 057/17 626) Age: NR |
Cases: 62% Controls: 59% | Cases: Expert: 1394 Intermediate: 1660 Beginner: 935 Controls: Expert: 4608 Intermediate: 7085 Beginner: 4608 |
Head injury: injury to scalp or skull above the hairline; includes ear and brain injury Facial injury: injury between lower jaw and hairline Neck injury: NR |
NR; ski patrol data |
| Russell et al.30 (Canada) | Case–control | 47 200 injured skiers and snowboarders reported by ski patrol; helmet use 24.3% among cases, 20.2% among controls | Sex: NR Age: 1–18 yr |
55.2% | NR | Neck injury: neck or cervical spine | NR; ski patrol data |
| Fukuda et al.24 (Japan) | Case–control | 1190 injured snowboarders who sought medical treatment for head injury at nearby medical facility; 92 with helmet, 1098 without helmet | Helmet: male 76% (70/92) Mean age 24.6 (SD 4.04) yr No helmet: male 64% (704/1098) Mean age 22.7 (SD 4.8) yr |
100% | Helmet: “Upper” technique level: 31 Other: 61 No helmet: “Upper” technique level: 129 Other: 969 |
Serious head injury: traumatic amnesia, loss of consciousness, craniofacial fracture or intracranial lesion | Physician data; cases and injured controls recruited from neurosurgery institute |
| Shealy et al.23 (United States) | Case–control | 4637 injured skiers at a ski resort in Vermont; 1113 with helmet, 3524 without helmet | NR | None | NR | Potentially serious head injury: diagnosed concussion, more severe closed head injury, skull fracture and/or death Less serious head injury: scalp lacerations and abrasions |
Physician data; cases diagnosed by hospital personnel or clinic staff |
| Sulheim et al.15 (Norway) | Case–control | 3562 injured skiers and snowboarders reported by ski patrol; 752 with helmet, 2810 without helmet | Cases (head injury): male 67% (388/576) Age < 13 yr: 78 13–20 yr: 251 > 20 yr: 237 Controls (non-head injury): male 60% (1801/2986) Age < 13 yr: 295 13–20 yr: 766 > 20 yr: 1919 |
Cases: 44% Controls: 26% | Cases: Expert:108 Good: 186 Intermediate: 147 Beginner: 123 Controls: Expert: 570 Good: 1055 Intermediate: 1005 Beginner: 348 |
Potentially severe head injury: head injury referred to physician or hospital by ski patrol | NR; ski patrol data |
| Ekeland et al.18 (Norway) | Case–control | Skiers and snowboarders with injuries recorded in a central registration of injuries over four major Norwegian ski hills | NR | 45% | NR | NR | NR |
| Hagel et al.16 (Canada) | Case–control/case-crossover | 3988 injured skiers and snowboarders reported by ski patrol; 1104 with helmet, 2884 without helmet | Cases (head/neck injury): male 58% (476/824) Age < 15 yr: 322 15–25 yr: 336 > 26 yr: 166 Controls (non-head/neck injury): male 44% (1457/3294) Age < 15 yr: 1277 15–25 yr: 1185 > 26 yr: 832 |
47% | Days per season Cases: 1 d: 191 2–10 d: 382 > 11 d: 209 Controls: 1 d: 929 2–10 d: 1690 > 11 d: 591 |
Potentially severe cases: isolated head or neck injury requiring evacuation by ambulance | NR; ski patrol data |
| Johnson et al.20 (Canada) | Case–control | 745 snowboarders who reported to hospital emergency department; 410 with helmet, 335 without helmet | Male 67% (501/745) Age ≤ 16 yr |
100% | NR | NR | NR |
| Macnab et al.21 (Canada) | Case–control | 307 injured snowboarders; 131 with helmet, 176 without helmet | Sex NR Age < 13 yr |
Helmet: 24% No helmet: 50% | NR | Inconsequential: no treatment or investigation Minor: investigation and local treatment Major: investigation and referral to hospital for further treatment |
Physician data; injury examined by physician |
| Ekeland et al.19 (Norway) | Case–control | 3605 skiers and snowboarders with injuries recorded in a central registration of injuries over four major Norwegian ski slopes; 397 with helmet, 3208 without helmet | NR | 34% | Helmet: Beginner: 23% Expert: 16% Cases: Beginner: 13% Expert: 17% |
NR | NR; ski patrol data |
| Machold et al.2 (Austria) | Cohort | 2562 students from 86 schools in Austria during 131 winter sport-weeks; 196 with helmet, 2366 without helmet | NR | NR | 100% | NR | Physician data (attending trauma surgeon or local hospital) |
| Sandegard et al.22 (Sweden) | Case–control | Injured skiers and snowboarders (n = NR) who were part of the Swedish Ski Lift and Ski Areas’ Organization injury registration | NR | NR | NR | NR | NR; physician data |
Note: NR = not reported, SD = standard deviation.
The median score for methodologic quality of the included studies was 20 out of 28 (interquartile range 14.25–21.25) (Table 2). The kappa statistic for the assessment of methodologic quality was 0.65 (95% CI 0.57–0.74).
Table 2.
Methodologic quality of the included studies
| Study | Study design | Adequate selection of cases and controls | Adequate assessment of exposure | Adequate assessment of outcome | Adequate control for confounding | Overall score* |
|---|---|---|---|---|---|---|
| Meuller et al.17 | Case–control | Characteristics given: yes Same population: yes Same period: yes |
Described: yes | Described: yes Accurate: yes |
Distribution given: yes Adjustment: yes |
22 |
| Fukuda et al.24 | Case–control | Characteristics given: yes Same population: yes Same period: yes |
Described: yes | Described: yes Accurate: yes |
Distribution given: yes Adjustment: yes |
21 |
| Russell et al.30 | Case–control | Characteristics given: yes Same population: yes Same period: yes |
Described: yes | Described: yes Accurate: yes |
Distribution given: yes Adjustment: yes |
23 |
| Shealy et al.23 | Case–control | Characteristics given: no Same population: yes Same period: yes |
Described: no | Described: yes Accurate: yes |
Distribution given: no Adjustment: no |
10 |
| Sulheim et al.15 | Case–control | Characteristics given: yes Same population: yes Same period: yes |
Described: yes | Described: yes Accurate: yes |
Distribution given: yes Adjustment: yes |
21 |
| Ekeland et al.18 | Case–control | Characteristics given: yes Same population: yes Same period: yes |
Described: yes | Described: yes Accurate: yes |
Distribution given: yes Adjustment: yes |
19 |
| Hagel et al.16 | Case–control and case-crossover | Characteristics given: yes Same population: yes Same period: yes |
Described: yes | Described: yes Accurate: yes |
Distribution given: yes Adjustment: yes |
22 |
| Johnson et al.20 | Case–control | Characteristics given: yes Same population: yes Same period: yes |
Described: yes | Described: yes Accurate: yes |
Distribution given: no Adjustment: no |
12 |
| Macnab et al.21 | Case–control | Characteristics given: yes Same population: yes Same period: yes |
Described: yes | Described: yes Accurate: yes |
Distribution given: no Adjustment: yes |
19 |
| Ekeland et al.19 | Case–control | Characteristics given: yes Same population: yes Same period: yes |
Described: yes | Described: yes Accurate: yes |
Distribution given: yes Adjustment: yes |
19 |
| Machold et al.2 | Cohort | Characteristics given: yes Same population: yes Same period: yes |
Described: no | Described: yes Accurate: yes |
Distribution given: no Adjustment: no |
15 |
| Sandegard et al.22 | Case–control | Characteristics given: no Same population: yes Same period: yes |
Described: no | Described: no Accurate: yes |
Distribution given: no Adjustment: no |
9 |
Overall scores for methodologic quality were determined with use of the Downs and Black checklist (maximum score 28).28
Helmet use and head injury
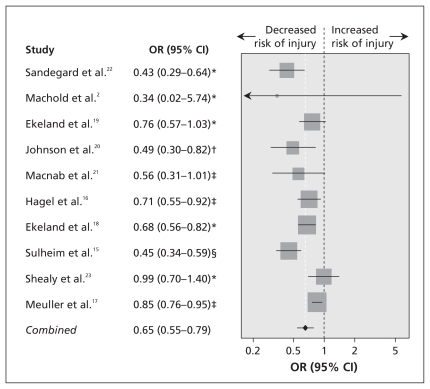
In our analysis of the nine studies that compared injured skiers and snowboarders with noninjured controls or controls who had an injury other than a head or neck injury, we found that the use of helmets significantly reduced the risk of head injury.15–23 The pooled analysis of these studies indicated that the risk was reduced by 35% (OR 0.66, 95% CI 0.55–0.79; I2 = 75.7%). Machold and associates reported no head injury among those who used helmets.2 Although their study suggests that helmets are protective, we were unable to obtain an odds ratio and include it in the pooled analysis. However, when we added 0.5 to the cells of the 2 × 2 table to enable calculation of an odds ratio31 and included this study in the analysis, we found no change in the estimate of effect (OR 0.65, 95% CI 0.55–0.79; I2 = 72.9%) (Figure 2).
Figure 2.
The effectiveness of helmets in preventing head injuries. The size of the data marker corresponds to the relative weight assigned in the pooled analysis. CI = confidence interval, OR = odds ratio. I2 = 72.9%. *Unadjusted OR and 95% CI calculated from data provided in original study. †OR and 95% CI provided in original study for patients 13–16 years old; an even greater protective effect for helmets was seen among children less than 12 years old (OR 0.21, 95% CI 0.12–0.36). ‡Adjusted OR and 95% CI provided in original study. §OR and 95% CI provided in original study.
When considering the five studies that compared injured skiers and snowboarders with noninjured controls, we found that the risk of head injury was significantly reduced among those wearing a helmet (OR 0.61, 95% CI 0.44–0.83; I2 = 75.0%).15,18,20,21,23 The same was true in the pooled analysis of the five studies that compared injured skiers and snowboarders with controls who had an injury other than a head or neck injury (OR 0.63, 95% CI 0.48–0.83; I2 = 84.7%).15–17,19,22
Four studies examined the effect of helmets on potentially severe head trauma.15,16,23,24 Sulheim and colleagues reported a significant protective effect (OR 0.43, 95% CI 0.25–0.77),15 as did Hagel and colleagues (OR 0.44, 95% CI 0.24–0.81).16 Potentially severe head injuries in these two studies were defined as referral to an emergency physician or hospital for treatment,15 and head injury requiring evacuation by ambulance.16 Shealy and colleagues reported no significant difference in the incidence of potentially serious head injury (concussion, severe closed head injury, skull fracture or death) between helmet users and nonusers.23 Fukuda and colleagues, after adjusting for jumping, reported a nonsignificant effect of helmet use on severe head injuries (traumatic amnesia, loss of consciousness, craniofacial fracture or intracranial lesion) compared with non-serious head injuries (OR 0.66, 95% CI 0.32–1.35).24
Subgroup and sensitivity analyses
The subgroup analyses are presented in Table 3. Among children less than 13 years old, the odds ratio for the effectiveness of helmets in reducing the risk of head injury was 0.39 (95% CI 0.23–0.65; I2 = 72.2%).15,17,20,21 The odds ratio among males was 0.80 (95% CI 0.70–0.92), and the odds ratio among females was 0.98 (95% CI 0.80–1.19);17 however, the p value for whether the effect estimates were modified by sex was 0.09. The use of helmets was associated with a significant reduction in the risk of head injury among skiers and snow-boarders at the beginner level; however, the p value for whether the effect of helmets was modified by experience was 0.15.17 The association between helmet use and head injury was similar among skiers and snowboarders.
Table 3.
Subgroup analysis of the effect of helmet use on head injuries
| Parameter | No. of studies | OR (95% CI) |
|---|---|---|
| Age, yr | ||
| < 13 | 4 | 0.41 (0.28–0.62) |
| 13–24 | 1 | 0.80 (0.69–0.89) |
| > 25 | 1 | 1.13 (0.93–1.36) |
| < 15 | 1 | 0.73 (NR) |
| 15–25 | 1 | 0.71 (NR) |
| > 25 | 1 | 0.75 (NR) |
| Sex | ||
| Male | 1 | 0.80 (0.70–0.92) |
| Female | 1 | 0.98 (0.80–1.19) |
| Ability | ||
| Beginner | 1 | 0.69 (0.53–0.89) |
| Intermediate | 1 | 0.86 (0.72–1.02) |
| Expert | 1 | 0.92 (0.77–1.09) |
| Activity | ||
| Skiing | 2 | 0.82 (0.69–0.98) |
| Snowboarding | 2 | 0.83 (0.75–0.98) |
| Location | ||
| Park/off-piste (backcountry or out of bounds) | 1 | 0.26 (0.14–0.50) |
| Prepared runs | 1 | 0.45 (0.31–0.64) |
| Lift-related* | 1 | 0.52 (0.19–1.38) |
| Age and activity | ||
| < 13 yr and skiing | 1 | 0.40 (0.20–0.96) |
| < 13 yr and snowboarding | 1 | 0.18 (0.04–0.74) |
| 13–20 yr and skiing | 1 | 0.52 (0.23–1.19) |
| 13–20 yr and snowboarding | 1 | 0.56 (0.32–0.95) |
| > 20 yr and skiing | 1 | 0.43 (0.18–1.02) |
| > 20 yr and snowboarding | 1 | 0.18 (0.03–0.39) |
Note: CI = confidence interval, NR = not reported, OR = odds ratio.
Injured while getting on or off a lift.
Table 4 describes the sensitivity analyses of methodologic quality. The summary estimates of effect did not vary by the methodologic parameters. None of the differences in methodologic quality accounted for the heterogeneity of the results. Compared with the studies of low methodologic quality (Downs and Black score < 18), the high-quality studies had a slightly more conservative, yet statistically significant, result (OR 0.68, 95% CI 0.55–0.82).
Table 4.
Sensitivity analysis of the effect of helmet use on head injuries
| Parameter | No. of studies | OR (95% CI) | Heterogeneity, I2 value, % |
|---|---|---|---|
| Methodologic quality* | |||
| High (score ≥ 18) | 6 | 0.68 (0.55–0.82) | 75.8 |
| Low (score < 18) | 4 | 0.59 (0.35–1.00) | 73.1 |
| Study design | |||
| Case–control | 9 | 0.66 (0.55–0.79) | 75.7 |
| Cohort | 1 | 0.48 (0.48–0.34) | NA |
| Adjusted for confounding | |||
| Yes | 6 | 0.68 (0.55–0.82) | 75.8 |
| No | 4 | 0.59 (0.35–1.00) | 73.1 |
| Adequate outcome assessment | |||
| Yes | 9 | 0.69 (0.58–0.82) | 69.3 |
| No | 1 | 0.43 (0.29–0.64) | NA |
| Adequate exposure assessment | |||
| Yes | 7 | 0.66 (0.54–0.79) | 74.0 |
| No | 3 | 0.63 (0.30–1.34) | 79.7 |
| Adequate selection of cases and controls | |||
| Yes | 8 | 0.66 (0.54–0.79) | 70.0 |
| No | 2 | 0.66 (0.29–1.49) | 89.6 |
Note: CI = confidence interval, NA = not applicable, OR = odds ratio.
Overall scores for methodologic quality were determined with use of the Downs and Black checklist (maximum score 28).28
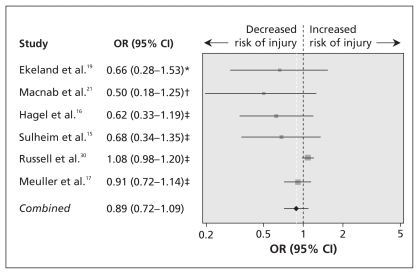
Helmet use and neck injury
The pooled analysis of the six studies that examined the association between the use of helmets and the risk of neck injury showed no increased risk (OR 0.89, 95% CI 0.72–1.09; I2 = 44.7%) (Figure 3).15–17,19,21,30 Two of the studies examined the risk of neck injury among children.21,30 Macnab and colleagues reported an OR of 0.50 (95% CI 0.18–1.25) for the association between cervical spine injury and helmet use among children under 13 years.21 Preliminary results based on our work suggested no significant association between helmet use and the risk of any neck injury among children after adjustment for age and activity (OR 1.08, 95% CI 0.98–1.20).30
Figure 3.
The effect of helmet use on the risk of neck injury. The size of the data marker corresponds to the relative weight assigned in the pooled analysis. CI = confidence interval, OR = odds ratio. I2 = 44.7%. *Unadjusted OR and 95% CI calculated from data provided in original study. †OR and 95% CI provided in original study. ‡Adjusted OR and 95% CI provided in original study.
Publication bias
Three of the four studies with the largest effect measures (OR < 0.6) all had the largest statistical variability.2,20,22 Four of the six remaining studies had a larger sample size and smaller statistical variability.16–19 This suggests that smaller studies reporting statistically nonsignificant effect measures may have been less likely to be published.
Interpretation
In our meta-analysis, the use of helmets had a significant protective effect against head injuries among skiers and snowboarders. The pooled analysis showed that the risk of head injury was reduced by 35% with helmet use (95% CI 21%–46%) and that 2–5 of every 10 head injuries among helmet users could be prevented. We found a protective effect among skiers and snowboarders, and among those participating in park/off-piste (backcountry or out-of-bounds) locations and on prepared runs.15,17,21 Although not statistically significant, there was some suggestion that helmets had a greater protective effect among males than among females, and among skiers and snowboarders of a lower ability level.17 Our results are similar to those of a recent review of concussions and use of protective equipment in a variety of summer and winter activities.32
Two of the studies included in our analysis reported similar, significant protective effects of helmets against potentially severe head injury.15,16 Conversely, Shealy and colleagues reported no such effect.23 Differences in the findings may have been due to the definitions used for severe head injury or to the extent of adjustment for confounding variables. In another study by Shealy and colleagues, which we did not include in our review because of a lack of detail about outcomes and the composition of the control group, helmet use was examined among skiers and snowboarders whose primary cause of death was a head injury and those with another primary cause of death (they may have had a nonfatal head injury or a fatal neck injury). The authors found that helmet use was significantly higher among those who died of a non-head-related injury than among those who died of a head injury.33
Although wearing a helmet reduces the risk of head injury, there is concern that helmets may increase the risk of neck injury, particularly among children. Our pooled results and the individual studies showed no significant association between helmet use and increased risk of neck injury. This is consistent with biomechanical data showing no increase in neck loads associated with helmet use in simulated snow-boarding falls.34
The use of helmets may provide a false sense of security, however, and result in more aggressive or dangerous participation, which could increase the risk of injury to other parts of the body.35 Several studies have examined risk compensation in relation to helmet use among skiers and snowboarders.15,24,36–39 The evidence is mixed: some of the studies showed increased risk-taking among those who used helmets,15,39 whereas others showed that helmet users were a more cautious subgroup of participants.37 Fukuda and associates noted that helmet users were more likely than nonusers to have injuries related to jumping, which indicates that helmet users may attempt more risky manoeuvres.24 Our work suggests no relation between helmet use and severity of injury or crash circumstances (non-helmet equipment damage, fast self-reported speed, participation in more difficult runs than normal, or jumping-related injury) after adjustment for confounding variables.36 The available evidence suggests that, if helmet users exhibit compensating behaviour, their level of injury risk is not higher than that of nonusers.
Limitations
Our review has limitations. First, the methodologic quality of the included studies was moderate. The most common shortcoming was an insufficient adjustment for and description of potential confounders. For five of the studies, we had to calculate the odds ratios from the authors’ data, and only the crude, unadjusted odds ratio could be calculated.2,18,19,22,23 However, although adjusted odds ratios were more conservative, the odds ratios for the adjusted and crude pooled estimates were similar and the 95% confidence intervals overlapped.
Two approaches were used to select control groups. Four of the studies included noninjured controls,18,20,21,23 four included controls with injuries other than head or neck injuries,16,17,19,22 and one study included both types of controls.15 The similarity of results in the studies using these approaches provides some support of the validity of both approaches in research of injuries among skiers and snowboarders.
Another limitation was the different definitions of head injury used. Also, the place of diagnosis and the personnel making the diagnosis differed between studies. Definitions of potential confounders, such as age groups and ability, were inconsistently recorded between studies, which made comparisons challenging.
We restricted the review to English-language studies. If English and non-English studies systematically differed in methodologic quality or outcome, then article selection bias would be present. Studies with significant findings are more likely to be in English.40 If a language bias was present in our review, the effect of helmets may have been overestimated. However, we included studies conducted in regions where skiing and snow-boarding are common: Canada, the United States, Europe and Japan.
We made a concerted effort to identify grey literature. Electronic databases, reference lists and conference proceedings were examined in an attempt to discover all literature that would meet our inclusion criteria. If publication bias existed, it would have resulted in an overestimation of the effect of helmets.
We were unable to examine results in terms of the design, quality or fit of the helmets. If helmets were of poor quality or condition, or were worn incorrectly, as has been shown among some users of bicycle helmets,41 then the effect of helmets would be underestimated relative to their true potential of reducing head injury.42
Conclusion
Our pooled analysis of evidence suggests that helmets are effective in reducing the risk of head injury among skiers and snowboarders. We found no significant association between helmet use and an increased risk of neck injury. Based on our findings, we encourage the use of helmets among skiers and snowboarders. Additional, methodologically rigorous research is required to determine which types of helmets provide the best protection.
Supplementary Material
Acknowledgement
The authors thank Vanessa Wainwright for her assistance in extracting study data.
Footnotes
Funding: No external funding was received for this study. Brent Hagel holds the Alberta Children’s Hospital Foundation Professorship in Child Health and Wellness, funded through the support of an anonymous donor and the Canadian National Railway Company; he also holds a Population Health Investigator Award from the Alberta Heritage Foundation for Medical Research and a New Investigator Award from the Canadian Institutes of Health Research. Kelly Russell holds a Doctoral Studentship from the Alberta Heritage Foundation for Medical Research.
Previously published at www.cmaj.ca
Competing interests: None declared.
Contributors: Kelly Russell was involved in the initial conception and design of the study, coordinated the project, assessed studies for inclusion, assessed the methodologic quality of included studies, extracted and checked data, contributed to the data analysis and critically reviewed the manuscript. Josh Christie conducted the literature search, assessed studies for inclusion, assessed the methodologic quality of included studies, extracted and checked data and drafted the manuscript. Brent Hagel was involved in the initial conception and design of the study, contributed to the data analysis and critically reviewed the manuscript. All of the authors approved the final version of the manuscript submitted for publication.
This article has been peer reviewed.
REFERENCES
- 1.Bladin C, McCrory P. Snowboarding injuries — an overview. Sports Med. 1995;19:358–64. doi: 10.2165/00007256-199519050-00005. [DOI] [PubMed] [Google Scholar]
- 2.Machold W, Kwasny O, Gassler P, et al. Risk of injury through snowboarding. J Trauma. 2000;48:1109–14. doi: 10.1097/00005373-200006000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Hagel BE, Meeuwisse WH, Mohtadi NGH, et al. Skiing and snowboarding injuries in the children and adolescents of Southern Alberta. Clin J Sport Med. 1999;9:9–17. doi: 10.1097/00042752-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Made C, Elmqvist LG. A 10-year study of snowboard injuries in Lapland Sweden. Scand J Med Sci Sports. 2004;14:128–33. doi: 10.1111/j.1600-0838.2003.00342.x. [DOI] [PubMed] [Google Scholar]
- 5.Xiang H, Kelleher K, Shields BJ, et al. Skiing- and snowboarding-related injuries treated in US emergency departments, 2002. J Trauma. 2005;58:112–8. doi: 10.1097/01.ta.0000151270.26634.dd. [DOI] [PubMed] [Google Scholar]
- 6.Hagel BE, Pless IB, Platt RW. Trends in emergency department reported head and neck injuries among skiers and snowboarders. Can J Public Health. 2003;94:458–62. doi: 10.1007/BF03405085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lamont MK. Ski field injuries: The snowboarders. In: Mote CD Jr, Johnson RJ, Hauser W, et al., editors. Skiing trauma and safety. Vol. 10. Philadelphia (PA): American Society for Testing Materials; 1996. pp. 82–6. [Google Scholar]
- 8.Pogorzelski A, McCrory P, Bladin C. Alpine sports injuries in Victoria. Proceedings of the Australian conference of science and medicine in sport and third national sports injury prevention conference; 2003 Oct. 25–28; Dickson ACT (Australia): Sports Medicine Australia; 2003. [(accessed 2010 Jan. 8)]. p. 52. Available: http://fulltext.ausport.gov.au/fulltext/2003/acsms/2003ACSMS.pdf. [Google Scholar]
- 9.Shealy JE, Sundman PD, Johnson RJ, et al. Skiing trauma and safety; seventh international symposium. Philadelphia (PA): American Society for Testing Materials; 1989. Snowboarding injuries on alpine slopes; pp. 75–81. [Google Scholar]
- 10.Davidson TM, Laliotis AT. Snowboarding injuries — a four-year study with comparison with alphine ski injuries. West J Med. 1996;164:231–7. [PMC free article] [PubMed] [Google Scholar]
- 11.Bridges EJ, Rouah F, Johnston KM. Snowblading injuries in Eastern Canada. Br J Sports Med. 2003;37:511–5. doi: 10.1136/bjsm.37.6.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hagel BE, Goulet C, Platt RW, et al. Injuries among skiers and snowboarders in Quebec. Epidemiology. 2004;15:279–86. doi: 10.1097/01.ede.0000120044.62029.b4. [DOI] [PubMed] [Google Scholar]
- 13.Levy AS, Hawkes AP, Hemminger LM, et al. An analysis of head injuries among skiers and snowboarders. J Trauma. 2002;53:695–704. doi: 10.1097/00005373-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Oh S, Schmid UD. Head-injuries in childhood caused by skiing accidents and optimal prevention. Z Kinderchir. 1983;38:66–72. doi: 10.1055/s-2008-1059941. [DOI] [PubMed] [Google Scholar]
- 15.Sulheim S, Holme I, Ekeland A, et al. Helmet use and risk of head injuries in alpine skiers and snowboarders. JAMA. 2006;295:919–24. doi: 10.1001/jama.295.8.919. [DOI] [PubMed] [Google Scholar]
- 16.Hagel BE, Pless IB, Goulet C, et al. Effectiveness of helmets in skiers and snow-boarders: Case-control and case crossover study. BMJ. 2005;330:281. doi: 10.1136/bmj.38314.480035.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mueller BA, Cummings P, Rivara FP, et al. Injuries of the head, face, and neck in relation to ski helmet use. Epidemiology. 2008;19:270–6. doi: 10.1097/EDE.0b013e318163567c. [DOI] [PubMed] [Google Scholar]
- 18.Ekeland A, Sulheim S, Rodven A, et al. Injury rates and injury types in alpine skiing, telemarking, and snowboarding. In: Johnson R, Shealy JE, Ahlbaumer MG, editors. Skiing trauma and safety: fifteenth volume. Philadelphia (PA): American Society for Testing Materials; 2005. pp. 31–9. [Google Scholar]
- 19.Ekeland A, Rodven A. Injuries in alpine skiing, telemarking, and snowboarding. In: Johnson RJ, Zucco P, Shealy JE, editors. Skiing trauma and safety: thirteenth volume. Philadelphia (PA): American Society for Testing Materials; 2001. pp. 87–94. [Google Scholar]
- 20.Johnson KN, Mohadi NGH, Sasyniuk TM. The prevalence of protective equipment use and injury prevention in snowboarding [abstract]. In: 2001 annual meeting of the Canadian Academy of Sport Medicine. Clin J Sport Med. 2002;12:65–71. [Google Scholar]
- 21.Macnab AJ, Smith T, Gagnon FA, et al. Effect of helmet wear on the incidence of head/face and cervical spine injuries in young skiers and snowboarders. Inj Prev. 2002;8:324–7. doi: 10.1136/ip.8.4.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sandegard J, Eriksson B, Lundkvist S. Nationwide registration of ski injuries in Sweden. In: Mote CD Jr, Johnson RJ, editors. Skiing trauma and safety. Philadelphia (PA): American Society for Testing Materials; 1991. pp. 170–6. [Google Scholar]
- 23.Shealy JE, Johnson RJ, Ettlinger CF. Head trauma and helmet usage in alpine skiing [abstract]. Knee Surg Sports Traumatol Arthrosc; 16th International Society of Skiing Safety Conference; Niigata, Japan. 17–23 April 2005; 2006. p. 97. [Google Scholar]
- 24.Fukuda O, Hirashima Y, Origasa H, et al. Characteristics of helmet or knit cap use in head injury of snowboarders. Neurol Med Chir (Tokyo) 2007;47:491–4. doi: 10.2176/nmc.47.491. [DOI] [PubMed] [Google Scholar]
- 25.Hunter RE. Skiing injuries. Am J Sports Med. 1999;27:381–9. doi: 10.1177/03635465990270032101. [DOI] [PubMed] [Google Scholar]
- 26.Deibert MC, Aronsson DD, Johnson RJ, et al. Skiing injuries in children, adolescents, and adults. J Bone Joint Surg Am. 1998;80:25–32. [PubMed] [Google Scholar]
- 27.Moher D, Pham B, Klassen TP, et al. What contributions do languages other than English make on the results of meta-analyses? J Clin Epidemiol. 2000;53:964–72. doi: 10.1016/s0895-4356(00)00188-8. [DOI] [PubMed] [Google Scholar]
- 28.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistencies in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Russell K, Nettel-Aguirre A, Goulet C, et al. Neck injury risk and helmet use in pediatric skiers and snowboarders [abstract]. Canadian Injury Prevention and Safety Promotion Conference; Toronto. Nov. 11–13, 2007; [(accessed 2010 Jan 25)]. Available: http://70.25.93.52/natconf/Oral_CIPSPC_Abstracts_2007.pdf. [Google Scholar]
- 31.Breslow NE, Day NE. Statistical methods in cancer research. Vol. 1. Lyon (France): International Agency for Research on Cancer; 1980. The analysis of case–control studies; p. 139. [PubMed] [Google Scholar]
- 32.Benson BW, Hamilton GM, Meeuwisse WH, et al. Is protective equipment useful in preventing concussion? A systematic review of the literature. Br J Sports Med. 2009;43(Suppl 1):i56–67. doi: 10.1136/bjsm.2009.058271. [DOI] [PubMed] [Google Scholar]
- 33.Shealy JE, Johnson RJ, Ettlinger CF. Do Helmets reduce fatalities or merely alter the patterns of death? J ASTM Int. 2008;5:1–4. [Google Scholar]
- 34.Scher I, Richards D, Carhart M. Head contact after catching an edge: an examination of snowboarding helmets [abstract]. Knee Surg Sports Traumatol Arthrosc; 16th International Society of Skiing Safety Conference; Niigata, Japan. 17–23 April 2005; 2006. p. 97. [Google Scholar]
- 35.Hedlund J. Risky business: Safety regulatons, risk compensation, and individual behaviour. Inj Prev. 2000;6:82–9. doi: 10.1136/ip.6.2.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hagel B, Pless IB, Goulet C, et al. The effect of helmet use on injury severity and crash circumstances in skiers and snowboarders. Accid Anal Prev. 2005;37:103–8. doi: 10.1016/j.aap.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 37.Scott MD, Buller DB, Andersen PA, et al. Testing the risk compensation hypothesis for safety helmets in alpine skiing and snowboarding. Inj Prev. 2007;13:173–7. doi: 10.1136/ip.2006.014142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shealy JE, Ettlinger CF, Johnson RJ, et al. Skiing trauma and safety. Vol. 13. Philadelphia (PA): American Society for Testing Materials; 2000. Rates and modalities of death in the U.S.: snowboarding and skiing differences —1991/92 through 1998/99; pp. 132–8. [Google Scholar]
- 39.Shealy JE, Ettlinger CF, Johnson RJ. How fast do people go on alpine slopes? [abstract]. Knee Surg Sports Traumatol Arthrosc; Proceedings from the 15th ISSS Conference in Pontresina; Switzerland. 27 April to 2 May 2003; 2004. p. 173. [Google Scholar]
- 40.Egger M, Smith GD. Meta-analysis — bias in location and selection of studies. BMJ. 1998;316:61–6. doi: 10.1136/bmj.316.7124.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee RS, Hagel BE, Karkhaneh M, et al. A systematic review of correct bicycle helmet use: How varying definitions and study quality influence the results. Inj Prev. 2009;15:125–31. doi: 10.1136/ip.2008.019695. [DOI] [PubMed] [Google Scholar]
- 42.Rivara FP, Astley SJ, Clarren SK, et al. Fit of bicycle safety helmets and risk of head injuries in children. Inj Prev. 1999;5:194–7. doi: 10.1136/ip.5.3.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.