Abstract
International studies suggest that cognitive-behavioural therapy (CBT) for the treatment of mental disorders results in improved clinical and economic outcomes. In Canada, however, publicly funded CBT is scarce, representing an inequity in service delivery. A research framework to evaluate the Canadian health economic impact of increasing access to CBT is proposed. Canadian data related to the epidemiology of mental disorders, patterns of usual care, CBT effectiveness, resource allocation and costs of care will be required and methodologies should be transparent and outcomes meaningful to Canadian decision-makers. Findings should be delivered by multidisciplinary teams of researchers and health professionals. Barriers to funding reform must be identified and knowledge translation strategies delineated and implemented. Canadian clinical and economic outcomes data are essential for those seeking to provide decision-makers with the evidence they need to evaluate whether CBT represents value for mental health dollars spent.
Abstract
Les études internationales suggèrent que la thérapie cognitivo-comportementale (TCC) pour le traitement des troubles mentaux améliore les résultats cliniques et économiques. Au Canada, cependant, la TCC subventionnée par les fonds publics est plutôt rare et présente une inégalité dans l'offre de services. Un cadre de recherche afin d'évaluer l'impact économique sur la santé canadienne d'un plus grand accès à la TCC est proposé. Les données canadiennes sur l'épidémiologie des troubles mentaux, sur les modèles d'utilisation des soins, sur l'efficacité de la TCC, sur l'allocation des ressources et sur le coût des soins seront nécessaires et les méthodologies doivent être transparentes et les résultats doivent être pertinents pour les décideurs au Canada. Les résultats devraient être présentés par des équipes multidisciplinaires composées de chercheurs et de professionnels de la santé. Il faut repérer les obstacles à la réforme du financement et concevoir des stratégies favorisant le transfert de connaissances. Les résultats cliniques et économiques canadiens sont indispensables pour ceux qui tentent de fournir aux décideurs les données nécessaires afin de leur permettre d'évaluer la rentabilité de la TCC en fonction de l'argent dépensé pour les services de santé mentale.
Canadian mental healthcare costs are formidable, with total annual direct expenditures estimated at CAD$5.5 billion in 2004 (Jacobs et al. 2008). Spending in this sector will undoubtedly increase, given goals delineated within the Canadian Mental Health Strategy to improve mental health treatment, accessibility and service delivery (Mental Health Commission of Canada 2009). Currently, only 40% of mentally ill Canadians present themselves for diagnosis and treatment (LeSage et al. 2006). As stigma is reduced and access to care improves (Mental Health Commission of Canada 2009), more Canadians will seek out the treatments they need. A rational, evidence-based approach to the allocation of limited mental healthcare dollars is more important than ever.
Health economic evaluations such as cost-effectiveness analyses (Gold et al. 1996) and budget impact evaluations (Trueman et al. 2001), are essential for informed funding decisions (Canadian Agency for Drugs and Technologies in Health 2006). While routine for pharmacotherapies, they are not so for non-pharmacological treatments (Evers et al. 1997). Cognitive-behavioural therapy (CBT), a psychological, guideline-recommended, first-line treatment for many mental disorders, has been an exception.
CBT is a problem-focused, empirically based psychotherapy that teaches patients to detect and modify thought patterns and change behaviour to reduce distress and promote well-being. It is as efficacious as medication for major depressive and anxiety disorders (Otto 2005). In combination with medications, CBT has improved outcomes in schizophrenia (Wykes et al. 2008) and bipolar disorder (Otto 2005). Compared to medications, CBT is associated with higher patient satisfaction (Turkington et al. 2002) and fewer side effects, relapses (Otto et al. 2000; Hollon et al. 2005) and drop-outs (Gould et al. 1995). In addition to its clinical benefits, a published systematic review has demonstrated that CBT for the treatment of mental disorders can also lead to improved economic outcomes, with cost-effectiveness ratios well below accepted thresholds (Myhr and Payne 2006). Unlike medications, CBT has enduring effects even after treatment's end, a benefit that comes at no additional cost (Hollon et al. 2005). In the United Kingdom (Lam et al. 2005; Scott et al. 2003; Haddock et al. 2003) and Australia (Haby et al. 2004b; Sanderson et al. 2003; Vos et al. 2005a; Heuzenroeder et al. 2004; Issakidis et al. 2004), compelling economic evidence has contributed to shifts in healthcare funding policy, resulting in increased access to publicly funded CBT in these countries.
In Canada, publicly funded CBT remains limited. While medical visits and “medically necessary” expenses are covered by the Canada Health Act (1985), many psychological services are not (Romanow and Marchildon 2003). Typically, provinces only fund physician-administered psychotherapy, or in the case of non-physicians, therapists employed by public institutions (Romanow and Marchildon 2003; Hunsley 2002). In most care settings, CBT is available mainly to those with private health insurance, or to those who can afford to pay out of pocket. This inequity in the delivery of optimal mental healthcare is an example of how socio-economic status can determine the quality of healthcare received.
Economic evaluations of the impact of treating more Canadians with CBT require a systematic approach to the gathering and analysis of clinical and economic data. The objectives of this paper are (a) to provide a compelling rationale to initiate Canadian health economic analyses of CBT and (b) to describe an organizational framework to identify, prioritize and coordinate research initiatives in support of these analyses, and effective knowledge translation.
Proposed Research Framework
Overview
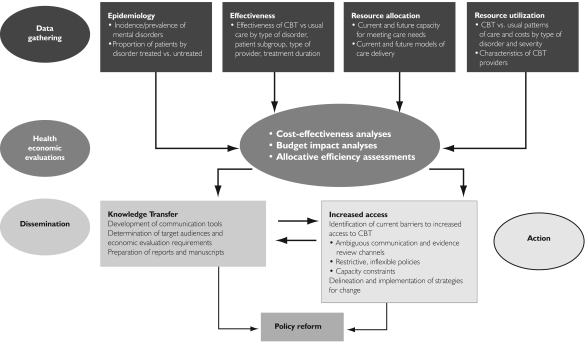
At the core of the research framework (Figure 1) are the health economic evaluations required for healthcare policy decisions. Researchers need to design analytical models identifying outcomes meaningful to decision-makers and specify the associated Canadian data requirements. Results must be communicated strategically to target audiences, such as multidisciplinary research teams and collaborative networks or coalitions of health professionals, interest groups and patients. Barriers to CBT-related mental health funding policy reform should be identified. This proposed CBT research framework is consistent with the vision for knowledge translation at the Canadian Institutes for Health Research (CIHR 2004): to develop a systematic, integrated approach to accelerate the optimal use of research evidence to improve the health of Canadians.
FIGURE 1.
Schematic overview of proposed CBT research framework in support of Canadian economic analyses and knowledge translation
Economic evaluations
Cost-effectiveness analyses quantify the efficiency of spending, considering both the costs and effectiveness of treatment (Gold et al. 1996). Budget impact evaluations assess the affordability of an intervention (Trueman et al. 2001; Langley 2000). Although the cost-effectiveness of CBT has been demonstrated in various patient populations and countries (Haby et al. 2004b; Lam et al. 2005; Lynch et al. 2005; Revicki et al. 2005; Sanderson et al. 2003; Scott et al. 2003; Von Korff et al. 1998; Vos et al. 2005a; Heuzenroeder et al. 2004; Issakidis et al. 2004; Otto et al. 2000; Katon et al. 2006; Haddock et al. 2003), no Canadian analyses have yet been undertaken. Also lacking are budget impact analyses, which would estimate the total cost of increasing access to CBT, including hiring and training providers (Myhr and Payne 2006). The conceptualization of these evaluations represents the first step in the organization of research activities described in the framework. Methodologies to evaluate the health economic impact of CBT have already been published (Haby et al. 2004a; Vos et al. 2005b), and Canadian health economic evaluation guidelines are available (Canadian Agency for Drugs and Technologies in Health 2006). Key questions to be addressed include:
What is the estimated per-patient treatment cost of CBT for each mental disorder in Canada? What are the main determinants of these costs? What cost savings are associated with CBT?
Is CBT for mentally ill Canadians cost effective? If so, for which subgroups, by which type of provider, over what duration and within which models of service delivery?
What is the projected rate of uptake of CBT if increased accessibility is achieved? To what extent would factors relevant to the Canadian context, such as geographic remoteness and special populations (e.g., First Nations peoples, immigrants), affect its uptake?
How can competency in CBT as a therapeutic modality be evaluated, monitored and regulated if significantly more CBT providers are required to meet demand?
What are the total training and employment costs associated with meeting the demand for adequate numbers of CBT providers?
In a recent systematic review of economic evaluations of CBT (Myhr and Payne 2006), 13 cost-effectiveness studies were identified (five from Australia, five from the United States and three from the United Kingdom). Limitations of the economic analyses reviewed were the omission of CBT provider training and start-up costs, the exclusion of productivity losses, short time horizons and the lack of effectiveness data from the usual care environment. Moreover, budget impact analyses of the affordability of CBT to healthcare payers have been lacking altogether. Canadian analyses must overcome these shortfalls.
Data gathering
Canadian economic evaluations of CBT require comprehensive data including the epidemiology of mental disorders in Canada, the proportion of Canadians who seek care, the type and patterns of care received and associated treatment costs. Acute and long-term effectiveness data by subgroup, type of provider and format (e.g., individual versus group; treatment length) will also be important to assess treatment costs and effectiveness outcomes over time.
The epidemiologic data supporting numerous Australian cost-effectiveness analyses (Vos et al. 2005a; Heuzenroeder et al. 2004; Issakidis et al. 2004) resulted from a national survey of more than 10,000 households (Australian Bureau of Statistics 1998), reporting patterns and types of mental healthcare received. Analyses quantified the cost-effectiveness of treating all mentally ill patients seeking treatment with optimal care (featuring CBT) relative to the patterns of usual care dominated by medication.
A mental health survey of similar scale was undertaken in Canada (Gravel and Beland 2005). The Canadian Community Health Survey, administered to almost 37,000 Canadian households, determined that approximately 10% of Canadians used services for their mental health in a one-year period. However, of those Canadians who reported a mental disorder, only 40% sought treatment (Lesage et al. 2006). These data would be key inputs for Canadian economic analyses.
Most published economic analyses have used clinical trial data to estimate the expected magnitude of CBT treatment effects (Gould and Clum 1993; Gould 1997). Although these data constitute strong clinical evidence, they lack external validity. Economic and clinical outcomes data from the real-world setting are warranted.
Emerging data and assessment tools suggest that better CBT treatment outcomes can be achieved in specific subgroups of patients (Myhr et al. 2007). The ability to identify patients optimally suited to CBT a priori will improve cost-effectiveness ratios further because increased effectiveness would be achieved at lower total cost.
While clinical outcomes data can be shared across countries, resource utilization data should be local (Gold et al. 1996). Only two Canadian studies reporting resource utilization and costs in relation to treatment with CBT have been identified (Roberge et al. 2005, 2008). More Canadian studies of this type will be necessary.
CBT may be administered by psychologists, psychiatrists, general practice physicians, nurses or other mental health professionals working within diverse care settings, with treatment costs varying accordingly. However, professional accreditation says nothing about specific CBT training and competency. As yet, there is no Canadian CBT accreditation body. The Academy of Cognitive Therapy (ACT) in Philadelphia is a multidisciplinary, international certifying organization that specifically evaluates applicants' knowledge and ability in CBT before granting certification. At the time of this writing, only 54 CBT providers in Canada were formally accredited by ACT (2010). The vast majority of CBT practitioners in Canada currently practising are not accredited by any independent body certifying CBT competency. The reimbursement of CBT with public dollars will necessitate a more standardized approach to training and evaluations of competency. The number of qualified providers needed to meet current and future demands, and the affordability of reimbursing these services, will be key concerns. Surveys of Canadian professional associations, accreditation and licensing bodies, as well as cohort studies of treatment outcomes by type of CBT provider, may help fill these information gaps. A step in the right direction is the recent inception of the Canadian Association of Cognitive and Behavioural Therapists in 2009, whose membership list will ascertain self-identified practitioners of CBT.
Dissemination
Target audiences, which could include government representatives, regional or institutional health administrators, healthcare providers and patients, should be identified before research is begun to ensure that analysis parameters and outcome variables are relevant to them (Canadian Agency for Drugs and Technologies in Health 2006). Moreover, the source that communicates the evidence may be just as important as the information that is communicated. Surveys suggest that clinical opinion and published reviews may be preferred over advice from health economists and external organizations (Weatherly et al. 2002; Hoffman and Graf von der Schulenberg 2000). Canadian economic evidence may be more persuasive if evaluations are conducted by multidisciplinary research teams rather than economists working in isolation.
Effective dissemination of economic outcomes requires improved interpretability and transparency (Weatherly et al. 2002; Fattore and Torbica 2006). Many decision-makers report a lack of health economics knowledge (Zwart-van Rijkom et al. 2000; Hoffmann et al. 2002; Payne and Proskorovsky 2007). Thus, explanations of the practical relevance of economic evaluation results to decision-makers should be provided (Hoffman and Graf von der Schulenberg 2000). Communications describing methodologies, data sources and limitations of economic evaluations of CBT will need to meet these criteria.
Action
Health economic evidence amassed in support of greater access to CBT will not be sufficient to reform mental health funding. Decision-makers must act on this evidence. What are the Canadian barriers to action?
First, formal health economic analyses of CBT are lacking. Even if available, the channels for submission of this evidence are difficult to determine. This situation contrasts with the clearly defined procedures for medications, which are evaluated via the Common Drug Review process (Canadian Agency for Drugs and Technologies 2009). Evidence is also more likely to be implemented when it includes systematic reviews. To date, only one review of the health economic impact of CBT has been published (Myhr and Payne 2006). Funding policy reform is more likely if a coalition of healthcare providers and other interest groups work together towards the common goal of increased public access to CBT. In the United Kingdom, for example, a high-profile government commission is credited with achieving the reimbursement of CBT services with public dollars (Layard 2006). Other barriers to reform include inflexible budgets, the inability to free resources (Drummond et al. 1997; Hoffman and Graf von der Schulenberg 2000) and healthcare system fragmentation (Latimer 2005). Health economists must consider local financing structures and budgeting processes in order to make economic evaluations more realistic and applicable to those who use them (Duthie et al. 1999). A final hurdle to increased access to CBT may well be the affordability of actually meeting the demand.
Integral to the proposed research framework (Figure 1) is the need for more detailed information about the actual barriers to increasing access to CBT in this country. Carefully designed qualitative surveys of mental health decision-makers may be useful in this regard.
Discussion
Although there have been previous calls for increased access to publicly funded CBT for mental health disorders (Romanow and Marchildon 2003; Canadian Alliance on Mental Health and Mental Illness 2006), economic analyses of the potential impact of CBT on Canadians with mental illness have been lacking (Myhr and Payne 2006). Much work needs to be done. Canadian health economic analyses should be performed and, if favourable, decision-makers must act. Without funding policy reform, optimal mental healthcare will remain available only to Canadians who can afford it, rather than to those who may need it the most. Goals of the Canadian Mental Health Strategy include equitable and timely access to effective treatment.
The United Kingdom and Australia have already reformed their policies to reimburse CBT (Department of Health 2000; Policy and Strategy Directorate 2006). In these countries, health economic analyses have been instrumental in reforming policy, as have effective lobbying and high-profile calls for action. Richard Layard, a UK economist, has called for the large-scale deployment of evidence-based psychological therapies through National Health Service reimbursement of CBT providers and the establishment of psychological treatment centres (Layard 2006). The target of 10,000 new CBT providers and one treatment centre for every 250,000 people by the year 2013 has been set. It was hypothesized that treating more patients would result in enough cost savings (due to increased productivity and taxation) to cover the costs of CBT reimbursement. While some have argued against these ideas (Zinkler 2006; Taylor 2006; Joseph 2006), pilot psychological treatment centres have been implemented and will be evaluated. In Australia, population-based economic assessments have resulted in increased public access to CBT (Pirkis et al. 2004; Wagner et al. 2002).
Conclusion
Mental illness is debilitating to patients and families and costly to governments. Internationally, CBT has been shown to result in improved clinical and health economic outcomes – and in some circumstances even cost savings (Myhr and Payne 2006). The same outcomes are likely to be demonstrated in the Canadian context. To this end, a research framework has been proposed and a call to action has been made. The intent is to motivate, unify, focus and coordinate researchers who are seeking to offer Canadian decision-makers objective evidence to evaluate if CBT represents good clinical and economic value for public healthcare dollars spent. If the answer is yes, then current funding policy must be reformed. In accordance with the Canadian Mental Health Strategy, all Canadians must have equitable and timely access to effective evidence-based treatments.
Contributor Information
Krista A. Payne, Research Scientist & Director, Healthcare Data Capture, United BioSource Corporation, Dorval, QC.
Gail Myhr, Psychiatrist & Director, Cognitive Behaviourial Therapy Program, McGill University Health Centre, Montreal, QC.
References
- Academy of Cognitive Therapy (ACT). Welcome to the Academy of Cognitive Therapy Website. Philadelphia: Author; 2010. Retrieved January 26, 2010. < http://www.academyofct.org/Library/CertifiedMembers/Index.asp?Country=Canada&Action=States&FolderID=1137&SessionID={DBFECF93-7685-478B-8790-B5EB0E72D745}>. [Google Scholar]
- Australian Bureau of Statistics. 1998Mental Health and Well-being: Profile of Adults,Australia, 1997 Canberra: Author [Google Scholar]
- Canada Health Act. RSC; 1985. pp. C–6. c. [Google Scholar]
- Canadian Agency for Drugs and Technologies in Health. Guidelines for the Economic Evaluation of Health Technologies: Canada. 3rd ed. Ottawa: Author; 2006. Retrieved January 12, 2010. < http://www.cadth.ca/media/pdf/186_EconomicGuidelines_e.pdf>. [Google Scholar]
- Canadian Agency for Drugs and Technologies. Procedure for Common Drug Review. Ottawa: Author; 2009. Retrieved January 12, 2010 < http://www.cadth.ca/media/cdr/process/CDR_Procedure_e.pdf>. [Google Scholar]
- Canadian Alliance on Mental Health and Mental Illness. Recommendations to Health and Social Policy Leaders of Canada for a National Action Plan on Mental Illness and Mental Health. Ottawa: Author; 2006. Retrieved January 12, 2010. < http://www.camimh.ca/frameworkforaction.htm>. [Google Scholar]
- Canadian Institutes for Health Research (CIHR). Knowledge Translation Strategy 2004–2009. Innovation in Action. Ottawa: Author; 2004. Retrieved January 12, 2010. < http://www.cihr-irsc.gc.ca/e/26574.html#defining>. [Google Scholar]
- Department of Health. NHS Plan – A Plan for Investment, a Plan for Reform (2000–2010) London, UK: Author; 2000. Retrieved January 12, 2010. < http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyandGuidance/DH_4002960>. [Google Scholar]
- Drummond M., Cooke J., Walley T. Economic Evaluation Under Managed Competition. Evidence from the UK. Social Science and Medicine. 1997;45(4):583–95. doi: 10.1016/s0277-9536(96)00398-x. [DOI] [PubMed] [Google Scholar]
- Duthie T., Trueman P., Chancellor J., Diez L. Research into the Use of Health Economics in Decision Making in the United Kingdom, Phase II: Is Health Economics ‘for Good or Evil’? Health Policy. 1999;46(2):143–57. doi: 10.1016/s0168-8510(98)00057-8. [DOI] [PubMed] [Google Scholar]
- Evers S.M., Van Wijk A.S., Ament A.J. Economic Evaluation of Mental Health Care Intervention. A Review. Health Economics. 1997;6(2):161–77. doi: 10.1002/(sici)1099-1050(199703)6:2<161::aid-hec258>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Fattore G., Torbica A. Economic Evaluation in Healthcare: The Point of View of Informed Physicians. Value in Health. 2006;9(3):157–65. doi: 10.1111/j.1524-4733.2006.00096.x. [DOI] [PubMed] [Google Scholar]
- Gold M.R., Siegel J.E., Russell L.B., Weinstein M.C. Cost-Effectiveness in Health and Medicine. Oxford: Oxford University Press.; 1996. [Google Scholar]
- Gould R.A. Cognitive Behavioral and Pharmacological Treatment of Generalized Anxiety Disorder: A Preliminary Meta-Analysis. Behavior Therapy. 1997;28(2):285–305. [Google Scholar]
- Gould R.A., Clum G.A. A Meta-Analysis of Self-Help Treatment Approaches. Clinical Psychology Review. 1993;13(169):186. [Google Scholar]
- Gould R.A., Otto M.W., Pollack M.H. A Meta-Analysis of Treatment Outcome for Panic Disorder. Clinical Psychology Review. 1995;15(8):819–44. [Google Scholar]
- Gravel R., Beland Y. The Canadian Community Health Survey: Mental Health and Well-Being. Canadian Journal of Psychiatry. 2005;50(10):573–79. doi: 10.1177/070674370505001002. [DOI] [PubMed] [Google Scholar]
- Haby M.M., Carter R., Mihalopoulos C., Magnus A., Sanderson K., Andrews G., Vos T. Assessing Cost-Effectiveness – Mental Health: Introduction to the Study and Methods. Australian & New Zealand Journal of Psychiatry. 2004a;38(8):569–78. doi: 10.1080/j.1440-1614.2004.01420.x. [DOI] [PubMed] [Google Scholar]
- Haby M.M., Tonge B., Littlefield L., Carter R., Vos T. Cost-Effectiveness of Cognitive Behavioural Therapy and Selective Serotonin Reuptake Inhibitors for Major Depression in Children and Adolescents. Australian & New Zealand Journal of Psychiatry. 2004b;38(8):579–91. doi: 10.1080/j.1440-1614.2004.01421.x. [DOI] [PubMed] [Google Scholar]
- Haddock G., Barrowclough C., Tarrier N., Moring J., O'Brien R., Schofield N., Quinn J., Palmer S., Davies L., Lowens I., McGovern J., Lewis S. Cognitive-Behavioural Therapy and Motivational Intervention for Schizophrenia and Substance Misuse: 18-Month Outcomes of a Randomised Controlled Trial. British Journal of Psychiatry. 2003;183(5):418–26. doi: 10.1192/bjp.183.5.418. [DOI] [PubMed] [Google Scholar]
- Heuzenroeder L., Donnelly M., Haby M. Cost-Effectiveness of Psychological and Pharmacological Interventions for Generalized Anxiety Disorder and Panic Disorder. Australian & New Zealand Journal of Psychiatry. 2004;38(8):602–12. doi: 10.1080/j.1440-1614.2004.01423.x. [DOI] [PubMed] [Google Scholar]
- Hoffman C., Graf von der Schulenberg J.M. The Influence of Economic Evaluations on Decision Making. A European Survey. The EUROMET Group. Health Policy. 2000;52(179):192. doi: 10.1016/s0168-8510(00)00076-2. [DOI] [PubMed] [Google Scholar]
- Hoffmann C., Stoykova B.A., Nixon J., Glanville J.M., Misso K., Drummond M.F. Do Health-Care Decision Makers Find Economic Evaluations Useful? The Findings of Focus Group Research in UK Health Authorities. Value in Health. 2002;5(2):71–78. doi: 10.1046/j.1524-4733.2002.52109.x. [DOI] [PubMed] [Google Scholar]
- Hollon S.D., DeRubeis R.J., Shelton R.C., Amsterdam J.D., Salomon R.M., O'Reardon J.P., Lovett M.L., Young P.R., Haman K.L., Freeman B.B., Gallop R. Prevention of Relapse Following Cognitive Therapy vs. Medications in Moderate to Severe Depression. Archives of General Psychiatry. 2005;62(4):417–22. doi: 10.1001/archpsyc.62.4.417. [DOI] [PubMed] [Google Scholar]
- Hunsley J. Ottawa: Canadian Psychological Association; 2002. May, The Cost-Effectiveness of Psychological Interventions. Retrieved January 12, 2010. < http://www.cpa.ca/cpasite/userfiles/Documents/Practice.../Cost_Effectiveness.pdf>. [Google Scholar]
- Issakidis C., Sanderson K., Corry J., Andrews G., Lapsley H. Modelling the Population Cost-Effectiveness of Current and Evidence-Based Optimal Treatment for Anxiety Disorders. Psychological Medicine. 2004;34(1):19–35. doi: 10.1017/s003329170300881x. [DOI] [PubMed] [Google Scholar]
- Jacobs P., Yim R., Ohinmaa A., Eng K., Dewa C.S., Bland R., Block R., Slomp M. Expenditures on Mental Health and Addictions for Canadian Provinces in 2003 and 2004. Canadian Journal of Psychiatry. 2008;53(5):306–13. doi: 10.1177/070674370805300505. [DOI] [PubMed] [Google Scholar]
- Joseph S.A. Psychological Treatment Centres: The Case Against. British Medical Journal. 2006;332(7550):1154–55. doi: 10.1136/bmj.332.7550.1154-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katon W., Russo J., Sherbourne C., Stein M.B., Craske M., Fan M., Roy-Byrne P. Incremental Cost-Effectiveness of a Collaborative Care Intervention for Panic Disorder. Psychological Medicine. 2006;36(3):353–63. doi: 10.1017/S0033291705006896. [DOI] [PubMed] [Google Scholar]
- Lam D.H., McCrone P., Wright K., Kerr N. Cost-Effectiveness of Relapse-Prevention Cognitive Therapy for Bipolar Disorder: 30-Month Study. British Journal of Psychiatry. 2005;186(6):500–06. doi: 10.1192/bjp.186.6.500. [DOI] [PubMed] [Google Scholar]
- Langley P.C. Is Cost-Effectiveness Modeling Useful? American Journal of Managed Care. 2000;6(2):250–51. [PubMed] [Google Scholar]
- Latimer E. Organizational Implications of Promoting Effective Evidence-Based Interventions for People with Severe Mental Illness. Canadian Public Policy. 2005;31:S47–S52. [Google Scholar]
- Layard R. The Case for Psychological Treatment Centres. British Medical Journal. 2006;332(7548):1030–32. doi: 10.1136/bmj.332.7548.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesage A., Vasiliadis H.M., Gagne M.A., Dudgeon S., Kasman N., Hay C. Prevalence of Mental Illnesses and Related Service Utilization in Canada: An Analysis of the Canadian Community Health Survey. Mississauga, Ontario, Canada: 2006. Report prepared for the Canadian Collaborative Mental Health Initiative. [Google Scholar]
- Lynch F.L., Hornbrook M., Clarke G.N., Perrin N., Polen M.R., O'Connor E., Dickerson J. Cost-Effectiveness of an Intervention to Prevent Depression in At-Risk Teens. Archives of General Psychiatry. 2005;62(11):1241–48. doi: 10.1001/archpsyc.62.11.1241. [DOI] [PubMed] [Google Scholar]
- Mental Health Commission of Canada. Toward Recovery and Well-Being. A Framework for a Mental Health Strategy for Canada 2009 Nov; [Google Scholar]
- Myhr G., Payne K. Cost-Effectiveness of Cognitive-Behavioural Therapy for Mental Disorders: Implications for Public Healthcare Funding Policy in Canada. Canadian Journal of Psychiatry. 2006;51(10):662–70. doi: 10.1177/070674370605101006. [DOI] [PubMed] [Google Scholar]
- Myhr G., Talbot J., Annable L., Pinard G. Suitability for Short-Term Cognitive-Behavioral Therapy. Journal of Cognitive Psychotherapy. 2007;21(4):334–45. [Google Scholar]
- Otto M.W. Combined Psychotherapy and Pharmacotherapy for Mood and Anxiety Disorders in Adults: Review and Analysis. Clinical Psychology: Science & Practice. 2005;12(1):72–86. [Google Scholar]
- Otto M.W., Pollack M.H., Maki K.M. Empirically Supported Treatments for Panic Disorder: Costs, Benefits, and Stepped Care. Journal of Consulting & Clinical Psychology. 2000;68(4):556–63. [PubMed] [Google Scholar]
- Payne K.A., Proskorovsky I. A Health Economics Survey of European Hospital Pharmacists. European Journal of Hospital Pharmacy Science. 2007;13:33–39. [Google Scholar]
- Pirkis J., Livingston J., Herrman H., Schweitzer I. et al. Improving Collaboration between Private Psychiatrists, the Public Mental Health Sector and General Practitioners: Evaluation of the Partnership Project. Australian & New Zealand Journal of Psychiatry. 2004;38(3):125–34. doi: 10.1080/j.1440-1614.2004.01314.x. [DOI] [PubMed] [Google Scholar]
- Policy and Strategy Directorate, Department of Health. Health Reform in England: Update and Commissioning Framework. London, UK: Author; 2006. Retrieved January 12, 2010. < http://www.dh.gov.uk/fs/en?CONTENT_ID=4137226&chk=D2YSig>. [Google Scholar]
- Revicki D.A., Siddique J., Frank L., Chung J.Y., Green B.L., Krupnick J., Prasad M., Miranda J. Cost-Effectiveness of Evidence-Based Pharmacotherapy or Cognitive-Behavior Therapy Compared with Community Referral for Major Depression in Predominantly Low-Income Minority Women. Archives of General Psychiatry. 2005;62(8):868–75. doi: 10.1001/archpsyc.62.8.868. [DOI] [PubMed] [Google Scholar]
- Roberge P., Marchand A., Reinharz D., Cloutier K., Mainguy N., Miller J.-M., Begin J., Turcotte J. Healthcare Utilization Following Cognitive-Behavioral Treatment for Panic Disorder with Agoraphobia. Cognitive Behaviour Therapy. 2005;34(2):79–88. doi: 10.1080/16506070510008443. [DOI] [PubMed] [Google Scholar]
- Roberge P., Marchand A., Reinharz D., Savard P. Cognitive-Behavioral Treatment for Panic Disorder with Agoraphobia: A Randomized, Controlled Trial and Cost-Effectiveness Analysis. Behavior Modification. 2008;32(3):333–51. doi: 10.1177/0145445507309025. [DOI] [PubMed] [Google Scholar]
- Romanow R.J., Marchildon G.P. Psychological Services and the Future of Health Care in Canada. Canadian Psychology. 2003;44(4):283–95. [Google Scholar]
- Sanderson K., Andrews G., Corry J., Lapsley H. Reducing the Burden of Affective Disorders: Is Evidence-Based Health Care Affordable? Journal of Affective Disorders. 2003;77(2):109–25. doi: 10.1016/s0165-0327(03)00134-4. [DOI] [PubMed] [Google Scholar]
- Scott J., Palmer S., Paykel E., Teasdale J., Hayhurst H. Use of Cognitive Therapy for Relapse Prevention in Chronic Depression. Cost-Effectiveness Study. British Journal of Psychiatry. 2003;182(3):221–27. doi: 10.1192/bjp.182.3.221. [DOI] [PubMed] [Google Scholar]
- Taylor S. Psychological Treatment Centres: Quality of Psychological Treatment Is Important. British Medical Journal. 2006;332(7550):1155. doi: 10.1136/bmj.332.7550.1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trueman P., Drummond M., Hutton J. Developing Guidance for Budget Impact Analysis. Pharmacoeconomics. 2001;19(6):609–21. doi: 10.2165/00019053-200119060-00001. [DOI] [PubMed] [Google Scholar]
- Turkington D., Kingdon D., Turner T. Effectiveness of a Brief Cognitive-Behavioural Therapy Intervention in the Treatment of Schizophrenia. British Journal of Psychiatry. 2002;180:523–27. doi: 10.1192/bjp.180.6.523. [DOI] [PubMed] [Google Scholar]
- Von Korff M., Katon W., Bush T., Lin E.H., Simon G.E., Saunders K., Ludman E., Walker E., Unutzer J. Treatment Costs, Cost Offset, and Cost-Effectiveness of Collaborative Management of Depression. Psychosomatic Medicine. 1998;60(2):143–49. doi: 10.1097/00006842-199803000-00005. [DOI] [PubMed] [Google Scholar]
- Vos T., Corry J., Haby M.M., Carter R., Andrews G. Cost-Effectiveness of Cognitive-Behavioural Therapy and Drug Interventions for Major Depression. Australian & New Zealand Journal of Psychiatry. 2005a;39(8):683–92. doi: 10.1080/j.1440-1614.2005.01652.x. [DOI] [PubMed] [Google Scholar]
- Vos T., Haby M.M., Magnus A., Mihalopoulos C., Andrews G., Carter R. Assessing Cost-Effectiveness in Mental Health: Helping Policy-Makers Prioritize and Plan Health Services. Australian & New Zealand Journal of Psychiatry. 2005b;39(8):701–12. doi: 10.1080/j.1440-1614.2005.01654.x. [DOI] [PubMed] [Google Scholar]
- Wagner R.W., Manicavasagar V., Silove D. Challenges and Early Experiences in the Development of an Anxiety Clinic in the Public Health Sector. General Hospital Psychiatry. 2002;24(6):406–11. doi: 10.1016/s0163-8343(02)00214-1. [DOI] [PubMed] [Google Scholar]
- Weatherly H., Drummond M., Smith D. Using Evidence in the Development of Local Health Policies. Some Evidence from the United Kingdom. International Journal of Technology Assessment in Health Care. 2002;18(4):771–81. doi: 10.1017/s0266462302000582. [DOI] [PubMed] [Google Scholar]
- Wykes T., Steel C., Everitt B., Tarrier N. Cognitive Behavior Therapy for Schizophrenia: Effect Sizes, Clinic Models, and Methodological Rigor. Schizophrenia Bulletin. 2008;34(3):523–37. doi: 10.1093/schbul/sbm114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinkler M. Psychological Treatment Centres: May Be Less Effective Than Suggested. Comment. British Medical Journal. 2006;332(7550):1155. doi: 10.1136/bmj.332.7550.1155-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwart-van Rijkom J.E., Leufkens H.G., Busschbach J.J., Broekmans A.W., Rutten F.F. Differences in Attitudes, Knowledge and Use of Economic Evaluations in Decision-Making in the Netherlands. The Dutch Results from the EUROMET Project. Pharmacoeconomics. 2000;18(2):149–60. doi: 10.2165/00019053-200018020-00005. [DOI] [PubMed] [Google Scholar]