Abstract
Background
Parenting interventions have achieved changes in factors associated with childhood obesity but few have tested the effects on multiple parental influences.
Purpose
This study examined the efficacy of an intervention aimed at improving several dimensions of parenting related to childhood obesity.
Design
2×2 factorial study design
Setting/Participants
In 2003, thirteen Southern California schools were randomized to one of four conditions: micro-environment only, macro-environment only, micro-plus-macro–environment, and no treatment control condition. Participants included 811 predominantly Mexican immigrant/Mexican-American mothers with children in grades kindergarten through second grade.
Intervention
In both micro conditions, participants received monthly home visits by a promotora over a 7-month period plus monthly mailed newsletters.
Main outcome measures
In 2008, intervention effects were examined on: (1) parenting strategies including limit setting, monitoring, discipline, control, and reinforcement related to children’s diet and physical activity; (2) parental support for physical activity; (3) parent-mediated family behaviors such as family meals eaten together and TV watching during family dinners; and (4) perceived barriers and other parent cognitions related to children’s eating and activity.
Results
At the 2-year follow-up, significant improvements were observed in three of five parenting strategies, parental support, and two of four parent-mediated family behaviors among parents receiving the micro intervention (i.e., those who received promotora visits and monthly newsletters), as compared with those in the macro-only and control conditions.
Conclusions
Aspects of parenting related to children’s risk for obesity and related health outcomes are modifiable with the support of a promotora and print media.
INTRODUCTION
The prevalence of overweight and obesity among U.S. children, especially pronounced among Mexican-American youth1, necessitates the implementation of interventions that target factors contributing to this epidemic. Socio-Ecological theory2, as well as frameworks presented by Rhee3, Ventura and Birch4 and Birch and Davison,5 indicate that parenting is among the most important family-level determinants of childhood obesity. At least five mechanisms by which Latino parents influence their children’s risk for obesity have been identified: (1) parenting style (a more indulgent parenting style is associated with greater risk for obesity6,7); (2) parenting strategies (parents who use more monitoring, more positive reinforcement, and less controlling parenting strategies have children who consume a healthier diet and are more physically active8); (3) provision of instrumental support (more instrumental support for physical activity is associated with normal weight9); (4) family behaviors (parents who purchase fast food for consumption at home at least once per week or more have children who consume more soda and more fat10); and (5) modeling of health behaviors (parents and children who eat away-from-home foods at least once per week or more versus less frequently are at greater risk for being overweight/obese11). These family-level determinants demonstrate that health status is determined, in part, by social and structural aspects of the home and community environments.12–16
Interventions targeting parenting for childhood obesity
Several interventions have targeted parenting skills related to childhood obesity,17–21 yet few have examined changes in parenting18,20,22 and others did not target parenting explicitly although intervention activities were directed at the parents.23–25 One study determined that changes in childhood weight were explained, in part, by reductions in mothers’ use of a permissive parenting style.18 Reductions have been noted in the use of restrictive child feeding practices subsequent to an intervention22, although in another study no intervention effects were observed on parents’ modeling of healthy behaviors.20 Moreover, most of these parenting interventions were delivered by highly trained professionals (e.g., clinician dietitians and social workers,18 early childhood specialist20), making it difficult to conclude that similar results could be achieved with intervention agents that do not have such formal training.
Present Study
The present study describes the implementation and long-term efficacy of a childhood obesity intervention targeting parental influences facilitated by promotoras. Specifically, this study examined the extent to which promotoras facilitate changes on four dimensions of parenting associated with childhood obesity risk: parenting strategies, parental support, parent-mediated family behaviors, and cognitive factors (i.e., perceptions). The promotora model involves community members who live among or at least are similar to the target population providing effective informational, instrumental and emotional support for health behavior change 26–30,31 and 31–33.
METHODS AND PROCEDURES
Study Design
The Aventuras para Niños [APN] study was an RCT with schools randomized to one of four conditions: micro-environmental change, macro-environmental change, micro-plus-macro–environmental change, and a no-treatment control condition34. The micro intervention targeted the home environment as described in detail below. The macro intervention targeted the school and community environments via physical and social changes (e.g., school: training of school personnel to promote healthy eating; community: child menus in local restaurants). The main outcome of the study was child BMI. Parenting variables, as described in this paper, and the child’s eating and activity behaviors were the primary behavioral targets of change. Thirteen public elementary schools were randomized to condition and 811 families were recruited from among those with children in kindergarten, 1st, or 2nd grade to serve in the evaluation cohort. Recruitment occurred in two waves, the first from August 2003 to January 2004, and the second from May 2004 to December 2004. The study was funded by the National Heart Lung and Blood Institute and all study protocols were approved by the IRB at San Diego State University.
Recruitment and Eligibility Screening
Study activities occurred in the South Bay region of San Diego County near the U.S.–Mexico border. The South Bay region encompasses 297,456 residents, 58.4% of whom identify as Hispanic or Latino.35 All schools in the target region were identified and screened for the following eligibility criteria: (1) Latino enrollment of at least 70%; (2) a defined attendance boundary (no charter or magnet schools); and (3) no other obesity-prevention programs or additional physical education training for teachers within the past 4 years. The Project Manager and Intervention Coordinator contacted the principal of each school, presented the study objectives and methods, determined inclusion criteria, and obtained consent to participate and be randomized to one of the four conditions. Twenty-five schools were identified, five were deemed ineligible given involvement in similar interventions, and seven refused to participate.
Parents were recruited directly on school grounds, during school presentations, and through fliers sent home with students. Eligible families had a child in kindergarten, first or second grade at one of the 13 schools; had no major health problems that limited participation, lived within the school attendance boundaries, and intended to stay in the area for at least 1 year. Parents received an incentive of $20 to enroll and complete the baseline survey.
Micro Intervention Methods
Micro intervention activities were delivered by eight promotoras. Promotora recruitment and selection occurred through schools to ensure their intimate knowledge of nearby relevant neighborhood resources and barriers. Additional inclusion criteria included female gender with a child attending the school, willingness to commit to the project for 1 academic year, ability to speak and read Spanish and English, having transportation, and basic literacy. Candidates were screened using a self-administered survey to assess basic literacy, followed by an interview with the Project Manager to assess important interpersonal skills.36 Several promotoras were known to study staff because of a previous working relationship or came highly recommended due to their experience in community-based health promotion.
Promotoras received 22 hours of training delivered over 11 sessions using a project-developed curriculum on behavior change, childhood obesity, and child nutrition and physical activity needs. The curriculum was informed by previous studies37,38, as well Social Cognitive Theory39 and the Socio-Ecologic Framework2. Promotora training included an orientation to the structure of and materials for the family home visits, as well as opportunities to role-play. Biweekly meetings occurred with the Intervention Coordinator throughout the intervention period to continue promotora skill building and troubleshoot difficult situations. On any given month, each promotora worked with 12 to 30 families depending on her availability. The promotoras were paid a flat rate of $14.00 per completed visit, based on an average of 1.5 hours per visit, plus a stipend for mileage.
Each participating family was assigned a promotora, who visited the home during 7 consecutive months over the course of 1 school year. At each visit, the promotora reviewed a four-page newsletter, provided other materials and guided the parent in setting incremental goals for the next month to improve the family’s lifestyle. The seven newsletters covered themes ranging from access to and availability of healthy options in the home to media messages and unhealthy food options. The newsletters used a story format with photographs depicting the lives of a real local family attempting to make similar changes. The health messages focused on increasing fruit and vegetable consumption, increasing water consumption instead of sugar-sweetened beverages, decreasing TV viewing and increasing active play. Targeted environmental changes included physical changes such as having cut veggies within a child's reach and moving a TV out of a child's bedroom, as well as social/policy changes such as rules and boundaries set by parents, discipline methods and use of positive reinforcement, and family recreation and eating habits.
All the materials and interpersonal interactions with the promotoras were in Spanish or English, depending on the family’s preference. If participants asked to discontinue the home visits, they were given the option of receiving the newsletter and other materials by mail; 23% switched to that option at some point, most saying that they did not have time for the home visits.
Following the monthly home visits, family intervention involvement continued in the form of four booster calls delivered over a 2-year period. Booster call training included a brief session on motivational interviewing techniques.40 The promotora called the parent three times during the school year and once more the following Fall to review points made during the home visits, asking about the family’s experience with changes made and setting further goals for improvement. A hand-written reminder of the new goals and the family’s most recent accomplishments was mailed to the parent within a few days. Continuity of promotora–family relationships was maintained wherever possible, and when promotora turnover required that a new promotora make the calls, she was given a folder with notes from all previous contacts.
Evaluation Procedures
Data were collected at four time points: baseline, immediate post-intervention (M2), 1-year follow-up (M3) and 2-year follow-up (M4). At their children’s school or their homes, parents completed a self-administered survey available in Spanish and English that took approximately 60 minutes to complete. Bilingual and bicultural evaluation assistants were available to help answer questions. Approximately 90% of the data collection occurred on school grounds at baseline, 79% at M2, 70% at M3, and 66% at M4.
Measures
Parenting strategies for eating and activity was measured with a 26-item scale developed for this project using qualitative and quantitative methods41. This measure consists of five subscales: limit setting (n=6), monitoring (n=7), discipline (n=5), control (n=6), and reinforcement (n=2). Response options include frequency (e.g., monitoring: 1=never to 5=always) and strength of agreement (discipline: 1=strongly disagree to 5=strongly agree) options. A mean score for each subscale was calculated and alpha coefficient for each subscale ranged from 0.73 to 0.87 suggesting moderate to good internal consistency.
Parental support for child physical activity was measured with three questions: on how many days parents provide encouragement, transportation, and/or actively participate in physical activity with their child. Response options ranged from 1 to 7 days per week. A total instrumental support score was created by summing the three questions. Previous analyses indicated that frequency of parental support was associated with perceptions that the child was more physically active than his/her peers.8
Away-from-home eating was measured with five questions developed in a previous study42 that asked how frequently families ate away-from-home foods obtained from five different settings: relatives’ homes, neighbors’/friends’ homes, sit down restaurants, fast-food restaurants, and restaurants in Mexico. Each question was presented with response options ranging from 1=never to 5=5 to 7 times per week and each question was then dichotomized to reflect whether the family consumed away-from-home foods at least once per week or more versus less than once per week in each setting, based on evidence linking at least weekly consumption of away-from-home food with BMI.43 Each dichotomous score was then used to create a final sum score reflecting the number of locations where away-from-home foods are consumed on a weekly basis.
Parent report on number of family meals consumed together was assessed using three yes/no questions on whether the family consumed breakfast, lunch, and dinner together at least four times a week or more. The three items were summed to create a total meals score. Parent report of giving money to purchase snacks was assessed using response options of 1=never to 7=5–7 times per week. Parent report of the family watching the TV while eating dinner was assessed with one question with a response option of 1=never to 5=very often. All three were developed in a previous study with the target population and were found to be related to children’s dietary intake.10
Two cognitive factors, parent-perceived barriers and parent-perceived self-efficacy to provide healthy food and physical activity options for their children, were assessed with 10 and 14 items respectively. For barriers, response options ranged from 1=strongly disagree to 5=strongly agree (α= .75). For self-efficacy, response options ranged from 1=not at all confident to 5=extremely confident (α= .91). These variables were modified based on a previous study which found significant changes in perceived barriers44; modifications to the scales reflected a focus on the child.
Demographic variables
Parents responded to open- and closed-ended questions on the following variables which were then recoded as follows: parent and child age and gender, marital status (married or living as married versus not married), household income (less or greater than $1,720/month), level of education (< high school versus > high school), employment status (employed versus unemployed), and parent and child country of origin.
Statistical Analysis
All analyses were based on the intention-to-treat approach. Each outcome was examined using mixed effects models for normal outcomes or generalized linear mixed effects models for nonnormal outcomes. Models accounted for repeated measures over M2 to M4 and adjusted for the M1 (baseline) level. All available data were utilized. Thus, although a participant may have data missing at M2, M3 or M4, data available at nonmissing time points were still included in the analysis. All models adjusted for parent and child age and gender, language of survey, marital status, household size, employment status, education status, homeowner, household income, and child generation status. In addition, all models adjusted for clustering at the school level. Terms were included in the model to account for the study design consisting of a 2×2 factorial (micro: yes versus no, and macro: yes versus no) and to account for and study time trends. Modeling began with a model including the time by macro by micro interaction and all lower-order terms. Nonsignificant terms (p>.05) were eliminated in a hierarchic manner.
RESULTS
Participant characteristics and retention rates
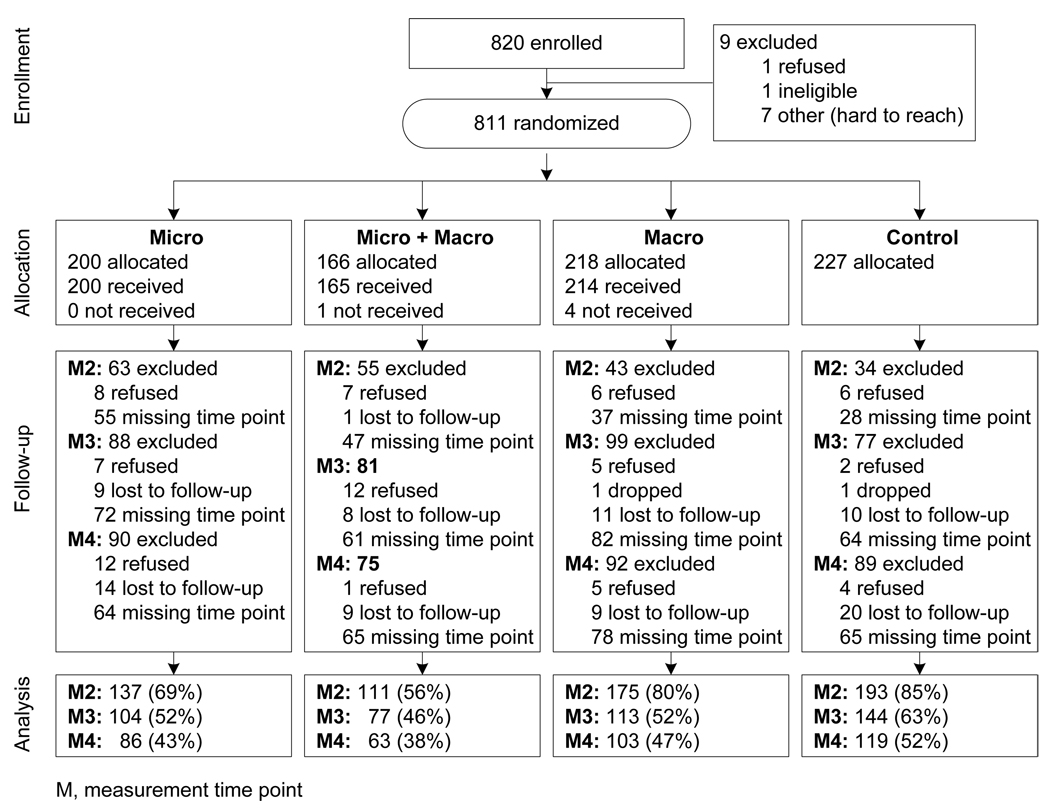
Table 1 illustrates the sample demographic characteristics. Approximately 71% of the parents identified as Latino and completed the survey in Spanish. Figure 1 depicts the study's CONSORT table. At M2, data were missing from 24% (n=195) of the baseline sample; at M3, 44% (n=345) of the retained sample; and at M4, 48% (n=346) of the retained sample. Primary analyses are based on data from baseline to M4 representing an overall retention rate of 45% and condition-specific retention rates of 43% (micro), 38% (micro–macro) 47% (macro only) and 52% (control). Analyses comparing families who remained in the intervention through M4 versus those who dropped out indicated that children retained in the study had parents who were married (p≤.01), not employed outside the home (p≤.001), and were homeowners (p≤.05). These parents were also more traditionally Mexican (p≤.05), had lived in the U.S. for fewer years (p≤.01) or were foreign born (p≤.05), and had children who were foreign-born (p≤.01). Parent or child age, parent or child gender, parent education, family income, household size and access to transportation were not associated with retention.
Table 1.
Child and parent demographics characteristics
| Children | Parents | |
|---|---|---|
| Median age, years | 6 | 33 |
| % women | 49% (399) | 97% (779) |
| % married or living as married | N/A | 77% (618) |
| % living in poverty (< $1,720/family of 4) | N/A | 35% |
| % completed less than high school | N/A | 35% (279) |
| % employed outside the home (vs homemaker) | N/A | 38% (306) |
| % born outside of U.S | 14% (109) | 71% (570) |
| Median household size | N/A | 5.00 (2–13) |
Figure 1.
CONSORT table reflecting study recruitment and retention based on analytic groupings
Intervention Effects
Table 2 shows the results for each parenting variable tested and Table 3 displays the mean and SD by condition at baseline and differences from baseline for significant outcomes identified in Table 2. One group-by-time interaction was significant: parents in the micro condition reported the largest increases in use of positive reinforcement at M2 with slight decreases observed at each subsequent time point. By M4, parents in the micro–macro condition reported more frequent use of positive reinforcement compared with parents in all other conditions.
Table 2.
Parenting outcomes involving micro-level intervention differences from baseline to 2-year follow-up
| Outcome | Tests of hypotheses involving the micro effect | Adjusted M (SE) | ||||
|---|---|---|---|---|---|---|
| Time × Micro × Macro Interaction |
Micro × Macro Interaction |
Time by Micro Interaction |
Micro Main Effect |
Micro intervention |
No micro intervention |
|
| Limit setting of diet and PA |
ns | ns | ns | ns | ||
| Monitoring of diet and PA |
ns | ns | ns | .014 | 4.01 (.051) | 3.87 (.048) |
| Discipline for diet and PA |
ns | ns | ns | ns | ||
| Control of diet and PA |
ns | ns | ns | ≤.001 | 2.34 (.072) | 2.65 (.067) |
| Reinforcement for diet and PA |
.012 | ns | ns | .002 | 4.13 (.065) | 3.92 (.061) |
| Parental support for PA |
ns | ns | ns | ≤.001 | 3.82 (.079) | 3.45 (.073) |
| Away from home foods |
ns | ns | ns | .045 | 0.74 (.077) | 0.91 (.072) |
| Family watches TV during dinner |
ns | ns | ns | .006 | 2.59 (.066) | 2.77 (.062) |
| Parent gives money for snacks |
ns | ns | ns | ns | ||
| Number of family meals together |
ns | ns | ns | ns | ||
| Parent- perceived barriers |
ns | ns | ns | ns | ||
| Parent- perceived self- efficacy |
ns | ns | ns | ns | ||
ns = not significant at ≤ .05. All tests were carried out using mixed effects models. The models accounted for repeated measures over M2 to M4 and adjusted for the M1 (baseline) level. All models adjusted for clustering at the school level and for language version of survey, parent gender and age, marital status, household size, employment status, education status, homeowner, household income, and child gender, age and generation status.
Table 3.
Descriptive statistics for parenting outcomes with significant findings by condition and time period
| Condition | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Micro + Macro | Micro only | Macro only | Control | ||||||
| Outcome | Time | M | SD | M | SD | M | SD | M | SD |
| Monitoring of diet and PA | M1 | 3.92 | 0.79 | 3.80 | 0.83 | 3.76 | 0.80 | 3.88 | 0.76 |
| M2–M1 | +.19 | +.32 | +.12 | +.04 | |||||
| M3–M1 | +.16 | +.21 | +.18 | +.03 | |||||
| M4–M1 | +.14 | +.12 | +.10 | +.13 | |||||
| Control of diet and PA | M1 | 2.99 | 1.10 | 2.99 | 1.08 | 2.90 | 1.15 | 2.97 | 1.07 |
| M2–M1 | −.38 | −.48 | +.05 | −.10 | |||||
| M3–M1 | −.49 | −.68 | −.24 | −.19 | |||||
| M4–M1 | −.50 | −.57 | −.31 | −.35 | |||||
| Reinforcement for diet and PA | M1 | 3.76 | 1.23 | 3.69 | 1.20 | 3.69 | 1.09 | 3.84 | 1.09 |
| M2–M1 | +.40 | +.58 | +.31 | +.15 | |||||
| M3–M1 | +.28 | +.48 | +.40 | +.05 | |||||
| M4–M1 | +.47 | +.36 | +.16 | +.12 | |||||
| Parental support for PA | M1 | 3.24 | 1.74 | 3.08 | 1.54 | 2.86 | 1.55 | 2.77 | 1.54 |
| M2–M1 | +.74 | +.84 | +.62 | +.61 | |||||
| M3–M1 | +.93 | +.72 | +.60 | +.72 | |||||
| M4–M1 | +.65 | +.76 | +.45 | +.94 | |||||
| Away from home foods | M1 | 0.90 | 1.02 | 1.03 | 1.12 | 1.04 | 1.14 | 1.03 | 1.21 |
| M2–M1 | +.01 | −.29 | −.03 | −.12 | |||||
| M3–M1 | −.08 | −.24 | −.04 | −.15 | |||||
| M4–M1 | −.10 | −.35 | −.19 | −.06 | |||||
| Family watches TV at dinner | M1 | 2.80 | 1.19 | 2.76 | 1.26 | 2.87 | 1.21 | 2.82 | 1.23 |
| M2–M1 | −.30 | −.10 | −.17 | −.14 | |||||
| M3–M1 | −.49 | −.23 | −.21 | −.14 | |||||
| M4–M1 | −.55 | −.14 | −.03 | −.14 | |||||
Significant micro main effects were observed on two of the four remaining parenting strategies, parental support, and two of four parent-mediated family behaviors. With respect to parenting strategies, the adjusted mean (+ SE) for monitoring among those receiving the micro intervention (micro or micro–macro) was significantly higher (4.01+.05) compared to those not receiving this intervention (3.87+.05). Similarly, the adjusted mean (+ SE) for use of controlling parenting strategies among those receiving the micro intervention was significantly lower (2.34+.07) than among those not receiving this intervention (2.66+.07).
Significant micro main effects were observed for parental support and two of the four parent-mediated family behaviors. The adjusted mean (± SE) for providing instrumental support for physical activity among those receiving the micro intervention was significantly higher (3.82±.08) compared to those not receiving this intervention (3.45±.07). The adjusted mean (± SE) for purchasing away-from-home foods was significantly lower (0.74±.08) among micro condition participants compared to those not receiving this intervention (0.91±.07). And, the adjusted mean (± SE) for watching TV during dinner was significantly lower (2.59±.07) among those receiving the micro intervention compared to those not receiving this intervention (2.77±.06).
DISCUSSION
It was found that the promotoras can successfully improve several dimensions of parenting. Parents who received the promotora visits reported more frequent monitoring of their child’s diet and physical activity, use of positive reinforcement, and instrumental support for physical activity; and less use of controlling strategies, consumption of away-from-home foods, and watching of TV during dinner. However, no changes were observed in the cognitive factors. These findings are encouraging because they suggest that a promotora-mediated intervention can improve several dimensions of parenting that are associated with a child’s risk for obesity.4
Limitations
The study’s attrition rate was higher than rates obtained in previous studies36,47. However, it was not inconsistent with other published work (e.g., 23% attrition at the 1-year follow-up17). Here, the attrition rate was higher among children whose parents were single, employed outside the home, renting, and involved in the intervention condition. This study was conducted on the U.S.–Mexico border where families are known to move between the two countries; particularly those who do not own a home in the U.S. In a previous study, it was observed that women who were employed received fewer home visits by a promotora48, indicating the need to further examine under what conditions the promotora model is most effective. Similarly, the finding regarding preferences for newsletters versus home visits among 23% of the micro condition parents reflects a problem observed in other research.17 This suggests that at least among some families, home visits may be too burdensome. A final limitation of this study is its reliance on self-report data. It is possible that parents who received the micro intervention depicted more socially desirable behaviors; however, the evaluation assistants were blinded to intervention condition.
Future Directions
Parenting interventions can help address the obesity epidemic among U.S. Latinos, as family-focused interventions are consistent with a cultural emphasis on the family and the group. Familismo, the concept that both immediate and extended family members are central to one’s personal identity, 49 and collectivism/ interdependence, a related concept implying the prioritization of the needs of the group over his/her own needs, may explain the relatively stronger familial aggregation of eating habits50 and physical activity behaviors.51 Future parenting interventions should consider methods for involving other family members, including how best to involve the father.52
To our knowledge, this is the first study to identify the promotora model as a viable approach to improve parenting influences associated with childhood obesity, although similar changes have been documented in asthma management.32 With the movement toward the integration of promotoras into the healthcare workforce53, programs such as these have the potential to be sustained in nonresearch settings. Building the evidence for meaningful and long-term parenting changes through promotora-led initiatives may help reduce disparities in childhood obesity.
Acknowledgements
This Aventuras para Niños study was funded by the National Heart Lung and Blood Institute (5R01HL073776). Additional support was provided to Dr. Ayala by the American Cancer Society (RSGPB 113653), to Dr. Arredondo by the American Cancer Society (PFT-04-156-01) and to Mr. Crespo by the National Institute of Diabetes and Digestive and Kidney Diseases (F31DK079345). No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of Overweight and Obesity in the U.S., 1999–2004. JAMA. 2006;295(13):1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996 Mar–Apr;10(4):282–298. doi: 10.4278/0890-1171-10.4.282. [DOI] [PubMed] [Google Scholar]
- 3.Rhee K. Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. The ANNALS of the American Academy of Political and Social Science. 2008;615(1):11–37. [Google Scholar]
- 4.Ventura AK, Birch LL. Does parenting affect children's eating and weight status? Int J Behav Nutr Phys Act. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatric Clinics of North America. 2001;48(4):893–907. doi: 10.1016/s0031-3955(05)70347-3. [DOI] [PubMed] [Google Scholar]
- 6.Hughes SO, Power TG, Fisher JO, Mueller S, Nicklas TA. Revisiting a neglected construct: parenting styles in a child-feeding context. Appetite. 2005;44(1):83–92. doi: 10.1016/j.appet.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Sherman JB, Alexander MA, Dean AH, Kim M. Obesity in Mexican-American and Anglo children. Prog Cardiovasc Nurs. 1995 Winter;10(1):27–34. [PubMed] [Google Scholar]
- 8.Arredondo EM, Elder JP, Ayala GX, Campbell N, Baquero B, Duerksen S. Is parenting style related to children's healthy eating and physical activity in Latino families? Health Educ Res. 2006 Dec;21(6):862–871. doi: 10.1093/her/cyl110. [DOI] [PubMed] [Google Scholar]
- 9.Elder JP, Arredondo EM, Campbell N, Baquero B, et al. Individual, family, and community environmental correlates of obesity in Hispanic elementary school children. Journal of School Health. doi: 10.1111/j.1746-1561.2009.00462.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ayala GX, Baquero B, Arredondo EM, Campbell N, Larios S, Elder JP. Association between family variables and Mexican American children's dietary behaviors. J Nutr Educ Behav. 2007 Mar–Apr;39(2):62–69. doi: 10.1016/j.jneb.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 11.Ayala GX, Rogers M, Arredondo EM, et al. Away-from-home food intake and risk for obesity: examining the influence of context. Obesity (Silver Spring) 2008 May;16(5):1002–1008. doi: 10.1038/oby.2008.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spence JC, Cutumisu N, Edwards J, Evans J. Influence of neighbourhood design and access to facilities on overweight among preschool children. International Journal of Pediatric Obesity. 2008;3(2):109–116. doi: 10.1080/17477160701875007. [DOI] [PubMed] [Google Scholar]
- 13.Paula B, Ford DAD. Disparities in obesity prevalence due to variation in the retail food environment: three testable hypotheses. Nutrition Reviews. 2008;66(4):216–228. doi: 10.1111/j.1753-4887.2008.00026.x. [DOI] [PubMed] [Google Scholar]
- 14.Richard R, Rosenkranz DAD. Model of the home food environment pertaining to childhood obesity. Nutrition Reviews. 2008;66(3):123–140. doi: 10.1111/j.1753-4887.2008.00017.x. [DOI] [PubMed] [Google Scholar]
- 15.W.Maziak KDWMBS. Childhood obesity: are we missing the big picture? Obesity Reviews. 2008;9(1):35–42. doi: 10.1111/j.1467-789X.2007.00376.x. [DOI] [PubMed] [Google Scholar]
- 16.Papas MA, Alberg AJ, Ewing R, Helzlsouer KJ, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev. 2007;29(1):129–143. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- 17.Golley RK, Magarey AM, Baur LA, Steinbeck KS, Daniels LA. Twelve-month effectiveness of a parent-led, family-focused weight-management program for prepubertal children: A randomized, controlled trial. Pediatrics. 2007;119(3):517–525. doi: 10.1542/peds.2006-1746. [DOI] [PubMed] [Google Scholar]
- 18.Golan M, Kaufman V, Shahar DR. Childhood obesity treatment: targeting parents exclusively v. parents and children. British Journal of Nutrition. 2006;95(05):1008–1015. doi: 10.1079/bjn20061757. [DOI] [PubMed] [Google Scholar]
- 19.Robertson W, Friede T, Blissett J, Rudolf MC, Wallis M, Stewart-Brown S. Pilot of "Families for Health": Community-based family intervention for obesity. Arch Dis Child. 2008;93(11):921–926. doi: 10.1136/adc.2008.139162. [DOI] [PubMed] [Google Scholar]
- 20.Haire-Joshu D, Brownson RC, Nanney MS, et al. Improving dietary behavior in African Americans: the Parents As Teachers High 5, Low-Fat Program. Preventive Medicine. 2003;36(6):684–691. doi: 10.1016/s0091-7435(03)00053-7. [DOI] [PubMed] [Google Scholar]
- 21.Epstein LH, Gordy CC, Raynor HA, Beddome M, Kilanowski CK, Paluch R. Increasing fruit and vegetable intake and decreasing fat and sugar intake in families at risk for childhood obesity. Obes Res. 2001 Mar;9(3):171–178. doi: 10.1038/oby.2001.18. [DOI] [PubMed] [Google Scholar]
- 22.Harvey-Berino J, Rourke J. Obesity Prevention in Preschool Native-American Children: A Pilot Study Using Home Visiting. Obesity. 2003;11(5):606–611. doi: 10.1038/oby.2003.87. [DOI] [PubMed] [Google Scholar]
- 23.Fitzgibbon ML, Stolley MR, Schiffer L, Van Horn L, KauferChristoffel K, Dyer A. Hip-Hop to Health Jr. for Latino Preschool Children[ast] Obesity. 2006;14(9):1616–1625. doi: 10.1038/oby.2006.186. [DOI] [PubMed] [Google Scholar]
- 24.Davis SM, Clay T, Smyth M, et al. Pathways curriculum and family interventions to promote healthful eating and physical activity in American Indian schoolchildren. Prev Med. 2003;37(6):S24–S34. doi: 10.1016/j.ypmed.2003.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodearmel SJ, Wyatt HR, Stroebele N, Smith SM, Ogden LG, Hill JO. Small changes in dietary sugar and physical activity as an approach to preventing excessive weight gain: The America on the Move family study. Pediatrics. 2007;120(4):e869–e879. doi: 10.1542/peds.2006-2927. [DOI] [PubMed] [Google Scholar]
- 26.Eng E, Parker E, Harlan C. Lay health advisor intervention strategies: a continuum from natural helping to paraprofessional helping. Health Educ Behav. 1997 Aug;24(4):413–417. doi: 10.1177/109019819702400402. [DOI] [PubMed] [Google Scholar]
- 27.Eng E, Parker E. Natural Helper Models to Enhance a Community's Health and Competence. In: DiClemente RJ, Crosby RA, Kegler MC, editors. Emerging Theories in Health Promotion Practice and Research: Strategies for Improving Public Health. Jossey-Bass: 2002. pp. 126–156. [Google Scholar]
- 28.Eng E, Young R. Lay health advisors as community change agents. Family &Community Health. 1992;15:24–40. [Google Scholar]
- 29.Service C, Salber E. Community health education: the lay health advisor approach. Durham, NC: Duke University Health Care System; 1979. [Google Scholar]
- 30.Kahssay H, ME T, PA B. Community Health Workers: The Way Forward. Geneva, Switzerland: WHO; 1998
- 31.Rhodes SD, Foley KL, Zometa CS, Bloom FR. Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. Am J Prev Med. 2007 Nov;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 32.Hanson J. Parental self-efficacy and asthma self-management skills. Journal of the Society of Pediatric Nurses. 1998;3(4):146–154. doi: 10.1111/j.1744-6155.1998.tb00222.x. [DOI] [PubMed] [Google Scholar]
- 33.Elder JP, Ayala GX, Parra-Medina D, Talavera GA. Health promotion in the Latino community: Communication issues and approaches. Annual Review of Public Health. :30. doi: 10.1146/annurev.publhealth.031308.100300. in press. [DOI] [PubMed] [Google Scholar]
- 34.Duerksen SC, Campbell N, Arredondo EM, Ayala GX, Baquero B, Elder JP. In: Aventuras para niños: Obesity prevention in the homes, schools, and neighborhoods of Mexican American children. Brettschneider W, Rue R, editors. Lang: 2007. [Google Scholar]
- 35.U.S. Census Bureau. American FactFinder fact sheet. [Retrieved August 28, 2008];San Diego County, CA: 2000 from factfinder.census.gov/servlet/
- 36.Elder JP, Ayala GX, Campbell NR, et al. Long-term effects of a communication intervention for Spanish-dominant Latinas. Am J Prev Med. 2006 Aug;31(2):159–166. doi: 10.1016/j.amepre.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 37.Elder JP, Ayala GX, Campbell NR, et al. Interpersonal and print nutrition communication for a Spanish-dominant Latino population: Secretos de la Buena Vida. Health Psychol. 2005 Jan;24(1):49–57. doi: 10.1037/0278-6133.24.1.49. [DOI] [PubMed] [Google Scholar]
- 38.Elder JP, Campbell NR, Candelaria JI, et al. Project Salsa: development and institutionalization of a nutritional health promotion project in a Latino community. Am J Health Promot. 1998 Jul–Aug;12(6):391–401. doi: 10.4278/0890-1171-12.6.391. [DOI] [PubMed] [Google Scholar]
- 39.Baranowski T, Perry CL, Parcel GS. How individuals, environments and health behavior interact: Social Cognitive Theory. In: Glanz K, editor. Health Behavior and Health Education. 3rd ed ed. San Francisco, CA: Jossey–Bass; 2002. [Google Scholar]
- 40.Miller BD, Wood BL. Childhood asthma in interaction with family, school, and peer systems: A developmental model for primary care. J Asthma. 1991;28(6):405–414. doi: 10.3109/02770909109110622. [DOI] [PubMed] [Google Scholar]
- 41.Larios S, Ayala GX, Arredondo EM, Baquero B, Elder JP. Development and validation of a scale to measure Latino parenting strategies related to children's obesigenic behaviors: The Parenting strategies for Eating and Activity Scale (PEAS) Appetite. 2009;52(1):166–172. doi: 10.1016/j.appet.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ayala GX, Mueller K, Lopez-Madurga E, Campbell NR, Elder JP. Restaurant and food shopping selections among Latinas in Southern California. Journal of the American Dietetic Association. 2005;105:38–45. doi: 10.1016/j.jada.2004.10.023. [DOI] [PubMed] [Google Scholar]
- 43.Duffey KJ, Gordon-Larsen P, Jacobs DR, Jr, Williams OD, Popkin BM. Differential associations of fast food and restaurant food consumption with 3-y change in body mass index: the Coronary Artery Risk Development in Young Adults Study. Am J Clin Nutr. 2007;85(1):201–208. doi: 10.1093/ajcn/85.1.201. [DOI] [PubMed] [Google Scholar]
- 44.Elder JP, Ayala GX, Slymen DJ, Arredondo E, Campbell NR. Evaluating psychosocial and behavioral mechanisms of change in a tailored communication intervention. Health Education and Behavior. 2007 doi: 10.1177/1090198107308373. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 45.Lutfiyya MN, Garcia R, Dankwa CM, Young T, Lipsky MSJ. Overweight and obese prevalence rates in African American and Hispanic children: an analysis of data from the 2003–2004 National Survey of Children's Health. J Am Board Fam Med. 2008;21(3):191–199. doi: 10.3122/jabfm.2008.03.070207. [DOI] [PubMed] [Google Scholar]
- 46.Epstein LH, Paluch RA, Gordy CC, Dorn J. Decreasing Sedentary Behaviors in Treating Pediatric Obesity. Arch Pediatr Adolesc Med. 2000;154(3):220–226. doi: 10.1001/archpedi.154.3.220. [DOI] [PubMed] [Google Scholar]
- 47.Litrownik AJ, Elder JP, Campbell NR, et al. Evaluation of a tobacco and alcohol use prevention program for Hispanic migrant adolescents: promoting the protective factor of parent-child communication. Prev Med. 2000 Aug;31(2 Pt 1):124–133. doi: 10.1006/pmed.2000.0698. [DOI] [PubMed] [Google Scholar]
- 48.Velasquez J, Moreno C, Ayala GX, Sandoval S, Elder JP. Promotoras as behavior change agents: What role do they serve?; Paper presented at: American Public Health Association; Atlanta, GA. 2001. [Google Scholar]
- 49.Sabogal F, Marin O, Otero-Sabogal R, Marin B, Perez-Stable EJ. Hispanic Familsm and Acculturation: What Changes and What Doesn't? Hispanic Journal of Behavioral Sciences. 1987;9:397–412. [Google Scholar]
- 50.Patterson TL, Rupp JW, Sallis JF, Atkins CJ, Nader PR. Aggregation of dietary calories, fats, and sodium in Mexican-American and Anglo families. Am J Prev Med. 1988 Mar–Apr;4(2):75–82. [PubMed] [Google Scholar]
- 51.Sallis JF, Patterson TL, Buono MJ, Atkins CJ, Nader PR. Aggregation of physical activity habits in Mexican-American and Anglo families. J Behav Med. 1988 Feb;11(1):31–41. doi: 10.1007/BF00846167. [DOI] [PubMed] [Google Scholar]
- 52.Hernandez EA, Baquero B, Ayala GX. Emerging evidence of fathers in Latino homes. Paper presented at: Society for Behavioral Medicine; Washington, D.C. 2007. [Google Scholar]
- 53.Viswanathan M, Kraschnewski J, Nishikawa B, et al. Outcomes of Community Health Worker Interventions. Rockville, MD: Agency for Healthcare Research and Quality; 2009. [Google Scholar]