Abstract
We examined whether extending the administration time of letter fluency from one minute per letter trial (standard administration) to two minutes increased the sensitivity of this test to cognitive status in aging. Participants (mean age = 84.6) were assigned to cognitive impairment (n=20) and control (n=40) groups. Pearson correlations and scatter plot analyses showed that associations between the Dementia Rating Scale scores and letter fluency were higher and less variable when performance on the latter was extended to two minutes. ANOVA showed that the cognitive impairment group generated fewer words in the second minute of the letter fluency task compared to the control group. Finally, discriminant function analyses revealed that extending the letter fluency trials to two minutes increased discrimination between the control and cognitive impairment groups.
Keywords: letter fluency, aging, cognitive impairment
Verbal Fluency tasks require the production of words with specific restrictions in a specified amount of time (Lezak, Loring & Howieson, 2004). Two types of verbal fluency tasks have been described in neuropsychological literature, both of which rely on verbal memory (Moscovitch, 1994). Category fluency requires production of words from a particular category, such as fruits or animals. This test is believed to tap semantic abilities and to rely heavily on left temporal regions (Moscovitch, 1994; Pihlajamaki et al., 2000). Letter fluency requires generation of words cued with a specific letter and depends on phonemic abilities (Benton & Hamsher, 1976). It has been suggested that letter fluency relies more on left frontal regions (Audenaert et al., 2000; Phelps, Hyder, Blamire, & Shulman 1997) and is the more difficult of the two tasks for older adults (Lezak, 1995). Norms for letter and category fluency are based on one-minute trials per individual letter (Lezak, 1995; Spreen & Strauss, 1998).
Letter fluency is sensitive the cognitive decline observed in Alzheimer’s (Duff Canning, Leach, Stuss, & Black, 2004; Lafosse et al., 1997), vascular (Duff et al., 2004) and frontotemporal (Robertson et al., 2005; Vicioso, 2002) dementias. Decline in performance on letter fluency is a risk factor for rapid disease progression and reduced survival (Robertson et al., 2005; Schupf et al., 2005). Retrieval of words from long term memory, processing speed and the ability to withhold previously provided responses and maintain a set have been shown to affect performance on fluency tests (Salthouse, 2005). In addition, pairing verbal fluency tests with an interference task results in disproportionate decline in word production in cognitively impaired elders (Holtzer, Burright, & Donovick, 2004) and in individuals with traumatic brain injuries (McDowell, Whyte & D’Esposito, 1997) compared to normal controls, suggesting that limited attentional resources affect letter fluency performance. Reports that most words are generated early in the task in cognitively impaired adults (Fernaeus & Almkvist, 1998) also support the notion that limited resources affect letter fluency performance.
However, whether extending the standard administration time of letter fluency (60 sec) increases demands on cognitive resources and thereby improves the test’s sensitivity to cognitive status in aging has not been examined. It is noteworthy that designing alternative administration procedures and interpretations to improve diagnostic limitations of commonly used neuropsychological tests has been previously proposed (Chertkow, Bergman, Schipper, Gauthier, Bouchard, Fontaine, & Clarfield, 2001; Chertkow, 2000; Förstl, 2005; Kilada et al., 2005; Mungas, Reed, & Kramer, 2003; Rentz et al., 2004).
Herein we examined whether increasing demands on cognitive resources by extending the administration time of a single letter trial from one to two minutes was associated with improved sensitivity to cognitive status in aging. Accordingly, we hypothesized that extending the administration time of letter fluency would: a) have a differential effect on older adults with cognitive impairments compared to normal controls, with the latter group generating more words in the second minute; and b) improve discrimination between the two groups.
Method
Participants
Sixty older adults participated in the study (for details see Holtzer et al., 2004). Mean age for the entire sample was 84.6 (5.3) years, and mean education was 14.2 (2.5) years. Sample characteristics are summarized in Table 1. Individuals were recruited from residential facilities and from a small retirement community designated solely for the elderly. Exclusion criteria for this study were as follows: diagnosis of any form of dementia, history of or current diagnosis of psychosis, alcohol abuse, drug abuse, cerebrovascular events, Huntington disease, Parkinson disease, traumatic brain injury, lead or heavy metal poisoning, seizure disorder and meningitis. Brief screening measures of vision, audition and motor skills were used to determine the participants’ ability to take part in the study.
Table 1.
Sample characteristics, DRS and letter fluency performance
| Cognitively Impaired (N = 20) | Control (N = 40) | |||
|---|---|---|---|---|
| Mean | (SD) | Mean | (SD) | |
| Age (years) | 85.1 | (6.33) | 84.4 | (4.74) |
| Education (years)** | 12.7 | (2.15) | 14.9 | (2.20) |
| % Female | 65% | 62.5% | ||
| DRS: Total Score** | 118.3 | (3.92) | 134.4 | (6.10) |
| DRS: Attention | 35.4 | (1.43) | 35.9 | (1.07) |
| DRS: I/P** | 27.8 | (4.05) | 34.5 | (2.88) |
| DRS: Construction* | 5.2 | (1.01) | 5.7 | (0.79) |
| DRS: Conceptualization** | 31.5 | (3.12) | 36.2 | (2.42) |
| DRS: Memory** | 18.5 | (3.38) | 22.1 | (2.53) |
| Letter Fluency 1 minute* | 8.25 | (2.4) | 10.4 | (3.4) |
| Letter Fluency 2 minutes** | 10.60 | (3.4) | 15.9 | (5.9) |
p ≤ .05
p ≤ .01
DRS denotes Dementia Rating Scale. LF denotes letter fluency; LF 1 minute = total number of words generated in the first minute of administration; LF 2 minutes = total number of words generated in two minutes of administration; I/P denotes Initiation/Perseveration. Independent-samples t tests (df = 58) were used to examine group differences on all continuous measures. Chi-square analysis was used to examine group differences in gender distribution.
Materials & Procedure
The Dementia Rating Scale (DRS; Mattis, 1988) was administered to assess cognitive status. This instrument taps five general domains including: Attention, Initiation/Perseveration, Construction, Conceptualization, and Memory. The DRS is commonly used for clinical and research purposes in older adults. Normative data and information concerning the psychometric properties of the test have been described in detail (Lezak et al., 2004; Mattis, 1988; Spreen & Straus, 1998). For the purpose of this study, and consistent with published data, individuals were deemed cognitively impaired if they scored below a total DRS cut-off score of 123 (n=20). Those who scored above the cut-off served as normal controls (n=40).
The letter fluency test requires the individual to generate words cued with a specific letter within a constrained amount of time, without using proper nouns, repeating previously generated words, or using the same word with a different suffix (Benton & Hamsher, 1976). The letters B and F, which occur with matching frequencies (Lezak, 1995), were used in this study. Letter trials were randomly assigned so that one half of the participants in each group was cued with the letter B, while the other half with the letter F. Letter fluency trials were extended to two minutes with the total number of words generated recorded for each 60-second interval.
Statistical Analyses
Descriptive statistics: Demographic information, DRS total and scales scores and the total number of words generated in one and two minutes of the letter fluency task were tabulated per group. Associations between letter fluency performance in the one and two-minute conditions and the DRS total score were assessed via Pearson correlations and scatter plot analyses. Pearson correlations were also used to examine associations between the letter fluency measures and the DRS scale scores, age and education. ANOVA with group status as the two-level independent variable and the difference in the number of words generated in the one and two-minute letter fluency conditions as the dependent variable examined whether increasing the administration time differentially affected performance in the two groups. Two separate Discriminant Function Analyses (DFA; Durate Silva & Stam, 1996), using the number of words generated in the 1 and 2-minute conditions as predictors and group status as the independent measure, examined whether extending the administration time of the letter fluency test increased classification accuracy.
Results
Demographic information, DRS total and scale scores, and the total number of words generated in the one and two- minute letter fluency conditions were summarized in Table 1. The cognitive impairment group had a mean DRS total score of 118.3, indicating a relatively mild level of cognitive dysfunction. The mean DRS total score for the control group (134.4) was well above the recommended DRS cut score for dementia. As expected, significant group differences were noted on the DRS total and scale scores (excluding the attention scale) and on the letter fluency measures.
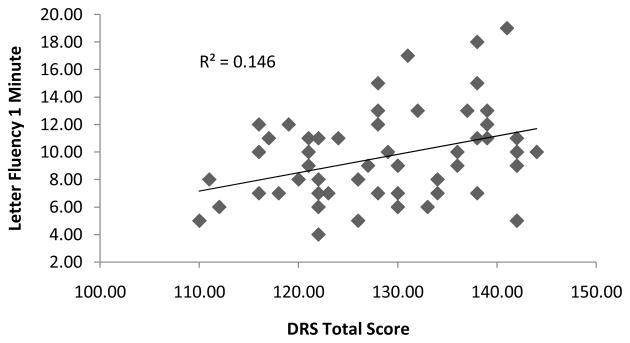
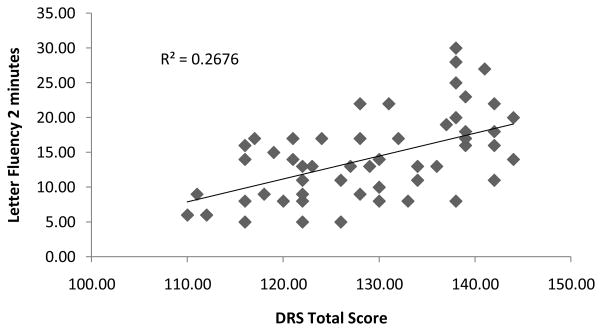
Associations between the letter fluency measures and cognitive function, as assessed by the DRS, were examined via Pearson correlations and scatter plot analyses.
Inspection of Table 2 and figures 1 and 2 suggests that the association between the DRS total score and letter fluency was higher and less variable when performance on the latter was extended to two minutes. Examining the correlations between letter fluency and the DRS scale scores revealed a similar trend in that the magnitude of the correlations appeared to be descriptively higher in the two-minute condition. The DRS conceptualization scale correlated only with the number of words generated in the two- minute interval and in the second minute alone. The DRS memory scale correlated only with the number of words generated during the second minute of the letter fluency test.
Table 2.
Correlations between letter fluency measures, DRS scores, age and education
| LF 1 minute | LF 2 minutes | LF difference | |
|---|---|---|---|
| r | r | r | |
| Age | .072 | .086 | .060 |
| Education | .355** | .389** | .340** |
| DRS Total | .382** | .517** | .539** |
| DRS Attention | .107 | .152 | .195 |
| DRS I/P | .479** | .575** | .533** |
| DRS Construction | .224 | .233 | .213 |
| DRS Conceptualization | .217 | .308* | .338** |
| DRS Memory | .046 | .197 | .292* |
p ≤ .05
p ≤.01
DRS denotes Dementia Rating Scale. LF denotes letter fluency; LF 1 minute = total number of words generated in the first minute of administration; LF 2 minutes = total number of words generated in two minutes of administration; LF difference = difference between number of words generated in 1 vs. 2 minutes of administration. I/P denotes Initiation/Perseveration.
Figure 1.
The total number of words generated in one minute in the Letter Fluency test plotted against the Dementia Rating Scale (DRS) total score.
Figure 2.
The total number of words generated in two minutes in the Letter Fluency test plotted against the Dementia Rating Scale (DRS) total score.
As hypothesized, the ANOVA adjusting for the level of education showed that the control group generated significantly more words in the second minute [(M = 5.47(3.3)] compared to the cognitive impairment group [(M = 2.5(1.8)], 1F(4,55) = 4.958, p = 0.002.
The first discriminant function, which used words generated only within the first minute of administration as a predictor of group membership, was statistically significant [Λ (1) = 0.895, p = 0.011]. Overall, classification accuracy was 68.3%. Only 5 of the 20 (25%) cognitively impaired participants and 36 of the 40 (90%) control participants were correctly classified.
The second discriminant function used the total number of words generated in the two-minute letter fluency task as a predictor of group membership. This discriminant function was also statistically significant [Λ (1) = 0.826, p = 0.001]. The overall classification accuracy increased to 77%, with 11 of the 20 (55%) cognitively impaired participants and 35 of the 40 (87.5%) normal controls classified into their respective groups.
Discussion
Extending the administration time of letter fluency from one to two minutes increased the sensitivity of this test to cognitive status in aging. Individuals with cognitive impairments generated significantly less words during the second minute of the task compared to controls, even when taking into account performance differences between the two groups in the first 60 seconds of each letter trial. Furthermore, increasing the administration time of single letter fluency trials to two minutes improved sensitivity with only a minimal cost to specificity. Typically, effort is made to shorten assessment procedures to reduce subject burden and improve efficiency. However, extending the administration time of letter fluency by one minute maybe a cost effective trade off.
The associations between the DRS total and scale scores and letter fluency were higher and less variable when performance on the latter was extended to two minutes. The DRS conceptualization scale correlated only with the number of words generated in the two- minute interval and in the second minute alone. Moreover, the DRS memory scale correlated only with the number of words generated in the second minute. This last finding might suggest that demands on word retrieval were increased during the second minute of the letter fluency task. Therefore, we suggest that extending the administration time of letter fluency increased demands on cognitive resources and on word retrieval and consequently improved the discrimination between individuals with cognitive impairments and controls.
A few studies suggested that the majority of words in letter fluency tasks are generated within the initial few seconds of administration (Crowe, 1998; Fernaeus & Almkvist, 1998). In contrast, we found that extending the administration time to two minutes yielded incremental information. However, we have not examined whether word generation performance varied within each minute. These seemingly contradictory findings may in fact be reconciled if shown that most words are generated early within the first and second minutes of the task. Future studies should examine this possibility as it might suggest that given sufficient time cognitive resources may be replenished and redirected toward task completion, at least in cognitively normal older adults.
The limitations of this study should be considered. The level of education was higher in the control group. While demographic variables including education have been associated with letter fluency performance (Kempler, Teng, & Dick, 1998; Lezak et al., 2004; Spreen & Strauss, 1998) the group differences reported in this study adjusted for the possible effect of such confounders. In addition, ethnicity may influence letter fluency performance (Acevedo, Loewenstein, & Barker, 2000; Kempler et al., 1998). Since the participants in this study were Caucasians future research should examine the generalizability of these findings to other ethnic groups as well. Finally, group status was determined using the DRS, which is a screening measure for cognitive function and dementia in the elderly. Thus it is possible that some subjects may have been misclassified. Nonetheless, as previously discussed, extending the administration time of letter fluency provided incremental information when cognitive function was examined as a continuous variable across the entire sample as well.
Implications
The findings suggest that extending the administration time of letter fluency increases the sensitivity of this test to cognitive function in aging. These results should be replicated in longitudinal studies and extended to mild cognitive impairments, dementia and other diseases known to affect verbal fluency performance.
Acknowledgments
Roee Holtzer is supported by a Paul B. Beeson Award (NIA-K23 AG030857).
Footnotes
Analyses that also adjusted for age and gender were not materially different
References
- Acevedo A, Loewenstein DA, Barker WW. Category fluency test: Normative data for English- and Spanish-speaking elderly. Journal of International Neuropsychological Society. 2000;6:760–769. doi: 10.1017/s1355617700677032. [DOI] [PubMed] [Google Scholar]
- Audenaert K, Brans B, Van Laere K, Lahorte P, Versijpt J, Van Heeringen K, et al. Verbal fluency as a prefrontal activation probe: A validation study using 99mTc-ECD Brain SPET. European Journal of Nuclear Medicine and Molecular Imaging. 2000;27:1800–1808. doi: 10.1007/s002590000351. [DOI] [PubMed] [Google Scholar]
- Benton A, Hamsher K. Multingual aphasia examination. Iowa City: University of Iowa; 1976. [Google Scholar]
- Chertkow H, Bergman H, Schipper HM, Gauthier S, Bouchard R, Fontaine S, Clarfield AM. Assessment of suspected dementia. Canadian Journal of Neurological Sciences. 2001;28(S1):S28–41. doi: 10.1017/s0317167100001189. [DOI] [PubMed] [Google Scholar]
- Chertkow HM. Mild cognitive impairment. Current Opinion in Neurology. 2000;15:401–407. doi: 10.1097/00019052-200208000-00001. [DOI] [PubMed] [Google Scholar]
- Craik FIM, Byrd M. Aging and cognitive deficits: The role of attentional resources. In: Craik FIM, Trehub S, editors. Aging and Cognitive Processes. New York: Plenum Press; 1982. pp. 191–211. [Google Scholar]
- Duff Canning SJ, Leach L, Stuss D, Ngo L, Black SE. Diagnostic utility of abbreviated fluency measures in Alzheimer disease and vascular dementia. Neurology. 2004;62:556–562. doi: 10.1212/wnl.62.4.556. [DOI] [PubMed] [Google Scholar]
- Durate Silva P, Stam A. Discriminant analysis. In: Grimm LG, Yarold PR, editors. Reading and understanding multivariate statistics. Washington D.C: American Psychological Association; 1996. pp. 277–318. [Google Scholar]
- Fernaeus S, Almkvist O. Word production: dissociation of two retrieval modes of semantic memory across time. Journal of Clinical and Experimental Neuropsychology. 1998;20:137–143. doi: 10.1076/jcen.20.2.137.1170. [DOI] [PubMed] [Google Scholar]
- Förstl H. Alzheimer’s disease: More data, but are we any more informed? Current Opinion in Psychiatry. 2005;18:615–620. doi: 10.1097/01.yco.0000185717.57117.08. [DOI] [PubMed] [Google Scholar]
- Holtzer R, Burright RG, Donovick PJ. The sensitivity of dual-task performance to cognitive status in aging. Journal of International Neuropsychological Society. 2004;10:230–238. doi: 10.1017/S1355617704102099. [DOI] [PubMed] [Google Scholar]
- Kempler D, Teng EL, Dick M. The effects of age, education, and ethnicity on verbal fluency. Journal of International Neuropsychological Society. 1998;4:531–538. doi: 10.1017/s1355617798466013. [DOI] [PubMed] [Google Scholar]
- Kilada S, Gamaldo A, Grant EA, Moghekar A, Morris JC, O’Brien RJ. Brief screening tests for the diagnosis of dementia: Comparison with the mini-mental state exam. Alzheimer Disease and Associated Disorders. 2005;19:8–16. doi: 10.1097/01.wad.0000155381.01350.bf. [DOI] [PubMed] [Google Scholar]
- Lafosse JM, Reed BR, Mungas D, Sterling SB, Wahbeh H, Jagust WJ. fluency and memory differences between ischemic vascular dementia and Alzheimer’s disease. Neuropsychology. 1997;11:514–522. doi: 10.1037//0894-4105.11.4.514. [DOI] [PubMed] [Google Scholar]
- Lezak MD. Neuropsychological assessment. 3. New York: Oxford University Press; 1995. [Google Scholar]
- Lezak MD, Loring DW, Howieson DB. Neuropsychological Assessment. 4. New York: Oxford University Press; 2004. [Google Scholar]
- Mattis S. Dementia rating scale. Odessa, FL: Psychological Assessment Resources; 1988. [Google Scholar]
- McDowell S, Whyte J, D’Esposito M. Working memory impairments in traumatic brain injury: Evidence from a dual-task paradigm. Neuropsychologia. 1997;35:1341–1353. doi: 10.1016/s0028-3932(97)00082-1. [DOI] [PubMed] [Google Scholar]
- Moscovitch M. Cognitive resources and dual-task interference effects at retrieval in normal people: The role of the frontal lobes and medial temporal cortex. Neuropsychology. 1994;8:524–534. [Google Scholar]
- Mungas D, Reed BR, Kramer JH. Psychometrically matched measures of global cognition, memory, and executive function for assessment of cognitive decline in older persons. Neuropsychology. 2003;17:380–392. doi: 10.1037/0894-4105.17.3.380. [DOI] [PubMed] [Google Scholar]
- Phelps EA, Hyder F, Blamire AM, Shulman RG. FMRI of the prefrontal cortex during overt verbal fluency. Neuroreport. 1997;8:561–565. doi: 10.1097/00001756-199701200-00036. [DOI] [PubMed] [Google Scholar]
- Pihlajamaki M, Tanila H, Hanninen T, Kononen M, Laakso M, Partanen K, et al. Verbal fluency activates the left medial temporal lobe: A functional magnetic resonance imaging study. Annals of Neurology. 2000;47(4):470–476. [PubMed] [Google Scholar]
- Rentz DM, Huh TJ, Faust RR, Budson AE, Scinto LFM, Sperling RA, et al. Use of IQ-adjusted norms to predict progressive cognitive decline in highly intelligent older individuals. Neuropsychology. 2004;18(1):38–49. doi: 10.1037/0894-4105.18.1.38. [DOI] [PubMed] [Google Scholar]
- Robertson ED, Hesse JH, Rose KD, Slama H, Johnson JK, Yaffe K, et al. Frontotemporal dementia progresses to death faster than Alzheimer’s disease. Neurology. 2005;65(1):719–725. doi: 10.1212/01.wnl.0000173837.82820.9f. [DOI] [PubMed] [Google Scholar]
- Salthouse TA. Relations between cognitive abilities and measures of executive functioning. Neuropsychology. 2005;19(4):532–545. doi: 10.1037/0894-4105.19.4.532. [DOI] [PubMed] [Google Scholar]
- Schupf N, Tang MX, Albert SM, Costa R, Andrews H, Lee JH, et al. Decline in cognitive and functional skills increases mortality risk in nondemented elderly. Neurology. 2005;65(2):1218–1226. doi: 10.1212/01.wnl.0000180970.07386.cb. [DOI] [PubMed] [Google Scholar]
- Spreen O, Strauss E. A compendium of neuropsychological tests. New York: Oxford University Press; 1998. [Google Scholar]
- Vicioso BA. Dementia: When is it not Alzheimer’s disease? The American Journal of the Medical Sciences. 2002;324(2):84–95. doi: 10.1097/00000441-200208000-00007. [DOI] [PubMed] [Google Scholar]