Abstract
The slow diffusion of empirically supported treatments and the rapid diffusion of treatments lacking empirical support play a significant role in the quality gap in the care of people with severe mental illnesses. Further, the rapid diffusion of treatments of low cost-effectiveness limits the system's ability to provide the full gamut of high-value treatments available to treat this vulnerable population. Using the case of schizophrenia as an illustrative case study, we review the context in which these paradoxical patterns of diffusion have occurred and propose policy solutions.
INTRODUCTION
Understanding and correcting anomalous patterns of diffusion of health care innovations is key to improving the performance of the US health care system.1,2 Low rates of adoption of empirically supported treatments –henceforth referred to as evidence-based practices, and high rates of adoption of non evidence-based practices plague the care of people with mental illnesses.3 We focus on people with severe and persistent mental illnesses (those with schizophrenia, bipolar disorder, and severe forms of major depression and anxiety disorders) because of their distinct needs and treatment circumstances in the US. Most people with severe mental illnesses are cared for in the specialty mental health sector, and their mental health and general health care is largely financed by public funds.4 In addition, evidence-based psychosocial practices aimed at facilitating community integration and rehabilitation are uniquely critical in the treatment of this population because of the significant functional impairment associated with these illnesses.5
Using the case of schizophrenia as an illustrative case study, we describe paradoxical patterns of diffusion and review factors likely to be associated with these patterns. Because current use offers a window into past patterns of diffusion, we assume that diffusion and use patterns are manifestations of the same underlying phenomenon.6 We conclude with a discussion of policy strategies aimed at correcting the diffusion paradox and improving care of this vulnerable population. Our discussion of factors associated with diffusion of treatments and of policy solutions applies to all people with severe mental illnesses (SMIs).
SIGNIFICANCE AND PATTERNS OF CARE OF SCHIZOPHRENIA
Although schizophrenia affects only 0.7% of the US population (2 million adults), it accounts for 5% of all burden of disease in the US and other developed countries as a result of its early age of onset (third decade or younger), chronic course, significant disability, and premature mortality.7
The economic burden of schizophrenia is also significant. By 2002, the overall US cost of the illness was estimated to be $63 billion: $23 for direct health care and $8 billion for non-health care costs, and $32 billion in indirect costs associated with lost productivity, premature mortality, and negative effects on family members.8 This represents nearly half the US cost of diabetes in 2002 in spite of the fact that diabetes is at least six times more prevalent than schizophrenia.9
THE DIFFUSION PARADOX IN THE CARE OF SCHIZOPHRENIA
Slow Diffusion of Evidence-based Practices
In the last two decades, basic and clinical research programs in schizophrenia have significantly expanded the therapeutic arsenal and improved patients’ odds of leading fuller lives.10 However, as in other areas of health care, some innovations have diffused very slowly from experimental to routine care settings.11 The resulting underuse of evidence-based practices (EBPs) has deprived scores of patients from potentially beneficial interventions.12 The schizophrenia Patient Outcomes Research Team (PORT) study found that in the late 1990s, adherence with recommended outpatient practices ranged between 10% and 46% for ten of eleven practices studied.13 Later studies have confirmed these results.14
Supported employment, family psychoeducation, and other evidence-based psychosocial practices used to treat schizophrenia are more likely to diffuse slowly and to be used less frequently than pharmacological EBPs.15 Moreover, limited evidence suggests that use of psychosocial EBPs is diminishing.16 A detailed discussion of underused EBPs is beyond this paper's scope. However, two EBPs are noteworthy: clozapine because of its unique role in the treatment of schizophrenia,17 and Supported Employment because of the importance of employment facilitating the community integration of these individuals.18
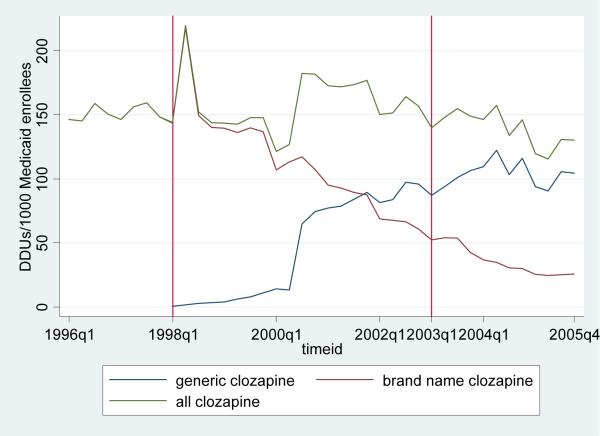
Although clozapine is the only drug approved by the Food and Drug Administration (FDA) for the management of treatment-resistant symptoms and recurrent suicidal behavior,19 its use rates are far lower than the estimated need.20 Strikingly, its diffusion and use were not boosted by the FDA approval in December 2002 of a second indication (see Exhibit 1). Underuse of clozapine is likely to be related to its potential for serious hematological adverse effects and mandatory blood tests instituted to monitor hematological indices.21 However, the substantial reduction of the drug's hematological risk as a result of the monitoring program and higher clozapine use rates observed in countries with similar blood test requirements as the US suggest that factors unrelated to the drug also contribute to underuse.22
Exhibit 1.
Daily dose units (DDUs) of clozapine per thousands of Medicaid enrollees, by clozapine form, over time (1996 − 2005, selected quarters shown)
Source: Authors’ calculations from 1996−2005, fee-for-service Medicaid claims data.
Supported Employment is an evidence-based approach to securing and maintaining competitive employment for people with schizophrenia and other SMIs.23 Most vocational services offered in routine care are not empirically supported. It is then troubling that rates of use of any vocational service in this population range between 0−23%, and only 5% of people were found to receive Supported Employment in one study.24 As with clozapine, its underuse is likely to be multi-factorial. Marshall and colleagues found that successful implementation of Supported Employment was associated with leadership, and the workforce's experience, training, and attitudes regarding the employability of people with SMIs.25
Rapid Diffusion of Non Evidence-based Practices
The rapid diffusion of practices lacking empirical support is a matter of great public health and policy concern because at worst their potential for harm exceeds their likely benefit and at best their use represents an inefficient use of resources; as such, their use constitutes overuse.26 An example of overuse in the care of people with schizophrenia is antipsychotic polypharmacy, the practice of using two or more antipsychotics simultaneously. Although this practice lacks empirical support, methodologically diverse US studies have found rates as high as 50% and its use appears to be on the rise.27 Although its contributing factors are not well understood, evidence suggests that physicians use antipsychotic polypharmacy in lieu of clozapine for patients with treatment-resistant symptoms.28
Rapid Diffusion of Treatment Practices of Lower Value
To address rising health care costs, policymakers have focused their attention not only on diffusion and use of treatments of proven effectiveness but cost-effectiveness as well.29 Peter Orzag, former director of the Congressional Budget Office, endorsed an expanded definition of overuse which includes situations in “which the added costs of a more expensive service did not exceed the added benefits it was expected to provide.”30 The rapid diffusion of atypical antipsychotic drugs and rise to standard of care status is an example of overuse defined in this manner (see Exhibit 2).31 With the exception of clozapine, initial claims of superior efficacy relative to conventional antipsychotic drugs have not been borne out.32 Further, branded atypical antipsychotics are far more costly, and based on recent research, less cost-effective than conventional antipsychotics.33 Although valid concerns about the methodological quality of the cost-effectiveness data have been raised by Richard Frank and others, available evidence suggests that the market dominance of non-clozapine atypical agents fits the expanded definition of overuse given above.34
Exhibit 2.
Percent* of persons with self-reported schizophrenia using each drug during the study year (n=237)
| Atypical Antipsychotic Drug | Percent with use in 1996/1997 | Percent with use in 2004/2005 | Growth in use (2004/2005 / 1996/1997) |
|---|---|---|---|
| Clozapine | 3.9% (2.4) | 4.8% (2.9) | 21.7% |
| Olanzapine | 12.1% (3.6) | 35.0% (6.2) | 189.9% |
| Quetiapine | -- | 14.4% (4.6) | -- |
| Risperidone | 12.9% (4.9) | 19.4% (4.6) | 51.2% |
| Ziprasidone | -- | 10.1% (3.7) | -- |
| Aripiprazole |
--
|
15.6% (4.4)
|
-- |
| Any | 26.7% (6.6) | 75.2% (5.0) | 181.9% |
Percents reflect percentage of people reporting one or more filled prescriptions during the year (quetiapine, ziprasidone, and aripiprazole were not available in 1996/1997). Persons may report use of more than one medication, so sum of percents is over 100%. Figures in parentheses are linearized standard errors.
Source: Authors’ calculations from 1996−2005 Medical Expenditure Panel Survey (pooled weights).
The National Implementing Evidence-based Practices for Severe Mental Illness Project, an Initiative to Increase EBP Adoption
The National Implementing Evidence-Based Practices for Severe Mental Illness Project (or Implementing EBPs Project for short) has sought to promote the implementation of underused EBPs for schizophrenia and other SMIs.35 Investigators developed implementation toolkits and piloted the implementation of five psychosocial EBPs in eight states.36 An indirect measure of the success of the Implementing EBPs Project is evidence that states have steadily expanded their offering of the psychosocial practices promoted by this initiative.37
FACTORS ASSOCIATED WITH THE DIFFUSION OF TREATMENTS
The rate at which treatment innovations spread through the health care system results from the interplay of several factors. The diffusion literature distinguishes factors related to the innovation (e.g., effectiveness, safety); patients (e.g., treatment preferences); clinicians (attitudes and knowledge/competencies); and the system of care.38 System-level factors include all aspects of the environment where care occurs (e.g., financial policies, regulations, structural and cultural characteristics of adopting organizations). In the US, the system of care for people with schizophrenia and other SMIs is the publicly funded specialty mental health sector. Public health programs play a crucial role in the financing, and to a lesser extent, the delivery of health care. Additional public sector dollars fund key social services for this population. These public programs operate in an environment characterized by short term constraints and chronic resource limitations, and the delivery system is a poorly coordinated web of public and private providers with few incentives to plan for the long term.
In what follows we discuss factors amenable to public policies that are likely to have an important role in the diffusion paradox in the care of people with schizophrenia.39
Financing of Care
We focus on Medicaid and Medicare although note that the Veterans Health Administration and state and local governments also play a role financing the care of this population, particularly veterans and uninsured people.40
Medicaid
Medicaid is the single largest payer for people with SMIs including those with schizophrenia. An important trend in Medicaid has been the expansion of managed care programs. For a large proportion of people with SMIs enrolled in these programs, non-pharmacy benefits for mental health and substance abuse care (together known as behavioral health care) are managed by Managed Behavioral Health Care Organizations in carve-out arrangements.41
The net effects of managed care on the diffusion process are poorly understood. Managed care is associated with greater use of ambulatory services, which in turn is associated with greater use of medications to treat mental illnesses (henceforth referred to as psychotropic drugs).42 However, managed care is also associated with greater use of management tools aimed at curbing the use of expensive drugs.43 Further, the separation of behavioral health and general health/pharmacy benefits that characterizes carve-out arrangements creates incentives for a psychotropic drug-based approach to treatment and a reduction in the use of psychosocial interventions.44 Overall, the evidence is mixed on the effects of Medicaid managed care on quality of care for people with schizophrenia.45 The only published study that has investigated the diffusion effects of carve-out arrangements found that they are associated with an increase in the use of newer antidepressants but not of atypical antipsychotics.46
Medicare
Many Medicare-covered disabled individuals, including people with schizophrenia, are dually eligible for Medicaid coverage.47 With the implementation of the Medicare Modernization Act (MMA) in 2006, pharmacy benefits of dually covered individuals were transferred to Medicare, significantly expanding Medicare's role among people with schizophrenia and other SMIs. Although little is known about the effects of MMA on quality of care for this population, preliminary evidence suggests that access to psychotropic drugs may be problematic.48
Regulatory Framework
Federal and state administrative practices
These practices aim to ensure the quality of providers –through their accreditation, and of clinicians –through their licensing and credentialing. Because accreditation allows payers to penalize providers that fail to meet contractual performance standards, it could play a role in correcting the diffusion paradox in the care of people with schizophrenia. Although performance measures of relevance to this population are available, the most widely used quality-monitoring tool (the Healthcare Effectiveness Data and Information Set, HEDIS) does not contain any schizophrenia measures.49 Similarly, oversight of quality of the mental health workforce by federal and state agencies remains an underused regulatory tool.
Payer and health plan utilization management strategies
Although physician profiling and other utilization management strategies could be used to promote high-quality care, they have been primarily used to contain costs.50 Further, these strategies have been exclusively used to modify psychotropic drug prescribing practices.51
Private Sector Initiatives
Private sector initiatives can influence the diffusion process. For example, advocacy by patients and families accelerated the adoption of Assertive Community Treatment, and advocates’ positive reviews of atypical antipsychotics may have contributed to the early surge in their use.52 Sponsorship of academic activities and other pharmaceutical marketing strategies increases demand for antidepressant and other prescription drugs.53 We are not aware of similar empirical research for antipsychotic agents, but it is likely that aggressive marketing of drugs still enjoying patent protection played a major role in the rapid diffusion of non-clozapine atypical agents.54
Other Factors
The heterogeneous workforce involved in the care of people with schizophrenia is generally lacking in the skills and competencies required to adopt EBPs and deliver high-quality care to this population.55 Further, the challenging implementation and uncertain sustainability of EBPs of higher complexity contribute to their underuse, and despite the valuable implementation tools and evidence generated by the Implementing EBPs Project, more research on the transport of EBPs to the real world is needed.56 In addition, the variable quality and conflicting nature of available evidence on the effectiveness and cost-effectiveness of treatments complicate decisions on which treatments to fund and implement.57 Lastly, the insufficient computerization of the specialty mental health sector may also contribute to the diffusion paradox because health information technology can be used to monitor processes of care and promote evidence-based and high-value care.58
POLICY STRATEGIES
Although the overriding objective of the strategies suggested below is to increase the use of EBPs in the care of people with schizophrenia and other SMIs, some of them aim to decrease the use of non evidence-based practices or increase the value (cost-effectiveness) of care for this population.
Federal, state, and local governments are uniquely positioned to shape the financing and organization as well as the content and quality of health and social services available to people with schizophrenia. Exercising their leadership, these public entities could implement a quality improvement agenda that among other things includes policies to influence diffusion of treatments. High-level leadership will be crucial to advancing this agenda because powerful institutions need to be mobilized, resources need to be reallocated, and public-private partnerships need to be forged.59 Main targets for this high-level effort include financial incentives, regulatory tools, quality of the workforce, and quality of the evidence.
Financial Incentives
Given Medicaid's central role in the financing of care for this population, the agency should play a more active role in guiding treatment diffusion. In 2006 more than half of all state Medicaid programs had adopted pay for performance approaches to promote high-value care, and more states are expected to move in that direction.60 However, their target populations and performance measures have largely excluded chronically ill adults and people with SMIs.61 Following Medicare's lead, the federal government could pilot and evaluate access, quality of care, and cost effects associated with the use of incentives to promote high-value care for people with schizophrenia and other SMIs.62 Although tying financial incentives to the preferred use of cost-effective treatments may encounter resistance, there is growing support for initiatives that aim to maximize value in publicly funded health care.63
State and regional Medicaid programs have two main policy levers to guide diffusion in their fee-for-service programs. First, by modifying the pool of reimbursable services they can promote the adoption of underused EBPs and discourage the use of non evidence-based or lower-value treatment practices. Second, Medicaid programs can increase reimbursement rates for EBPs and clarify existing coverage opportunities. Medicaid programs can also guide diffusion in their managed care programs. First, they can increase capitation rates to adequately reimburse high-value EBPs with high start-up or operating costs. Second, they can incorporate expectations for evidence-based care into their procurement and contracting processes, with performance provisions and other tools.
In addition, policymakers may consider making Managed Behavioral Health Care Organizations financially responsible for psychotropic drug utilization. In doing so, they would remove a financial incentive to delivering care that is largely based on psychotropic drugs and is lacking in psychosocial treatments. Regardless of the financing mechanism, contracts should promote long-term health planning and financial and administrative coordination between providers of health and social services.
With regard to Medicare, in addition to the policy strategies outlined above for Medicaid, it is critical to evaluate the quality of care effects of MMA for people with schizophrenia and other SMIs.
Regulatory Tools
Accreditation and Licensing/Credentialing
The accreditation process for providers serving people with schizophrenia and other SMIs needs to incorporate existing performance measures for these illnesses. Further, to address the educational and training deficits of the mental health workforce, policies should be enacted to standardize licensing and credentialing requirements of clinicians and to ensure their uniform application across disciplines, states, and health plans.
Utilization Management Strategies
Re-orienting the use of utilization management strategies toward the attainment of quality goals would provide payers and health plans with a powerful tool to correct the diffusion paradox in the care of people with schizophrenia. For example, physician profiling and step therapy -the requirement that patients fail lower-cost drugs before receiving coverage for higher-cost drugs, could be used to increase the adoption of EBPs and to curb the use of non evidence-based as well as lower-value practices.64
Quality of the Workforce
The inadequacies of the mental health workforce call for a policy response that goes beyond the changes in licensing and credentialing requirements mentioned above. A public-private partnership that includes educational institutions and their accreditors should be established with the goal of modernizing the curricula and training activities of mental health clinicians.65 In the short and medium-term, the federal government should take a more active role in training activities. For example, as recommended by Goldman and Azrin, the federal government could develop a national multidisciplinary training program charged with improving the quality of the workforce.66 Further, although several state mental health agencies are developing training programs as part of their EBP implementation activities, these state efforts should be expanded and sustained over time.67 Lastly, to address the growing influence of pharmaceutical marketing on provider decision-making, the federal government might consider public financing of academic detailing as well as mandating public disclosure of pharmaceutical industry payments to physicians.
Quality of the Evidence
Correcting the diffusion paradox will require greater governmental support for translational research aimed at bridging the science to services gap.68 For example, the Substance Abuse and Mental Health Services Administration could fund demonstrations focused on EBPs for schizophrenia to build upon and expand the knowledge base generated by the Implementing EBPs Project.69
Although more research is needed to achieve better outcomes for people with schizophrenia, it is equally important to better use existing knowledge. Similar to the National Institute for Health and Clinical Excellence (NICE) in the UK, the Agency for Healthcare Research and Quality (AHRQ) or a newly created entity could be charged with conducting appraisals of the comparative effectiveness and cost effectiveness of treatments for schizophrenia.70 In addition, AHRQ should sponsor research to develop and refine performance measures for schizophrenia and other SMIs.71 Appraisals of the evidence and improved performance measures would facilitate the implementation of payment methods aimed at improving quality and value of health care. To address concerns of bias in pharmaceutical industry-sponsored research, the source of the evidence used in the appraisals of the evidence should be transparent.
Other Policy Strategies
At a time when the federal government is about to launch an important initiative to promote the adoption of health information technology, greater use of its considerable financial and administrative leverage is needed to expedite the adoption process by providers serving people with SMIs.72 Strategies include building financial incentives into contracts or tying provider accreditation to a minimal level of computerization.
Lastly, engaging advocacy groups in initiatives aimed at correcting the diffusion paradox is critical to ensuring their success.73 An important component of this effort involves increasing advocates’ understanding of the variable quality of the empirical evidence and the need to include cost and value of treatments in resource allocation decisions for publicly funded health care.
Conclusions
Quality of care for people with schizophrenia and other SMIs is far from optimal in the US. This troubling reality is in large measure a consequence of the slow diffusion of EBPs and the rapid diffusion of non evidence-based or lower value practices. We have reviewed factors that are likely to contribute to the diffusion paradox and have proposed policy solutions with the potential to correct it.
Acknowledgements
Authors acknowledge grant support from the National Institute of Mental Health/National Institute of Health: KL2-RR024154-01 (JD); K01- MH065639 (MD); P50 MH073469 (MHL); R01-MH61434 (SLN). Authors are grateful to Howard Goldman MD PhD, Parmeeth “Par” Atwal JD MPH, deputy editor at Health Affairs, and three anonymous reviewers for helpful comments on an earlier draft of this manuscript.
Contributor Information
Marcela Horvitz-Lennon, University of Pittsburgh School of Medicine 201 North Craig St., office 250 Pittsburgh, PA 15213 Email: mvh3@pitt.edu Tel: (412) 383.5121 Fax: (412) 383.5121.
Julie M. Donohue, Department of Health Policy and Management University of Pittsburgh Graduate School of Public Health Crabtree Hall A613, 130 DeSoto St. Pittsburgh, PA 15261 Email: jdonohue@pitt.edu Tel: (412) 624.4562 Fax: (412) 624.3146.
Marisa E. Domino, Department of Health Policy and Administration University of North Carolina 1104G McGavran-Greenberg Hall, CB#7411 Chapel Hill, NC 27599 Email: domino@unc.edu Tel: (919) 966.3891 Fax: (919) 966.6961.
Sharon-Lise T. Normand, Department of Health Care Policy, Harvard Medical School Department of Biostatistics, Harvard School of Public Health 180 Longwood Ave. Boston, MA 02115 Email: sharon@hcp.med.harvard.edu Tel: (617) 432.3260 Fax: (617) 432.2563.
ENDNOTES
- 1.Although the diffusion literature tends to distinguish between active efforts to promote the adoption of innovations and their passive spread reserving the term diffusion to describe only the latter, our usage of the term diffusion encompasses both concepts.
- 2.Chassin M. Is Health Care Ready for Six Sigma Quality? The Milbank Quarterly. 1998;76(4):565–591. doi: 10.1111/1468-0009.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]; Congressional Budget Office (CBO) The Overuse, Underuse, and Misuse of Health Care. [22 October 2008];Statement of Peter Orzag before the US Senate. 2008 July 17; http://www.cbo.gov/ftpdocs/95xx/doc9567/07-17-HealthCare_Testimony.pdf.
- 3.Institute of Medicine . Improving the Quality of Health Care for Mental and Substance-Use Conditions. The National Academies Press; Washington: 2006. [PubMed] [Google Scholar]; U.S. Department of Health and Human Services . New Freedom Commission on Mental Health: Achieving The Promise: Transforming Mental Health Care in America. DHHS; Rockville, MD: 2003. Pub. no. SMA-03−3832. [Google Scholar]
- 4.Institute of Medicine Improving the Quality [Google Scholar]
- 5.Frank RG, Glied SA. Better but Not Well: Mental Health Policy in the U.S. since 1950. Johns Hopkins University Press; Baltimore: 2006. [Google Scholar]; Rutman ID. Psychosocial Rehabilitation Services: Important or Irrelevant? Psychosocial Rehabilitation Journal. 1997;21(1):1–2. [Google Scholar]
- 6.Drake R, Skinner J, Goldman HH. What Explains the Diffusion of Treatments for Mental Illness? American Journal of Psychiatry. 2008;165(11):1385–1392. doi: 10.1176/appi.ajp.2008.08030334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saha S, et al. A Systematic Review of the Prevalence of Schizophrenia. PLoS Medicine. 2005;2(5):413–433. doi: 10.1371/journal.pmed.0020141. [DOI] [PMC free article] [PubMed] [Google Scholar]; Murray CJ, Lopez AD, editors. The Global Burden of Disease. Harvard University Press; Cambridge, Massachusetts: 1996. [Google Scholar]
- 8.Wu EQ, et al. The Economic Burden of Schizophrenia in the United States in 2002. Journal of Clinical Psychiatry. 2006;66(9):1122–1129. doi: 10.4088/jcp.v66n0906. [DOI] [PubMed] [Google Scholar]
- 9.Anonymous, Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes. Diabetes Care. 2004;27(2):596–601. doi: 10.2337/diacare.27.2.596. [DOI] [PubMed] [Google Scholar]
- 10.US Department of Health and Human Services, Office of the Surgeon General . Mental Health: A Report of the Surgeon General. USDHHS, Public Health Service; Rockville, MD: 1999. [Google Scholar]
- 11.Berwick DM. Disseminating Innovations in Health Care. Journal of the American Medical Association. 2003;289(15):1969–1975. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- 12.Lehman AF. Quality of Care in Mental Health: The Case of Schizophrenia. Health Affairs. 1999;18(5):52–65. doi: 10.1377/hlthaff.18.5.52. [DOI] [PubMed] [Google Scholar]
- 13.Lehman AF, et al. Patterns of Usual Care for Schizophrenia: Initial Results from the Schizophrenia Patient Outcomes Research Team (PORT) Client Survey. Schizophrenia Bulletin. 1998;24(1):11–20. doi: 10.1093/oxfordjournals.schbul.a033303. [DOI] [PubMed] [Google Scholar]
- 14.Frank RG, et al. Quality-Constant Prices for the Ongoing Treatment of Schizophrenia: An Exploratory Study. The Quarterly Review of Economics and Finance. 2004;44(3):390–409. doi: 10.1016/j.qref.2004.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lehman, et al. Patterns of Usual Care [Google Scholar]; Drake, Skinner, Goldman What Explains the Diffusion [Google Scholar]
- 16.Frank RG, et al. Quality-Constant Prices for the Ongoing Treatment of Schizophrenia. doi: 10.1016/j.qref.2004.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lehman AF, et al. The Schizophrenia Patient Outcomes Research Team (PORT): Updated Treatment Recommendations. Schizophrenia Bulletin. 2003;30(2):193–217. doi: 10.1093/oxfordjournals.schbul.a007071. [DOI] [PubMed] [Google Scholar]
- 18.Bond GR. Supported Employment: Evidence for an Evidence-based Practice. Psychiatric Rehabilitation Journal. 2004;27(4):345–359. doi: 10.2975/27.2004.345.359. [DOI] [PubMed] [Google Scholar]
- 19.Physician's Desk Reference Inc. 62th Edition Medical Economics; Montvale, NJ: 2008. [Google Scholar]
- 20.Rothbard AB, Kuno E, Foley K. Trends in the Rate and Type of Antipsychotic Medications Prescribed to Persons with Schizophrenia. Schizophrenia Bulletin. 2003;29(3):531–540. doi: 10.1093/oxfordjournals.schbul.a007025. [DOI] [PubMed] [Google Scholar]
- 21.Stroup TS, McEvoy JP, Lieberman JA. Revised PORT Recommendations. Schizophrenia Bulletin. 2004;30(3):609–611. doi: 10.1093/oxfordjournals.schbul.a007106. [DOI] [PubMed] [Google Scholar]
- 22.Conley RR, et al. Comparison of Clozapine Use in Maryland and in Victoria, Australia. Psychiatric Services. 2005;56(3):320–323. doi: 10.1176/appi.ps.56.3.320. [DOI] [PubMed] [Google Scholar]
- 23.Lehman et al. The Schizophrenia Patient Outcomes [Google Scholar]
- 24.Dickey BD, et al. Guideline Recommendations for Treatment of Schizophrenia: The Impact of Managed Care. Archives of General Psychiatry. 2003;60(4):340–348. doi: 10.1001/archpsyc.60.4.340. [DOI] [PubMed] [Google Scholar]; West JC, et al. Patterns and Quality of Treatment for Patients with Schizophrenia in Routine Psychiatric Practice. Psychiatric Services. 2005;56(3):283–291. doi: 10.1176/appi.ps.56.3.283. [DOI] [PubMed] [Google Scholar]; Tashjian M, et al. Best Practice Study of Vocational Rehabilitation Services to Severely Mentally Ill Persons. Policy Study Associates; Washington DC: 1989. [Google Scholar]
- 25.Marshall T, et al. Key Factors for Implementing Supported Employment. Psychiatric Services. 2008;59(8):886–892. doi: 10.1176/ps.2008.59.8.886. [DOI] [PubMed] [Google Scholar]
- 26.Chassin Is Health Care Ready [Google Scholar]; CBO The Overuse [Google Scholar]
- 27.Correll CU, et al. Antipsychotic Combinations vs Monotherapy in Schizophrenia: A Meta-analysis of Randomized Controlled Trials. Schizophrenia Bulletin. 2008:1–15. doi: 10.1093/schbul/sbn018. (published online 21 April 2008; doi:10.1093/schbul/sbn018) [DOI] [PMC free article] [PubMed] [Google Scholar]; Gilmer TP, et al. Antipsychotic Polypharmacy Trends Among Medi-Cal Beneficiaries with Schizophrenia in San Diego County, 1999−2004. Psychiatric Services. 2007;58(7):1007–1010. doi: 10.1176/ps.2007.58.7.1007. [DOI] [PubMed] [Google Scholar]
- 28.Chong S-A, Remington GJ, Bezchlibnyk-Butler KZ. Effect of Clozapine on Polypharmacy. Psychiatric Services. 2000;51(2):250–252. doi: 10.1176/appi.ps.51.2.250. [DOI] [PubMed] [Google Scholar]
- 29.Rosenheck RA, Leslie DL, Doshi JA. Second-Generation Antipsychotics: Cost-Effectiveness, Policy Options, and Political Decision Making. Psychiatric Services. 2008;59(5):515–520. doi: 10.1176/ps.2008.59.5.515. [DOI] [PubMed] [Google Scholar]; Alliance for Health Reform [22 October 2008];Comparative Effectiveness: Better Value for the Money? 2008 August; http://www.allhealth.org/Publications/Quality_of_care/Comparative_Effectiveness_Better_Value_for_the_Money_84.pdf.
- 30.CBO The Overuse [Google Scholar]
- 31.Drake, Skinner, Goldman What Explains the Diffusion [Google Scholar]
- 32.Carpenter WT, Buchanan RW. Lessons to Take Home from CATIE. Psychiatric Services. 2008;59(5):523–525. doi: 10.1176/ps.2008.59.5.523. [DOI] [PubMed] [Google Scholar]
- 33.Lieberman JA, et al. Effectiveness of Antipsychotic Drugs in Patients with Chronic Schizophrenia. New England Journal of Medicine. 2005;353(12):1209–1223. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]; Duggan MG. Do New Prescription Drugs Pay for Themselves? The Case of Second-Generation Antipsychotics. Journal of Health Economics. 2005;24(1):1–31. doi: 10.1016/j.jhealeco.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 34.Frank RG. Policy Toward Second-Generation Antipsychotic Drugs: A Cautionary Note. Psychiatric Services. 2008;59(5):521–522. doi: 10.1176/ps.2008.59.5.521. [DOI] [PubMed] [Google Scholar]; Drake, Skinner, Goldman What Explains the Diffusion [Google Scholar]
- 35.Torrey WC, et al. Implementing Evidence-Based Practices for Persons with Severe Mental Illnesses. Psychiatric Services. 2001;52(1):45–50. doi: 10.1176/appi.ps.52.1.45. [DOI] [PubMed] [Google Scholar]
- 36.Isett KR, et al. The State Policy Context of Implementation Issues for Evidence-Based Practices in Mental Health. Psychiatric Services. 2007;58(7):914–921. doi: 10.1176/ps.2007.58.7.914. [DOI] [PubMed] [Google Scholar]
- 37.National Association of State Mental Health Program Directors Research Institute, Inc. (NRI) [18 October 2008];Results of a Survey of State Directors of Adult and Child Mental Health Services on Implementation of Evidence-Based Practices. 2005 January; http://www.nri-inc.org/reports_pubs/2005/EBPLillyFullReport2005.pdf.
- 38.Greenhalgh T, et al. Diffusion of Innovations in Service Organizations: Systematic Review and Recommendations. The Milbank Quarterly. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]; Drake, Skinner, Goldman What Explains the Diffusion [Google Scholar]
- 39.Institute of Medicine Improving the Quality [Google Scholar]; U.S. DHHS New Freedom Commission on Mental Health [Google Scholar]
- 40.Institute of Medicine Improving the Quality [Google Scholar]; Wu EQ, et al. Annual Prevalence of Diagnosed Schizophrenia in the USA: A Claims Data Analysis Approach. Psychological Medicine. 2006;36(11):1535–1540. doi: 10.1017/S0033291706008191. [DOI] [PubMed] [Google Scholar]
- 41.Institute of Medicine Improving the Quality [Google Scholar]
- 42.Domino ME, Frank RG, Rosenheck R. The Diffusion of New Antipsychotic Medications and Formulary Policy. Schizophrenia Bulletin. 2003;29(1):95–104. doi: 10.1093/oxfordjournals.schbul.a006995. [DOI] [PubMed] [Google Scholar]
- 43.Ibid.
- 44.Busch AB, Frank RG, Lehman AF. The Effect of a Managed Behavioral Health Carve-Out on Quality of Care for Medicaid Patients Diagnosed as Having Schizophrenia. Archives of General Psychiatry. 2004;61(5):442–448. doi: 10.1001/archpsyc.61.5.442. [DOI] [PubMed] [Google Scholar]
- 45.Dickey BD, et al. Guideline Recommendations [Google Scholar]
- 46.Ling DC, Berndt ER, Frank RG. Economic Incentives and Contracts: The Use of Psychotropic Medications. Contemporary Economic Policy. 2008;26(1):49–72. [Google Scholar]
- 47.Kaiser Family Foundation (KFF) Dual Eligibles: Medicaid's Role in Filling Medicare's Gaps. KFF; Washington DC: 2004. [Google Scholar]
- 48.Donohue J, Huskamp H, Zuvekas S. Dual-eligibles with Mental Disorders and Medicare Part D: How are they Faring? Health Affairs. 2009;(this issue) doi: 10.1377/hlthaff.28.3.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hermann RC, et al. Process Measures for the Assessment and Improvement of Quality of Care for Schizophrenia. Schizophrenia Bulletin. 2002;28(1):95–104. doi: 10.1093/oxfordjournals.schbul.a006930. [DOI] [PubMed] [Google Scholar]; National Committee for Quality Assurance HEDIS 2009 Summary Table of Measures, Product Lines, and Changes. http://www.ncqa.org/Portals/0/HEDISQM/HEDIS2009/2009_Measures.pdf (28 October 2008)
- 50.Koyanagi C, Forquer S, Alfano E. Medicaid Policies to Contain Psychiatric Drug Costs. Health Affairs. 2005;24(2):536–544. doi: 10.1377/hlthaff.24.2.536. [DOI] [PubMed] [Google Scholar]
- 51.Ibid.
- 52.Flynn LM. Commentary on the Schizophrenia Patient Outcomes Research Team (PORT) Studies. Schizophrenia Bulletin. 1998;24(1):20–32. doi: 10.1093/oxfordjournals.schbul.a033302. [DOI] [PubMed] [Google Scholar]; Mental Health America [21 January 2009];Factsheet: Schizophrenia: What You Need to Know. 2007 February 1; http://www.nmha.org/go/information/get-info/schizophrenia/schizophrenia-what-you-need-to-know.
- 53.Berndt ER, Donohue JM. The Economics of Advertising in Health Care Markets. In: Sloan F, Kasper H, editors. Incentives and Choice in Health Care. MIT Press; Cambridge, MA: 2008. [Google Scholar]
- 54.Drake, Skinner, Goldman What Explains the Diffusion [Google Scholar]
- 55.Goldman HH, Azrin ST. Public Policy and Evidence-Based Practice. Psychiatric Clinics of North America. 2003;26(4):899–917. doi: 10.1016/s0193-953x(03)00068-6. [DOI] [PubMed] [Google Scholar]; Institute of Medicine Improving the Quality [Google Scholar]
- 56.Schoenwald SK, Hoagwood K. Effectiveness, Transportability, and Dissemination of Interventions: What Matters When? Psychiatric Services. 2001;52(9):1190–1197. doi: 10.1176/appi.ps.52.9.1190. [DOI] [PubMed] [Google Scholar]
- 57.Alliance for Health Reform Comparative Effectiveness [Google Scholar]
- 58.Institute of Medicine Improving the Quality [Google Scholar]
- 59.Goldman and Azrin Public Policy [Google Scholar]
- 60.Kuhmerker K, Hartman T. Pay-for-Performance in State Medicaid Programs: A Survey of State Medicaid Directors and Programs. The Commonwealth Fund; New York: Apr, 2007. [Google Scholar]
- 61.Ibid.
- 62.Berman B. The Centers for Medicare and Medicaid Services’ Approach to Value-Based Purchasing. [30 October 2008];2008 June 17; Jefferson Digital Commons: http://jdc.jefferson.edu/cgi/viewcontent.cgi?article=1034&con text=vbp.; CBO The Overuse [Google Scholar]
- 63.Steinbrook R. Saying No Isn't NICE -- The Travails of Britain's National Institute for Health and Clinical Excellence. New England Journal of Medicine. 2008;359(19):1977–1981. doi: 10.1056/NEJMp0806862. [DOI] [PubMed] [Google Scholar]; CBO The Overuse [Google Scholar]
- 64.Rosenheck, Leslie, Doshi Second-Generation and Richard Frank's “cautionary note” that appears in the same issue: Frank, “Policy Toward.”
- 65.Institute of Medicine Improving the Quality [Google Scholar]
- 66.Goldman, Azrin Public Policy [Google Scholar]
- 67.Ganju V. Implementation of Evidence-Based Practices in State Mental Health Systems: Implications for Research and Effectiveness Studies. Schizophrenia Bulletin. 2003;29(1):125–131. doi: 10.1093/oxfordjournals.schbul.a006982. [DOI] [PubMed] [Google Scholar]
- 68.Dougherty D, Conway PH. The “3T's” Road Map to Transform US Health Care: The “How” of High-Quality Care. Journal of the American Medical Association. 2008;299(19):2319–2321. doi: 10.1001/jama.299.19.2319. [DOI] [PubMed] [Google Scholar]
- 69.Goldman, Azrin Public Policy [Google Scholar]
- 70.Alliance for Health Reform Comparative Effectiveness [Google Scholar]
- 71.Institute of Medicine Improving the Quality [Google Scholar]
- 72.Lohr S. Technology Gets a Piece of Stimulus. The New York Times. 2009 January 25; [Google Scholar]
- 73.Birkel RC, et al. Consumers and Families as Partners in Implementing Evidence-Based Practices. Psychiatric Clinics of North America. 2003;26(4):867–81. doi: 10.1016/s0193-953x(03)00065-0. [DOI] [PubMed] [Google Scholar]