Abstract
Background
Acupuncture is a popular complementary and alternative treatment for chronic back pain. Recent European trials suggest similar short-term benefits from real and sham acupuncture needling. This trial addresses the importance of needle placement and skin penetration in eliciting acupuncture effects for patients with chronic low back pain.
Methods
638 adults with chronic mechanical low back pain were randomized to: individualized acupuncture, standardized acupuncture, simulated acupuncture, or usual care. Ten treatments were provided over 7 weeks by experienced acupuncturists. The primary outcomes were back-related dysfunction (Roland Disability score, range: 0 to 23) and symptom bothersomeness (0 to 10 scale). Outcomes were assessed at baseline and after 8, 26 and 52 weeks.
Results
At 8 weeks, mean dysfunction scores for the individualized, standardized, and simulated acupuncture groups improved by 4.4, 4.5, and 4.4 points, respectively, compared with 2.1 points for those receiving usual care (P<0.001). Participants receiving real or simulated acupuncture were more likely than those receiving usual care to experience clinically meaningful improvements on the dysfunction scale (60% vs. 39%, P<0.0001). Symptoms improved by 1.6 to 1.9 points in the treatment groups compared with 0.7 points in the usual care group (P<0.0001). After one year, participants in the treatment groups were more likely than those receiving usual care group to experience clinically meaningful improvements in dysfunction (59% to 65% versus 50%, respectively, P=0.02) but not in symptoms (P>0.05).
Conclusions
Although acupuncture was found effective for chronic low back pain, tailoring needling sites to each patient and penetration of the skin appear to be unimportant in eliciting therapeutic benefits. These findings raise questions about acupuncture’s purported mechanisms of action. It remains unclear whether acupuncture, or our simulated method of acupuncture, provide physiologically important stimulation or represent placebo or non-specific effects.
INTRODUCTION
Americans spend at least $37 billion annually on medical care for back pain1, 2 and our economy suffers another $19.8 billion in lost worker productivity.3 There is no evidence that escalating expenses for spine care have improved self-assessed health status.2
Many back pain patients are dissatisfied with medical care4 and seek care from complementary and alternative medical providers, including acupuncturists.5, 6 Back pain is the leading reason for visits to licensed acupuncturists,7 and medical acupuncturists consider acupuncture an effective treatment for back pain.8
Several recent well-designed European trials have suggested that real acupuncture and sham acupuncture (e.g., shallow needling of points considered ineffective) are equally effective,9, 10 and both superior to best-practice medical care,10 usual care11–13 and a wait-list control.9
Our trial expands upon the findings of the European studies by: 1) including a non-insertive method of stimulating acupuncture points which permitted assessment of the need for needle insertion to achieve therapeutic benefit, 2) including both individualized and standardized forms of acupuncture, and 3) following patient outcomes for longer than most of the European trials. Thus, this trial was designed to address the following questions about the value of acupuncture for chronic low back pain:
Is acupuncture more effective than usual medical care alone?
Is real acupuncture more effective than simulated (non-insertive) acupuncture?
Is individualized acupuncture more effective than standardized acupuncture?
METHODS
Study Design
We conducted a four-arm randomized controlled trial comparing the effectiveness of individualized acupuncture, standardized acupuncture, simulated acupuncture and usual care. Study design details are described elsewhere.14 This trial was approved by the Institutional Review Boards of Group Health Cooperative and Kaiser Permanente, Northern California. All participants gave written informed consent.
Study Population
Patients 18 through 70 years of age receiving care for a back problem from an integrated health care delivery system in Western Washington and one in Northern California within the prior year were potentially eligible. We used electronic records to identify persons with diagnosis codes consistent with uncomplicated chronic low back pain within the prior 3–12 months. We excluded persons with 1) specific causes of back pain (e.g., cancer, fractures, spinal stenosis, infections), 2) complicated back problems (e.g., sciatica, prior back surgery, medico-legal issues), 3) possible contraindications for acupuncture (e.g., coagulation disorders, cardiac pacemakers, pregnancy, seizure disorder), 4) conditions making treatment difficult (e.g., paralysis, psychoses), and 5) conditions that might confound treatment effects or interpretation of results (severe fibromyalgia, rheumatoid arthritis, concurrent care from other providers). Persons with less than 3 months of back pain or previous acupuncture treatment for any condition were excluded.
Recruitment and Randomization Procedures
Recruitment occurred March 2004 through August 2006. Three to 12 months after back-related visits, potential participants were mailed invitation letters. Study staff telephoned respondents to determine final eligibility, which required a severity rating of at least 3 on the 0 to 10 back pain bothersomeness scale. We also mailed letters to members without recent visits for back pain and advertised in clinics and newsletters.
Those found eligible were administered a baseline questionnaire and randomly allocated using a centrally generated variable-sized block design to one of four treatment groups. Treatments began within two weeks of randomization. The study was described only as a comparison of three methods of stimulating acupuncture points without information about how treatments differed.
Study Treatments
Participants assigned to a real or simulated acupuncture treatment were treated twice weekly for three weeks, and then weekly for four weeks (10 treatments total). Participants were asked to wear eye masks and lie prone with their heads in a face cradle. Electrostimulation, moxibustion, herbs and other non-needle adjuncts were proscribed.
One of five Diagnostician acupuncturists with 7 to 18 years experience evaluated participants at each visit using Traditional Chinese Medical (TCM) diagnostic techniques and prescribed individualized TCM treatments to be used only for participants randomized to individualized acupuncture. A Therapist acupuncturist then delivered the assigned treatments, interacting minimally with participants and the Diagnostician, who remained masked to treatment. Treatments were performed in Research Clinics at the two sites by 6 licensed acupuncturists with a with 4 to 19 years experience. All acupuncturists were experienced using TCM acupuncture for musculoskeletal pain. Nine of the 11 study acupuncturists had at least 3 years of formal training and the two others had practiced for over 15 years.
Acupuncturists used sterile disposable 32-gauge needles (0.25 mm) at least 1.5 inches in length. Needling depth varied slightly, depending on the acupoint, but was generally between 1 and 3 cm.
Individualized acupuncture: This was the treatment prescribed by the Diagnostician at the beginning of each visit. It could include any acupoints that could be needled with the participant lying prone. There were no constraints on number of needles, depth of insertion, or needle manipulation. Treatments averaged 10.8 needles (range 5 to 20) retained for 18 minutes (range 15 to 20). Seventy-four distinct points were used, half on the “Bladder meridian” that includes points on the back and legs.
Standardized acupuncture: We used a standardized acupuncture prescription considered effective by experts for chronic low back pain.15 This included 8 acupoints commonly used for chronic low back pain (Du 3, Bladder 23- bilateral, low back ashi point, Bladder 40-bilateral, Kidney 3-bilateral) on the low back and lower leg.14 All acupoints were needled for 20 minutes, with stimulation by twirling the needles at 10 minutes and again just prior to needle removal. Therapists manipulated the needles to elicit “de qi,” which they perceive as a biomechanical response in tissue as it tightens around the inserted needle and constricts its movement.16
Simulated acupuncture: We developed a simulated acupuncture technique using a toothpick in a needle guidetube, which was found a credible acupuncture treatment by acupuncture-naïve patients with back pain.14,17 Simulating insertion involved holding the skin taut around each acupoint and placing a standard acupuncture needle guidetube containing a toothpick against the skin. The acupuncturist tapped the toothpick gently, twisting it slightly to simulate an acupuncture needle grabbing the skin, and then quickly withdrew the toothpick and guidetube while keeping his or her fingers against the skin for a few additional seconds to imitate the process of inserting the needle to the proper depth. All acupoints were “stimulated” with toothpicks at 10 minutes (i.e., the acupuncturist touched each acupoint with the tip of a toothpick without the guidetube, rotated the toothpick clockwise and then counterclockwise less than 30 degrees) and again at 20 minutes just before they were “removed.” To simulate withdrawal of the needle, the acupuncturist tightly stretched the skin around each acupoint, pressed a cotton ball firmly on the stretched skin, then momentarily touched the skin with a toothpick (without the guidetube) and quickly pulled the toothpick away using the same hand movements as in regular needle withdrawal. The acupuncturists simulated insertion and removal of needles at the eight acupoints used in the standardized treatment.
Usual Care Comparison Group: Participants in the usual care group received no study-related care—just the care, if any, they and their physicians chose (mostly medications, primary care, and physical therapy visits).
All participants received a self-care book with information on managing flare-ups, exercise, and life-style modifications.18
Outcome Measures
Outcomes were measured at baseline and after 8, 26 and 52 weeks using computer-assisted telephone interviews by interviewers masked to treatment. Pre-specified primary outcomes were back-related dysfunction and symptom bothersomeness at end of treatment (8 weeks). Dysfunction was measured using the modified Roland Disability Questionnaire, a reliable, valid and sensitive measure19 appropriate for telephone administration. Participants were also asked to rate how bothersome their pain had been during the past week on a 0 ("not at all bothersome") to 10 ("extremely bothersome") scale. This measure demonstrates substantial construct validity20–22.
Secondary outcomes included: 1) 26- and 52-week outcomes for the primary outcome measures, 2) proportion of participants with clinically meaningful improvements23 in dysfunction (3 or more point decrease on the Roland scale) and back pain (2 or more point decrease in symptom bothersomeness), 3) self-reported medication use for back pain in the prior week, 4) Physical and Mental Health Component Summary Scores of the SF-3624, and 5) number of days spent in bed, lost from work or school, or cutting down on usual activities due to back problems during past month. 25 Finally, participants’ use of health services for back pain during the year following randomization was measured using interview data and, for the Washington site, automated health plan utilization data.
We also asked questions to determine if participants in the acupuncture groups perceived different experiences and to assess efforts to mask the Diagnostician acupuncturists and outcomes assessors to study treatment.
Finally, participants were asked about adverse experiences at each visit and during the 8-week telephone follow-up. This trial was monitored by the National Center for Complementary and Alternative Medicine Data Safety Monitoring Board.
Statistical Analyses
Analyses were based on an intent-to-treat approach using randomized group assignment. The primary outcomes were analyzed as continuous measures. Analysis of covariance was used to test for treatment differences at follow-up, adjusting for the baseline measure. We also adjusted for site, age group (18–29, 30–39, 40–49, 50–59, 60+), and gender. Interactions of treatment group with age and site were added to test for effect modification by each of these covariates. Because expectations may influence outcomes, we also examined models that included expectation of acupuncture helpfulness and expectation of low back pain improvement as covariates and tested for effect modification with treatment groups dichotomized as treatment (real or simulated acupuncture) versus usual care.
Separate analyses were performed for each follow-up time. The 8-week follow-up was the primary end-point. Pair-wise comparisons using Tukey-Kramer adjustment were performed if the global test for differences among groups was significant at the p<0.05 (two-sided) level. The study was powered to detect mean differences of 2.0 points on the Roland-Morris scale and 1.5 points on the symptom bothersomeness scale, using variance estimates from our pilot study14. Previous studies have suggested that these cutoff values are at the lower end of clinically important differences21–23, so their use should result in ample statistical power. We had 99% power to detect such differences in the overall analysis and approximately 80% power to detect pair-wise differences after adjustment for multiple comparisons. To test for overall differences in our secondary outcomes, a chi-squared test was used for categorical outcomes and analysis of covariance was used for continuous outcomes. We used SAS/STAT Version 9.1. 26
RESULTS
Study Recruitment and Follow-up
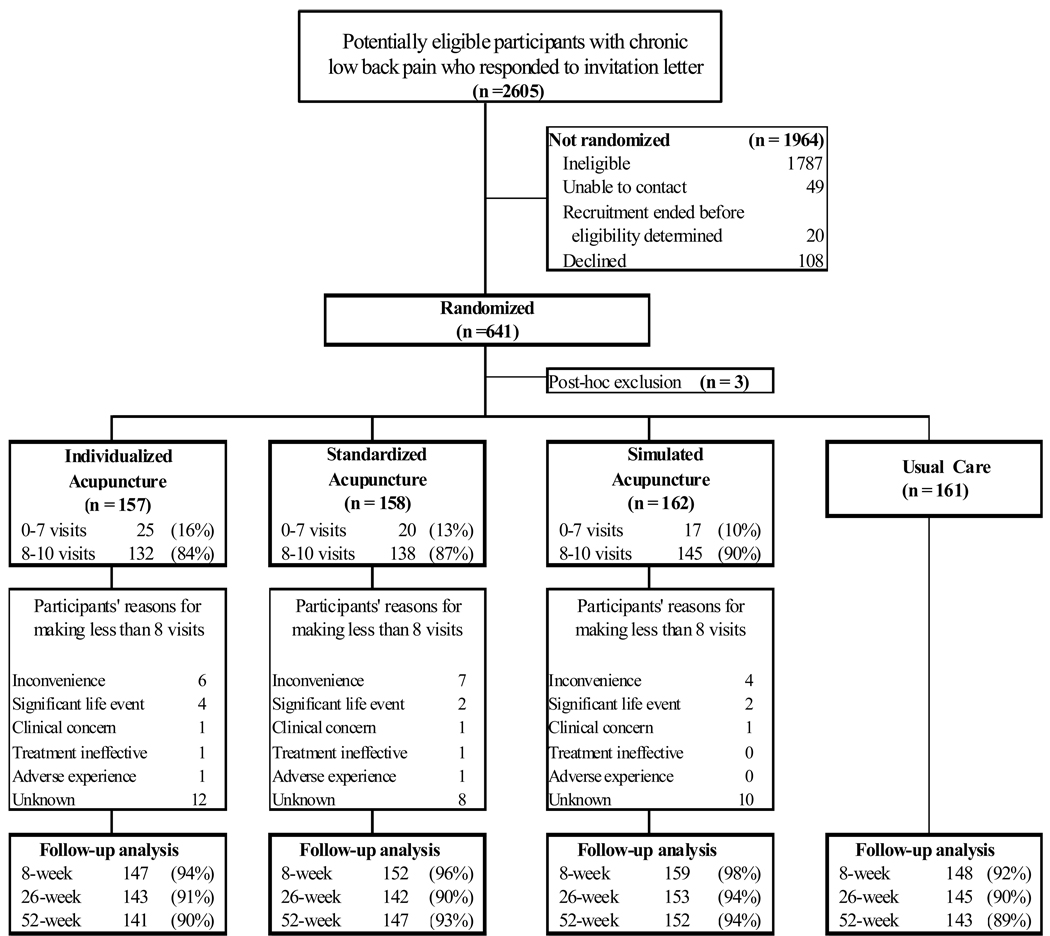
We evaluated 2,605 potential participants for eligibility; 641 (25%) were eligible and randomized (Figure 1). The main reasons for ineligibility were less than three months of back pain, sciatica, previous acupuncture, and inability to attend treatment visits. Three participants were excluded after randomization when we learned they had had exclusionary criteria when randomized (previous acupuncture treatment, involvement in litigation, and fibromyalgia). Therefore, analyses included 638 participants randomized to individualized acupuncture (n=157), standardized acupuncture (n=158), simulated acupuncture (n=162) or usual care (n=161). Follow-up rates were 95%, 91%, and 91% at 8, 26, and 52 weeks, respectively and were similar across groups.
Figure 1.
Study Participant Flow Diagram
Baseline Characteristics
Study participants had a mean age of 47 years, and were 62% female, 68% white, and 53% college graduates (Table 1). Overall mean scores of 10.6 on the Roland scale and 5.1 for symptom bothersomeness indicated moderately severe chronic back problems. Two-thirds of participants reported at least one year of pain and current use of low back pain medication. Overall, participants were moderately optimistic that acupuncture would help (mean of 6.7 on a 0–10 scale).
Table 1.
Baseline characteristics of 638 participants with chronic low back pain (LBP) by treatment group
| Treatment Group | |||||
|---|---|---|---|---|---|
| Characteristic | Individualized acupuncture (n=157) |
Standardized acupuncture (n=158) |
Simulated acupuncture (n=162) |
Usual care (n=161) |
Total (n=638) |
| Age, mean (SD), y | 47 (13) | 49 (13) | 47 (14) | 46 (13) | 47 (13) |
| Female, % | 68 | 56 | 60 | 64 | 62 |
| White, % | 67 | 69 | 72 | 65 | 68 |
| Hispanic origin, % | 7 | 9 | 8 | 8 | 8 |
| College graduate, % | 49 | 57 | 56 | 51 | 53 |
| Married, % | 55 | 60 | 61 | 60 | 59 |
| Annual household income ≥$45,000, % | 71 | 71 | 67 | 75 | 71 |
| Employed, % | 78 | 80 | 78 | 81 | 79 |
| Chronic pain for at least 1 year, % | 69 | 74 | 60 | 70 | 68 |
| Pain days in last 3 months, mean (SD) | 68 (26) | 74 (22) | 70 (24) | 74 (23) | 71 (24) |
| Pain below knee, % | 21 | 22 | 21 | 21 | 21 |
| Reduced activity ≥ 7 days in last 3 months due to LBP, % |
29 | 23 | 22 | 27 | 25 |
| Reduced activity on > 7 days in last 4 weeks due to LBP, % |
27 | 25 | 20 | 28 | 25 |
| Kept in bed or lying down ≥ day in last 4 weeks due to LBP, % |
17 | 22 | 21 | 22 | 21 |
| Kept from work/school for ≥1 day in last 4 weeks due to LBP, % |
19 | 22 | 22 | 18 | 21 |
| SF-36 Physical Health scale score, mean (SD) |
41 (9) | 42 (8) | 42 (8) | 42 (8) | 42 (8) |
| SF-36 Mental Health scale score, mean (SD) |
53 (8) | 54 (8) | 54 (7) | 53 (8) | 53 (8) |
| Symptom bothersomeness in past week (0–10 scale), mean (SD) |
5.0 (2.4) | 5.0 (2.3) | 4.9 (2.3) | 5.4 (2.3) | 5.1 (2.3) |
| Roland disability score (0–23 scale), mean (SD) |
10.8 (5.2) | 10.8 (5.5) | 9.8 (5.1) | 11.0 (5.1) | 10.6 (5.2) |
| Any medication use in past week, % | 62 | 62 | 63 | 65 | 63 |
| Expect at least moderate improvement in LBP in 1 year, % |
43 | 46 | 48 | 49 | 46 |
| Expectation of acupuncture helpfulness (0–10 scale), mean (SD) |
6.6 (1.8) | 6.5 (1.8) | 6.7 (1.9) | 7.0 (1.8) | 6.7 (1.8) |
Study Treatments
A priori, we defined treatment adherence as completion of 8 or more of the 10 possible visits. By this definition, 84%, 87%, and 90% of participants were adherent in the individualized, standardized, and simulated acupuncture groups, respectively. At 8 weeks, 18% of participants reported having read more than two-thirds of the self-care book with no differences among groups (p=0.42).
Primary Outcomes
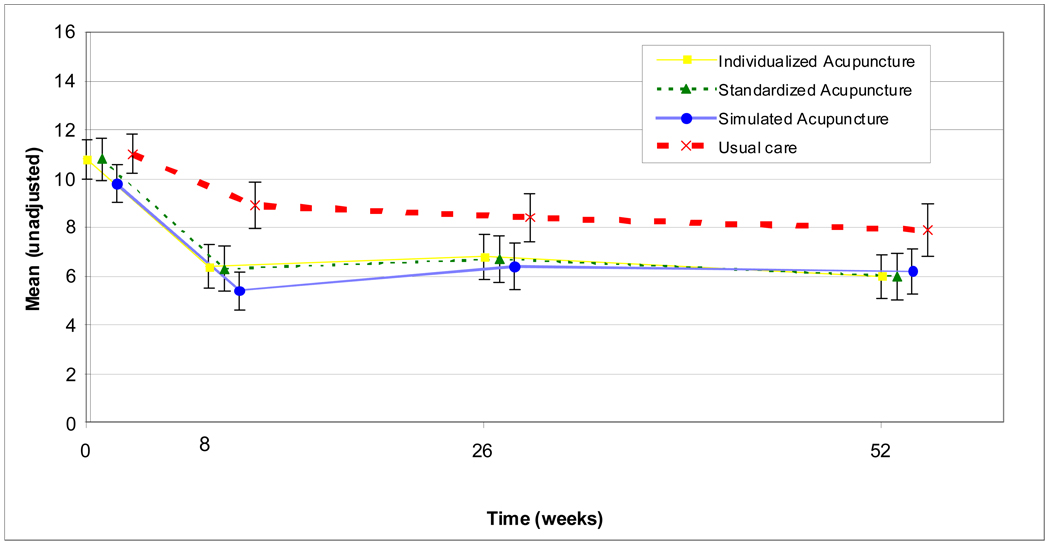
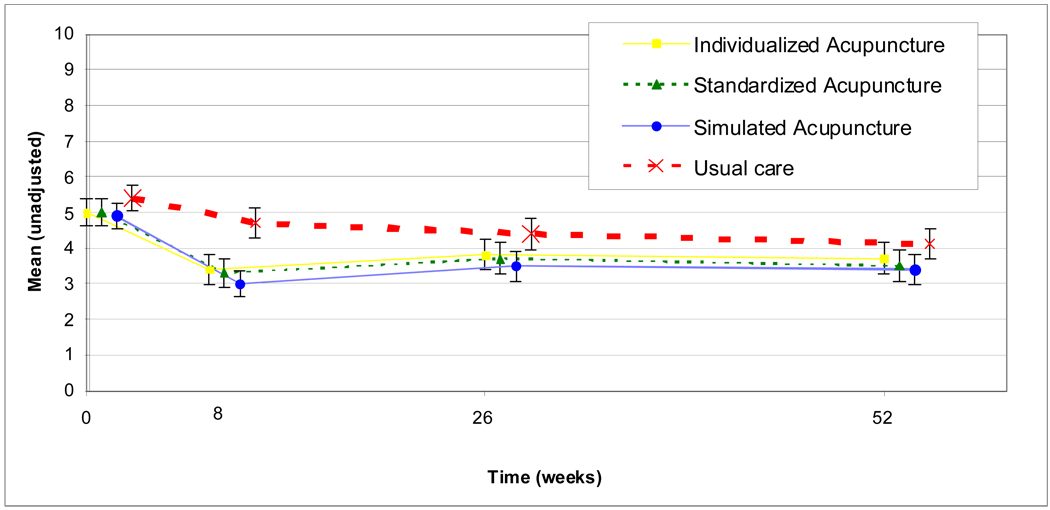
All groups showed improved function and decreased symptoms at the primary end-point of 8 weeks (Table 2, Figure 2 and Figure 3) in both the adjusted and unadjusted analyses. However, as seen in Table 2, unadjusted mean dysfunction scores for the individualized, standardized, and simulated acupuncture groups improved 4.4 to 4.5 points, compared with 2.1 points for those receiving usual care. There was a statistically significant difference in function among all four groups (P<0.0001 after adjustment for covariates) and statistically significant differences between usual care and each of the acupuncture groups adjusted for covariates and multiple comparisons (Table 3). However, there were no significant pairwise differences among the three acupuncture groups: individualized acupuncture was not significantly better than standardized acupuncture and real acupuncture was not significantly better than simulated acupuncture.
Table 2.
Mean Roland disability score and symptom bothersomeness score at baseline and follow-up by randomized treatment assignment
| Baseline | 8 weeks | 26 weeks | 52 weeks | |
|---|---|---|---|---|
| ROLAND DISABILITY | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| Individualized Acupuncture | 10.8 (5.2) | 6.4 (5.3) | 6.8 (5.5) | 6.0 (5.4) |
| Standardized Acupuncture | 10.8 (5.6) | 6.3 (5.7) | 6.7 (5.8) | 6.0 (5.8) |
| Simulated Acupuncture | 9.8 (5.2) | 5.4 (4.9) | 6.4 (6.0) | 6.2 (5.8) |
| Usual Care | 11.0 (5.2) | 8.9 (6.0) | 8.4 (6.0) | 7.9 (6.5) |
| Unadjusted p-value | P <0.0001 | P = 0.01 | P = 0.02 | |
| Adjusted p-value1 | P <0.0001 | P = 0.003 | P = 0.001 | |
| BOTHERSOMENESS | ||||
| Individualized Acupuncture | 5.0 (2.5) | 3.4 (2.7) | 3.8 (2.5) | 3.7 (2.6) |
| Standardized Acupuncture | 5.0 (2.3) | 3.3 (2.5) | 3.7 (2.6) | 3.5 (2.7) |
| Simulated Acupuncture | 4.9 (2.4) | 3.0 (2.4) | 3.5 (2.7) | 3.4 (2.7) |
| Usual Care | 5.4 (2.4) | 4.7 (2.6) | 4.4 (2.6) | 4.1 (2.6) |
| Unadjusted p-value | P <0.0001 | P = 0.03 | P = 0.12 | |
| Adjusted p-value1 | P <0.0001 | P = 0.04 | P = 0.12 | |
Adjusted for baseline outcome measure, site, age group (18–29, 30–39, 40–49, 50–59, 60–71), and gender
Figure 2.
Mean Roland disability scores and 95% confidence intervals by treatment group and time since randomization
Figure 3.
Mean symptom bothersomeness score and 95% confidence intervals by treatment group and time since randomization
Table 3.
Adjusted1 mean difference and 95% confidence intervals for pair-wise comparisons of Roland disability score and symptom bothersomeness score by treatment group and time since randomization
| 8 weeks | 26 weeks | 52 weeks | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Standardized Acupuncture |
Simulated Acupuncture |
Usual Care |
Standardized Acupuncture |
Simulated Acupuncture |
Usual Care |
Standardized Acupuncture |
Simulated Acupuncture |
Usual Care |
|
| Roland Disability | |||||||||
| Individualized Acupuncture |
0.16 −0.90, 1.22 |
0.45 −0.61, 1.50 |
−2.47* −3.53, −1.40 |
−0.05 −1.18, 1.08 |
−0.41 −1.53, 0.70 |
−1.86* −2.98, −0.74 |
−0.26 −1.40, 0.87 |
−1.10 −2.23, 0.04 |
−2.08* −3.22, −0.94 |
| Standardized Acupuncture |
0.29 −0.76, 1.33 |
−2.63* −3.69, −1.56 |
−0.36 −1.48, 0.75 |
−1.81* −2.94, −0.68 |
−0.84 −1.95, 0.28 |
−1.82* −2.95, −0.69 |
|||
| Simulated Acupuncture |
−2.91* −3.96, −1.86 |
−1.45 −2.56, −0.34 |
−0.98 −2.11, 0.14 |
||||||
| Bothersomeness | |||||||||
| Individualized Acupuncture |
0.22 −0.34, 0.77 |
0.52 −0.03, 1.07 |
−1.05* −1.60, −0.49 |
0.17 −0.43, 0.77 |
0.24 −0.35, 0.83 |
−0.54 −1.13, 0.06 |
0.20 −0.39, 0.79 |
0.17 −0.42, 0.76 |
−0.45 −1.04, 0.15 |
| Standardized Acupuncture |
0.30 −0.24, 0.85 |
−1.26* −1.82, −0.71 |
0.07 −0.52, 0.66 |
−0.71 −1.31, −0.11 |
−0.03 −0.61, 0.55 |
−0.65 −1.24, −0.06 |
|||
| Simulated Acupuncture |
−1.56* −2.11, −1.02 |
−0.78* −1.36, −0.19 |
−0.62 −1.21, −0.03 |
||||||
Adjusted for baseline outcome measure, site, age group (18–29, 30–39, 40–49, 50–59, 60–71), and gender
Significant at p<0.05 level after adjustment for multiple comparisons
Secondary Outcomes
Mean values of the primary outcomes remained relatively stable from 8 to 52 weeks (Figure 2 and Figure 3). The usual care group continued to have greater dysfunction than the real or simulated acupuncture groups through 52 weeks (p=0.001). The real and simulated acupuncture groups did not differ significantly from one another, accounting for multiple comparisons (P>0.05). The results for symptom bothersomeness were generally similar, but the differences among the four groups were smaller and no longer statistically significant at 52 weeks. Inclusion of the expectation measures did not alter the results and were not kept in the final models. There was no significant interaction between group and either age or site.
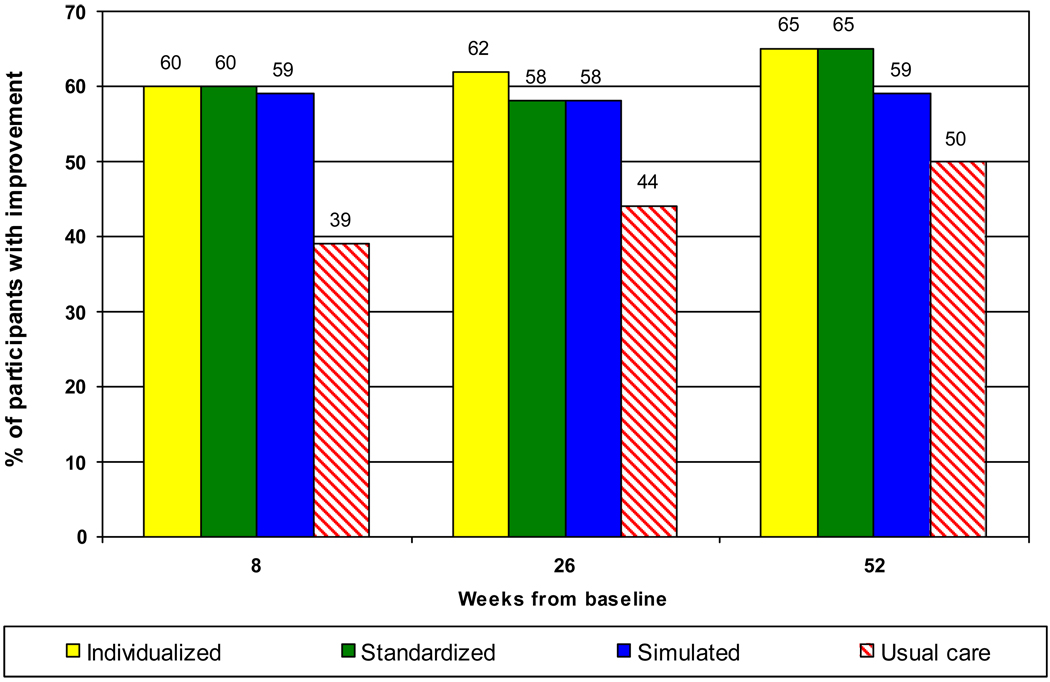
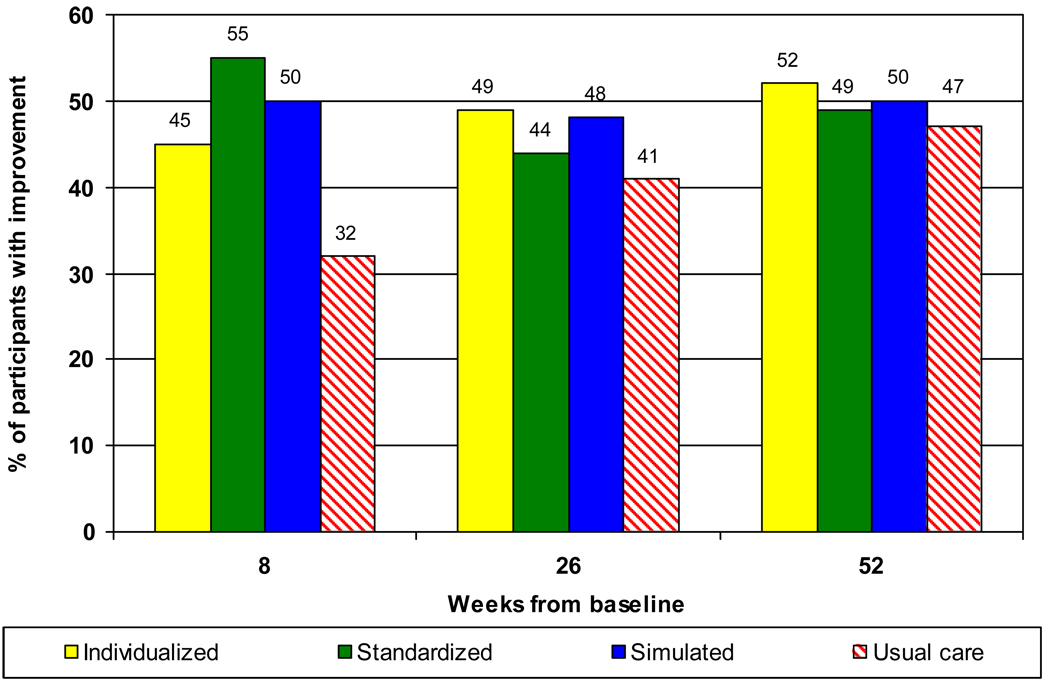
At 8 weeks, the proportion of participants improving at least 3 points on the Roland scale was about 60% in the real and simulated acupuncture groups, compared with only 39% in the usual care group (global test p<0.001) (Figure 4). These superior outcomes in function for the real and simulated acupuncture groups remained significant at 26 weeks (p=0.01) and 52 weeks (p=0.02). Similar results were found for improvements of at least 2 points on the symptom bothersomeness score at 8-weeks (p=0.0004) (Figure 5). However, overall differences were no longer significant at 26 or 52 weeks.
Figure 4.
Percent of participants improving by at least 3 points on the Roland scale
Figure 5.
Percent of participants improving by at least 2 points on the symptom bothersomeness scale
The use of medications for back pain in the past week (mostly non-steroidal anti-inflammatory drugs) was similar across groups at baseline (i.e., 62% to 65%) but by 8 weeks had decreased to 47% in the real and simulated acupuncture groups versus 59% in the usual care group (p=0.01). This difference persisted at 26 and 52 weeks.
There was an overall group difference (favoring real and simulated acupuncture) at 8 weeks in both the SF-36 Mental (p=0.03) and Physical (p=0.0008) component scores but these differences were small (less than 4 points) and no longer significant at 52 weeks. At 52 weeks, significantly more participants reported cutting down on activities for more than 7 days in the past month in the usual care group (18%) than in the real or simulated acupuncture groups (5–7%, p=0.0005). Similarly, more participants in the usual care group missed work or school for more than a day in the past month (16%) than in the real or simulated acupuncture groups (5–10%, p=0.01).
Co-interventions
Use of non-study treatments for back pain reported at the 8-week interview was similar across the real and simulated acupuncture groups so pooled results are reported. Participants in the usual care group were twice as likely as those receiving real or simulated acupuncture to report a physician or physical therapist visit (21% versus 11%; P=0.001) or have visited a complementary and alternative medicine (CAM) provider (18% versus 8%; P=0.0005).
Costs of Back-Related Health Care After Randomization
In the Washington site, mean total costs of back-related health services for the year after randomization were similar in the four treatment groups (range: $160–$221; P=0.65). This excludes costs of the study’s real and simulated acupuncture treatments and the cost of the one spine operation in the usual care group.
Treatment Credibility and Masking
Participants rated the two acupuncture and sham acupuncture treatments almost identically with regard to provider skills and caring. The Diagnostician acupuncturists rated the two acupuncture and simulated acupuncture groups very similarly with regard to apparent efficacy and likelihood of receiving individualized treatment.
Adverse Events
Eleven of the 477 participants receiving real or simulated acupuncture reported a moderate adverse experience possibly related to treatment (mostly short-term pain) and one reported a severe experience (pain lasting one month). One participant reported dizziness and another, back spasms. Rates of adverse experiences differed by treatment group: 6/157 for individualized acupuncture, 6/158 for standardized acupuncture, and 0/162 for simulated acupuncture (p=0.04).
DISCUSSION
Compared with usual care, individualized acupuncture, standardized acupuncture, and simulated acupuncture had beneficial and persisting effects on chronic back pain. These treatments resulted in clinically meaningful improvements in function. Substantial adverse experiences with needle insertion were infrequent (1/315 participants). Self-reported medication use in the real and simulated acupuncture groups decreased significantly more than in the usual care group and remained lower through the one year follow-up. However, the 8–10 acupuncture treatments received by most participants (which would cost between $600 and $1200) did not result in cost savings to the health plan during the year after randomization.
This trial differs from our earlier study--which found similar effects for acupuncture and a more rigorous educational intervention—in having a usual care group, subjects with more chronic pain, and participants who were all acupuncture-naïve. 25 However, our findings are consistent with those of recent high quality trials. One German trial found both real acupuncture and sham acupuncture (superficial needling at non-acupuncture points) to have similar effects that were superior to those of guideline-based conventional medical treatment.10 A second German trial found both real and sham acupuncture superior to a wait list control group, but not significantly different from each other.9 Finally, a British trial found traditional acupuncture care delivered in a primary care setting to have modestly superior results to usual care after 2 years.12 Our trial extends these studies, by demonstrating that needle insertion is not necessary to achieve therapeutic benefits and by measuring longer term outcomes.
Collectively, these recent trials provide strong and consistent evidence that real acupuncture needling using the Chinese meridian system is no more effective for chronic back pain than various purported forms of “sham” acupuncture. However, both real and sham acupuncture appear superior to usual care. Possible explanations for these findings are: 1) superficial acupoint stimulation directly stimulates physiological processes that ultimately lead to improved pain and function, or, 2) participants’ improved functioning resulted from non-specific effects such as therapist conviction, patient enthusiasm, or receiving a treatment believed to be helpful.
The appropriateness of using minimal, superficial, or sham control groups in trials of acupuncture remains controversial. 28 In fact, the use of blunt needles that did not penetrate the skin was described two thousand year-old ago in the classic book on acupuncture needling. 29 A study using functional magnetic resonance imaging found that superficial and deep needling of an acupuncture point elicited similar blood oxygen level dependent responses. 30 Another study demonstrated that light touch of the skin can stimulate mechanoreceptors that induce emotional and hormonal reactions which in turn alleviate the affective component of pain. 31 This could explain why trials evaluating acupuncture for pain have failed to find real acupuncture superior to sham or superficial control treatments and raises questions about whether sham treatments truly serve as inactive controls.
The possibility that an acupuncture treatment “experience” could be beneficial due to non-specific effects is also credible. 32 A recent acupuncture trial for irritable bowel syndrome reported that non-specific effects (especially the patient-clinician relationship) produced statistically and clinically significant outcomes. 33,34 The potency of non-specific effects has also been noted in placebo-controlled randomized trials of surgical interventions for pain conditions. 35,36
The main strengths of this trial are its size, high compliance and follow-up rates, long-term follow-up, inclusion of a simulated acupuncture control, and effective masking. Limitations include restricting treatment to a single component (needling) of normal Traditional Chinese Medicine acupuncture; 37 pre-specification of the number and duration of treatments; limited conversation between acupuncturists and participants; and, exclusion of a medical attention control group. However, a recent trial using a similar number and duration of visits for both the acupuncture and medical care control groups, also found acupuncture superior.10
Our results have important implications for key stakeholders. For clinicians and patients seeking a relatively safe 38,39 and effective treatment for a condition for which conventional treatments are often ineffective, various methods of acupuncture point stimulation appear to be reasonable options, even though the mechanism of action remains unclear. Furthermore, the reduction in chronic exposure to the potential side effects of medications is an important benefit that may enhance the safety of conventional medical care. The number of patients that would need to be treated with insertive or superficial acupuncture stimulation to result in one person achieving meaningful improvement in function ranges from 5 (for short term benefits) to 8 (for persisting benefits).
In conclusion, acupuncture-like treatments significantly improved function in persons with chronic low back pain. However, the finding that benefits of real acupuncture needling were no greater than those of non-insertive stimulation raises questions about acupuncture’s purported mechanism of action. Future research is needed to determine the relative contributions of the physiologic effects of non-insertive stimulation, patient expectations, and other non-specific effects.
Acknowledgments
Source of Funding and Support and Role of Sponsor
This trial was funded through an NIH Cooperative Agreement (U01 AT 001110) with the National Center for Complementary and Alternative Medicine (NCCAM). The sponsor (NIH), through its Project Officer, Dr. Partap Khalsa, was involved in the analysis and interpretation of data and review and approval of the manuscript. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of NCCAM. We thank our original NCCAM Project Officer, Dr. Richard Nahin, for helpful advice.
Acknowledgement of Persons Making Substantial Contributions Who are Not Authors
We also thank the following people for their assistance with this study: Diagnostician and Therapist acupuncturists in private practice (Sara Bayer, LAc; Ramey Fair, LAc; Larry Forsberg, LAc; Roxanne Geller, LAc; Caryn Goldman, LAc; Paul Griffin, LAc; Susan M. Kaetz, MPH, LAc, Ken Morris, LAc; Sabi Inderkum, LAc; Sachiko Nakano, LAc; Deborah Stanfill, LAc; Eliot Wagner, LAc), Clinic Research Assistants at Group Health Center for Health Studies (Zoe Bermet, Marissa Brooks, John Ewing, Erika Holden, Danielle Huston, Christel Kratohvil, Melissa Parson); Clinic Research Assistants at Kaiser Permanente Northern California Division of Research (Olivia Anaya, Pete Bogdanos, Cynthia H. Huynh, Rebecca Rogot, Caroline M. Sison), consultant acupuncturist in private practice Kabba Anand, DAc, LAc; physician with Kaiser Permanente Northern California Harley Goldberg, DO; Juanita Jackson (Administrative Assistant, Group Health Center for Health Studies) and John Maio (programmer, Kaiser Permanente Northern California Division of Research). All individuals named above were compensated for their roles in the project. We also thank Lhasa OMS, Weymouth Massachusetts, for donating the Seirin acupuncture needles used in this study.
Author’s Contributions
Daniel C Cherkin
conception and design
acquisition of data
analysis and interpretation of data
drafting the manuscript
critical revision of the manuscript for important intellectual content
obtaining funding
administrative, technical, or material support
supervision
Karen J. Sherman PhD
conception and design
acquisition of data
analysis and interpretation of data
drafting the manuscript
critical revision of the manuscript for important intellectual content
obtaining funding
supervision
Andrew L. Avins MD, MPH
acquisition of data
analysis and interpretation of data
critical revision of the manuscript for important intellectual content
obtaining funding
supervision
Janet H. Erro, RN, MN
acquisition of data
critical revision of the manuscript for important intellectual content
administrative, technical, or material support
supervision
Laura Ichikawa, MS
analysis and interpretation of data
critical revision of the manuscript for important intellectual content
statistical analysis
William E. Barlow, PhD
conception and design
acquisition of data
analysis and interpretation of data
drafting the manuscript
critical revision of the manuscript for important intellectual content
statistical analysis
supervision
Kristin Delaney, MPH
acquisition of data
analysis and interpretation of data
critical revision of the manuscript for important intellectual content
statistical analysis
Rene Hawkes, BA
acquisition of data
critical revision of the manuscript for important intellectual content
administrative, technical, or material support
Luisa Hamilton
drafting the manuscript
critical revision of the manuscript for important intellectual content
administrative, technical, or material support
supervision
Alice Pressman
analysis and interpretation of data
drafting the manuscript
statistical analysis
Partap S. Khalsa PhD
analysis and interpretation of data
critical revision of the manuscript for important intellectual content
supervision
Richard A. Deyo MD, MPH
conception and design
analysis and interpretation of data
critical revision of the manuscript for important intellectual content
administrative, technical, or material support
Footnotes
TRIAL REGISTRATION: NCT00065585 [ClinicalTrials.gov].
Author Access to Data
The Principal Investigator, Dan Cherkin, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosure of Potential Conflicts of Interest
None of the authors had a conflict of interest; including financial interests, relationships or affiliations relevant to the subject of this manuscript.
Previous Presentation of Information Reported in the Manuscript
Portions of the results described in this manuscript were presented at the the Ninth International Forum for Primary Care Research on Low Back Pain, Majorca, Spain, October 6, 2007.
REFERENCES
- 1.Luo X, Pietrobon R, Sun SX, Liu GG, Hey L. Estimates and patterns of direct health care expenditures among individuals with back pain in the United States. Spine. 2004 Jan 1;29(1):79–86. doi: 10.1097/01.BRS.0000105527.13866.0F. [DOI] [PubMed] [Google Scholar]
- 2.Martin BI, Deyo RA, Mirza SK, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008 Feb 13;299(6):656–664. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 3.Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA. 2003 Nov 12;290(18):2443–2454. doi: 10.1001/jama.290.18.2443. [DOI] [PubMed] [Google Scholar]
- 4.Consumer Reports. How is your doctor treating you? 1995
- 5.Wolsko PM, Eisenberg DM, Davis RB, Kessler R, Phillips RS. Patterns and perceptions of care for treatment of back and neck pain: results of a national survey. Spine. 2003 Feb 1;28(3):292–297. doi: 10.1097/01.BRS.0000042225.88095.7C. discussion 298. [DOI] [PubMed] [Google Scholar]
- 6.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004 May 27;(343):1–19. [PubMed] [Google Scholar]
- 7.Cherkin DC, Deyo RA, Sherman KJ, et al. Characteristics of visits to licensed acupuncturists, chiropractors, massage therapists, and naturopathic physicians. J Am Board Fam Pract. 2002 Nov–Dec;15(6):463–472. [PubMed] [Google Scholar]
- 8.Diehl DL, Kaplan G, Coulter I, Glik D, Hurwitz EL. Use of acupuncture by American physicians. J Altern Complement Med. 1997 Summer;3(2):119–126. doi: 10.1089/acm.1997.3.119. [DOI] [PubMed] [Google Scholar]
- 9.Brinkhaus B, Witt CM, Jena S, et al. Acupuncture in patients with chronic low back pain: a randomized controlled trial. Arch Intern Med. 2006 Feb 27;166(4):450–457. doi: 10.1001/archinte.166.4.450. [DOI] [PubMed] [Google Scholar]
- 10.Haake M, Muller HH, Schade-Brittinger C, et al. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007 Sep 24;167(17):1892–1898. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- 11.Thomas KJ, MacPherson H, Ratcliffe J, et al. Longer term clinical and economic benefits of offering acupuncture care to patients with chronic low back pain. Health Technol Assess. 2005 Aug;9(32):iii–iv. ix–x, 1–109. doi: 10.3310/hta9320. [DOI] [PubMed] [Google Scholar]
- 12.Thomas KJ, MacPherson H, Thorpe L, et al. Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain. BMJ. 2006 Sep 23;333(7569):623. doi: 10.1136/bmj.38878.907361.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Witt CM, Jena S, Selim D, et al. Pragmatic randomized trial evaluating the clinical and economic effectiveness of acupuncture for chronic low back pain. Am J Epidemiol. 2006 Sep 1;164(5):487–496. doi: 10.1093/aje/kwj224. [DOI] [PubMed] [Google Scholar]
- 14.Cherkin DC, Sherman KJ, Hogeboom CJ, et al. Efficacy of acupuncture for chronic low back pain: protocol for a randomized controlled trial. Trials. 2008;9:10. doi: 10.1186/1745-6215-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sherman KJ, Cherkin DC. Developing methods for acupuncture research: rationale for and design of a pilot study evaluating the efficacy of acupuncture for chronic low back pain. Altern Ther Health Med. 2003 Sep–Oct;9(5):54–60. [PubMed] [Google Scholar]
- 16.Langevin HM, Churchill DL, Fox JR, Badger GJ, Garra BS, Krag MH. Biomechanical response to acupuncture needling in humans. J Appl Physiol. 2001 Dec;91(6):2471–2478. doi: 10.1152/jappl.2001.91.6.2471. [DOI] [PubMed] [Google Scholar]
- 17.Sherman KJ, Hogeboom CJ, Cherkin DC, Deyo RA. Description and validation of a noninvasive placebo acupuncture procedure. J Altern Complement Med. 2002 Feb;8(1):11–19. doi: 10.1089/107555302753507140. [DOI] [PubMed] [Google Scholar]
- 18.Moore JE, Lorig K, Von Korff M, Gonzalez V, Laurent D. The Backpain Helpbook. Reading, MA: Perseus Publishing; 1999. [Google Scholar]
- 19.Bombardier C. Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine. 2000 Dec 15;25(24):3100–3103. doi: 10.1097/00007632-200012150-00003. [DOI] [PubMed] [Google Scholar]
- 20.Dunn KM, Croft PR. Classification of low back pain in primary care: using "bothersomeness" to identify the most severe cases. Spine. 2005 Aug 15;30(16):1887–1892. doi: 10.1097/01.brs.0000173900.46863.02. [DOI] [PubMed] [Google Scholar]
- 21.Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20:1899–1909. doi: 10.1097/00007632-199509000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Cherkin DC, Deyo RA, Street JH, Barlow W. Predicting poor outcomes for back pain seen in primary care using patients' own criteria. Spine. 1996;21:2900–2907. doi: 10.1097/00007632-199612150-00023. [DOI] [PubMed] [Google Scholar]
- 23.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine. 2008 Jan 1;33(1):90–94. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 24.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–483. [PubMed] [Google Scholar]
- 25.Riess PW. Current estimates from the national health interview survey: United States, 1984. Hyattsville, MD: 1986. PHS 86–1584. [PubMed] [Google Scholar]
- 26.SAS/STAT 9.1 User's Guide [computer program]. Version. Cary, NC: SAS Institute Inc; 2004. [Google Scholar]
- 27.Cherkin DC, Eisenberg D, Sherman KJ, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med. 2001 Apr 23;161(8):1081–1088. doi: 10.1001/archinte.161.8.1081. [DOI] [PubMed] [Google Scholar]
- 28.Lewith GT, White PJ, Kaptchuk TJ. Developing a research strategy for acupuncture. Clin J Pain. 2006 Sep;22(7):632–638. doi: 10.1097/01.ajp.0000210908.42299.1a. [DOI] [PubMed] [Google Scholar]
- 29.Birch SJ, Felt RL. Understanding Acupuncture. New York: Churchill Livingstone; 1999. [Google Scholar]
- 30.MacPherson H, Green G, Nevado A, et al. Brain imaging of acupuncture: comparing superficial with deep needling. Neurosci Lett. 2008 Mar 21;434(1):144–149. doi: 10.1016/j.neulet.2008.01.058. [DOI] [PubMed] [Google Scholar]
- 31.Lund I, Lundeberg T. Are minimal, superficial or sham acupuncture procedures acceptable as inert placebo controls? Acupunct Med. 2006 Mar;24(1):13–15. doi: 10.1136/aim.24.1.13. [DOI] [PubMed] [Google Scholar]
- 32.Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. Lancet. 2001 Mar 10;357(9258):757–762. doi: 10.1016/s0140-6736(00)04169-6. [DOI] [PubMed] [Google Scholar]
- 33.Kaptchuk TJ, Kelley JM, Conboy LA, et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008 May 3;336(7651):999–1003. doi: 10.1136/bmj.39524.439618.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spiegel D, Harrington A. What is the placebo worth? BMJ. 2008 May 3;336(7651):967–968. doi: 10.1136/bmj.39535.344201.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cobb LA, Thomas GI, Dillard DH, Merendino KA, Bruce RA. An evaluation of internal-mammary-artery ligation by a double-blind technic. N Engl J Med. 1959 May 28;260(22):1115–1118. doi: 10.1056/NEJM195905282602204. [DOI] [PubMed] [Google Scholar]
- 36.Moseley JB, O'Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002 Jul 11;347(2):81–88. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 37.Sherman KJ, Cherkin DC, Eisenberg DM, Erro J, Hrbek A, Deyo RA. The practice of acupuncture: who are the providers and what do they do? Ann Fam Med. 2005 Mar–Apr;3(2):151–158. doi: 10.1370/afm.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.MacPherson H, Thomas K, Walters S, Fitter M. A prospective survey of adverse events and treatment reactions following 34,000 consultations with professional acupuncturists. Acupunct Med. 2001 Dec;19(2):93–102. doi: 10.1136/aim.19.2.93. [DOI] [PubMed] [Google Scholar]
- 39.White A, Hayhoe S, Hart A, Ernst E. Adverse events following acupuncture: prospective survey of 32 000 consultations with doctors and physiotherapists. BMJ. 2001 Sep 1;323(7311):485–486. doi: 10.1136/bmj.323.7311.485. [DOI] [PMC free article] [PubMed] [Google Scholar]