Abstract
Lack of a dengue hemorrhagic animal model recapitulating human dengue virus infection has been a significant impediment in advancing our understanding of the early events involved in the pathogenesis of dengue disease. In efforts to address this issue, a group of rhesus macaques were intravenously infected with dengue virus serotype 2 (strain 16 681) at 1 × 107 PFU/animal. A classic dengue hemorrhage developed 3 to 5 days after infection in 6 of 6 animals. Blood chemistry appeared to be normal with exception of creatine phosphokinase, which peaked at 7 days after infection. A modest thrombocytopenia and noticeable neutropenia concomitant with slight decrease of hemoglobin and hematocrit were registered. In addition, the concentration of D-dimer was elevated significantly. Viremia peaked at 3 to 5 days after infection followed by an inverse relationship between T and B lymphocytes and a bimodal pattern for platelet-monocytes and platelet-neutrophil aggregates. Dengue virus containing platelets engulfed by monocytes was noted at 8 or 9 days after infection. Thus, rhesus macaques inoculated intravenously with a high dose of dengue virus produced dengue hemorrhage, which may provide a unique platform to define the early events in dengue virus infection and help identify which blood components contribute to the pathogenesis of dengue disease.
Introduction
Dengue is one of the most important mosquito-borne viral diseases affecting humans, with more than half of the world's population at risk. Previously, dengue infections occurred primarily as epidemics in tropical and subtropical countries. But over time, increasing globalization has contributed to the geographic spread of dengue vectors, including Aedes aegypti and A albopictus mosquitoes, leading to a steady penetration of dengue virus infection in just about every corner of the world.1,2 A wide spectrum of clinical manifestations has been noted, which range from asymptomatic, mild febrile illness (dengue fever [DF]) to dengue hemorrhagic fever (DHF)/dengue shock syndrome (DSS), a life-threatening illness. There are 4 serotypes of the dengue virus (DENV 1-4), and each serotype is capable of inducing DHF/DSS on infection. The pathologic hallmarks that determine disease severity and distinguish DHF from DF and other viral hemorrhagic fevers are plasma/vascular leakage resulting from increased vascular permeability and abnormal hemostasis. However, little is known about the mechanisms leading to DF and DHF/DSS. Although DHF/DSS has been reported to occur at a higher frequency after secondary infection with a heterologous dengue serotype, numerous reports have also documented DHF in primary dengue virus infections3–9 and dengue viral loads appear to correlate with severity of dengue disease,10 suggesting that the level of virus replication may dictate the occurrence of clinical disease. Currently, there are no effective vaccines or therapeutic drugs available to prevent or treat dengue viral infection.
A central problem in understanding the pathogenesis of dengue virus infection is the paucity of small animal models of human dengue virus infection.11,12 Each of the small animal models that have been described so far, although clearly informative, possess inherent limitations and do not faithfully mimic human dengue virus illness. The development of neurovirulence not typically observed in dengue-infected humans in one such small animal model of dengue infection highlights the limitations of using such animal models.13,14 Thus, the development of a reliable animal model of DHF that recapitulates the clinical sequelae of human dengue virus infection would provide a powerful tool to begin to examine some of the fundamental issues that have remained unresolved with regards to the mechanisms of dengue virus–induced pathogenesis. The availability of such a model also provides a tool for the optimal screening of dengue virus–directed antiviral drugs and, more importantly, as a model for the evaluation of effective prophylactic and/or therapeutic dengue virus vaccines. Moreover, the availability of such a model might provide a consensus regarding the initial lineage of the host cell that serves as the target of initial infection and replication, an issue that remains a subject of debate despite all these years of dengue virus research.
The Asian rhesus macaque (Macaca mulatta; RM) has been accepted to be a valid nonhuman primate (NHP) model to study select aspects of dengue viral infection and disease.15–19 The subcutaneous and/or intramuscular experimental inoculation of rhesus monkeys with dengue virus has been reasoned to mimic the route of natural mosquito infection; however, infection of such monkeys via these routes results in viral loads that are several orders of magnitude below human viral loads in patient experiencing DHF/DSS; and probably because of this modest replication, clinical sequelae typical of human dengue virus infection have never been observed in macaques. Although the reasons for this remain unclear, perhaps the failure may indeed be the result of the route of infection. This view is supported by studies conducted almost a half a century ago that documented evidence for the direct deposit of dengue virus into the capillary by the A aegypti mosquito during the engorgement period.20 Interestingly, Ashburn and Craig, in an attempt to identify the etiology of dengue, demonstrated that intravenous injection of unfiltered dengue blood into healthy men is capable of producing signs and symptoms typical of human dengue virus infection.21 Results of the studies reported herein indeed substantiate this hypothesis. Thus, “intravenous” experimental infection with a high virus inoculum (1 × 107 PFU/animal) of a group of adult RMs with dengue virus serotype 2 resulted in readily visible hemorrhage on day 3 to 5 after infection, which is one of the cardinal features of human DHF. We submit that, although these findings are preliminary, they do, for the first time, provide a model that can readily be tested and verified. The systematic evaluation of the dynamics of the clinical, immunologic, and virologic manifestations of “intravenous” dengue virus infection in these RMs is the subject of this communication.
Methods
Nonhuman primates, virus, and cells
We inoculated a total of 6 RMs (Table 1) of Indian origin with 1 mL of dengue serotype 2 (16681 strain, Vero grown, kindly provided by Dr Gubler, University of Hawaii Asia-Pacific Institute of Tropical Medicine and Infectious Diseases) containing 107 PFU/mL intravenously, whereas one control animal received control Vero cell supernatant fluid. Virus titrations were carried out by plaque assay in Vero cells.22 All experimental protocols and procedures were conducted following approval by the Emory Institutional Animal Care and Use Committee (IACUC), and all animals were housed at the Yerkes National Primate Research Center of Emory University and cared for in conformance to the guidelines of the Committee on the Care and Use of Laboratory Animals of the Institute of Laboratory Animal Resources, National Research Council and the Health and Human Services.23 There were basically 2 types of monkeys used (Table 1): older ovariectomized females (12-14 years old, n = 4) and young adult males (∼ 3 years old).
Table 1.
Animal specifications
| Monkey | Sex | Age, y | Weight, kg | Notes |
|---|---|---|---|---|
| RM1 (RDf-4)* | F | 14.10 | 10.39 | Ovariectomized |
| RM2 (RNm-5) | F | 12.8 | 10.29 | Ovariectomized |
| RM3 (RRd-5) | F | 12.10 | 8.66 | Ovariectomized |
| RM4 (REj-5) | F | 14 | 11.4 | Ovariectomized |
| RM5 (Ryc-11) | M | ∼ 3.5 | 7.65 | — |
| RM6 (RNe-11) | M | 3 | 6.7 | — |
| RM7 (RRv-10)† | M | 3 | 6.6 | — |
| RM8 (RBv-10)‡ | M | 3 | 6.8 | — |
All monkeys used in this study were Indian RMs. Each monkey bore a specific tattoo mark (shown in parentheses). — indicates not applicable.
Killed on day 7 after infection.
Mock infection with media from Vero cells cultured for the dengue virus serotype 2 stock. This animal was used as a control.
Uninfected RM for the deriving values of the normal levels of coagulation parameters.
Complete blood count and coagulation parameter assays
Samples were collected under ketamine anesthesia: Blood was collected by venipuncture using 3.2% citrate as an anticoagulant, and bone marrow was aspirated from the iliac crest and supplemented with heparin. Complete blood counts were performed with each blood collection by the Yerkes Clinical Pathology Laboratory, and complete serum chemistries were analyzed on the samples by Antech. Citrated plasma samples were submitted to the Emory University Hospital Laboratories for analyses of the coagulation parameters.
Quantitation of viral load with real-time RT-PCR
Plasma viral load was determined according to a method described previously.24 Briefly, RNA was extracted from 140 μL of plasma using the QIAmp Viral RNA Mini kit (QIAGEN). The dengue 2 fluorogenic probe and its flanking primers were prepared as described by Houng et al25 and custom synthesized by Operon. The viral RNA copy number was determined using a real-time one-step quantitative reverse-transcribed polymerase chain reaction (RT-PCR) assay using the TaqMan RT kit (Perkin Elmer Applied Biosystem) and Bio-Rad iCycler system using a standard control for virus quantitation by the quantitative RT-PCR assay similar to the one previously described.25 The limit of detection is approximately 100 copies of RNA equivalent viral genome per milliliter in this assay.
FACS analysis and immunohistochemistry
Whole blood was stained with a panel of cell surface markers conjugated with various fluorochromes, lysis of red blood cells, and subjected to multicolor fluorescence-activated cell sorter (FACS) analysis according to a protocol standardized in our laboratory. Two panels of antibodies were used: one was for T-cell, B-cell, and NK-cell subset phenotyping, which included CD16/NKG2A/CD14/CD45/CD4/CD8 /CD56/CD3/CD20; and the second panel was for platelet-leukocyte aggregation and included CD41/CD61/CD62P/CD14/CD45. The frequency of leukocyte subpopulations that aggregate with platelet was identified by gating on CD41+ CD61+ CD62P+. In addition, the characterization of monocyte and neutrophil populations was performed as described by Lafont et al.26 Multicolor flow cytometric analysis was performed on an LSRII flow cytometer (BD Biosciences) using BD FACSDiva software (BD Biosciences). All data were analyzed by FlowJo software (TreeStar). Immunohistochemistry was performed according to the standard protocol.
ELISA
Serum titers of antidengue IgM and IgG were determined by antibody-capture enzyme-linked immunosorbent assay (ELISA) as described elsewhere.27 The increase of antibody titers was expressed as a percentage of the optical density (OD) values obtained on samples from the same monkey on day 0 (before infection). The following formula was used to calculate the percentage of the antibody increase in each monkey:
Percentage of antibody increase (%) = ([daily OD readings − OD reading of day 0]/OD reading of day 0) × 100.
Statistical analyses
Data analysis was performed using GraphPad software (Prism 5, www.graphpad.com). The t test was used for the comparisons of specific populations of subphenotype of lymphocytes between lymphocytes and the sublymphocyte populations. P values less than .05 were considered statistically significant.
Results
The need to conduct detailed multiple analyses during the acute infection period, coupled with the constraints placed on the volume of blood that can be collected from individual animals within a fixed period of time, dictated that select studies be performed on samples from individual animals only. The data presented therefore are representative of staggered sample collections from individual animals or when available an average from combined data in the case when a complete set of the parameters were available.
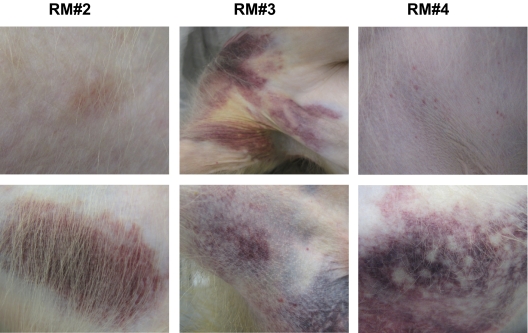
Hemorrhage in dengue-infected rhesus monkeys
For these studies, we infected 6 rhesus monkeys with a high dose of dengue virus intravenously and unexpectedly succeeded, for the first time, in inducing coagulopathy reminiscent of dengue hemorrhagic symptoms previously documented in human cases of DHF in 6 of the 6 infected animals (Figure 1; supplemental Figure 1, available on the Blood website; see the Supplemental Materials link at the top of the online article). By day 3 to 5, all 6 monkeys exhibited petechiae (small red spot) and mild to extensive subcutaneous hematoma consistent with coagulopathy, which lasted for approximately 10 days before symptoms resolved by day 14 after infection. Figure 1 shows representative gross morphologic images that appear to be similar to the hemorrhagic manifestations observed in dengue-infected human patients. In one animal, a rash characterized by a general morbilliform eruption with petechiae and islands of sparing, white islands in a sea of red (Figure 1, rhesus macaque 4 [RM4]), a general pattern thought to be an immune response to the dengue virus,28–30 was observed. Clinical symptoms were in general more extensive and apparent in the older females than the young adult males, suggesting potential relative differences in susceptibility secondary to gender and/or age, an aspect that will require being addressed in future studies. Of note, the animals did not show any other apparent clinical symptoms, such as fever, inappetence, or lethargy.
Figure 1.
Dengue hemorrhage in rhesus monkeys. Rhesus monkeys were intravenously infected with dengue virus as described in “Nonhuman primates, virus, and cells.” Hemorrhagic manifestations were captured with digital camera on days 3 (RM2), 4 (RM4), and 5 (RM3) after infection. Different severity of hemorrhage, ranging from petechiae to severe coagulopathy, was seen. A classic clinical hemorrhage was observed in infected animal RM4. The top and bottom panels indicate that the images of the skin hemorrhage were captured from different parts of the body within the same animal.
The laboratory evaluations included blood chemistries, measurements of proteins involved in the coagulation system, and complete blood counts. A modest increase in the plasma levels of the liver enzymes aspartate aminotransferase (or serum glutamic-oxaloacetic transaminase) and alanine aminotransferase (or serum glutamate pyruvate transaminase), or the myocardial infarction indicator enzyme creatine phosphokinases was noted in samples obtained on day 7 after infection. Plasma glucose levels also experienced an increase by day 7 after infection, whereas phosphorus showed a late decline by day 14 (Table 2).
Table 2.
Blood chemistry
| RM1 |
RM2 |
RM3 |
Reference range* | |||||
|---|---|---|---|---|---|---|---|---|
| Day 1 | Day 0 | Day 7 | Day 14 | Day 0 | Day 7 | Day 14 | ||
| Glucose, mg/dL | 74 | 65 | 99 | 102 | 77 | 159 | 127 | 99 ± 34.9 |
| Protein, g/dL | 7.2 | 6.8 | 6.4 | 6.3 | 7.1 | 6.6 | 6.6 | 7.9 ± 0.6 |
| Serum glutamate pyruvate transaminase, U/L | 39 | 39 | 114 | 51 | 35 | 66 | 72 | 36.2 ± 25.6 |
| Serum glutamic-oxaloacetic transaminase, U/L | 32 | 32 | 43 | 27 | 36 | 68 | 62 | 25.2 ± 10.4 |
| Phosphorus, g/dL | 4.3 | 4.8 | 4 | 2.7 | 3.6 | 3.1 | 2.7 | 5 ± 1.4 |
| Creatine phosphokinases, U/L | 386 | 410 | 3768 | 276 | 144 | 1311 | 651 | 277 ± 303 |
Reference ranges are based on values previously published by Matsuzawa et al.31
Coagulation parameters are summarized in Table 3. The data from these studies revealed that, although there was a marked increase in the plasma values of D-dimer noted in samples obtained on day 7 after infection, AT, thrombin-antithrombin, and protein S, showed marked elevations starting on day 1 after infection. In contrast, there did not appear to be any detectable change from baseline values in the levels of soluble fibrin monomers, protein C, prothrombin, and activated partial thromboplastin time in the samples examined from these monkeys (Table 3). Results of the evaluations of blood parameters are summarized in Table 4. As seen, although there was a modest decrease in platelet count and a noticeable decrease in total white blood cell count (WBC) during the first week of infection, values for both of these parameters remained within the normal ranges and returned to preinfection levels during the second week after infection. In addition, there appeared to be a consistent reduction of hematocrit values and a slight decrease in the levels of hemoglobin on all samples collected after infection. In contrast, there was no detectable change in the values for total red blood cell count in these same samples.
Table 3.
Coagulation parameters
| RM1 |
RM2 |
RM3 |
RM7 | RM8 | Reference range* | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day 0 | Day 1 | Day 5 | Day 7 | Day 0 | Day 1 | Day 5 | Day 10 | Day 0 | Day 5 | Day 10 | Day 14 | ||||
| Prothrombin, seconds | — | 9.9 | 8.9 | 9.7 | — | 10.1 | 9.1 | 8.8 | 10.1 | 9.6 | 9.2 | 9.3 | 9.7 | 10.4 | 10.7 ± 4.5 |
| Activated partial thromboplastin time, seconds | 45.6 | 46.5 | 33.7 | 33.6 | — | 40.2 | 32.5 | 37.4 | 59.0 | 29.6 | 42.0 | 44.5 | 48.5 | 34.6 | 25 ± 20 |
| D-dimer, ng/mL | — | < 150 | 486 | 1102 | < 150 | 862 | 1170 | 1131 | — | 586 | 725 | 882 | < 150 | < 150 | < 260 |
| Antithrombin III, percentage | — | 134 | 174 | 128 | 120 | 138 | 124 | 138 | — | 140 | 138 | 137 | 125 | 113 | 82-133 |
| Soluble fibrin monomers, mg/dL | — | < 7 | < 7 | < 7 | — | 40 | < 7 | < 7 | < 7 | < 7 | < 7 | < 7 | < 7 | < 7 | < 10 |
| Thombin-antithrombin complexes, μg/mL | 19.0 | 7.2 | > 60 | 16.8 | — | > 60 | > 60 | > 60 | 14.8 | > 60 | 11.6 | 53.0 | 7.0 | 7.6 | 4-33 |
| Protein C, percentage | 301 | < 10 | 292 | 276 | 151 | 221 | > 301 | > 301 | 299 | 269 | > 301 | 290 | 140 | 134 | 76-208 |
| Protein S, percentage | 83 | 166 | 151 | 127 | 86 | 94 | 164 | 175 | 149 | 123 | 101 | 114 | 47 | 48 | 62-153 |
— indicates not applicable.
Reference ranges are based upon those reported by Matsuzawa et al.31
Table 4.
Laboratory evaluations of blood parameters
| Day after infection | Hemoglobin, g/dL | Hematocrit, percentage | White blood cells/μL | Red blood cells × 106/μL | Platelets × 1000/μL |
|---|---|---|---|---|---|
| 0 | 13.90 ± 1.22 | 43.57 ± 4.49 | 6500 ± 1833 | 5.90 ± 0.50 | 386 ± 89 |
| 1 | 12.98 ± 1.13 | 39.88 ± 3.72 | 5566 ± 1268 | 5.47 ± 0.48 | 356 ± 138 |
| 3 | 12.98 ± 1.44 | 39.74 ± 4.92 | 4622 ± 1692 | 5.47 ± 0.60 | 320 ± 112 |
| 5 | 11.80 ± 0.67 | 36.70 ± 2.63 | 4898 ± 2124 | 5.03 ± 0.38 | 375 ± 85 |
| 7 | 11.46 ± 0.53 | 35.50 ± 2.20 | 4436 ± 1050 | 4.88 ± 0.37 | 411 ± 71 |
| 10 | 11.90 ± 0.42 | 37.20 ± 1.84 | 6034 ± 2007 | 5.06 ± 0.36 | 389 ± 71 |
| 14 | 11.96 ± 1.17 | 37.14 ± 4.13 | 7584 ± 3100 | 5.04 ± 0.47 | 399 ± 56 |
| Reference range | 10.5-12.5 | 35.4-41.4 | 4200-9200 | 5.55-6.63 | 195-339 |
Viremia is one of the major clinical manifestations of dengue virus infection. The dengue viral RNA in the plasma of infected monkeys was quantified using real-time RT-PCR. The monkeys were infected in 2 separate studies with slightly differing monitoring schedules. In the initial study, which included 3 monkeys (Figure 2A), blood specimens for viral load determination were collected before and then on alternate days after infection. Plasma viral loads rose to 105 copies/mL by day 1 after infection and then reached a peak at approximately 106 copies/mL on day 3 followed by a gradual decline with values dipping below the detectable level by day 14 after infection. To derive an even more detailed view of the kinetics of virus replication, daily instead of alternate-day blood specimens were collected from the second series of animals. The trend of viral RNA kinetics appeared to be similar to that noted for samples from the first study, except that a transient but consistent 1 log drop in the level of plasma viral RNA was noted in samples collected on day 2 after infection from their day 1 values (Figure 2B). The viral loads did, however, peak by day 3 to 4 in all animals, and the viremia was completely controlled by 2 weeks after infection. The viral titers were also evaluated using an focus forming unit (FFU) assay (supplemental Figure 2), which showed that the level of viremia peaked on day 3 after infection with a gradual decline to undetectable levels on day 10 after infection. The lower FFU titer compared with that noted by quantitative RT-PCR assays was expected because of differences in the sensitivity of the 2 assays.
Figure 2.
Viral load in plasma. Blood was drawn at the indicated days, RNA was isolated from plasma, and purified viral RNA was quantified by real-time RT-PCR in specimens collected at alternate day (A) and daily (B) as described in “Quantitation of viral load with real-time RT-PCR.” The peak of dengue viremia in infected RM was from 3 to 7 days after infection. P.I. indicates postinfection.
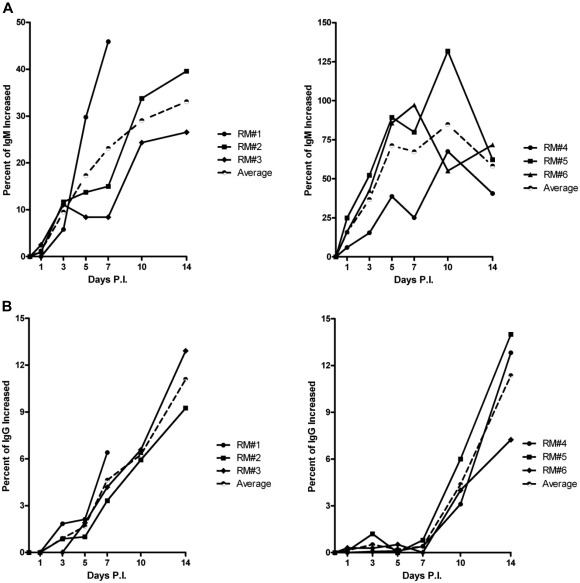
Serum IgM and IgG specific for dengue viral antigens were measured by ELISA. As expected, a typical profile of dengue virus specific IgM and IgG antibodies was noted in these infected monkeys (Figure 3A and B, respectively).
Figure 3.
Typical primary IgM and IgG antibody responses. Presence of dengue specific antibodies in the sera was assayed by ELISA as described in “Methods.” Variations of IgM response in individual RM were observed. But in general, a typical quick and robust response of IgM antibody (A) and a delayed response of IgG antibody (B) were registered. P.I. indicates postinfection.
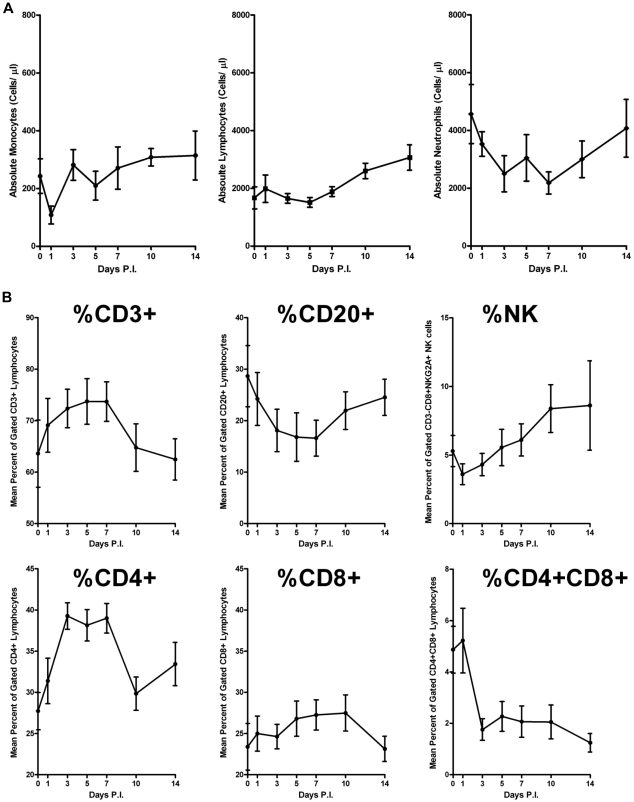
Leukocyte subpopulation in dengue hemorrhagic monkeys
Subpopulation of leukocytes.
A transient decrease of the WBC was observed as early as day 1 with a nadir on day 7 and then returning to normal levels by day 10 as determined by values of complete blood count (Table 4). These changes, however, were within the normal reference range for RMs. The analysis of the leukocyte subsets based on absolute counts showed that a decrease in the absolute number of neutrophils most probably accounted for WBC decrease. There did not appear to be any detectable change in the absolute number of monocytes during the acute infection period (Figure 4, monocytes) and a modest increase was noted in the absolute number of lymphocytes toward the end of the acute infection period (Figure 4). The transient neutropenia (Figure 4) noted in samples from the dengue virus–infected monkeys is similar to those documented to occur during natural infection in dengue patients.
Figure 4.
Profiling of leukocyte subpopulation. Cell surface markers conjugated with proper fluorochrome, which can differentiate the leukocyte subpopulation, were used to stain the fresh-drawn blood and subjected to FACS as described in “FACS analysis and immunohistochemistry.” (A) Absolute counts of each leukocyte subpopulation with SE bar from each animal were presented. A noticeable reduction of monocytes on day 1 after infection was observed, and thereafter a rebounded pattern to normal level was registered. A slight fluctuation with a trend of gradual increase in lymphocytes during acute infection was seen. A consistent and gradual reduction of neutrophils was documented during the acute period, which returned to uninfected level 14 days after infection. (B) Percentage of lymphocyte subpopulation with SE bar from each animal was presented. P.I. indicates postinfection.
Subpopulation of lymphocytes.
Because logistic issues make it difficult to ascertain the kinetic effects of dengue virus infection on changes in lymphoid cell subsets during the acute viremia period in humans, the experimentally infected NHP model provides a valuable tool to begin to address this issue. Flow cytometric analysis of sequential peripheral blood mononuclear cell samples from the experimentally dengue virus–infected RMs before and after acute infection was therefore performed in detail. The lymphoid cells were identified as those that expressed high levels of CD45 accompanied by low side scatter (supplemental Figure 3).
There were 3 basic observations that highlight the changes consistently observed in each of the experimentally dengue virus–infected RMs. Thus, although there was no detectable difference in the total number of lymphoid cells during the first week after infection (Figure 4A), there appeared to be an increase (P < .005) in the frequency of T cells (Figure 4B) with a concomitant decrease in the frequency of total B cells (Figure 4B; P < .001). Of interest also was the observation of a decrease in the frequency of NK cells on day 1 after infection (Figure 4B) followed by a marked sustained increase thereafter. These changes were also apparent when the values for each of these subsets were calculated as absolute numbers (data not shown). The values for T cells, B cells, and NK cells each returned to baseline values by 14 days after infection (Figure 4B). Further analysis of changes in the absolute number of T-cell subsets revealed that the increase in total T cells was secondary predominantly to an increase in the CD4+ T-cell subset with only a modest increase in the absolute number of CD8+ T cells and a decrease in CD4/CD8 double-positive subsets (DP, Figure 4B). This rapid decrease in DP cells was seen consistently in each of the monkeys, and it is not clear whether this is a signature for dengue virus infection uniquely seen in NHPs or is also potentially induced in dengue-infected patients after acute infection.
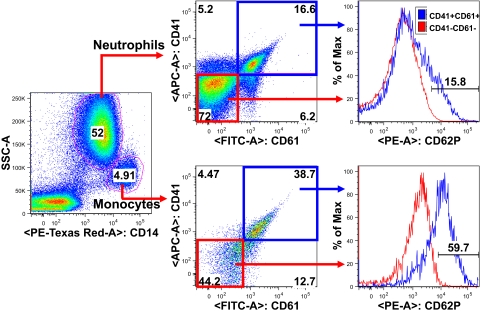
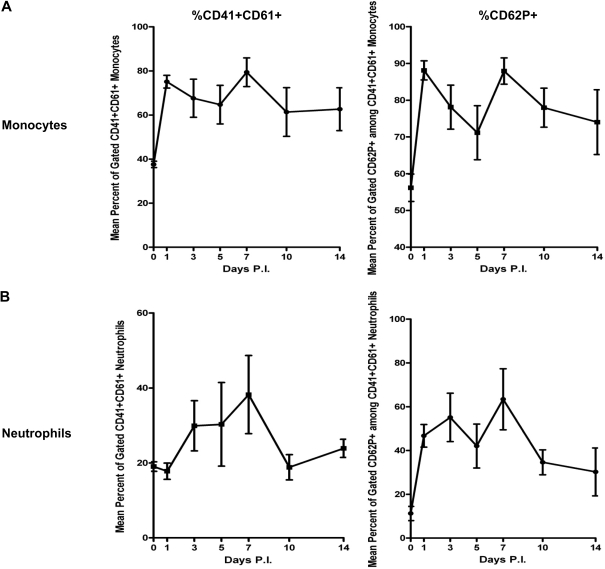
Platelet-leukocyte aggregation.
Thrombocytopenia, although often subclinical, is one of the clinical hallmarks in dengue virus–infected patients, which may contribute to the coagulopathies observed in our animals (Figure 1). The etiology of this phenomenon remains ill defined. One explanation for this observation is that the decrease is primarily the result of platelet-leukocyte aggregation, which has been documented in several physiologic and pathologic states32–34 and has been implicated to contribute to inflammatory processes.35 Flow cytometric analysis using platelet-specific monoclonal antibodies was used to investigate the formation of platelet-leukocyte aggregation during the acute dengue virus infection. The gating strategy of citrate whole blood samples used is illustrated in Figure 5. Briefly, the appropriate cocktail of various fluorochrome-labeled monoclonal antibodies was added to an aliquot of whole blood. Antibodies against the platelet-specific surface markers CD41 and CD61 in addition to markers that identify unique lymphoid cell subsets were used in efforts to determine the identity of lymphoid cell subsets that demonstrated platelet adhesion. The platelet-activated surface glycoprotein p-selectin (CD62p) was used as a marker of platelet aggregation. As shown in Figure 6A, a significant amount of platelet aggregation was noted with monocytes as previously noted on peripheral blood mononuclear cell samples from human patients during acute dengue virus infection.36 Platelet-neutrophil aggregates were also detected, albeit at lower frequencies (Figure 6B). Interestingly, platelet-leukocyte aggregates showed 2 consistent separate peaks after infection (day 1-3 and day 7 after infection), for reasons that remain to be elucidated. The lower percentage of the platelet-neutrophil aggregates compared with that of platelet-monocyte aggregates may be a reflection of higher numbers of neutrophils circulating in the blood; thus, in absolute numbers, neutrophil-platelet aggregates markedly surpass the numbers of monocyte-platelet aggregates.
Figure 5.
Strategy to profile the aggregation of platelets with neutrophils or monocytes. Whole blood flow cytometry was performed after samples were stained with specific cell surface markers conjugated with proper fluorochrome as described in “FACS analysis and immunohistochemistry.” The strategy to gate the specific platelet-leukocyte aggregation was described. The first step is to differentiate neutrophils from monocytes with CD14 surface marker, which then further identified with makers for platelets, respectively.
Figure 6.
Profiles of platelet-monocyte or neutrophil-leukocyte aggregation. Kinetics of platelet-leukocyte aggregation were presented as percentage of the gated event. A similar pattern of platelet aggregation with monocytes (A) or neutrophils (B) was observed. P.I. indicates postinfection. Error bars indicate 1 SD.
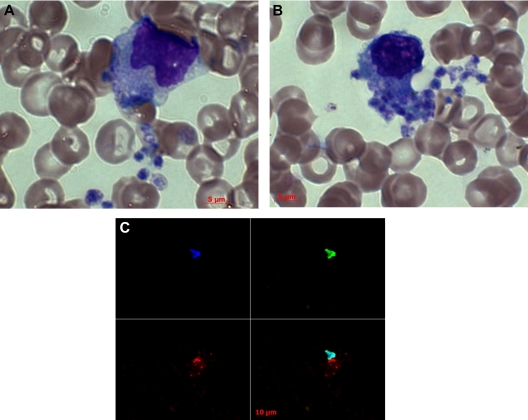
Blood film smears performed in parallel confirmed the occurrence of platelet-leukocyte aggregates (Figure 7; supplemental Figure 4). Platelet-monocyte aggregates were observed on blood smears obtained from monkeys on day 8 and day 9 after infection (Figure 7A and B, respectively). Immunofluorescence staining with dengue-specific antibody (clone 3H5) also revealed that some of these platelets were positive for dengue antigen (Figure 7C). These results are consistent with previous reports that have documented the presence of dengue antigen-positive leukocytes (or monocytes) in samples from patients examined toward the end of the acute infection period coincident with the disappearance of virus from the plasma.37 It is reasonable to assume that the presence of dengue viral antigens within monocytes in samples obtained toward the end of the acute infection period may be secondary to the process of phagocytosis. Interestingly, a recent report also suggests a prominent role of monocytes and/or macrophages in the control of dengue virus in infected mice.38 However, the contribution of platelet-leukocyte aggregation in promoting the phagocytic activity of monocytes requires further study.
Figure 7.
Engulfment of platelets by monocytes/macrophages. Blood smears were prepared from dengue virus–infected rhesus monkeys and Wright Giemsa and immunofluorescence stainings were performed. Images were acquired on a Zeiss AxioImager A1 epifluorescence microscope with an AxioCam MRC5 camera. Images were captured with a Zeiss 100×/1.3 Plan Neofluar oil objective lens and then processed with AxioVision Release 4.5 software. (A-B) Wright Giemsa staining revealed that tangled platelets were engulfed by monocytes. (C) Immunofluorescence staining revealed that some of these platelets were positive for dengue viral antigen (3H5, red). Nuclear was stained with DAPI (blue) and SYTOX Green.
In addition, attempts to identify the phenotype of the cells that harbor dengue antigen were performed (supplemental Figure 4A). Dengue antigen appeared associated with a cell that expressed a cell surface marker normally expressed by platelets. These dengue antigen-positive “platelets” were localized within or on the membrane of a cell with an unknown phenotype, although probably belonging either to the neutrophil or monocyte lineages as seen by Wright Giemsa staining. However, the true identity of the phenotype of these cells remains to be verified.
Discussion
NHPs have been used to investigate several aspects of dengue virus infection. These studies have included those involved with the effect of natural and experimental infection, studies of the immune response of animals infected with dengue viruses, and the evaluation of several candidate dengue viral vaccine formulations.15–19,39–42 The generation of dengue virus–specific antibody and the kinetics of dengue viremia in these monkeys have been shown to be essentially similar to that seen in human dengue virus infection.19 The dengue virus–infected NHPs have therefore been viewed as an acceptable animal model to study the compendium of virologic and immunologic aspects of experimental dengue virus infection. The only major exception to the use of the NHP model has been the failure of the dengue virus–infected animals to develop any detectable signs of disease, including manifestations of DHF and DSS, which is characteristic of a defined frequency of human dengue virus infection.40,43–45
Using a high-dose intravenous route, we were surprised to observe that all 3 monkeys during the first series of studies developed visible signs of cutaneous hemorrhage, recapitulating one of the clinical manifestations characteristic of dengue virus infection of humans. The age-matched RM that was inoculated with mock cell culture supernatant fluid from the same cell line used for producing the dengue virus stock used for the present studies failed to show any detectable signs of cutaneous hemorrhage. It is important to note that only a single monkey was used as a control for this first set of studies. However, within the same context, it is also important to note that the subcutaneous dengue hemorrhage seen during the first set of studies was also noted in the second set of rhesus monkeys using the same dose and route of IV infection. Coagulopathy was manifest by extensive subcutaneous bleeding, petechiae, and a marked delay in blood clotting time in venous blood being collected during this time period. These initial hemorrhagic manifestations were similar to those of dengue patients and appeared starting on days 3 to 5 after infection. Although petechiae could be found in several parts of the body, in general, the presence of petechiae was observed initially on the rear thigh, and sequentially around the abdomen, shoulder, and chest as a function of time. However, these petechiae were similar in each of these locations and faded away over time, which is somewhat similar to human dengue virus infection. In addition, on pressing, the red spot of the petechiae did not disappear, branch, or fade away, which is typical of dengue petechiae in dengue patients. Petechiae are the most common clinical manifestations in dengue patients in dengue endemic countries, such as Thailand,46 and can occur on any part of the body in dengue patients and can worsen on trauma, such as a bump with an object, a blood draw, or tourniquet test. Although these coagulopathies were noted in each of the 6 dengue-infected rhesus monkeys, the animals fully recovered by approximately 14 days after infection and cleared their symptoms shortly thereafter.
Although epidemiologic data suggest that DHF/DSS occurs predominantly after secondary infection with a heterologous dengue serotype, numerous reports have also documented DHF after primary dengue virus infection.3–6 Such primary infection-induced DHF/DSS has been documented in dengue naive travelers who visit dengue endemic regions,7–9 suggesting that DHF/DSS may be primarily linked to permissiveness of viral replication and the levels of viral load, which tend to be magnified during secondary exposure of humans to a different serotype reasoned to be the result of a phenomenon termed antibody mediated enhancement.47 Of note, the viremia detected in our monkeys, although high, was still approximately 1 to 2 log below the viremia noted in patients with DHF/DSS,10 which may account for the relatively benign overall disease course in the monkeys. Perhaps a threshold viral load is required to induce fulminant DHF/DSS, whereas the lower viral load in our monkeys is sufficient to induce mild hemorrhage but not high enough to induce the more severe form of dengue DHF/DSS. Future manipulations of the model are expected to address the link between viremia and disease in vivo. Thus, this nonhuman primate model for dengue virus infection may not only provide a valuable tool for the detailed study of the various pathophysiologic effects of dengue virus infection but will also provide a comprehensive analysis of host-virus interactions, with the potential to lead to the identification of the cellular and molecular mechanisms that lead to DHF/DSS and the lineage of cells that serve as the primary target of infection and virus replication. In addition, such a model also provides an important model for the testing and evaluation of potential dengue virus vaccines, specifically those that have the added benefit of protecting patients from the development of DHF/DSS.
Although alterations of blood immune cell subsets, including a transient CD4/CD8 ratio inversion, in dengue patients have been noted,36,48,49 we did not find such a change in our dengue-infected animals. The reason for the difference might be the result of decreased disease severity that we observed in our animals. In addition, an increase in CD19+ B cells was also observed in human dengue virus infection.50 However, we did not observe any increase in B cells when using CD20 as a B-cell marker. It is possible that it is the result of differences in the type of infection because most human patients who have been studied are the result of secondary dengue virus infection, whereas our animals were studied during primary infection. The secondary infection in humans might induce a rapid expansion of memory B cells that are specific for dengue virus and thus result in an increase in CD20+ B cells.
In our sequential and systematic phenotypic analyses, we frequently observed platelet-leukocyte aggregation, in particular in association with monocytes and, to some extent, with neutrophils. The flow cytometry–based observation of platelet-monocyte aggregation was further strengthened by immunofluorescence assays, in which monocytes appeared to engulf platelets containing dengue antigen (Figure 7; supplemental Figure 4). Attempting to identify the cell lineage that was positive for intracellular expression of dengue antigen by FACS, immunofluorescence assay (IFA), or immunohistochemistry with proper isotype antibody control was inconclusive, partly because of high fluorescence background. In addition, alteration of dengue antigens or epitopes engulfed by the phagocytic cells may result in the failure for the antibody to react. Thus, there is a need for a suitable dengue antigen staining method for the detection of the viral antigen by standard flow cytometry and IFA or immunohistochemistry. This may partially explain why even up to date, the identity of the cell lineage(s) that harbor dengue antigens in the circulating blood of patients is still an enigma. Nevertheless, the combination of single staining and Wright Giemsa staining supports the results noted by FACS analysis.
Interestingly, the importance of monocytes/macrophages in the control of dengue virus infection has been recently emphasized.38 Because dengue is a disease of timing, studies reported so far have involved specimens collected from dengue patients primarily collected after the onset of clinical manifestations. Although there is a considerable amount of variability in the kinetics of the various pathologic manifestations of dengue virus infection among persons, it is probable that the studies reported involved samples representing the peak of dengue viremia. This may partially explain why Durbin et al36 observed quite a few immune cells with a variety of cell surface markers that were positive for dengue viral antigens PrM or NS3. Thus, data collected and analyzed from sequential and systematic specimens in a suitable dengue animal model may provide a more objective analysis of the early events during acute dengue virus infection.
One of the major clinical and pathologic features that differentiate DHF from DF is plasma leakage, which is reasoned to be a consequence of increased vascular permeability.51 Disseminated intravascular coagulation (DIC) is not only a very prominent feature that occurs in patients with DSS but DIC has also been noted in some cases of DHF.51 Obviously, an imbalance or dysregulation between the prothombotic proteins and the natural anticoagulant pathway(s) may contribute to the tendency to develop hemorrhage in select patients after dengue infection. This view is supported by the data of aberrant levels of several plasma coagulation factors in DHF patients resulting from either intravascular consumption or impaired synthesis by the liver.52,53 The precise mechanisms involved in the induction of hemorrhage in DHF patients, however, are thought to be multiple. It is of interest to note that, in the studies reported herein, no detectable changes were noted in the prothrombin and partial thromboplastin time levels, whereas levels of protein C appeared to fluctuate but did not show a distinct pattern of change. However, distinct elevations were noted in the levels of D-dimer, an accepted marker for DIC,54 as well as those of AT, thombin-antithrombin, and protein S. In addition, compared with human DHF/DSS, only mild levels of thrombocytopenia were noted in the dengue virus–infected rhesus monkeys in the present study. One possible explanation for this discrepancy is that the changes in the aforementioned coagulation proteins in conjunction with the other changes are more typical of liver function perturbations rather than procoagulant DIC. The other could be because the peripheral blood of RMs as a species consists of 3 or 4 times more platelets than humans. Thus, a 10% to 20% drop in platelet count may not be noted as being significant in dengue virus–infected monkeys but nonetheless significant in terms of absolute numbers. Furthermore, the kinetics by which these changes occur is an important issue to keep in mind because the clinical changes seen in human dengue virus illness are notably a function of time after infection. Thus, to accurately define the mechanisms that lead to DHF with specimens collected at, during, or after the clinical symptoms develop may not be an easy task to achieve. Consequently, descriptive reports on the coagulation parameters are somewhat inconsistent.55–59 The NHP model of dengue virus infection, in which cutaneous hemorrhage is consistently observed, may perhaps, for the first time, provide a valuable model for the investigation of the bleeding mechanisms that are a cardinal feature of DHF in patients.
Acknowledgments
The authors thank the veterinary and research staff of the Yerkes National Primate Center at Emory for technical assistance, and Dr Tristram Parslow and Dr. Shiyoung Li, Department of Pathology and Laboratory Medicine, Emory University School for Medicine, for their helpful and knowledgeable suggestions and discussions to the manuscript.
This work was supported in part by the U19 Pilot Project Funds (RFA-AI-02-042), National Institutes of Health/SERCEB, Emory URC grants, and the p51 support to the Yerkes National Primate Research Center DRR000165.
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: N.O. designed and performed the FACS experiments and analyses; S.N. discussed the experimental strategy and performed FACS experiments and analyses; H.-M.H. performed the immunohistochemistry staining, real-time PCR, and ELISA; A.D. discussed the experimental strategy, performed the coagulation parameter assays, and edited the manuscript; F.V. discussed the experimental strategy, directed the monkey experiments, and edited the manuscript; A.A.A. discussed the experimental strategy, assisted in approval of IACUC protocol, and edited the manuscript; and G.C.P. designed, defined, and discussed the experimental strategy, wrote the IACUC protocol, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Guey Chuen Perng, Dental School Bldg, Rm 429, Emory Vaccine Center, 1462 Clifton Rd, Atlanta, GA 30322; e-mail: gperng@emory.edu.
References
- 1.Clark G, Gubler D, Rigau J. Dengue fever: CDC traveler's information on dengue fever. http://www.cdc.gov/travel/diseases/dengue.htm.
- 2.Guzman M, Kouri G, Diaz M, et al. Dengue, one of the great emerging health challenges of the 21st century. Expert Rev Vaccines. 2004;3(5):511–520. doi: 10.1586/14760584.3.5.511. [DOI] [PubMed] [Google Scholar]
- 3.Chang SF, Huang JH, Chen LK, et al. Retrospective serological study on sequential dengue virus serotypes 1 to 4 epidemics in Tainan City, Taiwan, 1994 to 2000. J Microbiol Immunol Infect. 2008;41(5):377–385. [PubMed] [Google Scholar]
- 4.Chan KP, Lau GK, Doraisingham S, Chan YC. Adult dengue deaths in Singapore. Clin Diagn Virol. 1995;4(3):213–222. doi: 10.1016/0928-0197(95)00004-r. [DOI] [PubMed] [Google Scholar]
- 5.Anantapreecha S, Chanama S, An A, et al. Serological and virological features of dengue fever and dengue haemorrhagic fever in Thailand from 1999 to 2002. Epidemiol Infect. 2005;133:503–507. doi: 10.1017/s0950268804003541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cordeiro MT, Silva AM, Brito CA, et al. Characterization of a dengue patient cohort in Recife, Brazil. Am J Trop Med Hyg. 2007;77(6):1128–1134. [PubMed] [Google Scholar]
- 7.Senanayake S. Dengue fever and dengue haemorrhagic fever: a diagnostic challenge. Aust Fam Physician. 2006;35(8):609–612. [PubMed] [Google Scholar]
- 8.Martyn-Simmons CL, Powell SE, Sudhanva M, Selim AG, Creamer D, Pearson IC. A florid skin rash in a returning traveller. Clin Exp Dermatol. 2007;32(6):779–781. doi: 10.1111/j.1365-2230.2007.02419.x. [DOI] [PubMed] [Google Scholar]
- 9.Wichmann O, Gascon J, Schunk M, et al. Severe dengue virus infection in travelers: risk factors and laboratory indicators. J Infect Dis. 2007;195(8):1089–1096. doi: 10.1086/512680. [DOI] [PubMed] [Google Scholar]
- 10.Vaughn DW, Green S, Kalayanarooj S, et al. Dengue viremia titer, antibody response pattern, and virus serotype correlate with disease severity. J Infect Dis. 2000;181(1):2–9. doi: 10.1086/315215. [DOI] [PubMed] [Google Scholar]
- 11.Bente DA, Rico-Hesse R. Models of dengue virus infection. Drug Discov Today Dis Models. 2006;3(1):97–103. doi: 10.1016/j.ddmod.2006.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yauch LE, Shresta S. Mouse models of dengue virus infection and disease. Antiviral Res. 2008;80(2):87–93. doi: 10.1016/j.antiviral.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sabin AB. Research on dengue during World War II. Am J Trop Med Hyg. 1952;1(1):30–50. doi: 10.4269/ajtmh.1952.1.30. [DOI] [PubMed] [Google Scholar]
- 14.Bhamarapravati N. Pathology of dengue infections. In: Gubler D, JaK G, editors. Dengue and Dengue Hemorrhagic Fever. Wallingford, United Kingdom: CAB International; 1997. pp. 115–132. [Google Scholar]
- 15.Rosen L. Experimental infection of New World monkeys with dengue and yellow fever viruses. Am J Trop Med Hyg. 1958;7(4):406–410. doi: 10.4269/ajtmh.1958.7.406. [DOI] [PubMed] [Google Scholar]
- 16.Simmons JS, St John JH, Reynolds FHK. Experimental studies of dengue. Philippine J Sci. 1931;44:1–252. [Google Scholar]
- 17.Whitehead RH, Chaicumpa V, Olson LC, Russell PK. Sequential dengue virus infections in the white-handed gibbon (Hylobates lar). Am J Trop Med Hyg. 1970;19(1):94–102. doi: 10.4269/ajtmh.1970.19.94. [DOI] [PubMed] [Google Scholar]
- 18.Halstead SB. In vivo enhancement of dengue virus infection in rhesus monkeys by passively transferred antibody. J Infect Dis. 1979;140(4):527–533. doi: 10.1093/infdis/140.4.527. [DOI] [PubMed] [Google Scholar]
- 19.Marchette NJ, Halstead SB. Immunopathogenesis of dengue infection in the rhesus monkey. Transplant Proc. 1974;6(2):197–201. [PubMed] [Google Scholar]
- 20.O'Rourke F. Observations on pool and capillary feeding in Aedes aegypti. Nature. 1956;177:1087–1088. [Google Scholar]
- 21.Ashburn PM, Craig CF. Experimental investigations regarding the etiology of dengue. J Infect Dis. 1907;4:440–475. doi: 10.1086/383418. [DOI] [PubMed] [Google Scholar]
- 22.Eckels KH, Harrison VR, Summers PL, Russell PK. Dengue-2 vaccine: preparation from a small-plaque virus clone. Infect Immun. 1980;27(1):175–180. doi: 10.1128/iai.27.1.175-180.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Institute of Laboratory Animal Research, Commission on Life Sciences, National Research Council. Guide for the Care and Use of Laboratory Animals. Washington, DC: The National Academic Press; 1996. [Google Scholar]
- 24.Klungthong C, Gibbons RV, Thaisomboonsuk B, et al. Dengue virus detection using whole blood for reverse transcriptase PCR and virus isolation. J Clin Microbiol. 2007;45(8):2480–2485. doi: 10.1128/JCM.00305-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Houng HH, Hritz D, Kanesa-thasan N. Quantitative detection of dengue 2 virus using fluorogenic RT-PCR based on 3′-noncoding sequence. J Virol Methods. 2000;86(1):1–11. doi: 10.1016/s0166-0934(99)00166-4. [DOI] [PubMed] [Google Scholar]
- 26.Lafont BA, Gloeckler L, D'Hautcourt JL, Gut JP, Aubertin AM. One-round determination of seven leukocyte subsets in rhesus macaque blood by flow cytometry. Cytometry. 2000;41(3):193–202. doi: 10.1002/1097-0320(20001101)41:3<193::aid-cyto6>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 27.Innis BL, Nisalak A, Nimmannitya S, et al. An enzyme-linked immunosorbent assay to characterize dengue infections where dengue and Japanese encephalitis co-circulate. Am J Trop Med Hyg. 1989;40(4):418–427. doi: 10.4269/ajtmh.1989.40.418. [DOI] [PubMed] [Google Scholar]
- 28.Waterman SH, Gubler DJ. Dengue fever. Clin Dermatol. 1989;7(1):117–122. doi: 10.1016/0738-081x(89)90034-5. [DOI] [PubMed] [Google Scholar]
- 29.Radakovic-Fijan S, Graninger W, Muller C, Honigsmann H, Tanew A. Dengue hemorrhagic fever in a British travel guide. J Am Acad Dermatol. 2002;46(3):430–433. doi: 10.1067/mjd.2002.111904. [DOI] [PubMed] [Google Scholar]
- 30.Pincus LB, Grossman ME, Fox LP. The exanthem of dengue fever: clinical features of two US tourists traveling abroad. J Am Acad Dermatol. 2008;58(2):308–316. doi: 10.1016/j.jaad.2007.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Matsuzawa T, Nomura M, Unno T. Clinical pathology reference ranges of laboratory animals: Working Group II, Nonclinical Safety Evaluation Subcommittee of the Japan Pharmaceutical Manufacturers Association. J Vet Med Sci. 1993;55(3):351–362. doi: 10.1292/jvms.55.351. [DOI] [PubMed] [Google Scholar]
- 32.Gawaz MP, Mujais SK, Schmidt B, Gurland HJ. Platelet-leukocyte aggregation during hemodialysis. Kidney Int. 1994;46(2):489–495. doi: 10.1038/ki.1994.299. [DOI] [PubMed] [Google Scholar]
- 33.Faint RW. Platelet-neutrophil interactions: their significance. Blood Rev. 1992;6(2):83–91. doi: 10.1016/0268-960x(92)90010-n. [DOI] [PubMed] [Google Scholar]
- 34.Rinder HM, Bonan JL, Rinder CS, Ault KA, Smith BR. Activated and unactivated platelet adhesion to monocytes and neutrophils. Blood. 1991;78(7):1760–1769. [PubMed] [Google Scholar]
- 35.Bazzoni G, Dejana E, Del Maschio A. Platelet-neutrophil interactions: possible relevance in the pathogenesis of thrombosis and inflammation. Haematologica. 1991;76(6):491–499. [PubMed] [Google Scholar]
- 36.Durbin AP, Vargas MJ, Wanionek K, et al. Phenotyping of peripheral blood mononuclear cells during acute dengue illness demonstrates infection and increased activation of monocytes in severe cases compared to classic dengue fever. Virology. 2008;376(2):429–435. doi: 10.1016/j.virol.2008.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marchette NJ, Halstead SB, Falkler WA, Jr, Stenhouse A, Nash D. Studies on the pathogenesis of dengue infection in monkeys: III. Sequential distribution of virus in primary and heterologous infections. J Infect Dis. 1973;128(1):23–30. doi: 10.1093/infdis/128.1.23. [DOI] [PubMed] [Google Scholar]
- 38.Fink K, Ng C, Nkenfou C, Vasudevan S, van Rooijen N, Schul W. Depletion of macrophages in mice results in higher dengue virus titers and highlights the role of macrophages for virus control. Eur J Immunol. 2009;39(10):2809–2821. doi: 10.1002/eji.200939389. [DOI] [PubMed] [Google Scholar]
- 39.Rudnick A, Marchette NJ, Garcia R. Possible jungle dengue: recent studies and hypotheses. Jpn J Med Sci Biol. 1967;20:69–74. [PubMed] [Google Scholar]
- 40.Guy B, Barban V, Mantel N, et al. Evaluation of interferences between dengue vaccine serotypes in a monkey model. Am J Trop Med Hyg. 2009;80(2):302–311. [PubMed] [Google Scholar]
- 41.Goncalvez AP, Engle RE, St Claire M, Purcell RH, Lai CJ. Monoclonal antibody-mediated enhancement of dengue virus infection in vitro and in vivo and strategies for prevention. Proc Natl Acad Sci U S A. 2007;104(22):9422–9427. doi: 10.1073/pnas.0703498104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McArthur JH, Durbin AP, Marron JA, et al. Phase I clinical evaluation of rDEN4Delta30-200,201: a live attenuated dengue 4 vaccine candidate designed for decreased hepatotoxicity. Am J Trop Med Hyg. 2008;79(5):678–684. [PMC free article] [PubMed] [Google Scholar]
- 43.Velzing J, Groen J, Drouet MT, et al. Induction of protective immunity against Dengue virus type 2: comparison of candidate live attenuated and recombinant vaccines. Vaccine. 1999;17(11):1312–1320. doi: 10.1016/s0264-410x(98)00393-4. [DOI] [PubMed] [Google Scholar]
- 44.Guirakhoo F, Pugachev K, Arroyo J, et al. Viremia and immunogenicity in nonhuman primates of a tetravalent yellow fever-dengue chimeric vaccine: genetic reconstructions, dose adjustment, and antibody responses against wild-type dengue virus isolates. Virology. 2002;298(1):146–159. doi: 10.1006/viro.2002.1462. [DOI] [PubMed] [Google Scholar]
- 45.Koraka P, Benton S, van Amerongen G, Stittelaar KJ, Osterhaus AD. Characterization of humoral and cellular immune responses in cynomolgus macaques upon primary and subsequent heterologous infections with dengue viruses. Microbes Infect. 2007;9(8):940–946. doi: 10.1016/j.micinf.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 46.Chuansumrit A, Tanfnaratchakit K. Pathophysiology and management of dengue hemorrhagic fever. Transfusion Alternatives Transfusion Med. 2006;8(1):3–11. [Google Scholar]
- 47.Halstead SB. Pathogenesis of dengue: challenges to molecular biology. Science. 1988;239(4839):476–481. doi: 10.1126/science.3277268. [DOI] [PubMed] [Google Scholar]
- 48.Green S, Pichyangkul S, Vaughn DW, et al. Early CD69 expression on peripheral blood lymphocytes from children with dengue hemorrhagic fever. J Infect Dis. 1999;180(5):1429–1435. doi: 10.1086/315072. [DOI] [PubMed] [Google Scholar]
- 49.Liu CC, Huang KJ, Lin YS, Yeh TM, Liu HS, Lei HY. Transient CD4/CD8 ratio inversion and aberrant immune activation during dengue virus infection. J Med Virol. 2002;68(2):241–252. doi: 10.1002/jmv.10198. [DOI] [PubMed] [Google Scholar]
- 50.Jampangern W, Vongthoung K, Jittmittraphap A, et al. Characterization of atypical lymphocytes and immunophenotypes of lymphocytes in patients with dengue virus infection. Asian Pac J Allergy Immunol. 2007;25(1):27–36. [PubMed] [Google Scholar]
- 51.Srichaikul T, Nimmannitya S. Haematology in dengue and dengue haemorrhagic fever. Baillieres Best Pract Res Clin Haematol. 2000;13(2):261–276. doi: 10.1053/beha.2000.0073. [DOI] [PubMed] [Google Scholar]
- 52.Mitrakul C. Bleeding problem in dengue haemorrhagic fever: platelets and coagulation changes. Southeast Asian J Trop Med Public Health. 1987;18(3):407–412. [PubMed] [Google Scholar]
- 53.Srichaikul T, Nimmanitaya S, Artchararit N, Siriasawakul T, Sungpeuk P. Fibrinogen metabolism and disseminated intravascular coagulation in dengue hemorrhagic fever. Am J Trop Med Hyg. 1977;26(3):525–532. doi: 10.4269/ajtmh.1977.26.525. [DOI] [PubMed] [Google Scholar]
- 54.Lippi G, Franchini M, Targher G, Favaloro EJ. Help me, Doctor! My D-dimer is raised. Ann Med. 2008;40(8):594–605. doi: 10.1080/07853890802161015. [DOI] [PubMed] [Google Scholar]
- 55.Sosothikul D, Seksarn P, Pongsewalak S, Thisyakorn U, Lusher J. Activation of endothelial cells, coagulation and fibrinolysis in children with Dengue virus infection. Thromb Haemost. 2007;97(4):627–634. [PubMed] [Google Scholar]
- 56.Jong JB, Pohan HT, Zulkarnain I, et al. The correlation between coagulation test and albumin with antithrombin III in Dengue hemorrhagic fever. Acta Med Indones. 2004;36(2):57–61. [PubMed] [Google Scholar]
- 57.Krishnamurti C, Kalayanarooj S, Cutting MA, et al. Mechanisms of hemorrhage in dengue without circulatory collapse. Am J Trop Med Hyg. 2001;65(6):840–847. doi: 10.4269/ajtmh.2001.65.840. [DOI] [PubMed] [Google Scholar]
- 58.van Gorp EC, Minnema MC, Suharti C, et al. Activation of coagulation factor XI, without detectable contact activation in dengue haemorrhagic fever. Br J Haematol. 2001;113(1):94–99. doi: 10.1046/j.1365-2141.2001.02710.x. [DOI] [PubMed] [Google Scholar]
- 59.Huang YH, Liu CC, Wang ST, et al. Activation of coagulation and fibrinolysis during dengue virus infection. J Med Virol. 2001;63(3):247–251. doi: 10.1002/1096-9071(200103)63:3<247::aid-jmv1008>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]