Abstract
Our goal was to analyze the results of a multicity program offering rapid HIV testing in a mobile unit in central locations. Between October 2006 and December 2007, 7138 persons were tested, providing a finger-prick blood sample and filling out a brief questionnaire while waiting for the results of the Determine® test. Seventy people were classified as reactive and 3 as indeterminate. Confirmatory test results were obtained for 83.6%. Of the 56 reactive persons contacted, 2 were confirmed as negative, giving a positive predictive value of 96.6%. Those tested were primarily men (60.6%), persons with university education (47.4%), and included a large percentage of immigrants (26.2%), especially from Latin America, and 37.3% were men who have sex with men (MSM). Forty-seven percent had ever been tested for HIV. Global HIV prevalence was 0.98% (confidence interval [CI]: 0.75–1.21), 1.59%, (CI: 1.21–1.97) in men and 0.19%, (CI: 0.02–0.35) in women. In the tree analysis the high prevalence node included Latin Americans with only primary studies (study level finished at least at the age of 12). Of the 64% HIV-positive tests in 2007 with available CD4 counts, 18.75% had CD4 counts under 350. Street-based mobile units offering rapid HIV testing in selected sites, may diagnose HIV at an earlier stage of infection than clinic-based sites, and have a low rate of false-positives.
Introduction
Spain is one of the European countries with the highest estimated number of HIV-infected people.1,2 Approximately 37.3% of those who were newly diagnosed between 2003 and 2007 had fewer than 200 CD4 lymphocytes at diagnosis, and 19% had between 200 and 350.3 In Spain HIV testing is offered free of charge in a wide range of places: primary care, specialty care health centers, and HIV/sexually transmitted infection (STI) centers of large cities; 4 of every 10 persons aged 18–49 years have ever been tested.4 Late diagnosis has a considerable impact on control of the epidemic because it increases the probability of transmission given that persons unaware of their HIV infection less often adopt protective measures with their partners and often have higher viral loads.5
In this context, reducing the number of HIV-positive persons who are not aware of their serologic status and reducing as much as possible the time between infection and diagnosis has become one of the priority prevention policies to reduce the incidence of new infections in many countries,6,7 including Spain.8 Offering rapid diagnostics tests, which ensures that the great majority of those who take the test will receive their results, is one of the innovations developed in recent years to achieve this objective.9,10 Most of these programs to date, however, have been restricted to different clinical settings, so that only those who attend such settings can benefit from these initiatives. Some programs have also been developed in places where population groups with a high risk of infection live or congregate.11 Many people may be dissuaded from accessing these services so as not to be identified with socially stigmatized groups, as the so-called prevention groups (injection drug users, men who have sex with men, or sex workers) may still be considered in many settings. However, few experiences with easily accessible rapid testing programs have been described. Moreover, most of the programs evaluated in the developed countries have been carried out in the United States.9
The objective of the present study was to analyze the results of a program offering rapid testing services without an appointment in a mobile unit in centrally located squares in Madrid and other cities in Spain, in places and at times of maximum traffic of all types of persons, especially young people.
Methods
The program was conducted during several months between October 2006 and December 2007 mainly in Madrid. On certain days it was also offered in three cities in the region of Valencia and in two cities in the Balearic Islands. In Madrid, a mobile unit (van) was located in a square in a commercial city center street frequented by young people and on the limits of Chueca, known to be the gay neighborhood in Madrid. In the cities in the region of Valencia and in the Balearic Islands, the van was also placed in busy central streets but with no proximity to any gay neighborhoods.
In a storefront desk next to the van, information was given in a brief precounseling session about the conditions for receiving the test (rapid result, confidential, no charge) as well its limitations (preliminary positive test results need confirmation). There was no active encouragement carried out by the staff at the testing site: those who decided to have the test entered the mobile testing unit, completed the precounseling session, signed an informed consent form, and gave a blood sample by finger-prick. They were also asked if, during the 20 minutes before the test results would be available, they would be willing to complete an anonymous questionnaire to which the test result would then be added. The 2007 questionnaire included only four epidemiologic variables (gender, age, birthplace, and previous receipt of test). Along with these, the 2006 questionnaire included four more variables (level of studies, source of income, sexual orientation, and previous HIV test).
HIV testing was performed with the rapid test (Determine HIV-1/2 ®, Inverness Medical, Waltham, MA). Those with a first positive or indeterminate test were informed that the result was not totally conclusive, and underwent a second rapid test. In the postcounseling session, those who had double positive or double indeterminate results were referred for a confirmatory test and medical follow-up in public centers where the test can be performed without previous appointment, or were advised to see their primary care physician. In Spain, the test can be performed in both places confidentially and free of charge. Subjects were also asked if they would provide a telephone number so that the confirmatory test result could be made available to the program.
Data analysis
A descriptive analysis was made of the variables collected, stratified by gender. Given the low prevalence found in women, all analyses of HIV prevalence according to different variables were restricted to men, calculating first the prevalence and then the 95% confidence intervals (CI). The multivariate analysis of the factors associated with infection was limited to 2006, the year when the study was conducted only in Madrid and a larger number of epidemiologic variables were available. Given the limited number of positive outcomes (18 HIV infections), these analysis were performed by classification and regression tree analysis (C&RT). This is a nonparametric statistical procedure that identifies mutually exclusive subgroups whose members share common characteristics that influence the dependent variable (HIV prevalence, in this case). The C&RT procedure examines all possible independent or splitting variables and selects the one that results in binary groups that are most highly differentiated with respect to the dependent variable, according to a predetermined splitting criterion (the Gini index, in our case). This method appears to have more affinity with the way clinicians make decisions.11,12 The procedure was performed with the SPSS module Answer Tree 2.0 (SPSS Inc., Chicago, IL).
Results
We present data on 7138 persons who agreed to be tested and who filled out the questionnaire, after excluding 2 reactive people who indicated in the postcounseling session that they already knew they were HIV positive. The proportion of missing values was 5.4% for gender, and did not exceed 10.4% for any of the other variables in women. However, in men this percentage was higher, reaching 17% for age (Table 1). All the missing values for the variables finally analyzed in the tree analysis were from persons who had a negative test result.
Table 1.
Attenders at a Mobile Unit for Rapid HIV Testing in the Streets of Several Spanish Cities in 2006–2007: General Characteristics of the Total Sample and HIV Prevalence in Men
| |
General characteristics by gender |
HIV prevalence in men |
|||||
|---|---|---|---|---|---|---|---|
| |
Women |
Men |
|
|
|
||
| n | % | n | % | p | % | 95% CI | |
| Autonomous Community (region) | <0.001 | ||||||
| Madrid | 2058 | 77.3 | 3450 | 84.4 | 1.54 | 1.13–1.95 | |
| C. Valenciana | 311 | 11.7 | 302 | 7.4 | 1.66 | 0.21–3.10 | |
| Balearic Islands | 293 | 11.0 | 337 | 8.2 | 2.08 | 0.55–3.61 | |
| Age | <0.001 | ||||||
| <30 | 1763 | 73.5 | 1913 | 56.6 | 1.36 | 0.84–1.88 | |
| ≥30 | 636 | 26.5 | 1465 | 43.4 | 2.53 | 1.72–3.33 | |
| Unknown | 263 | 711 | |||||
| Country of birth | 0.528 | ||||||
| Spain | 1845 | 73.1 | 2845 | 74.3 | 1.27 | 0.85–1.68 | |
| Latin America | 445 | 17.6 | 659 | 17.2 | 3.64 | 2.21–5.08 | |
| Others | 233 | 9.2 | 327 | 8.5 | 1.53 | 0.19–2.87 | |
| Unknown | 139 | 258 | |||||
| Level of studiesa | <0.001 | ||||||
| Primary | 52 | 6.6 | 130 | 11.1 | 3.85 | 0.52–7.17 | |
| Secondary | 305 | 38.7 | 546 | 46.4 | 1.65 | 0.58–2.72 | |
| University | 432 | 54.8 | 500 | 42.5 | 0.4 | 0.15–0.95 | |
| Unknown | 73 | 168 | |||||
| Source of Incomea | 0.407 | ||||||
| Work | 594 | 76.9 | 962 | 84.2 | 1.14 | 0.47–1.82 | |
| Others | 178 | 23.1 | 180 | 15.8 | 1.66 | 0.21–3.54 | |
| Unknown | 90 | 202 | |||||
| Sexual orientationa | <0.001 | ||||||
| Heterosexual | 706 | 89.8 | 729 | 62.7 | 0.82 | 0.17–1.48 | |
| Homo–bisexual | 80 | 10.2 | 434 | 37.3 | 2.76 | 1.22–4.31 | |
| Unknown | 76 | 181 | |||||
| Drug injectiona | 0.967 | ||||||
| No | 769 | 98.8 | 1131 | 98.9 | b | b | |
| Yes | 9 | 1.2 | 13 | 1.1 | b | b | |
| Unknown | 84 | 200 | |||||
| Previous HIV test | <0.001 | ||||||
| No | 1748 | 68.3 | 1961 | 51.3 | 0.19 | 0.34–1.09 | |
| Yes | 813 | 31.8 | 1865 | 48.8 | 2.03 | 1.40–2.68 | |
| Unknown | 101 | 263 | |||||
Variables collected only in Madrid during 2006.
Not calculated due to low prevalence of injection.
Seventy people were classified as reactive and 3 with an indeterminate test result. The result of the confirmatory test was known for 61 of these 73 persons (83.6%). Of the 58 contacted who had been classified as reactive, only 2 were later definitively diagnosed as negative, which represents a positive predictive value (PPV) of 96.6%; of the 3 persons with an indeterminate result, only 1 was finally classified as positive. The 12 persons with a reactive test who could not be located to notify of the result of the confirmatory test were considered to be positive in the analysis of the prevalence of HIV infection.
Those who asked to be tested were primarily men (60.6%), 51.6% younger than 30 years of age, 74.3% were born in Spain, 17.4% were born in Latin America, and 8.8% in other countries. Almost half had university studies (with a significantly larger percentage in women), 26.2% reported having had sex with someone of the same sex (a significantly larger percentage in men, reaching 37.3%), only 1.2% had ever injected drugs, and 41.7% had ever been tested (a significantly larger proportion of men than women; Table 1).
All subjects who gave a blood sample received their test results, although a few persons who did not pick up the result directly left a contact number and were notified by phone. The overall prevalence of infection in the 2 years of the study was 0.98% (CI: 0.75–1.21) and was eight times higher in men (1.59%, CI: 1.21–1.97) than in women (0.19%, CI: 0.02–0.35). Among men, the prevalence was significantly higher in those born in Latin America and those who had been tested previously; it was also higher (although not reaching statistical significance) in persons over 30 years of age, those with low educational level, those whose main source of income was not from paid work, and those who reported having sex with persons of the same sex.
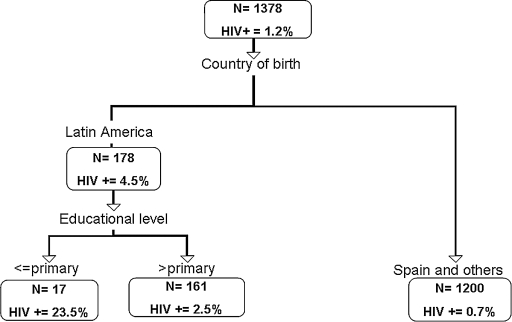
In the tree analysis three nodes emerged, which could be called high, medium, and low prevalence of HIV infection. The high prevalence node included Latin Americans with only primary studies; the medium prevalence node included Latin Americans with higher than primary studies, and the low prevalence node included Spanish or foreign-born persons other than Latin Americans (Fig. 1).
FIG. 1.
Classification tree analysis for binary outcome of HIV prevalence in men who accept rapid HIV testing, Madrid, 2006.
At least 83.6% of those considered reactive or indeterminate confirmed the result in health care centers where they began medical treatment. This percentage does not include those who could not be contacted a posteriori, although it is reasonable to suppose that some of them would have gone to other centers to confirm the result. CD4 data were self-reported by individuals and correspond to first CD4 analysis. The specific date was not registered. In 2007, CD4 counts were available for 64% of those diagnosed as reactive. Only 18.75% of these persons had fewer than 350 CD4 cells at the time of their first analysis. However, because the date of this analysis was not registered, the percentage of persons diagnosed in an advanced stage of infection is probably lower than 18.75% estimated.
Discussion
This study shows that the HIV testing method described was used by a large percentage of young men with high educational level and men who have sex with men (MSM). Likewise, it attracted a large percentage of immigrants. The highest HIV prevalence was found among those from Latin America with a low educational level. At least 4 of 5 persons with positive or indeterminate results received a confirmatory test result, and for these persons the positive predictive value of the test was 96.6%. Fewer than 1 of every 5 seropositive persons was diagnosed at an advanced stage of infection.
The overall prevalence (0.98%) was practically the same as that described in a study conducted in various U.S. cities between 2004 and 2006,13 and was higher than what has been found in some emergency departments.14 Although the Spanish program was not conducted in places specifically frequented by high-risk groups, the reality is that, in practice, over one third of attendees reported being MSM, perhaps due to the proximity of the Madrid testing site to the gay quarter; it may also be that information about the existence of the service was disseminated more easily among networks of this social group. Moreover, MSM made up 2 of every 3 cases of infection detected in men. The number of cases in MSM may actually have been higher, since the question referred to sexual orientation and not to sexual practice. The large proportion of immigrants, and especially the fact that those from Latin America with low educational level had the highest prevalence, suggests that these types of programs may be a highly acceptable strategy to capture these population groups. Despite the existence of free and anonymous diagnostic centers in these cities, it is very likely that immigrants—particularly those with low educational level—are less aware of them and do not really believe they can use these services in the same conditions as Spaniards, with no legal implications for those without legal residence in Spain.
The conservative estimate that more than 4 of 5 persons confirmed their results in a different health center can be considered very acceptable, given what other programs carried out in health centers have found.9 The proportion was probably higher in reality, since we considered that those who could not be contacted a posteriori had not confirmed their result. Finally, it should be noted that the percentage of those who were diagnosed at a relatively advanced stage of infection (<350 CD4) was three times lower than the 57.3% described for all cases diagnosed between 2003 and 2006 in the Spanish regions with a reporting system for new HIV diagnoses.3 This would indicate that the program resulted in an important benefit with regard to earlier diagnosis.
Although it could not be evaluated formally, the perception of the program staff was that the need for a finger-prick to extract blood, with no availability of less aggressive tests such as those based on saliva, was not an element that deterred anyone from being tested. On the contrary, the blood-based test showed an extremely high PPV in actual application; as a result only two persons received a presumptive diagnosis that could not later be confirmed, which is a far different situation from that recently described with saliva samples in the United States.14,15
Among the study limitations is the fact that the non-governmental organization (NGO) that runs the program was strongly action-oriented, thus the information collected included very few variables, which limits the breadth of the analysis. Moreover, the variables collected included a not inconsiderable proportion of unknowns, although this was largely limited to those who were HIV negative. In any event, partial data for 2008 (not shown) confirm the main findings reported herein.
It can be concluded that this type of program, although used primarily by low-risk groups who probably know very well how to access other types of diagnostic services (heterosexual Spaniards with a high educational level), is also useful in capturing other less favored populations with a higher risk of infection and in whom a larger number of cases is detected. By reducing late diagnoses by one third, with a very low rate of false-positives, the program also helps to ensure that most diagnoses are made at an earlier stage of infection as compared to currently existing diagnostic centers.
Acknowledgments
Data analysis and manuscript preparation was supported by the Fundación para Investigación y la Prevención del Sida en España (Fipse 24530/05) and by CIBERESP AI08_005. Madrid Positivo rapid HIV testing program was funded mainly by the Secretaría del Plan Nacional sobre el Sida, and a contribution by Gilead Sciences SL.
The Madrid Rapid HIV Testing Group: Carmen Rodríguez, Jorge del Romero, M Isabel Mencía, José Pulido, Gemma Molist, and María José Bravo.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Castilla J. de la Fuente L. [Trends in the number of human immunodeficiency virus infected persons and AIDS cases in Spain: 1980–1998] Med Clin (Barc) 2000;115:85–89. doi: 10.1016/s0025-7753(00)71473-4. [DOI] [PubMed] [Google Scholar]
- 2.Merson MH. O'Malley J. Serwadda D. Apisuk C. The history and challenge of HIV prevention. Lancet. 2008;372:475–488. doi: 10.1016/S0140-6736(08)60884-3. [DOI] [PubMed] [Google Scholar]
- 3.Centro Nacional de Epidemiología.Vigilancia epidemiológica del VIH en España. Valoración de los nuevos diagnósticos de VIH en España a partir de los sistemas de notificación de casos de las CCAA. Periodo 2003–2007 [HIV Epidemiologic surveillance in Spain.Assessment of new HIV diagnoses in Spain based on the autonomic case notification system. 2003–2007] www.isciii.es/htdocs/pdf/nuevos_diagnosticos_ccaa.pdf. [Oct;2008 ]. www.isciii.es/htdocs/pdf/nuevos_diagnosticos_ccaa.pdf
- 4.Instituto Nacional de Estadística and Ministerio de Sanidad y Consumo.Encuesta de Salud y Hábitos Sexuales 2003, Informe general [National Health and Sexual Behaviour Survey 2003, General Report]. Madrid: Instituto Nacional de Estadística. 2006. www.ine.es/prodyser/pubweb/saludyhs03/saludyhs03.htm. [Sep 12;2008 ]. www.ine.es/prodyser/pubweb/saludyhs03/saludyhs03.htm
- 5.Marks G. Crepaz N. Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20:1447–1450. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- 6.Branson BM. Handsfield HH. Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55:1–17. [PubMed] [Google Scholar]
- 7.British HIV Association, British Association of Sexual Health, HIV British Infection Society. London: British HIV Association; 2008. [Nov 3;2008 ]. UK National Guidelines for HIV Testing 2008. [Google Scholar]
- 8.Secretaría del Plan Nacional sobre el Sida.Plan Multisectorial frente al VIH y el sida. Madrid: Ministerio de Sanidad y Consumo; 2008. [Apr 7;2008 ]. España 2008–2012 [Multisectorial Plan against HIV and AIDS. Spain 2008–2012] [Google Scholar]
- 9.Roberts KJ. Grusky O. Swanson AN. Outcomes of blood and oral fluid rapid HIV testing: a literature review, 2000–2006. AIDS Patient Care STDs. 2007;21:621–637. doi: 10.1089/apc.2006.0196. [DOI] [PubMed] [Google Scholar]
- 10.Guenter D. Greer J. Barbara A. Robinson G. Roberts J. Browne G. Rapid point-of-care HIV testing in community-based anonymous testing program: A valuable alternative to conventional testing. AIDS Patient Care STDs. 2008;22:195–204. doi: 10.1089/apc.2007.0137. [DOI] [PubMed] [Google Scholar]
- 11.Lemon SC. Roy J. Clark MA. Friedmann PD. Rakowski W. Classification and regression tree analysis in public health: methodological review and comparison with logistic regression. Ann Behav Med. 2003;26:172–181. doi: 10.1207/S15324796ABM2603_02. [DOI] [PubMed] [Google Scholar]
- 12.Marshall RJ. The use of classification and regression trees in clinical epidemiology. J Clin Epidemiol. 2001;54:603–609. doi: 10.1016/s0895-4356(00)00344-9. [DOI] [PubMed] [Google Scholar]
- 13.Center for Disease Control and Prevention. Rapid HIV testing in outreach and other community settings–United States, 2004–2006. MMWR Morb Mortal Wkly Rep. 2007;56:1233–1237. [PubMed] [Google Scholar]
- 14.Walensky RP. Arbelaez C. Reichmann WM, et al. Revising expectations from rapid HIV tests in the emergency department. Ann Intern Med. 2008;149:153–160. doi: 10.7326/0003-4819-149-3-200808050-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jafa K. Patel P. MacKellar DA et al. Investigation of false positive results with an oral fluid rapid HIV-1/2 antibody test. PLoS ONE. 2007;2:e185. doi: 10.1371/journal.pone.0000185. [DOI] [PMC free article] [PubMed] [Google Scholar]