Abstract
Background:
The World Trade Center (WTC) collapse produced a massive exposure to respirable particulates in New York City Fire Department (FDNY) rescue workers. This group had spirometry examinations pre-September 11, 2001, and post-September 11, 2001, demonstrating declines in lung function with parallel declines in FEV1 and FVC. To date, the underlying pathophysiologic cause for this has been open to question.
Methods:
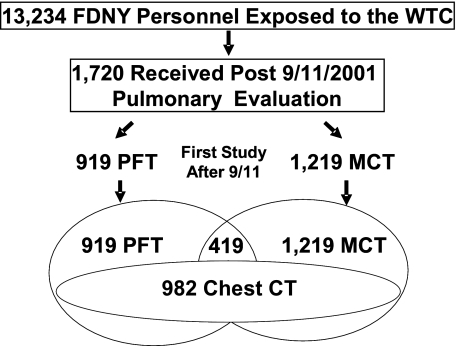
Of 13,234 participants in the FDNY-WTC Monitoring Program, 1,720 (13%) were referred for pulmonary subspecialty evaluation at a single institution. Evaluation included 919 full pulmonary function tests, 1,219 methacholine challenge tests, and 982 high-resolution chest CT scans.
Results:
At pulmonary evaluation (median 34 months post-September 11, 2001), median values were FEV1 93% predicted (interquartile range [IQR], 83%-101%), FVC 98% predicted (IQR, 89%-106%), and FEV1/FVC 0.78 (IQR, 0.72-0.82). The residual volume (RV) was 123% predicted (IQR, 106%-147%) with nearly all participants having normal total lung capacity, functional residual capacity, and diffusing capacity of carbon monoxide. Also, 1,051/1,720 (59%) had obstructive airways disease based on at least one of the following: FEV1/FVC, bronchodilator responsiveness, hyperreactivity, or elevated RV. After adjusting for age, gender, race, height and weight, and tobacco use, the decline in FEV1 post-September 11, 2001, was significantly correlated with increased RV percent predicted (P < .0001), increased bronchodilator responsiveness (P < .0001), and increased hyperreactivity (P = .0056). CT scans demonstrated bronchial wall thickening that was significantly associated with the decline in FEV1 post-September 11, 2001 (P = .024), increases in hyperreactivity (P < .0001), and increases in RV (P < .0001). Few had evidence for interstitial disease.
Conclusions:
Airways obstruction was the predominant physiologic finding underlying the reduction in lung function post-September 11, 2001, in FDNY WTC rescue workers presenting for pulmonary evaluation.
Two commercial jets struck the World Trade Center (WTC) on September 11, 2001, resulting in the collapse of three skyscrapers and the deaths of 2,751 persons, including 343 firefighters from the New York City Fire Department (FDNY). Surviving rescue workers and bystanders were exposed to respirable particulates and combustion by-products.1 Respiratory symptoms, either new or increased in severity, have been documented in FDNY rescue workers,2-7 other exposed workers,8 and residents.9-11 In a screening study using spirometry during the first year post-September 11, 2001, 12,079 FDNY rescue workers had a decline in FEV1 equal to an annual rate 12 times that found pre-September 11, 2001, with an exposure-response gradient based on arrival time at the WTC.3 Parallel declines in FEV1 and FVC resulted in a low FVC with normal FEV1/FVC.2-4 In non-FDNY WTC rescue/recovery workers, similar screening spirometry studies have also shown that the most common abnormality was a low FVC with normal FEV1/FVC,8,12,13 affecting anywhere from 16% to 20% of the cohort. However, without a complete pulmonary evaluation utilizing pulmonary function testing (bronchodilator response, lung volumes, diffusing capacity), methacholine challenge testing, and high-resolution chest CT as appropriate, it remains unclear whether the underlying pathophysiologic condition responsible for reductions in lung function is due to restrictive interstitial or obstructive lung disease.
FDNY rescue workers (firefighters and emergency medical service personnel) have been intensively screened as part of the FDNY-WTC Medical Monitoring Program (FDNY-WTC-MMP). We now report on the results of 1,720 FDNY rescue workers who were referred for pulmonary subspecialty evaluations using criteria consistent with the standard of care in a screening/monitoring or primary care practice (eg, symptom reports of functional impairment or abnormalities in screening spirometry or chest radiographs). Patients received physiologic and radiographic testing at a single center of excellence. The goal of this study was to determine the pathophysiologic basis for the observed reductions in lung function in this selected group referred for pulmonary subspecialty evaluation.
Materials and Methods
Since 1997, FDNY has performed periodic health evaluations, including spirometry, on all FDNY rescue workers at approximately 18-month intervals. All rescue workers employed by FDNY before the end of the WTC site rescue/recovery activities (725/02) were offered enrollment into the FDNY-WTC-MMP, and those agreeing to participate completed a questionnaire and received spirometry and chest radiography examinations. Physicians referred patients for pulmonary subspecialty evaluations based on symptom reports, functional impairment, or abnormalities in screening spirometry or chest radiographs. All subspecialty evaluations were performed by two FDNY pulmonologists, both of whom followed the same protocol and required all patients to receive physiologic and radiographic testing at a single center of excellence. All subjects agreed to the use of their data for analysis by signing a research consent approved by our institutional review board at Montefiore Medical Center.
Demographic Variables
Data on age, gender, race/ethnicity, and years of service at FDNY were obtained from the FDNY World Trade Center Medical Monitoring database. BMI was calculated from height and weight measured immediately before obtaining pulmonary functions.
Exposure Levels
Degree of exposure was self-reported and determined from the first FDNY-WTC-MMP Questionnaire. Using the FDNY-WTC Exposure Intensity Index,2-7 exposure intensity was categorized based on first arrival time at the WTC site as follows: high exposure if they arrived during the morning of September 11, 2001, intermediate exposure if they arrived after the morning of September 11, 2001, but within the first 2 days, and low exposure if they arrived between days 3 and 14. Those arriving after Day 14 were excluded from analysis as a result of their low numbers and significant demographic differences.
Smoking History
“Ever-smokers” reported smoking cigarettes ever during their lifetime on any FDNY-WTC-MMP post-September 11, 2001, questionnaire. “Never-smokers” consistently reported not smoking both pre-September 11, 2001, and post-September 11, 2001.
Pulmonary Function and Airway Hyperreactivity
FDNY spirometry was performed according to American Thoracic Society (ATS) guidelines14 using Portascreen Spirometry (S&M Instruments; Doylestown, PA). To provide three acceptable spirograms, seated workers wearing nose clips performed up to eight forced expiratory maneuvers per testing session. Spirograms were accepted if they (1) did not show artifacts such as cough or glottis closure during the first second of exhalation, early termination, variable effort, leakage, and obstructed mouthpiece (tongue or dentures); (2) had good starts with back-extrapolated volume not exceeding 5% of FVC or 150 mL (whichever was larger), (3) had satisfactory exhalation length (at least 6 s and/or a plateau in the volume/time curve); and (4) spirometric measurements were considered reproducible if the best and second-best FVC or FEV1 measurements were within 200 mL of each other. The largest FVC and FEV1 from among all acceptable spirograms were selected for electronic archiving. All acceptable measures were expressed in absolute values (liters) and as percent predicted of normal.15-17
Pulmonary function tests (PFTs) were performed according to ATS guidelines8 using a Jaeger Masterscreen PFT System (Viasys Healthcare; Yorba Linda, CA). Total lung capacity (TLC), functional residual capacity (FRC), and residual volume (RV) were obtained by plethysmography and diffusing capacity of carbon monoxide (DLCO) by single breath methods. All acceptable measures were expressed in absolute values (liters) and as percent predicted of normal.15-17 Normal limits for FEV1, FVC, and FEV1/FVC were based on the lower limits of normal (LLN).18 For clinical reference, the LLN for white men aged 40 in this population, calculated using pre-September 11, 2001, data, corresponds to an FEV1 of 82% predicted, an FVC of 79% predicted, and an FEV1/FVC < 0.76. Normal limits for TLC, FRC, RV, and DLCO were 80% or less of predicted.16-18 Flow rates and lung volumes were reassessed 15 min after albuterol inhalation, with a significant postbronchodilator response defined as an increase in FEV1 of 12% or more and 200 mL or more.18 In patients with multiple PFTs, the one obtained earliest during the pulmonary evaluation post-September 11, 2001, was used for analysis.
To account for intersubject differences in time intervals between pre-September 11, 2001, and post-September 11, 2001, PFTs, the decline in FEV1, was calculated as the ratio of the percent predicted post-September 11, 2001, to the pre-September 11, 2001, value.
Methacholine challenge testing (MCT) was performed according to ATS guidelines.19 Exclusion criteria were an FEV1 < 65% predicted, nonreproducible flow-volume loops, use of inhaled or systemic corticosteroids or leukotriene receptor antagonists within the preceding month, or bronchodilators or caffeine on the test day. Increasing concentrations of aerosolized methacholine were inhaled until the provocative concentration of methacholine at which the FEV1 declined by 20% from the baseline value (PC20) or the maximal concentration was reached (25 mg/mL methacholine). For this study, hyperreactivity was defined as a PC20 < 16 mg/mL methacholine.
Chest CT
High-resolution chest CT scans were obtained with 7-mm-thick images reconstructed at 6-mm intervals. Images were read for airway and parenchymal abnormalities by dedicated, board-certified radiologists who had no knowledge of the subjects’ exposure status or clinical findings. Bronchial wall thickening was interpreted qualitatively and analyzed as a yes/no variable.
Statistical Analysis
Continuous variables are expressed as medians with the 25th to 75th percentile interquartile range (IQR) and categorical variables as percentages with CI. Hyperreactivity was analyzed as a dichotomous variable (PC20 < 16 mg/mL methacholine) and as a continuous variable (methacholine response slope). Indicators of airway injury including FEV1 decline, bronchodilator response, and methacholine slope were plotted by group in separate analyses. Using the Kruskal-Wallis test, χ2 test, multivariable regression analyses, or P test for trend, as appropriate, we compared findings among groups. All tests were two-tailed. P values ≤ .05 were considered statistically significant. Analysis was performed using SAS, version 9.1 (SAS Institute; Cary, NC) and Graphpad Prism V (Graphpad Software; La Jolla, CA) software.
Results
Study Population and Demographics
Between September 12, 2001, and March 10, 2008, 1,720 of 13,234 (13%) FDNY WTC rescue workers received pulmonary subspecialty evaluation, with all specialized tests performed at the same center. Comparisons between this group and the remaining participants (n = 11,514) are shown in Table 1. There were small but statistically significant differences in age, years of FDNY service, height, gender, and race. There were no significant differences in BMI or tobacco use history. Findings were similar when comparisons between these groups were limited to only those with pre-September 11, 2001, spirometry (not shown; 1,590 vs 9,927). Of the 1,720 patients referred for pulmonary evaluation, 919 had PFTs, 1,219 had MCT, 419 had both PFTs and MCT, and 982 had CT scans (Fig 1).
Table 1.
—Demographics
| Patients Presenting for Pulmonary Evaluation No. (% or IQR) |
||||
| Demographics | Yes | No | P Value | |
| Total | 1,720 (100) | 11,514 (100) | <.0001a | |
| Firefighter | 1,684 (98) | 9,590 (83) | ||
| EMS worker | 36 (2) | 1,924 (17) | ||
| Exposure status | ||||
| High (arrived day 1, morning) | 404 (23) | 1,748 (15) | <.0001a | |
| Intermediate | 1,230 (72) | 8,450 (73) | ||
| Low (arrived days 3-14) | 86 (5) | 1,316 (11) | ||
| Age on September 11, 2001 (IQR) | 42 (37-46) | 39 (33-45) | <.0001b | |
| Years of service on September 11, 2001 (IQR) | 15 (8-20) | 11 (5-18) | <.0001b | |
| Gender, male | 1,703 (99) | 1,1068 (96) | <.0001a | |
| Tobacco use | ||||
| Ever | 609 (35) | 3961 (35) | <.4359a | |
| Never | 1,108 (65) | 7517 (65) | ||
| Race | ||||
| White | 1,580 (92) | 9,993 (87) | <.0001a | |
| African-American | 57 (3) | 662 (6) | ||
| Hispanic | 78 (5) | 784 (7) | ||
| Height, cm (IQR) | 178 (175-183) | 178 (173-182) | <.0005b | |
| BMI, IQR | 28 (26-30) | 28 (26-30) | .0446b | |
| Pre-September 11, 2001, FDNY spirometryc | ||||
| FEV1, L (IQR) | 4.16 (3.73-4.65) | 4.32 (3.83-4.82) | <.0001d | |
| FVC, L (IQR) | 4.94 (4.46-5.52) | 5.07 (4.49-5.67) | <.0036 d | |
| FEV1/FV (IQR) | 0.85 (0.81-0.88) | 0.86 (0.82-0.89) | <.0001d | |
EMS = emergency medical services; FDNY = New York City Fire Department; IQR = interquartile range.
P values from χ2 test.
P values from Kruskal-Wallis test.
Pre-September 11, 2001, FDNY spirometry data were available for 1,590 of the 1,720 and 9,927 of the 11,514.
Controlling for smoking, gender, BMI, age, and race.
Figure 1.
Schematic representation of those receiving pulmonary evaluation and further diagnostic testing. FDNY = New York City Fire Department; MCT = methacholine challenge testing; PFT = pulmonary function test; WTC = World Trade Center.
After controlling for BMI and tobacco use, an exposure-response gradient was evident. The proportion of patients presenting for pulmonary evaluation in each exposure category was 19% (CI, 17%-21%) of those with high exposure as compared with 13% (CI, 12%-13%) of those with intermediate exposure and only 6% (CI, 5%-8%) of those with low exposure (P < .0001) (Fig 2).
Figure 2.
Proportion of exposed FDNY rescue workers presenting for pulmonary evaluation. The number (percent) of each exposure category presenting for evaluation differed significantly (P = .0001); 1,720/13,234 (13%) of the total population, 404/2,152 (19%) of those in the high-intensity exposure category, 1,230/9,680 (13%) of those in the intermediate-exposure category (Inter), and 86/1,402 (6%) of those in the low-exposure category received subspecialty evaluation. The total number of individuals in each group is shown in parentheses below the group label. The error bars show the 95% CIs. See Figure 1 legend for expansion of abbreviation.
Pre- to Post-September 11, 2001, FDNY Spirometry
Pre-September 11, 2001, spirometry was available for 1,590 of 1,720 (92%) referred for pulmonary evaluation and 9,927 of 11,514 (86%) who were not referred for evaluation Tables 1,2). The median time interval between the pre-September 11, 2001, spirometry and post-September 11, 2001, for the pulmonary evaluation group was 9.60 months (IQR, 4.56-16.56) and for the nonreferral group was 8.92 months (IQR, 4.13-15.18). Differences in FEV1, FVC, and FEV1/FVC ratio between the pulmonary evaluation group and the nonreferral group were small but statistically significant (Table 1). There were significant declines in FEV1, and FEV1/FVC when spirometry obtained within 1 year post-September 11, 2001, was compared to spirometry from 1 year pre-September 11, 2001 (Table 2).
Table 2.
—Spirometry Before and After September 11, 2001, of the Pulmonary Evaluation Group
| Evaluation Period |
||
| Pulmonary Evaluation | Pre-September 11, 2001 | Post-September 11, 2001 |
| FEV1, value (IQR) | 4.16 (3.73-4.65) | 3.78 (3.32-4.21) |
| FEV1, % predicted (IQR) | 99 (89-108) | 93 (83-101) |
| FVC, value (IQR) | 4.94 (4.46-5.52) | 4.93 (4.40-5.47) |
| FVC, % predicted (IQR) | 93.5 (85-102) | 96 (89-106) |
| FEV1/FVC (IQR) | 0.85 (0.81-0.88) | 0.77 (0.72-0.82) |
| Post-September 11, 2001, declinea | ||
| FEV1 | 0.94 | |
| IQR | 0.87-1.01 | |
| FVC | 1.05 | |
| IQR | 0.97-1.13 | |
Data represented as medians. See Table 1 for expansion of the abbreviations.
Decline is post-September 11, 2001, % predicted divided by pre-September 11, 2001, % predicted.
Post- to Post-September 11, 2001, PFTs and MCT
Complete PFTs were obtained at the beginning of the pulmonary subspecialty evaluation (Table 3). The median time interval between the pre-September 11, 2001, spirometry and the post-September 11, 2001, pulmonary subspecialty testing was 48 months (IQR, 32-67). The median time interval from the day of the attack on September 11, 2001, and the pulmonary subspecialty testing was 34 months (IQR, 23-56). Noteworthy median values were FEV1 93% predicted (IQR, 83%-101%), FVC 98% predicted (89%-106%), and FEV1/FVC 0.78 (0.72-0.82). Seven hundred fifteen (42%) participants had an FEV1/FVC below the LLN (< 0.76). The RV was 123% (106%-147%) predicted. Of those with complete PFTs, 199 (23%) had a significant bronchodilator response. Of those with MCT, 299 (25%) had methacholine dose response slopes greater than 0.13, which corresponds to a PC20 < 16 mg/mL. One thousand fifteen of the 1,720 (59%) patients with PFTs and/or MCT had obstructive airways disease, based on at least one of the following criteria: an FEV1/FVC < 0.76 (LLN), bronchodilator responsiveness, hyperreactivity, or an RV > 120% predicted. Exposure-response gradients for PFT measures, bronchodilator response, or hyperactivity were not statistically significant.
Table 3.
—PFT Results from the Pulmonary Subspecialty Evaluation
| Exposure Status |
|||||
| Pulmonary Evaluation | Total | High | Intermediate | Low | P Valuea |
| FEV1, value (IQR) | 3.78 (3.32-4.21) | 3.84 (3.28-4.18) | 3.78 (3.35-4.23) | 3.67 (3.17-4.23) | .6922 |
| FEV1, % predicted (IQR) | 93.0 (83.0-101.0) | 93.0 (83.0-101.0) | 93.0 (83.0-102.0) | 92.5 (79.0-102.0) | .7665 |
| FVC, value (IQR) | 4.93 (4.40-5.47) | 4.88 (4.32-5.42) | 4.94 (4.44-5.49) | 4.91 (4.41-5.32) | .6559 |
| FVC, % predicted (IQR) | 98.0 (89.0-106) | 96.0 (88.0-105.0) | 98.0 (89.0-106.0) | 99.5 (92.0-106.0) | .0363 |
| FEV1/FVC × 100 (IQR) | 77.47 (72.19-81.61) | 78.52 (73.19-82.39) | 77.18 (71.88-81.38) | 76.79 (69.30-81.46) | .7751 |
| BD, % change (IQR) | 6.0 (3.0-12.0) | 5.0 (3.0-12.0) | 6.0 (3.0-12.0) | 6.0 (4.0-12.0) | .8599 |
| RV, value (IQR) | 2.38 (2.01-2.91) | 2.37 (1.96-2.88) | 2.38 (2.01-2.89) | 2.85 (2.01-3.32) | .0154 |
| RV, % predicted (IQR) | 123.0 (106.0-147.0) | 124.5 (106.0-149.0) | 122.0 (106.0-146.0) | 131.0 (105.0-161.0) | .9603 |
| FRC, value (IQR) | 3.35 (2.85-3.95) | 3.31 (2.84-3.89) | 3.35 (2.85-3.96) | 3.73 (3.07-4.20) | .9016 |
| FRC, % predicted (IQR) | 96.0 (83.0-112.0) | 96.0 (83.0-111.0) | 96.0 (83.0-112.0) | 104.0 (93.0-118.0) | .8721 |
| TLC, value (IQR) | 7.14 (6.38-7.86) | 7.02 (6.26-7.79) | 7.14 (6.41-7.89) | 7.34 (6.57-7.81) | .8279 |
| TLC, % predicted (IQR) | 101.0 (91.0-109.0) | 99.0 (90.0-109.0) | 101.0 (92.0-109.0) | 101.0 (91.0-114.0) | .9360 |
| DLCO, value (IQR) | 29.82 (26.09-33.47) | 29.49 (25.40-33.67) | 30.02 (26.27-33.30) | 28.23 (24.16-33.96) | .5041 |
| DLCO, % predicted (IQR) | 104.0 (91.0-114.0) | 102.0 (90.0-114.0) | 104.0 (92.0-114.0) | 103.5 (90.0-117.0) | .6058 |
BD = bronchodilator; DLCO = diffusing capacity of carbon monoxide; FRC = functional residual capacity; PFT = pulmonary function test; RV = residual volume; TLC = total lung capacity. See Table 1 for expansion of other abbreviations.
P test for trend controlling for tobacco use, gender, height, weight, age, and race. Data represented as medians with interquartile range.
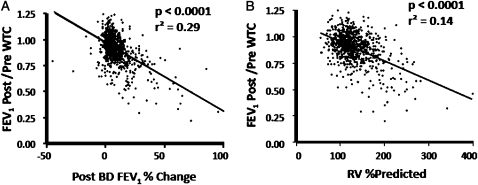
Decline in FEV1 Post-September 11, 2001, Correlates With Measures Airway Injury
After adjusting for age, gender, race, height and weight, and tobacco use, the decline in FEV1 was significantly correlated with increased response to bronchodilators (P < .0001, r2 = 0.29) (Fig 3A) and with increases in RV% predicted (P < .0001, r2 = 0.14) (Fig 3B). Hyperreactivity as measured by an increased response to methacholine was significantly correlated with the decline in FEV1 (P < .0056, r2 = 0.04) and with increases in RV% predicted (P < .0001, r2 = 0.08). Thus, airway injury was the predominant physiologic abnormality.
Figure 3.
Correlation of decline in FEV1 post-September 11, 2001, with other physiologic measures of airway injury. After adjusting for age, gender, race, height and weight (or BMI instead of height and weight), and tobacco-smoking status, the post-September 11, 2001, decline in FEV1, calculated as the %FEV1 post-September 11, 2001,/%FEV1 pre-September 11, 2001, correlates with bronchodilator response (P<.0001; r2 = 0.29) (A) and RV% predicted (P<.0001; r2 = 0.14) (B). BD = bronchodilator; RV = residual volume. See Figure 1 legend for expansion of other abbreviations.
Chest CT Findings
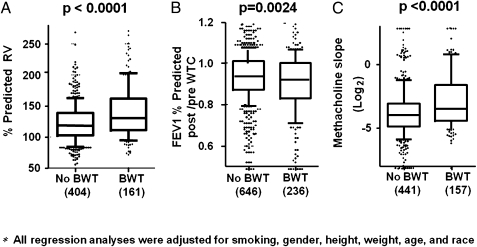
Chest CT scans were performed on 982 of 1,720 (57%) patients to screen for parenchymal lung disease, with bronchial wall thickening in 26%, emphysema in 12%, evidence of sarcoidosis (confirmed by biopsy) in 4%, and evidence of pulmonary fibrosis (confirmed by biopsy) in less than 1%. Bronchial wall thickening was associated with statistically significant increases in RV (P < .0001) (Fig 4A), the decline in FEV1 post-September 11, 2001, (P = .024) (Fig 4B), and increases in the methacholine slope (P < .0001)(Fig 4C). Importantly, airway abnormalities on CT scans correlated with physiologic measures.
Figure 4.
Correlation of BWT on CT scan with measures of airway injury. The presence of BWT is associated with air trapping as measured by elevated RV percent (P < .0001) (A); FEV1 decline in the interval from the pre-September 11, 2001, spirometry to the post-September 11, 2001, measurement at the time of the pulmonary evaluation as calculated from the difference between percent predicted values (P = .0024) (B); and airway reactivity as measured by methacholine challenge slope (L/mg) (P < .0001) (C). BWT = bronchial wall thickening. See Figures 1 and 3 legends for expansion of other abbreviations.
Discussion
Prior studies have shown lung injury in individuals exposed to the WTC disaster.2-13 We and others2-4,8,12, 13 have reported a low FVC with parallel declines in FEV1 yielding a normal FEV1/FVC as a common abnormality on screening spirometry, raising concerns of endemic interstitial lung disease.8,20 This was supported by an initial case of acute eosinophilic pneumonia in an FDNY firefighter in the first weeks after September 11, 2001,21 and reports of sarcoidosis in FDNY rescue workers and other rescue/recovery workers post-September 11, 2001.22-24
We now report our experience with 1,720 WTC-exposed FDNY rescue workers referred for subspecialty pulmonary evaluation for reports of functional impairment or abnormalities in screening spirometry or chest radiographs. These criteria reflect the standard of care found in a screening/monitoring program or primary care practice. Symptomatic patients with WTC exposure most frequently present with parallel declines in FEV1 and FVC.2-4,8,12,13 Pre-September 11, 2001, and post-September 11, 2001, pulmonary function data in this group referred for pulmonary subspecialty evaluation provide a unique opportunity to characterize the underlying pathophysiologic characteristics.
Airways obstruction was the predominant physiologic abnormality post-September 11, 2001, and this remained true even when we analyzed only the subgroup (424/1,688) with a low FVC (< 79% predicted) and normal FEV1/FVC (≥ 0.76). Lung volumes were measured by plethysmography to avoid underestimations due to airways obstruction. Air trapping, demonstrated by the increase in RV, correlated with the decline in FEV1 post-September 11, 2001, bronchodilator responsiveness, hyperreactivity, and bronchial wall thickening on CT scans. Thus, the parallel declines in FEV1 and FVC previously reported were due to air trapping rather than restriction, a conclusion further supported by the normal TLC, FRC, and DLCO found in this group. To avoid associations between measures of airways obstruction or air trapping and age, height, weight, or BMI, all analyses were adjusted for these potential confounders. Our results demonstrate that for the vast majority of our patients, respirable particulate matter and other pollutants (eg, combustion byproducts) released by the WTC collapse caused airway injury rather than interstitial lung disease.
Prior studies in patients with airways obstruction unrelated to the WTC showed that the degree of air trapping as determined by RV% predicted, but not TLC% predicted, was strongly associated with FEV1,% predicted.25 Additional studies in patients with COPD showed that when air trapping is present, static lung volumes such as RV% predicted, but not TLC% predicted, were responsive to bronchodilators.26,27 We observed a similar finding in our group of WTC-exposed patients, where following bronchodilator administration, there was a significant association between the decline in RV% predicted and the increase in FVC% predicted. We also noted an association between RV% predicted and hyperreactivity. This extends findings from a prior study of non-FDNY WTC patients, in which Oppenheimer and coworkers28measured airways resistance (impulse oscillometry) and frequency dependence of compliance, both physiologic probes for distal airways disease, and demonstrated elevated airways resistance that was responsive to bronchodilators in patients with normal spirometry.
Just over half of our patients received high-resolution CT scans. Bronchial wall thickening, which reflects proximal airway inflammation and/or remodeling,29 correlated well with FEV1 decline post-September 11, 2001, and methacholine reactivity, physiologic parameters that are predominantly influenced by large airway dysfunction, providing further evidence for airways injury in this cohort. A prior report in a small case series of patients with WTC dust exposure demonstrated a correlation between a semiquantitative measure of air trapping and FVC reductions.30 A limitation of our study was that it did not include quantitative radiographic measurement of air trapping.
Chest CT scans served another purpose by identifying the minority of patients who had interstitial lung diseases, with or without obstruction, that is, 43 patients with sarcoidosis proven by biopsy specimen examination (27 with the diagnosis made post-September 11, 2001) and three patients with pulmonary fibrosis proven by biopsy specimen examination (all post-September 11, 2001), included in our analysis so as not to bias our conclusions. Reduced lung volumes and DLCO were found in two patients with pulmonary fibrosis, and a reduced DLCO was found in one patient with sarcoidosis. In fact, consistent with prior studies, 60% of the patients with sarcoidosis had obstructive physiology.31 That patients subsequently found to have interstitial lung disease were too few in number to influence our findings is further support for our conclusion that interstitial disease is rare and airways obstruction is the predominant pathophysiologic characteristic in WTC patients who present for pulmonary evaluation.
Pollution studies demonstrate a significant epidemiologic link between the exposure to airborne particulates and adverse health effects.32,33 The WTC collapse produced a massive exposure to respirable particulates, with the larger-size dust fractions having a pH ranging from 9 to 11, leading to an alkaline “burn” of mucosal surfaces. Inorganic material was also concentrated in the large particles.1,20 WTC dust produced pulmonary inflammation and airway hyperreactivity in mice34 and a dose-dependent cytokine response in cultured human alveolar macrophages.35 Induced sputum from FDNY firefighters, 10 months after their WTC exposure, showed high levels of particulates and evidence of continuing inflammation.36 These studies provide a biologically plausible rationale for the ongoing impact of WTC exposure producing acute and chronic inflammation resulting in decreased lung function within months of exposure,2-5 followed by the development of airways obstruction and the continued need for pulmonary evaluation months to years later.
We previously observed a dose-response gradient for the decline in lung function during the first year post-September 11, 2001, with those arriving during the morning of the collapse having the greatest decline in FEV1 and FVC2-4 and the highest incidence of hyperreactivity.5,6 We and others2-11 observed similar dose-response gradients for pulmonary symptoms and abnormal spirometry at the time of the first post-September 11, 2001, monitoring exam.2-5,8 In our current study, a greater proportion of highly exposed rescue workers presented for pulmonary subspecialty evaluation, 19% of those arriving during the morning of day 1 as compared with 6% of those who arrived after day 2. However, in this group of patients presenting for pulmonary evaluation, exposure intensity no longer had a significant impact on lung function. This suggests that while initial exposure intensity is the critical determinant of acute inflammation and early reductions in lung function, the clinical course of nonresolving airway inflammation and airways obstruction is dependent not only on the intensity of the initial insult but also on the host’s inflammatory response, reflecting the complexity of genetic-environmental interactions.
This report is a comprehensive description of WTC-exposed FDNY rescue workers who presented for pulmonary evaluation during the first 7 years postexposure. Multiple independent diagnostic modalities (obtained at a single center) were used, allowing us to report correlations between physiologic and radiographic measures. All modalities point to persistent airway injury and obstruction as the predominant underlying pathophysiologic characteristics in this cohort. The effect of treatment on the clinical course of these findings and the extent to which these findings can be applied to other WTC-exposed patients remain to be determined.
Acknowledgments
Author Contributions: Dr Weiden: had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, designed the study, recruited participants, wrote and prepared the manuscript, and reviewed, edited and approved the manuscript.
Dr Ferrier: collected data, analyzed data, and reviewed, edited, and approved the manuscript.
Dr Nolan: collected data, analyzed data, wrote and prepared the manuscript, and reviewed, edited, and approved the manuscript.
Dr Rom: wrote and prepared the manuscript, and reviewed, edited, and approved the manuscript.
Ms Comfort: collected data, analyzed data, and reviewed, edited, and approved the manuscript.
Mr Gustave: analyzed data, and reviewed, edited, and approved the manuscript.
Ms Zeig-Owens: analyzed data, and reviewed, edited, and approved the manuscript.
Dr Zheng: collected data, and reviewed, edited, and approved the manuscript.
Dr Goldring: performed pulmonary function quality assurance, wrote and prepared the manuscript, and reviewed, edited, and approved the manuscript.
Dr Berger: performed pulmonary function quality assurance, wrote and prepared the manuscript, and reviewed, edited, and approved the manuscript.
Ms Cosenza: collected data, and reviewed, edited, and approved the manuscript.
Mr Lee: analyzed data, and reviewed, edited, and approved the manuscript.
Dr Webber: analyzed data, wrote and prepared the manuscript, and reviewed, edited, and approved the manuscript.
Dr Kelly: recruited participants, wrote and prepared the manuscript, and reviewed, edited, and approved the manuscript.
Dr Aldrich: performed pulmonary function quality assurance, wrote and prepared the manuscript, and reviewed, edited, and approved the manuscript.
Dr Prezant: had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis, designed the study, recruited participants, wrote and prepared the manuscript, and reviewed, edited, and approved the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: the authors received federal funding from National Institute of Occupational Safety and Health and the National Institutes of Health.
Other contributors: The authors wish to thank the New York City Fire Department firefighters and emergency medical services workers for the selfless dedication to their job, the city, and our country.
Abbreviations
- ATS
American Thoracic Society
- DLCO
diffusing capacity of carbon monoxide
- FDNY
New York City Fire Department
- FDNY-WTC-MMP
New York City Fire Department-World Trade Center Medical Monitoring Program
- FRC
functional residual capacity
- IQR
interquartile range
- LLN
lower limits of normal
- MCT
methacholine challenge testing
- PC20
provocative concentration of methacholine at which the FEV1 declines by 20% of baseline
- PFT
pulmonary function test
- RV
residual volume
- TLC
total lung capacity
- WTC
World Trade Center
Funding/Support: This study was funded by the Centers for Disease Control and Prevention [U1Q/CCU221158] and the National Institute of Occupational Safety and Health [U10-OH008243, U10-OH008242, and R01-OH07350], NIH [M01 00096, K23HL084191, K24A1080298, and R01HL057879].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestpubs.org/site/misc/reprints.xhtml).
References
- 1.McGee JK, Chen LC, Cohen MD, et al. Chemical analysis of World Trade Center fine particulate matter for use in toxicologic assessment. Environ Health Perspect. 2003;111(7):972–980. doi: 10.1289/ehp.5930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prezant DJ, Weiden M, Banauch GI, et al. Cough and bronchial responsiveness in firefighters at the World Trade Center site. N Engl J Med. 2002;347(11):806–815. doi: 10.1056/NEJMoa021300. [DOI] [PubMed] [Google Scholar]
- 3.Banauch GI, Hall C, Weiden M, et al. Pulmonary function after exposure to the World Trade Center collapse in the New York City Fire Department. Am J Respir Crit Care Med. 2006;174(3):312–319. doi: 10.1164/rccm.200511-1736OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feldman DM, Baron SL, Bernard BP, et al. Symptoms, respirator use, and pulmonary function changes among New York City firefighters responding to the World Trade Center disaster. Chest. 2004;125(4):1256–1264. doi: 10.1378/chest.125.4.1256. [DOI] [PubMed] [Google Scholar]
- 5.Banauch GI, Dhala A, Alleyne D, et al. Bronchial hyperreactivity and other inhalation lung injuries in rescue/recovery workers after the World Trade Center collapse. Crit Care Med. 2005;33(1 Suppl):S102–S106. doi: 10.1097/01.ccm.0000151138.10586.3a. [DOI] [PubMed] [Google Scholar]
- 6.Banauch GI, Alleyne D, Sanchez R, et al. Persistent hyperreactivity and reactive airway dysfunction in firefighters at the World Trade Center. Am J Respir Crit Care Med. 2003;168(1):54–62. doi: 10.1164/rccm.200211-1329OC. [DOI] [PubMed] [Google Scholar]
- 7.Banauch GI, Dhala A, Prezant DJ. Pulmonary disease in rescue workers at the World Trade Center site. Curr Opin Pulm Med. 2005;11(2):160–168. doi: 10.1097/01.mcp.0000151716.96241.0a. [DOI] [PubMed] [Google Scholar]
- 8.Herbert R, Moline J, Skloot G, et al. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect. 2006;114(12):1853–1858. doi: 10.1289/ehp.9592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC) Self-reported increase in asthma severity after the September 11 attacks on the World Trade Center—Manhattan, New York, 2001. MMWR Morb Mortal Wkly Rep. 2002;51(35):781–784. [PubMed] [Google Scholar]
- 10.Reibman J, Lin S, Hwang SA, et al. The World Trade Center residents’ respiratory health study: new-onset respiratory symptoms and pulmonary function. Environ Health Perspect. 2005;113(4):406–411. doi: 10.1289/ehp.7375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Szema AM, Khedkar M, Maloney PF, et al. Clinical deterioration in pediatric asthmatic patients after September 11, 2001. J Allergy Clin Immunol. 2004;113(3):420–426. doi: 10.1016/j.jaci.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 12.Skloot GS, Schechter CB, Herbert R, et al. Longitudinal assessment of spirometry in the World Trade Center medical monitoring program. Chest. 2009;135(2):492–498. doi: 10.1378/chest.08-1391. [DOI] [PubMed] [Google Scholar]
- 13.Salzman SH, Moosavy FM, Miskoff JA, Friedmann P, Fried G, Rosen MJ. Early respiratory abnormalities in emergency services police officers at the World Trade Center site. J Occup Environ Med. 2004;46(2):113–122. doi: 10.1097/01.jom.0000111612.68916.d0. [DOI] [PubMed] [Google Scholar]
- 14.Miller MR, Hankinson J, Brusasco V, et al. ATS/ERS Task Force Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 15.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159(1):179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 16.Crapo RO, Morris AH, Clayton PD, Nixon CR. Lung volumes in healthy nonsmoking adults. Bull Eur Physiopathol Respir. 1982;18(3):419–425. [PubMed] [Google Scholar]
- 17.Burrows B, Kasik JE, Niden AH, Barclay WR. Clinical usefulness of the single-breath pulmonucy diffusing capacity test. Am Rev Respir Dis. 1961;84:789–806. doi: 10.1164/arrd.1961.84.6.789. [DOI] [PubMed] [Google Scholar]
- 18.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–968. doi: 10.1183/09031936.05.00035205. [DOI] [PubMed] [Google Scholar]
- 19.Crapo RO, Casaburi R, Coates AL, et al. Guidelines for methacholine and exercise challenge testing—1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000;161(1):309–329. doi: 10.1164/ajrccm.161.1.ats11-99. [DOI] [PubMed] [Google Scholar]
- 20.Landrigan PJ, Lioy PJ, Thurston G, et al. NIEHS World Trade Center Working Group Health and environmental consequences of the World Trade Center disaster. Environ Health Perspect. 2004;112(6):731–739. doi: 10.1289/ehp.6702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rom WN, Weiden M, Garcia R, et al. Acute eosinophilic pneumonia in a New York City firefighter exposed to World Trade Center dust. Am J Respir Crit Care Med. 2002;166(6):797–800. doi: 10.1164/rccm.200206-576OC. [DOI] [PubMed] [Google Scholar]
- 22.Izbicki G, Chavko R, Banauch GI, et al. World Trade Center “sarcoid-like” granulomatous pulmonary disease in New York City Fire Department rescue workers. Chest. 2007;131(5):1414–1423. doi: 10.1378/chest.06-2114. [DOI] [PubMed] [Google Scholar]
- 23.Safirstein BH, Klukowicz A, Miller R, Teirstein A. Granulomatous pneumonitis following exposure to the World Trade Center collapse. Chest. 2003;123(1):301–304. doi: 10.1378/chest.123.1.301. [DOI] [PubMed] [Google Scholar]
- 24.Jordan HT, Thorpe L, Cone J. Sarcoidosis diagnosed after September 11 2001 among persons exposed to the 9/11/2001 World Trade Center disaster [Abstract] http://apha.confex.com/apha/136am/webprogram/Paper182085.html. AccessedOctober 23, 2009. [DOI] [PubMed]
- 25.Dykstra BJ, Scanlon PD, Kester MM, Beck KC, Enright PL. Lung volumes in 4,774 patients with obstructive lung disease. Chest. 1999;115(1):68–74. doi: 10.1378/chest.115.1.68. [DOI] [PubMed] [Google Scholar]
- 26.Gelb AF, Taylor CF, McClean PA, et al. Tiotropium and simplified detection of dynamic hyperinflation. Chest. 2007;131(3):690–695. doi: 10.1378/chest.06-1662. [DOI] [PubMed] [Google Scholar]
- 27.Newton MF, O’Donnell DE, Forkert L. Response of lung volumes to inhaled salbutamol in a large population of patients with severe hyperinflation. Chest. 2002;121(4):1042–1050. doi: 10.1378/chest.121.4.1042. [DOI] [PubMed] [Google Scholar]
- 28.Oppenheimer BW, Goldring RM, Herberg ME, et al. Distal airway function in symptomatic subjects with normal spirometry following World Trade Center dust exposure. Chest. 2007;132(4):1275–1282. doi: 10.1378/chest.07-0913. [DOI] [PubMed] [Google Scholar]
- 29.Müller NL, Miller RR. Diseases of the bronchioles: CT and histopathologic findings. Radiology. 1995;196(1):3–12. doi: 10.1148/radiology.196.1.7784583. [DOI] [PubMed] [Google Scholar]
- 30.Mendelson DS, Roggeveen M, Levin SM, Herbert R, de la Hoz RE. Air trapping detected on end-expiratory high-resolution computed tomography in symptomatic World Trade Center rescue and recovery workers. J Occup Environ Med. 2007;49(8):840–845. doi: 10.1097/JOM.0b013e3180d09e87. [DOI] [PubMed] [Google Scholar]
- 31.Lynch JP, III, Ma YL, Koss MN, White ES. Pulmonary sarcoidosis. Semin Respir Crit Care Med. 2007;28(1):53–74. doi: 10.1055/s-2007-970333. [DOI] [PubMed] [Google Scholar]
- 32.Dockery DW. Epidemiologic study design for investigating respiratory health effects of complex air pollution mixtures. Environ Health Perspect. 1993;101(Suppl 4):187–191. doi: 10.1289/ehp.93101s4187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dockery DW, Pope CA, III, Xu X, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993;329(24):1753–1759. doi: 10.1056/NEJM199312093292401. [DOI] [PubMed] [Google Scholar]
- 34.Gavett SH, Haykal-Coates N, Highfill JW, et al. World Trade Center fine particulate matter causes respiratory tract hyperresponsiveness in mice. Environ Health Perspect. 2003;111(7):981–991. doi: 10.1289/ehp.5931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Payne JP, Kemp SJ, Dewar A, et al. Effects of airborne World Trade Center dust on cytokine release by primary human lung cells in vitro. J Occup Environ Med. 2004;46(5):420–427. doi: 10.1097/01.jom.0000126021.25149.64. [DOI] [PubMed] [Google Scholar]
- 36.Fireman EM, Lerman Y, Ganor E, et al. Induced sputum assessment in New York City firefighters exposed to World Trade Center dust. Environ Health Perspect. 2004;112(15):1564–1569. doi: 10.1289/ehp.7233. [DOI] [PMC free article] [PubMed] [Google Scholar]