Abstract
Purpose
Oblique proximal tibial osteotomy is a useful option for correcting deformity associated with Blount’s disease (tibia vara). Safe, adequate correction depends on technical issues that have evolved since the original description of the procedure.
Methods
Retrospective review of surgical experience.
Results
The refinement of osteotomy plane orientation, based on the distal rather than the proximal tibia, reduces the likelihood of procurvatum after surgery. The stability of the osteotomy is enhanced by an improved screw fixation technique. The risk of compartment syndrome is low if prophylactic partial fasciotomy is performed concurrently. Avoidance of spinal or regional block anesthesia minimizes the possibility of failure to detect post-operative compartment syndrome.
Conclusions
Improvements in the technical execution of oblique proximal tibial osteotomy enhances the correction and predictability of the procedure.
Keywords: Blount’s disease, Tibial osteotomy, Oblique osteotomy
Introduction
Oblique proximal tibial osteotomy is a surgical option for the correction of deformity associated with the tibia vara (Blount’s disease), especially when significant internal tibial torsion is present. Its main advantages are the maintenance of significant cancellous bone contact while correcting deformities in two planes, and the excellent cosmetic appearance afforded by both the bi-planar correction and the lateral translation of the distal fragment [1, 2]. In fact, the lateral translation occurs because the osteotomy rotates near the center of the knee (at the site of deformity) and not at the location of the osteotomy site itself (Fig. 1).
Fig. 1.
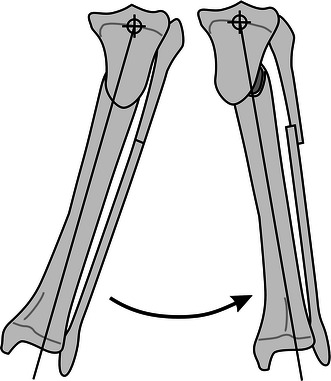
As the distal fragment of the osteotomy slides along the cut surface, the center of frontal rotation is in the proximal tibia, and external rotation of the distal fragment occurs
The exact orientation of an oblique osteotomy is critical to the success of the correction of multi-planar deformity. In Blount’s disease, the deformity typically includes varus, internal rotation, and (sometimes) procurvatum. Mathematical [3] and graphical analytic [4] methods have been applied to this problem, as well as a small published clinical series using prepared graphs to analyze any complex three-dimensional deformity suitable for oblique single-cut osteotomy correction [5].
Shortly after the published description of one method for the operation in 1988 [2], several modifications were made to the published technique that have improved the reliability of the procedure and have corrected minor problems reported informally by other surgeons. This paper provides an updated technical description of the procedure.
Draping
To improve visualization, limbs are draped completely free from the inguinal area to the toe. It may be wise to include both limbs in the field, particularly if the tibia vara is unilateral, to assist in the clinical assessment of the correction. A sterile tourniquet is used to avoid covering the upper limb by drapes.
Incision
The transverse incision described in the original paper is not extensible and has not proven to be especially cosmetic after healing. More useful is an oblique incision [6] that begins near the medial joint line in the mid-medial line, directed 45° laterally and inferiorly, and ends in the mid-lateral line (Fig. 2). This wound heals readily, allows excellent visualization, allows access for medial tibial plateau elevation or physeal resection (if desired), fibular osteotomy and prophylactic partial fasciotomy (see below), and is cosmetically acceptable.
Fig. 2.
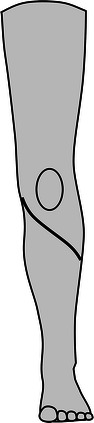
The incision currently favored for oblique proximal tibial osteotomy allows access to the medial tibial physis and lateral exposure for fibular osteotomy and partial fasciotomy
Angle of cut
It is theoretically possible to modify the extent of angular correction in each plane by varying the angle of cut in the sagittal plane [1, 2]. Most cases of Blount’s disease have equal degrees of tibia vara and tibial internal rotation. For this reason, variations from a 45° upward cut have not proven to be necessary. More acute angles are difficult to achieve, and the natural tendency for a surgeon is to make the cut slightly more transverse than the optimum cut.
Orienting the plane of cut
Informal reports from surgeons following the initial publication [2] mentioned that excessive procurvatum of the tibia (beyond that which is typical of Blount’s disease) was seen with larger angular corrections. While this can remodel and does not seem to be clinically troublesome, it is the result of an osteotomy plane that is started too laterally. The procurvatum can be improved by basing the approach for the plane of cut on the direction of the foot (internally rotated) and not the knee. In other words, the 45° upward cut should be made proximally, based on the coordinate system of the distal tibia, not the proximal (Fig. 3). Once rotated to the corrected position, the faces of the osteotomy may shorten several millimeters; this has not proven to be a problem.
Fig. 3.
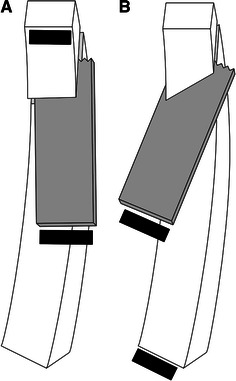
a Starting the oblique cut from the anterior surface of the upper tibia can lead to procurvatum with higher angles of correction. b This can be improved by orienting the starting plane to correspond with the distal, internally rotated tibial surface
Fluoroscopic imaging
Rather than using an image intensifier suspended over the patient, it is convenient and safe to simply bring a vertically oriented image intensifier beside the knee, tilt it slightly, and externally rotate the hip with the knee flexed to provide lateral views of the proximal tibia for guide pin positioning.
Fixation
The published technique used a screw that crossed the osteotomy site perpendicular to the plane of the cut. The reason for this was so that the cast could be removed and the corrected tibia could be rotated around the screw, to change the osteotomy position if needed. However, reducing the corrected position has not been necessary in clinical practice, as there have been no cases of compartment syndrome or vascular compromise requiring it. Modern management of compartment syndrome, should it occur, would involve fasciotomy that can be carried out through an extension of the lateral distal incision. It is effective to use two or three screws (usually cortical) inserted directly in an antero-posterior direction (Fig. 4). This more rigidly fixes the tibia and resists the shortening that an oblique screw might allow. An advantage of this is that the leg can then be examined clinically without applying valgus force, and any residual varus angulation caused by narrowing of the medial joint space can be appreciated and corrected, without relying on an arthrogram. The fixation using these screws eliminates the problem of undercorrection; there has been no loss of accepted correction using this limited fixation.
Fig. 4.
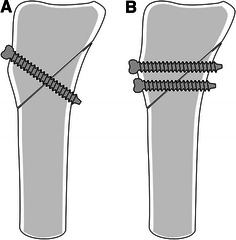
a Previously used fixation screw technique, while allowing positional adjustment, could allow shortening or instability. b Orienting fixation screws perpendicular to long axis of the tibia enhances stability and prevents shortening
Fibular osteotomy
Fibular osteotomy allows safer and easier correction into the valgus and should be done in all cases. It can be performed in the distal-most portion of the oblique incision described above. To reduce the exposure, the surgeon can use a large rongeur to grasp, twist, and break the fibula, rather than actually cutting it with a saw or osteotome.
Fasciotomy
Prophylactic fasciotomy of the proximal anterior compartment can be performed easily through the oblique incision. The proximal portion must be done carefully due to the proximity of the anterior tibial recurrent artery, and can be carried over the top of the muscle to include release of the periosteum behind it; the distal portion can be performed subcutaneously under the distal skin using long Metzenbaum scissors. This limited fasciotomy is performed on all patients. Prophylactic anterior compartment fasciotomy was felt to be a major technical factor in the avoidance of compartment syndrome in 30 tibial osteotomies in children reviewed by Pinkowski and Weiner [7].
Because of concerns for the development of compartment syndrome, spinal or regional blocks, which could mask the symptoms and delay the diagnosis, have not been used.
Drain
The original technique article described a drain. This practice was stopped shortly after publication of the paper, and there have been no observed problems related to its discontinuation.
Casting
Above-knee casts have been used for all osteotomies. These have rarely been uni-valved because of concern for instability; when this was performed, the cast is later re-wrapped before the patient leaves the hospital. In obese children, there is a potential for loss of position, since the proximal cast has poor control of a large thigh; however, this has not been observed. External fixation or rigid plate fixation of the osteotomy have not been used, although these are reasonable alternatives based on the surgeon’s preference.
Summary
Experience with oblique tibial osteotomy has led to minor technical modifications that make it easier to perform and more reliable. The most significant of these are the more medial direction for the oblique cut (oriented to the distal tibia) and the change in fixation to two or three transverse screws. The procedure has provided accurate and cosmetically satisfactory correction of all cases of tibia vara, no matter how severe.
Acknowledgments
The author gratefully acknowledges the support of the Ben Ali Shriners’ Chair in Pediatric Orthopedics.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Kruse RW, Bowen JR, Heithoff S. Oblique tibial osteotomy in the correction of tibial deformity in children. J Pediatr Orthop. 1989;9:476–482. doi: 10.1097/01241398-198907000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Rab GT. Oblique tibial osteotomy for Blount’s disease (tibia vara) J Pediatr Orthop. 1988;8:715–720. doi: 10.1097/01241398-198811000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Sangeorzan BP, Judd RP, Sangeorzan BJ. Mathematical analysis of single-cut osteotomy for complex long bone deformity. J Biomech. 1989;22:1271–1278. doi: 10.1016/0021-9290(89)90230-3. [DOI] [PubMed] [Google Scholar]
- 4.Paley D. Principles of deformity correction. Berlin: Springer-Verlag; 2002. pp. 256–268. [Google Scholar]
- 5.Sangeorzan BJ, Sangeorzan BP, Hansen ST, Jr, Judd RP. Mathematically directed single-cut osteotomy for correction of tibial malunion. J Orthop Trauma. 1989;3:267–275. doi: 10.1097/00005131-198912000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Morrissy RT, Weinstein SL, editors. Atlas of pediatric orthopaedic surgery. 3. Philadelphia: Lippincott Williams & Wilkins; 2001. pp. 665–670. [Google Scholar]
- 7.Pinkowski JL, Weiner DS. Complications in proximal tibial osteotomies in children with presentation of technique. J Pediatr Orthop. 1995;15:307–312. doi: 10.1097/01241398-199505000-00009. [DOI] [PubMed] [Google Scholar]


