SYNOPSIS
The past three years of research on materials for all-ceramic veneers, inlays, onlays, single-unit crowns, and multi-unit restorations are reviewed. The primary changes in the field were the proliferation of zirconia-based frameworks and computer-aided fabrication of prostheses, as well as, a trend toward more clinically relevant in vitro test methods. This report includes an overview of ceramic fabrication methods, suggestions for critical assessment of material property data, and a summary of clinical longevity for prostheses constructed of various materials.
BACKGROUND
Ceramic materials are best able to mimic the appearance of natural teeth. However, two obstacles have limited the use of ceramics in the fabrication of dental prostheses: 1) brittleness leading to a lack of mechanical reliability and 2) greater effort and time required for processing in comparison to metal alloys and dental composites. Recent advances in ceramic processing methods have simplified the work of the dental technician and have allowed greater quality control for ceramic materials, which has increased their mechanical reliability. As a result, the proportion of restorative treatments using all-ceramic prostheses is rapidly growing.
Several authors previously reviewed progress in the field of dental ceramics [1–12]. This article reviews the research literature and commercial changes over the past three years since the last review in this field. The recent developments in dental ceramic technology can be categorized into three primary trends:
There has been a rapid diversification of equipment and materials available for computer-aided design/computer-aided manufacturing (CAD-CAM) of ceramic prostheses.
The availability of CAD-CAM processing permitted the use of polycrystalline zirconia coping and framework materials. The relatively high stiffness and good mechanical reliability of partially stabilized zirconia allows thinner core layers, longer bridge spans, and the use of all-ceramic fixed partial dentures (FPDs) in posterior locations.
Basic science researchers are increasingly using clinically relevant specimen geometry, surface finish, and mechanical loading in their in vitro studies. This implies that in vitro results will more accurately predict clinical performance of ceramic prostheses, but clinicians still need to be cautious in extrapolating from the laboratory to the clinical case.
METHODS OF CERAMIC FABRICATION
A recent review of the literature included a taxonomy of dental ceramics, in which materials were categorized according to their composition and indications [4]. The following section is categorized by method of fabrication. This complements the previous review and reflects the recent diversification of CAD-CAM systems (Table 1). Ceramics having similar composition may be fabricated by different laboratory techniques, and each method of forming results in a different distribution of flaws, opportunity for depth of translucency, and accuracy of fit. These differences should be important to the clinician because they persist beyond the walls of the dental laboratory and affect clinical performance.
Table 1.
Methods of forming ceramics for all-ceramic prostheses.
| Fabrication Method | Commercial Examples | Composition |
|---|---|---|
| Powder condensation | Duceram LFCa | glass |
| Finesse Low Fusinga | leucite-glass | |
| IPS e.max Ceramb | fluoroapatite-glass | |
| IPS Erisb | fluoroapatite-glass | |
| LAVA Ceramc | leucite-glass | |
| Vita Dd | leucite-glass | |
| Vitadur Alphad | leucite-glass | |
| Vitadur Nd | alumina-glass | |
| Slip casting | In-Ceram Aluminad | glass-alumina |
| In-Ceram Spinelld | glass-alumina-spinel | |
| In-Ceram Zirconiad | glass-alumina-PS zirconia | |
| Hot pressing | Finesse All-Ceramica | leucite-glass |
| Fortress Pressablee | leucite-glass | |
| IPS Empressb | leucite-glass | |
| IPS Empress 2b | lithium disilicate-glass | |
| IPS e.max Pressb | lithium disilicate-glass | |
| IPS e.max ZirPressb | fluoroapatite-glass | |
| OPCf | leucite-glass | |
| CAD-CAM | ||
| Presintered | Cercona | partially stabilized zirconia |
| DC-Zirkong | partially stabilized zirconia | |
| Everest ZS-Blanksh | partially stabilized zirconia | |
| IPS e.max ZirCADb | partially stabilized zirconia | |
| LAVA Framec | partially stabilized zirconia | |
| Procera AllCerami | alumina | |
| Procera AllZirkoni | partially stabilized zirconia | |
| Vita YZd | partially stabilized zirconia | |
| Densely sintered | Denzirj | partially stabilized zirconia |
| Digiceram Lk | leucite-glass | |
| Digizonk | partially stabilized zirconia | |
| Everest G-Blanksh | leucite-glass | |
| Everest ZH-Blanksh | partially stabilized zirconia | |
| IPS e.max CADb | lithium disilicate-glass | |
| ProCADb | leucite-glass | |
| Vitablocs Mark IId | leucite-glass | |
| Vitablocs TriLuxed | leucite-glass | |
| ZirKonl | partially stabilized zirconia | |
| Glass infiltrated | In-Ceram Aluminad | glass-alumina |
| In-Ceram Spinelld | glass-alumina-spinel | |
| In-Ceram Zirconiad | glass-alumina-PS zirconia |
Dentsply-Ceramco, York, PA, USA;
Ivoclar-Vivadent, Schaan, Liechtenstein;
3M ESPE, St. Paul, MN, USA;
Vita Zahnfabrik, Bad Säckingen, Germany;
Mirage Dental Systems, Kansas City, KS, USA;
Pentron Clinical Technologies, Wallingford, CT, USA;
DCS Dentalsysteme, Kelkheim, Germany;
KaVo, Lake Zurich, IL, USA;
Nobel Biocare, Kloten, Switzerland;
Cad.esthetics, Skellefteå, Sweden;
Digident, Pforzheim, Germany;
Cynovad, Saint-Laurent, Canada
Powder Condensation
This traditional method of forming ceramic prostheses involves applying a moist porcelain powder with an artist’s brush and removing excess moisture to compact the powder particles. The porcelain is further compacted by viscous flow of the glassy component during firing under vacuum. This method results in a large amount of residual porosity. The crystalline particles that strengthen the material on a microscopic scale are not connected to each other but are separated by glassy regions. The porosity and discontinuous nature of the crystalline phase lead to relatively low strength and a wide variation in strength. Ceramics fabricated by powder condensation have greater translucency than can be achieved using other methods [13], so these materials are usually applied as the esthetic veneer layers on stronger cores and frameworks.
Slip Casting
A slip is a low viscosity slurry or mixture of ceramic powder particles suspended in a fluid (usually water). Slip casting involves forming a mold or negative replica of the desired framework geometry and pouring a slip into the mold. The mold is made of a material (usually gypsum) that extracts some water from the slip into the walls of the mold through capillary action, and some of the powder particles in the slip become compacted against the walls of the mold forming a thin layer of green ceramic that is to become the framework. The remaining slip is discarded, and the framework can be removed from the mold after partial sintering to improve the strength to a point where the framework can support its own weight. The resulting ceramic is very porous and must be either infiltrated with molten glass or fully sintered before veneering porcelain can be applied. Ceramics fabricated by slip casting can have higher fracture resistance than those produced by powder condensation because the strengthening crystalline particles form a continuous network throughout the framework. Use of this method in dentistry has been limited to one series of three products for glass infiltration (In-Ceram, Vita Zahnfabrik). The limited application of slip casting in dentistry is probably because the method requires a complicated series of steps, which provide a challenge to achieving accurate fit [14–16] and may result in internal defects that weaken the material from incomplete glass infiltration [17].
Hot Pressing
The lost wax method is used to fabricate molds for pressable dental ceramics. Pressable ceramics are available from manufacturers as prefabricated ingots made of crystalline particles distributed throughout a glassy material. The microstructure is similar that of powder porcelains, however, pressable ceramics do not contain much porosity and can have a higher crystalline content because the ingots are manufactured from non-porous glass ingots by applying a heat treatment that transforms some of the glass into crystals. This process can be expected to produce a well controlled and homogeneous material. In the dental laboratory, the pressable ingots are heated to a temperature at which they become a highly viscous liquid, and they are slowly pressed into the lost wax mold. The advantage of hot pressing is that dental technicians are already experienced at achieving good accuracy of fit using the lost wax method with metal alloys [15, 16]. Contrary to intuition, the higher crystalline content and lack of porosity do not lead to increased fracture resistance or decreased variability of strength [18]. Pressable ceramics usually have application only as core and framework materials. Pressable veneering materials, such as IPS e.max ZirPress (Ivoclar-Vivadent) are available, but the depth of layered esthetics may be limited when using pressable ceramics for veneering materials.
CAD-CAM
Like pressable ceramics, CAD-CAM ceramics are available as prefabricated ingots. These ingots are milled or cut by computer-controlled tools. In the case of presintered ceramics, the ingots are porous, which enables fast milling without bulk fracture of the ceramic. The disadvantage of presintered ingots is the need for subsequent sintering treatment to eliminate the porosity. The computer software must compensate for the shrinkage that occurs during sintering to achieve good accuracy of fit. Densely sintered ceramics are available in non-porous ingots, which are more difficult to mill, but they do not require any further sintering. Glass infiltrated CAD-CAM ingots have similar composition to slip cast ceramics, but starting with a porous ingot eliminates the complicated steps of slip casting. After milling, the porosity is eliminated by molten glass infiltration. One might question whether the milling process introduces surface cracks that weaken CAD-CAM ceramics, especially in the case of densely sintered ingots, but no evidence of this effect is available in the current literature [19]. Dental CAD-CAM systems have been available for 20 years. In recent years, the increasing use of polycrystalline alumina and zirconia as framework materials and the increasing popularity and variety of CAD-CAM systems seem to be mutually accelerating trends.
INTERPRETATION OF IN VITRO REPORTS
The results of in vitro tests reported in the scientific literature and in manufacturer’s advertisements may not be predictive of clinical performance, so it is important for clinicians to be familiar with the following trends and to critically assess materials performance data.
There were 189 in vitro studies published from 2004 to 2006 on materials for all-ceramic prostheses (Table 2). The majority of studies pertained to comparison of mechanical reliability, marginal adaptation, or bonding to resin cements of commercially available materials or the effects of varying fabrication protocols or surface treatments on these aspects of performance. Few studies were published regarding esthetic properties or the synthesis of novel ceramic compositions.
Table 2.
Common topics for in vitro dental ceramic studies (2004–2006).
| Method/Topic of Research | Number of Studies* |
|---|---|
| Layered specimen geometry | 70 (37%) |
| CAD-CAM fabrication | 70 (37%) |
| Surface roughness/defects | 57 (30%) |
| Cyclic mechanical/thermal loading | 51 (27%) |
| Ceramic-resin bond strength | 45 (24%) |
| Polycrystalline zirconia | 33 (17%) |
| Marginal adaptation/degradation | 24 (13%) |
| Contact loading | 22 (12%) |
| Weibull statistics | 22 (12%) |
| Polycrystalline alumina | 11 (6%) |
some studies were related to more than one of these methods/topics
Most notably there was a trend toward specimen geometry and loading conditions that better mimic the actual clinical situation. Many investigators have started testing multi-layered specimens with actual or simulated dentin, luting agent, core ceramic, and veneering ceramic layers. This is important because the surface treatments to prepare the core ceramic for application of the veneering ceramic have been shown to change the strength of the core ceramic [20], and the presence of the luting agent also has an effect on ceramic strength [21, 22]. In addition, differential contraction of the core and veneering ceramics upon cooling creates thermally induced stresses, which alters the resistance of prostheses to stresses induced by mechanical loading [23]. It is also important to load specimens in a manner that reproduces the failure modes observed in the clinic. This includes blunt contact loading, cyclic fatigue loading, and loading in an aqueous environment [24], although reproducing all of these conditions does not guarantee a clinically relevant failure mode. For example, a recent study on model glass-polymer systems showed that propagation of an “inner cone crack” from the contact surface results in bulk fracture of in vitro specimens [25], but analyses of clinically failed crowns show that bulk fracture originates from the core ceramic [26–28]. Edge chipping originating from wear on contact surfaces has been observed clinically [29, 30], and recent experiments with novel loading geometry have reproduced that failure mode in the laboratory [31, 32]. There will always be a need for some simple standard geometry specimens to study the micromechanisms associated with crack growth. However, clinicians should not assume that simple specimens are predictive of clinical performance. In other words, ceramic specimens that have been finely polished, tested dry, or loaded quickly can be expected to have much higher strength than prostheses fabricated from the same materials, and the relative ranking of commercial products may change depending on test method.
An area that has seen only modest improvement is the reporting of Weibull statistics to describe ceramic strength data. The failure load and strength of a ceramic prosthesis or test specimen is controlled by the size of the largest flaw in the highly stressed location – not the average flaw. This causes the distribution of ceramic strengths to be skewed toward the lower end (Fig. 1). The strengths fit a Weibull distribution instead of a Gaussian (normal) distribution, and the shape of the Weibull distribution can be described by the Weibull modulus and the stress corresponding to a particular probability of failure, such as the median strength (50% chance of failure) or the characteristic strength (63%). The Weibull modulus is a measure of variation in strength with higher Weibull modulus corresponding to less variation. The Weibull modulus can be more important than the median strength for predicting clinical performance because the Weibull modulus can be used to predict the effect of prosthesis size on strength and because it controls the stress level corresponding to low probabilities of failure. The median strength corresponds to a 50% chance of failure, but clinicians are not interested in such a high failure rate. Fig. 2 illustrates how an all-ceramic system with lower median strength and higher Weibull modulus can survive higher stress levels at low probability of failure (5%). A slowly increasing number of basic science researchers are reporting Weibull statistics, however, they usually lack sufficient number of specimens to accurately estimate the Weibull modulus. Most studies published in the past three years had six to 10 specimens per group, even though the recommended number is 30 per group [33]. If a study estimates a Weibull modulus of m=5 using a sample size of 10 specimens per group, then there is a 95% chance that the actual Weibull modulus for the restorative system is in the range 3.7–9.2 and a 5% chance that the true value is outside that range [34]. So, clinicians should be cautious and note the sample size when interpreting in vitro studies because a study may conclude no difference in Weibull modulus between groups when there is not enough statistical power to detect a difference.
Figure 1.
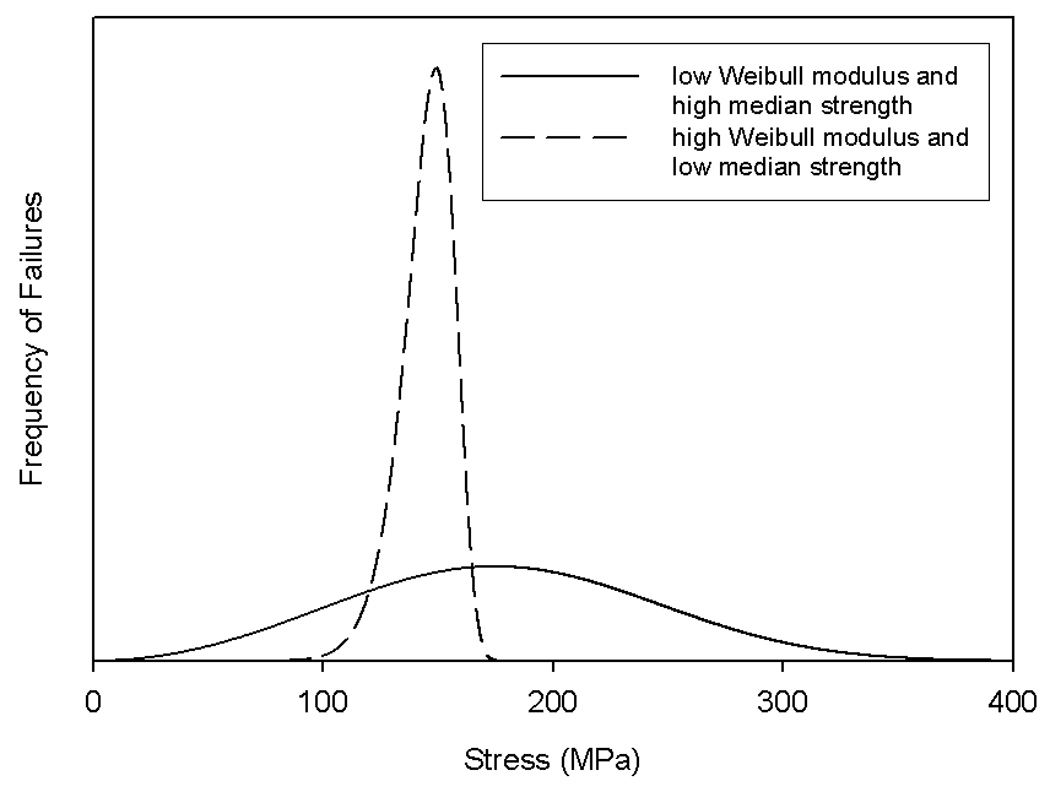
Strength distributions for prostheses fabricated from two hypothetical dental ceramics.
Figure 2.
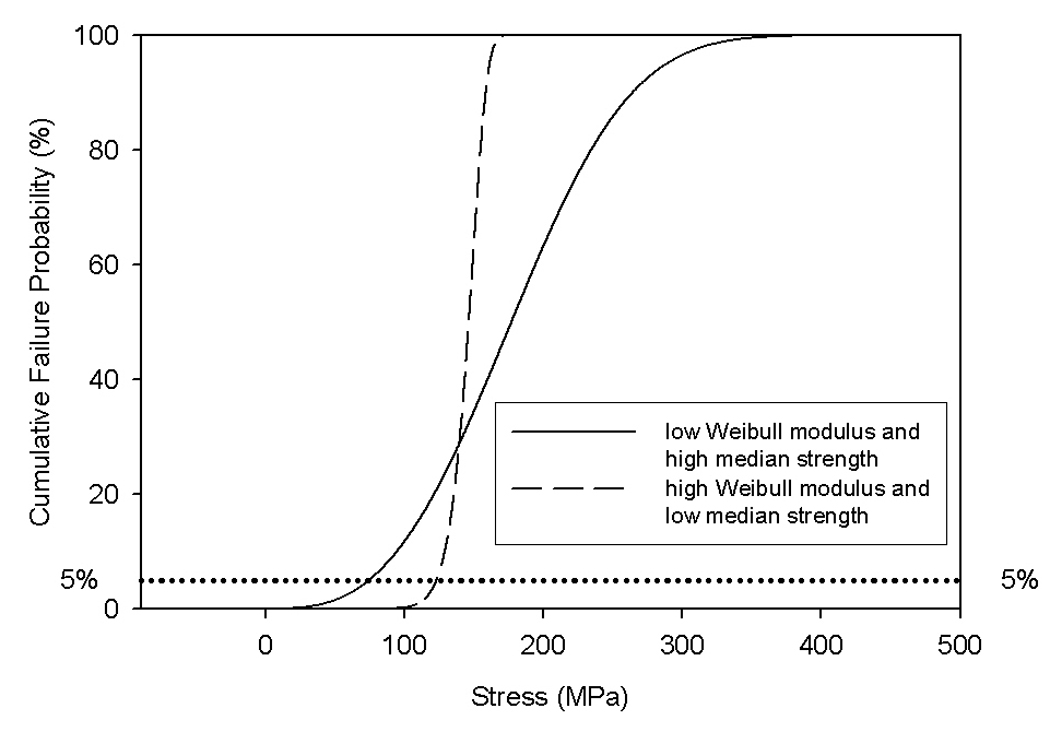
Cumulative failure probabilities for prostheses fabricated from two hypothetical dental ceramics.
SURVIVAL OF ALL-CERAMIC RESTORATIONS
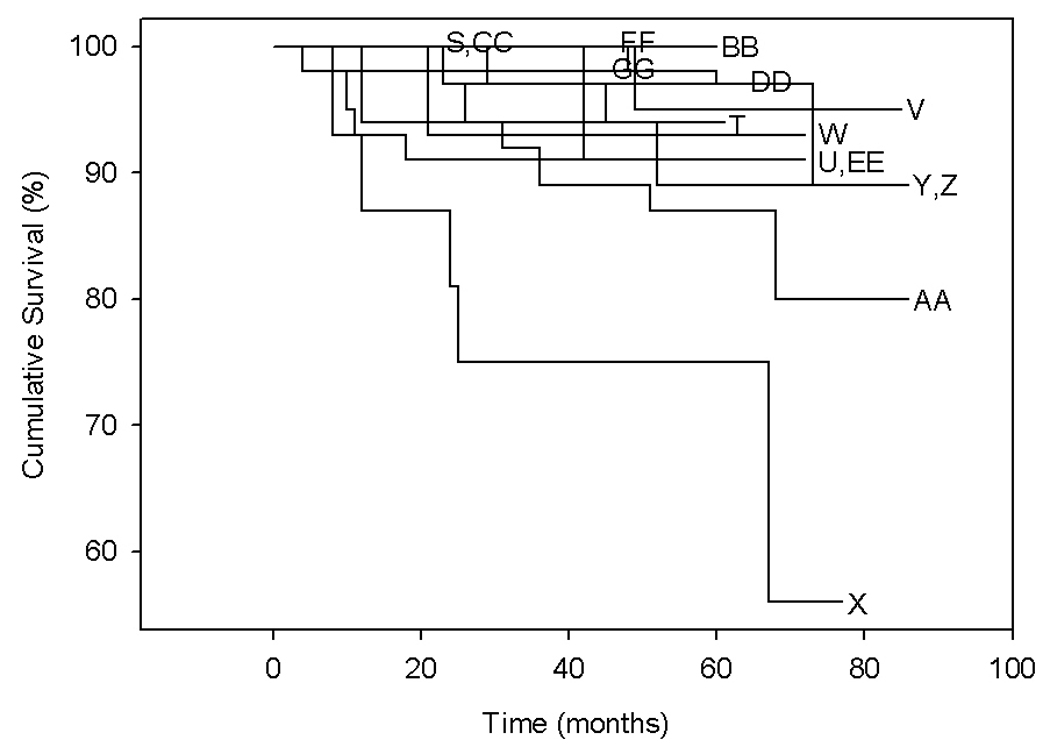
There were 34 clinical studies published from 2004 to 2006 on the longevity of all-ceramic restorations. It is important to analyze longevity data using Kaplan-Meier analysis [35] because simply dividing the number of failures observed by the total number of restorations placed results in artificially high reliability predictions [4]. Many of the reports did not provide sufficient details to perform the appropriate analysis, but those that did are separated here according to restoration type (veneer, inlay/onlay, crown, or FPD), and the cumulative survival probabilities are graphed in Fig. 3–Fig. 6. Table 3 [36–55] summarizes the experimental factors for those studies.
Figure 3.
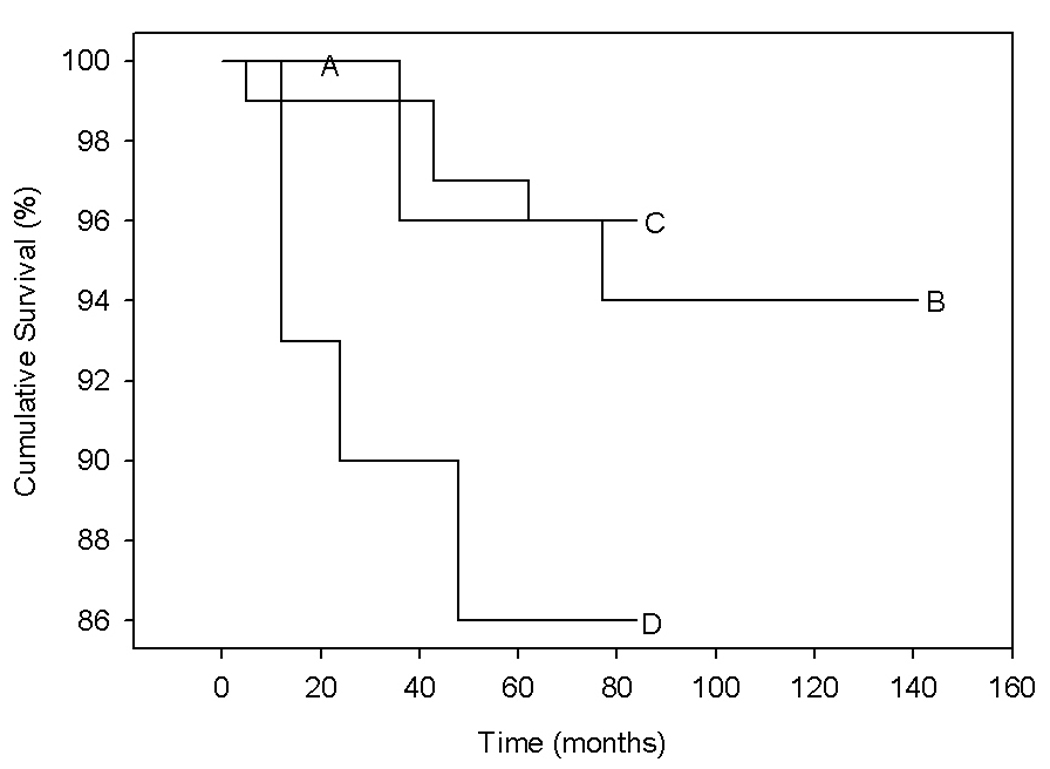
Cumulative survival probabilities for all-ceramic veneers over time calculated from data published in recent clinical studies.
Figure 6.
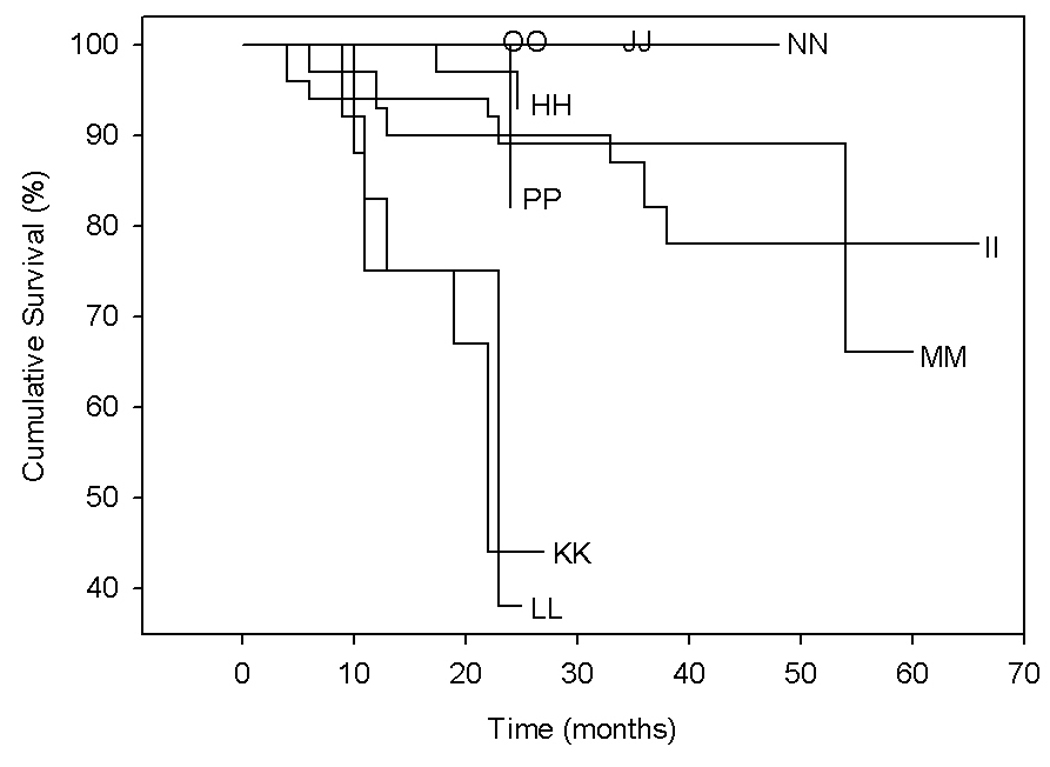
Cumulative survival probabilities for all-ceramic fixed partial dentures over time calculated from data published in recent clinical studies.
Table 3.
Clinical studies reporting longevity of all-ceramic restorations.
| Graph Label |
Reference | Framework Material |
Veneer Material |
Luting Agent |
Restoration Type |
Location | Support |
|---|---|---|---|---|---|---|---|
| A | Barnes [36] | Finesse All-Ceramic | Finesse | DC | veneer | anterior | NS |
| B | Fradeani [41] | IPS Empress | Vitadur Alpha | DC | veneer | anterior | NS |
| C | Smales [48] | Mirage | Mirage | DC | veneer | anterior | NS |
| D | Smales [48] | Mirage | none | DC | veneer | anterior | NS |
| E | Coelho Santos [39] | Duceram Plus | Duceram LFC | DC | inlay | posterior | NS |
| F | Coelho Santos [39] | IPS Empress | NS | DC | inlay | posterior | NS |
| G | Sjogren [47] | Vita Mark II | NS | SC | inlay | posterior | NS |
| H | Sjogren [47] | Vita Mark II | NS | DC | inlay | posterior | NS |
| I | Thordrup [51] | NS (CEREC) | NS | NS | inlay | posterior | NS |
| J | Thordrup [51] | Vitadur N | NS | NS | inlay | posterior | NS |
| K | Barnes [36] | Finesse Pressable | Finesse | DC | inlay/onlay | posterior | NS |
| L | Kramer [44] | IPS Empress | NS | NS | inlay/onlay | posterior | NS |
| M | Kramer [43] | IPS Empress | NS | DC,SE | inlay/onlay | posterior | NS |
| N | Kramer [43] | IPS Empress | NS | DC,ER | inlay/onlay | posterior | NS |
| O | Schulte [46] | IPS Empress | NS | LC | inlay/onlay | posterior | NS |
| P | Coelho Santos [39] | Duceram Plus | Duceram LFC | DC | onlay | posterior | NS |
| Q | Coelho Santos [39] | IPS Empress | NS | DC | onlay | posterior | NS |
| R | Kaytan [42] | IPS Empress | NS | DC | onlay | posterior | NS |
| S | Barnes [36] | Finesse Pressable | Finesse | DC | single-unit crown | NS | NS |
| T | Bindl [37] | Vita Mark II | none | DC | single-unit crown | anterior | NS |
| U | Bindl [37] | In-Ceram Spinell | Vitadur Alpha | DC | single-unit crown | anterior | NS |
| V | Bindl [38] | Vita Mark II | NS | DC | single-unit crown | posterior | classic premolar |
| W | Bindl [38] | Vita Mark II | NS | DC | single-unit crown | posterior | reduced premolar |
| X | Bindl [38] | Vita Mark II | NS | DC | single-unit crown | posterior | endo. premolar |
| Y | Bindl [38] | Vita Mark II | NS | DC | single-unit crown | posterior | classic molar |
| Z | Bindl [38] | Vita Mark II | NS | DC | single-unit crown | posterior | reduced molar |
| AA | Bindl [38] | Vita Mark II | NS | DC | single-unit crown | posterior | endo. molar |
| BB | Marquardt [45] | IPS Empress 2 | IPS Eris | DC | single-unit crown | NS | NS |
| CC | Taskonak [50] | IPS Empress 2 | NS | DC | single-unit crown | NS | NS |
| DD | Walter [53] | Procera AllCeram | NS | GIC | single-unit crown | anterior | NS |
| EE | Walter [53] | Procera AllCeram | NS | GIC | single-unit crown | posterior | NS |
| FF | Zarone [55] | Procera AllCeram | NS | mod GIC | single-unit crown | anterior | natural tooth |
| GG | Zarone [55] | Procera AllCeram | NS | mod GIC | single-unit crown | anterior | implant |
| HH | Esquivel-Upshaw [40] | IPS Empress 2 | NS | NS | three-unit FPD | posterior | NS |
| II | Marquardt [45] | IPS Empress 2 | IPS Eris | DC | three-unit FPD | NS | NS |
| JJ | Suarez [49] | In-Ceram Zirconia | NS | NS | three-unit FPD | posterior | NS |
| KK | Taskonak [50] | IPS Empress 2 | NS | DC | three-unit FPD | anterior | NS |
| LL | Taskonak [50] | IPS Empress 2 | NS | DC | three-unit FPD | posterior | NS |
| MM | Wolfart [54] | IPS e.max Press | stain | NS | three-unit FPD | NS | NS |
| NN | Wolfart [54] | IPS e.max Press | stain | DC | three-unit FPD | posterior | NS |
| OO | Vult von Steyern [52] | DC-Zirkon | Vita D | ZP | five-unit FPD | anterior | NS |
| PP | Vult von Steyern [52] | DC-Zirkon | Vita D | ZP | five-unit FPD | posterior | NS |
NS indicates experimental factor was not specified or was not separated in the presentation of results
LC = light-cure resin cement, SC = self-cure resin cement, DC = dual-cure resin cement, GIC = glass-ionomer cement, mod GIC = resin-modified glass ionomer cement, ZP = zinc phosphate cement, SE = self-etch adhesive, ER = etch-and-rinse adhesive
Fig. 3 shows the survival of porcelain veneers over time. Groups C and D were part of a study to determine the effect of incisal porcelain on veneer longevity [48]. Group D veneers had no incisal porcelain and exhibited much shorter lifetimes than Group C veneers, which had incisal porcelain, and veneers from other studies. It is also noteworthy that the only groups with 100% short term survival (36 months) were veneers with a layer of pressable ceramic.
Fig. 4 shows the survival of all-ceramic inlays and onlays over time. All of the groups have similar short term survival. The most distinct trend is that long term survival was related to ceramic fabrication method. The highest long term survival probability (Groups F, L, M, N, and O) corresponded to inlays and onlays made from pressable ceramics. Groups H and I had the next highest long term survival and were both made from CAD-CAM ceramics. The lowest long term survival probability (Group J) corresponded to inlays made by powder condensation.
Figure 4.
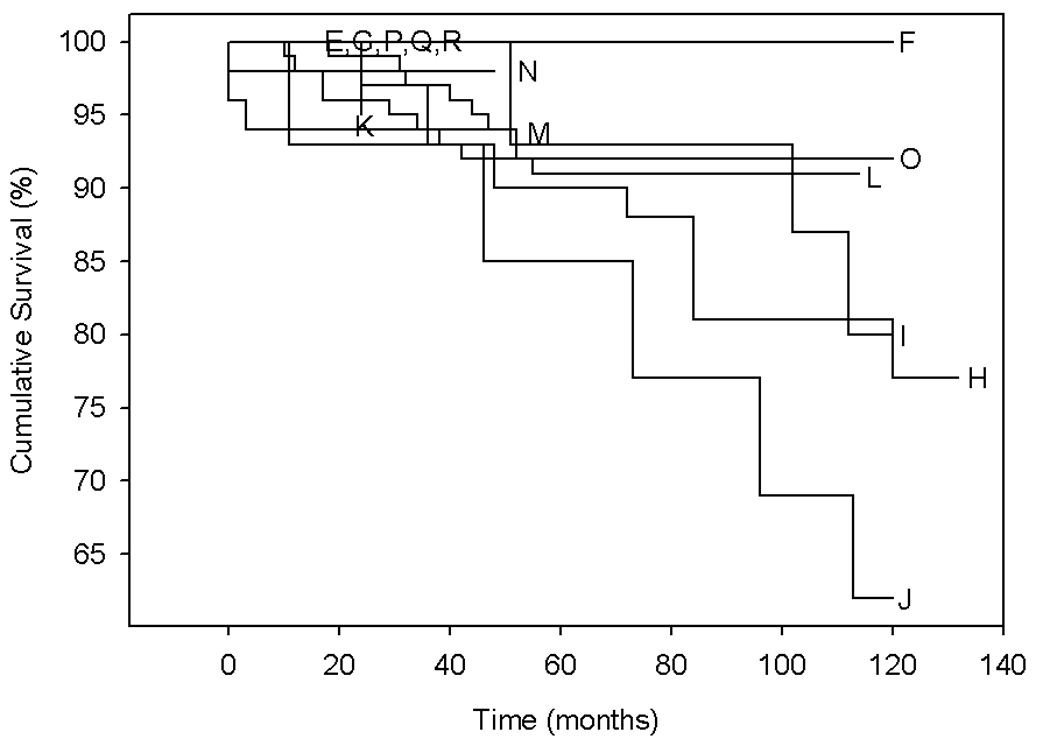
Cumulative survival probabilities for all-ceramic inlays and onlays over time calculated from data published in recent clinical studies.
Fig. 5 shows the survival of single-unit crowns over time. Groups X and AA showed much poorer longevity than the other groups. These crowns were part of a study to determine the effect tooth preparation on CAD-CAM crowns (Vita Mark II, Vita Zahnfabrik) [38]. Crowns in Groups V and Y were placed on teeth with sufficient healthy tissue for a classic crown preparation. Groups W and Z were placed on preparations with a reduced stump height. The shortest lived crowns (Group X) were placed on endodontically treated premolars, and the next shortest lived crowns (Group AA) were placed on endodontically treated molars. Another interesting observation is that anterior crowns (Groups T and U) performed similarly to posterior crowns even though lower biting forces, and hence longer prosthesis survival, are expected in the anterior.
Figure 5.
Cumulative survival probabilities for all-ceramic crowns over time calculated from data published in recent clinical studies.
Fig. 6 shows the survival of fixed partial dentures over time. The expected anterior-posterior relationship was observed here. Five-unit zirconia FPDs exhibited higher survival probability in anterior locations (Group OO) than in posterior locations (Group PP) [52]. Likewise, three-unit glass-ceramic FPDs exhibited higher survival probability in the anterior (Group KK) than the posterior (Group LL) [50]. This effect is not evident for another pressable glass-ceramic (Groups MM and NN), but it may have been confounded by the other experimental factors, such as glass ionomer cement in the anterior vs. resin-based cement in the posterior. In fact, debonding was the primary cause of failure in that study [54]. The IPS Empress 2 FPDs (Group KK and LL) had such poor performance because specimens in that study had smaller connector dimensions than recommended by the manufacturer [56].
Instead of ceramic fracture data, some studies reported survival in terms of percentage of restorations scoring “excellent” or “alpha” ratings at followup in each of the following categories: color match, marginal adaptation, marginal staining, secondary caries, and postoperative sensitivity. Most of those studies showed a lack of color match as the primary cause of low ratings at placement and marginal deterioration (staining and lack of adaptation) as the primary problem at followup [36, 41, 42, 57]. Hayashi et al. [58] collected more detailed observations on marginal deterioration than other investigators. They reported rapid wear of resin-based cements during the first six to 21 months followed by a period of little change. At 72 months, inlay margins were widened by a rapid progression of ceramic microfractures.
REFERENCES
- 1.Anusavice KJ. Recent developments in restorative dental ceramics. J Am Dent Assoc. 1993 Feb;124(2):72–74. 6–8, 80–84. doi: 10.14219/jada.archive.1993.0031. [DOI] [PubMed] [Google Scholar]
- 2.Deany IL. Recent advances in ceramics for dentistry. Crit Rev Oral Biol Med. 1996;7(2):134–143. doi: 10.1177/10454411960070020201. [DOI] [PubMed] [Google Scholar]
- 3.Hayashi M, Wilson NH, Yeung CA, Worthington HV. Systematic review of ceramic inlays. Clin Oral Investig. 2003 Mar;7(1):8–19. doi: 10.1007/s00784-002-0186-z. [DOI] [PubMed] [Google Scholar]
- 4.Kelly JR. Dental ceramics: current thinking and trends. Dent Clin North Am. 2004 Apr;48(2):viii, 513–530. doi: 10.1016/j.cden.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Kelly JR, Nishimura I, Campbell SD. Ceramics in dentistry: historical roots and current perspectives. J Prosthet Dent. 1996 Jan;75(1):18–32. doi: 10.1016/s0022-3913(96)90413-8. [DOI] [PubMed] [Google Scholar]
- 6.Martin N, Jedynakiewicz NM. Clinical performance of CEREC ceramic inlays: a systematic review. Dent Mater. 1999 Jan;15(1):54–61. doi: 10.1016/s0109-5641(99)00014-7. [DOI] [PubMed] [Google Scholar]
- 7.McLean JW. Evolution of dental ceramics in the twentieth century. J Prosthet Dent. 2001 Jan;85(1):61–66. doi: 10.1067/mpr.2001.112545. [DOI] [PubMed] [Google Scholar]
- 8.Mormann WH, Bindl A. All-ceramic, chair-side computer-aided design/computer-aided machining restorations. Dent Clin North Am. 2002 Apr;46(2):405–426. viii. doi: 10.1016/s0011-8532(01)00007-6. [DOI] [PubMed] [Google Scholar]
- 9.Peumans M, Van Meerbeek B, Lambrechts P, Vanherle G. Porcelain veneers: a review of the literature. J Dent. 2000 Mar;28(3):163–177. doi: 10.1016/s0300-5712(99)00066-4. [DOI] [PubMed] [Google Scholar]
- 10.Piddock V, Qualtrough AJ. Dental ceramics--an update. J Dent. 1990 Oct;18(5):227–235. doi: 10.1016/0300-5712(90)90019-b. [DOI] [PubMed] [Google Scholar]
- 11.Qualtrough AJ, Piddock V. Ceramics update. J Dent. 1997 Mar;25(2):91–95. doi: 10.1016/s0300-5712(96)00018-8. [DOI] [PubMed] [Google Scholar]
- 12.Raigrodski AJ. Contemporary all-ceramic fixed partial dentures: a review. Dent Clin North Am. 2004 Apr;48(2):viii, 531–544. doi: 10.1016/j.cden.2003.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Antonson SA, Anusavice KJ. Contrast ratio of veneering and core ceramics as a function of thickness. Int J Prosthodont. 2001 Jul–Aug;14(4):316–320. [PubMed] [Google Scholar]
- 14.Pallis K, Griggs JA, Woody RD, Guillen GE, Miller AW. Fracture resistance of three all-ceramic restorative systems for posterior applications. J Prosthet Dent. 2004 Jun;91(6):561–569. doi: 10.1016/j.prosdent.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 15.Sulaiman F, Chai J, Jameson LM, Wozniak WT. A comparison of the marginal fit of In-Ceram, IPS Empress, and Procera crowns. Int J Prosthodont. 1997 Sep–Oct;10(5):478–484. [PubMed] [Google Scholar]
- 16.Yeo IS, Yang JH, Lee JB. In vitro marginal fit of three all-ceramic crown systems. J Prosthet Dent. 2003 Nov;90(5):459–464. doi: 10.1016/j.prosdent.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 17.Griggs JA, Taskonak B, Mecholsky JJ, Jr, Yan J-H. American Association for Dental Research. Orlando, FL: 2006. Reliability model for framework ceramic with multiple flaw populations. [Google Scholar]
- 18.Tinschert J, Zwez D, Marx R, Anusavice KJ. Structural reliability of alumina-, feldspar-, leucite-, mica- and zirconia-based ceramics. J Dent. 2000 Sep;28(7):529–535. doi: 10.1016/s0300-5712(00)00030-0. [DOI] [PubMed] [Google Scholar]
- 19.Sundh A, Sjogren G. Fracture resistance of all-ceramic zirconia bridges with differing phase stabilizers and quality of sintering. Dent Mater. 2006 Aug;22(8):778–784. doi: 10.1016/j.dental.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 20.Carrier DD, Kelly JR. In-Ceram failure behavior and core-veneer interface quality as influenced by residual infiltration glass. J Prosthodont. 1995 Dec;4(4):237–242. doi: 10.1111/j.1532-849x.1995.tb00348.x. [DOI] [PubMed] [Google Scholar]
- 21.Fleming GJ, Maguire FR, Bhamra G, Burke FM, Marquis PM. The strengthening mechanism of resin cements on porcelain surfaces. J Dent Res. 2006 Mar;85(3):272–276. doi: 10.1177/154405910608500313. [DOI] [PubMed] [Google Scholar]
- 22.Rosenstiel SF, Gupta PK, Van der Sluys RA, Zimmerman MH. Strength of a dental glass-ceramic after surface coating. Dent Mater. 1993 Jul;9(4):274–279. doi: 10.1016/0109-5641(93)90074-z. [DOI] [PubMed] [Google Scholar]
- 23.Taskonak B, Mecholsky JJ, Jr, Anusavice KJ. Residual stresses in bilayer dental ceramics. Biomaterials. 2005 Jun;26(16):3235–3241. doi: 10.1016/j.biomaterials.2004.08.025. [DOI] [PubMed] [Google Scholar]
- 24.Kelly JR. Clinically relevant approach to failure testing of all-ceramic restorations. J Prosthet Dent. 1999 Jun;81(6):652–661. doi: 10.1016/s0022-3913(99)70103-4. [DOI] [PubMed] [Google Scholar]
- 25.Zhang Y, Song JK, Lawn BR. Deep-penetrating conical cracks in brittle layers from hydraulic cyclic contact. J Biomed Mater Res B Appl Biomater. 2005 Apr;73(1):186–193. doi: 10.1002/jbm.b.30195. [DOI] [PubMed] [Google Scholar]
- 26.Kelly JR, Campbell SD, Bowen HK. Fracture-surface analysis of dental ceramics. J Prosthet Dent. 1989 Nov;62(5):536–541. doi: 10.1016/0022-3913(89)90075-9. [DOI] [PubMed] [Google Scholar]
- 27.Quinn JB, Quinn GD, Kelly JR, Scherrer SS. Fractographic analyses of three ceramic whole crown restoration failures. Dent Mater. 2005 Oct;21(10):920–929. doi: 10.1016/j.dental.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 28.Thompson JY, Anusavice KJ, Naman A, Morris HF. Fracture surface characterization of clinically failed all-ceramic crowns. J Dent Res. 1994 Dec;73(12):1824–1832. doi: 10.1177/00220345940730120601. [DOI] [PubMed] [Google Scholar]
- 29.Scherrer SS, Quinn JB, Quinn GD, Kelly JR. Failure analysis of ceramic clinical cases using qualitative fractography. Int J Prosthodont. 2006 Mar–Apr;19(2):185–192. [PubMed] [Google Scholar]
- 30.Scherrer SS, Quinn JB, Quinn GD, Wiskott HW. Fractographic ceramic failure analysis using the replica technique. Dent Mater. 2007 Jan 30; doi: 10.1016/j.dental.2006.12.002. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flanders LA, Quinn JB, Wilson OC, Jr, Lloyd IK. Scratch hardness and chipping of dental ceramics under different environments. Dent Mater. 2003 Dec;19(8):716–724. doi: 10.1016/s0109-5641(03)00018-6. [DOI] [PubMed] [Google Scholar]
- 32.Qasim T, Ford C, Bush MB, Hu X, Malament KA, Lawn BR. Margin failures in brittle dome structures: Relevance to failure of dental crowns. J Biomed Mater Res B Appl Biomater. 2005 August 29; doi: 10.1002/jbm.b.30571. published online. [DOI] [PubMed] [Google Scholar]
- 33.ASTM. Annual Book of ASTM Standards. Philadelphia, PA: American Society for Testing Materials; 2006. C1239-06a Standard Practice for Reporting Uniaxial Strength Data and Estimating Weibull Distribution Parameters for Advanced Ceramics; pp. 309–315. [Google Scholar]
- 34.Thoman DR, Bain LJ, Antle CE. Inferences on the parameters of the Weibull distribution. Technometrics. 1969;11:445–460. [Google Scholar]
- 35.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. Journal of the American Statistical Association. 1958;53:457–481. [Google Scholar]
- 36.Barnes D, Gingell JC, George D, Adachi E, Jefferies S, Sundar V. Clinical evaluation of an all-ceramic restorative system: 24-month report. Am J Dent. 2006 Aug;19(4):206–210. [PubMed] [Google Scholar]
- 37.Bindl A, Mormann WH. Survival rate of mono-ceramic and ceramic-core CAD/CAM-generated anterior crowns over 2–5 years. Eur J Oral Sci. 2004 Apr;112(2):197–204. doi: 10.1111/j.1600-0722.2004.00119.x. [DOI] [PubMed] [Google Scholar]
- 38.Bindl A, Richter B, Mormann WH. Survival of ceramic computer-aided design/manufacturing crowns bonded to preparations with reduced macroretention geometry. Int J Prosthodont. 2005 May–Jun;18(3):219–224. [PubMed] [Google Scholar]
- 39.Coelho Santos MJ, Mondelli RF, Lauris JR, Navarro MF. Clinical evaluation of ceramic inlays and onlays fabricated with two systems: two-year clinical follow up. Oper Dent. 2004 Mar–Apr;29(2):123–130. [PubMed] [Google Scholar]
- 40.Esquivel-Upshaw JF, Anusavice KJ, Young H, Jones J, Gibbs C. Clinical performance of a lithia disilicate-based core ceramic for three-unit posterior FPDs. Int J Prosthodont. 2004 Jul–Aug;17(4):469–475. [PubMed] [Google Scholar]
- 41.Fradeani M, Redemagni M, Corrado M. Porcelain laminate veneers: 6- to 12-year clinical evaluation--a retrospective study. Int J Periodontics Restorative Dent. 2005 Feb;25(1):9–17. [PubMed] [Google Scholar]
- 42.Kaytan B, Onal B, Pamir T, Tezel H. Clinical evaluation of indirect resin composite and ceramic onlays over a 24-month period. Gen Dent. 2005 Sep–Oct;53(5):329–334. [PubMed] [Google Scholar]
- 43.Kramer N, Ebert J, Petschelt A, Frankenberger R. Ceramic inlays bonded with two adhesives after 4 years. Dent Mater. 2006 Jan;22(1):13–21. doi: 10.1016/j.dental.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 44.Kramer N, Frankenberger R. Clinical performance of bonded leucite-reinforced glass ceramic inlays and onlays after eight years. Dent Mater. 2005 Mar;21(3):262–271. doi: 10.1016/j.dental.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 45.Marquardt P, Strub JR. Survival rates of IPS empress 2 all-ceramic crowns and fixed partial dentures: results of a 5-year prospective clinical study. Quintessence Int. 2006 Apr;37(4):253–259. [PubMed] [Google Scholar]
- 46.Schulte AG, Vockler A, Reinhardt R. Longevity of ceramic inlays and onlays luted with a solely light-curing composite resin. J Dent. 2005 May;33(5):433–442. doi: 10.1016/j.jdent.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 47.Sjogren G, Molin M, van Dijken JW. A 10-year prospective evaluation of CAD/CAM-manufactured (Cerec) ceramic inlays cemented with a chemically cured or dual-cured resin composite. Int J Prosthodont. 2004 Mar–Apr;17(2):241–246. [PubMed] [Google Scholar]
- 48.Smales RJ, Etemadi S. Long-term survival of porcelain laminate veneers using two preparation designs: a retrospective study. Int J Prosthodont. 2004 May–Jun;17(3):323–326. [PubMed] [Google Scholar]
- 49.Suarez MJ, Lozano JF, Paz Salido M, Martinez F. Three-year clinical evaluation of In-Ceram Zirconia posterior FPDs. Int J Prosthodont. 2004 Jan–Feb;17(1):35–38. [PubMed] [Google Scholar]
- 50.Taskonak B, Sertgoz A. Two-year clinical evaluation of lithia-disilicate-based all-ceramic crowns and fixed partial dentures. Dent Mater. 2005 Dec 19; doi: 10.1016/j.dental.2005.11.028. published online. [DOI] [PubMed] [Google Scholar]
- 51.Thordrup M, Isidor F, Horsted-Bindslev P. A prospective clinical study of indirect and direct composite and ceramic inlays: ten-year results. Quintessence Int. 2006 Feb;37(2):139–144. [PubMed] [Google Scholar]
- 52.Vult von Steyern P, Carlson P, Nilner K. All-ceramic fixed partial dentures designed according to the DC-Zirkon technique. A 2-year clinical study. J Oral Rehabil. 2005 Mar;32(3):180–187. doi: 10.1111/j.1365-2842.2004.01437.x. [DOI] [PubMed] [Google Scholar]
- 53.Walter MH, Wolf BH, Wolf AE, Boening KW. Six-year clinical performance of all-ceramic crowns with alumina cores. Int J Prosthodont. 2006 Mar–Apr;19(2):162–163. [PubMed] [Google Scholar]
- 54.Wolfart S, Bohlsen F, Wegner SM, Kern M. A preliminary prospective evaluation of all-ceramic crown-retained and inlay-retained fixed partial dentures. Int J Prosthodont. 2005 Nov–Dec;18(6):497–505. [PubMed] [Google Scholar]
- 55.Zarone F, Sorrentino R, Vaccaro F, Russo S, De Simone G. Retrospective clinical evaluation of 86 Procera AllCeram anterior single crowns on natural and implant-supported abutments. Clin Implant Dent Relat Res. 2005;7 Suppl 1:S95–0. doi: 10.1111/j.1708-8208.2005.tb00081.x. [DOI] [PubMed] [Google Scholar]
- 56.Taksonak B. 2006 [Google Scholar]
- 57.Reich SM, Wichmann M, Rinne H, Shortall A. Clinical performance of large, all-ceramic CAD/CAM-generated restorations after three years: a pilot study. J Am Dent Assoc. 2004 May;135(5):605–612. doi: 10.14219/jada.archive.2004.0248. [DOI] [PubMed] [Google Scholar]
- 58.Hayashi M, Tsubakimoto Y, Takeshige F, Ebisu S. Analysis of longitudinal marginal deterioration of ceramic inlays. Oper Dent. 2004 Jul–Aug;29(4):386–391. [PubMed] [Google Scholar]


