Introduction
Obesity has received considerable attention as a major health hazard. This review aims at describing some of the epidemiological features of obesity including global prevalence, secular trends, risk factors, and burden of illness related to obesity. We have placed special emphasis on obesity trends in the United States.
Definitions for Overweight and Obesity
The “reference” measures of body composition include densitometry, single-cut imaging of the abdomen using computed tomography scan or magnetic resonance imaging, and dual-energy X-ray absorptiometry, but these methods are used mostly for research purposes. Body mass index (BMI), defined as the weight in kilograms divided by the height in meters squared (kg/m2), is the most widely used measure of obesity due to its low cost and simplicity. The World Health Organization (WHO) and the National Institutes of health (NIH)1, 2 have defined overweight as having a BMI between 25.0 and 29.9 kg/m2; and obesity as having a BMI greater than 30.0 kg/m2. In the United States, criteria for overweight in children are based on the 2000 U.S. Centers for Disease Control and Prevention (CDC) BMI-for-age growth charts. Overweight is defined as at or above the age-specific 95% BMI percentile. At risk for overweight is defined as having a BMI between 85th–95th percentiles of the BMI-for-age growth charts.3
However, increasing evidence suggests that abdominal obesity, rather than total body fat, is also a useful, independent predictor of several cardiovascular- and cancer-related outcomes.2 Some of the commonly used measures of abdominal obesity are waist circumference, hip circumference, and waist-to-hip ratio.
Obesity Trend in Adults and Children
We will review a few important sources of epidemiological data on obesity in the United States.
The Behavioral Risk Factor Surveillance System (BRFSS) is a state-based cross-sectional random telephone survey of the US population aged ≥18 years. At the time of the survey, BMI was calculated from self-reported weight and height.3 The 2008 BRFSS data show considerable differences in the prevalence of obesity across states. Five states (Alabama, Mississippi, Oklahoma, Tennessee, and West Virginia) had a prevalence of obesity equal to or greater than 30%, and 32 states had a prevalence of obesity equal to or greater than 25%. For comparison, in 1990, no states had a prevalence of obesity greater than 15%; ten states had a prevalence of obesity less than 10% and the rest had an obesity prevalence of 10–15%.3
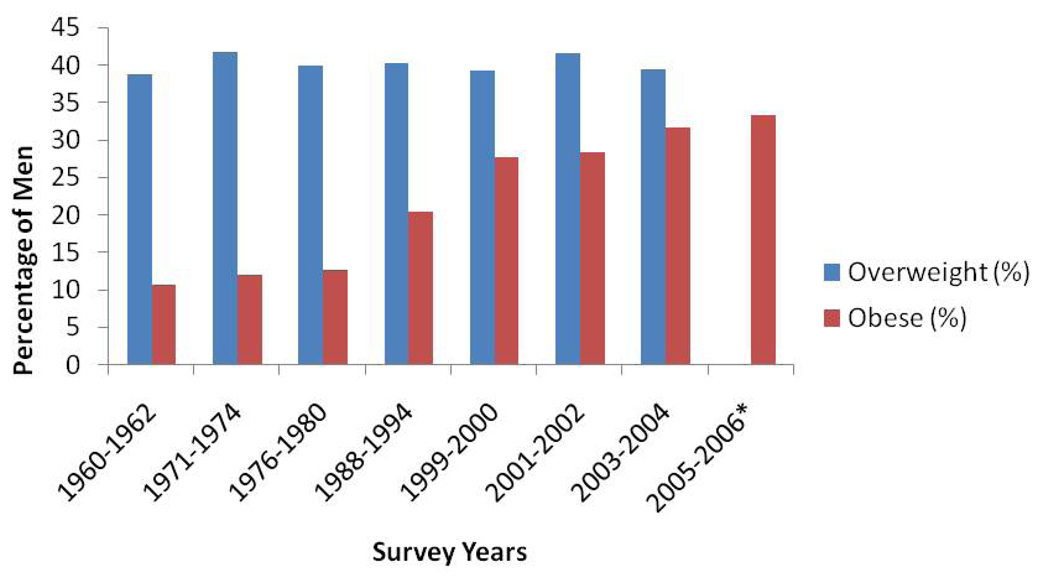
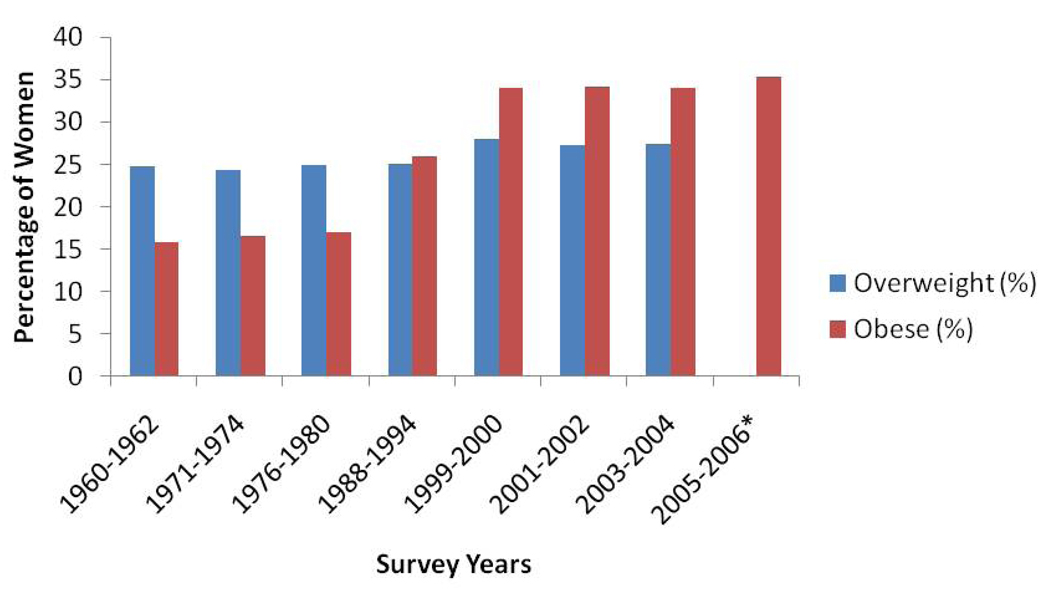
The National Health and Nutrition Examination Survey (NHANES) is another cross-sectional, nationally representative series of surveys conducted by the National Center for Health Statistics of the U.S. Centers for Disease Control and Prevention. All surveys included a standardized physical examination conducted in a mobile examination center with measurement of weight and height, using standardized protocols.4, 5 According to NHANES data in 2003–2004, 66.2% of U.S. adults 20–74 years old were either overweight or obese, 33.4% were overweight and 32.9% were obese. More recent data from NHANES show no significant changes in the prevalence of obesity for either men or women between 2003–2004 and 2005–2006 (Fig 1 and 2).6, 7 This possible stabilization in the obesity trends may be an early sign of a plateau in the obesity epidemic. The obesity prevalence was relatively low and stable between 1960 and 1980, but more than doubled from 15% in 1980 to 34% in 2006 6, 7
Figure 1.
Prevalence and Trends of Overweight and Obesity Among men Ages 20–74 Years in the United States: 1960–2006
* Included all people older than 20 years of age, only data in obese category are available.
Figure 2.
Prevalence and Trends of Overweight and Obesity Among Women Ages 20–74 Years in the United States: 1960–2006
* Included all people older than 20 years of age, only data in obese category are available.
Data from NHANES show large ethnic differences in the prevalence of obesity, but do not include an adequate number of minorities other than African American and Mexican American. Based on the data from NHANES 2003–2004, African Americans had the highest obesity prevalence of 45% for men and women between 20 and 74 years of age; the obesity prevalence was 30.6% for Caucasians and 36.8% for Mexican Americans.7 The data from NHANES 2005–2006 show large differences in obesity prevalence by ethnic group among women 40–59 years of age, but not significant difference by ethnic group among men. Approximately 53% of African American women and 51% of Mexican American women were obese, compared with 39% Caucasian women6.
Overweight Trends in U.S. Children
National estimates of overweight or obesity in children based on the NHANES data show that in 2003–2006, 31.9% of children 2–19 years old had a BMI at or above the 85th percentile of the 2000 CDC BMI-for-age growth charts, and 16.3% were at or above the 95th percentile of BMI for age. The most recent data from NHANES show no significant changes in the prevalence of obesity for children 2–19 years of age between 2003–2004 and 2005–2006.8 The overweight prevalence changed dramatically between 1980 and 2006 for children 2–19 years of age, increasing from 5.5% to 16.3%.
Global Trends of Obesity
The current epidemic of obesity has been reported in several but not all regions globally. The highest rate of obesity has been reported in the Pacific Islands and the lowest rates have been seen in Asia. The rates in Europe and North American are generally high, while the rates in Africa and Middle Eastern countries are variable.9 The prevalence of obesity around the world is monitored by the WHO through the Global Database on BMI. The survey data included in the database are identified from the literature or from a wide network of collaborators. However, high quality data from systematic nationally representative samples is sparse. As of November 2004, the database has compiled data covering approximately 86% of the adult population worldwide.1 The WHO estimates that in 2005 approximately 1.6 billion people worldwide were overweight and that at least 400 million adults were obese. They further project that, by 2015, approximately 2.3 billion adults will be overweight and that at least 700 million will be obese. According to the data from the Global Database on Body Mass Index, there are wide variations in the prevalence of obesity throughout the world, ranging from India, where 1% or less of the population is obese, to the Pacific Islands, where the prevalence of obesity can reach up to 80% in some regions.1
The change over time in adult obesity prevalence was calculated for 28 countries that have two or more nationally representative surveys recorded in the Global Database on BMI. Overall, most countries have rising trends of obesity. Only two of the 28 countries showed a falling trend in the prevalence of obesity in men (Denmark and Saudi Arabia), and five of the 28 countries showed a falling trend in the prevalence of obesity in women (Denmark, Ireland, Saudi Arabia, Finland, and Spain).10
Possible Causes of the Obesity Epidemic
Obesity is caused by a complex interaction between the environment, genetic predisposition, and human behavior.
Environmental factors are likely to be major contributors to the obesity epidemic. It is certain that obesity develops when there is a positive imbalance between energy intake and energy expenditure, but the relative contribution of these factors is poorly understood. Evidence supports the contribution of both excess energy intake and decreased energy expenditure in the obesity epidemic.11–13 Kant et al. used dietary data from four consecutive NHANES studies consisting of 39,094 adults in the United States to show that the temporal trends in the increase of the quantity and energy density of foods consumed by adults parallel the increasing prevalence of obesity in the U.S. population.11 Data from the Central Statistical Office show that car ownership and television viewing, proxy measures of physical inactivity, closely parallel the rising trends in obesity in England.12 Using data from NHANES, Dietz et al. demonstrated that the prevalence of obesity increased by 2% for each additional hour of television viewed.13 There is also evidence that the relative availability and price of different food products affect food consumption,14 and that the built environment, such as quality of local parks, affects the level of physical activities in a community.15 These findings not only emphasize the impact of environmental factors on the obesity epidemic but also indicate that policies affecting the availability of high-caloric-density food, the cost of fruits and vegetables, and the built environment may contribute to the obesity epidemic.
In addition to environmental factors, there is genetic predisposition to obesity. It is known that single gene mutations are responsible for rare forms of monogenic obesity (leptin (LEP), leptin receptor (LEPR), melanocortin-4 receptor (MC4R), and pro-opiomelanocortin (POMC)).16 However, there is growing evidence that common genetic variants or single-nucleotide polymorphisms (SNP) may play an important role in the obesity epidemic. These SNPs have modest effects on an individual susceptibility to common forms of obesity, but due to their high frequency, they can have a large contribution to obesity on the population level.17 Frayling et al. was the first to use a genome-wide association (GWA) study to identify a SNP located in the fat mass and an obesity-associated gene (FTO) that is associated with an increase risk of common obesity.18 The finding that the FTO gene variant is a risk factor for common obesity has now been replicated in multiples studies.19–21 FTO was initially identified in a GWA study to be associated with an increased risk of type 2 diabetes mediated through an effect BMI. In a GWA study of 38,759 patients, Frayling et al. found that a person who is homozygous for the risk allele (rs9939609 A allele) had a 1.67-fold increased odds of obesity when compared with those who do not have the risk allele.18
There is growing recognition that social networks may have an important role in the obesity epidemic. Christakis et al. explored the hypothesis that obesity may spread through social networks by evaluating an interconnected social network of more than 12,000 people from the Framingham Heart Study to examine the effects of weight gain among friends, siblings, and spouses.22 They found that a person’s risk of becoming obese increased by 57% if a friend became obese. The association was smaller among siblings and spouses: the risk of becoming obese increased by 40% and 37% if a person had a sibling or spouse who became obese, respectively.22 By exploring the role of social networks and obesity, this study showed that the obesity epidemic is affected by the complex interaction between the environment, genetic factors, and human behavior (e.g., passive permission).
Burden of Illness Associated with Obesity
Obesity is associated with an increased risk of death. Adams et al. estimated the risk of death in a prospective cohort of more than 500,000 U.S. men and women after 10 years of follow-up, and reported that, among patients who had never smoked, the risk of death is increased by 20% to 40% in overweight patients and by 2- to 3-fold in obese compared with normal-weight patients.23
Obesity is also associated with increased risk for numerous chronic diseases, including diabetes, hypertension, heart disease, and stroke.24 Furthermore, obesity is linked to several digestive diseases, including gastroesophageal reflux disease (GERD) and its complications (e.g. erosive esophagitis, Barrett’s esophagus and esophageal adenocarcinoma), colorectal polyps and cancer, and liver disease (e.g. non-alcoholic fatty liver disease, cirrhosis and hepatocellular carcinoma).25
Because of the increased risk of death and the increased risk of costly chronic diseases associated with obesity, the obesity epidemic places a large financial burden on the economy. The U.S. Department of Health and Human Services has estimated the total economic cost of overweight and obesity in the United States to be close to $117 billion using data from 1995, updated to 2001 dollars.26 However, because the prevalence of overweight and obesity has increased since 1995, the costs today are likely to be considerably higher than previous estimates. Trogdon et al. estimated that the total indirect cost was $65.67 billion in the United States for 1999, based on data from a systematic review.27 A recent study by Finkelstein et al. projected the annual medical spending due to overweight and obesity approached $92.6 billion in 200228, or about 9% of US health expenditures.26
Summary and Conclusions
The prevalence of obesity in the U.S. has increased dramatically since 1980 in both adults and children, with evidence of possible recent stabilization, according to data from 2003–2004 to 2005–2006 for both children and adult in the U.S. The epidemic of obesity is not limited to the U.S. but has been documented in several regions worldwide, with the prevalence of obesity rising in most countries. Obesity is affected by a complex interaction between the environment, genetic predisposition, and human behavior. It is associated with an increased risk of numerous chronic diseases, from diabetes and cancers to many digestive diseases. In addition, the obesity epidemic exerts a heavy toll on the economy with its massive healthcare costs. The problem of overweight and obesity has therefore emerged as one of the most pressing global issues that we will face during the next several decades, and demands attention from the healthcare community, researchers, and policy makers. The implications for gastrointestinal health care providers is readily apparent and will be addressed in the text of this entire issue of Gastroenterology Clinics.
Acknowledgment
The following research was partially supported by R01 “Obesity, H. pylori, and Risk of Barrett’s Esophagus”, and K24 “Epidemiology and Outcomes of Digestive & Liver Diseases”. It was also partly supported by the Houston VA HSR&D Center of Excellence (HFP90-020).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.World Health Organization. [Accessed October 22, 2009];Obesity. 2008 Available at: http://www.who.int/topics/obesity/en/
- 2.Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science) Circulation. 2008 July 22;118(4):428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- 3.US Centers for Disease control and Prevention. [Accessed October 22, 2009];Overweight and obesity. 2008 Available at: http://www.cdc.gov/nccdphp/dnpa/obesity/trend/maps/index.htm.
- 4.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002 October 9;288(14):1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 5.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002 October 9;288(14):1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity among adults in the United States— no change since 2003–2004. NCHS data brief no 1 National Center for Health Statistics. 2007 [PubMed] [Google Scholar]
- 7.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007 May;132(6):2087–2102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 8.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008 May 28;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 9.Prentice AM. The emerging epidemic of obesity in developing countries. Int J Epidemiol. 2006 February;35(1):93–99. doi: 10.1093/ije/dyi272. [DOI] [PubMed] [Google Scholar]
- 10.Nishida C, Mucavele P. Monitoring the rapidly emerging public health problem of overweight and obesity: The WHO Global Database on Body Mass Index. SCN News. 2005;(29):5–12. [Google Scholar]
- 11.Kant AK, Graubard BI. Secular trends in patterns of self-reported food consumption of adult Americans: NHANES 1971–1975 to NHANES 1999–2002. Am J Clin Nutr. 2006 November;84(5):1215–1223. doi: 10.1093/ajcn/84.5.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prentice AM, Jebb SA. Obesity in Britain: gluttony or sloth? BMJ. 1995 August 12;311(7002):437–439. doi: 10.1136/bmj.311.7002.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dietz WH, Jr, Gortmaker SL. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics. 1985 May;75(5):807–812. [PubMed] [Google Scholar]
- 14.Holsten JE. Obesity and the community food environment: a systematic review. Public Health Nutr. 2008;May(14):1–9. doi: 10.1017/S1368980008002267. [DOI] [PubMed] [Google Scholar]
- 15.Kipke MD, Iverson E, Moore D, et al. Food and park environments: neighborhood-level risks for childhood obesity in east Los Angeles. J Adolesc Health. 2007 April;40(4):325–333. doi: 10.1016/j.jadohealth.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 16.Andreasen CH, Andersen G. Gene-environment interactions and obesity-further aspects of genomewide association studies. Nutrition. 2009 October;25(10):998–1003. doi: 10.1016/j.nut.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 17.Tiret L, Poirier O, Nicaud V, et al. Heterogeneity of linkage disequilibrium in human genes has implications for association studies of common diseases. Hum Mol Genet. 2002 February 15;11(4):419–429. doi: 10.1093/hmg/11.4.419. [DOI] [PubMed] [Google Scholar]
- 18.Frayling TM, Timpson NJ, Weedon MN, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007 May 11;316(5826):889–894. doi: 10.1126/science.1141634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hunt SC, Stone S, Xin Y, et al. Association of the FTO gene with BMI. Obesity (Silver Spring) 2008 April;16(4):902–904. doi: 10.1038/oby.2007.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Haupt A, Thamer C, Machann J, et al. Impact of variation in the FTO gene on whole body fat distribution, ectopic fat, and weight loss. Obesity (Silver Spring) 2008 August;16(8):1969–1972. doi: 10.1038/oby.2008.283. [DOI] [PubMed] [Google Scholar]
- 21.Andreasen CH, Stender-Petersen KL, Mogensen MS, et al. Low physical activity accentuates the effect of the FTO rs9939609 polymorphism on body fat accumulation. Diabetes. 2008 January;57(1):95–101. doi: 10.2337/db07-0910. [DOI] [PubMed] [Google Scholar]
- 22.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007 July 26;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 23.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006 August 24;355(8):763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 24.Field AE, Coakley EH, Must A, et al. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001 July 9;161(13):1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 25.American College of Gastroenterology. [Accessed November 9, 2008];Obesity and Digestive Disorders A Physician Reference. 2008 Available at: http://www.acg.gi.org/obesity/pdfs/ACG_Obesity_Physician_Reference.pdf.
- 26.NIDDK Weight Control Information Network. [Accessed November 9, 2008];Statistics related to overweight and obesity Economic costs related to overweight and obesity. 2008 Available at: http://win.niddk.nih.gov/statist.
- 27.Trogdon JG, Finkelstein EA, Hylands T, Dellea PS, Kamal-Bahl SJ. Indirect costs of obesity: a review of the current literature. Obes Rev. 2008 September;9(5):489–500. doi: 10.1111/j.1467-789X.2008.00472.x. [DOI] [PubMed] [Google Scholar]
- 28.Finkelstein EA, Fiebelkorn IC, Wang G. State-level estimates of annual medical expenditures attributable to obesity. Obes Res. 2004 January;12(1):18–24. doi: 10.1038/oby.2004.4. [DOI] [PubMed] [Google Scholar]