Abstract
This study qualitatively examined the social-ecological stressors that youth experience during the first year following an HIV diagnosis. Thirty HIV-positive youth (16 males, 14 females) between the ages of 16–24 participated in either focus groups or individual interviews. All sessions were transcribed and themes were identified through cross-case and comparative analyses. Participants reported experiencing stressors within multiple social-ecological systems, including interactions with their families, sexual partners, health care providers, work, and school. The results from this study highlight the need for youth-focused services that assist with multiple layers of stressors during the first year following an HIV diagnosis.
Keywords: HIV/AIDS, youth, psychological stressors
INTRODUCTION
In the United States, it is estimated that 15% of all new HIV infections are among people under 25 years of age, and the vast majority of these infections are a result of sexual activity (Centers for Disease Control and Prevention [CDC], 2006; The Joint United Nations Program on HIV/AIDS [UNAIDS], 2004). In the 35 states with long-term confidential name-based reporting through 2004, 62% of the 17,824 adolescents between the ages of 13–24 who were given either an HIV or AIDS diagnosis were males and 38% were females (CDC, 2005). Young men who have sex with men (YMSM) represent the largest group of males between the ages of 13–24 living with HIV and AIDS, and their rates of infection are increasing at alarming rates; especially among African American and Latino youth (CDC, 2001; CDC, 2005; Garofalo & Harper, 2003; MacKellar et al., 2005; Valleroy, MacKellar, Karon, & Rosen, 2000; Wolitski, Valdiserri, Denning, & Levine, 2001). Female adolescents of color also have disproportionately higher rates of infection with HIV than White females, especially those living in low-income urban environments (Aral, 2001; CDC, 2005; Krieger, Waterman, Chen, Soobader, & Subramanian, 2003).
These epidemiological data demonstrate that despite multiple prevention efforts aimed at thwarting the spread of HIV, significant numbers of adolescents and young adults are still becoming infected with HIV on a consistent basis. Once these youth receive their HIV diagnosis, they must contend with adjusting to the news that they are now living with a chronic health condition that requires long-term medical management. Unlike adolescents living with other chronic health conditions like asthma or diabetes, those living with HIV also must contend with high levels of social stigma that may result in discrimination and oppression, as well as negative societal messages that place blame on them for the acquisition of their disease (Greene & Banjeree, 2006; Rao, Ketwaletswe, Hosek, Martinez, & Rodriguez, 2007).
Adolescents who test positive for HIV are often confronted with a myriad of stressors as they struggle with normal adolescent developmental issues while carrying the burden of living with a highly stigmatized and life-threatening illness. Prior research focused on adolescents living with other chronic and terminal illnesses has provided strong evidence regarding the difficulty youth have adjusting to their diagnosis, particularly in the areas of developmental tasks, psychological functioning, and medical management (Gavaghan and Roach, 1987; Lavigne and Faier-Routman, 1992; Sayer, Hauser, Jacobson, Willett, & Cole, 1995; Wallander & Thompson, 1995). For adolescents and young adults living with HIV, unique difficulties may arise due to the highly stigmatized nature of their illness, which will interfere with their ability to adjust and cope with their diagnosis (Brown, Lourie, & Pao, 2000; Rao et al., 2007).
One common stressor among adolescents living with HIV is the experience of negative affective states, such as depression and anxiety (Hosek, Harper, & Domanico, 2000). Poorer psychological functioning can not only result in decreased quality of life and impaired social functioning, but has also been associated with increased participation in sexual and substance use risk behaviors (Murphy et al., 2001), as well as decreased adherence to anti-retroviral therapies (Hosek, Harper, & Domanico, 2005; Murphy, Wilson, Durako, Muenz, & Belzer, 2001) among adolescents living with HIV.
Given the continued stigma associated with HIV, many of these youth are apprehensive about disclosing their HIV status to parents, friends, and sexual partners (Hosek, Harper, & Robinson, 2002; Rao et al., 2007). In addition to the lack of social support associated with not disclosing to family/close friends, fear of the negative impact of disclosure among adolescents living with HIV has also been associated with poorer adherence to medical regimens (Pugatch, Bennett, & Patterson, 2002). Given the potential for negative psychological and medical outcomes associated with the stress of receiving an HIV diagnosis, interventions are urgently needed to assist adolescents who are newly diagnosed with HIV to adjust to their disease status. Before effective interventions that meet the specific psychosocial and developmental needs of adolescents newly diagnosed with HIV can be developed, formative research is needed to better understand the range of stressors that impact youth during the initial year of their diagnosis. This research will best be guided by frameworks and models that account for the complexity of adolescent development.
Ecological Systems Understandings of Development and Illness
Urie Bronfenbrenner’s Ecological Systems Theory of Human Development (1979) examines the complex interactions and relationships between an individual and his/her multiple social and physical surroundings during adolescent development. The interactions that individuals have with others and with these various environments are seen as key to human development. Bronfenbrenner (1979) identifies four ecological systems: the microsystem, the mesosystem, the exosystem, and the macrosystem. The microsystem (i.e., family, school, peers) is the immediate environment in which a person is operating. When microsystems interact, a mesosystem is formed and encompasses the relationship between two or more settings (i.e., relationship between school and peers). The exosystem is an environment in which the individual is not directly involved, but that impacts him/her anyway (i.e., relationship between parents, caregiver’s place of employment, local media, community agencies). For example, an adolescent does not have a direct decision-making role in his/her parents’ relationship, but an argument between them may directly or indirectly impact the adolescent. The final ecological system identified by Bronfenbrenner (1979) is that of the macrosystem. The macrosystem consists of larger societal structures and values (i.e., social, cultural, political, religious) that do not directly impact the life of an individual adolescent, but rather society as a whole.
More recently, Bronfenbrenner (1986) proposed an additional system, the chronosystem, which examines over time the influence of environmental changes on an individual’s development. The chronosystem focuses on “normative” (i.e., entering school, puberty, marriage) and “non-normative” (i.e., death, divorce, chronic illness) transitions that can occur across the lifespan and may indirectly impact development by affecting family processes.
These ecological systems are interactive and are characterized by roles, relationships, and norms. The relationship and interactions between these structures change as a function of development (Muuss, 1996). According to Bronfenbrenner (1979, 1986), when the relation between different microsystems is compatible, development progresses smoothly. For example, when role expectations are similar across school and home, it is expected that youth will perform better than if substantial differences in role expectations occur across settings.
Kazak, Segal-Andrews, and Johnson (1995) have applied the Bronfenbrenner model to the ecological system of the chronically ill child. In this model, the microsystem extends to include the disease itself since it places demands on both the child and the family. The mesosystem considers the interactions between caregivers and hospitals as well as the health-care team. The exosystem is primarily a consideration of the parents’ or care-givers’ social networks and the extent to which the disease impacts those networks. Finally, the macrosystem includes laws and policies that may directly impact the care and services available to children with pediatric illness.
While Kazak and colleagues’ (1995) application of the social-ecological model reflects the experience of chronically ill children, it may not apply directly to adolescents and young adults living with HIV. Many youth diagnosed with HIV are either young adults or emancipated minors who lack a parental or caregiver support network. What may fall into a mesosystem or exosystem for a child with a caregiver, may actually be part of the adolescents’ microsystem as he/she negotiates these systems in isolation. Thus, further exploration of the socio-ecological model as it applies specifically to adolescents and young adults living with HIV is warranted.
The purpose of the current study was to better understand the subjective experiences of adolescents and young adults living with HIV during the first year of their diagnosis by exploring the challenges, strengths, and needed areas of support/assistance associated with receiving an HIV diagnosis. Elements of Bronfenbrenner’s (1979, 1986) Ecological Systems Theory of Human Development and Kazak et al.’s (1995) social-ecological model of chronically ill children guided both the data collection and analysis. This information was collected in order to create a socio-ecological model and understanding of the myriad stressors that impact these youth during the initial stages of accepting their HIV diagnosis. Findings from this study will guide the development of a psychosocial intervention aimed at improving adjustment to HIV diagnosis among adolescents and young adults recently diagnosed with HIV.
METHODS
Participants
A total of 30 adolescents and young adults who had been recently diagnosed with HIV participated in either focus groups or individual interviews. All participants were behaviorally-infected and had been aware of their HIV diagnosis for 12–24 months, with an average of 16.7 months (SD 4.89). They ranged in age from 16 to 24 years, with a mean age of 21.5 (SD 2.2). The gender composition of the sample was balanced, with 14 females and 16 males. The ethnic composition was distributed across three groups and represented the disproportionate number of Black and Hispanic adolescents and young adults living with HIV: 15 Black (8 female, 7 male), 13 Hispanic (6 female, 7 male), and 2 White (2 male).
Procedures
Youth were recruited from Adolescent Medicine Trials Units involved in the Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN) located in Chicago, New York, and San Juan, Puerto Rico to participate in either focus groups or individual interviews. This study was approved by the Institutional Review Boards of all three participating sites. Each participant received compensation for their time as well as transportation costs associated with the focus groups/interviews (the amount of compensation was determined by each ATN site’s IRB). Participants were recruited by Study Coordinator nurses when the youth appeared for their regular medical visits, and were only approached regarding participation if they had received their diagnosis within 12 to 24 months of the study visit date. This criteria was selected in order to recruit key informants that had received their diagnosis recently enough so that they could recall the experiences of their first year after receiving the diagnosis, but also had enough distance from that first year so that they could be more introspective when recalling the stressors associated with that time period. Youth were informed of the nature of information collected and discussed in the focus groups and informed of the confidential nature of such material. Written informed consent/assent was obtained from all participants who expressed interest in the study. As some youth were hesitant to discuss sensitive issues in a group setting, they were offered the option of participating in an individual interview if they did not feel comfortable being a part of a focus group. Additionally, participants that were not able to participate in the focus group due to scheduling conflicts were also offered the option to participate in an individual interview. Participants were recruited sequentially and focus groups were convened once a minimum of 4 youth had agreed to participate.
Four gender-specific focus groups were conducted with a total of 15 participants (9 female, 6 male), and 15 individual interviews (10 male, 5 female) were completed (Table 1). All groups and interviews took place in private rooms and were audiotaped; and facilitators took additional process and content notes. Each focus group was co-facilitated by two trained interviewers with specializations in psychology and public health (one PhD-level male, one MPH-level female), and individual interviews were conducted by the same trained interviewers. The focus groups and interviews were conducted in either English or Spanish, depending on the comfort level and language preference of the participants. Interviewers followed a semistructured guide, which was identical for both focus groups and individual interviews, with suggested probes to elicit and clarify responses. Questions in the focus group/interview guide asked about general critical areas of stress (e.g., “tell me what you think were the most difficult issues you had to deal with during the first 6 months after receiving your diagnosis”), coping, and support (e.g., tell me what you think would have helped you to adjust to living with HIV during the first 6 months after receiving your diagnosis”) for youth newly diagnosed with HIV. Participants were also asked about the most challenging physical/medical and psychosocial aspects for youth living with HIV.
TABLE 1.
Interview Type, Gender, and Race of Participants by ATN Site
| ATN Site |
|||
|---|---|---|---|
| Bronx, NY (N = 12) | Chicago, IL (N = 10) | San Juan, PR (N = 8) | |
| Interview Type | |||
| Focus group | 3 | 9 | 3 |
| Individual interviews | 9 | 1 | 5 |
| Gender | |||
| Female | 7 | 3 | 4 |
| Male | 5 | 7 | 4 |
| Race | |||
| White | 0 | 2 | 0 |
| Black | 8 | 7 | 0 |
| Hispanic | 4 | 1 | 8 |
Analysis
After initial review of the data by the authors and direct feedback from the focus group/interview facilitators, it was determined that the content of the focus group data and the individual interview data did not differ markedly. Given the content similarities of the data collected, and the overall advantages of synthesizing mixed methods data to gain a richer understanding of a phenomena of interest by eliciting a broader range and greater variety of perspectives from participants (Creswell, 2003), data from the focus groups and individual interviews were combined for the analysis. Audiotapes of the focus groups/interviews were transcribed verbatim, and all Spanish-language focus groups/interviews were translated from Spanish to English. Data analysis was conducted by three members of the research team, two of whom were interviewers who collected the data. Analysts coded and analyzed data individually and then met in a series of analysis meetings to review the developing concepts and themes, and to develop consensus across the three analysts. The team kept data analysis meeting minutes and memos following each meeting to track the development of concepts and themes, and to document the initial and developing ideas for the analysis. QSR International’s NVivo 2.0 software was used for coding data, searching text, and conducting cross-case analysis.
After reading and reviewing the transcripts individually, members of the analysis team generated codes which were discussed during team meetings and modified based on group consensus. From this, the protocol team developed a coding structure, (i.e., a hierarchical set of constructs that account for the phenomena seen in the data) and then further developed and refined the list of codes as additional transcripts were coded and discussed. After all of the transcripts were coded and the concepts were examined as they were presented in each individual interview, the analysis team conducted cross-case and comparative analyses. To do this, the team identified consistent patterns in meaning, concepts, and themes across the focus groups/interviews (cross-case) and then examined comparative differences based on gender (Creswell, 1998; Miles & Huberman, 1994). Where gender differences emerged related to these ecosystems, they are noted in the explanation of the results.
The general approach to analysis was guided by a phenomenological framework as the team sought to understand the lives and stressors of adolescents newly diagnosed with HIV (Creswell, 1998; Patton, 1990). Our focus was on individual experiences and meanings given to those experiences, as well as shared experiences. At the core of this analytic approach is the assumption that all findings are circumscribed by context, and that individuals and groups of individuals (e.g., HIV+ youth) have unique realities within which and by which they live their lives. Phenomenological principles may challenge common assumptions about how individuals and groups may perceive their values and behavior. The specific approach to coding and analysis was inductive in nature since this procedure allows for the patterns, themes, and categories of analysis to emerge from the data (Patton). This procedure allows for an exploration of indigenous concepts and typologies. Once patterns and themes were established through inductive analysis, the final stage of qualitative analysis was deductive in nature, as the major themes were categorized according to elements of both Bronfenbrenner’s (1979) Ecological Systems Theory of Human Development and Kazak et al.’s (1995) social-ecological model of chronically ill children.
RESULTS
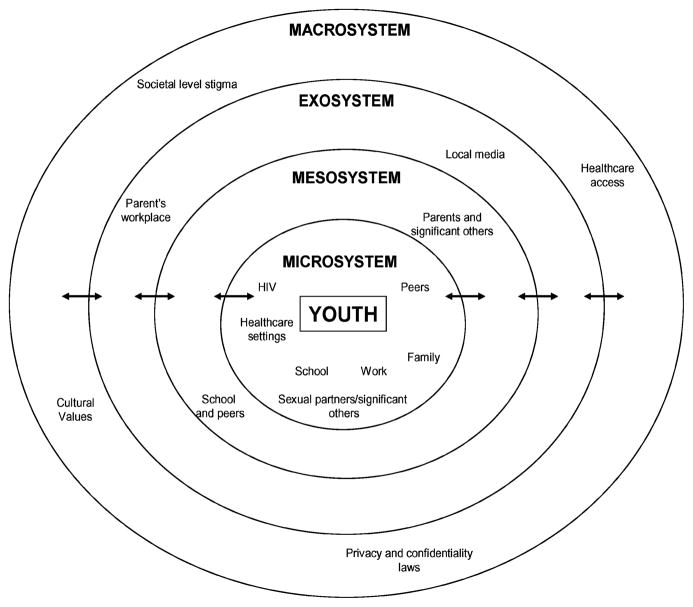
Adolescents revealed the most salient stressors they experienced and discussed how their lives were impacted during the first year following their HIV diagnosis. The major themes that emerged are presented and organized into four ecological systems: microsystem, mesosystem, exosystem, and macrosystem (see Figure 1). Organizing the themes around these systems avoids limiting the presentation of themes to only those that were endorsed by the majority of participants, since one of the major strengths of qualitative research is the representation of different voices (Creswell, 1998). Illustrative phrases and quotes from the focus group/individual interviews are presented below along with the gender of the individual. For these youth, the adolescent’s microsystem consisted of their direct interactions with HIV, family, sexual partners/significant others, peers, health-care providers, work, and school. The mesosystem encompassed interactions between those in the microsystem including school and peers, work and parents, and significant others that may have caused aggravated stress among these youth. Additionally, the macrosystem includes societal-level stigma and violation of privacy and confidentiality laws that youth reported caused stress during that critical period following diagnosis.
FIGURE 1.
Ecological Model of Stressors Experienced by Youth Newly Diagnosed with HIV
Microsystem
The stressors within the microsystem as identified by the youth include systems that the youth interact with directly. Themes that emerged within this system include HIV disease, family, sexual partners/significant others, peers, health-care settings, and work/school.
Stressors Related to HIV Diagnosis
Youth reported that receiving the HIV diagnosis was a pivotal moment in their life. Many recalled immediate thoughts of death and hopelessness about their future and a general feeling of numbness. Within the general theme of HIV disease, several subthemes emerged which include: (a) information related to HIV, (b) the manifestations of the illness, (c) medication, and (d) acceptance of the diagnosis.
Many youth expressed that it was stressful for them to sort through and understand all of the information they were receiving about HIV and AIDS. Youth described being hyper-vigilant for potential symptoms of the illness after receiving the HIV diagnosis, including feelings of panic over the slightest cold or cough.
Youth reported having difficulty understanding the manifestations of HIV and the mechanisms of the disease. They described fears related to disease progression, physical signs/symptoms, and prognosis and how the illness would impact their future goals.
I just got depressed, and I’ve basically had it embedded in my head that I was on borrowed time and I’m not gonna be able to get to do any of the things that I wanted to do with my life. -Male
Another theme related to the HIV diagnosis was the challenges of taking HIV medications and dealing with demands of the treatment, such as finding a safe and private place to store and take the medication, as well as figuring out how and when to take the medications.
… but anyway, the biggest problem for youth, at least with taking the medications is the fear that if that person knows…knows what the medications are or that they forget. -Female
Those participants who were not yet taking medication described their fear of taking the medication in the future and how it would impact their lives.
Yes, how to take them…I already see people that are taking medications and there are lots of pills. Apart from that, I have also seen how they deteriorate because of that [medication]. That gets me really scared. For real, it has really frightened me. Having to get to that point, do you understand? -Male
The final subtheme that emerged related to the HIV diagnosis was learning to accept the diagnosis. Disbelief was a common reaction to the diagnosis and some youth discussed taking the HIV antibody test as many as three different times to confirm their HIV status. Other participants struggled to accept the diagnosis because they did not look or feel sick.
I’m like, how can I not know? I don’t feel anything. I feel normal, but I was in denial for those additional two weeks. And I was like, how do you know I’m positive? Is there something you can see in me? I didn’t get any counseling which I should of at that time. I didn’t. -Female
Stressors Related to Family
Youth from all focus groups and individual interviews revealed that family stressors were among the most common during the year following their diagnosis. Within this theme, several sub-themes related to the youth’s interactions with family emerged, including (a) disclosure, (b) misinformation, and (c) rejection.
Fear of disclosing their HIV diagnosis to family members was a common stressor reported by participants. One reason cited for this fear of disclosure was concern about how the parent would react to the news. Within this theme, youth reported being primarily concerned for the well-being of their parents who may worry excessively as a result of the diagnosis.
I mean my mom is my best friend in the whole world. And she knows everything about me. And she’s my everything. But I KNOW she would be very supportive, but I know that as soon as I hang up the phone she’s gonna be sitting there and she’s gonna be worrying, losing sleep and, I just, I don’t know, I don’t think I will ever tell my mom. Because I don’t think it’s necessary for her to worry at this point. -Male
Another stressful experience related to youth’s disclosure to family members was the anticipated reaction due to the family’s religious values.
The whole “I told you so” and, my family is very religious so I guess I’m just afraid that I’ll hear what I’m expecting to hear. Which is nothing good. Pentecostals are very difficult people and, especially my mom, so to tell her, it would be just like “that’s what you get.” -Male
Many adolescents felt like they were leading a double life living with the diagnosis and trying to hide it from their family during the initial stages of living with HIV; like one youth remarked—“it’s confusing and it’s just a headache.” They were also concerned about family members noticing dramatic changes in their behaviors.
And I noticed that my family, they noticed a dramatic change in my personality during my first month, because I was withdrawn, I stayed in my room all the time…Watched TV. I cried a lot in the room. -Female
The subtheme of misinformation on the part of both participants and family members was explained in terms of the lack of information about HIV transmission that, in turn, lead to fears of accidental infection from casual contact. For some participants, family members’ lack of information was also associated with concerns that the family would associate the HIV diagnosis with AIDS and death.
I always worried, like I said, I didn’t tell my parents. I’m living in their house and I’m eating off their forks and utensils, their plates. Should I tell them? You can’t get it through saliva, I’m like should I do something extra to make sure I won’t spread it to my family, because I don’t want to be that kind of person. -Female
Fear of rejection or discrimination following disclosure was another common concern and tended to be related to the participants’ experiences of observing family members’ negative reactions to other family member’s HIV diagnosis. Some participants reported hearing family members’ negative comments about HIV/AIDS and the people who become infected. These observances from the youth led them to abstain from disclosure because they felt they would receive the same reaction from family members.
My uncle, he was a transvestite or a transsexual, I should say, and he had it [HIV], too, and everybody in the family discriminated against him. Whenever he came to dinner, they were throwing away the dishes he ate off of. When he went to the bathroom they were cleaning up the bathroom with bleach and when he passed they burned all of his belongings. And if they found out about me…. -Female
Stressors Related to Sexual Partners/Significant Others
Participants discussed at great length the stressors related to romantic/sexual partners or significant others. In general, participants reported experiencing anger toward their partner. For some participants, this was related to the partner completely withdrawing emotionally and physically after learning of the participant’s HIV diagnosis. For others, there were questions of mistrust directed at the partners for concealing their HIV status, their extramarital affairs, or in the case of females with male partners, their partner’s undisclosed sexual relationships with other men.
That’s what I thought about my husband. I was thinking maybe he was sleeping with other men behind my back. And that’s how it all happened. -Female
Disclosing one’s HIV status to a current or potential sexual/romantic partner was a great source of stress for the youth. There were several discussions among the participants related to fear of the partner rejecting them or distancing themselves. A participant that disclosed her status reported the following:
And I kept so much to myself, and I would have had somebody else to talk to besides myself, because my husband, well, my fiancée at the time, wasn’t even there for me. He completely withdrew from me. -Female
Aside from the emotional rejection from current romantic/sexual partners, there were also concerns about violent reactions to HIV status disclosure.
And nowadays out here, if you have HIV, and ever do try to tell them right then and there, your face is about to end up is in his fist. That’s how it is. -Female
Stressors related to future sexual/romantic partners and potential relationships were discussed. Youth reported that during their first year of living with an HIV diagnosis there was no desire for being involved in a sexual relationship; as one male participant stated, “I went through the I hate men phase.” Regarding becoming involved in a romantic relationship, one male participant reported that he “needed to get comfortable with having HIV before [he] imposed it upon someone else.” Others participants described that they felt their partners would have “less quality of life” being in a relationship with an HIV+ person. There were discussions around the feeling that they did not deserve a partner because they were HIV+ and, therefore, not “normal.”
It’s true, if you put me next to a person that is [HIV] negative, you are going to choose her. Because I am [HIV] positive and you are going to see me as less quality of life, because you are going to see that it is much a harder life with me! -Female
Additionally, themes arose about infecting sexual partners and dealing with that potential guilt. One participant reported having suicidal ideations shortly after receiving her diagnosis since she could not cope with the thought of not being able to have sex anymore because of the potential for infecting others.
I’m just like I should have killed myself, because even when they first told me, I was like damn, I can’t have sex no more. I’ll feel guilty that any little thing is gonna pass it [HIV]. So it’s like, I’ll go just kill myself. Can’t enjoy boys. -Female
Stressors Related to Peers
The thought of peer disclosure was another stressor for youth and was related to fear of rejection or fear of losing those peers. Participants reported being fearful that physical changes, such as sudden weight loss, would be noticed by peers and their HIV status would be questioned and/or rumors begin to surface.
Everyone looked at me, like why you so skinny, like I know there’s something going on with you, you know what I mean, but I didn’t want to let them know, I don’t let people know my business. -Male
Participants reported fearing that after disclosing, peers would tell other people in their community and/or school about their HIV status. Several youth shared experiences in which they disclosed to a peer and that individual revealed the youth’s status to others. This intentional disclosure led some youth to discuss how they felt they had to clear their reputation or “fight for my name.”
I told three of my friends. One of them went back and told people, I had to fight her for it…That the third one had to get messed up, that’s so people don’t know, that [they think] she lied. -Female
Among those participants who had disclosed to their peers, several reported being rejected by them. Others said that, although they were not rejected, their friends began to treat them differently and to spend less time with them. As one female participant stated, “they [friends] don’t leave you totally…but it’s like ‘no, I’m too busy.’”
I don’t have any of the friends I had before and I suffered from it…they rejected me and well, what could I do? -Female
Stressors Related to Health-care Settings
Most of the participants reported not having routine health care previous to the diagnosis, therefore there was considerable distress surrounding seeking medical services, finding a suitable doctor, and fitting HIV into their life. Others reported that the providers did not treat them the same as non-HIV patients or that they were treated “like you are just a number” by the providers. Youth also reported that some providers did not understand what it was like to live with HIV. As one youth stated:
Hearing doctors say there is hope, don’t give up, but it didn’t click in. Because I’m like, okay, you’re not experiencing it. You deal with it, yes, you’re a doctor, you deal with it, however I’m experiencing it, and this is how I feel right now. I was just thinking about death. It was very depressing, very stressful. -Female
There was also considerable discussion about the need for repeated disclosure within the health-care system since participants had to continually reveal their status to various health facility personnel. Additionally, there was the challenge of dealing with incidents where hospital staff and testing laboratories allegedly revealed their status without the youth’s authorization.
I get flustered because there [the clinic] the employees see you; there everyone knows me. -Female
For participants with children, the fear of discrimination was another concern when receiving health-care services for themselves or for their children.
I do have a condition, I know he doesn’t, thank God, and the process that was used. But I know they [the clinic staff] are going to deny my son or they are not going to treat him. -Female
Stressors Related to School
Youth who were in school at the time of their diagnosis often reported a change in grades, while others reported that they stopped going to school altogether. Youth reported losing interest in school or school-related activities.
It was just like I stopped going to school for a while and everybody was coming over, why you not coming to school? Why you not coming to school? Like nah, I been down. So it was just like my whole world felt crumpled. -Female
For youth that stayed in school, there were concerns about missing classes due to their medical appointments. Aside from attending classes and keeping up with grades, youth reported feeling stressed about the images of those living with HIV that were discussed in class (including sex education classes), as well as misinformed comments made in the classroom.
You have health class and they mention HIV and sexually transmitted diseases and condoms and stuff like that. And I don’t know. I asked questions. I’m not ashamed. I asked questions. But you still worry or like somebody says the wrong information and you get afraid and you’re like, nobody ever told me that. -Female
Stressors Related to Work
Among the factors that youth reported as stressful during the initial year of their diagnosis was the difficulty keeping their diagnosis a secret from their coworkers. Many expressed fear that if they disclosed their status their employers would “wait until the first day that I am absent and then fire me” or that they would be rejected by their coworkers.
The fear is that other people will reject you, for example, at your work, if they find out about your condition, they could fire you from your job…I said that, it’s like, I know that is like that, because that happened to me. This is…sad. -Female
There was also discussion about the physical and emotional ailments that made it difficult for the youth to function while at work. Many reported worrying about losing too much weight and looking very sick, whereas others had to deal with depression and extreme fatigue at work. Some commented on the difficulty of functioning at work because of the side effects from medication, such as nausea or upset stomach.
It made me really fatigued when I would go early to work, I would feel like a zombie, like if I was a little bit drunk. Like…I had just woken up—the whole morning! -Male
Mesosystem
Mesosystems are formed when there is interaction between two or more microsystems. Mesosystemic themes emerged for participants in the areas of school/peers and family/partners.
Stressors Related to School-Peer Interaction
Many youth reported experiencing stress within the school system when their peers make negative or judgmental comments about HIV or people living with HIV. Additionally, youth reported on the negative perception of HIV presented in health education classes as compared to more neutral presentations about other sexually transmitted diseases.
Because everybody’s giving you these negative images…Because you gotta sit there and listen to the kids make jokes about it and everything. Like they don’t know it’s really serious out there, especially when you HAVE it. -Female
Stressors Related to Family-Partner Interaction
Several female participants reported stress related to the interaction between their families, who were recently informed of their HIV status, and their romantic/sexual partners. This was related to their experiences of the family members knowing about the participant’s HIV status and then blaming the participant’s sexual/romantic partner for the infection. Participants often described their families as “overprotective” or disapproving of their current and/or future relationships. For those who continued their relationships with their partners following the HIV diagnosis, some participants discussed the family’s rejection or blaming the partner.
So my parents felt like he was at fault for what happened, but I felt that as well, I started feeling that way. -Female
Exosystem
Exosystem describes environments in which the individual is not directly involved, the other people and places that the youth may not interact with often, but that still impact him/her anyway. Exosystemic themes emerged in the areas of parental workplace and local media.
Stressors Related to Parent’s Workplace
The stress that parents experienced at their respective workplace negatively impacted some of the participants. The parents who had private health insurance supplied by their employer dealt with the stress at work of ensuring health-care coverage for their adolescent living with HIV. Additionally, parents faced stress relating to disclosure of their adolescent’s HIV status. These sources of stress that occurred indirectly at the parent’s workplace had a direct impact on the adolescent. As the adolescent tried to cope with their own HIV status, they were burdened by the stress that the parents faced at the work place.
Just now I believe that at 22 years they will take me off my dad’s medical plan…When he called and told them, well that I had the condition …she told him that she needed to verify it…they (coworkers) found out there because they sent him a fax. And it was painful for him because his coworkers quickly looked at him like…you know. And…I can’t handle anything else! I have to survive! -Female
Stressors Related to Local Media
Participants identified the influence of the media as a major source of stress. They felt that television, in particular, and the media, in general, portrayed HIV in a negative light. According to participants, this often occurs when HIV is confused or seen as synonymous with AIDS. Also, participants perceive the media as underemphasizing the severity of other sexually transmitted diseases while highlighting HIV.
…And because you hear more about AIDS and you see the word AIDS more than HIV on TV and radio and news these days more than anything…. -Male
Even if you sit and watch a talk show, they’ll make it seem like this STD [HIV] is really bad, but I mean, it’s livable now. -Male
Macrosystem
Macrosystems generally consist of larger societal structures, including social, cultural, and political values, that impact society as a whole. For these participants, the high level of stigma attached to HIV/AIDS at the societal level as well as the violation of privacy and confidentiality laws created a tremendous amount of individual stress. Cultural values and access to healthcare were also reported as stressors by some participants.
Stressors Related to Societal Stigm
Many youth reported on the role of societal stigma and discrimination and how it increased their experience of stress.
People discriminate…with people that have HIV and that is why it is so difficult for youth to accept that they have the condition. I think that’s it. -Female
Society has a large influence on one getting depressed because of the “what will they say” that affects us more than having the condition. Because I have the condition, but well, I am good but when I leave here [the clinic] it affects me, “Well, I am sick” and I think it’s mainly due to that society. -Female
The participants expressed concerns about gossip or rumors pertaining to their diagnosis. Fears were expressed about being labeled as promiscuous, a drug user, or a prostitute due to societal misconceptions of people living with HIV. Another common reaction experienced by the participants from other people was that the participant “looked for it” or in some way deserved to get HIV.
For you to be labeled like stamps on your face, I have HIV, so they know to avoid you and don’t cross the same street that you’re on, or don’t hold that pole that you just held. -Female
One worries about what people say. And that one the most … it’s not the family, not even my parents, not my son, it’s what all those other people are going to say. That they could reject me, discriminate against me, judge me without thinking that they could be a victim just like me. -Male
Stressors Related to Privacy/Confidentiality Laws
Violation of privacy and/or confidentiality laws was a major concern voiced by participants. Several participants shared experiences where the laboratory technicians, school nurses, or other hospital staff revealed their HIV status to other people without the adolescent’s authorization. One person revealed that a staff member at a pharmacy provided information to a family member about the purpose of the participant’s prescription thus, perhaps inadvertently, revealing the participant’s HIV status.
People look to find a way to find out … and … it is difficult because there is no confidentiality, there is no privacy, there isn’t … and one isn’t normal. Because you live with the fear that the people around you … what do they think about you? What could they say about me? -Female
Stressors Related to Cultural Values
Participants felt that the cultural emphasis on individuality in the United States, was a barrier to demystifying the HIV/AIDS stigma. They discussed that, in general, people were less likely to try to learn about HIV/AIDS unless they were directly impacted by the disease. Additionally, participants discussed how they felt society’s value on individualism facilitated the lack of empathy or understanding for people living with HIV.
Everybody is not gonna get involved until they’re put in a certain situation. I mean, because I can’t just tell you to go out… it’s like they already have World AIDS Day and stuff like that, but I mean, it’s people who are diagnosed or health practitioners, stuff like that, who are involved. I mean, most, normal society, they really don’t care. It’s not a big issue for them unless they’re directly being affected by it. -Male
Stressors Related to Health-care Access
The participants discussed how the lack of funding for quality health-care centers for children and adolescents can be a source of stress for youth newly diagnosed with HIV. In certain regions, there were very few doctors experienced in HIV treatment. Additionally, the lack of appropriate funding for HIV services and centers was another source of stress reported by participants. For example, if they wanted to move to another city or state, they would have to consider the treatment options available to them. Participants also reported that the quality of the medical care varied dramatically from rural to urban areas.
And that little boy needs support and in the Fajardo clinic there isn’t any and it is in dire condition. And he is a little boy that looks like it has affected him emotionally, mentally and of course, physically! And I know that these are things that we need to improve. I know that possibly there are no funds, but why! -Female
DISCUSSION
Youth recently diagnosed with HIV face challenges that they continually struggle with during the first year after receiving the diagnosis. The youth in this study described a range of stressors within multiple social-ecological systems that may be confounded by the typical challenges of normal adolescent development. In turn, these stressors can be exacerbated by living with a stigmatized and potentially life-threatening illness. Data gathered from both the focus groups and individual interviews provides a clearer understanding of the subjective experience of stress for youth newly diagnosed with HIV through an exploration of the challenges, strengths, and needed areas of support/assistance associated with receiving an HIV diagnosis.
Results from this study suggest that the first year after receiving an HIV diagnosis is very challenging for youth since they are experiencing multiple stressors across complex ecological systems. For youth, challenges in their microsystemic interactions were the most stressful, particularly those dealing with the actual HIV diagnosis and disclosure of their status to others. Youth reported being under enormous emotional stress during this critical period suggesting the need for more intensive services early after the diagnosis.
After the youth became aware of their diagnosis, they reported continually facing other challenges unique to HIV. First, these youth struggle with learning to accept the diagnosis. This period of acceptance was tumultuous for youth as they described intense feelings of depression, isolation, and at times, suicidal ideation. Youth described that many of their concerns were related to the lack of information about the disease that they had received, misinformation about HIV from various sources, and fears related to HIV medications and the development of physical symptoms.
Next, youth may contend with decisions around disclosure of their HIV status within multiple areas of their lives. Many of the youth reported worrying almost constantly about accidental disclosure, which created high levels of stress for them because of the fear that they may “slip up” when talking to someone and accidentally talk about their HIV status with someone to whom they had not yet disclosed. Choosing to disclose their HIV status to others and the process of disclosing was a major concern for this group. Although most HIV-positive youth reported struggling with disclosure, greater levels of stress were reported by those who were conflicted about disclosure to a family member, particularly their mother. The tremendous effort that these youth exert to maintain secrecy around their diagnosis may lead to negative mental health effects, while there is evidence that disclosure can lead to improved self-efficacy and increased social support, which in turn has positive effects for psychological well-being (Kalichman, DiMarco, Austin, Luke, & DiFonzo, 2003; Parsons et al., 2005; Zea, Reisen, Poppen, Bianchi, & Echeverry, 2005). However, the potential positive results of disclosure are dependent upon the acceptance and support of the person to whom the participant discloses.
Youth may also feel that they lack the skills to be able to identify someone they can trust and disclose their status in a knowledgeable manner while simultaneously having the emotional stability to deal with the outcome of the disclosure. Three primary types of relationships were discussed when describing the stress surrounding disclosure: family, friends/peers, and romantic/sexual partners. These relationships were seen as important to the youth and disclosure to individuals in each of these areas may have induced a great deal of stress. However, for some who were able to disclose their status to an important person in their lives, new sources of support and coping were created.
Compared to other ecological (Bronfenbrenner, 1979, 1986) and social-ecological (Kazak et al., 1995) models, similarities as well as distinct differences emerged from the data of the experiences of adolescents and young adults living with HIV. For example, similar to Kazak’s model, for youth living with HIV the microsystem includes the disease itself since many youth experience the demands and stressors of the illness directly. Conversely, while the mesosystem in Kazak’s model considers the interactions between caregivers and hospitals as well as the healthcare team, this did not hold up as well in our model since most of the youth were directly responsible for their disease management and did not have the traditional family caregivers that may be present with other chronic childhood illnesses. Other mesosystemic influences that appear unique to this population include the school-peer and family-partner interactions and relationships.
For children with other chronic illness, the exosystem is primarily a consideration of the parents’ or caregivers’ social networks and the extent to which the disease impacts those networks (Kazak et al., 1995). For youth living with HIV, the same type of influence on the social networks of the family members or caregivers was not as common since many of the families are unaware of the youth’s HIV status. While the participants did not speak about it directly, it is possible that once they disclosed their status to family or caregivers, there may have been some differential treatment within the extended family structure since several participants reported cases where previous relatives with HIV had been shunned by the family network. Another unique aspect of the exosystem for HIV-positive youth is their experience of the media and the presence of misinformation and misconceptions surrounding the HIV disease and AIDS.
Finally, compared to youth with other chronic illnesses, the macrosystem of youth living with HIV may include increased experiences with stress on the societal level due to the highly stigmatized nature of HIV. Additionally, where the macrosystem includes laws and policies that may directly impact the care and services available to children with pediatric illness, we found that youth living with HIV often perceived violation of these laws, particularly as they related to confidentiality and privacy.
Implications for Intervention Development
These data demonstrate a myriad of stressors experienced by adolescents and young adults living with HIV, particularly within the first year following the diagnosis. Because youth reported experiencing stressors in so many areas of their lives, it is important that interventions teach and/or enhance coping skills across the content domains. Interventions need to be developed to address the unique challenges faced by these youth, as opposed to adults living with HIV and youth perinatally infected with HIV, and should contain modules addressing HIV-specific concerns such as disclosure, relationships (i.e., family, peers, partners), school or work, the health-care system, and social stigma. Given the gender-specific concerns (i.e., pregnancy concerns for females) of some of the participants, it may be useful for interventions to be split by gender in order to sufficiently address these issues. While the focus group participants reported enjoying the group experience, many youth reported initial hesitancy. Thus, interventions for newly diagnosed youth may want to incorporate individual sessions prior to group sessions in order to prepare youth for the group experience.
Youth need to learn specific skills surrounding how to disclose their status to different types of people: school personnel, work/job colleagues/boss, family members, peers, romantic/sexual partners. Interventions may help by improving communication within the three primary relationship areas where the most assistance is needed: family, peers, and partners.
Youth also need to learn their legal rights related to confidentiality and information about what to do when those rights may be threatened. Local nonprofit agencies and large national agencies are often available to address these concerns. Fidelity to the respect of patient confidentiality and privacy in health care settings has profound implications to health care utilization by youth.
Strengths and Limitations
Many of the strengths of this study surround the diversity of the sample of a unique and understudied population. The participants represented a mix of males and females across ethnic groups and with geographic representation from the Midwest, East Coast, and Puerto Rico. Additionally, the methodology of using both focus groups and individual interviews allowed youth to choose the setting in which they felt most comfortable sharing sensitive information.
One major limitation of this study is the cross-sectional design. Only interviewing youth at one occasion did not allow the researchers to confirm the themes with the participants, nor allow the opportunity to delve deeper into the themes. The cross-sectional nature of the project also inhibited us from examining chronosystemic factors (Bronfenbrenner, 1986) that may impact the youth’s adjustment to their diagnosis over time. Another limitation may be the reliance of distal recall to explore the participants’ experiences being diagnosed with HIV. Our methodology specifically identified youth who had been diagnosed for over one year so that they could reflect back on the diagnosis experience. However, the distance between diagnosis and participation in the study could be a limitation of the study depending on the reliability of the participants self-report.
Future Research
Intervention development studies are needed in order to test the feasibility and acceptability of interventions for youth newly diagnosed with HIV. Studies should examine the type of setting most appropriate for conducting interventions as well as the format that is most acceptable to youth participants. Once preliminary efficacy can be established for an intervention, there is a need to translate and pilot interventions with Spanish-speaking youth as well. Descriptively, it would be useful for interventions to recruit larger sample sizes across ethnic groups in order to conduct ethnic specific analyses. It would also be valuable to follow youth longitudinally throughout the first year of living with HIV to explore differences among the frequency and intensity of psychosocial stressors over time.
Acknowledgments
The Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN) is funded by grant No. U01 HD040533–06 from the National Institutes of Health through the National Institute of Child Health and Human Development (Bill Kappogianis, MD; Sonia Lee, PhD; Audrey Smith Rogers, PhD, MPH) with supplemental funding from the National Institutes on Drug Abuse (Nicolette Borek, PhD), Mental Health (Susannah Allison, PhD; Pim Brouwers, PhD). We would like to thank Donna Futterman, MD, PI of the Adolescent Trials Unit at the Montefiore Medical Center and the staff of the Adolescent AIDS Program (Elizabeth Enriquez, Maria Campos); Jaime Martinez, MD, PI of the Adolescent Trials Unit at John Stroger, Jr. Hospital of Cook County and the staff of the Ruth M. Rothstein CORE Center (Lisa Henry-Reid, Kelly Bojan, Rachel Jackson); Irma Febo, MD, PI of the Adolescent Trials Unit and the staff at the Gamma Project, Cardiovascular Program, University of Puerto Rico (Evelyn Rivera and Hazel Ayala); and the staff at DePaul University, Department of Psychology (Eric Werner, Jessica Gehle, and Jason Johnson). ATN 055 has been scientifically reviewed by the ATN’s Behavioral Leadership Group. We would also like to thank individuals from the ATN Data and Operations Center (Westat, Inc.) including Jim Korelitz, PhD, Barbara Driver, RN, MSN, and Protocol Specialist, Julie Davidson, MSN; and individuals from the ATN Coordinating Center at the University of Alabama including Craig Wilson, MD; Cindy Partlow, MEd; Marcia Berck, BA; and Pam Gore. We would also like to acknowledge the thoughtful input given by participants of our national and local Youth Community Advisory Boards. We would also like to thank the young women and men who participated in this study for their willingness to share their stories with us.
References
- Aral SO. Sexually transmitted diseases: Magnitude, determinants and consequences. International Journal of STDs and AIDS. 2001;12(4):211–215. doi: 10.1258/0956462011922814. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development. American Psychologist. 1986;32:513–531. [Google Scholar]
- Brown LK, Lourie KJ, Pao M. Children and adolescents living with HIV and AIDS: A review. Journal of Child Psychology and Psychiatry. 2000;41(1):81–96. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . HIV incidence among young men who have sex with men—Seven U.S. cities, 1994–2000. MMWR. 2001;50(21):440–444. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS surveillance report. Atlanta, GA: Author; 2006. [Google Scholar]
- Creswell J. Qualitative inquiry and research design: Choosing among five traditions. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- Creswell JW. Research design: Qualitative, quantitative and mixed methods approaches. 2. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- Garofalo R, Harper G. Providing health care to the gay and bisexual male adolescent. Adolescent Medicine: State of the Art Reviews. 2003;14:595–611. doi: 10.1016/S1041349903500470. [DOI] [PubMed] [Google Scholar]
- Gavaghan MP, Roach JE. Ego identity development of adolescents with cancer. Journal of Pediatric Psychology. 1987;12(2):203–213. doi: 10.1093/jpepsy/12.2.203. [DOI] [PubMed] [Google Scholar]
- Greene K, Banjeree SC. Disease-related stigma: Comparing predictors of AIDS and cancer stigma. Journal of Homosexuality. 2006;50(4):185–209. doi: 10.1300/J082v50n04_08. [DOI] [PubMed] [Google Scholar]
- Hosek SG, Harper GW, Domanico R. The psychological and social difficulties of adolescents living with HIV: A qualitative analysis. Journal of Sex Education and Therapy. 2000;25(4):269–276. [Google Scholar]
- Hosek SG, Harper GW, Domanico R. Psychological predictors of medication adherence among HIV-infected youth. Psychology, Health, and Medicine. 2005;10(2):166–179. doi: 10.1080/1354350042000326584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosek SG, Harper GW, Robinson WL. Identity development in adolescents living with HIV disease. Journal of Adolescence. 2002;25(4):355–364. doi: 10.1006/jado.2002.0480. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, DiMarco M, Austin J, Luke W, DiFonzo K. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. Journal of Behavioral Medicine. 2003;26(4):315–332. doi: 10.1023/a:1024252926930. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Segal-Andrews AM, Johnson K. Pediatric psychology research and practice: A family/systems approach. In: Roberts MC, editor. Handbook of pediatric psychology. 2. New York: Guilford Press; 1995. [Google Scholar]
- Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis and violence: Geocoding and choice of area-based socioeconomic measures—The public health disparities geocoding project. Public Health Reports. 2003;118(3):240–260. doi: 10.1093/phr/118.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavigne J, Faier-Routman J. Psychological adjustment to pediatric physical disorders: A meta-analytic review. Journal of Pediatric Psychology. 1992;17:133–157. doi: 10.1093/jpepsy/17.2.133. [DOI] [PubMed] [Google Scholar]
- MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, et al. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: Opportunities for advancing HIV prevention in the third decade of HIV/AIDS. Journal of Acquired Immune Deficiency Syndrome. 2005;38(5):603–614. doi: 10.1097/01.qai.0000141481.48348.7e. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative data analysis. 2. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- Murphy DA, Durake SJ, Moscicki A, Vermund SH, Ma Y, Schwarz DF, et al. No change in health risk behaviors over time among HIV infected adolescents in care: The role of psychological distress. Journal of Adolescent Health. 2001;29(3):57–63. doi: 10.1016/s1054-139x(01)00287-7. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Wilson CM, Durako SJ, Muenz LR, Belzer M. Antiretroviral medication adherence among the REACH HIV-infected adolescent cohort in the USA. AIDS Care. 2001;13(1):27–40. doi: 10.1080/09540120020018161. [DOI] [PubMed] [Google Scholar]
- Muuss RE. Theories of adolescence. 6. New York: The McGraw-Hill Companies, Inc; 1996. Erik Erikson’s theory of identity development. [Google Scholar]
- Parsons JT, Schrimshaw EW, Bimbi DS, Wolitski RJ, Gomez CA, Halkitis PN. Consistent, inconsistent, and non-disclosure to casual sexual partners among HIV-seropositive gay and bisexual men. AIDS. 2005;19(Suppl 1):S87–97. doi: 10.1097/01.aids.0000167355.87041.63. [DOI] [PubMed] [Google Scholar]
- Patton MQ. Qualitative evaluation and research methods. 2. Newbury Park, CA: Sage; 1990. [Google Scholar]
- Pugatch D, Bennett L, Patterson D. HIV medication adherence in adolescents: A qualitative study. Journal of HIV/AIDS Prevention and Education for Adolescents and Children. 2002;5(1–2):9–29. [Google Scholar]
- Rao D, Ketwaletswe TC, Hosek SG, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care. 2007;19(1):28–33. doi: 10.1080/09540120600652303. [DOI] [PubMed] [Google Scholar]
- Sayer AG, Hauser ST, Jacobson AM, Willett JB, Cole CF. Developmental influences on adolescent health. In: Wallander JL, Siegel LJ, editors. Adolescent health problems. New York: Guilford Press; 1995. [Google Scholar]
- The Joint United Nations Program on HIV/AIDS. HIV/AIDS and young people: Hope for tomorrow. Geveva, Switzerland: Author; 2004. [Google Scholar]
- Valleroy LA, MacKellar DA, Karon JM, Rosen DH. HIV prevalence and associated risks in young men who have sex with men. Journal of American Medical Association. 2000;284(2):198–204. doi: 10.1001/jama.284.2.198. [DOI] [PubMed] [Google Scholar]
- Wallander JL, Thompson RJ. Psychosocial adjustment of children with chronic physical conditions. In: Roberts MC, editor. Handbook of pediatric psychology. 2. New York: Guilford Press; 1995. [Google Scholar]
- Wolitski RJ, Valdiserri RO, Denning PH, Levine WC. Are we headed for a resurgence in the HIV epidemic among men who have sex with men? American Journal of Public Health. 2001;91:883–888. doi: 10.2105/ajph.91.6.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zea MC, Reisen CA, Poppen PJ, Bianchi FT, Echeverry JJ. Disclosure of HIV status and psychological well-being among Latino gay and bisexual men. AIDS and Behavior. 2005;9(1):15–26. doi: 10.1007/s10461-005-1678-z. [DOI] [PubMed] [Google Scholar]