Abstract
Negative cognitive styles are an important cognitive vulnerability for depression, but stability of high cognitive risk, once developed, is unclear. The current study examined stability of cognitive vulnerability to depression in individuals at high and low cognitive risk (extreme scores on both the CSQ and DAS) over a 7-year period from late adolescence through early adulthood. Cognitive vulnerability showed high relative stability, as evidenced by the moderate to high correlation (rs = .62) between cognitive risk status at study onset and at final assessment 7 years later. Consistent with stability, subgroups were identified using growth mixture modeling, and most cognitively high-risk (62.22% for CSQ, 68.89% for DAS) and low-risk (55.05% for CSQ, 57.96% for DAS) participants showed stable trajectories of cognitive vulnerability. Despite this overall pattern of stability, small mean group changes were found, and a minority of participants showed changing trajectories, consistent with regression toward the mean. Predictors of change and implications for risk for depression in high- and low-risk individuals are discussed.
Keywords: cognitive vulnerability, depression, trajectory, stability
Once an individual develops vulnerability to depression, can it change without intervention? According to cognitive theories of depression (Abramson, Metalsky, & Alloy, 1989; Beck, 1967), some individuals have a characteristic way of negatively interpreting life events that provides risk for depression, and this vulnerability appears to coalesce and become fully operational during adolescence (Gibb & Alloy, 2006; Hankin & Abramson, 2001; Hyde, Mezulis, & Abramson, 2008). The current study examines stability of cognitive vulnerability to depression in individuals at high and low cognitive risk during the transition from late adolescence, when this vulnerability already has developed, to early adulthood, a critical developmental period (Arnett, 2000).
Cognitive Theories of Depression
Hopelessness theory (Abramson, Metalsky, & Alloy, 1989) and Beck’s (1967) theory of depression are both vulnerability-stress models in which a cognitive pattern serves as a vulnerability that interacts with negative events to predict depression. In hopelessness theory, the cognitive vulnerability is a negative cognitive style, or the tendency to make inferences that negative life events have stable and global causes, have significant negative consequences for the future, and are indicative of negative self-characteristics. This negative cognitive style interacts with the experience of negative life events to predict hopelessness, the proximal cause of depression in hopelessness theory.
In Beck’s theory of depression, the cognitive vulnerability is a negative self-schema containing dysfunctional attitudes involving themes of loss, failure, worthlessness, and inadequacy. When this self-schema is activated by negative life events, it leads to specific negative cognitions, or automatic thoughts, that are negative generalizations about the self, world and future (the negative cognitive triad). In Beck’s theory, the negative cognitive triad leads to depression.
Both conceptualizations of cognitive vulnerability to depression have received empirical support in numerous cross-sectional and prospective studies (see Abramson et al., 2002, for review). In general, empirical work indicates that both dysfunctional attitudes and negative cognitive style precede depressive episodes, as well as interact with negative life events to predict depression (although with some exceptions, e.g., Lewinsohn, Joiner, & Rohde, 2001).
Continuity and Change of Cognitive Vulnerability
Cognitive vulnerability is influential in the development of depression, but in order to fully understand the vulnerability, it is helpful to explore whether the vulnerability is stable or changes over time. Few studies have examined relative stability of dysfunctional attitudes, the cognitive vulnerability in Beck’s theory. Adult studies have found moderate to high stability of dysfunctional attitudes in depressed patients over time (r = .53 for 10-12 months; Dysfunctional Attitude Scale, DAS; Farmer, Harris, & Redman, 2001) or during treatment and post-treatment follow-up (r = .65 for 16 weeks, r = .76 for 18 months; DAS; Zuroff et al., 1999). Non-depressed adults showed high stability of dysfunctional attitudes as well (r = .70 for 10-12 months; DAS; Farmer et al., 2001). We are aware of only one study of stability of dysfunctional attitudes prior to adulthood, which found low stability in adolescents aged 11-17 (r = .34 for 5 months; Child Dysfunctional Attitude Scale, CDAS; Hankin, 2008).
Several studies have examined relative stability of attributional style or negative cognitive style, the cognitive vulnerability in hopelessness theory, during different developmental time periods. Cognitive vulnerability appears to be relatively unstable in childhood (r = .37 for 6 months, r =.29 for 1 year; Children’s Attributional Style Questionnaire, CASQ); however, by 3rd, 4th or 5th grade, the hypothesized diathesis-stress interaction is detectable (Gibb & Alloy, 2006; Nolen-Hoeksema, Girgus, & Seligman, 1992). Indeed, attributional style appears to solidify during adolescence (r = .41-.66 for 6- and 12-months; CASQ; Hankin, 2008; Garber & Flynn, 2001; Nolen-Hoeksema et al, 1992) and shows moderate to high stability during high school (r = .51 for 2 years, Adolescent Cognitive Style Questionnaire, ACSQ; Hankin & Abramson, 2002), college (r = .80 for 1 year; Cognitive Style Questionnaire, CSQ; Alloy et al., 2000), and across the adult lifespan (r = .54 for 52 years; Attributional Style Questionnaire, ASQ; Burns & Seligman; 1989).
The most comprehensive study of developmental stability of attributional style assessed children of three age cohorts longitudinally over four years using the CASQ (Cole et al., 2008). Results indicated that attributional style is cross-sectionally consistent across situations for children ages 7-14. However, attributional style first emerged as a trait-like factor at ages 9.5-14.5. Additionally, the predicted diathesis-stress interaction was first detectable at ages 12.5-13.5.
Overall, cognitive vulnerability begins to show fairly high relative stability during adolescence, such that individuals maintain their level of vulnerability relative to peers. However, does cognitive vulnerability show mean level stability or change developmentally over time? That is, regardless of whether individuals maintain relative rank in vulnerability, is there a developmental shift in vulnerability overall? Previous studies have found mixed results, with a meta-analysis of cross-sectional studies indicating differences in attributional style in different developmental stages (ASQ, CASQ, & CSQ; Mezulis, Abramson, Hyde, & Hankin, 2004), but other studies finding no mean change over time in adolescents (CASQ; Garber, Keiley, & Martin, 2002) and adults (DAS; Zuroff et al., 1999). Inferences from the latter two studies are complicated by use of a high-risk population (children of depressed mothers) and a post-treatment sample, respectively. Understanding the role of cognitive vulnerability in the development of depression requires exploration of how the vulnerability functions once developed across a full developmental time period and without focused therapeutic intervention.
The transition from late adolescence to early adulthood is an important developmental phase in which to explore continuity and change in cognitive vulnerability to depression. By this time, individuals have an established level of cognitive vulnerability (negative cognitive style; Alloy & Abramson, 2007; Hankin & Abramson, 2001; Hyde et al., 2008). The developmental phase from late adolescence to early adulthood is characterized by experimentation and change (Arnett, 2000), and individuals are encountering many dramatic life events during this time. Many factors that are associated with changes in cognitive vulnerability, such as episodes of depression (Abramson et al., 2002) and repeated or chronic negative events (Rose & Abramson, 1992; Garber & Flynn, 2001; Gibb et al., 2001, 2004; Nolen-Hoeksema, et al., 1992) would be expected to occur during this time period. Additionally, research suggests that most personality change occurs in young adulthood (Caspi, Roberts, & Shiner, 2005). Thus, if cognitive vulnerability does change in a naturalistic setting, the transition from late adolescence to early adulthood is a likely time frame for change to occur.
It is also important to explore the possibility of subgroups with different change trajectories. Like depression, cognitive vulnerability may be a heterogeneous construct. Indeed, development and changes of negative attributional style or cognitive style are influenced by numerous factors in addition to negative events and depressive episodes, such as genetic factors (Schulman, Keith, & Seligman, 1993), temperament (Mezulis, Hyde, & Abramson, 2006), and parental cognitive style (e.g., Alloy et al., 2001). Individuals may vary greatly in the number of factors influencing their level of cognitive vulnerability, and therefore may vary in stability of cognitive vulnerability over time as some of those factors change (e.g., parental influence) or continue to exert influence (e.g., temperament). Additionally, if some individuals have highly stable trajectories of cognitive vulnerability while others fluctuate over time, this information could inform further research on how to distinguish these subgroups to best focus interventions on those who show greatest continual risk for depression.
The Current Study
The current study examined mean level of change and relative stability of cognitive vulnerability to depression longitudinally across approximately 7 years for individuals at high and low cognitive risk for depression, based on both Beck’s theory and hopelessness theory, from late adolescence to early adulthood. Additionally, we examined whether subgroups exist within the sample showing different change trajectories, and whether experience of an episode of DSM-IV major depressive disorder (MDD) or treatment modified change trajectories.
The current study explores stability of cognitive vulnerability for individuals at high and low cognitive risk, rather than stability of cognitive vulnerability across a continuum. We chose this design because we are particularly interested in stability as it relates to risk for depression. This rationale is exemplified by analogy to high blood pressure and risk for heart disease. For the purposes of predicting heart disease, it is useful to know whether individuals who have high blood pressure at one time (and are therefore at heightened risk for heart disease) will continue to have high blood pressure (and continue to be at risk). Similarly, for the purposes of predicting depression, it is useful to know whether individuals who are high in cognitive vulnerability (and are therefore at heightened risk for depression) will continue to be at risk over time.
Additionally, the current study examines stability of cognitive vulnerability in individuals at high and low cognitive risk based on both Beck’s theory and hopelessness theory. We chose these joint risk criteria to maximize the potential risk conferred to participants in the risk groups.
We predicted several possibilities for mean change over time. Although negative cognitive styles precede and predict depression, they continue to be correlated with depression once it is experienced (see Abramson et al., 2002 for review). Thus, changes in level of cognitive vulnerability over time may map on to changes in depression rates from adolescence to young adulthood. Previous research indicates a dramatic increase in both depression rates (Hankin et al., 1998) and negative attributional style (Mezulis et al., 2004) during adolescence. If this increase continues into early adulthood, it is expected that cognitive vulnerability would increase over time in the sample. However, research on depression rates beyond adolescence suggests that depression rates may decrease across the college years (Wong & Whitaker, 1993) or that depressive symptoms show high stability from adolescence to adulthood (Lewinsohn, Pettit, Joiner, & Seeley, 2003). Although changes in cognitive vulnerability may be consistent with changes in depression prevalence, it is unclear from the previous literature how depression rates change during this time frame.
We predicted that experience of an episode of MDD would be associated with higher levels of cognitive vulnerability over time, and that treatment would be associated with lower levels of cognitive vulnerability over time. Predictions of subgroups in the sample with unique trajectories are exploratory.
Method
Participants
Participants were from the Cognitive Vulnerability to Depression (CVD) Project, a longitudinal, behavioral high-risk study spanning approximately 7 years. Participants were recruited at both Temple University and the University of Wisconsin using a two-phase screening procedure that was identical at both sites. Details of and rationale for the selection procedure are detailed elsewhere (Alloy & Abramson, 1999). In Phase I of the screening process, 5,378 college freshmen (2,438 at Temple University and 2,940 at University of Wisconsin) completed the Cognitive Style Questionnaire (CSQ; Alloy et al., 2000), which assesses the cognitive vulnerability featured in hopelessness theory, and the Dysfunctional Attitudes Scale (DAS; Weissman & Beck, 1978), which assesses the cognitive vulnerability featured in Beck’s theory.
Both the CSQ and DAS have been supported as reliable and valid measures of cognitive vulnerability to depression. The CSQ assesses the internality, stability and globality of causal attributions, inferred consequences, and implications about self-worth for 24 hypothetical negative and positive events. Coefficient alpha (n = 5378) for the negative event composite was .88 and test-retest reliability over one year (n=347) was r = .80 (Alloy et al., 2000) in the CVD Project.
The CSQ has also been validated in other studies (see Haeffel, et al., 2008, for a review). Haeffel et al. (2005) found the CSQ had high internal consistency in adolescents and adults (alpha = .93). Additionally, scores on the CSQ predict inferences about naturally occurring negative life events (Metalsky et al., 1987, 1993; Alloy et al., 2000; Panzarella, Alloy, & Whitehouse, 2006), and high scores on the CSQ show the predicted relationship with information-processing deficits seen in depression (Alloy et al., 1997). Finally, extensive support for the CSQ has been found in the cross-sectional, retrospective and prospective studies, including the CVD Project, which found a relationship between cognitive vulnerability and depression (see Abramson et al., 2002 and Alloy et al., 2006 for reviews).
The DAS used in the CVD Project was an expanded form of the original scale that assessed dysfunctional attitudes about perfectionism and concern about others’ approval. The expanded version had an additional 24 items, added to better assess dysfunctional beliefs in achievement and interpersonal domains. Coefficent alpha (n=5378) was .90 and test-retest reliability over one year (n=349) was r = .78 in the CVD Project (Alloy et al., 2000).
The DAS has also been validated in other studies. Haeffel et al. (2005) found good internal consistency (alpha = .88). Nelson, Stern, and Cicchetti (1992) found that 73% of participants with high DAS scores had independently assessed depression versus 36% of participants with low DAS scores. Finally, extensive support for the DAS has been found in the cross-sectional, retrospective and prospective studies, including the CVD Project, which found a relationship between cognitive vulnerability and depression (see Abramson et al., 2002 and Alloy et al., 2006, for reviews).
Based on the initial screening, 619 potential high-risk participants (261 at Temple University and 358 at University of Wisconsin) and 585 potential low-risk participants (234 at Temple University and 351 at University of Wisconsin) were identified. To be identified as high- or low-risk, participants at each site had to score in the highest and lowest quartiles, respectively, on both the DAS (high-risk item score cut point ≥ 3.69 at Temple University and ≥ 3.81 at University of Wisconsin; low-risk item score cut point ≤ 2.60 at Temple University and ≤ 2.86 at University of Wisconsin) and the composite CSQ for negative events (high-risk item score cut point ≥ 4.43 at Temple University and ≥ 4.50 at University of Wisconsin; low-risk item score cut point ≤ 3.30 at Temple University and ≤ 3.47 at University of Wisconsin).
A randomly selected subset of high-risk and low-risk participants who were younger than 30 years old were recruited for Phase 2 screening. There were 313 high-risk participants (167 at Temple University and 146 at University of Wisconsin) and 236 low-risk participants (130 at Temple University and 106 at University of Wisconsin) invited for Phase 2 screening, at which they completed an expanded Schedule for Affective Disorders and Schizophrenia – Lifetime (SADS-L) interview (Endicott & Spitzer, 1978) and also several self-report measures of depression and psychopathology, including the Beck Depression Inventory (BDI; Beck, Rush, Shaw, & Emery, 1979). Participants with current Diagnostic and Statistical Manual of Mental Disorders (3rd ed., rev.; DSM-III-R; American Psychiatric Association, 1987) or Research Diagnostic Criteria (RDC; Spitzer, Endicott, & Robins, 1978) diagnosis of any episodic or chronic mood disorder, current diagnosis of any other Axis I disorder, current psychotic symptoms, past history of mania, hypomania, bipolar disorder, or cyclothymia, and serious medical illness were excluded. Participants with a previous depressive disorder who had remitted for a minimum of two months were included in the sample if they met all other criteria, based on logic that selecting cognitively vulnerable participants with no history of a mood disorder would inappropriately bias the sample to include only those cognitively vulnerable participants who were especially resistant to developing depression (see Alloy et al., 2000 for elaboration of this logic).
The 209 high-risk (114 at Temple University and 95 at University of Wisconsin) and 207 low-risk (110 at Temple University and 97 at University of Wisconsin) eligible participants who met Phase 2 screening criteria were invited to participate in the prospective phase of the study. Eighteen eligible high-risk (14 at Temple University and 4 at University of Wisconsin) and 13 eligible low-risk (9 at Temple University and 4 at University of Wisconsin) participants refused participation in the prospective phase of the study. Another 16 high-risk (15 at Temple University and 1 at University of Wisconsin) and 24 low-risk (20 at Temple University and 4 at University of Wisconsin) were excluded from analyses due to factors such as inability to locate participant, five or more missed appointments, or poor English-speaking ability.
The final sample included in the current analyses consisted of 175 high-risk (85 at Temple University and 90 at University of Wisconsin) and 170 low-risk (81 at Temple University and 89 at University of Wisconsin) participants. The samples at each site were similar in CSQ and DAS scores, but differed on ethnic composition, socioeconomic status (SES), age, and screening BDI scores. A higher proportion of Temple University participants were minorities, and Temple University participants had lower mean parental education and income, were older, and had higher initial BDI scores than University of Wisconsin participants (see Table 1 for sex, ethnicity, and age demographic information; see Alloy et al., 2000, for more details of cohort composition). Not all participants completed all prospective assessments; however, participants with missing data were retained in the current analyses. See Table 2 for mean CSQ and DAS scores for each risk group at each assessment.
I. Demographic Information for Final Sample.
| UW | TU | |||
|---|---|---|---|---|
| High Risk | Low Risk | High Risk | Low Risk | |
| Age (Mean, SD) | 18.10 (SD = 0.43) |
18.14 (SD = 1.12) |
18.78 (SD = 2.12) |
19.99 (SD = 3.95) |
| Sex (% Female) | 69% | 67% | 66% | 68% |
| Ethnicity (%) | ||||
| Caucasian | 96% | 92% | 64% | 53% |
| African-American | 0% | 3% | 17% | 31% |
| Asian | 0% | 2% | 5% | 1% |
| Hispanic | 0% | 1% | 2% | 5% |
| Other/ Not Specified |
0% | 1% | 1% | 5% |
II. Mean CSQ and DAS Item Scores at Each Assessment.
| High Risk | Low Risk | ||||
|---|---|---|---|---|---|
| CSQ | DAS | CSQ | DAS | ||
| Assessment | |||||
| 1 | M | 5.08 | 4.41 | 2.77 | 2.24 |
| SD | 0.49 | 0.60 | 0.43 | 0.34 | |
| N | 171 | 171 | 166 | 166 | |
| 2 | M | 4.85 | 4.00 | 2.99 | 2.27 |
| SD | 0.72 | 0.77 | 0.68 | 0.49 | |
| N | 174 | 175 | 170 | 170 | |
| 3 | M | 4.78 | 3.70 | 3.29 | 2.35 |
| SD | 0.75 | 0.78 | 0.78 | 0.54 | |
| N | 166 | 166 | 167 | 167 | |
| 4 | M | 4.73 | 3.66 | 3.30 | 2.36 |
| SD | 0.82 | 0.81 | 0.83 | 0.55 | |
| N | 152 | 150 | 154 | 153 | |
| 5 | M | 4.63 | 3.64 | 3.32 | 2.34 |
| SD | 0.89 | 0.84 | 0.80 | 0.63 | |
| N | 128 | 128 | 128 | 127 | |
| 6 | M | 4.72 | 3.52 | 3.29 | 2.36 |
| SD | 0.86 | 0.79 | 0.81 | 0.67 | |
| N | 96 | 97 | 115 | 116 | |
| 7 | M | 4.68 | 3.65 | 3.29 | 2.32 |
| SD | 0.81 | 0.76 | 0.78 | 0.65 | |
| N | 88 | 87 | 112 | 114 | |
Procedure
Participants completed the CSQ and DAS questionnaires 7 times: at initial screening (Phase 1), follow-up screening (Phase 2), and then at approximately yearly prospective assessments over 5 years. Participants also completed the SADS-L diagnostic interview at Phase 2 assessments and the SADS-Change (SADS-C) every six weeks after that for approximately 3 years. After that, participants completed SADS-C diagnostic interviews every 4 months.
Analysis
Correlation between initial and final cognitive risk status and hierarchical linear modeling(HLM; Bryk & Raudenbush, 1987) were used to determine relative stability and mean level of change, respectively. HLM is a good fit to examine overall group trajectories because it allows for missing data. Growth mixture modeling (GMM; Nagin, 1999) was then used to examine subgroups. This technique is an excellent fit for the study and for answering the proposed research questions because it allows for identification of distinct trajectories rather than just an overall trend for all participants. Both HLM and GMM also allow for determination of the factors that predict group membership and any identified trajectories, respectively. Current analyses included experience of DSM-IV episode of MDD and receipt of treatment occurring throughout the study as predictor variables.
Additionally, GMM allows for calculation of the percentage of the sample belonging to each trajectory (Nagin, 1999). GMM also accommodates missing data, unequal intervals between assessment times and different assessment periods for different participants, all of which are important factors for examining data from a longitudinal study like the CVD project.
Results
Relative Stability of Cognitive Vulnerability
Relative stability of cognitive vulnerability to depression for individuals at both high and low cognitive risk was examined using correlation between risk group membership at the beginning and end of the study (approximately 7 years). Using the same cut points for the CSQ and the DAS from original group classification, participants were classified as high-, moderate- and low-risk based on their scores from the final cognitive vulnerability assessment. Again, participants were classified as high- and low-risk only if scores on both measures were in the upper or lower quartile, respectively. The correlation between group membership at the beginning and end of the study was significant, rs = .62, p < .001, indicating high relative stability over the 7 years as participants at high and low cognitive risk transitioned from late adolescence to early adulthood. Correlations between group membership at each time point showed similar stability (see Table 3).
III. Correlation Matrix For Group Membership Using Original Cut Points at Each Time Point (Spearman’s Rho)*.
| Time Point | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1 | 1.00 | ||||||
| 2 | .787 | 1.00 | |||||
| 3 | .675 | .723 | 1.00 | ||||
| 4 | .696 | .712 | .755 | 1.00 | |||
| 5 | .672 | .693 | .691 | .779 | 1.00 | ||
| 6 | .663 | .593 | .685 | .671 | .684 | 1.00 | |
| 7 | .622 | .696 | .655 | .706 | .714 | .699 | 1.00 |
All correlations are significant at the 0.01 level (2-tailed).
Another useful way to approach stability of CSQ and DAS over time is to consider the sample sites separately, one as an initial sample and the second as a replication. The correlation between group membership at the beginning and end of the study for University of Wisconsin was significant, rs = .60, p < .001, and the replication in the Temple University sample was also significant, rs = .68, p < .001.
Consistent with these correlations, the vast majority of participants did not “change colors”, or transition to the other extreme risk group. Indeed, only four participants (.02% of high-risk participants) changed from high- to low-risk group status. No participants changed from low- to high-risk group status. Approximately 27% of all participants were classified differently for final CSQ and DAS scores than their original classification, with most of these changing to a moderate risk level that did not meet either high- or low-risk group criteria. The percentage of participants who changed to a moderate risk level was similar for each risk group (28% for low-risk participants; 26% for high-risk participants).Thus, 72% of low-risk participants retained low-risk status, and approximately 74% of high-risk participants retained high-risk status.
Mean Change for Different Risk Groups
A hierarchical linear model (HLM) for variable occasion designs was used to determine mean change modeled by age for participants at high and low cognitive risk on both the CSQ and DAS separately. Intercept-only, linear, and nonlinear growth trajectories were fit using restricted maximum likelihood estimation and the results reported are based on the robust standard errors.
Next, DSM-IV diagnosis of an episode of MDD occurring during the study (binary; present or not at any time) and treatment during the study (binary; present or not at any time) were included as level one time-varying covariates to examine if these factors (that occurred during the course of the study) modified growth trajectories. Finally, gender was included as a level two predictor of intercept and slope.
The first model specified included the intercept only. Linear and quadratic components, time-varying covariates, and the group-level predictor were added one at a time and change in model fit was assessed. Model components that significantly improved fit according to Chi-square model comparisons were retained.
CSQ High-risk Trajectories
The final model for CSQ scores for high-risk participants included random intercept, linear slope, and nonlinear slope components. This model fit the data significantly better than a model with linear slope only, Chi-square (3, N = 175) = 30.84, p < .001), and addition of covariates failed to improve fit. There was a positive correlation between intercept and linear slope (r = .36), such that participants with higher initial CSQ scores showed a greater decrease in CSQ score over time. There was a negative correlation between intercept and nonlinear slope (r = −.59), such that participants with higher initial CSQ scores showed less change in linear slope over time. There was also a negative correlation between linear slope and nonlinear slope (r = −.88), such that participants with steeper linear slopes showed less change in linear slope over time.
The intercept coefficient was 5.02, which indicates the average CSQ score at initial assessment. The linear slope coefficient was significant, t(174) = −4.70, p < .001, such that participants showed an average decrease in CSQ score of 0.13 points between each assessment. The nonlinear slope coefficient was significant, t(174) = 2.47, p = .02, such that participants showed an average positive change in linear slope of CSQ score over time.
Taken together, the HLM analyses suggest that there was some decrease in CSQ scores for high-risk participants that changed in rate over time, such that the rate of decrease in CSQ scores lessened.
DAS High-risk Trajectories
The final model for DAS scores for high-risk participants included random intercept, linear slope, and nonlinear slope components. This model fit the data significantly better than a model with linear slope only, Chi-square (3, N = 175) = 45.73, p < .001), and addition of covariates failed to improve fit. There was a slight positive correlation between intercept and linear slope (r = .11), such that participants with higher initial DAS scores showed a greater decrease in DAS score over time. There was a negative correlation between intercept and nonlinear slope (r = −.26), such that participants with a higher initial DAS score showed less change in linear slope over time. There was also a negative correlation between linear slope and nonlinear slope (r = −.92), such that participants with steeper linear slopes showed less change in linear slope over time.
The intercept coefficient was 4.27, which indicates the average DAS score at initial assessment. The linear slope coefficient was significant, t(174) = −9.72, p < .001, such that participants showed an average decrease in DAS score of 0.26 points between each assessment. The nonlinear slope coefficient was significant, t(174) = 5.84, p < .001, such that participants showed a positive change in linear slope of DAS score over time.
Taken together, the HLM analyses suggest that there was some decrease in DAS scores for high-risk participants that changed in rate over time, such that the rate of decrease in DAS scores lessened. These results are largely consistent with those found for CSQ scores for high-risk participants.
CSQ Low-risk Trajectories
The final model for CSQ scores for low-risk participants included random intercept, linear slope, and nonlinear slope components. This model fit the data significantly better than a model with linear slope only, Chi-square (3, N = 170) = 43.24, p < .001), and addition of covariates failed to improve fit. There was a positive correlation between intercept and linear slope (r = .64), such that participants with higher initial CSQ scores showed a greater increase in CSQ score over time. There was a negative correlation between intercept and nonlinear slope (r = −.86), such that participants with a higher initial CSQ scores showed less change in linear slope over time. There was also a negative correlation between linear slope and nonlinear slope (r = −.94), such that participants with steeper linear slopes showed less change in linear slope over time.
The intercept coefficient was 3.04, which indicates the average CSQ score at initial assessment. The linear slope coefficient was significant, t(169) = 7.18, p < .001, such that participants showed an average increase in CSQ score of 0.12 points between each assessment. The nonlinear slope coefficient was significant, t(169) = −6.12, p < .001, such that participants showed a negative change in linear slope of CSQ score over time.
Taken together, the HLM analyses suggest that there was some increase in CSQ scores for low-risk participants that changed in rate over time, such that the rate of increase of CSQ scores lessened.
DAS Trajectories for Low-risk Participants
The final model for DAS scores for low-risk participants included random intercept, linear slope, and nonlinear slope components. This model fit the data significantly better than a model with linear slope only, Chi-square (3, N = 170) = 21.89, p < .001, and addition of covariates failed to improve fit. There was a positive correlation between intercept and linear slope (r = .60), such that participants with higher initial DAS scores showed a greater increase in DAS score over time. There was a negative correlation between intercept and nonlinear slope (r = −.97), such that participants with a higher initial DAS score showed less change in linear slope over time. There was also a negative correlation between linear slope and nonlinear slope (r = −.77), such that participants with steeper linear slopes showed less change in linear slope over time.
The intercept coefficient was 2.30, which indicates the average DAS score at initial assessment. The linear slope coefficient was significant, t(169) = 3.69, p = .001, such that participants showed an average increase in DAS score of 0.04 points between each assessment. The nonlinear slope coefficient was significant, t(169) = −3.61, p = .001, such that participants showed a negative change in linear slope of DAS score over time.
Taken together, the HLM analyses suggest that there was some increase in DAS scores for low-risk participants that changed in rate over time, such that the increase in DAS scores lessened. These results are largely consistent with those found for CSQ scores for low-risk participants.
Summary of HLM Analyses
The results of HLM analyses of mean change for high- and low-risk participants indicate decreases and increases over time, respectively, on both the CSQ and DAS. The rates of linear change lessened over time for both high- and low-risk participants.
Additionally, those high-risk participants with the highest CSQ and DAS scores showed the greatest decreases over time, consistent with regression toward the mean. In contrast, those low-risk participants with the highest CSQ and DAS scores (and thus those who were less extreme within the low-risk group) showed the greatest increases over time.
Empirically Identifying Cognitive Vulnerability Subgroup Trajectories
Individual growth trajectories were examined using growth mixture modeling (GMM), a semi-parametric, group-based approach that identifies distinct groups in the population and their growth patterns (Nagin, 1999). SAS PROC TRAJ, a platform for SAS, was used in the analyses (Jones, Nagin, & Roeder, 2001). Trajectories were modeled by age across 7 time points covering approximately 7 years (varying per participant).
Growth trajectories were examined separately for high- and low-risk participants using CSQ scores and DAS scores. The highest order polynomial specified was quadratic. For each model, non-significant higher-order polynomial trends were trimmed. First, a single group model was specified, followed by increasing numbers of groups up to a 5 group model, using an approximation of the Bayes information criterion (BIC) log Bayes factor to evaluate change in model fit. The log form of the Bayes factor is interpreted as evidence favoring the alternative model. A log form of the Bayes factor of 0 to 2 indicates evidence not worth mentioning, 2 to 6 indicates positive evidence, 6 to 10 indicates strong evidence and >10 indicates very strong evidence against the null model (Jones et al., 2001). Next, predictor variables were added to the models. Experience of an episode of MDD and treatment during the course of the study were included in the model as binary time-varying covariates. Because these factors were not defined prior to entry into the study, they were analyzed as time-varying covariates rather than stable risk factors and are analyzed as predictors of trajectory, rather than group membership. The current analysis evaluates the impact of the experience of these predictors at any time in the course of the study on change trajectories (Nagin, 2005). For each participant group analysis, the reported model fit is based on the unconditional form of the model. Group membership statistics are based on the full model with predictors.
CSQ High-Risk Trajectories
A four-group model had the most parsimonious fit for CSQ trajectories for high-risk participants (change in log BIC of 15.14 vs. 14.04 for a five-group solution; a fifth trajectory group was rejected because it consisted of only 4.4% of participants). Support for the four-group solution was seen in the high average posterior probability of group membership (.84; Nagin, 2005). CSQ high-risk trajectory groups are shown in Figure 1. The largest group of participants (43.20% of the sample; 95% CI: 37.97%, 48.43%; average probability of group membership = .83) showed a moderately high start point and stable trajectory. One other group showed a stable trajectory with a higher start point (19.02% of the sample; 95% CI: 14.87%, 23.17%, average probability of group membership = .83). Combined, these two stable trajectory subgroups include a majority of high-risk participants (62.22%). A third group (25.49% of the sample; 95% CI: 20.83%, 30.15%; average probability of group membership = .84) showed a moderately high start point and slightly decreasing trajectory. The remaining group (12.30% of the sample; 95% CI: 8.99%, 15.61%; average probability of group membership = .88) decreased over time.
Figure 1.
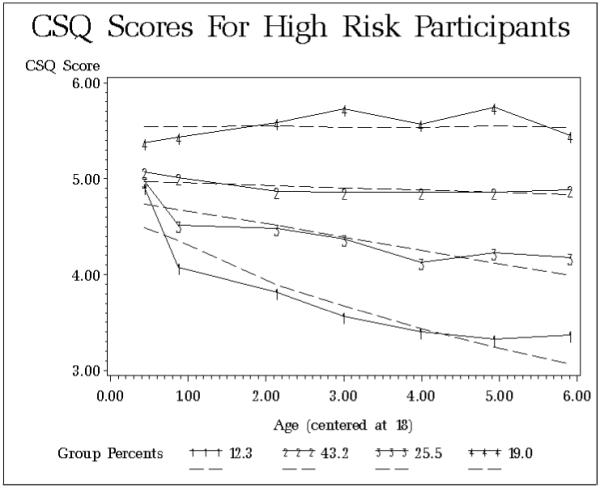
CSQ trajectories for high-risk participants.
When considered alone, experience of an episode of MDD was not a significant predictor of CSQ trajectory for any subgroup. When considered alone, treatment was a significant predictor of CSQ trajectory in one subgroup. High-risk participants who showed a high and stable trajectory had lower CSQ scores if they received treatment, t(174) = −3.15, p < .002.
When both predictors were included, experience of an episode of MDD was a significant predictor of trajectories for two subgroups. High-risk participants who showed a decreasing trajectory had higher CSQ scores if they experienced an episode of MDD, t(174) = 2.45, p = .02. High-risk participants who showed a slightly decreasing trajectory also had higher CSQ scores if they experienced an episode of MDD, t(174) = 2.96, p = .003. When both predictors were included, treatment was a significant predictor of trajectories for two subgroups. High-risk participants who showed a decreasing trajectory, t(174) = 2.44, p = .01, had higher CSQ scores if they received treatment. High-risk participants who showed a high and stable trajectory had lower CSQ scores if they received treatment, t(174) = −3.69, p < .001.
CSQ high-risk subgroups varied on percentage of participants experiencing an episode of MDD and treatment. The decreasing trajectory group had the highest prevalence of an episode of MDD (24%), and the remaining subgroups had prevalence that ranged from 10-17%. In contrast, the high stable trajectory group had the highest prevalence of treatment (19%), and the remaining subgroups had prevalence that ranged from 7-11%.
DAS High-Risk Trajectories
A four-group model most parsimoniously fit the DAS trajectories for high-risk participants (change in log BIC of 15.62 vs. 3.72 for a five-group solution; a fifth trajectory group was rejected because it consisted of only 7.3% of participants). Further support for the four-group model was found in the high average posterior probability of group membership (.83). DAS high-risk trajectory groups are shown in Figure 2. The largest group of participants (40.80% of the sample; 95% CI: 35.03%, 46.57%; average probability of group membership = .79) showed a stable DAS score trajectory over time. The next largest group (28.09% of the sample; 95% CI: 22.63%, 33.55%; average probability of group membership = .75) showed a slightly decreasing trajectory but was mostly stable over time. Combined, these two mostly stable trajectory groups included a majority of participants (68.89%). The next largest group (16.18% of the sample; 95% CI: 11.96%, 20.40%; average probability of group membership = .90) decreased over time. The final group (14.93% of the sample; 95% CI: 9.47%, 20.39%; average probability of group membership = .89) had a high start point and showed a slight decrease over time.
Figure 2.
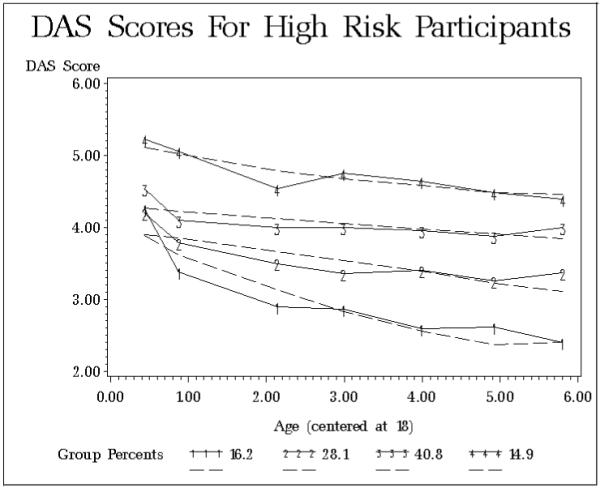
DAS trajectories for high-risk participants.
When considered alone, experience of an episode of MDD was a significant predictor of DAS trajectory in one subgroup. High-risk participants who showed a moderate start and slightly decreasing trajectory had higher DAS scores if they experienced an episode of MDD, t(174) = 2.33, p = .02. When considered alone, treatment was a significant predictor of DAS trajectory in one subgroup. High-risk participants who showed a moderate start and slightly decreasing trajectory had higher DAS scores if they received treatment, t(174) = 2.47, p < .01.
When both predictors were included, experience of an episode of MDD was a significant predictor of trajectories for one subgroup. High-risk participants who showed a stable trajectory had lower DAS scores if they experienced an episode of MDD, t(174) = −2.84, p = .01. When both predictors were included, treatment was a significant predictor of trajectories for two subgroups. High-risk participants who showed a decreasing trajectory had lower DAS scores if they received treatment, t(174) = −2.17, p = .03. In contrast, high-risk participants who showed a moderate start and slightly decreasing trajectory had higher DAS scores if they received treatment, t(175) = 2.38, p = .02.
DAS high-risk subgroups varied on percentage of participants experiencing an episode of MDD and treatment. Three subgroups had comparable prevalence of episodes of MDD (approximately 16%), with lower prevalence in the moderate start and slightly decreasing trajectory group (10%). Three subgroups had comparable prevalence of treatment (approximately 9%), with higher prevalence in the stable trajectory group (16%).
Summary: High-Risk Trajectories
The majority of high-risk participants showed stable CSQ and DAS trajectories over time. The remaining participants showed decreasing trajectories, potentially indicative of regression toward the mean. The relationships between experience of an episode of MDD or treatment during the study and subgroup trajectories were not consistent and often contradictory within and across measures. When both predictors were included, experience of an episode of MDD was associated with increased CSQ scores for some subgroups; however, treatment was associated with both increased and decreased CSQ scores for different subgroups. In contrast, experience of an episode of MDD was associated with decreased DAS scores for one subgroup, and treatment again was associated with both increased and decreased DAS scores for different subgroups.
CSQ Low-Risk Trajectories
A four-group model had the most parsimonious fit for CSQ trajectories for low-risk participants (change in log BIC of 42.68 vs. 7.56 for a five-group solution; a fifth trajectory group was rejected for interpretability, as it was redundant with other trajectories). The four-group model was further supported by a high average posterior probability of group membership (.88). CSQ low-risk trajectory groups are shown in Figure 3. The largest group of participants (36.87% of the sample; 95% CI: 30.19%, 43.55%; average probability of group membership = .80) and one other group of participants (18.18% of the sample; 95% CI: 13.73%, 22.63%; average probability of group membership = .89) showed stable trajectories with different start points. Combined, these two stable trajectory groups include a majority of low-risk participants (55.05%). Another group showed a slight early increase and then stable trajectory (36.63% of the sample; 95% CI: 30.22%, 43.03%; average probability of group membership = .87) and the remaining group showed an increasing trajectory (8.31% of the sample; 95% CI: 4.68%, 11.94%; average probability of group membership = .95).
Figure 3.
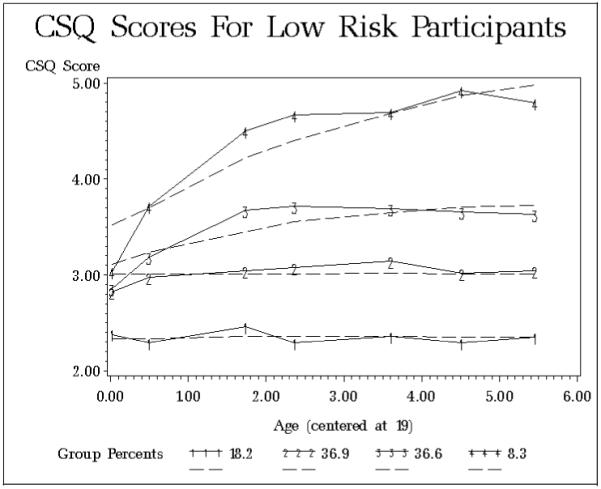
CSQ trajectories for low-risk participants.
When considered alone, experience of an episode of MDD was a significant predictor of CSQ trajectory in one subgroup. Low-risk participants who showed an increasing trajectory had lower CSQ scores if they experienced an episode of MDD, t(169) = −2.66, p = .01. When considered alone, treatment was not a significant predictor of CSQ trajectory for any subgroup.
When both predictors were included, results were similar to individual predictor analyses. For low-risk participants who showed an increasing trajectory, experience of an episode of MDD significantly predicted lower CSQ scores, t(169) = −3.03, p = .003. Treatment was not a significant predictor of CSQ trajectories.
CSQ low-risk subgroups varied on percentage of participants experiencing an episode of MDD and treatment. The increasing trajectory subgroup had the highest prevalence of an episode of MDD (7%), and prevalence for the remaining three subgroups ranged from 0-3%. Similarly, the increasing trajectory subgroup had the highest prevalence of treatment (14%), and prevalence for the remaining three subgroups ranged from 3-8%.
DAS Low-Risk Trajectories
A three-group model most parsimoniously fit the data for the DAS trajectories for low-risk participants (change in log BIC of 108 vs. −7.76 for a four-group solution; a negative change in log BIC indicates a decrement in fit). Further support for the three-group solution was found in the high average posterior probability of group membership (.91). DAS low-risk trajectories are shown in Figure 4. The majority of participants (57.96% of the sample; 95% CI: 53.24%, 62.68%; average probability of group membership = .90) had a stable trajectory. Another group (n = 45; 25.87% of the sample; 95% CI: 21.65%, 30.09%; average probability of group membership = .90) showed a slight increase over time. A third group decreased over time (16.17% of the sample; 95% CI: 12.93%, 19.41%; average probability of group membership = .93).
Figure 4.
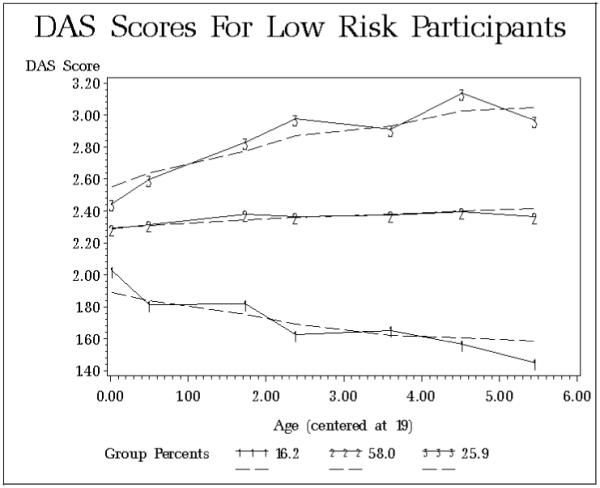
DAS trajectories for low-risk participants.
When considered alone, experience of an episode of MDD was a significant predictor of DAS trajectory in one subgroup. Low-risk participants who showed a slightly increasing trajectory had lower DAS scores if they experienced an episode of MDD, t(169) = −2.78, p = .01. When considered alone, treatment was a significant predictor of DAS trajectory for one subgroup. Low-risk participants who showed a decreasing trajectory had higher DAS scores if they received treatment, t(169) = 4.02, p < .001.
When both predictors were included, results were similar to individual predictor analyses. For low-risk participants who showed a slightly increasing trajectory, experience of an episode of MDD significantly predicted lower DAS scores, t(169) = −2.67, p = .01. For low-risk participants who showed a decreasing trajectory, treatment significantly predicted higher DAS scores, t(169) = 4.19, p < .001.
DAS low-risk subgroups varied on percentage of participants experiencing an episode of MDD and treatment. The increasing trajectory subgroup had the highest prevalence of an episode of MDD (4%), and prevalence for the remaining two subgroups was approximately 2%. In contrast, the decreasing trajectory subgroup had the highest prevalence of treatment (12%), while the increasing trajectory subgroup sought no treatment (0%) and the stable subgroup fell between these extremes (6%).
Summary: Low-Risk Trajectories
The majority of low-risk participants showed stable CSQ and DAS trajectories over time. Most of the remaining participants showed increasing trajectories, potentially indicative of regression toward the mean. One subgroup showed decreasing DAS scores over time. Experience of an episode of MDD or treatment during the study significantly predicted trajectories in some subgroups, but patterns were in the opposite direction of the expected effects. When both predictors were included, an episode of MDD predicted lower CSQ and DAS scores for one subgroup each. For the DAS, treatment predicted higher scores for one subgroup.
Dual-Trajectory Analysis
A dual-trajectory analysis was performed to examine whether changes in cognitive vulnerability over time differed between measures. A dual-trajectory analysis allows for direct comparison of trajectories for two contemporaneous measures, in this case the DAS and CSQ. It is an improvement over simple correlation analyses because it allows full use of the entire longitudinal dataset (Jones & Nagin, 2007).
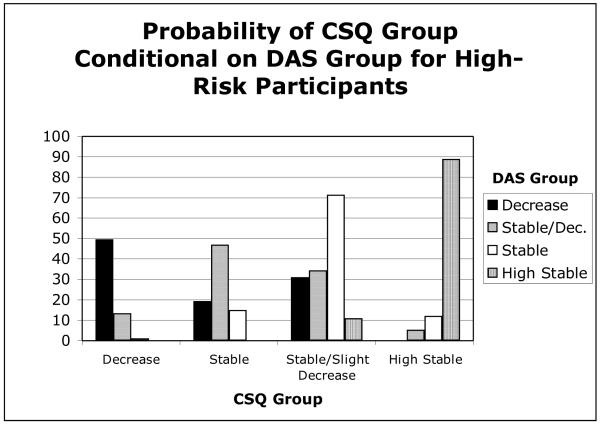
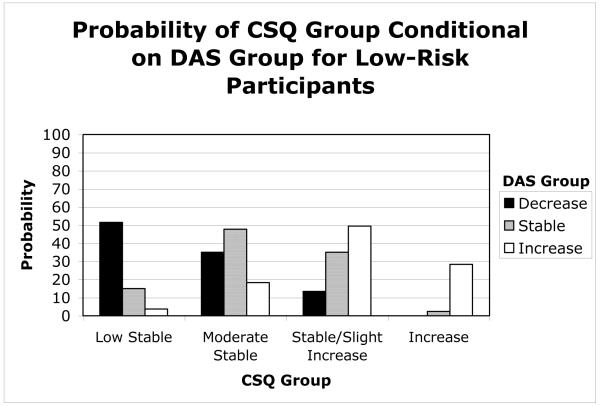
A summary of the dual-trajectory analysis can be found in Figures 5 and 6 for high-risk and low-risk participants, respectively. Probability of membership in each CSQ group was calculated, given membership in DAS group. These probabilities were calculated separately for each risk group. For both risk groups, the highest probability of membership for each CSQ group corresponded with membership in a DAS group with a similar trajectory. For example, high-risk participants were most likely to be assigned to the CSQ decreasing trajectory group if they were assigned to the DAS decreasing trajectory group. Overall, it appears that CSQ and DAS group memberships were generally consistent, suggesting that both measures assessed cognitive vulnerability similarly.
Figure 5.
Relationship between DAS and CSQ trajectories for high-risk participants.
Figure 6.
Relationship between DAS and CSQ trajectories for low-risk participants.
Discussion
Relative Stability
The current study found considerable relative stability in cognitive vulnerability to depression (based on both Beck’s theory and hopelessness theory) during the transition from late adolescence to early adulthood, as evidenced by the moderate to high correlation (rs = .62) between cognitive risk status at study onset and at final assessment 7 years later. Individuals at high cognitive risk at study onset tended to remain at high cognitive risk, while individuals at low cognitive risk tended to remain at low cognitive risk. Indeed, 72% of low-risk participants retained low-risk status, and approximately 74% of high-risk participants retained high-risk status. The level of stability found in the current study is comparable to the 2-year stability of attributional style found by Hankin and Abramson (2002) in a high school sample, consistent with the hypothesis that cognitive styles coalesce during adolescence. Although the current study’s correlation was lower than the test-retest correlation found for cognitive style by Alloy et al. (2000) among college students, that is to be expected considering the difference in time interval of approximately 7 years in the current study and 1 year in the Alloy et al. study. The current findings are also consistent with the stability estimates of attributional style for adults across the life span found by Burns and Seligman (1989).
Consistent with stability of cognitive vulnerability, very few participants in the current study “changed colors” from high- to low-risk and vice versa. However, it is of interest that some participants did change from high- or low-risk to a more moderate level of cognitive vulnerability. This finding is consistent with regression toward the mean, and may also be due in part to the extreme nature of the risk groups in the current study. Given that participants were selected based on extreme scores on two measures of risk, participants changing to moderate risk level no longer may have been high- or low-risk on both measures, but may have remained high- or low-risk based on one of the two measures alone.
Mean Level of Change
Although the overall pattern of results suggests considerable stability of high and low cognitive risk for depression, examination of mean level of change revealed significant linear and nonlinear trends. For high-risk participants, CSQ and DAS scores showed decreasing trends that lessened in rate over time, while for low-risk participants, CSQ and DAS scores showed increasing trends that lessened in rate over time. Again, these trends most likely represent regression toward the mean. Additionally, inclusion of experience of an episode of MDD or treatment during the study as covariates did not significantly improve the models.
Subgroup Trajectories
Patterns of mean stability and potential regression towards the mean found in the growth mixture modeling (GMM) analyses were similar to those in the hierarchical linear modeling (HLM) analyses. The current study did identify multiple trajectories of change in cognitive vulnerability to depression from late adolescence to early adulthood. However, for both the CSQ and DAS, and for both high- and low-risk participants, the majority of the sample exhibited a mostly stable trajectory over time. Deviations from these trajectories were most frequently decreasing scores for high-risk participants and increasing scores for low-risk participants. Again, this pattern is consistent with regression toward the mean.
Experience of an episode of MDD or treatment during the study significantly predicted trajectories for several subgroups; however, no consistent patterns emerged and effects were often in the opposite direction than predicted. There are several possible explanations for these results. First, the nature of the predictors may be more complex than assumed in the original predictions. For example, treatment may be an indicator of experience of an episode of MDD and may not have been successful. Therefore, treatment may be associated with higher levels of cognitive vulnerability rather than lower levels for some participants.
Second, the overall majority of participants did not experience episodes of MDD or treatment, and this is particularly true of low-risk participants. When predictors were analyzed at the level of subgroups, individual participants with unusual experiences may have largely influenced the results. Consistent with this hypothesis, episodes of MDD and treatment were significant predictors of trajectories most frequently in non-majority subgroups. The number of participants included in each of these smaller subgroups is likely insufficient to appropriately test for influence of rarely-occurring predictors.
Summary of Analyses
Across all analyses, results consistently showed stability of cognitive vulnerability over time for individuals at high and low cognitive risk. Change that was observed represented decreases and increases over time for high- and low-risk participants, respectively. These changes are consistent with regression towards the mean, and this pattern was reflected in all analyses. However, regression toward the mean would work against findings of stability, and it is noteworthy that results showed considerable relative stability despite potential regression toward the mean. In fact, if all participants had regressed from extreme groups to more moderate risk, the relative stability of risk group membership would be nil.
Taken together, the current results suggest that cognitive vulnerability to depression is quite a stable trait once it solidifies during adolescence. We predicted that changes in cognitive vulnerability would map onto changes in depression rates, and stability in the current study is consistent with high stability of depression prevalence in a similar time frame (Lewinsohn et al., 2003).
Our results are also contrary to the prediction of increasing cognitive vulnerability beyond adolescence. Although attributional style may become increasingly negative and depression rates increase during adolescence, our results suggest that this increase may hit an asymptote and become trait-like by the time individuals reach late adolescence and young adulthood, consistent with findings of Cole et al. (2008).
The high relative stability and low mean change found in the current study have important implications for the understanding of risk for depression. Because cognitive vulnerability has been found to be an important risk factor for depression, the current findings indicate that the augmented risk for depression in vulnerable adolescents who are high in both negative cognitive style and dysfunctional attitudes will continue to provide risk throughout early adulthood. This has important implications for how to approach intervention and treatment for depression. If depression is treated with no attention to cognitive vulnerability, the vulnerable cognitive style may remain and continue to place the recovered individual at greater risk for experiencing another episode of depression. If, however, cognitive vulnerability is targeted and changed through treatment, there is greater hope that recurrences of depression can be avoided (Hollon et al., 1990).
Limitations
Although the current study provided strong evidence that, once developed, cognitive vulnerability to depression is a stable trait across late adolescence to early adulthood, there are several limitations of the current study. First, although HLM and GMM account for missing data and uneven time intervals, it is important to note that many participants did not complete all 7 assessments of cognitive vulnerability.
Second, the current study used an extreme groups approach rather than a continuous variable approach to examine stability of cognitive vulnerability to depression. However, stability of cognitive vulnerability across the continuum is an interesting question in its own right, which should be addressed in future research. Furthermore, we identified participants as high- and low-risk if they scored in the top and bottom quartiles on both the CSQ and DAS, respectively. Although we used these dual-risk criteria to maximize level of risk for depression, it is unclear whether the current results generalize to stability of cognitive risk based on one of these measures alone.
To address this issue, we examined the screening data for participants in the CVD project and found moderate overlap between participants identified as high- and low-risk based on either the CSQ or DAS alone, and participants identified using both the CSQ and DAS as in the present study. Percentages of participants who qualified as high- or low-risk on the CSQ or DAS alone, using quartile cutoffs, who also qualified as high- or low-risk on both the CSQ and DAS (as in the present study) ranged from 45-47%. That nearly half of the participants who qualified for risk group status on either measure alone also qualified for risk group status using both measures suggests some generalizability of the current results to individuals at-risk based on either measure alone.
Although the current results do not address stability of cognitive vulnerability across the continuum, the high-risk participants in the current study represent an interesting group of individuals who may be at particularly high risk for depression, and understanding the nature of cognitive vulnerability in these individuals is useful to inform intervention in this vulnerable population. Indeed, previous results from the CVD project indicate that individuals at high cognitive risk based on both the DAS and CSQ are significantly more likely to experience a depressive episode prospectively (Alloy et al., 2006).
Third, participants in the current study were undergraduate students at the University of Wisconsin or Temple University. Young adults who attend college may differ in important ways from other young adults, and may show different trajectories in cognitive vulnerabilities over time than those who do not attend college. However, although all participants in the current study were undergraduate students at the outset, the generalizability of the current findings is supported by the similar findings at University of Wisconsin and Temple University. Temple University participants were significantly older and from families with significantly lower SES than University of Wisconsin participants, and the Temple University sample was more ethnically and racially diverse than the University of Wisconsin sample. However, the stability data from both sites were remarkably similar.
Fourth, the current study was not able to address whether stability of cognitive vulnerability was due to stability of other variables. For instance, it is possible that stability of depressive symptoms affected stability of cognitive vulnerability. However, experience of an episode of MDD in the current study did not predict changes in cognitive vulnerability trajectories. It is possible that subthreshold depressive symptoms do affect stability of cognitive vulnerability, and this cannot be clearly determined from the current study.
However, data from the CVD project indicates that individuals at high cognitive risk were more likely to experience first onsets and recurrences of depressive episodes over time, even after controlling for depressive symptoms (Alloy et al., 2006). This suggests that even if stability of depressive symptoms contributes to stability of cognitive vulnerability, cognitive vulnerability is providing additional risk for depression above and beyond previous experience of depression. Thus, stability of this risk factor (even if partially due to some other factor) is important for understanding risk for depression.
It is also possible that participant factors, such as temperament, interpersonal skills, attractiveness, or health were stable over time, and that these factors all impact cognitive vulnerability. Stability over time could be due largely to stability of other factors that influence cognitive vulnerability. Consistent with this hypothesis, previous research has found a relationship between early temperament, especially negative withdrawal tendencies, and negative cognitive style in response to negative life events (Mezulis, et al., 2006). Because the current study cannot differentiate between the stability of cognitive vulnerability and the stability of other participant factors, results must be interpreted with caution. However, if individuals with certain temperaments are more likely to have high levels of cognitive vulnerability to depression, stability of either factor over time contributes to understanding stability of risk for depression.
Environmental factors, such as socioeconomic status and life events also could be stable over time and impact cognitive vulnerability. However, this explanation is less plausible, as environmental variables are likely to change from late adolescence to early adulthood during the transition into college and eventually into careers and new family roles (Arnett, 2000). Additionally, individuals with a negative cognitive style and dysfunctional attitudes have been found to experience more negative life events that those without these cognitive vulnerabilities, consistent with a stress generation hypothesis (Safford, Alloy, Abramson, & Crossfield, 2007). Therefore, even if environmental factors are stable over time, this may be partly due to cognitive vulnerability level, rather than the other way around.
Finally, late adolescence to early adulthood has been emphasized as an important developmental context in which to study stability of cognitive vulnerability to depression. However, few studies have carefully examined stability of cognitive vulnerability over time, and it is important to extend the current research by conducting longitudinal research of individuals across different developmental time frames.
Conclusion
Depression is one of the most burdensome diseases (WHO; in Murray & Lopez, 1996), and earlier interventions that target a risk factor before an individual develops depression may be the key to reducing the economic and social burden of the illness. Our results suggest that once cognitive vulnerability has formed in adolescence, it is stable and continues to provide risk for depression into adulthood, and therefore such interventions may need to occur in adolescence or earlier. More careful examination of how and when cognitive vulnerability to depression develops and solidifies as a risk factor may help in the development and implementation of intervention programs.
References
- Abramson LY, Alloy LB, Hankin BL, Haeffel GJ, MacCoon DL, Gibb BE. Cognitive vulnerability-stress models of depression in a self-regulatory and psychobiological context. In: Gotlib IH, Hammen CL, editors. Handbook of Depression. 2nd ed. The Guilford Press; New York: 2002. pp. 268–294. [Google Scholar]
- Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: A theory based subtype of depression. Psychological Review. 1989;96:358–372. [Google Scholar]
- Alloy LB, Abramson LY. The adolescent surge in depression and emergence of gender differences: A biocognitive vulnerability-stress model in developmental context. In: Romer D, Walker EF, editors. Adolescent psychopathology and the developing brain: Integrating brain and prevention science. Oxford University Press; New York: 2007. pp. 284–312. [Google Scholar]
- Alloy LB, Abramson LY. The Temple-Wisconsin Cognitive Vulnerability to Depression (CVD) Project: Conceptual background, design, and methods. Journal of Cognitive Psychotherapy: An International Quarterly. 1999;13:227–262. [Google Scholar]
- Alloy LB, Abramson LY, Hogan ME, Whitehouse WG, Rose DT, Robinson MS, Kim RS, Lapkin JB. The Temple – Wisconsin Cognitive Vulnerability to Depression Project: Lifetime history of Axis I psychopathology in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2000;109:403–418. [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Murray LA, Whitehouse WG, Hogan ME. Self-referent information processing in individuals at high and low cognitive risk for depression. Cognition and Emotion. 1997;11:539–568. [Google Scholar]
- Alloy LB, Abramson LY, Tashman NA, Berrebbi DS, Hogan ME, Whitehouse WG, Crossfield AG, Moroco A. Developmental origins of cognitive vulnerability to depression: Parenting, cognitive, and inferential feedback styles of the parents of individuals at high and low cognitive risk for depression. Cognitive Therapy and Research. 2001;25:397–423. [Google Scholar]
- Alloy LB, Abramson LY, Whitehouse WG, Hogan ME, Panzarella C, Rose DT. Prospective incidence of first onsets and recurrences of depression in individuals at high and low cognitive risk for depression. Journal of Abnormal Psychology. 2006;115:145–156. doi: 10.1037/0021-843X.115.1.145. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3rd ed., rev. Author; Washington, DC: 1987. [Google Scholar]
- Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. [PubMed] [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. Harper & Row; New York: 1967. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. Guilford Press; New York: 1979. [Google Scholar]
- Bryk AS, Raudenbush SW. Application of hierarchical linear models to assessing change. Psychological Bulletin. 1987;101:147–158. [Google Scholar]
- Burns MO, Seligman MEP. Explanatory style across the life span: Evidence for stability over 52 years. Journal of Personality and Social Psychology. 1989;56:471–477. doi: 10.1037//0022-3514.56.3.471. [DOI] [PubMed] [Google Scholar]
- Caspi A, Roberts BW, Shiner RL. Personality development: Stability and change. Annual Review of Psychology. 2005;56:453–484. doi: 10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- Cole DA, Ciesla JA, Dallaire DH, Jacquez FM, Pineda AQ, LaGrange B, Truss AE, Folmer AS, Tilghman-Osborne C, Felton JW. Emergence of attributional style and its relation to depressive symptoms. Journal of Abnormal Psychology. 2008;117:16–31. doi: 10.1037/0021-843X.117.1.16. [DOI] [PubMed] [Google Scholar]
- Endicott J, Spitzer RA. A diagnostic interview: The Schedule for Affective Disorders and Schizophrenia. Archives of General Psychiatry. 1978;35:837–844. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- Farmer A, Harris T, Redman K. The Cardiff Depression Study: A sib-pair study of dysfunctional attitudes in depressed probands and healthy control subjects. Psychological Medicine. 2001;31:627–633. doi: 10.1017/s0033291701003932. [DOI] [PubMed] [Google Scholar]
- Garber J, Flynn C. Predictors of depressive cognitions in young adolescents. Cognitive Therapy and Research. 2001;25:353–376. [Google Scholar]
- Garber J, Keiley MK, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology. 2002;70:79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Gibb BE, Abramson LY, Alloy LB. Emotional maltreatment from parents, verbal peer victimization, and cognitive vulnerability to depression. Cognitive Therapy and Research. 2004;28:1–21. [Google Scholar]
- Gibb BE, Alloy LB. A prospective test of the hopelessness theory of depression in children. Journal of Clinical Child and Adolescent Psychology. 2006;35:264–274. doi: 10.1207/s15374424jccp3502_10. [DOI] [PubMed] [Google Scholar]
- Gibb BE, Alloy LB, Abramson LY, Rose DT, Whitehouse WG, Donovan P, Hogan ME, Cronholm J, Tierney S. History of childhood maltreatment, negative cognitive styles, and episodes of depression in adulthood. Cognitive Therapy and Research. 2001;25:425–446. [Google Scholar]
- Haeffel GJ, Abramson LY, Voelz ZR, Metalsky GI, Halberstadt L, Dykman BM, Donovan P, Hogan ME, Hankin BL, Alloy LB. Negative cognitive styles, dysfunctional attitudes, and the remitted depression paradigm: A search for the elusive cognitive vulnerability to depression factor among remitted depressives. Emotion. 2005;5:343–348. doi: 10.1037/1528-3542.5.3.343. [DOI] [PubMed] [Google Scholar]
- Haeffel G, Gibb BE, Metalsky GI, Alloy LB, Abramson LY, Hankin BL, Joiner TE, Swendsen J. Measuring cognitive vulnerability to depression: Development and validation of the Cognitive Style Questionnnaire. Clinical Psychology Review. 2008;28:824–836. doi: 10.1016/j.cpr.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL. Stability of cognitive vulnerabilities to depression: A short-term prospective multiwave study. Journal of Abnormal Psychology. 2008;117:324–333. doi: 10.1037/0021-843X.117.2.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127:773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Measuring cognitive vulnerability to depression in adolescence: Reliability, validity and gender differences. Journal of Clinical Child and Adolescent Psychology. 2002;31:491–504. doi: 10.1207/S15374424JCCP3104_8. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hollon SD, Evans MD, DeRubeis RJ. Cognitive mediation of relapse prevention following treatment for depression. In: Ingram RE, editor. Contemporary psychological approaches to depression: Theory, research, and treatment. Plenum Press; New York: 1990. [Google Scholar]
- Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychological Review. 2008;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS. Advances in Group-based Trajectory Modeling and a SAS Procedure for Estimating Them. Sociological Methods and Research. 2007;35:542–571. [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods and Research. 2001;29:374–393. [Google Scholar]
- Lewinsohn PM, Joiner TE, Jr., Rohde P. Evaluation of cognitive diathesis-stress models in predicting major depressive disorder in adolescents. Journal of Abnormal Psychology. 2001;110:203–215. doi: 10.1037//0021-843x.110.2.203. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Pettit JW, Joiner TE, Jr., Seeley JR. The symptomatic expression of major depressive disorder in adolescents and young adults. Journal of Abnormal Psychology. 2003;112:244–252. doi: 10.1037/0021-843x.112.2.244. [DOI] [PubMed] [Google Scholar]
- Metalsky GI, Halberstadt LJ, Abramson LY. Vulnerability to depressive mood reactions: Toward a more powerful test of the diathesis-stress and causal mediation components of the reformulated theory of depression. Journal of Social and Personality Psychology. 1987;52:386–393. doi: 10.1037//0022-3514.52.2.386. [DOI] [PubMed] [Google Scholar]
- Metalsky GI, Joiner TE, Hardin TS. Depressive reactions to failure in a naturalistic setting: A test of the hopelessness and self-esteem theories of depression. Journal of Abnormal Psychology. 1993;102:101–109. doi: 10.1037//0021-843x.102.1.101. [DOI] [PubMed] [Google Scholar]
- Mezulis AH, Abramson LY, Hyde JS, Hankin BL. Is there a universal positivity bias in attributions? A meta-analytic review of individual, developmental, and cultural differences in the self-serving attributional bias. Psychological Bulletin. 2004;130:711–747. doi: 10.1037/0033-2909.130.5.711. [DOI] [PubMed] [Google Scholar]
- Mezulis AH, Hyde JS, Abramson LY. The developmental origins of cognitive vulnerability to depression: Temperament, parenting, and negative life events in childhood as contributors to negative cognitive style. Developmental Psychology. 2006;42:1012–1025. doi: 10.1037/0012-1649.42.6.1012. [DOI] [PubMed] [Google Scholar]
- Murray CJL, Lopez AD. The global burden of disease: Summary. Harvard University Press; Cambridge, MA: 1996. [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: A semiparametric, group based approach. Psychological Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-based modeling of development. Harvard University Press; Cambridge, Massachusetts: 2005. [Google Scholar]
- Nelson LD, Stern SL, Cicchetti DV. The Dysfunctional Attitude Scale: How well can it measure depressive thinking? Journal of Psychopathology and Behavioral Assessment. 1992;14:217–223. [Google Scholar]
- Nolen-Hoeksema S, Girgus J, Seligman MEP. Predictors and consequences of childhood depressive symptoms: A 5-year longitudinal study. Journal of Abnormal Psychology. 1992;101:405–422. doi: 10.1037//0021-843x.101.3.405. [DOI] [PubMed] [Google Scholar]
- Panzarella C, Alloy LB, Whitehouse WG. Expanded hopelessness theory of depression: On the mechanisms by which social support protects against depression. Cognitive Therapy and Research. 2006;30:307–333. [Google Scholar]
- Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychological Bulletin. 2000;126:3–25. doi: 10.1037/0033-2909.126.1.3. [DOI] [PubMed] [Google Scholar]
- Rose DT, Abramson LY. Developmental predictors of depressive cognitive style: Research and theory. In: Cicchetti DT, editor. Developmental perspectives on depression. University of Rochester Press; Rochester, NY: 1992. pp. 323–349. S.L. [Google Scholar]
- Safford SM, Alloy LB, Abramson LY, Crossfield AG. Negative cognitive style as a predictor of negative life events in depression-prone individuals: A test of the stress generation hypothesis. Journal of Affective Disorders. 2007;99:147–154. doi: 10.1016/j.jad.2006.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulman P, Keith D, Seligman MEP. Is optimism heritable: A study of twins. Behaviour Research and Therapy. 1993;31:569–574. doi: 10.1016/0005-7967(93)90108-7. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E. Research diagnostic criteria: Rationale and reliability. Archives of General Psychiatry. 1978;35:773–782. doi: 10.1001/archpsyc.1978.01770300115013. [DOI] [PubMed] [Google Scholar]
- Weissman A, Beck AT. Development and validation of the Dysfunctional Attitudes Scales: A preliminary investigation; Paper presented at the meeting of the American Educational Research Association; Toronto, Canada. 1978. [Google Scholar]
- Wong JL, Whitaker DJ. Depressive mood states and their cognitive and personality correlates in college students: They improve over time. Journal of Clinical Psychology. 1993;49:615–621. doi: 10.1002/1097-4679(199309)49:5<615::aid-jclp2270490503>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Zeiss AM, Lewinsohn PM. Enduring deficits after remissions of depression: A test of the scar hypothesis. Behaviour Research and Therapy. 1988;26:151–158. doi: 10.1016/0005-7967(88)90114-3. [DOI] [PubMed] [Google Scholar]
- Zuroff DC, Blatt SJ, Sanislow CA, Bondi CM, Pilkonis PA. Vulnerability to depression : Reexamining state dependence and relative stability. Journal of Abnormal Psychology. 1999;108:76–89. doi: 10.1037//0021-843x.108.1.76. [DOI] [PubMed] [Google Scholar]