Abstract
Objectives
Acupressure, a complementary and alternative medicine (CAM) treatment, uses fingertips, rather than needles, to stimulate acupoints on the skin and has been implicated as a successful treatment for a variety of medical disorders. However, acupressure’s underlying mechanisms remain unclear. One theory is that acupoint stimulation modulates autonomic nervous system activity. Previous studies have suggested that acupressure may positively affect heart rate and blood pressure. The current study investigated the effects of a type of acupressure, Jin Shin, on cardiovascular function in stroke survivors, a population that could especially benefit from a treatment promoting cardiovascular health. The study tested the hypothesis that active acupressure treatments would reduce heart rate and blood pressure (i.e., induce a greater relaxation response) above and beyond that seen during placebo acupressure treatments.
Methods
A randomised, placebo-controlled, single-blind crossover design was utilised, in which 16 participants received 8 weeks of either active or placebo acupressure followed by washout and crossover into the opposite treatment condition. Heart rate and blood pressure measurements were taken throughout treatments.
Results
Active acupressure treatments were associated with a significantly greater (p = .043, partial η2 =.30) and faster (p = .002, partial η2 = .76) reduction in heart rate compared to that seen during placebo treatments. No treatment effect on blood pressure was found.
Conclusions
Active acupressure reduced heart rate significantly more than did placebo acupressure during treatments. Although no treatment effect on blood pressure was found, this could be due to 67% of participants taking antihypertensive medications during the study.
Keywords: complementary medicine, humans, adults, heart rate, relaxation response
Acupressure, a complementary and alternative medicine (CAM) treatment, has been practiced for thousands of years and has become increasingly popular in the United States 1. Acupressure is particularly intriguing because, with appropriate instruction, acupressure can be learned by the novice individual, allowing for self-administered treatment independent of a practitioner, funds, or insurance. Although acupressure has shown efficacy for issues such as nausea 2, back pain 3, and depression 4, the underlying mechanisms remain unknown. Stimulation of acupoints on the skin is key to acupressure treatment. Consequently, to determine potential mechanisms, it is imperative to establish whether stimulation of acupoints elicits different physiological effects than stimulation of non-acupoints (points not designated in traditional Chinese medicine theory as acupoints). Stimulation of these points is not believed to elicit the same therapeutic effects as stimulation of real acupoints 5.
One theory is that acupoint stimulation may modulate the autonomic nervous system (ANS) by increasing parasympathetic nervous system (PNS) activity and suppressing sympathetic nervous system (SNS) activity 6–9. Modulation of the ANS can be assessed via heart rate and blood pressure, which are both increased by activation of the SNS and decreased by activation of the PNS 10. Previous studies in the literature have found acupressure treatment to significantly reduce heart rate 6, 11 and blood pressure 6. However, because appropriate control groups were not utilised, it remains unclear if stimulation of real versus placebo acupoints was responsible for the treatment effect.
Although the aforementioned studies suggest that ANS modulation may result from acupressure treatment, we are aware of no other studies in the English-language literature investigating this potential mechanism in the stroke population. ANS modulation could be of particular import to stroke survivors, as elevated heart rate and blood pressure following stroke have been found to increase mortality and/or risk of recurrent stroke 12, 13. Pilot data from our laboratory suggests that acupressure may affect cardiovascular function in stroke survivors: Active treatments resulted in greater heart rate reduction than placebo treatments 14. The present study attempts to replicate and extend these findings by utilizing a randomised, placebo-controlled, single-blind, cross-over design to assess the effects of acupressure (specifically, Jin Shin acupressure 15–17) on heart rate and blood pressure following stroke. It was hypothesised that active acupressure treatments would decrease heart rate and blood pressure over and above the reduction expected from placebo treatments.
METHODS
Participants
Participants at least 19 months post-stroke were recruited from the Denver/Boulder community via electronic and print media. Inclusion criteria required participants to have experienced a unilateral stroke, to have resulting persistent deficits (e.g., hemiplegia or hemiparesis), and to have a forearm skin-surface temperature differential between their affected and unaffected sides. Participants were excluded if they had previously experienced acupressure treatment, were currently undergoing treatment for acute non-stroke related issues (e.g., cancer), or if they had an unstable or degenerative chronic condition, such as Alzheimer’s disease. Prior to beginning the study, participants met with a physician at the Clinical Translation Research Center (CTRC) to ascertain their medical history and determine general health using electrocardiogram (ECG) and blood pressure measures. Only participants deemed physically fit for the study were included. Participants gave informed consent and all aspects of the present study were in accordance with and approved by the University of Colorado Institutional Review Board.
Design
A randomised, placebo-controlled, single-blind, cross-over design was used. Consented individuals were randomly assigned to condition A (Active Treatment Phase, Washout, Placebo Treatment Phase) or B (Placebo Treatment Phase, Washout, Active Treatment Phase) (see Table 1). The CTRC biostatistician used a random number generator to assign participants to condition in blocks of 2, and was responsible for all randomisation and maintenance of the blind. The practitioner was provided with a sealed envelope prior to each participant beginning their first treatment session, revealing the treatment she was to administer. As such, only the acupressure practitioner and the CTRC biostatistician knew the type of treatment being administered within each phase. Each treatment phase and the washout period lasted 8 weeks. The treatment phases consisted of active or placebo acupressure treatments occurring once per week for 40 minutes. Participants were blinded to which treatment condition they were assigned and all data collection, entry, and analyses were done by blinded individuals. The data presented here are part of a larger investigation of the effects of acupressure on functional recovery following stroke 18. Because the focus of the present study is only on heart rate and blood pressure during active and placebo acupressure treatments, only those measures will be discussed.
Table 1.
Experimental design.
| Random Assignment to A or B | ||
|---|---|---|
| First 8 weeks | Second 8 weeks | Third 8 weeks |
| A. Active phase | Washout period | Placebo phase |
| B. Placebo phase | Washout period | Active phase |
Procedure
All treatment sessions were administered at the CTRC at the University of Colorado at Boulder. During treatment sessions, participants lay face up on a massage table, fully clothed with shoes removed, as is common practice for acupressure treatments 15,16. A Jin Shin (acupressure) practitioner with over 20 years of clinical and educational experience and appropriate certification administered treatments (active or placebo) behind a closed curtain. The practitioner was also trained in use of the placebo acupoints14. The practitioner began treatment administration by holding the radial aspect of the participant's wrists (i.e., pulse diagnosis) with her fingertips, which determined the appropriate treatment sequence to begin the session. During treatment, the practitioner applied pressure with her fingertips to different sites (e.g., points) on the body, in sequence. After a sequence was complete, the radial wrists of the participants were held again by the practitioner to determine the next treatment sequence. The entire treatment, itself, lasted 40 minutes. The placebo control procedure was designed to be indistinguishable from the active treatment session, to last the same duration, and contain the same amount of physical contact. As with the active treatment, the practitioner began by holding the radial aspect of the participant's wrists for pulse diagnosis. The PI established a set of placebo acupressure points 14 not found on established acupressure point charts, each of which was assigned a number. Using a random number generator, these points were put into a matching sequence for each customary Jin Shin (acupressure) treatment. Consequently, if pulse diagnosis dictated treatment of the gall bladder, there was a placebo Gall Bladder treatment containing the same number of steps in matching sequence to the standard active Gall Bladder treatment. To guarantee matching practitioner/participant interactions for both treatment types, only scripted dialogue was used. A research assistant seated on the other side of the curtain was present during all treatment sessions to monitor the interaction between participants and the practitioner.
Heart Rate/Blood Pressure Measurements
A DINAMAP Pro 100 vital signs monitor (GE Healthcare) was used to measure heart rate and blood pressure during treatments. Once participants were supine, baseline heart rate and blood pressure were measured following a 5-minute rest period, after which the treatment began. Measurements were repeated every 5 minutes throughout treatment.
Expectancy and Credibility
Participants were asked to rate their expectancy levels 19 prior to each treatment phase by answering questions such as “how much improvement in your stroke symptoms do you think will occur?” on a scale of 0%–100%, with 100% indicating most improvement. After each treatment phase, participants rated treatment credibility 20 on a scale of 1–9 (with 9 indicating greater credibility), with questions such as “how reasonable does the treatment seem to you?”
Statistical Analyses
The data were analysed using SPSS 16.0 (Chicago, IL).
Heart Rate and Blood Pressure
For each participant, a heart rate change score was calculated to reflect heart rate change from baseline (prior to treatment initiation) to each 5-minute period during treatments in active and placebo phases. A repeated measures ANOVA was used to determine effects of treatment type, treatment number, and time point during treatment on heart rate and blood pressure (systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP)). Since previous studies in the literature have reported the effects of 20-minute acupressure treatments 6, 11, heart rate and blood pressure during the first 20 minutes of the 40-minute treatment were also analysed. To determine whether the 8-week washout period was sufficient to return participants to baseline heart rate and blood pressure, a paired t-test was used to determine if baseline heart rate and blood pressure were the same for both treatment phases (active and placebo).
Expectancy and Credibility
Differences in expectancy ratings prior to treatment were analysed using a paired-samples t-test to compare pre-active to pre-placebo expectancy ratings. To investigate differences in credibility ratings after treatment, a paired-samples t-test was used to compare post-active to post-placebo credibility ratings.
RESULTS
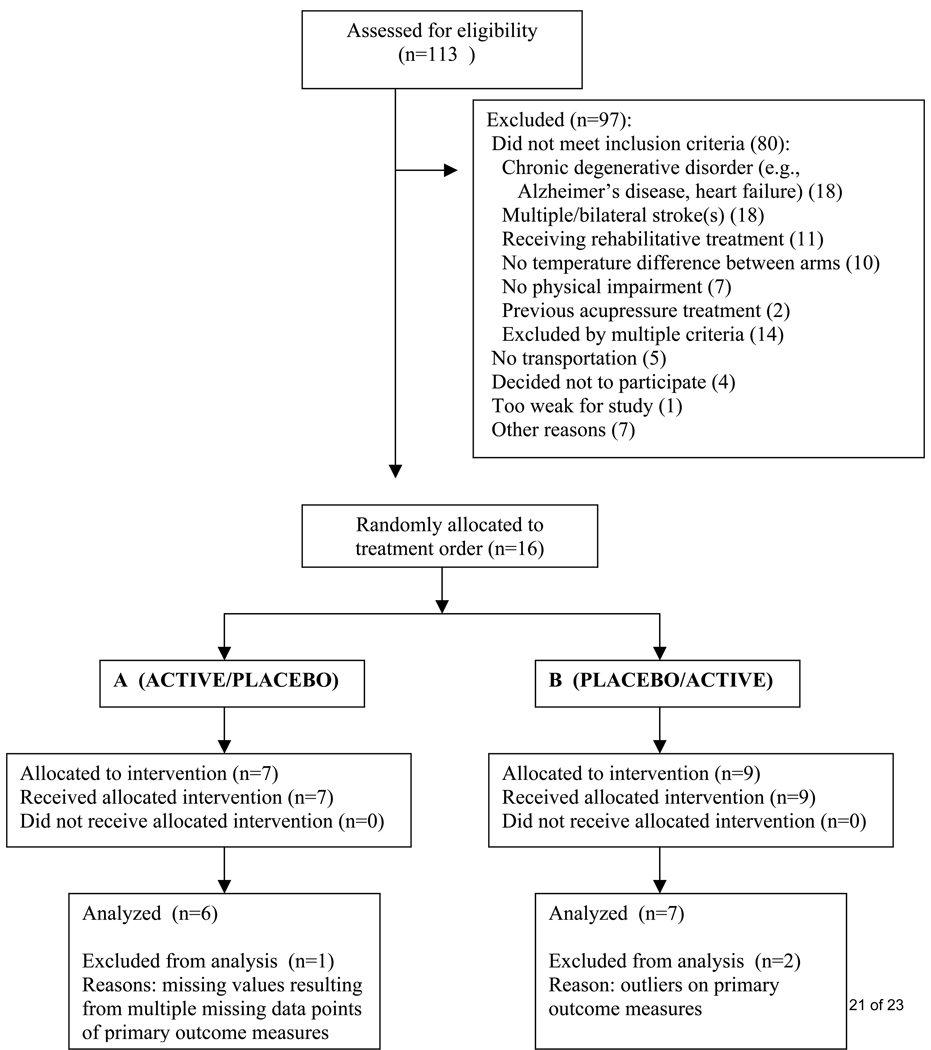
Participants
Of 113 candidates assessed for eligibility, 16 participants completed the study. The majority of candidates assessed were ineligible due to chronic debilitative conditions or having had multiple or bilateral strokes (see Figure 1). Of the 16 participants completing the study, 2 were excluded from analyses because their measurements were determined to be outliers, based on graphical observation and Grubbs’ outlier test 21. For personal reasons, one participant requested that heart rate and blood pressure measurements only be taken sporadically, resulting in missing data for most time points during treatments; consequently, data from this participant were not included. The remaining 13 participants were included in data analyses (see Table 2). Random assignment, unblinded at the end of the study, resulted in 6 participants receiving active acupressure treatments for the first phase and placebo acupressure treatments for the second phase; 7 participants received placebo acupressure treatments for the first phase and active acupressure treatments for the second phase.
Figure 1.
Participant flow through study.
Table 2.
Participant characteristics.
| Sample Size | 13 |
| (Drop-out rate) | (0%) |
| Gender (% male) | 61.5% |
| Age (mean years ± SEM) | 58.38 ± 4.50 |
| Ethnicity | |
| % Caucasian | 92.3% |
| % Asian | 7.7% |
| Stroke hemisphere | |
| % left | 46.2% |
| % right | 53.8% |
| Type of Stroke | |
| % ischemic | 23.1% |
| % hemorrhagic | 30.8% |
| % both | 15.4% |
| % unknown | 30.8% |
| Time since stroke (mean months ± SEM) | 52.17 ± 10.33 |
Baseline Functional Level
Participant stroke-associated level of disability was as follows. The mean temperature differential between stroke-affected and unaffected arm was an average of 2.36 degrees Celsius, such that the stroke-affected side was that much cooler. Mean summary score on the Stroke-Specific Quality of Life Scale (SSQOL) was 4.29 ± .12 (range: 3.38 – 4.82, on a scale of 1–5, with 5 indicating higher reported quality of life). Mean score for stroke-affected limbs on an adaptation of the Motor Strength Scale (22 and P. Elser, R.N., Boulder Community Hospital) was 3.69 ± .24 (range: 2.5–5, on a scale of 0–5, with 5 indicating better function).
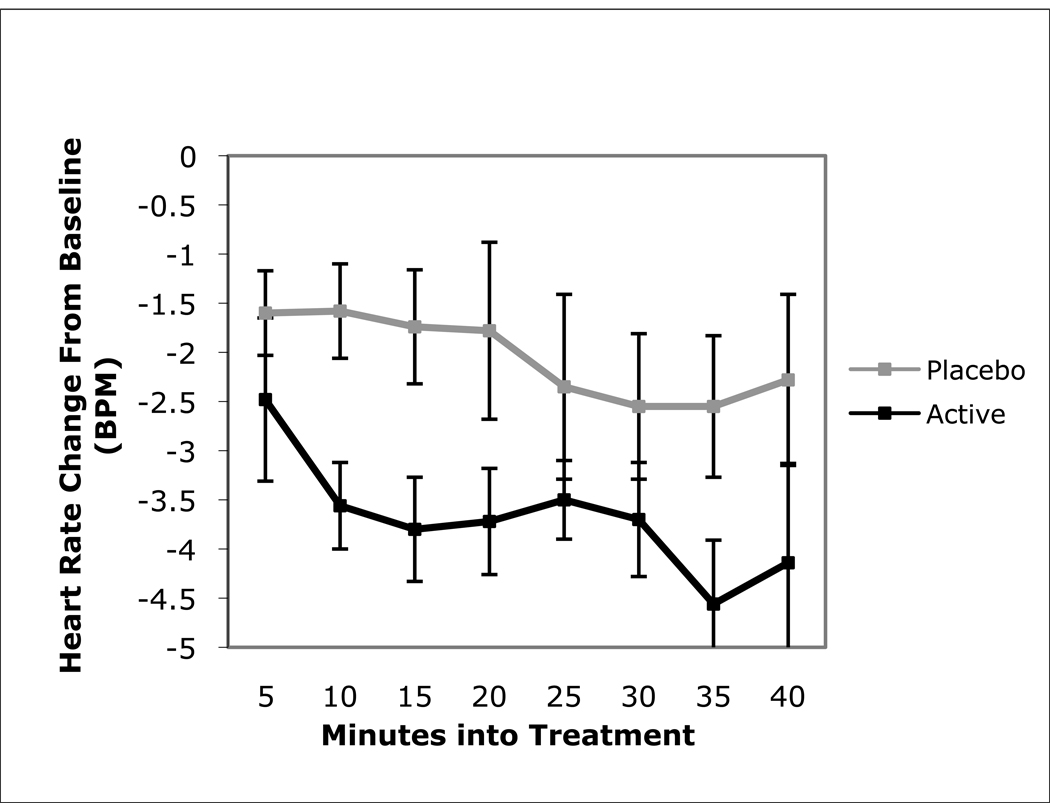
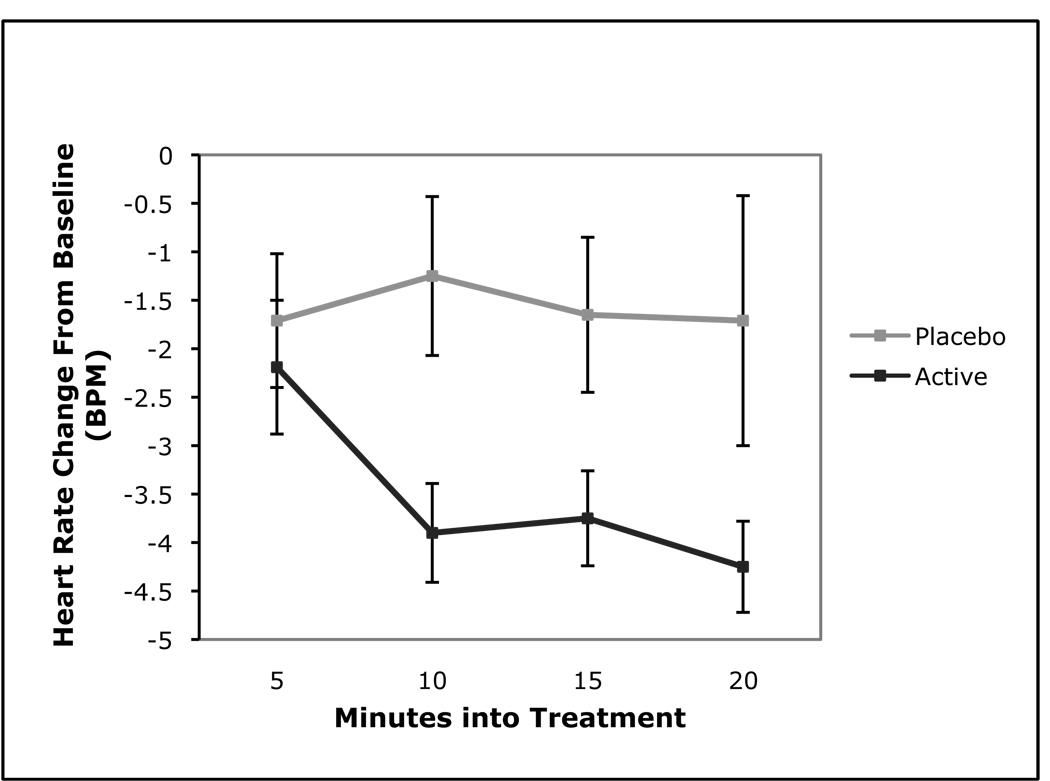
Heart Rate and Blood Pressure
Across the entire 8-session treatment phase, a significant main effect of treatment type on heart rate was found. Active acupressure reduced heart rate significantly more than did placebo acupressure, F (1, 12) = 5.14, p = .043, partial η2 = .30 (see Figure 2). In addition, a significant interaction between treatment type and treatment time point was found when isolating the first 20 minutes of treatment, such that active acupressure reduced heart rate faster during treatments than did placebo acupressure, F (3, 10) = 10.49, p = .002, partial η2 = .76 (see Figure 3). This effect was only seen during the last 4 treatments in the 8-treatment series; it was not observed during the first 4 treatment sessions. These significant treatment effects persisted even when accounting for condition assignment (A = Active/Washout/Placebo vs. B = Placebo/Washout/Active), age, gender, and time since stroke. Furthermore, baseline heart rate measures did not contribute to the significant treatment effect. Active (M = 66.38, SEM ± 3.17) and placebo (M = 65.92, SEM ± 3.42) treatment phase heart rate were not significantly different at baseline. Overall, there was no significant difference in blood pressure reduction associated with treatment, ns, or between active and placebo baseline blood pressure measures, ns However, as an example of the degree of reduction seen, mean SBP reduction during the first 20 minutes of the last 4 treatments was −1.34 mmHg (SEM ± 1.45) during placebo treatments and −1.42 mmHg (SEM ± 1.32) during active treatments (ns).
Figure 2.
Mean (±SEM) heart rate change within treatment session averaged across the 8-week treatment phase.
Figure 3.
Mean (±SEM) heart rate change in the first 20 minutes of treatment sessions, averaged across the last 4 weeks of each treatment phase.
Expectancy and Credibility
Expectancy rating prior to the active acupressure treatment phase (M = 41.67, SEM ± 8.69) was not significantly different from that prior to the placebo acupressure treatment phase (M = 31.69, SEM ± 5.91), t (12) = 1.36, p = .20. There was also no significant difference between credibility rating after the active (M = 4.38, SEM ± .59) and placebo (M = 4.46, SEM ± .50) treatment phases, t (12) = .16, p = .88.
DISCUSSION
Active acupressure treatment in chronic stroke patients reduced heart rate significantly more and significantly faster than did placebo acupressure treatment. Thus, while both treatment types induced a typical relaxation response, perhaps due to being supine, the relaxation response associated with active treatment was above and beyond that seen during placebo treatment. To determine if these results replicated those from other studies in the literature using 20-minute treatments, the first and last halves of treatments were also analysed separately. It was found that most of the treatment effect occurred during the first 20 minutes of treatment, after which the effects of placebo and active treatment on heart rate become equivalent. This makes sense, as it would be undesirable to have heart rate continue to decrease indefinitely.
Furthermore, it was discovered that most of the treatment effect occurred in the last four sessions of the treatment phase rather than the first four. This is an important discovery and the first to identify an appropriate “dose” of acupressure treatments necessary to elicit an effect. Prior to this, unpublished pilot data from our laboratory showed a trend towards active acupressure reducing heart rate more than placebo acupressure after 4 treatments. The current study suggests that while 4 treatments may have been necessary, they were not sufficient to observe a treatment effect. Instead, 8 treatments were sufficient. These treatment effects were not due to other variables such as condition assignment, age, gender, time since stroke or baseline heart rate measures.
A significant treatment effect on blood pressure was not found. A possible reason for this finding is that over the course of the study, 67% of participants were taking antihypertensive medications. The variety of antihypertensives taken by participants (e.g., ACE inhibitors, diuretics, beta-blockers), and the heterogeneity of mechanisms by which these medications modulate blood pressure, make it difficult to ascertain in a sample of this size if the lack of a significant blood pressure treatment effect is drug-related or not. Future studies with a sufficiently powered sample size could address these issues.
Treatment effects could not be accounted for by expectation. Since higher expectancy can potentially lead to an enhanced effect of treatment 20, 23, it is important that participants experienced the same level of expectancy, on average, prior to each treatment phase. Treatment effects could also not be accounted for by differences in credibility. Based on participants’ credibility ratings, placebo treatments were as credible as active treatments, suggesting that participants were unaware of when active or placebo acupressure treatments were administered. This is further supported by a post-study questionnaire in which participants were asked during which treatment phase (first or second) they thought active acupressure was administered. Sixty percent of participants correctly guessed when they received active treatments and 40% of participants guessed incorrectly, further suggesting that participants were unaware of when they were receiving active treatments.
Previous studies in the literature have also shown heart rate reduction following acupressure treatment 6, 11. However, as previously noted, appropriate control conditions were not employed, making it difficult to attribute heart rate differences definitively to acupressure, or more specifically, to stimulation of acupoints versus non-acupoints. The current study’s use of a placebo control that matched for attention, physical contact, and time suggests that the treatment effect seen on heart rate may be attributable to the stimulation of active acupoints.
Heart rate change, or other autonomic modulation, is important to investigate in stroke survivors. Stroke is a prevalent problem in the United States, being the number one cause of adult disability, and can be difficult to treat 24. Cardiovascular function is persistently impaired in those who have had a stroke, even up to a year following stroke and perhaps longer. This persistent dysfunction is thought to underlie the high risk of subsequent stroke or heart attack seen after an initial stroke 25. Because the stress response has been linked to disease 26, it has been hypothesised that the relaxation response could break the stress-disease link by reducing the response to stress 27. A potential benefit of the short-term relaxation response seen in the current study is facilitation of stress resilience, which, importantly in this population, could lead to reduced risk of further cardiovascular disease 26, 27. If confirmed to be beneficial in stroke survivors, future studies could investigate acupressure’s effects on other conditions in which ANS function is of concern, such as coronary heart disease (CHD).
A potential limitation to the current study is the number of participants taking antihypertensive medications (67%). Although representative of a population of stroke-survivors 28, this may have interfered with the ability to observe any effects of acupressure treatment on blood pressure. Another possible limitation to the current study is the small sample size, but given that significant treatment effects and large effect sizes were found, the present results suggest that a larger study of acupressure (e.g., Jin Shin) is warranted. A randomised controlled trial without crossover into the opposite treatment type would be the next logical step. Such a study would also allow for follow-up assessment to determine the duration of treatment effects, as well as further explore the optimal dosing of acupressure treatments. Future studies could also investigate the effects of relaxation in and of itself, independent of acupressure’s contribution, by including a relaxation control group in addition to a placebo control.
In conclusion, the present findings extend and are consistent with those found in previous studies: Active acupressure treatment appears to modulate ANS activity. As such, heart rate reduction and the relaxation response were enhanced over and above that seen during placebo acupressure treatment. This indicates a possible physiological mechanism by which stimulation of acupoints affects the body, and could help determine for which medical conditions acupressure could be a useful addition to conventional treatment methods. These data suggest that the CAM modality acupressure, and specifically Jin Shin, warrants further study as a possible adjunct treatment for stroke survivors. This is especially important given acupressure's potential as a self-sustaining treatment tool that, once learned, can be used independently.
Acknowledgments
We appreciate Alicia Segal, M.S.W., for technical support, Jin Shin practitioners Beeara Edmonds and Christine Palafox, as well as study participants and their families. We also thank Dr. Greg Carey for aid with randomisation and maintaining the study blind, as well as undergraduate research assistants Shelah Huerta, Bonnie Kemph, Amanda Stahl and Christina Gavito for help with data acquisition/entry. Support for this study was provided by funding from NIH/NCCAM, NIH/NCRR and the University of Colorado’s Undergraduate Research Opportunities Program and HHMI (Howard Hughes Medical Institute).
Funding Sources
This work was supported by K01 AT0011-77 (to Theresa D. Hernández) from NIH/NCCAM and M01 RR00051 from NIH/NCRR, as well as the University of Colorado’s Undergraduate Research Opportunities Program and HHMI (Howard Hughes Medical Institute).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement:
None of the authors have a conflict of interest.
References
- 1.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004:1–19. [PubMed] [Google Scholar]
- 2.Alkaissi A, Evertsson K, Johnsson VA, Ofenbartl L, Kalman S. P6 acupressure may relieve nausea and vomiting after gynecological surgery: An effectiveness study in 410 women. Can J Anaesth. 2002;49:1034–1039. doi: 10.1007/BF03017897. [DOI] [PubMed] [Google Scholar]
- 3.Hseih LL-C, Kuo C-H, Lee L-H, Yen AM-F, Chien K-L, Chen TH-H. Treatment of low back pain by acupressure and physical therapy: Randomized controlled trial. BMJ. 2006;332:696–700. doi: 10.1136/bmj.38744.672616.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu HS, Lin LC, Wu SC, Lin JG. The psychologic consequences of chronic dyspnea in chronic pulmonary obstruction disease: The effects of acupressure on depression. J Altern Complement Med. 2007;13:253–261. doi: 10.1089/acm.2006.5342. [DOI] [PubMed] [Google Scholar]
- 5.Hammerschlag R. Methodological and ethical issues in clinical trials of acupuncture. J Altern Complement Med. 1998;4:159–171. doi: 10.1089/acm.1998.4.159. [DOI] [PubMed] [Google Scholar]
- 6.Felhendler D, Lisander B. Effects of non-invasive stimulation of acupoints on the cardiovascular system. Complement Ther Med. 1999;7:231–234. doi: 10.1016/s0965-2299(99)80007-7. [DOI] [PubMed] [Google Scholar]
- 7.Haker E, Egekvist H, Bjerring P. Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in healthy subjects. J Auton Nerv Syst. 2000;79:52–59. doi: 10.1016/s0165-1838(99)00090-9. [DOI] [PubMed] [Google Scholar]
- 8.Nishijo K, Mori H, Yosikawa K, Yazawa K. Decreased heart rate by acupuncture stimulation in humans via facilitation of cardiac vagal activity and suppression of cardiac sympathetic nerve. Neurosci Lett. 1997;227:165–168. doi: 10.1016/s0304-3940(97)00337-6. [DOI] [PubMed] [Google Scholar]
- 9.Wang JD, Kuo TB, Yang CC. An alternative method to enhance vagal activities and suppress sympathetic activities in humans. Auton Neurosci. 2002;100:90–95. doi: 10.1016/s1566-0702(02)00150-9. [DOI] [PubMed] [Google Scholar]
- 10.Iversen S, Iversen L, Saper CB. The autonomic nervous system and the hypothalamus. In: Kandel ER, Schwartz JH, Jessell TM, editors. Principles of neural science. 4th edn. New York, NY: McGraw-Hill; 2000. pp. 960–981. [Google Scholar]
- 11.Sugiura T, Horiguchi H, Sugahara K, et al. Heart rate and electroencephalogram changes caused by finger acupressure on planta pedis. J Physiol Anthropol. 2007;26:257–259. doi: 10.2114/jpa2.26.257. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan RC, Tirschwell DL, Longstreth WT, et al. Blood pressure level and outcomes in adults aged 65 and older with prior ischemic stroke. J Am Geriatr Soc. 2006;54:1309–1316. doi: 10.1111/j.1532-5415.2006.00838.x. [DOI] [PubMed] [Google Scholar]
- 13.Reunanen A, Karjalainen J, Ristola P, Heliovaara M, Knekt P, Aromaa A. Heart rate and mortality. J Intern Med. 2000;247:231–239. doi: 10.1046/j.1365-2796.2000.00602.x. [DOI] [PubMed] [Google Scholar]
- 14.Hernández TD, Ramsberger G, Kurland J, Hadler B. Functional consequences of Jin Shin Tara treatment after stroke: A preliminary investigation. Society for Acupuncture Research Abstracts. 2003;43 [Google Scholar]
- 15.Burmeister A. Jin Shin Jyutsu: The touch of healing. New York, NY: Bantam; 1997. [Google Scholar]
- 16.Mines S. Jin Shin Jyutsu. WellSpring. 1982;11:16. [Google Scholar]
- 17.Mines S. We are all in shock: How overwhelming experiences shatter you and what you can do about it. Franklin Lakes, NJ: New Page Books; 2003. [Google Scholar]
- 18.Hernández TD, McFadden K, Segal A, Ivankovich BG, Gavito C, Huerta S. Functional improvement after stroke: A role for complementary medicine. J Neuropsychiatry Clin Neurosci. 2007;19:213. [Google Scholar]
- 19.Myers SS, Phillips RS, Davis RB, et al. Patient expectations as predictors of outcome in patients with acute low back pain. J Gen Intern Med. 2008;23:148–153. doi: 10.1007/s11606-007-0460-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shapiro DA. Comparative credibility of treatment rationales: Three tests of expectancy theory. Br J Clin Psychol. 1981;20:111–122. doi: 10.1111/j.2044-8260.1981.tb00504.x. [DOI] [PubMed] [Google Scholar]
- 21.Grubbs FE. Procedures for detecting outlying observations in samples. Technometrics. 1969;11:1–21. [Google Scholar]
- 22.Barker E. Neuroscience nursing: A spectrum of care. St. Louis, MO: Mosby Elsevier; 2008. pp. 70–71. [Google Scholar]
- 23.Price DD, Finniss DG, Benedetti F. A comprehensive review of the placebo effect: Recent advances and current thought. Annu Rev Psychol. 2008;59:565–590. doi: 10.1146/annurev.psych.59.113006.095941. [DOI] [PubMed] [Google Scholar]
- 24.Dobkin BH. Rehabilitation after stroke. N Engl J Med. 2005;352:1677–1684. doi: 10.1056/NEJMcp043511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McLaren A, Kerr S, Allan L, Steen IN, Ballard C, Allen J, Murray A, Kenny RA. Autonomic function is impaired in elderly stroke survivors. Stroke. 2005;36:1026–1030. doi: 10.1161/01.STR.0000160748.88374.ce. [DOI] [PubMed] [Google Scholar]
- 26.Esch T, Stefano GB, Fricchione GL, Benson H. Stress in cardiovascular diseases. Med Sci Monit. 2002;8:RA93–RA101. [PubMed] [Google Scholar]
- 27.Esch T, Fricchione GL, Stefano GB. The therapeutic use of the relaxation response in stress-related diseases. Med Sci Monit. 2003;9:RA23–RA34. [PubMed] [Google Scholar]
- 28.Paul SL, Thrift AG. Control of hypertension 5 years after stroke in the North East Melbourne Stroke Incidence Study. Hypertension. 2006;48:260–265. doi: 10.1161/01.HYP.0000230610.81947.04. [DOI] [PubMed] [Google Scholar]