Abstract
Purpose
Physicians have an ethical obligation to honor patients' values for care, including at the end of life (EOL). We sought to evaluate factors that help patients to receive care consistent with their preferences.
Methods
This was a longitudinal multi-institutional cohort study. We measured baseline preferences for life-extending versus symptom-directed care and actual EOL care received in 325 patients with advanced cancer. We also measured associated sociodemographic, health, and communication characteristics, including EOL discussions between patients and physicians.
Results
Preferences were assessed a median of 125 days before death. Overall, 68% of patients (220 of 325 patients) received EOL care consistent with baseline preferences. The proportion was slightly higher among patients who recognized they were terminally ill (74%, 90 of 121 patients; P = .05). Patients who recognized their terminal illness were more likely to prefer symptom-directed care (83%, 100 of 121 patients; v 66%, 127 of 191 patients; P = .003). However, some patients who were aware they were terminally ill wished to receive life-extending care (17%, 21 of 121 patients). Patients who reported having discussed their wishes for EOL care with a physician (39%, 125 of 322 patients) were more likely to receive care that was consistent with their preferences, both in the full sample (odds ratio [OR] = 2.26; P < .0001) and among patients who were aware they were terminally ill (OR = 3.94; P = .0005). Among patients who received no life-extending measures, physical distress was lower (mean score, 3.1 v 4.1; P = .03) among patients for whom such care was consistent with preferences.
Conclusion
Patients with cancer are more likely to receive EOL care that is consistent with their preferences when they have had the opportunity to discuss their wishes for EOL care with a physician.
INTRODUCTION
Despite principles of patients' rights to self-determination of treatment, studies of end-of-life (EOL) care tend to focus on factors that put patients at risk of receiving life-prolonging care,1–10 indicating a general perception that this is an undesirable outcome for patients with poor prognoses.11,12 Inaccurate expectations about prognosis may explain some patients' desire for life-prolonging care1,2,13–15; however, goals for care may vary even when patients recognize that they are terminally ill. Younger patients and patients with dependent children, for example, are more likely to choose therapies directed at life-prolongation,1,15,16 perhaps reflecting a desire to live or be available to their children as long as possible. Attainment of one's goals for EOL care may therefore be an important outcome of EOL care, whether goals involve life-prolonging or symptom-directed care.
Care inconsistent with patient preferences is associated with some negative outcomes such as higher healthcare utilization costs.17 But we know little about patient-specific outcomes of attainment of EOL care goals or about factors that assist with the attainment of goals. We evaluated preferences for life-extending or symptom-directed care among 325 patients with advanced cancer, assessed the care they received at the EOL, and determined factors associated with receipt of care consistent with baseline preferences. We hypothesized that patients would be more likely to attain their EOL care goals if physicians engaged in conversations about EOL care and if patients had a strong therapeutic alliance with physicians. We also evaluated preferences and care received among a subset of 121 patients who recognized that they were terminally ill at the time of baseline assessment, based on our hypothesis that these patients would be most likely to have stable preferences between baseline assessment and death. Finally, we sought to evaluate the extent to which the care received by patients achieved their goals. We assessed survival time as one possible outcome of life-prolonging care, and caregiver reports of distress and quality of life in the last week as possible outcomes of symptom-directed care.
METHODS
Subjects were recruited as part of the Coping with Cancer Study, a multi-institutional longitudinal investigation of patients with advanced cancer and their primary (unpaid) caregivers.4,18 This report describes 325 patients recruited between October 2002 and September 2007 whose self-reported treatment preferences were available and who died during the course of the study. Thirty-nine patients who did not express treatment preferences, designated by a response of “don't know” to our question about preferences, were excluded; excluded patients did not differ significantly from those included with respect to race, sex, education, marital status, religious preference, income, or EOL care received, although excluded patients were more likely to be uninsured (P = .0004).
Participating sites included Yale Cancer Center and Veterans' Affairs Connecticut Healthcare System Comprehensive Cancer Clinics (New Haven and West Haven, CT), Simmons Comprehensive Cancer Care Center and Parkland Hospital Palliative Care Service (Dallas, TX), Massachusetts General Hospital and Dana-Farber Cancer Institute (Boston, MA), and New Hampshire Oncology-Hematology (Hooksett, NH). Recruitment at Massachusetts General Hospital and Dana-Farber Cancer Institute started during the course of the study, resulting in few participants with postmortem data from this site (n = 8).
Patients were eligible to participate if they had cancer with distant metastases and failure of first-line chemotherapy, were 20 years of age or older, and were able to identify an unpaid caregiver. Patient-caregiver dyads were excluded if the patient or caregiver met criteria for dementia or delirium by neurobehavioral cognitive status examination (n = 93),19 did not have adequate stamina to complete the interview (n = 200), or was unable to speak English or Spanish (n = 9). Of 983 eligible patients, 691 enrolled in the larger study (70.3%), of whom we focus here on the 325 deceased patients with preferences data. All study participants provided written informed consent.
Patients participated in a baseline interview in English or Spanish for a $25 payment. Chart review was performed at enrollment and after death. A postmortem questionnaire was administered within 2 weeks of death to a caregiver (paid health care provider, n = 147, or family member, n = 139; caregiver type not known, n = 39) who had cared for the patient during the last week of life.
The institutional review boards of participating institutions approved study procedures. Measures used in analysis are described below.
Main Outcome Measures
Treatment preferences.
Patients were asked, “If you could choose, would you prefer (1) a course of treatment that focused on extending life as much as possible, even if that meant more pain and discomfort, or (2) a plan of care that focused on relieving pain and discomfort, even if that meant not living as long?” Patients who chose the former were designated as preferring life-extending care, and those who chose the latter were designated as preferring symptom-directed care. This question was used previously in the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments.2
EOL treatment received.
Location of death (intensive care unit [ICU], hospital [non-ICU], nursing home, inpatient hospice, or home) and interventions in the last week of life (ICU care, use of a ventilator, resuscitation, feeding tube, or chemotherapy) were determined through chart review and caregiver interviews. We defined receipt of life-extending care as use of any of the following in the last week of life: mechanical ventilation, resuscitation, feeding tube, chemotherapy, or ICU care.
Receipt of care consistent with preferences.
Patients who desired and received life-extending measures were designated as having received care consistent with their preferences, as were patients who desired symptom-directed care who did not receive life-extending measures. As a sensitivity analysis, we also evaluated receipt of hospice care for more than 1 week, reported in the postmortem interview,4 as one indicator of symptom-directed care.
Secondary Outcome Measures
Quality of life and distress.
In the postmortem assessment, caregivers were asked to report, “In your opinion, how would you rate the overall quality of the patient's death/last week of life?” with response options ranging from 0 (worst possible) to 10 (best possible). Similar questions assessed physical and psychological distress in the last week, with response options 0 (none) to 10 (most possible).
Survival.
Survival was defined as time from baseline assessment to death.
Primary Predictors of Interest
Terminal illness awareness.
Patients were asked to “describe your current health status,” with response options of “relatively healthy,” “seriously but not terminally ill,” and “seriously and terminally ill.” Patients who described themselves as “seriously and terminally ill” were considered to have awareness of their terminal illness.
EOL discussions.
Patients were asked in “yes/no” format whether they and their physician had discussed any wishes about the care they would want to receive if they were dying.
Therapeutic alliance.
Patients were asked five “yes/no” questions about trust in the physician, respect from the physician, respect of the physician, being seen as a whole person by the physician, and comfort in asking questions of the physician. Given the preponderance of positive responses, patients who responded in the affirmative to all five questions were defined as having the strongest therapeutic alliance.
Additional Covariates
Sociodemographic characteristics.
Subjects reported sex, age, race/ethnicity, marital status, income, health insurance status, religion, and highest grade completed in school.
Psychiatric illness.
The Structured Clinical Interview for the Diagnostic and Statistical Manual20,21 was used to diagnose current major depressive disorder, generalized anxiety disorder, panic disorder, and post-traumatic stress disorder. A single variable was used to designate patients with any psychiatric illness.
Performance status.
The Karnofsky score22 was determined by the research interviewer at enrollment in consultation with the treating physician.
Statistical Methods
We assessed relationships between preferences, awareness of terminal illness, and care received. We used χ2 tests to compare proportions, the κ statistic to assess the degree of agreement, and McNemar's test to assess the distribution of discrepancies between care preferred and received. The binary outcome variable, receipt of care consistent with preferences, was created as described. Associations between receipt of care consistent with preferences and independent variables were determined using logistic regression with generalized estimating equations to account for clustering by site. Multivariable models were adjusted for factors associated with treatment preferences and care received. After developing a theory-driven list of factors to be considered for inclusion, we used a threshold for entry in bivariable analysis of P < .05; these factors were included in the final models regardless of their significance in multivariable models. Finally, we evaluated associations between care preferred and received and possible outcomes of care, including survival time, quality of life, and physical and psychological distress, using t tests for pairwise comparisons. All analyses were conducted using the SAS statistical package, version 9.1 (SAS Institute, Cary, NC).
RESULTS
Patient characteristics are listed in Table 1. Treatment preferences were assessed a median of 125 days before death. A total of 234 (72%) of 325 patients preferred treatment focused on relieving pain and discomfort, whereas 91 patients (28%) preferred life-extending treatment. One hundred twenty-one (39%) of 312 patients recognized that they were terminally ill at the time of baseline assessment, and these patients were more likely to prefer symptom-directed therapy over life-extending therapy (odds ratio [OR] = 2.40; 95% CI, 1.37 to 4.19; P = .002; Table 2). However, 21 (17%) of 121 patients who recognized that they were terminally ill wished to receive life-extending therapy.
Table 1.
Patient Characteristics
| Characteristic | No. | % |
|---|---|---|
| Female sex, n = 324 | 146 | 45 |
| Age, years, n = 324 | ||
| Mean | 58.8 | |
| SD | 12.4 | |
| Race/ethnicity, n = 324 | ||
| White | 210 | 65 |
| Black | 60 | 19 |
| Asian | 3 | 1 |
| Hispanic | 49 | 15 |
| Married, n = 302 | 180 | 60 |
| Income, n = 310 | ||
| < $31,000 | 103 | 33 |
| ≥ $31,000 | 103 | 33 |
| Don't know | 77 | 25 |
| Declined | 27 | 9 |
| Highest grade completed in school, n = 325 | ||
| Mean | 12.5 | |
| SD | 4.1 | |
| Health insurance, n = 319 | 197 | 62 |
| Religion, n = 324 | ||
| Catholic | 125 | 39 |
| Protestant | 109 | 34 |
| Other | 76 | 23 |
| None | 14 | 4 |
| Recruitment site, n = 323 | ||
| Yale Cancer Center and Veterans Affairs Connecticut | 90 | 28 |
| Parkland Hospital and Simmons Comprehensive Cancer Center | 159 | 49 |
| Massachusetts General Hospital and Dana-Farber Cancer Institute | 8 | 2 |
| New Hampshire Oncology-Hematology | 66 | 20 |
Abbreviation: SD, standard deviation.
Table 2.
Patients' Awareness of Terminal Illness and Preferences for End-of-Life Care (n = 312)*
| Awareness of Terminal Illness | Baseline Preference for Treatment Focused on Relieving Pain and Discomfort |
Baseline Preference for Life-Extending Treatment |
||
|---|---|---|---|---|
| No. | % | No. | % | |
| Aware | 100 | 32 | 21 | 7 |
| Not aware | 127 | 41 | 64 | 21 |
NOTE. P = .003.
Due to rounding, sum of percentages exceeds 100.
Overall, 68% of patients (220 of 325 patients) received EOL care that was consistent with baseline preferences (Table 3). This included 28 patients (9%) who preferred and received life-extending therapy, defined as use of a feeding tube (n = 9), chemotherapy (n = 5), ventilator (n = 13), resuscitation (n = 5), and/or care in the ICU (n = 18) in the last week of life. Among patients who recognized that they were terminally ill at baseline, 74% (90 of 121 patients) received care consistent with baseline preferences, including five patients (4%) who wished to receive life-extending care.
Table 3.
Patient Preferences for End-of-Life Care and Actual Care Received
| Actual Care Received | Baseline Preference for Treatment Focused on Relieving Pain and Discomfort |
Baseline Preference for Life-Extending Treatment |
||
|---|---|---|---|---|
| No. | % | No. | % | |
| All patients, N = 325* | ||||
| Did not receive life-extending treatment in the last week of life | 192 | 59 | 63 | 19 |
| Received life-extending treatment in the last week of life | 42 | 13 | 28 | 9 |
| Patients who are aware they have a terminal illness, n = 121† | ||||
| Did not receive life-extending treatment in the last week of life | 85 | 70 | 16 | 13 |
| Received life-extending treatment in the last week of life | 15 | 12 | 5 | 4 |
κ = .14, McNemar's P = .04.
κ = .09, McNemar's P = .86.
Thirty-nine percent of patients (125 of 322 patients) reported that they had discussed their wishes for EOL care with their physicians. Patients who were aware they were terminally ill were more likely to have discussed their wishes for EOL care than patients who were not aware they were terminally ill (P < .0001). However, even among patients who were aware that they were terminally ill, 44% (52 of 118 patients) did not report discussions with physicians about EOL care preferences.
In bivariable analyses among all patients (n = 325), terminal illness awareness (OR = 1.64; P = .05) and an EOL discussion with a physician (OR = 2.04; P = .006) were associated with receipt of EOL care consistent with preferences (Table 4). EOL discussions remained associated with receipt of care consistent with preferences when we adjusted for race, insurance status, education, performance status, survival, age, and sex, and for clustering by recruitment site (OR = 2.26; P < .0001; Table 5).
Table 4.
Factors Associated With Receipt of EOL Care That Is Consistent With Preferences: Bivariable Logistic Regression
| Factor | All Patients (N = 325) |
Patients Who Are Aware They Have a Terminal Illness (n = 121) |
||||
|---|---|---|---|---|---|---|
| Receipt of EOL Care Consistent With Preferences |
P | Receipt of EOL Care Consistent With Preferences |
P | |||
| OR | 95% CI | OR | 95% CI | |||
| Sociodemographic characteristics | ||||||
| Female sex | 1.82 | 1.13 to 2.94 | .01 | 1.51 | 0.62 to 3.66 | .36 |
| White race | 1.21 | 0.74 to 1.96 | .45 | 1.01 | 0.38 to 2.68 | .99 |
| Age, per increasing year | 0.99 | 0.98 to 1.01 | .56 | 0.98 | 0.95 to 1.02 | .38 |
| Higher education, per increasing year | 1.02 | 0.97 to 1.08 | .41 | 1.08 | 0.96 to 1.21 | .18 |
| Income ≥ $31,000 | 0.87 | 0.47 to 1.63 | .67 | 0.70 | 0.22 to 2.27 | .55 |
| Health insurance | 0.85 | 0.52 to 1.37 | .50 | 0.75 | 0.31 to 1.83 | .53 |
| Health characteristics | ||||||
| Karnofsky performance status | 1.00 | 0.99 to 1.02 | .97 | 0.99 | 0.96 to 1.01 | .28 |
| Survival time from baseline assessment, days | 1.00 | 0.99 to 1.00 | .45 | 1.00 | 0.99 to 1.01 | .15 |
| Any psychiatric diagnosis | 1.07 | 0.48 to 2.34 | .88 | 1.00 | 0.25 to 4.02 | .99 |
| Patient-physician communication | ||||||
| Therapeutic alliance | 1.07 | 0.65 to 1.77 | .79 | 1.22 | 0.52 to 2.88 | .65 |
| Terminal illness awareness | 1.64 | 0.99 to 2.72 | .05 | NA | ||
| Discussion of EOL wishes | 2.04 | 1.23 to 3.37 | .006 | 3.50 | 1.46 to 8.39 | .005 |
Abbreviations: EOL, end-of-life; OR, odds ratio; NA, not applicable.
Table 5.
Factors Associated With Receipt of EOL Care That Is Consistent With Preferences: Multivariable Logistic Regression With Adjustment for Clustering by Recruitment Site*
| Factor | Receipt of EOL Care Consistent With Preferences |
|||||
|---|---|---|---|---|---|---|
| All Patients (n = 286) |
Patients Who Are Aware They Have a Terminal Illness (n = 106) |
|||||
| Adjusted Odds Ratio | 95% CI | P | Adjusted Odds Ratio | 95% CI | P | |
| Patient reports discussing EOL wishes with physician | 2.26 | 1.64 to 3.11 | < .0001 | 3.94 | 1.82 to 8.51 | .0005 |
Adjusted for race, insurance status, education, Karnofsky performance status, number of days between assessment and death, age, and sex.
As a sensitivity analysis, we revised our definition of receipt of care consistent with preferences to include hospice care as an indicator of receipt of symptom-directed care. Using this designation, 179 (55%) of 324 patients received care consistent with preferences, and EOL discussions remained associated with receipt of care consistent with preferences (OR = 2.05; 95% CI, 1.29 to 3.27; P = .002).
Patients who received life-extending therapy did not live longer than patients who did not (159 v 203 days, respectively; P = .10). Similarly, among patients who preferred life-extending therapy, length of life did not differ according to whether they actually received such therapy (171 days for patients who received life-extending therapy v 203 days for patients who did not; P = .49). Findings were similar when we adjusted for age and performance status.
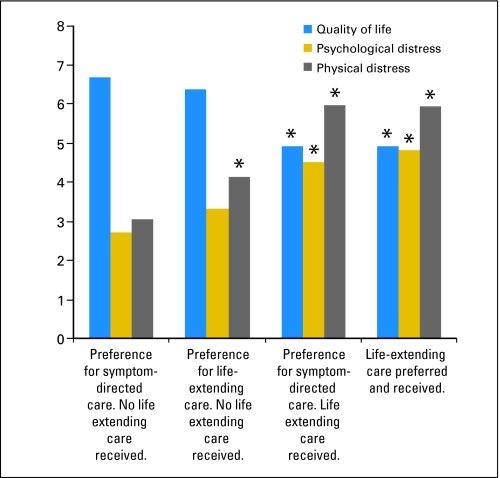
In contrast, caregiver-rated quality of life and physical and psychological distress in the last week of life varied by care preferred and received, such that receipt of life-extending therapy was associated with poorer quality of life and increased distress (Fig 1; Table 6). In comparison with patients who received no life-extending measures, patients who received life-extending care experienced greater physical and psychological distress and poorer quality of life regardless of their preferences (Table 6). Among patients who did not receive life-extending measures, physical distress was lowest (mean scores, 3.1 v 4.1; P = .03) among patients for whom such care fit with their preferences. Findings were similar when we adjusted for the source of the assessment (formal v informal caregiver) and for baseline quality of life.
Fig 1.
Quality of life, physical distress, and psychological distress in the last week of life according to end-of-life care preferred and received. *P < .05 in reference to group who preferred symptom-directed care and did not receive life-extending care.
Table 6.
Pairwise Comparisons Between Quality of Life, Psychological Distress, and Physical Distress
| Variable | Preference for Symptom-Directed Care (no life-extending care received) |
Preference for Life-Extending Care (no life-extending care received) |
Preference for Symptom-Directed Care (life-extending care received) |
Life-Extending Care Preferred and Received |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | P | Mean | SD | P | Mean | SD | P | |
| Quality of life | 6.69 | 2.77 | 6.38 | 2.68 | .44 | 4.90 | 3.36 | .0003 | 4.93 | 2.69 | .002 |
| Psychological distress | 2.71 | 2.94 | 3.33 | 3.31 | .16 | 4.52 | 3.37 | .0005 | 4.82 | 3.32 | .0006 |
| Physical distress | 3.05 | 3.19 | 4.13 | 3.56 | .03 | 5.95 | 3.53 | < .0001 | 5.93 | 3.09 | < .0001 |
NOTE. The reference group for all comparisons is the group of patients who preferred symptom-directed care and did not receive life-extending care.
Abbreviation: SD, standard deviation.
When we limited our analysis to patients who were aware they had a terminal illness (n = 121), discussion of EOL wishes with a physician was again associated with receipt of care consistent with baseline preferences, in bivariable (OR = 3.50; P = .005; Table 4) and multivariable (OR = 3.94; P = .0005; Table 5) analyses. Findings were similar when we considered receipt of hospice care to be an indicator of receipt of symptom-directed care (OR = 4.01; 95% CI, 1.80 to 8.95; P = .001).
DISCUSSION
More than two thirds of the patients we studied received EOL care that reflected their previously stated preferences. Such patients were more likely to be aware that they were terminally ill and to have had the opportunity to discuss their wishes for EOL care with a physician. In addition, the patients with the best quality of life and lowest distress in their last week were those who wished for symptom-directed care and did not receive life-extending measures at the EOL.
Strikingly, forty-two patients (13%) received life-prolonging care despite a previously stated goal of minimizing suffering. These patients constituted the majority of patients who received life-prolonging measures. The presence of this group raises concerns that a desire to forgo invasive measures is not always recognized or honored. This pattern of care was associated with greater distress and lower quality of life in the last week of life, a finding that strongly suggests that the primary goal of these patients' care—minimizing suffering—was not met.
A minority of patients who recognized that they were terminally ill wished to receive life-extending therapy. Their experiences require careful consideration. First, a small group of patients both preferred and received life-extending care. Although receipt of care consistent with preferences might be valued as upholding the patient's right to self-determination, the high burden of distress and low quality of life in this group are worrisome. Our data may help to inform discussions about such care. In addition, these patients lived no longer than patients who did not receive life-prolonging therapy. Although we cannot fully account for differences between patients, these findings suggest that extension of life may be a difficult goal to achieve.2,23,24
We should consider the possibility that there may be other benefits of life-prolonging care for patients who want the opportunity to make this choice. Some patients16,25 may simply want to know that they have done everything possible to live as long as possible. Consideration of a broader array of outcomes might allow us to explore other benefits or consequences of life-prolonging therapy.
We also found that most of the patients who preferred life-prolonging care ultimately did not receive such care in the last week of life. Perhaps these patients later recognized that death was imminent and agreed to forgo life-extending care. These patients did have better ratings for quality of life and less physical and psychological distress than patients who received life-extending care in the last week of life. However, these patients had more physical distress in the last week than patients who neither desired nor received life-extending measures, even though the two groups received similar care, at least by our measures. This finding suggests that distress at the EOL is in part a function of patient preferences, not just care received.
This study has some limitations. Because we assessed preferences a median of 4 months before death, we do not know if preferences remained stable, or if shifting preferences may account for some differences between preferences and care received. Previous research suggests that such changes do occur, though in relatively small numbers of patients.26–28 However, we found discrepancies between preferences and actual care even among patients who recognized that they were terminally ill at baseline, a group whose preferences arguably may be most stable over time. We also found no relationship between survival from baseline and either treatment preferences or care consistent with preferences. Nonetheless, a longitudinal assessment would be useful.
We relied on patient reports of EOL discussions; future research is needed to determine the extent to which patient reports provide an accurate assessment. As with our assessment of patient preferences, we assessed reports of EOL discussions at baseline rather than longitudinally; additional discussions may have occurred after the baseline assessment. In addition, although our findings have led us to speculate that EOL discussions help patients to attain their care goals at the end of life, our study does not allow us to determine causation. It is possible that physicians selectively engage in EOL discussions with patients most receptive to such conversations. However, patients who desire symptom-directed care might be particularly receptive to EOL discussions. Our finding that patients who desired symptom-directed care were more likely to receive life-prolonging care when EOL discussions did not take place strongly suggests that more patients would benefit from EOL discussions.
With the exception of hospice use, we did not measure specific markers of receipt of symptom-directed care. We therefore considered a lack of receipt of life-extending measures to indicate concordance with patient goals of minimizing suffering. Our measures of quality of life and physical and psychological distress suggest that this definition was reasonable, and use of hospice care as an indicator of symptom-directed care provided similar findings. However, future work should consider symptom management specifically. Finally, we included patients whose cancer had failed to respond to first-line chemotherapy; in doing so, we rendered patients who never received chemotherapy ineligible. This choice may have resulted in a sample with a greater tendency to pursue life-prolonging care.
We have evaluated the extent of concordance between patient preferences for EOL care and the care received. Despite the complexity of some of the circumstances we have evaluated, three findings seem relatively clear. First, patients are more likely to choose symptom-directed care when they understand they are terminally ill. Second, patients whose physicians engage them in conversation about their wishes for EOL care are more likely to receive care consistent with their preferences. And finally, the majority of the patients who receive life-extending measures have previously expressed a desire to receive symptom-directed care. Although changes in preferences before death could explain this finding, the burden of suffering experienced by these patients at the EOL is high. Physician-initiated discussions to elicit and document their wishes have significant potential to reduce their suffering at the EOL.
Footnotes
Supported in part by the following grants to H.G.P.: MH63892 from the National Institute of Mental Health and CA106370 from the National Cancer Institute; a Fetzer Religion at the End-of-Life Grant; and the Center for Psycho-Oncology and Palliative Care Research, Dana-Farber Cancer Institute. J.W.M. was supported by an American Cancer Society Mentored Research Scholar Grant.
Authors' disclosures of potential conflicts of interest and author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The author(s) indicated no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
Conception and design: Jennifer W. Mack, Jane C. Weeks, Alexi A. Wright, Susan D. Block, Holly G. Prigerson
Financial support: Holly G. Prigerson
Provision of study materials or patients: Holly G. Prigerson
Collection and assembly of data: Holly G. Prigerson
Data analysis and interpretation: Jennifer W. Mack, Jane C. Weeks, Alexi A. Wright, Susan D. Block, Holly G. Prigerson
Manuscript writing: Jennifer W. Mack, Jane C. Weeks, Alexi A. Wright, Holly G. Prigerson
Final approval of manuscript: Jennifer W. Mack, Jane C. Weeks, Alexi A. Wright, Susan D. Block, Holly G. Prigerson
REFERENCES
- 1.Haidet P, Hamel MB, Davis RB, et al. Outcomes, preferences for resuscitation, and physician-patient communication among patients with metastatic colorectal cancer: SUPPORT Investigators—Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Am J Med. 1998;105:222–229. doi: 10.1016/s0002-9343(98)00242-3. [DOI] [PubMed] [Google Scholar]
- 2.Weeks JC, Cook EF, O'Day SJ, et al. Relationship between cancer patients' predictions of prognosis and their treatment preferences. JAMA. 1998;279:1709–1714. doi: 10.1001/jama.279.21.1709. [DOI] [PubMed] [Google Scholar]
- 3.Earle CC, Park ER, Lai B, et al. Identifying Potential Indicators of the Quality of End-of-Life Cancer Care From Administrative Data. J Clin Oncol. 2003;21:1133–1138. doi: 10.1200/JCO.2003.03.059. [DOI] [PubMed] [Google Scholar]
- 4.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Earle CC, Landrum MB, Souza JM, et al. Aggressiveness of cancer care near the end of life: Is it a quality-of-care issue? J Clin Oncol. 2008;26:3860–3866. doi: 10.1200/JCO.2007.15.8253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rady MY, Johnson DJ. Admission to intensive care unit at the end-of-life: Is it an informed decision? Palliat Med. 2004;18:705–711. doi: 10.1191/0269216304pm959oa. [DOI] [PubMed] [Google Scholar]
- 7.Sharma G, Freeman J, Zhang D, et al. Continuity of care and intensive care unit use at the end of life. Arch Intern Med. 2009;169:81–86. doi: 10.1001/archinternmed.2008.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Temel JS, McCannon J, Greer JA, et al. Aggressiveness of care in a prospective cohort of patients with advanced NSCLC. Cancer. 2008;113:826–833. doi: 10.1002/cncr.23620. [DOI] [PubMed] [Google Scholar]
- 9.Barnato AE, McClellan MB, Kagay CR, et al. Trends in inpatient treatment intensity among Medicare beneficiaries at the end of life. Health Serv Res. 2004;39:363–375. doi: 10.1111/j.1475-6773.2004.00232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Braga S, Miranda A, Fonseca R, et al. The aggressiveness of cancer care in the last three months of life: A retrospective single centre analysis. Psychooncology. 2007;16:863–868. doi: 10.1002/pon.1140. [DOI] [PubMed] [Google Scholar]
- 11.Workman S, McKeever P, Harvey W, et al. Intensive care nurses' and physicians' experiences with demands for treatment: Some implications for clinical practice. J Crit Care. 2003;18:17–21. doi: 10.1053/jcrc.2003.YJCRC4. [DOI] [PubMed] [Google Scholar]
- 12.Breen CM, Abernethy AP, Abbott KH, et al. Conflict associated with decisions to limit life-sustaining treatment in intensive care units. J Gen Intern Med. 2001;16:283–289. doi: 10.1046/j.1525-1497.2001.00419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346:1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 14.Murphy D, Burrows D, Santilli S, et al. The influence of the probability of survival on parents' preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330:545–549. doi: 10.1056/NEJM199402243300807. [DOI] [PubMed] [Google Scholar]
- 15.Phillips RS, Wenger NS, Teno J, et al. Choices of seriously ill patients about cardiopulmonary resuscitation: Correlates and outcomes—SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Am J Med. 1996;100:128–137. doi: 10.1016/s0002-9343(97)89450-8. [DOI] [PubMed] [Google Scholar]
- 16.Nilsson ME, Maciejewski PK, Zhang B, et al. Mental health, treatment preferences, advance care planning, location, and quality of death in advanced cancer patients with dependent children. Cancer. 2009;115:399–409. doi: 10.1002/cncr.24002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teno JM, Fisher ES, Hamel MB, et al. Medical care inconsistent with patients' treatment goals: Association with 1-year Medicare resource use and survival. J Am Geriatr Soc. 2002;50:496–500. doi: 10.1046/j.1532-5415.2002.50116.x. [DOI] [PubMed] [Google Scholar]
- 18.Mack JW, Nilsson M, Balboni T, et al. Peace, Equanimity, and Acceptance in the cancer experience (PEACE): validation of a scale to assess acceptance and struggle with terminal illness. Cancer. 2008;112:2509–2517. doi: 10.1002/cncr.23476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kiernan RJ, Mueller J, Langston JW, et al. The Neurobehavioral Cognitive Status Examination: A brief but quantitative approach to cognitive assessment. Ann Intern Med. 1987;107:481–485. doi: 10.7326/0003-4819-107-4-481. [DOI] [PubMed] [Google Scholar]
- 20.Williams JB, Gibbon M, First MB, et al. The Structured Clinical Interview for DSM-III-R (SCID): II. Multisite test-retest reliability. Arch Gen Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- 21.First MB, Gibbon M, Williams JB. New York, NY: New York State Psychiatric Institute; 1995. Structured Clinical Interview for the DSM IV Axis I Disorders: Patient Edition (SCID-I/P, version 2.0) [Google Scholar]
- 22.Karnofsky DA. Determining the extent of the cancer and clinical planning for cure. Cancer. 1968;22:730–734. doi: 10.1002/1097-0142(196810)22:4<730::aid-cncr2820220407>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 23.von Gruenigen V, Daly B, Gibbons H, et al. Indicators of survival duration in ovarian cancer and implications for aggressiveness of care. Cancer. 2008;112:2221–2227. doi: 10.1002/cncr.23391. [DOI] [PubMed] [Google Scholar]
- 24.Rose JH, O'Toole EE, Dawson NV, et al. Perspectives, preferences, care practices, and outcomes among older and middle-aged patients with late-stage cancer. J Clin Oncol. 2004;22:4907–4917. doi: 10.1200/JCO.2004.06.050. [DOI] [PubMed] [Google Scholar]
- 25.Smith AK, McCarthy EP, Paulk E, et al. Racial and ethnic differences in advance care planning among patients with cancer: Impact of terminal illness acknowledgment, religiousness, and treatment preferences. J Clin Oncol. 2008;26:4131–4137. doi: 10.1200/JCO.2007.14.8452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borum ML, Lynn J, Zhong Z. The effects of patient race on outcomes in seriously ill patients in SUPPORT: An overview of economic impact, medical intervention, and end-of-life decisions—Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000;48(suppl):S194–198. doi: 10.1111/j.1532-5415.2000.tb03132.x. [DOI] [PubMed] [Google Scholar]
- 27.Fried TR, Van Ness PH, Byers AL, et al. Changes in preferences for life-sustaining treatment among older persons with advanced illness. J Gen Intern Med. 2007;22:495–501. doi: 10.1007/s11606-007-0104-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fried TR, O'Leary J, Van Ness P, et al. Inconsistency over time in the preferences of older persons with advanced illness for life-sustaining treatment. J Am Geriatr Soc. 2007;55:1007–1014. doi: 10.1111/j.1532-5415.2007.01232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]