Abstract
A key problem in studying a hypothesized spectrum of severity of delusional ideation is determining that ideas are unfounded. The first objective was to use virtual reality to validate groups of individuals with low, moderate, and high levels of unfounded persecutory ideation. The second objective was to investigate, drawing upon a cognitive model of persecutory delusions, whether clinical and nonclinical paranoia are associated with similar causal factors. Three groups (low paranoia, high nonclinical paranoia, persecutory delusions) of 30 participants were recruited. Levels of paranoia were tested using virtual reality. The groups were compared on assessments of anxiety, worry, interpersonal sensitivity, depression, anomalous perceptual experiences, reasoning, and history of traumatic events. Virtual reality was found to cause no side effects. Persecutory ideation in virtual reality significantly differed across the groups. For the clear majority of the theoretical factors there were dose–response relationships with levels of paranoia. This is consistent with the idea of a spectrum of paranoia in the general population. Persecutory ideation is clearly present outside of clinical groups and there is consistency across the paranoia spectrum in associations with important theoretical variables.
Keywords: delusions, paranoia, cognitive, schizophrenia, continuum
An emerging literature focuses on the clinically important experience of persecutory delusions (see Freeman, Bentall, & Garety, 2008). Similar to the occurrence of emotional disorders, the delusions seen in psychiatric services are likely to be at the severe end of a spectrum of such phenomena in the general population (e.g., Chapman & Chapman, 1980; Claridge, 1997; van Os, Linscott, Myin-Germeys, Delespaul, & Krabbendam, 2009); mistrust, suspiciousness, worries about threats from others, persecutory ideas, and persecutory delusions may be related. However, there is an underlying difficulty to work in this area: knowing that the ideation is unfounded. Such judgments can seem easier in clinical cases where the content is (sometimes) implausible but they become much more difficult lower down the spectrum; for instance, it is difficult to know whether fears about hostility from the neighbors are unrealistic or when mistrust of work colleagues is excessive. In this unique article the experience of persecutory ideation was validated in an experimental test.
The solution developed for determining the occurrence of unfounded persecutory ideation is exposure to neutral virtual reality social environments (see review by Freeman, 2008). Virtual reality is an interactive computer-generated environment. Its attraction lies in the tendency for individuals to react in virtual reality as they would in the real-life situation (Sanchez-Vives & Slater, 2005). Paranoid responses in the virtual reality social environments must be unfounded, as the computer characters are programmed to behave neutrally. No matter what a person does, the characters will remain neutral in their responses. It is therefore an excellent laboratory test of paranoid ideation. In the first studies the occurrence of persecutory ideation in virtual reality was established with students (Freeman et al., 2003, 2005), individuals at high risk of psychosis (Valmaggia et al., 2007), and individuals with persecutory delusions (Fornells-Ambrojo et al., 2008). The potential of the methodology to advance theoretical understanding was then demonstrated by the identification in a large general population sample of psychological factors predictive of paranoia (Freeman, Gittins, et al., 2008; Freeman, Pugh, et al., 2008). In this new study we set out to test three groups varying along the paranoia continuum: individuals with low levels of paranoia, individuals with high nonclinical paranoia, and individuals with persecutory delusions. It was predicted that individuals with clinical delusions would have a higher level of persecutory ideation in virtual reality than individuals with nonclinical paranoia, who, in turn, would be more suspicious than individuals low in paranoia. Potential adverse effects (e.g., nausea) of spending time in virtual reality were also monitored for each group.
Epidemiological studies indicated the presence of a psychosis continuum by establishing that delusions and hallucinations are not confined to psychotic groups (e.g., Eaton, Romanoski, Anthony, & Nestadt, 1991; van Os, Hanssen, Bijl, & Ravelli, 2000) and that the risk of clinical disorder is raised by the earlier occurrence of low-level symptoms (Chapman, Chapman, Kwapil, Eckbald, & Zinser, 1994; Dominguez, Wichers, Lieb, Wittchen, & van Os, 2009; Poulton et al., 2000). The continuum perspective also leads to an important prediction: Low-level psychotic-like experiences and clinical symptoms should be understandable in terms of similar factors. This has been termed etiological continuity (Myin-Germeys, Krabbendam, & van Os, 2003). The epidemiological studies, consistent with this prediction, find that clinical and nonclinical psychotic experiences have similar associations with demographic and social variables such as age, sex, urbanicity, and cannabis use (see review by van Os et al., 2009). Researchers in the Netherlands have also examined single psychological variables, such as theory of mind and attributional style, across a hypothesized positive symptom continuum (e.g., Janssen et al., 2006; Vermissen et al., 2008). Typically a dose–response relationship is shown between a putative causal factor and position along the psychosis continuum. In the current study the focus is on paranoid experiences: A cognitive model of persecutory delusions was used to test potential similarities in causal factors across the paranoia spectrum.
The threat anticipation model (Freeman, 2007; Freeman & Freeman, 2008; Freeman, Garety, Kuipers, Fowlers, & Bebbington, 2002) identifies multiple causes of paranoid thinking (see Figure 1), but the following are particularly important: affective processes, especially anxiety, worry, and interpersonal sensitivity; anomalous experiences, such as hallucinations and perceptual anomalies; reasoning biases, particularly jumping to conclusions and belief inflexibility; and social factors, such as adverse events and environments. It is hypothesized that at a time of stress the individual experiences a changed (and confusing) anomalous internal state (e.g., perceptual disturbances occur). In essence, the person feels different and this needs an explanation. A negative affective state makes a threatening interpretation likely: Anxiety leads to the anticipation of danger; interpersonal sensitivity highlights the potential threat from other people; and engagement in worry results in more negative, implausible ideas. Paranoid explanations are particularly likely in the context of previous experience of adverse events such as victimization. The fears reach a delusional level of conviction when reasoning biases, such as “jumping to conclusions,” are present. In the current study each of these model components was examined in the groups assessed in virtual reality. It was predicted that dose–response relationships would be found across the three groups for the presence of anomalous internal experiences, jumping to conclusions, anxiety, interpersonal sensitivity, worry, and history of trauma. These putative causal factors would be increasingly present as paranoia levels increase.
Figure 1. Outline of factors involved in persecutory delusion development.
Method
Participants
A low nonclinical paranoia group (n = 30), a high nonclinical paranoia group (n = 30), and a persecutory delusions group (n = 30) were tested. All participants were required to be within the ages of 18 to 65 and to be able to read and write in English. For the nonclinical groups there was a screening stage to identify members of the general public high and low in paranoid thinking. Sixty thousand leaflets advertising the study were distributed to local postcodes. The text of the leaflet headed “Virtual Reality Research at King’s College London” was as follows:
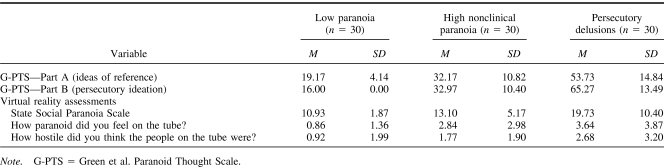
Virtual reality is a computer-generated world that you can walk around in. In research taking place in Denmark Hill, we are studying people’s reactions in virtual reality. We are looking for adult volunteers. Participation in the research would take 90 minutes for which you would be paid £20. The research has been approved by an ethics committee. If you are interested in taking part then find out more by telephoning or e-mailing.
A total of 291 individuals made contact. Thirteen individuals could not be recontacted, 6 people changed their minds about participating, 10 individuals were excluded for having a history of treatment for severe mental illness (e.g., schizophrenia, bipolar disorder), and 4 other individuals did not meet entry criteria. The 258 eligible respondents were then asked to complete several questionnaires (so that the focus on paranoia was not easily discernible). A total of 202 people returned fully completed questionnaires. The participants were selected on the basis of their level of persecutory thinking in the past month as assessed by the 16-item Green et al. (2008) Paranoid Thought Scale (G-PTS)—Part B, which can have scores ranging between 16 and 80. The 202 participants had a mean score of 20.1 (SD = 8.6, range 57, mode = 16, median = 17). Almost half of the sample (49%) scored at the bottom of this scale, indicating the absence of persecutory thinking in the past month. The low paranoia group were required to score 16 on this measure, indicating the absence of persecutory thinking. The high nonclinical paranoia group were required to score 21 or above; this cutoff selects the top 20% of the study respondents on the measure (and the top half of those endorsing paranoia items). We aimed to match the nonclinical groups with the clinical group for age and sex. The clinical group were recruited from adult psychiatric services at the South London and Maudsley National Health Service (NHS) Foundation Trust. The entry criteria were the presence of a current persecutory delusion, which met the criteria of Freeman and Garety (2000), and a clinical diagnosis of schizophrenia, schizoaffective disorder, or delusional disorder. The presence of a persecutory delusion was established using the Present State Examination—10 (World Health Organization, 1992). The case-note diagnoses of those recruited were schizophrenia (n = 24), schizoaffective disorder (n = 4), and delusional disorder (n = 2). Antipsychotic medication data were converted into chlorpromazine equivalents grouped into low (0–200 mg), medium (200–400 mg), and high (≥400 mg); 1 person was not taking any medication, 11 were on a low dose, 14 were on a medium dose, and 4 were on a high dose. As would be expected, the three groups clearly differed on the self-report G-PTS (see Table 1). There were significant differences for ideas of reference, F(2, 97) = 77.39, p < .001, and persecutory ideation, F(2, 87) = 194.33, p < .001. The groups significantly differed from each other on each of the scales (p < .001).
Table 1. Levels of Paranoia Across the Groups.
Virtual Reality
The equipment, environment, and procedure were identical to that reported by Freeman, Pugh, et al. (2008). The head-mounted display was a Virtual Research VR1280 (Virtual Research Systems, Aptos, CA), which has a resolution of 1280 × 1024 pixels in each eye, a 60° diagonal field of view, and a refresh rate of 60 Hz. The tracking system used was the InterSense IS900 (InterSense Inc., Billerica, MA). The tracker uses a hybrid of inertial and ultrasonic sensors to determine the orientation and position of the user during the simulation. The sensors were laid out in a ceiling constellation grid above the user. The tracker data were accessed by a Virtual Reality Peripheral Network (VRPN) IS900 server (Taylor et al., 2001).
The virtual reality environment comprised a 4-min journey between two stops on a visual and auditory simulation of a London Underground train which was populated by computer characters (see Figure 2). The Distributed Immersive Virtual Environment (DIVE) software platform was used to create the overall scenario (Frecon, Smith, Steed, Stenius, & Stahl, 2001). Both the train shell and the computer characters (avatars) were created using 3D Studio Max (Autodesk, San Rafael, CA). The avatar motions were made using an optical motion capture system. Each avatar had its own background motion that repeated throughout the scenario. Each avatar had one motion that approximated their breath and another motion that randomized the direction of their gaze. In addition, several of the avatars responded to participants’ gaze by looking in their direction, which was enabled through head tracking of the participants. When looked at, one particular avatar would occasionally smile at the user. The audio for the scene, comprising background tube noise and low-level snippets of conversation, was rendered in stereo, without spatialization, using a Creative sound card.
Figure 2. The virtual reality equipment (top panel) and scenario (bottom panel).
Measures
All measures were completed before entering the virtual reality environment. The exceptions were the State Social Paranoia Scale (Freeman et al., 2007) and the Visual Analogue Scales, which assess paranoid thinking in virtual reality, and were therefore administered directly after the headset was removed. The Simulator Sickness Questionnaire (Kennedy, Lane, Berbaum, & Lilienthal, 1993) was repeated after the virtual train ride.
Paranoia
Green et al. Paranoid Thought Scales (G-PTS; Green et al., 2008)
The G-PTS is a 32-item measure of paranoid thinking over the past month. Part A assesses ideas of reference (e.g., “It was hard to stop thinking about people talking about me behind my back”) and Part B assesses ideas of persecution (e.g., “I was convinced there was a conspiracy against me”). Each item is rated on a 5-point scale. Higher scores indicate greater levels of paranoid thinking. The internal consistency of the scale and test–retest reliability are good. Convergent validity has been shown with the Paranoia Scale (Fenigstein & Vanable, 1992).
State Social Paranoia Scale (SSPS; Freeman et al., 2007)
The SSPS was designed to assess paranoia in virtual reality. It has 10 persecutory items each rated on a 5-point scale (e.g., “Someone stared at me in order to upset me,” “Someone was trying to isolate me,” “Someone was trying to make me distressed”). The SSPS has excellent internal reliability, adequate test–retest reliability, convergent validity with both independent interviewer ratings and self-report measures, and divergent validity in regards to measures of positive and neutral thinking. Higher scores on the SSPS indicate greater levels of persecutory thinking. In order to reduce skew, the responses were grouped into six ordinal categories (corresponding to scores of 10, 11–15, 16–20, 21–25, 26–30, and ≤30; as previously carried out by Freeman, Pugh, et al., 2008).
Visual Analogue Rating Scales
Participants marked on separate 10-cm lines the degree to which the people on the virtual reality train were hostile and whether they had felt paranoid on the train. Higher ratings indicate greater endorsement of the characteristic.
Affective Processes
Depression Anxiety Stress Scales (DASS; Lovibond & Lovibond, 1995)
The DASS is a 42-item instrument with three subscales measuring current symptoms of depression, anxiety, and stress. Each of the subscales consists of 14 items with a 0–3 scale (0 = did not apply to me at all, 3 = applied to me very much). Higher scores indicate higher levels of emotional distress. The scale has been shown to be reliable and valid in large clinical and nonclinical populations (Brown, Chorpita, Korotitsch, & Barlow, 1997; Crawford & Henry, 2003; Page, Hooke, & Morrison, 2007). The Anxiety and Depression subscales were used in the current study.
Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990)
The PSWQ is the most established measure of trait worry style and has been used in nonclinical and clinical populations (see review by Startup & Erickson, 2006). Each of the 16 items are rated on a 5-point scale. Higher scores indicate a greater tendency to worry.
Interpersonal sensitivity measure (Boyce & Parker, 1989)
This is a 36-item scale designed to assess interpersonal sensitivity, defined as undue and excessive awareness of, and sensitivity to, the behavior and feelings of others. Statements are rated on a 4-point scale (1 = very unlike self, 2 = moderately unlike self, 3 = moderately like self, 4 = very like self). High scores indicate greater interpersonal sensitivity. The psychometric properties of the scale have been tested in nonclinical individuals, general practice attenders, and psychiatric patients.
Reasoning
Beads task (Garety et al., 2005)
Data gathering was assessed with a probabilistic reasoning task that has been extensively used with people who experience delusions (see reviews by Fine, Gardner, Craigie, & Gold, 2007; Freeman, 2007; Garety & Freeman, 1999). Participants are asked to request as many pieces of evidence (colored beads) as they would like before making a decision (from which of two hidden jars the beads are drawn). The two jars have beads of two different colors (orange and black) in opposite ratios of 60:40. The key variable is the number of beads requested before making a decision (and a lower number has been associated with delusions).
Anomalous Experience
Cardiff Anomalous Perceptions Scale (Bell, Halligan, & Ellis, 2006)
This 32-item questionnaire assesses perceptual anomalies. It comprises nine subscales including sensory intensity, distortion of the external world, sensory experience from an unexplained source, sensory flooding, and hallucinations. A higher score represents the reporting of a greater number of perceptual anomalies. The scale also has three factor scores. The first factor, Temporal Lobe Experience, contains items such as “Do you ever see shapes, lights, or colors even though there is nothing really there?” The second factor, Chemosensation, contains items such as “Do you ever notice that food or drink seems to have an unusual taste?” The third factor, Clinical Psychosis, contains items such as “Do you ever hear voices commenting on what you are thinking or doing?” The questionnaire was developed with clinical and nonclinical groups and displayed good internal reliability, test–retest reliability, and construct and criterion validity.
Social
Life Stressor Checklist (Wolfe & Kimerling, 1997)
The checklist asks respondents about the occurrence of a range of severe life events (e.g., serious accident, physical attack, and sexual abuse). If the respondent reports the occurrence of an event, subsequent questions ask when the event happened, whether the person thought at the time that serious harm or death could result, and whether feelings of intense helplessness, fear, or horror occurred. Only checklist items that referred to Criterion A events as defined in the Diagnostic and Statistical Manual of Mental Disorders (4th ed., text rev.; American Psychiatric Association, 2000) were used. Only events that reached the severity criterion related to posttraumatic stress disorder diagnosis were scored as occurring. The total number of traumatic events was recorded. McHugo et al. (2005) reported adequate test–retest reliability of the measure in a sample of 200 women.
Side Effects
Simulator Sickness Questionnaire (Kennedy et al., 1993)
Particularly in the past, virtual reality was known to cause side effects similar to motion sickness. Possible causes may have been flicker, visual distortion, and the slow response of earlier systems to participants’ movements. The 16-item Simulator Sickness Questionnaire, derived from a large factor analysis, assesses three symptom clusters: oculomotor (e.g., blurred vision), disorientation (e.g., dizziness), and nausea (e.g., vomiting). Each item is assessed on a 4-point scale (from none to very strong). The total score is weighted. Higher scores indicate a higher level of symptoms.
Intellectual Functioning
Wechsler Test of Adult Reading (Wechsler, 2001)
The Wechsler Test of Adult Reading provides an estimate of premorbid intellectual functioning by asking participants to read a list of 50 words with irregular pronunciations.
Analysis
Analyses were carried out using SPSS Version 15.0 (SPSS, 2006) and Stata Version 10.0 (StataCorp, 2008). Group differences for demographic variables were tested using one-way analysis of variance (ANOVA) and, when appropriate, least significant difference planned comparisons. Ordinal logistic regressions (using the Stata ologit command) were used to test differences in paranoia in virtual reality. The main procedure for testing overall group differences on the cognitive model measures was one-way ANOVA; when significant these were then followed by least significant difference pairwise comparisons (i.e., there was no correction applied for multiple testing). Covariates were not used (Miller & Chapman, 2001). There were no missing data for the main analyses.
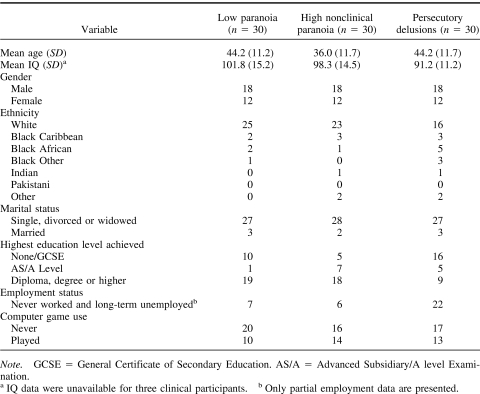
Results
Basic demographic information for the three groups is displayed in Table 2. It can be seen that the groups were matched for sex and marital status. There was a significant group difference in age, F(2, 87) = 4.97, p = .009; the high nonclinical paranoia group was younger than the two other groups (p < .01). The clinical group had fewer individuals of White ethnicity compared with the low paranoia group, χ2(1) = 6.24, p = .012, and the high nonclinical paranoia group, χ2(1) = 3.59, p = .058. There was also a significant difference in intellectual functioning, F(2, 84) = 4.31, p = .017; the clinical group scored significantly lower than the low paranoia group (p = .005) and tended to score lower than the high nonclinical paranoia group (p = .057). The scores on the intellectual functioning measure are consistent with the lower levels of educational qualifications of the clinical group. The clinical group were more likely to be unemployed than the low paranoia group, χ2(1) = 12.38, p < .001, and the high nonclinical paranoia group, χ2(1) = 19.81, p < .001. For computer game playing the low paranoia group did not differ from either the clinical group, χ2(1) = 0.64, p = .426, or the high nonclinical paranoia group, χ2(1) = 1.11, p = .292.
Table 2. Demographic Information.
Validation of the Groups
Group differences in persecutory ideation in virtual reality as assessed by the SSPS were tested using ordinal logistic regression. The persecutory delusions group was 12.51 times more likely than the low paranoia group to be in a higher category of persecutory ideation in virtual reality, p < .001, CI [4.20, 37.22]. This means, for instance, that the delusions group was approximately 12 times more likely to report paranoid ideation in virtual reality. The high nonclinical paranoia group were 2.86 times more likely than the low paranoia group to be in a higher category of persecutory ideation in virtual reality, p = .044, CI [1.03, 7.96]. This means, for instance, that the high nonclinical group were approximately 3 times more likely to report paranoid ideation in virtual reality. When the ordinal regression for paranoia in virtual reality was repeated with the high nonparanoia group as the reference category, the clinical paranoia group were 4.37 times more likely to be in a higher SSPS category, p = .003, CI [1.63, 11.71]. Therefore the groups significantly differed from each other in levels of unfounded persecutory ideation.
Side Effects: Simulator Sickness
Total weighted simulator sickness scores indicated that there were no changes from pre- to postvirtual reality for the persecutory delusions group (Time 1 M = 67.34, SD = 65.40; Time 2 M = 61.71, SD = 65.20), the high nonclinical paranoia group (Time 1 M = 17.45, SD = 17.74; Time 2 M = 22.19, SD = 24.75), or the low paranoia group (Time 1 M = 5.24, SD = 11.05; Time 2 M = 5.98, SD = 13.77). A mixed-design ANOVA, with time as a within-subjects factor and group as a between-subjects factor, confirmed no significant main effect of time, F(1, 87) < 0.01, p = .984, or significant interaction between time and group, F(2, 87) = 1.58, p = .212. There was, however, a main effect of group, F(2, 87) = 18.93, p < .001. The persecutory delusions group scored higher on the Simulator Sickness Questionnaire than both of the nonclinical groups (p < .001). This higher reporting by the psychiatric group of symptoms such as headache, nausea, and dizziness—which was independent of being in virtual reality—may reflect their generally higher levels of affective disturbance or side effects of antipsychotic medication.
Cognitive Model Variables
Comparisons on the model measures, using one-way ANOVA and least significant difference testing, are displayed in Table 3. Increasing levels of paranoia across the three groups are clearly associated with increases in anxiety, depression, interpersonal sensitivity, anomalies of experience, and number of traumatic events. (The difference in number of traumatic events between the low paranoia and high nonclinical paranoia approached significance, p = .052.) Only reduced data gathering is specific to the clinical group.
Table 3. Mean Scores and Group Comparisons for the Model Measures.
The anomalous experiences questionnaire was examined further because of the variety in types of perceptual anomalies. The three factor scores and two of the subscales (one concerning hallucinatory experiences, the other concerning much milder anomalies) were analyzed. There is a clear increase in the temporal lobe factor score across the groups (see Table 3). A similar pattern is found for the Clinical Psychosis factor, which was dichotomized because of its skew. Ten (33%) individuals in the low paranoia group, 20 (67%) individuals in the high nonclinical paranoia group, and 26 (87%) individuals in the clinical group had at least one clinical psychosis anomaly. The high nonclinical paranoia group, χ2(1) = 6.67, p = .010, and the clinical group, χ2(1) = 17.78, p < .001, were more likely to have clinical psychosis anomalies than the low paranoia group. The high nonclinical paranoia group tended to have a lower likelihood to experience such anomalies when compared with the clinical group, χ2(1) = 3.35, p = .067. A similar pattern of results was found for the subscale concerning sensory experience from an unexplained source. The relationships for the Chemosensation factor and the Sensory Intensity subscale scores were slightly different; the general pattern here was that the high nonclinical paranoia group had the highest scores, which were similar to the clinical group but significantly different from the low paranoia group.
Finally, all the variables (anxiety, worry, interpersonal sensitivity, depression, total number of anomalous experiences, beads drawn, number of traumatic events) were considered together in an ordinal logistic regression with group as the dependent variable; the only significant predictors of the paranoia spectrum were anxiety, odds ratio = 1.21, p = .008, CI [1.05, 1.40], and number of anomalous experiences, odds ratio = 1.16, p = .006, CI [1.04, 1.29].
Discussion
Virtual reality proved to be a safe method of studying paranoia. It was used to identify three groups: individuals with low levels of persecutory ideation, individuals with nonclinical persecutory ideation, and individuals with clinical persecutory delusions. This provided the opportunity to examine the cognitive correlates of persecutory delusions and the intriguing issue of whether the persecutory ideation common in the general population is the counterpart of the clinical phenomena. This process was informed by theory: The groups were assessed on measures related to a cognitive model of persecutory delusions. There was a consistency in the results. Across the groups there was a step change in levels of anxiety, worry, interpersonal sensitivity, depression, anomalies of experience, and trauma history. This pattern of results is expected if nonclinical and clinical paranoia are related experiences.
The particular associations across the groups are consistent with the existing literature testing the cognitive model. A number of studies have reported an association of paranoia with anxiety, worry, and interpersonal sensitivity (e.g., Bassett, Sperlinger, & Freeman, 2009; Freeman & Garety, 1999; Martin & Penn, 2001; Startup, Freeman, & Garety, 2007). Paranoia may even be a type of anxious fear (Freeman & Freeman, 2008). However, experimental research indicates that anomalies of experience differentiate persecutory ideation from anxiety (Freeman et al., 2005; Freeman, Gittins, et al., 2008). In the current study anomalies of experience were the second key factor associated with paranoia. It should be recognized, however, that perceptual anomalies vary greatly in severity. The milder anomalies, such as changes in levels of sensory intensity (e.g., “Do you ever notice that sounds are much louder than they normally would be?”), were associated with paranoia, but their presence did not distinguish between clinical and nonclinical instances. In contrast, the presence of more severe anomalies, such as hallucinations, did discriminate between the two paranoia groups. It is plausible that there is a qualitative shift in the types of anomalous experiences associated with severe instances of paranoia.
Indeed, even though the study provides further support for the view that complete discontinuity between clinical and nonclinical experiences is unlikely, the exact nature of a paranoia spectrum remains to be established. Van Os and Verdoux (2003) described how the shape of a delusion continuum in the general population would depend on the number of causal factors, the differences in their effect sizes, the degree to which they interact, and their prevalence but argued that if there are a number of interacting factors then it is unlikely that the distribution will be normal. Instead the distribution in the general population is likely to be skewed, with many people not having any delusional experiences (i.e., quasicontinuous). Such skewness in the occurrence of persecutory thinking was found in the current study’s screening sample. It is of interest that in large epidemiological studies new statistical methods are now being applied to understanding distributions of psychological problems (e.g., Krueger, Markon, Patrick, Benning, & Kramer, 2007). At an individual level there may be nonlinear shifts into clinical disorder. Detailed analysis of potential differences in the content of clinical and nonclinical paranoia is also required. Specific aspects of the content of persecutory thoughts (e.g., beliefs about the power of the persecutor) relate to emotional distress but have not been examined across the spectrum (Freeman, Garety, & Kuipers, 2001). Put simply, there may be differences between clinical and nonclinical groups other than in levels of belief conviction, preoccupation, and distress.
One of the assessments did not show a dose–response relationship to level of paranoia; limited data gathering in the reasoning task was apparent only in individuals with persecutory delusions. The data-gathering bias (“jumping to conclusions”) has been found in studies with clinical and nonclinical groups to be specifically associated with levels of delusional conviction (Freeman, Pugh, & Garety, 2008; Garety et al., 2005). Delusional conviction was not the focus of the current study, but the nonclinical paranoia group will have had higher levels of belief conviction than the low paranoia group on the screening measure of persecutory ideation. Therefore a difference in data gathering would be expected, similar to that reported by Freeman, Pugh, and Garety (2008). Van Dael et al. (2006) also did not find an association of the reasoning bias with nonclinical delusional ideation. Given the occasional failure to replicate the jumping to conclusions finding in nonclinical groups, it may well be that a range of more subtle and taxing reasoning tasks are required to separate reliably nonclinical groups high and low in delusional ideation. Alternatively, anxiety, worry, and anomalous experiences may be enough on their own to create moderately held thoughts of a paranoid content, and the extreme data-gathering bias only operates to produce very high degrees of belief conviction—an account which does not assume a simple correlation between the continuum of paranoia and reasoning biases. In the high nonclinical paranoia group the absence of a hasty reasoning style is likely to be protective against the development of severe paranoia by allowing doubt and the consideration of alternative explanations for events.
The research study could have been strengthened in a number of ways. The recruitment of a nonclinical group having comparable levels of paranoia to the delusions group would have provided a stronger test of differences between clinical and nonclinical experiences. This would have entailed recruiting the top 5% of scorers on the paranoia scale from the general population. Having four groups varying in paranoia levels (i.e., sampling the putative spectrum at more points) would have been informative. Improved matching on age and intellectual functioning would have been desirable. It is also of note that the initial leafleting had a very low response rate and therefore the representativeness of the participant sample is unknown. A central weakness is that the data collected in the current study do not establish that the cognitive factors are linked to the occurrence of persecutory ideation or rule out the possibility that they are secondary consequences. Moving beyond a cross-sectional design in future research would be particularly valuable; for instance, incorporating a longitudinal element could have addressed the issue of whether the factors from the cognitive model maintain persecutory ideation across the spectrum. Manipulating key factors in each of the groups would enable stronger causal inference (Kendler & Campbell, 2009; Shadish, Cook, & Campbell, 2002).
What are the broader implications of the continuum approach for clinicians and researchers? More information, written with less reference to diagnosis, is needed for those on the paranoia spectrum (Freeman, Freeman, & Garety, 2008). It is often helpful for individuals with distressing persecutory thoughts to know that their experiences are commoner than they had realized. The large affective component to paranoid experience can be valuable to recognize. Clinicians should be aware that paranoia is not inevitably a sign of severe mental illness; a debate has already begun concerning the introduction of a dimensional approach to psychosis in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (Allardyce, Gaebel, Zielasek, & van Os, 2007; Dutta et al., 2007). Importantly for researchers, the understanding of persecutory delusions can be informed by studying milder variants. Studying nonclinical variants has the advantages of facilitating the recruitment of large sample sizes in order to test complex models, obviating complicating issues such as the prescription of medication and appraisals of illness, and enabling manipulationist experiments where putative causal factors are increased. The continuum approach also implies that delusional ideas can often be understood in terms of normal processes gone awry rather than substantial deficits. Overall a focus is needed on the individual experiences, the symptoms, which have hitherto made up diagnoses such as schizophrenia.
Acknowledgments
This work was funded by a Wellcome Trust Fellowship awarded to Daniel Freeman.
References
- Allardyce J., Gaebel W., Zielasek J., & van Os J. (2007). Deconstructing Psychosis Conference February 2006: The validity of schizophrenia and alternative approaches to the classification of psychosis. Schizophrenia Bulletin, 33, 863–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. [Google Scholar]
- Bassett M., Sperlinger D., & Freeman D. (2009). Fear of madness and persecutory delusions. Psychosis, 1, 39–50. [Google Scholar]
- Bell V., Halligan P. W., & Ellis H. D. (2006). The Cardiff Anomalous Perceptions Scale (CAPS). Schizophrenia Bulletin, 32, 366–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyce P., & Parker G. (1989). Development of a scale to measure interpersonal sensitivity. Australian and New Zealand Journal of Psychiatry, 23, 341–351. [PubMed] [Google Scholar]
- Brown T. A., Chorpita B. F., Korotitsch W., & Barlow D. H. (1997). Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research and Therapy, 35, 79–89. [DOI] [PubMed] [Google Scholar]
- Chapman L. J., & Chapman J. P. (1980). Scales for rating psychotic and psychotic-like experiences as continua. Schizophrenia Bulletin, 6, 476–489. [PubMed] [Google Scholar]
- Chapman L. J., Chapman J. P., Kwapil T. R., Eckbald M., & Zinser M. C. (1994). Putatively psychosis-prone subjects 10 years later. Journal of Abnormal Psychology, 103, 171–183. [DOI] [PubMed] [Google Scholar]
- Claridge G. (1997). Schizotypy: Implications for illness and health. Oxford, England: Oxford University Press. [Google Scholar]
- Crawford J. R., & Henry J. D. (2003). The Depression Anxiety Stress Scales (DASS): Normative data and latent structure in a large non-clinical sample. British Journal of Clinical Psychology, 42, 111–131. [DOI] [PubMed] [Google Scholar]
- Dominguez M., Wichers M., Lieb R., Wittchen H., & van Os J. (2009). Evidence that onset of clinical psychosis is an outcome of progressively more persistent subclinical psychotic experiences: An 8-year cohort study. Schizophrenia Bulletin. Advance online publication. doi:10.1093/schbul/sbp022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta R., Greene T., Addington J., McKenzie K., Phillips M., & Murray R. M. (2007). Biological, life course, and cross-cultural studies all point toward the value of dimensional and developmental ratings in the classification of psychosis. Schizophrenia Bulletin, 33, 868–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton W. W., Romanoski A., Anthony J. C., & Nestadt G. (1991). Screening for psychosis in the general population with a self-report interview. Journal of Nervous and Mental Disease, 179, 689–693. [DOI] [PubMed] [Google Scholar]
- Fenigstein A., & Vanable P. A. (1992). Paranoia and self-consciousness. Journal of Personality and Social Psychology, 62, 129–138. [DOI] [PubMed] [Google Scholar]
- Fine C., Gardner M., Craigie J., & Gold I. (2007). Hopping, skipping or jumping to conclusions? Clarifying the role of the JTC bias in delusions. Cognitive Neuropsychiatry, 12, 46–77. [DOI] [PubMed] [Google Scholar]
- Fornells-Ambrojo M., Barker C., Swapp D., Slater M., Antley A., & Freeman D. (2008). Virtual reality and persecutory delusions: Safety and feasibility. Schizophrenia Research, 104, 228–236. [DOI] [PubMed] [Google Scholar]
- Frecon E., Smith G., Steed A., Stenius M., & Stahl O. (2001). An overview of the COVEN platform. Presence-Teleoperators and Virtual Environments, 10, 109–127. [Google Scholar]
- Freeman D. (2007). Suspicious minds: The psychology of persecutory delusions. Clinical Psychology Review, 27, 425–457. [DOI] [PubMed] [Google Scholar]
- Freeman D. (2008). Studying and treating schizophrenia using virtual reality (VR): A new paradigm. Schizophrenia Bulletin, 34, 605–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman D., Bentall R., & Garety P. A. (Eds.). (2008). Persecutory delusions: Assessment, theory and treatment. Oxford, England: Oxford University Press. [Google Scholar]
- Freeman D., & Freeman J. (2008). Paranoia: The 21st century fear. Oxford, England: Oxford University Press. [Google Scholar]
- Freeman D., Freeman J., & Garety P. (2008). Overcoming paranoid and suspicious thoughts. New York, NY: Basic Books. [Google Scholar]
- Freeman D., & Garety P. A. (1999). Worry, worry processes and dimensions of delusions: An exploratory investigation of a role for anxiety processes in the maintenance of delusional distress. Behavioural & Cognitive Psychotherapy, 27, 47–62. [Google Scholar]
- Freeman D., & Garety P. A. (2000). Comments on the content of persecutory delusions: Does the definition need clarification? British Journal of Clinical Psychology, 39, 407–414. [DOI] [PubMed] [Google Scholar]
- Freeman D., Garety P. A., Bebbington P., Slater M., Kuipers E., Fowler D., . . . & Dunn G. (2005). The psychology of persecutory ideation: II. A virtual reality experimental study. Journal of Nervous and Mental Disease, 193, 309–315. [DOI] [PubMed] [Google Scholar]
- Freeman D., Garety P. A., & Kuipers E. (2001). Persecutory delusions: Developing the understanding of belief maintenance and emotional distress. Psychological Medicine, 31, 1293–1306. [DOI] [PubMed] [Google Scholar]
- Freeman D., Garety P. A., Kuipers E., Fowler D., & Bebbington P. E. (2002). A cognitive model of persecutory delusions. British Journal of Clinical Psychology, 41, 331–347. [DOI] [PubMed] [Google Scholar]
- Freeman D., Gittins M., Pugh K., Antley A., Slater M., & Dunn G. (2008). What makes one person paranoid and another person anxious? The differential prediction of social anxiety and persecutory ideation in an experimental situation. Psychological Medicine, 38, 1121–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman D., Pugh K., Antley A., Slater M., Bebbington P., Gittins M., . . . & Garety P. A. (2008). A virtual reality study of paranoid thinking in the general population. British Journal of Psychiatry, 192, 258–263. [DOI] [PubMed] [Google Scholar]
- Freeman D., Pugh K., & Garety P. (2008). Jumping to conclusions and paranoid ideation in the general population. Schizophrenia Research, 102, 254–260. [DOI] [PubMed] [Google Scholar]
- Freeman D., Pugh K., Green C., Valmaggia L., Dunn G., & Garety P. (2007). A measure of state persecutory ideation for experimental studies. Journal of Nervous and Mental Disease, 195, 781–784. [DOI] [PubMed] [Google Scholar]
- Freeman D., Slater M., Bebbington P. E., Garety P. A., Kuipers E., Fowler D., . . . & Vinayagamoorthy V. (2003). Can virtual reality be used to investigate persecutory ideation? Journal of Nervous and Mental Disease, 191, 509–514. [DOI] [PubMed] [Google Scholar]
- Garety P. A., & Freeman D. (1999). Cognitive approaches to delusions: A critical review of theories and evidence. British Journal of Clinical Psychology, 38, 113–154. [DOI] [PubMed] [Google Scholar]
- Garety P. A., Freeman D., Jolley S., Dunn G., Bebbington P. E., Fowler D., . . . & Dudley R. (2005). Reasoning, emotions, and delusional conviction in psychosis. Journal of Abnormal Psychology, 114, 373–384. [DOI] [PubMed] [Google Scholar]
- Green C., Freeman D., Kuipers E., Bebbington P., Fowler D., Dunn G., & Garety P. A. (2008). Measuring ideas of persecution and reference: The Green et al. Paranoid Thought Scales (G-PTS). Psychological Medicine, 38, 101–111. [DOI] [PubMed] [Google Scholar]
- Janssen I., Versmissen D., Campo J. A., Myin-Germeys I., van Os J., & Krabbendam L. (2006). Attribution style and psychosis. Psychological Medicine, 36, 771–778. [DOI] [PubMed] [Google Scholar]
- Kendler K. S., & Campbell J. (2009). Interventionist causal models in psychiatry. Psychological Medicine, 39, 881–887. [DOI] [PubMed] [Google Scholar]
- Kennedy R. S., Lane N. E., Berbaum K. S., & Lilienthal M. G. (1993). Simulator Sickness Questionnaire: An enhanced method for quantifying simulator sickness. International Journal of Aviation Psychology, 3, 203–220. [Google Scholar]
- Krueger R. F., Markon K. E., Patrick C. J., Benning S. D., & Kramer M. D. (2007). Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology, 116, 645–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond P. F., & Lovibond S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33, 335–343. [DOI] [PubMed] [Google Scholar]
- Martin J. A., & Penn D. L. (2001). Brief report: Social cognition and subclinical paranoid ideation. British Journal of Clinical Psychology, 40, 261–265. [DOI] [PubMed] [Google Scholar]
- McHugo G. J., Caspi Y., Kammerer N., Mazelis R., Jackson E. W., Russell L., . . . & Kimerling R. (2005). The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence. Journal of Behavioural Health Services and Research, 32, 113–127. [DOI] [PubMed] [Google Scholar]
- Meyer T. J., Miller M. L., Metzger R. L., & Borkovec T. D. (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research & Therapy, 28, 487–495. [DOI] [PubMed] [Google Scholar]
- Miller G. A., & Chapman J. P. (2001). Misunderstanding analysis of covariance. Journal of Abnormal Psychology, 110, 40–48. [DOI] [PubMed] [Google Scholar]
- Myin-Germeys I., Krabbendam L., & van Os J. (2003). Continuity of psychotic symptoms in the community. Current Opinion in Psychiatry, 16, 443–449. [Google Scholar]
- Page A. C., Hooke G. R., & Morrison D. L. (2007). Psychometric properties of the Depression Anxiety Stress Scales (DASS) in depressed clinical samples. British Journal of Clinical Psychology, 46, 283–297. [DOI] [PubMed] [Google Scholar]
- Poulton R., Caspi A., Moffitt T. E., Cannon M., Murray R., & Harrington H. (2000). Children’s self-reported psychotic symptoms and adult schizophreniform disorder. Archives of General Psychiatry, 57, 1053–1058. [DOI] [PubMed] [Google Scholar]
- Sanchez-Vives M. V., & Slater M. (2005). From presence to consciousness through virtual reality. Nature Reviews Neuroscience, 6, 332–339. [DOI] [PubMed] [Google Scholar]
- Shadish W. R., Cook T. D., & Campbell D. T. (2002). Experimental and quasi-experimental designs for generalized causal inference. Boston, MA: Houghton Mifflin. [Google Scholar]
- SPSS. (2006). SPSS base 15.0 user’s guide. Chicago, IL: Author. [Google Scholar]
- Startup H. M., & Erickson T. M. (2006). The Penn State Worry Questionnaire. In Davey G. & Wells A. (Eds.), Worry and its psychological disorders (pp. 101–120). Chichester, England: Wiley. [Google Scholar]
- Startup H., Freeman D., & Garety P. A. (2007). Persecutory delusions and catastrophic worry in psychosis: Developing the understanding of delusion distress and persistence. Behaviour Research and Therapy, 45, 523–537. [DOI] [PubMed] [Google Scholar]
- StataCorp. (2008). Stata statistical software: Release 10.0. College Station, TX: Stata Corporation. [Google Scholar]
- Taylor R. M. II, Hudson T. C., Seeger A., Weber H., Juliano J., & Helser A. T. (2001). VRPN: A device-independent, network-transparent VR peripheral system. In Proceedings of the ACM Symposium on Virtual Reality Software and Technology (pp. 55–61). New York, New York: ACM. doi:10.1145/505008.505019 [Google Scholar]
- Valmaggia L., Freeman D., Green C., Garety P., Swapp D., Antley A., . . . & McGuire P. (2007). Virtual reality and paranoid ideations in people with an ’at risk mental state’ for psychosis. British Journal of Psychiatry, 191, s63–s68. [DOI] [PubMed] [Google Scholar]
- Van Dael F., Versmissen D., Janssen I., Myin-Germeys I., van Os J., & Krabbendam L. (2006). Data gathering: Biased in psychosis? Schizophrenia Bulletin, 32, 341–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J., Hanssen M., Bijl R. V., & Ravelli A. (2000). Strauss (1969) revisited: A psychosis continuum in the general population. Schizophrenia Research, 45, 11–20. [DOI] [PubMed] [Google Scholar]
- van Os J., Linscott R. J., Myin-Germeys I., Delespaul P., & Krabbendam L. (2009). A systematic review and meta-analysis of the psychosis continuum. Psychological Medicine, 39, 179–195. [DOI] [PubMed] [Google Scholar]
- van Os J., & Verdoux H. (2003). Diagnosis and classification of schizophrenia: Categories versus dimensions, distributions versus disease. In Murray R. M., Jones P. B., Susser E., van Os J., & Cannon M. (Eds.), The epidemiology of schizophrenia (pp. 364–410). Cambridge, England: Cambridge University Press. [Google Scholar]
- Vermissen D., Janssen I., Myin-Germeys I., Mengelers R., Campo J. A., van Os J., & Krabbendam L. (2008). Evidence for a relationship between mentalising deficits and paranoia over the psychosis continuum. Schizophrenia Research, 99, 103–110. [DOI] [PubMed] [Google Scholar]
- Wechsler D. (2001). Wechsler Test of Adult Reading: Manual. San Antonio, TX: Harcourt Assessment. [Google Scholar]
- Wolfe J., & Kimerling R. (1997). Gender issues in the assessment of posttraumatic stress disorder. In Wilson J. & Keane T. (Eds.), Assessing psychological trauma and PTSD (pp. 192–238). New York, NY: Guilford Press. [Google Scholar]
- World Health Organization. (1992). SCAN: Schedules for Clinical Assessment in Neuropsychiatry. Geneva, Switzerland: Author. [Google Scholar]