Abstract
The authors respond to the article by H. F. Coelho, P. H. Canter, and E. Ernst (2007),A. T. Beck, C. H. Ward, M. Mendelson, J. Mock, & J. Erbaugh, 1961) after treatment.
Keywords: mindfulness, MBCT, depression, treatment studies, intragroup correlation (IGC)
Mindfulness-based cognitive therapy (MBCT) was developed as a manualized group-skills training program that would address vulnerability between episodes of recurrent major depression (Segal, Williams, & Teasdale, 2002; Williams, Teasdale, Segal, & Kabat-Zinn, 2007). It was derived from a model of cognitive vulnerability to depressive relapse (Segal, Williams, Teasdale, & Gemar, 1996; Teasdale, 1988; Teasdale, Segal, & Williams, 1995); according to the model, individuals who have previously experienced episodes of major depression differ from those who have not in the patterns of negative thinking that become activated in mildly depressed moods. For these individuals, small downward mood shifts are more likely to produce recurrence, because they activate patterns of self-denigrating depressogenic thinking similar to those that prevailed in preceding episodes.
MBCT integrates aspects of cognitive–behavioral therapy for depression (Beck, Rush, Shaw, & Emery, 1979) into the mindfulness-based stress reduction (MBSR) program developed by Kabat-Zinn (1990). MBCT teaches patients who are currently in remission from recurrent major depression to become more aware of, and to relate differently to, their thoughts, feelings, and bodily sensations. For example, patients are encouraged to relate to thoughts and feelings as passing events in the mind, rather than to identify with them or treat them as accurate representations of reality. MBCT teaches skills that allow individuals to disengage from habitual (“automatic”) dysfunctional cognitive routines, in particular, depression-related ruminative thought patterns, as a way to reduce future risk of relapse and recurrence of depression.
The article by Coelho, Canter, and Ernst (2007) gave a good account of the current empirical status of this approach and highlighted the two main randomized controlled trials (RCTs). These trials (Ma & Teasdale, 2004; Teasdale et al., 2000) reported that, for patients with a history of three or more episodes, MBCT substantially reduced the rate of recurrence over the following 12 months.
Coelho et al. (2007) rightly pointed out that many important questions were left unanswered by these trials. It could be argued that the timing of their review of MBCT was premature. Despite recent promising evidence (Barnhofer et al., 2007; Kenny & Williams, 2007; Kingston, Dooley, Bates, Lawlor, & Malone, 2007), there simply have not yet been sufficient randomized trials for us to form a definitive view of the efficacy of MBCT. Specifically, if one applies the principles of Onken and Rounsaville (Onken, Blaine, & Battjes, 1997; Rounsaville, Carroll, & Onken, 2001), who describe a model for research on the development of novel behavioral therapies, one sees that MBCT remains a rather new treatment that has not had sufficient time to accrue a sufficient body of work to provide all the nuances expected by Coelho et al. The Onken and Rounsaville approach for developing novel treatments involves three progressive stages that guide the process of treatment development in a manner informed by ever more complex and rigorous tests of the novel protocol. At Stage 1, investigators conduct pilot/feasibility studies, manual writing, training program development, and adherence/fidelity measure development. This process, described in detail in Segal et al. (2002) and Segal, Teasdale, Williams, & Gemar (2002), took place during the early 1990s.
Stage 2 consists of RCTs that evaluate efficacy and can include investigation of mechanisms of action. The first trial was done between 1995 and 1998 and was published in 2000; the second trial was published in 2004. Stage 3 research focuses on issues such as treatment transportability and generalizability. Several trials are in progress but have not yet been concluded. The Onken and Rounsaville model for behavior therapies offers a blueprint for treatment development that is widely accepted (e.g., at the National Institutes of Health) and that guides the development of evidence-based treatments.
With these criteria in mind, how can we best respond to the points raised at this stage by Coelho et al. (2007)? In this article, we seek to do three things. First, we briefly clarify the existing trial data to answer the questions raised. Second, we discuss in more detail the issues that arise for those designing the next generation of trials. Third, in the light of Onken and Rounsaville's criteria for Stage 3, we show that there is at least one more important issue that this domain of research needs to address in the future: the problems that accompany use of traditional statistical analyses when patients are treated in groups and that, thus, may influence each other's outcomes.
Issues in Trials of MBCT
Details of Previous Trials
Coelho et al. (2007) mentioned lack of clarity in randomization procedures in Teasdale et al. (2000) and Ma and Teasdale (2004). These studies gave the following details:
Randomization involved treatment sites faxing patient initials, date of birth, gender, date of assessment, and details of number and recency of previous episodes of depression to a central independent allocator. Information was sent for groups of eligible patients at a time. The central allocator randomly allocated patients to treatment condition, gave each a study number, and faxed the allocations and study numbers back to treatment sites. (Teasdale et al., 2000, p. 617)
Randomization of patients to treatment condition was by a statistician, who was not part of the research team, on receipt of the participant's date of birth, gender, date of assessment, number of previous episodes of depression, and severity of last episode. (Ma & Teasdale, 2004, p. 32)
Thus, although the first of these trials began before the original publication of the CONSORT guidelines for the conduct and reporting of RCTs (Begg et al., 1996; updated by Moher, Schulz, & Altman, 2001), both Teasdale et al. (2000) and Ma and Teasdale (2004) kept random allocation concealed from trial participants and staff before recruitment, a key requirement of these guidelines.
Second, Coelho et al. (2007) wondered whether more data on mood variables (e.g., Beck Depression Inventory [BDI] scores; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) would have been beneficial. Such data might, for instance, indicate that participants who were allocated to the control arm that received “treatment as usual” (TAU) suffered from “resentful demoralization” (Cook & Campbell, 1979) at not receiving treatment. We have therefore checked the mean BDI scores for the 66 participants allocated to TAU (in trials of both Teasdale et al., 2000, and Ma & Teasdale, 2004), who had at least three previous episodes and valid BDI scores at each follow-up point. Their scores were as follows: baseline (M = 11.8, SD = 8.5), immediate posttreatment (or equivalent; M = 12.1, SD = 8.1), and final follow-up (M = 11.9, SD = 9.5). Repeated-measures analysis showed no significant differences between these time points (p = .95). Thus, there is no evidence that the mood of those not receiving treatment worsened during the trial. Although we cannot rule out the possibility that resentful demoralization prevented an improvement that would otherwise have occurred in the control group, it is very unlikely to account for the large treatment effect on both BDI and time to recurrence described later in this article. We are grateful to Coelho et al. for the opportunity to return to these data to clarify this point.
What Control Treatment?
Coelho et al. (2007) rightly pointed out that trials of MBCT have compared the effects of adding MBCT to TAU only with the effects of TAU alone. So, these trials have not been able to control either for the effects of the considerable psychological education component of MBCT or for nonspecific factors, such as group affiliation and therapist support. As Teasdale et al. (2000, p. 617) mentioned this limitation explicitly, Coelho et al. are right to advocate that future RCTs need to compare MBCT not only with TAU but with a group-based therapy that has equal plausibility and acceptability to patients.
When one selects the appropriate control treatment, several choices are available. One option is comparison of the MBCT package with an effective group-based package (e.g., group-based CBT) that requires comparable attendance and homework. This option has the advantage of comparing the treatment of interest with a practical alternative but has two disadvantages. First, if one aims to prevent recurrence, it is important to recognize that many comparable treatments are intended to treat acute depression rather than to prevent relapse and thus may have smaller effects on relapse (Bockting et al., 2005). Second, whatever the outcome of such a comparison, it could not yield an unambiguous answer to the scientific question we wish to answer: Which component of relapse-prevention treatment is critical to success? Another option is to assess mediating variables (Kraemer, Wilson, Fairburn, & Agras, 2002), but this approach suffers from multicollinearity and thus ambiguity.
A better choice than either practical alternatives or mediating variables is use of a “dismantling” paradigm, in which the comparison treatment is identical to the experimental treatment except for a critical component (cf. Jacobson et al., 1996). Given that the most complex aspect of MBCT is intensive training in meditation, in a dismantling design, the control treatment should follow the group format of MBCT but should not include training in meditation. This is the design we have chosen for our next trial of MBCT, with recurrently depressed patients who are suicidal. The control treatment is essentially the psychological education component of MBCT; it will include the same number and length of sessions as does MBCT, thus controlling for group and therapist support, but will incorporate short educational presentations followed by discussions instead of meditation training. Teaching will cover learning about depression, links between thoughts and feelings, and self-monitoring these links for signs of impending recurrence. This design will enable us to answer the key question: How much any reduction in recurrence is attributable to training in meditation rather than to group attendance, therapist support, and psychoeducation. If we find no difference between psychoeducation and MBCT and both are more effective than is TAU, we shall know that meditation is unnecessary.
However, all these designs require compromise. For example, though psychoeducation includes self-monitoring and homework, the dismantling design does not ensure equal homework, as meditation demands more homework. This design does not, therefore, allow us to test the extent to which homework per se adds to the effectiveness of treatment. Though other forms of homework, such as exercise or relaxation, could substitute for meditation, this substitution would create a new package that, like existing packages, cannot identify which component is essential for reducing relapse. If MBCT is found to be more effective than is psychoeducation, therefore, further research will be needed to test whether any homework would have enhanced effectiveness.
The Problem of Correlated Data in Group-Based Interventions
Onken and Rounsaville have shown that a novel treatment approach requires a staged approach. Those conducting treatment research proceed by ensuring firm foundations before progressing to the next stage. That is why it is beneficial to see whether, as Coelho et al. (2007) have allowed us to do, even the foundations are secure. However, one element of the foundational work that was not addressed in the existing trials, nor by Coelho et al., is potentially as or more threatening than are the issues they raise: the problem of intragroup dependency. We raise this possibility here, because it needs to be taken into account in the next round of treatment research on MBCT.
Baldwin, Murray, and Shadish (2005) showed that, when treatments such as CBT are administered in groups, the individuals who receive the treatment may influence each other and thus create dependencies between observations. One or two very depressed or unmotivated participants could aggravate outcomes across their group. By contrast, one or two very motivated individuals could facilitate progress by their entire group. Despite this potential dependence, virtually all of the trials reviewed by Baldwin et al. (2005) involved statistical tests that treat each participant as an individual, as if his or her outcomes were independent of those of other participants. Both trials of MBCT also treated each participant as an individual for statistical analysis. However, intragroup dependence violates the assumption of most traditional statistical tests that observations are independent. Analyses that ignore the resulting inflation in variance risk underestimating the standard error of the treatment effect. The intragroup correlation (IGC) measures the extent to which group membership has created such dependency between observations. As Baldwin et al. (2005) pointed out, IGC does not alter the underlying data but increases the chance of Type 1 error when we claim to have found statistical significance. The trials of MBCT may not have found a significant effect of MBCT on relapse and recurrence, after all.
To address these issues, we returned to the data of Teasdale et al. (2000) and Ma and Teasdale (2004) to (a) estimate IGCs; (b) reanalyze those data by the unbiased statistical technique of multilevel modeling; (c) where possible, combine results from the two studies; and (d) reassess the claim that MBCT reduces the risk of relapse in participants with three or more previous episodes.
Reanalysis of MBCT Trials
We have reanalyzed data from both Teasdale et al. (2000) and Ma and Teasdale (2004). These trials recruited participants in eight and four cohorts, respectively, and allocated them to groups (MBCT + TAU vs. TAU alone) within each cohort. However, in the original analyses, cohorts were ignored; the analyses used simple comparisons, based on chi-square tests, odds ratios (ORs), and Cox regression, for relapse and t tests for the BDI. We have responded to Baldwin et al. (2005) by including cohort and group effects. We have combined findings for outcomes that were identical in both papers, after checking for homogeneity and goodness of fit across trials. In addition, we have improved the precision of comparisons by adjusting measured outcomes for baseline BDI.
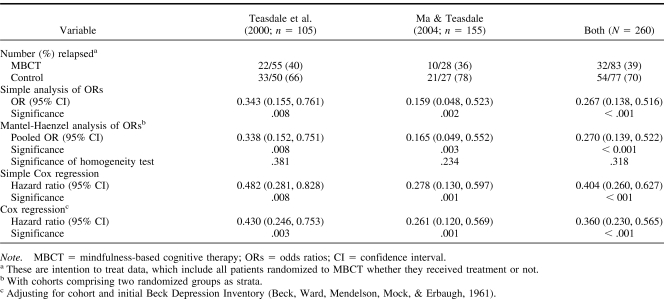
In Table 1, we have allowed for cohort by pooling separate ORs for each cohort and by testing whether ORs varied between cohorts. This approach made little difference to the estimated OR, the associated confidence interval (CI), or the significance of the result. Furthermore, the homogeneity test showed that the OR was consistent between cohorts. In other words, MBCT had essentially the same effect in each cohort. The original articles also analyzed survival (“time to relapse”) by Cox regression. We refined this analysis by including both a cohort term and the initial BDI in the model. Although initial BDI contributed significantly to all three Cox regression models and strengthened the effect of MBCT, there was no significant cohort effect. Indeed, cohort contributed less than was expected by chance, in the equivalent of a negative IGC. The analyses in Table 1 were possible because each MBCT group was selected at random from a given cohort, with the unselected control participants within that cohort forming a matched group. Thus, the effect of MBCT consistently remained significant in all reanalyses and achieved the highest level of significance and the narrowest CIs in the combined analysis.
Table 1. Relapse at 12 Months (Binary Outcome and Cox Regressions) by Trial.
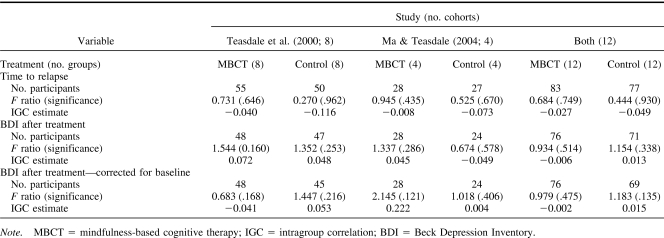
Although each cohort comprises an MBCT group and a control group, we have estimated separate IGCs for each type of group (see Table 2). Homogeneity within control groups is likely to be demographic in origin (Cause A), but MBCT groups may be more homogeneous if groups differed in their effectiveness (Cause B) or if participants tended to follow the responses of others (Cause C). In both studies and the combined analysis, however, all IGCs for time to relapse were negative, which makes all three causes unlikely. Although most but not all IGCs for BDI were positive but generally small, there was no consistent tendency for IGCs to be larger in either MBCT groups or control groups. Furthermore, no IGC was significantly greater or less than zero. Thus, the data in Table 2 show no evidence of any intragroup dependency.
Table 2. Time to Relapse and Beck Depression Inventory After Treatment: Comparison Between Randomized Groups.
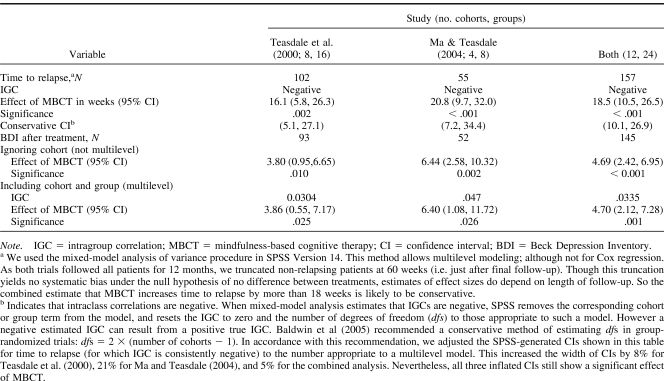
Against this reassuring background, Table 3 shows the effect of MBCT on BDI after treatment (adjusted for baseline BDI, without and with consideration of cohort effects). These analyses remained significant but showed increased significance levels and wider confidence intervals, as we expected from small positive estimates of IGC. Nevertheless, the combined analyses are still highly significant and confirmed that MBCT improves BDI by 4.7 points (95% CI, 2.1–7.3). Table 3 also includes the reanalysis of time to relapse, which showed that MBCT increases the average time to relapse by at least 18 weeks (95% CI, 10–27 weeks).
Table 3. Time to Relapse and Beck Depression Inventory After Treatment: Multilevel Model With Analysis of Covariance to Adjust for Baseline BDI.
Conclusions and Recommendations
Coelho et al. (2007) were right to propose that trials of MBCT should be rigorous in the choice of control treatments, randomization procedures, and methods of analysis. Baldwin et al. (2005) were right to criticize the statistical analysis of most trials of group therapy for the use of traditional methods that assume independent observations.
We have shown how randomization in accordance with the CONSORT guidelines (Moher et al., 2001) and use of a dismantling design can address the issues raised by Coelho et al. (2007). In response to Baldwin et al. (2005), we have used multilevel modeling to reanalyze participants within their groups and have combined the findings of both of the main MBCT trials, in what is sometimes described as a meta-analysis. We found that the IGC for time to relapse was always negative and that the IGC for the BDI after treatment was generally small, though positive. We conclude that the attempt by Baldwin et al. (2005) to correct published analyses by simulating intraclass correlation coefficients of up to .3 was unduly pessimistic.
More important, we conclude that MBCT reduces the percentage of participants who relapse within 12 months from 70% to 39%, increases the average time to relapse by at least 18 weeks, and decreases the BDI score after treatment by nearly 5 points (all statistically significant at the 0.1% level). In short, our rigorous reanalysis of both trials together has strengthened all of the original findings.
We recommend that those planning trials of group-based therapy in general and class-based mindfulness training in particular should take account of IGC. In designing these trials, they should seek to estimate IGC, the resulting variance inflation, and, thus, the necessary sample size. Those implementing such trials should seek to maximize the intrinsic therapeutic effect of group work while they seek to minimize group effects on evaluation, in particular by keeping individual responses personal and confidential. In analyzing such trials, they should use multilevel models. In reporting such trials, they should follow the extension of the CONSORT statement to cluster randomized trials (Campbell, Elbourne, & Altman, 2004).
Acknowledgments
We thank the Wellcome Trust for its support of this research through Grant GR067797 and Thorsten Barnhofer for his help with this article.
References
- Baldwin S. A., Murray D. M., & Shadish W. R. (2005). Empirically supported treatments or Type I errors? A revaluation of group-administered treatments on the empirically supported treatments list. Journal of Consulting and Clinical Psychology, 73, 924–935. [DOI] [PubMed] [Google Scholar]
- Barnhofer T., Duggan D., Crane C., Hepburn S., Fennell M., & Williams J. M. G (2007). Effects of meditation on frontal alpha asymmetry in previously suicidal patients NeuroReport, 18, 707–712. [DOI] [PubMed] [Google Scholar]
- Beck A. T., Rush A. J., Shaw B. F., & Emery G. (1979). Cognitive therapy of depression. New York: Guilford. [Google Scholar]
- Beck A. T., Ward C. H., Mendelson M., Mock J., & Erbaugh J. (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571. [DOI] [PubMed] [Google Scholar]
- Begg C. B., Cho M. K., Eastwood S., Horton R., Moher D., Olkin I., et al. (1996). Improving the quality of reporting of randomized controlled trials: The CONSORT statement. Journal of the American Medical Association, 276, 637–639. [DOI] [PubMed] [Google Scholar]
- Bockting C. L. H., Schene A. H., Spinhoven P., Koeter M. W. J., Wouters L. F., Huyser J., et al. (2005). Preventing relapse/recurrence in recurrent depression with cognitive therapy: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 73, 647–657. [DOI] [PubMed] [Google Scholar]
- Campbell M. K., Elbourne D. R., & Altman D. G. (2004). CONSORT statement: Extension to cluster randomised trials. British Medical Journal, 328, 702–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coelho H. F., Canter P. H., & Ernst E. (2007). Mindfulness-based cognitive therapy: Evaluating current evidence and informing future research. Journal of Consulting and Clinical Psychology, 75, 1000–1005. [DOI] [PubMed] [Google Scholar]
- Cook T. D., & Campbell D. T. (1979). Quasi-experimental evaluation: Design issues for field settings. Boston: Houghton-Mifflin. [Google Scholar]
- Jacobson N. S., Dobson K. S., Truax P. A., Addis M. E., Koerner K., Gollan J. K., et al. (1996). A component analysis of cognitive–behavioral treatment for depression. Journal of Consulting and Clinical Psychology, 64, 295–304. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. (1990). Full catastrophe living: How to cope with stress, pain and illness using mindfulness meditation. New York: Dell. [Google Scholar]
- Kenny M., & Williams J. M. G. (2007). Treatment-resistant depressed patients show a good response to mindfulness-based cognitive therapy. Behaviour Research and Therapy, 45, 617–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingston T., Dooley B., Bates A., Lawlor E., & Malone K. (2007). Mindfulness-based cognitive therapy for residual depressive symptoms. Psychology & Psychotherapy, 80, 193–203. [DOI] [PubMed] [Google Scholar]
- Kraemer H. C., Wilson T., Fairburn C. G., & Agras W. S. (2002). Mediators and moderators of treatment effects in randomized controlled trials. Archives of General Psychiatry, 59, 877–883. [DOI] [PubMed] [Google Scholar]
- Ma S. H., & Teasdale J. D. (2004). Mindfulness-based cognitive therapy for depression: Replication and exploration of differential relapse prevention effects. Journal of Consulting and Clinical Psychology, 72, 31–40. [DOI] [PubMed] [Google Scholar]
- Moher D., Schulz K. F., & Altman D. G. (2001). The CONSORT statement: Revised recommendations for improving the quality of parallel-group randomized trials. Lancet, 357, 1191–1194. [PubMed] [Google Scholar]
- Onken L. S., Blaine J. D., & Battjes R. (1997). Behavioral therapy research: A conceptualization of a process. In Henggeler S. W. & Amentos R. (Eds.), Innovative approaches from difficult to treat populations (pp. 477–485). Washington, DC: American Psychiatric Press. [Google Scholar]
- Rounsaville B. J., Carroll K. M., & Onken L. S. (2001). A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science and Practice, 8, 133–142. [Google Scholar]
- Segal Z. V., Teasdale J. D., Williams J. M., & Gemar M. C. (2002). The Mindfulness-Based Cognitive Therapy Adherence Scale: Interrater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology and Psychotherapy, 9, 131–138. [Google Scholar]
- Segal Z. V., Williams J. M. G., & Teasdale J. D. (2002). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford. [Google Scholar]
- Segal Z. V., Williams J. M. G., Teasdale J. D., & Gemar M. (1996). A cognitive science perspective on kindling and episode sensitization in recurrent affective disorder. Psychological Medicine, 26, 371–380. [DOI] [PubMed] [Google Scholar]
- Teasdale J. D. (1988). Cognitive vulnerability to persistent depression. Cognition and Emotion, 2, 247–274. [Google Scholar]
- Teasdale J. D., Segal Z., & Williams J. M. G. (1995). How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help. Behaviour Research and Therapy, 33, 25–39. [DOI] [PubMed] [Google Scholar]
- Teasdale J. D., Segal Z. V., Williams J. M. G., Ridgeway V. A., Soulsby J. M., & Lau M. A. (2000). Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. Journal of Consulting and Clinical Psychology, 68, 615–623. [DOI] [PubMed] [Google Scholar]
- Williams J. M. G., Teasdale J. D., Segal Z. V., & Kabat-Zinn J. (2007). The mindful way through depression: Freeing yourself from chronic unhappiness. New York: Guilford. [Google Scholar]